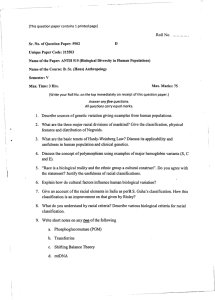
Journals of Gerontology: Social Sciences cite as: J Gerontol B Psychol Sci Soc Sci, 2020, Vol. 75, No. 9, 1937–1950 doi:10.1093/geronb/gbz068 Advance Access publication June 21, 2019 Original Article Death by a Thousand Cuts: Stress Exposure and Black– White Disparities in Physiological Functioning in Late Life Courtney Boen, MPH, PhD* Department of Sociology, Population Studies Center, and Population Aging Research Center, University of Pennsylvania, Philadelphia. *Address correspondence to: Courtney Boen, MPH, PhD, Department of Sociology, Population Studies Center, and Population Aging Research Center, University of Pennsylvania, 232 McNeil Building, 3718 Locus Walk, Philadelphia, PA 19104-6299. E-mail: cboen@sas.upenn.edu Received: September 24, 2018; Editorial Decision Date: May 20, 2019 Decision Editor: Deborah Carr, PhD Abstract Objectives: This paper investigates Black–White differences in stress—including diverse measures of chronic, acute, discrimination-related, and cumulative stress exposure—and examines whether race differences in these stress measures mediate Black–White disparities in C-reactive protein (CRP) and metabolic dysregulation in later life. Methods: Using data from the Health and Retirement Study (HRS) (2004–2012), this study uses stepwise ordinary least squares (OLS) regression models to examine the prospective associations between multiple stressors—including traumatic and stressful life events, financial strain, chronic stress, everyday and major life discrimination, and measures of cumulative stress burden—and CRP and metabolic dysregulation. Mediation analyses assessed the contribution of stress exposure to Black–White disparities in the outcomes. Results: Blacks experienced more stress than Whites across domains of stress, and stress exposure was strongly associated with CRP and metabolic dysregulation. Race differences in financial strain, everyday and major life discrimination, and cumulative stress burden mediated Black–White gaps in the outcomes, with measures of cumulative stress burden mediating the greatest proportion of the racial disparities. Discussion: The “thousand cuts” that Blacks experience from their cumulative stress exposure across domains of social life throughout the life course accelerate their physiological deterioration relative to Whites and play a critical role in racial health disparities at older ages. Keywords: Life course, Physiological functioning, Racial health disparities, Stress Research documents stark Black–White health disparities from mid through late life, whereby Blacks in the United States experience earlier onset of disease, greater severity of illness, and poorer survival rates than Whites (Williams, Mohammed, Leavell, & Collins, 2010). Because of their positioning in both the social class and racial hierarchies, Blacks in the United States are exposed to greater levels of material deprivation (Boen, 2016) and report higher levels of related psychosocial stress (Turner & Avison, 2003) than Whites. Given documented links between psychosocial stress exposure and health (Cohen et al., 2012; Thoits, 2010), scholars hypothesize Blacks’ cumulative exposure to stressors across the life course may play an essential role in racial health inequality (Ferraro & Shippee, 2009; Geronimus et al., 2010; Goosby, Straley, & Cheadle, 2017; Strenthal, Slopen, & Williams, 2011; Turner, 2013; Williams, Yu, Jackson, & Anderson, 1997). Despite a growing body of research in this area, critical gaps in our understanding of the role of stress exposure in the production of racial health inequality at older ages remain. First, most studies assess the associations between single domains of stress—such as discrimination—and © The Author(s) 2019. Published by Oxford University Press on behalf of The Gerontological Society of America. All rights reserved. For permissions, please e-mail: journals.permissions@oup.com. 1937 1938 health, leaving questions about whether and how race differences in the accumulation of stress exposure across domains of social life are implicated in Black–White health gaps at older ages. Few studies incorporate measures of cumulative life course stress exposure—including diverse indicators of acute, chronic, discrimination-related, and total stress burden—which may underestimate the role of stress in health inequality at older ages. Second, while studies have examined how stress relates to single indicators of disease or self-reported health status, fewer assess how stress exposure impacts multiple markers of physiological functioning, which restricts understanding of the social and biological processes contributing to disparities in disease emergence and progression in later life. Further, because Blacks are less likely than Whites to receive a diagnosis (Williams & Jackson, 2005), the use of disease outcomes in studies of racial health inequality may be particularly worrisome, as it risks underestimation of both the magnitude of Black–White health gaps and the role of social exposures in racial health disparities. Finally, few studies of stress and health use longitudinal data or formal mediation techniques to assess the role of stress exposure in population health gaps, which raises concerns about reverse causality and limits understanding of the relative contributions of stressors in racial health disparities. Using nationally representative, longitudinal data from the Health and Retirement Study (HRS), the current study expands understanding of the role of stress in racial health inequality by examining how exposure to multiple forms of stress—including domain-specific measures of acute, chronic, and discrimination-related stress as well as composite indicators of cumulative stress burden—contribute to racial disparities in inflammation and metabolic risk from mid through late life. The study begins by assessing race gaps in physiological functioning and stress exposure. Then, using a combination of prospective OLS regression models and mediation analyses, the study examines the relative contributions of diverse indicators of stress exposure to Black–White disparities in physiological functioning, paying particular attention to the role of cumulative life course stress exposure in the production of racial health inequality at older ages. By expanding the conceptualization and operationalization of “racialized social stress” to include a host of racially patterned psychosocial exposures and assessing the relative contributions of a variety of domain-specific and composite measures of stress to Black– White disparities across multiple physiological systems, this study provides new evidence of how race differences in the accumulation of stress across domains of social life throughout the life span contribute to stark Black–White disparities in physiological functioning in late life. Black–White Disparities in Health and Physiological Function Blacks in the United States experience higher rates of morbidity and mortality from a host of conditions, including Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 cardiovascular diseases (National Center for Health Statistics, 2016). Still, less is known about the physiological processes and social exposures that produce racial disparities in death and disease. Increasingly, scholars have integrated markers of biological risk and physiological dysregulation in studies of population health inequality in order to elucidate the biophysiological processes undergirding social disparities in disease. Indeed, research documents stark racial disparities in biological risk at older ages, including Black–White disparities in inflammatory and metabolic risk (Mitchell & Aneshensel, 