Odontogenic & Non-Odontogenic Tumors: Dentistry Study Guide
advertisement

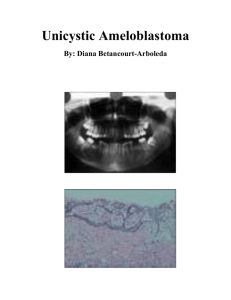
lOMoARcPSD|3413111 Odontogenic and Non-odontogenic Tumors Dentistry (Centro Escolar University) Studocu is not sponsored or endorsed by any college or university Downloaded by Micheal KL (up828456@myport.ac.uk) lOMoARcPSD|3413111 ODONTOGENIC TUMORS DISEASE A. Epithelial Tumor 1. Amelobla stoma OTHER TERM/S CAUSE Amel (English) – enamel Blastos (greek) germ Unknown cause, but trauma and infection can be one of the causes LOCATION Mandibular molar-ramus area – the most favored site AGE SEX CLINICAL HISTOPATH RADIOGRAPH DIFFERENTIAL DIAGNOSIS TREATMENT PROGNOSIS occurs predominantl y in the 4th and 5th decades of life no gender predilectio n for this tumor - usually asymptomatic - discovered during routine radiographic examinations - jaw expansion - initial presenting signs: tooth movement or malocclusion 1. Follicular type – composed of islands of tumor cells that mimic the normal dental follicle. Most common histological type. 2. Plexiform ameloblastoma – neoplastic cells developed into a network of epithelium. - “Fish Net Pattern” 3. Desmoplastic ameloblastoma – the stroma is desmoplastic and the tumor islands become squamoid or elongated 4. Basal cell or basaloid ameloblastoma – microscopically similar to basal cell carcinoma 5. Granular cell ameloblastoma – the central neoplastic cells exhibit prominent cytoplasmic granularity - large polygonal epithelial cells, seen in sheets or islands - cytoplasm is abundant and eosinophilic - focal zones of clear cells (clear cell variant) - concentric calcific deposits (Liesegang rings) -calcified amyloid or amyloid-like material - either unilocular or multilocular - radiographic margins are usually well defined and sclerotic - root resorption occasionally occurs in association with ameloblastoma -radioluscent 1. Odontogenic tumors – CEOT, Odontogenic Myxoma 2. Non-odontogenic tumors – Central giant cell granuloma, Ossifying fibroma, Central hemangioma 3. Cyst – Dentigerous cyst -Surgical excision -Block excision or resection – for large lesions -Conservative treatment – for peripheral ameloblastoma -Radiotherapy – rarely used (radioresistant) For curettage – 50% to 90% recurrence rate - associated with impacted teeth - may be unilocular or multilocular - well circumscribed radiographically (radiolucent or may contain opaque foci) - dentigerous cyst - odontogenic keratocyst - ameloblastoma - odontogenic myxoma - adenomatoid odontogenic tumor - ameloblastic fibroodontoma - ossifying fibroma - osteoblastoma - surgical excision ranging from enucleation to resection - aggressive surgery is contraindicated - overall recurrence has been less than 20% -intracystic - well circumscribed - Dentigerous cyst Conservative Good prognosis Maxilla – molar area is more frequently affected than the pre-molar and anterior regions *originates within mand or max from epi that is involve in the formation of teeth 2. Calcifyin g Epithelial Odontog enic Tumor (CEOT) Pinborg Tumor Mandible – molar-ramus region 2nd to 10th decade Mean age: 40 yrs no gender predilectio n for this tumor -jaw expansion -discovered after routine radiographic examination 3. Adenom Adenoam anterior Between 5 to Female rarely seen in *ameloblastoma on maxilla difficult to manage bc of high content of cancellous bone Downloaded by Micheal KL (up828456@myport.ac.uk) lOMoARcPSD|3413111 atoid Odontogen ic Tumor B. Mesenchy mal Tumors 1. Periapica l Cemento ssseous Dysplaci a 2.Cementobl astoma C. Mixed Tumors 1. Ameloblast ic Fibroodont oma / Ameloblast ic Fibroma eloblasto ma (subtype of ameloblas toma) Cemento ma True Cemento ma - unusual response of periapical bone and cementu m to some undeterm ined local factor maxilla, generally in association with the crowns of impacted teeth 30 years with most appearing the 2nd decade -mandible – anterior periapical region -2 or more teeth are affected middle age (around 40 years) mandible – posterior region mandibular molar-ramus region peripheral gingival