2017; Mitchell, Ailshire, & Crimmins, 2019), which may contribute to racial disparities across a host of disease outcomes. Given that biological risk profiles in later life have been linked to the accumulation of psychological, social, and environmental exposures (Ferraro & Shippee, 2009), scholars hypothesize that racial differences in physiological functioning at older ages may reflect race differences in cumulative exposure to racialized risks and opportunities— including psychosocial exposures—across the life course (Geronimus et al., 2010). In particular, research increasingly highlights the critical role of immune function and energy metabolism in shaping health and disease risk (Finch, 2010). Both chronic inflammation—a marker of sustained immune system activation—and metabolic disorders are identified as key pathogenic pathways affecting mortality risk at older ages, particularly from cardiovascular diseases (Yang & Kozloski, 2011), a leading cause of death among older adults. As such, understanding how social exposures shape individual health risk and pattern population-level racial health disparities through inflammatory and metabolic processes can inform prevention efforts aimed at identifying the psychosocial and physiological predecessors of multiple forms of disease, including cardiovascular diseases, from mid through late life (Mitchell & Aneshensel, 2017; Mitchell et al., 2019). The Role of Stress in Racial Health Inequality A large body of literature seeks to understand the social determinants of racial health disparities, with a number of studies indicating that stress may be an important—but largely underestimated—mechanistic pathway underlying Black–White gaps in health (Ferraro & Shippee, 2009; Geronimus et al., 2010; Goosby et al., 2017; Strenthal et al., 2011; Turner, 2013; Williams et al., 1997). More than 40 decades of research document the substantial effects of stress on health (Cohen et al., 2012; Thoits, 2010). Studies on the health consequences of stress typically draw on the stress process model (Pearlin, Menaghan, Lieberman, & Mullan, 1981) to infer the pathways through which stress exposure “gets under the skin” to affect disease risk. In the face of stress, the hypothalamic-pituitary-adrenal axis and sympathetic nervous system respond by secreting hormones to upregulate functioning across physiological systems, including inflammatory and cardiometabolic Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 functioning (McEwen, 2007). While this upregulation in response to immediate threats and infections is necessary to protect health in the short term, repeated activation of the body’s stress response systems results in physiological “exhaustion,” where the bodily mechanisms used to defend against stressors become inefficient and ineffective (Seyle, 1974). Repeated exposure to stress diminishes the ability of physiological systems to downregulate (Cohen et al., 2012), such that they become hypervigilant, operating under “threat levels” even in the absence of an immediate threat. In this way, long term and repeated stress exposure can promote physiological dysregulation and increased disease and mortality risk from a host of causes (Cohen et al., 2012; McEwen, 2007). Research documents that stress exposure is not randomly distributed in the population. Socially disadvantaged groups are exposed to more negative life events and greater levels of chronic strain than advantaged groups (Pearlin, 1999) from birth through late life, in ways that shape the life course patterning of health inequality (Ferraro & Shippee, 2009). With regard to racial health inequities, racism patterns exposure to a variety of stressors, both discrimination-related and more generalized (Pearlin, 1999), in ways that burden people of color with greater lifetime stress burden than Whites. The United States is a racialized social system (Bonilla-Silva, 1997), with racism operating across domains of social life and at the institutional, interpersonal, and internalized levels to shape exposure to risks and opportunities to contribute to the racial patterning of health (Jones, 2000). While most studies on the role of racism in shaping stress exposure and health risk focus on perceived discrimination (Goosby et al., 2017), racism patterns exposure to a host of stressors— both discrimination-related and more generalized—in ways that are linked to United States’s racialized social system. For example, research documents striking Black–White disparities in exposure to the deaths of family members and friends (Umberson et al., 2017) and financial instability and insecurity (Boen, 2016)—disparities in stress exposure that are not captured by studies of perceived racial discrimination. As such, examinations of the ways in which racialized social stress may contribute to population health gaps must consider how living in a racialized social system patterns exposure to a host of psychosocial stressors, both discrimination-related and more generalized, across domains of social life. Gaps in the Literature Taken together, work on the physiological consequences of stress, on the one hand, and the racial patterning of stress exposure, on the other, suggests that Blacks’ greater cumulative exposure to racialized social stress across the life course may contribute to their disproportionate physiological deterioration relative to Whites and play a critical role in producing Black–White disparities across a host 1939 of disease outcomes (Brown & Hargrove, 2018; Ferraro & Shippee, 2009; Geronimus et al., 2010; Goosby et al., 2017; Strenthal et al., 2011). Despite a growing body of literature in this area, three critical gaps in the literature remain. First, most studies measure stress exposure use one or two indicators of stress, which suggests that the role of stress in Black–White disparities in health and aging has been underestimated (Turner, 2013). As discussed, while a growing body of literature on the role of stress in racial health disparities considers the health consequences of racial discrimination (Goosby et al., 2017), both discrimination and more generalized indicators of social stress are patterned by race and associated with health. As such, failure to include multiple dimensions of stress exposure in studies of racial health inequality risks underestimating the contribution of stress to racial disparities in health. Further, while evidence suggests that cumulative exposure to social stressors play a role in Black–White health gaps (Brown & Hargrove, 2018; Strenthal et al., 2011), few studies assess how the accumulation of stress across domains throughout the life span contribute to racial health gaps. Insights from cumulative inequality theory (Ferraro & Shippee, 2009) suggest that stressors accumulate across the life course and across domains of social life to produce population health inequality at older age. Consistent with this notion, research by Strenthal and colleagues (2011) and Brown and Hargrove (2018) used count indices of high stress exposure to show that individuals with high exposure across domains of stress had increased health risk. Still, few studies incorporate these cumulative stress measures to more holistically estimate the role of stress in racial health inequality and document the unique and joint contributions of diverse measures of stress exposure to racial disparities in health. Second, most studies of the role of stress exposure in population health inequality use markers of disease (e.g., Strenthal et al., 2011) or self-reported health status (e.g., Brown and Hargrove, 2018) as outcomes, which restricts understanding of how stress exposure impacts a range of biological processes to ultimately impact health and disease risk and contribute to health inequality across a range of outcomes. For one, studies that utilize measures of disease or diagnosis as outcomes risk misclassification error, whereby individuals who do not yet have the disease or have not yet been diagnosed with the disease are classified as “well” (Aneshensel, Rutter, & Lachenbruch, 1991). The misclassification of individuals with high levels of physiological dysregulation as “healthy” could result in an underestimation of the role of stress in shaping individual health and mortality risk, which is a particular concern for studies of racial health gaps given documented disparities in health care access and diagnosis that make Blacks less likely to receive a diagnosis than Whites with similar health profiles (Williams & Jackson, 2005). Further, because studies on stress exposure and health usually rely on indicators of disease, diagnosis, or self-reported health status as outcomes, less is known about how stress exposure affects multiple physiological systems 1940 Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 to predispose individuals to host of poor outcomes (Turner, 2013). Studies that consider the effects of stress on multiple, predisease markers of physiological well-being would be consistent with the nonspecificity hypothesis that guides the stress process model, whereby stress exposure elicits a range of physiological changes that, over time, serve to increase disease risk from a host of causes (Seyle, 1974). Research by Geronimus et al. (2010) suggests that Blacks may experience accelerated physiological deterioration relative to Whites—in a process called “weathering”—due largely to racial differences in social exposures across the life course. Still, more research using multiple predisease markers of physiological well-being is needed, as such studies can elucidate the processes through which cumulative exposure to racialized social stress over the life course “gets under the skin” to accelerate biological aging processes and ultimately shape population patterns of racial disparities in disease risk in old age (Ferraro & Shippee, 2009). Finally, few studies of the relationship between stress and health use longitudinal data or formally test the contribution of stress exposure to population health gaps using mediation analyses and nationally representative data. The use of longitudinal data can reduce concerns about reverse causality and improve causal inference, while the use of mediation analyses with nationally representative samples can provide new knowledge of the relative contributions of various stressors to population-level racial health disparities, which can inform policy and intervention efforts. Data and Methods Aims of the Present Study Measures While research documents race differences in health and physiological risk and provides strong evidence of racial disparities in stress exposure, these two bodies of literature have not been fully integrated to assess whether cumulative stress exposure is a key mechanistic pathway producing race difference in biological aging and physiological functioning in later life. This study uses nationally representative, longitudinal data to assess relative contributions of various measures of stress exposure to Black–White disparities in inflammatory and metabolic risk in mid to late life by addressing four overarching research questions: 1. What is the patterning of Black–White disparities in stress exposure and physiological well-being in late life? 2. How do diverse measures of stress exposure relate to markers of inflammatory and metabolic risk at older ages? 3. Do racial differences in stress exposure account for Black–White disparities in physiological well-being in mid to late life? 4. Do composite measures of cumulative stress exposure, quantified by summing high risk cut off points or by using factor analysis, account for more of the racial gaps in physiological functioning than the domainspecific stressors? Data and Samples Data for this study come from five waves of the HRS, a nationally representative, longitudinal study of adults aged 50 years and older in the United States. The HRS collects information about the well-being of older adults, primarily through the use of in-home interviews. More information about the design of HRS can be found in Heeringa and Connor (1995). The HRS collected blood-based biomarkers on a random half of the sample in 2006, and the other half of the sample provided biomarker data in 2008. These sample respondents were then reinterviewed in 2010 and 2012, respectively, when they again provided biomarker samples. Measures of stress exposure were collected in a leave behind questionnaire conducted every other year starting in 2004, though respondents did not answer questions about stress exposure at every one of these waves. This study uses data from five waves of the HRS that include data on physiological functioning and stress exposure: 2004, 2006, 2008, 2010, and 2012. The analytic samples include Black and White respondents aged 50 years and older with valid sampling weights. Supplementary analyses revealed that the greatest source of missing data among eligible respondents was stress exposure. I use multiple imputation by chained equations (MICE) procedures to adjust for missing stress exposure data (10 multiply imputed data sets). Outcomes This study includes two outcomes from the 2010/2012 waves of the HRS that represent critical markers of health that are strongly predictive of disease risk in later life with documented links to stress exposure. C-reactive protein (CRP), a marker of inflammatory response and immune function, is an acute-phase protein produced by the liver. Elevated levels of circulating CRP indicate systemic inflammation (Finch, 2010). Studies document a relationship between inflammation and health risk, including prospective associations of CRP with higher rates of coronary heart disease and mortality risk (Harris et al., 1999). Because of a skewed distribution, I include CRP as a log-transformed measure. Consistent with previous studies (Yang, Gerken, Schorpp, Boen, & Harris, 2017), I construct a composite measure of metabolic dysregulation, which indicates overall level of metabolic burden using clinical markers. For each individual metabolic marker, I construct a dummy measure where “1” indicates high risk, with cut points for high risk defined by clinical practice (blood pressure: systolic blood pressure > 140 mmHG or diastolic blood pressure > 90 mmHg; Hba1c ≥ 5.7%; waist circumference ≥ 102 cm for males or 88 cm for females; total cholesterol ≥ 240 mg/dL; high-density lipoprotein cholesterol ≤ 40 mg/ Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 dL; and body mass index ≥ 30 kg/m2). I then summed the scores from each of the markers to construct the index of overall metabolic dysregulation, which ranges from 0 (low) to 6 (high). 1941 education (1 = <high school, 2 = high school, 3 = some college, 4 = bachelor’s degree or higher), total household wealth (continuous), total household income (continuous), and marital status (1 = married, 2 = partnered, 3 = separated or divorced, 4 = widowed, and 5 = never married). Key Explanatory Variables Key explanatory variables for this study include a number of measures indicating stress exposure. I utilize psychosocial stress exposure data from the 2004, 2006, and 2008 waves of the HRS, though respondents did not answer questions about stress exposure at every wave. First, I constructed standardized count indices of the following domain-specific stressors, corresponding to stress exposure in different domains of social life: lifetime traumas (Krause, Shaw, & Cairney, 2004), recent stressful life events (Turner, 2013), financial strain (Campbell, Converse, & Rodgers, 1976), ongoing chronic strains (Troxel, Matthews, Bromberger, & Sutton-Tyrrell, 2003), everyday discrimination (Williams et al., 1997), and major lifetime discrimination (Williams et al., 1997). These widely used measures include both recent and lifetime stressors and discrimination-related and generalized stressors. For detailed information on the construction of the individual stress measures, see Supplementary Appendix A. For individuals with valid stress exposure data in multiple waves, stress exposure was included as average exposure across the waves. Supplementary analyses utilizing the most recent wave of stress exposure for each respondent produced substantively similar results. Next, I created two composite measures of stress exposure. Consistent with previous studies (Strenthal et al., 2011), I created a measure of high risk stress burden, which indicates the number of stressors for which the respondent is in the highest quartile (0 = low cumulative stress, 1 = high risk on one stressor; 2 = high risk on two stressors; 3 = high risk on three stressors; 4 = high risk on four or more stressors). Next, I used factor analysis to create a composite measure of cumulative stress burden using the individual domain-specific stressors. Results from the factor analyses revealed a one factor structure for total stress burden (Eigen value = 2.273) with strong item-rest correlations for all of the individual stress measures (all above 0.50), indicating strong internal consistency. While similar to the high risk stress burden measure, the cumulative stress burden measure does not use cutoffs and places no restrictions on reporting high levels of stress but instead reflects total stress exposure across domains of stress. Other Measures The racial disparity in the outcomes is measured by a dummy variable, where “1” indicates Black. Other covariates include age (continuous), gender (1 = female), Analytic Strategy First, I use descriptive statistics to assess Black–White disparities in the measures of health, stress exposure, and other characteristics, using t tests (two-tailed) and chisquare tests to formally assess race differences. Next, I use multivariate OLS regression analyses to model the prospective associations between the stressors and the measures of CRP and metabolic dysregulation. At the time of analysis, the HRS had released only two complete waves of biomarker data, collected at relatively short intervals, which prevented modeling racial disparities in trajectories of CRP or metabolic dysregulation. As such, for both outcomes, I exploit the temporal sequencing of the data by modeling the outcomes in 2010–2012 as a function of stress exposure and other covariates in 2004–2008, based on when respondents had valid data. Supplementary analyses with the metabolic dysregulation outcome indicated that the results were robust to alternative modeling strategies, including Poisson and negative binomial regression. The models for all outcomes proceed in a stepwise fashion. Model 1 adjusts for age, gender, and race and provides evidence of the unadjusted race gaps in the outcomes; Model 2 builds on Model 1 by also including the socioeconomic measures; and Models 3–8 include each of the domain-specific stressors individually. Model 9 includes the composite measure of high risk stress burden, and Model 10 includes the measure of cumulative stress burden. In this way, results from Models 3 to 10 indicate the associations of the stressors with the outcomes and the contribution of the stress measures to Black–White health disparities net of race differences in socioeconomic status (SES), which is a conservative approach given both the strong racial patterning of SES and the documented associations between SES and stress (Lantz, House, Mero, & Williams, 2005). In reporting the multivariate results, I pay particular attention to whether inclusion of the stressor measures in the models reduces the racial disparity in the markers of health. To formally test whether the stress measures help to “explain” the race gaps in CRP and metabolic dysregulation, I compute direct and indirect effects for each imputed dataset, combine the estimates using Rubin’s rules for combining estimates from multiple imputed datasets (Rubin, 2004), and finally examine the equality of coefficients across models (Preacher & Hayes, 2008). All descriptive statistics and multivariate model estimates are weighted to adjust for survey design effects and nonresponse. Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 1942 Results Descriptive Statistics Table 1 presents descriptive statistics by race, and results indicate that Blacks have greater physiological risk than Whites, including higher levels of CRP (p < .001) and metabolic dysregulation (p < .001). Blacks also report more psychosocial stress exposure than Whites across virtually all domains of stress, with the exception of lifetime traumas. Table 1 also reveals racial disparities in the composite stress measures, with Blacks reporting more high risk stress burden (p < .001) and cumulative stress burden (p < .001) than Whites. Further, compared to Whites, Blacks also experience more socioeconomic disadvantage in mid to late life, with Blacks having lower levels of education, wealth, and income (p < .001) than Whites. Multivariate Models CRP Results in Table 2 document the prospective associations between stress exposure and log CRP (N = 7,280). Table 2 also shows the results of the mediation analyses that indicate the proportion of the race gap in log CRP “explained” Table 1. Descriptive Statistics by Race (HRS 2004–2012) (N = 7,280) Outcomes Log C-reactive protein Metabolic dysregulation Domain-specific stressors Lifetime traumas Stressful events Financial strain Ongoing chronic strains Everyday discrimination Major discrimination Composite stressors High risk stress burden High on 0 stressors High on 1 stressor High on 2 stressors High on 3 stressors High on 4 or more stressors Cumulative stress burden Sociodemographic characteristics Age Gender (1 = female) Socioeconomic factors Education <High school High school Some college BA+ Total household wealth Total household income Marital status Married Partnered Separated or divorced Widowed Never married Full sample Whites Blacks (N = 7,280) (N = 6,276) (N = 1,004) Mean/Prop. Mean/Prop. Mean/Prop. p-value 1.173 2.464 1.150 2.410 1.385 2.988 <.001 <.001 0.160 0.058 2.456 1.521 1.682 0.091 0.160 0.057 2.417 1.514 1.664 0.086 0.165 0.072 2.821 1.591 1.849 0.142 .420 .015 <.001 .003 <.001 <.001 0.301 0.272 0.189 0.12 0.118 0.08 0.313 0.277 0.186 0.115 0.109 0.047 0.193 0.221 0.223 0.160 0.203 0.390 <.001 63.924 0.541 64.119 0.533 62.117 0.615 <.001 <.001 0.012 0.355 0.253 0.277 567,240 75,482 0.097 0.358 0.255 0.290 612,905 79,241 0.283 0.327 0.232 0.157 144,040 40,647 <.001 0.643 0.037 0.137 0.147 0.036 0.672 0.036 0.120 0.141 0.031 0.379 0.051 0.294 0.197 0.079 <.001 <.001 <.001 <.001 Note: Weighted descriptive statistics. Sample sized based on CRP analytic sample, with exception of metabolic dysregulation outcome (N = 6,542). p-value of t test (two-tailed test) or chi-square test indicating race difference in mean/proportion. HRS = Health and Retirement Study. Gender (1 = female) Proportion race gap mediated by stressor(s)a Sociodemographic characteristics Age Cumulative stress burden High on 4 or more stressors High on 3 stressors High on 2 stressors Composite stressors High risk stress burden (high on 0 stressors is ref.) High on 1 stressor Major discrimination Everyday discrimination Ongoing chronic strains Financial strain Stressful life events Domain-specific stressors Lifetime traumas Racial disparity Race (1 = Black) (SE) (SE) −0.001 (0.001) 0.105*** (0.021) - −0.003* (0.001) 0.072*** (0.022) - 0.142*** (0.036) Coeff. Coeff. 0.225*** (0.034) Model 2 Model 1 −0.002* (0.001) 0.079*** (0.022) NS 0.328*** (0.081) 0.145*** (0.035) (SE) Coeff. Model 3 Table 2. Stress Exposure and Log C-Reactive Protein (N = 7,280) −0.002† (0.001) 0.073*** (0.022) NS 0.107 (0.096) 0.142*** (0.036) (SE) Coeff. Model 4 −0.002 (0.001) 0.072*** (0.022) 0.033* 0.033* (0.013) 0.137*** (0.036) (SE) Coeff. Model 5 −0.002 (0.001) 0.067** (0.022) NS 0.097*** (0.026) 0.142*** (0.036) (SE) Coeff. Model 6 −0.002 (0.001) 0.077*** (0.022) 0.023* 0.029† (0.015) 0.138*** (0.036) (SE) Coeff. Model 7 −0.002† (0.001) 0.079*** (0.022) 0.072** 0.198** (0.074) 0.133*** (0.036) (SE) Coeff. Model 8 −0.001 (0.001) 0.077*** (0.022) 0.066*** 0.007 (0.030) 0.066† (0.036) 0.078 (0.050) 0.134** (0.042) 0.133*** (0.036) (SE) Coeff. Model 9 −0.001 (0.001) 0.079*** (0.022) 0.058*** (0.013) 0.067*** 0.134*** (0.036) (SE) Coeff. Model 10 Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 1943 Coeff. (SE) Coeff. (SE) −0.038 (0.051) 0.094** (0.034) 0.025 (0.031) −0.026 (0.061) 0.093** (0.034) −0.050† (0.027) −0.178*** (0.027) −0.000*** (0.000) −0.000* (0.000) Model 2 Model 1 −0.045 (0.051) 0.083* (0.034) 0.015 (0.031) −0.016 (0.061) 0.085* (0.033) −0.055* (0.027) −0.175*** (0.027) −0.000*** (0.000) −0.000* (0.000) (SE) Coeff. Model 3 −0.040 (0.051) 0.090** (0.034) 0.023 (0.031) −0.028 (0.061) 0.093** (0.034) −0.052† (0.027) −0.179*** (0.027) −0.000*** (0.000) −0.000* (0.000) (SE) Coeff. Model 4 −0.042 (0.051) 0.085* (0.035) 0.019 (0.031) −0.027 (0.061) 0.091** (0.034) −0.049† (0.027) −0.175*** (0.027) −0.000** (0.000) −0.000* (0.000) (SE) Coeff. Model 5 −0.046 (0.051) 0.082* (0.035) 0.016 (0.031) −0.023 (0.061) 0.092** (0.034) −0.051† (0.027) −0.177*** (0.027) −0.000** (0.000) −0.000* (0.000) (SE) Coeff. Model 6 −0.041 (0.051) 0.091** (0.034) 0.023 (0.031) −0.024 (0.061) 0.092** (0.034) −0.050† (0.027) −0.177*** (0.027) −0.000*** (0.000) −0.000* (0.000) (SE) Coeff. Model 7 −0.043 (0.051) 0.086* (0.034) 0.023 (0.031) −0.032 (0.061) 0.094** (0.034) −0.056* (0.027) −0.183*** (0.027) −0.000*** (0.000) −0.000* (0.000) (SE) Coeff. Model 8 −0.053 (0.051) 0.077* (0.035) 0.015 (0.031) −0.024 (0.061) 0.090** (0.034) −0.055* (0.027) −0.178*** (0.027) −0.000** (0.000) −0.000* (0.000) (SE) Coeff. Model 9 Note: Results based on OLS regression models. CRP was assessed in 2010–2012; all other covariates were measured in 2004–2008. Model estimates are weighted. HS = High school. a Proportion of racial disparity in CRP observed in Model 2 “explained away” by the stress measure(s) included in the model. p-value of mediation test. “NS” indicates no statistically significant mediation. ***p < .001, **p < .01, *p < .05, †p < .1. Never married Widowed Separated or divorced Marital status (Married is reference) Partnered Total household income Total household wealth BA+ Some college Socioeconomic factors Education (HS is reference) <HS Table 2. Continued −0.050 (0.051) 0.073* (0.035) 0.012 (0.031) −0.026 (0.061) 0.090** (0.033) −0.056* (0.027) −0.179*** (0.027) −0.000** (0.000) −0.000* (0.000) (SE) Coeff. Model 10 1944 Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 by the stress measures included in the respective models. As indicated by the coefficient for race, the Black–White disparity in inflammation is largest in Model 1. Including the measures of SES in Model 2 reduces the racial disparity over Model 1. Models 3–8 introduce each of the domainspecific stressors in a stepwise fashion. In several cases, the Black–White disparity in log CRP is further attenuated by the inclusion of the stress exposure measures in the models, net of SES. Model 3 indicates that lifetime traumas are positively associated with inflammation (0.328, p < .001), such that individuals who reported more traumas over the course of their lives had higher CRP. However, results of mediation analyses reveal that differences in lifetime traumas did not account for a significant portion of the Black–White disparity in CRP. Model 4 reveals no significant association between stressful life events and log CRP. Results from Models 5 and 6 show that financial strain (0.033, p = .012) and ongoing chronic strain (0.097, p < .001) are positively associated with inflammation. Mediation analyses show that including the measure of financial strain in Model 5 reduces the race gap in log CRP by approximately 3.4% (p = .015), net of SES. This suggests that, even after adjusting for racial differences in socioeconomic resources, Black–White differences in financial stress account for a portion of the racial disparity in physiological inflammation. Results in Models 7 and 8 of Table 2 indicate that everyday (0.029, p = .063) and major life discrimination (0.198, p = .007) are positively associated with inflammation. Further, results from mediation analyses indicate that including the measures of everyday and major life discrimination in the models reduces the race gap in inflammation by 2.3 (p = .043) and 7.2% (p = .001), respectively. Models 9–10 include the composite stress measures. The measure of high risk stress burden is positively associated with CRP, indicating that, compared to individuals who report lower levels of stress, individuals reporting high stress across domains of stress are at increased inflammatory risk. Mediation analyses reveal that Black–White differences in high risk stress burden account for approximately 6.6% of the race gap in CRP (p < .001). The measure of cumulative stress burden is also associated with increased inflammation. Including the measure of cumulative stress burden in Model 10 results in a 6.7% reduction of the race gap in CRP (p < .001). Metabolic dysregulation Table 3 displays results of the metabolic dysregulation models (N = 6,452). The racial disparity in metabolic risk is greatest in Model 1 and is attenuated after adjusting for SES in Model 2. Results from Models 3–8 reveal that, with the exception of major life discrimination, all domainspecific stressors are positively associated with metabolic dysregulation. Further, results from mediation analyses indicate that racial differences in financial strain and everyday discrimination are drivers of the Black–White gap 1945 in metabolic risk net of racial differences in SES. Lifetime traumas, stressful life events, and ongoing chronic strains— while prospectively associated with metabolic risk—do not account for significant portions of the Black–White gap in metabolic risk in late life. Results from Models 9 indicate that high risk stress burden is positively associated with metabolic dysregulation, particularly for those who reported high levels of exposure on four or more of the stressors, and that race differences in high risk stress burden partially “explain” the Black– White gap in metabolic risk. Finally, in Model 10, the composite measure of cumulative stress burden is strongly associated with metabolic dysregulation (0.090, p < .001) and accounts for approximately 3% of the Black–White metabolic gap (p = .004), net of SES. Across the models in Table 3, the race gap in metabolic risk is smallest in Models 7 and 10, which include the measures of everyday discrimination and cumulative stress burden, respectively. Discussion The divergence of Black–White health gaps through mid and late life has led scholars to hypothesize that Blacks may experience accelerated aging and physiological deterioration relative to Whites due to racial differences in social exposures, including stress (Geronimus et al., 2010). Still, while research documents that Blacks experience greater levels of stress exposure than Whites (Turner & Avison, 2003) and that repeated exposure to stress can increase disease risk (Cohen et al., 2012; Thoits, 2010), these two bodies of literature have not been fully integrated to adequately assess the role of cumulative stress exposure in Black–White health gaps in later life. Using nationally representative, longitudinal data and diverse measures of physiological functioning and stress exposure, this study offers three contributions to understanding of the links between racism, stress, and health inequality from mid to late life. First, results provide strong evidence of the racial patterning of physiological well-being and stress exposure at older ages. Consistent with previous research (Geronimus et al., 2010; Mitchell & Aneshensel, 2017; Mitchell et al., 2019), results from both the descriptive and multivariate analyses indicated that older age Blacks have higher levels of systemic inflammation and metabolic dysregulation than Whites. These results are consistent with the notion of “weathering” (Geronimus et al., 2010), whereby older aged Blacks in the United States experience accelerated physiological dysregulation compared to Whites in ways that relate to population patterns of health and disease risk in later life. Also, consistent with previous research (Brown & Hargrove, 2018; Strenthal et al., 2011), results indicated that Blacks experience more cumulative stress burden than Whites, including more stressful events, financial strain, ongoing chronic strain, and everyday and major life discrimination. In this way, findings show that racism, as a system of oppression and domination, patterns exposure Proportion race gap mediated by stressor(s)a Cumulative stress burden High on 4 or more stressors High on 3 stressors High on 2 stressors Composite stressors High risk stress burden (high on 0 stressors is ref.) High on 1 stressor Major discrimination Everyday discrimination Ongoing chronic strains Financial strain Stressful life events Domain-specific stressors Lifetime traumas Racial disparity Race (1 = Black) (SE) (SE) - - 0.493*** (0.060) Coeff. Coeff. 0.566*** (0.058) Model 2 Model 1 NS 0.285* (0.144) 0.496*** (0.060) (SE) Coeff. Model 3 Table 3. Stress Exposure and Metabolic Dysregulation (N = 6,452) NS 0.359† (0.185) 0.492*** (0.060) (SE) Coeff. Model 4 0.016† 0.048† (0.026) 0.486*** (0.060) (SE) Coeff. Model 5 NS 0.113* (0.051) 0.493*** (0.060) (SE) Coeff. Model 6 0.024** 0.101*** (0.029) 0.479*** (0.060) (SE) Coeff. Model 7 NS 0.199 (0.144) 0.484*** (0.061) (SE) Coeff. Model 8 0.017† (0.081) 0.078 (0.055) 0.029 (0.062) 0.139 (0.093) 0.172* 0.483*** (0.060) (SE) Coeff. Model 9 0.090*** (0.025) 0.029** 0.480*** (0.060) (SE) Coeff. Model 10 1946 Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 −0.135 (0.112) −0.109† (0.061) 0.010 (0.053) −0.069 (0.120) −0.141 (0.112) −0.117† (0.061) 0.001 (0.053) −0.060 (0.120) −0.137 (0.112) −0.122* (0.061) 0.004 (0.053) −0.078 (0.121) 0.106† (0.060) −0.047 (0.049) −0.236*** (0.052) −0.000*** (0.000) 0.000 (0.000) −0.005* (0.002) 0.050 (0.040) (SE) Coeff. Model 4 −0.140 (0.113) −0.119† (0.061) 0.001 (0.053) −0.070 (0.120) 0.101† (0.059) −0.041 (0.049) −0.227*** (0.052) −0.000** (0.000) 0.000 (0.000) −0.005* (0.002) 0.045 (0.040) (SE) Coeff. Model 5 −0.145 (0.113) −0.121* (0.061) 0.001 (0.053) −0.066 (0.120) 0.103† (0.059) −0.044 (0.049) −0.232*** (0.051) −0.000*** (0.000) 0.000 (0.000) −0.005* (0.002) 0.040 (0.040) (SE) Coeff. Model 6 −0.146 (0.113) −0.117† (0.061) 0.007 (0.053) −0.065 (0.120) 0.102† (0.059) −0.042 (0.049) −0.231*** (0.051) −0.000*** (0.000) 0.000 (0.000) −0.004† (0.002) 0.060 (0.040) (SE) Coeff. Model 7 −0.140 (0.112) −0.116† (0.061) 0.007 (0.053) −0.076 (0.121) 0.106† (0.060) −0.048 (0.049) −0.237*** (0.052) −0.000*** (0.000) 0.000 (0.000) −0.006* (0.002) 0.053 (0.040) (SE) Coeff. Model 8 −0.151 (0.112) −0.127* (0.061) −0.001 (0.053) −0.071 (0.121) 0.102† (0.059) −0.049 (0.049) −0.234*** (0.051) −0.000*** (0.000) 0.000 (0.000) −0.004* (0.002) 0.052 (0.040) (SE) Coeff. Model 9 −0.153 (0.112) −0.138* (0.061) −0.009 (0.053) −0.071 (0.121) 0.101† (0.059) −0.051 (0.049) −0.235*** (0.051) −0.000** (0.000) 0.000 (0.000) −0.003 (0.002) 0.055 (0.040) (SE) Coeff. Model 10 Note: Results based on OLS regression models. Metabolic dysregulation was assessed in 2010–2012; all other covariates were measured in 2004–2008. Model estimates are weighted. HS = High school. a Proportion of racial disparity in metabolic dysregulation observed in Model 2 “explained away” by the stress measure(s) included in the model. p-value of mediation test. “NS” indicates no statistically significant mediation. ***p < .001, **p < .01, *p < .05, †p < .1. Never married Widowed Separated or divorced Marital status (married is reference) Partnered Total household income Total household wealth BA+ Some college 0.098 (0.060) −0.046 (0.049) −0.229*** (0.052) −0.000*** (0.000) 0.000 (0.000) (SE) 0.104† (0.060) −0.042 (0.049) −0.231*** (0.052) −0.000*** (0.000) 0.000 (0.000) (SE) (SE) Coeff. −0.006** (0.002) 0.051 (0.040) Coeff. Coeff. Model 3 −0.006** (0.002) 0.046 (0.040) Model 2 Model 1 Sociodemographic characteristics Age −0.004† (0.002) Gender (1 = female) 0.072† (0.038) Socioeconomic factors Education (HS is reference) <HS Table 3. Continued Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 1947 1948 to a variety of acute and chronic stressors and strains— both discrimination-related and more generalized—across domains of social life in ways that produce stark racial disparities in cumulative life course stress exposure. Second, results in Tables 2 and 3 offer robust, consistent evidence of the prospective associations between stress exposure and physiological well-being, where stress exposure is consistently linked to greater health risk in mid to late life. While previous research has relied largely on cross-sectional data, this study used lagged stress exposure measures to offer a more rigorous examination of the role of stress in shaping trajectories of health. Further, while extant research on stress and health has been largely restricted by the use of single health or disease outcomes, findings from this study indicate that stress exposure contributes to population health inequality through numerous physiological processes. Both systemic inflammation and metabolic function have been increasingly identified as critical pathogenic pathways shaping disease and mortality risk across the life course (Finch, 2010; Yang & Kozloski, 2011), and findings from this study consistently indicated that these physiological processes may be particularly critical pathways through which social stressors “get under the skin” to produce population health disparities from mid through late life. Third, this study is among the first to use formal mediation analyses to document the unique and joint contributions of various stress exposure measures to racial gaps in physiological functioning and provides new evidence of the role of cumulative stress exposure in producing Black–White gaps in physiological risk in late life. Results from the mediation analyses indicated that Black–White disparities in exposure to financial strain, everyday discrimination, major life discrimination, and the composite stress measures, in particular, helped to “explain away” significant portions of the racial gaps in the outcomes. Importantly, racial differences in the composite indicator of cumulative stress burden accounted for the greatest proportion of the race gaps in metabolic risk and also played a prominent role in contributing to Black–White gaps in inflammation. Previous research on the links between stress and health generally examines one stressor at a time, despite evidence that stressors often co-occur, meaning that studies that utilize single stressors risk overestimating the association between particular stressors and health (Green et al., 2010) and underestimating the role of cumulative stress burden in the production of health inequality. By contrast, composite indicators of stress exposure may better reflect the co-occurrence of stressors and, consistent with cumulative inequality theory (Ferraro & Shippee, 2009), may more effectively capture how the accumulation of stressors over time and across domains of social life collectively contribute to racial disparities in health among older adults than any single stressor measure. Results from this study indeed showed that Black–White differences in cumulative stress burden as indicated by the factor score mediated the greatest proportion of Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 racial disparities in both outcomes. Importantly, the proportion of the Black–White gap mediated by cumulative stress exposure was more than twice as high for CRP than metabolic dysregulation, suggesting that inflammatory processes may play a particularly prominent role in linking racial disparities in cumulative stress to Black– White gaps in health and disease risk. While stress exposure played a prominent role in producing racial gaps in CRP, the proportion of the race gap in metabolic risk mediated by the stressors was more modest, indicating that other factors—such as health behaviors—may play a more central role in shaping metabolic risk. Taken together, the results presented here show that the physiological toll of the “thousand small cuts” resulting from the accumulation of stress exposure across domains of social life throughout the life course—including experiencing multiple traumatic and stressful events as well as repeated exposure to more chronic stressors and strains—can accelerate the physiological functioning of older age Blacks relative to Whites. It is worth noting that the contribution of stress exposure to Black–White health gaps persisted net of racial differences in socioeconomic factors, which is a relatively conservative test for mediation, given that both stress exposure is patterned by SES (Turner & Avison, 2003) and that SES is strongly patterned by race (Boen, 2016). This study is not without limitations, which should be addressed in future research. First, while the current study exploited the temporal sequencing of the data by assessing how stress exposure at baseline was associated with inflammatory and metabolic risk at follow-up, future work utilizing multiple waves of biomarkers will improve causal inference and further elucidate how stress exposure shapes trajectories of health inequality as individuals age. In supplementary analysis, I ran lagged dependent variable models, regressing the outcomes in 2010/2012 on the outcomes measured at baseline, while also adjusting for the covariates. I found minimal evidence that baseline stress exposure contributed to race differences in physiological changes over the period, though four years may be too short of a time period for stress exposure to account for Black–White differences in change in the biomarkers. Still, more research utilizing longitudinal biomarker data is needed. Second, while the present study integrates multiple measures of life course stress exposure, there are other stressors and traumas not included here that may play a role in Black–White health gaps, including vicarious stressors related to the experiences of family and friends (Williams & Mohammed, 2009) and neighborhood level stressors (Clarke et al., 2014). The proportion of the race gaps mediated by the stressors included in the present study is modest, so more research on how the accumulation of other stressors may also contribute to Black–White health gaps is needed. Finally, future research should consider the psychological, emotional, and behavioral mechanisms that underlie the links between stress exposure and physiological functioning. Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 Taken together, these results indicate that studies of racial health inequality should consider the role of Black–White differences in cumulative stress burden—rather than race differences in single measures of domain-specific stressors—in order to more accurately capture the role of stress in racial health inequality. Failure to measure race differences in the accumulation of stress exposure across domains of social life in the study of Black–White health disparities can result in overestimating the role of any singular stressor in racial health gaps and underestimating the total contribution of stress to racial health disparities. Importantly, the findings presented here also suggest that studies of Black–White health disparities that do not attempt to comprehensively measure the accumulation of recent and lifetime traumas and events, chronic stressors and strains, and discrimination-related stress—or even fail to account for stress exposure at all—may risk overestimating the race residual, or the “unexplained” racial health gap, which is not without implications. In particular, when studies are left with significant, unaccounted for racial disparities in health, authors speculate about the potential explanations for these “unexplained” gaps. As such, there has been a resurgence of biological and genetic explanations for Black–White health differences (see Roberts, 2013 for a review), which is concerning in the face of overwhelming evidence that social explanations for racial health gaps have been underestimated. This study, then, serves as both essential evidence of the key role of stress exposure in racial health inequality and as further proof that more research on the social origins—including the psychosocial determinants—of racial health gaps is needed. By linking Black–White gaps in systemic inflammation and metabolic dysregulation to racial disparities cumulative exposure to social stressors, findings from this study indicate that Black–White disparities in physiological functioning observed from mid through late life in part reflect the accumulation of racialized social stressors that occur across domains of life and across the entire life span. The “thousand cuts” that Blacks experience across the life course as a result of living in a racially stratified society play a role in producing their accelerated physiological deterioration in mid to late life relative to Whites. The racial patterning of stress exposure extends beyond explicit incidences of racial discrimination to include a variety of stressors and strains across domains of social life. As such, reducing racial health disparities at older ages will require policy and intervention efforts targeting both the material and psychosocial factors underlying population health inequality across the life course. Supplementary Material Supplementary data is available at The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences online. Funding This publication was made possible by funding from the Population Research Infrastructure Program of the National Institutes of Health’s (NIH)’s Eunice Kennedy Shriver 1949 National Institute of Child Health and Human Development awarded to the Population Studies Center at the University of Pennsylvania, NIH grant number: R24 HD044964. Acknowledgments I would like to thank Y. Claire Yang, Karolyn Tyson, Robert Hummer, Kathleen Mullan Harris, and Anthony Perez for their feedback on earlier drafts of the paper. I also want to thank the anonymous reviewers for their insightful comments and suggestions. Author contributions C. Boen planned the study, conducted the data analysis, and wrote the paper. Conflict of Interest None reported. References Aneshensel, C. S., Rutter, C. M., & Lachenbruch, P. A. (1991). Social structure, stress, and mental health: Competing conceptual and analytic models. American Sociological Review, 56, 166–178. doi:10.2307/2095777 Boen, C. (2016). The role of socioeconomic factors in black-white health inequities across the life course: Point-in-time measures, long-term exposures, and differential health returns. Social Science & Medicine, 170, 63–76. doi:10.1016/j.socscimed.2016.10.008 Bonilla-Silva, E. (1997). Rethinking racism: Toward a structural interpretation. American Sociological Review, 62, 465–480. doi:10.2307/2657316 Brown, T. H., & Hargrove, T. W. (2018). Psychosocial mechanisms underlying older black men’s health. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73, 188– 197. doi:10.1093/geronb/gbx091 Campbell, A., Converse, P. E., & Rodgers, W. (1976). The quality of American life: Perceptions, evaluations, and satisfactions. New York, NY: Russell Sage Foundation. Clarke, P., Morenoff, J., Debbink, M., Golberstein, E., Elliott, M. R., & Lantz, P. M. (2014). Cumulative exposure to neighborhood context consequences for health transitions over the adult life course. Research on Aging, 36, 115–142. doi:10.1177/0164027512470702 Cohen, S., Janicki-Deverts, D., Doyle, W. J., Miller, G. E., Frank, E., Rabin, B. S., & Turner, R. B. (2012). Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proceedings of the National Academy of Sciences of the United States of America, 109, 5995–5999. doi:10.1073/pnas.1118355109 Ferraro, K. F., & Shippee, T. P. (2009). Aging and cumulative inequality: How does inequality get under the skin? The Gerontologist, 49, 333–343. doi:10.1093/geront/gnp034 Finch, C. E. (2010). The biology of human longevity: Inflammation, nutrition, and aging in the evolution of lifespans. Burlington, MA: Academic Press. Geronimus, A. T., Hicken, M. T., Pearson, J. A., Seashols, S. J., Brown, K. L., & Cruz, T. D.. (2010). Do US black women 1950 experience stress-related accelerated biological aging? Human Nature, 21, 19–38. doi:10.1007/s12110-010-9078-0 Goosby, B. J., Straley, E., & Cheadle, J. E. (2017). Discrimination, sleep, and stress reactivity: Pathways to African American-white cardiometabolic risk inequities. Population Research and Policy Review, 36, 699–716. doi:10.1007/s11113-017-9439-z Green, J. G., McLaughlin, K. A., Berglund, P. A., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2010). Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 67, 113–123. doi:10.1001/archgenpsychiatry.2009.186 Harris, T. B., Ferrucci, L., Tracy, R. P., Corti, M. C., Wacholder, S., Ettinger, W. H., Heimovitz, H., Cohen, H. J., & Wallace, R. (1999). Associations of elevated interleukin-6 and C-reactive protein levels with mortality in the elderly. The American Journal of Medicine, 106, 506–512. doi:10.1016/ S0002-9343(99)00066-2 Heeringa, S. G., & J. H. Connor. (1995). Technical description of the health and retirement survey sample design. Ann Arbor, MI: University of Michigan. Jones, C. P. (2000). Levels of racism: A theoretic framework and a gardener’s tale. American Journal of Public Health, 90, 1212– 1215. doi:10.2105/ajph.90.8.1212 Krause, N., Shaw, B. A., & Cairney, J. (2004). A descriptive epidemiology of lifetime trauma and the physical health status of older adults. Psychology and Aging, 19, 637–648. doi:10.1037/0882-7974.19.4.637 Lantz, P. M., House, J. S., Mero, R. P., & Williams, D. R. (2005). Stress, life events, and socioeconomic disparities in health: Results from the Americans’ Changing Lives Study. Journal of Health and Social Behavior, 46, 274–288. doi:10.1177/002214650504600305 McEwen, B. S. (2007). Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological reviews, 87, 873–904. doi:10.1152/physrev.00041.2006 Mitchell, U. A., & Aneshensel, C. S. (2017). Social inequalities in inflammation: Age variations in older persons. Journal of Aging and Health, 29, 769–787. doi:10.1177/0898264316645546 Mitchell, U. A., Ailshire, J. A., & Crimmins, E. M. (2019). Change in cardiometabolic risk among blacks, whites, and hispanics: Findings from the health and retirement study. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 74, 240–246. doi:10.1093/gerona/gly026 National Center for Health Statistics (US). (2016). Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Pearlin, L. I. (1999). The stress process revisited. In Handbook of the sociology of mental health. “The stress process revisited” (pp. 395–415). New York, NY: Springer. Pearlin, L. I., Menaghan, E. G., Lieberman, M. A., & Mullan, J. T. (1981). The stress process. Journal of Health and Social Behavior, 22, 337–356. doi: 10.2307/2136676 Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. doi:10.3758/BRM.40.3.879 Journals of Gerontology: SOCIAL SCIENCES, 2020, Vol. 75, No. 9 Roberts, D. (2013). Fatal invention: How science, politics, and big business re-create race in the twenty-first century. New York, NY: The New Press. Rubin, D. B. (2004). Multiple imputation for nonresponse in surveys. New York: John Wiley and Sons. Seyle, H. (1974). Stress without distress. Philadelphia, PA: Lippincott Williams & Wilkins. Sternthal, M. J., Slopen, N., & Williams, D. R. (2011). Racial disparities in health: how much does stress really matter?. Du Bois Review: Social Science Research on Race, 8, 95–113. doi:10.1017/S1742058X11000087 Thoits, P. A. (2010). Stress and health: Major findings and policy implications. Journal of Health and Social Behavior, 51 Suppl, S41–S53. doi:10.1177/0022146510383499 Troxel, W. M., Matthews, K. A., Bromberger, J. T., & SuttonTyrrell, K. (2003). Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychology, 22, 300–309. doi:10.1037/0278-6133.22.3.300 Turner, R. J. (2013). Understanding health disparities the relevance of the stress process model. Society and Mental Health, 3, 170–186. doi:10.1177/2156869313488121 Turner, R. J., & Avison, W. R. (2003). Status variations in stress exposure: Implications for the interpretation of research on race, socioeconomic status, and gender. Journal of Health and Social Behavior, 44, 488–505. doi:10.2307/1519795 Umberson, D., Olson, J. S., Crosnoe, R., Liu, H., Pudrovska, T., & Donnelly, R.. (2017). Death of family members as an overlooked source of racial disadvantage in the United States. Proceedings of the National Academy of Sciences of the United States of America, 114, 915–920. doi:10.1073/ pnas.1605599114 Williams, D. R., Yu, Y., Jackson, J. S., & Anderson, N. B. (1997). Racial differences in physical and mental health: Socioeconomic status, stress and discrimination. Journal of Health Psychology, 2, 335–351. doi:10.1177/135910539700200305 Williams, D. R., & Jackson, P. B. (2005). Social sources of racial disparities in health. Health affairs (Project Hope), 24, 325–334. doi:10.1377/hlthaff.24.2.325 Williams, D. R., & Mohammed, S. A. (2009). Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine, 32, 20–47. doi:10.1007/ s10865-008-9185-0 Williams, D. R., Mohammed, S. A., Leavell, J., & Collins, C. (2010). Race, socioeconomic status, and health: Complexities, ongoing challenges, and research opportunities. Annals of the New York Academy of Sciences, 1186, 69–101. doi:10.1111/j.1749-6632.2009.05339.x Yang, Y., & Kozloski, M. (2011). Sex differences in age trajectories of physiological dysregulation: Inflammation, metabolic syndrome, and allostatic load. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 66, 493–500. doi:10.1093/gerona/glr003 Yang, Y. C., Gerken, K., Schorpp, K., Boen, C., & Harris, K. M. (2017). Early-life socioeconomic status and adult physiological functioning: A life course examination of biosocial mechanisms. Biodemography and Social Biology, 63, 87–103. doi:10.1080/1 9485565.2017.1279536