location epithelial proliferation is composed of polyhedral to spindle cells - rosettes and ductlike structures of columnar epithelial cells – characteristic microscopic features unilocular lesion usually around the crown of an impacted tooth - lesions are typically radiolucent - Calcifying odontogenic cyst - CEOT treatment (Enucleation) (No recurrence – benign and encapsulated) women – especially black women occurs at the apex of the vital teeth -asymptomatic mixture of benign fibrous tissue, bone and cementum discovered on a routine radiographic examination 3 stages: 1. osteolytic stage – appears as periapical lucency that is continuous with the periodontal space 2. Cementoblastic stage – the lucent lesion develops into a mixed or mottled pattern because of bone repair 3. Mature stage – appears as solid, opaque mass that is often surrounded by a thin, lucent ring - the process may take months to years to reach the final stage 1. chronic osteomyelitis 2. ossifying fibroma 3. periapical granuloma or cyst - no treatment is required - once the opaque stage (final) is reached, the lesion stabilizes and causes no complications Good 2nd and 3rd decades of life (particularly before 25 years of age) no gender predilectio n - associated with the root of the tooth - tooth remains vital - may cause cortical expansion - low-grade intermittent pain - appears as a dense mass of mineralized cementum-like material with numerous reversal lines - cementoclast are also evident the neoplasm is an opaque lesion that replaces the root of the tooth surrounded by a radiolucent ring - odontoma - osteoblastoma - focal sclerosing osteomyelitis - hypercementosis Extraction of the tooth Good No recurrence mean age – 12 years no gender predilectio n - the lesions are lobulated and usually surrounded by a fibrous capsule - tumor mass is composed of myxoid connective tissue - the lesions are well circumscribed and are usually surrounded by a sclerotic margin - may be unilocular or multilocular and associated with the crown of an impacted tooth For ameloblastic fibroma - ameloblastoma - odontogenic myxoma - dentigerous cyst - odontogenic keratocyst - central giant cell granuloma Conservative surgical procedure (Curettage or excision) Good Recurrence is uncommon rarely before the age of 20 upper age limit – 40 years Downloaded by Micheal KL (up828456@myport.ac.uk) lOMoARcPSD|3413111 In ameloblastic fibroodontoma, one or more foci contain enamel and dentin 2. Odontoma 3. Amelobla stic Odon toma Odontoam eloblasto ma characteri zed by simultane ous occurrenc e of an amelobla stoma and odontom a - ameloblastic fibroodontoma – an opaque focus appears due to odontoma - ameloblastic fibroma – completely lucent radiographically - histiocytosis - focal sclerosing osteitis - osteoma - periapical cemental dysplasia - ossifying fibroma - cementoblastoma - maxilla is affected slightly than mandible - compound odontoma – anterior jaws - complex odontoma – posterior jaws - children and young adult - most are discovered in the 2nd decade - age range: extend into later adulthood no gender predilectio n - clinical signs suggestive of an odontoma - retained deciduous tooth - impacted tooth - alveolar swelling asymptomati c normal appearing enamel, dentin and pulp may be seen in these lesions - compound odontoma – appears as numerous tiny teeth in a single focus; in a tooth bearing area, between the roots or over the crown of an impacted tooth - complex odontoma – appears in the same region but a s amorphous opaque mass Mandible any age/children no gender predilectio n slowly expanding lesion - facial deformity - bone destruction - mild pain - delayed eruption of teeth consist of great variety of cells and tissues in a complex distribution presence of numerous radiopaque masses Downloaded by Micheal KL (up828456@myport.ac.uk) For ameloblastic fibroodontoma - CEOT - calcifying odontogenic cyst - developing odontoma - adenomatoid odontogenic tumor Enucleation Good No recurrence Same with ameloblastoma Expect recurrence if not totally removed lOMoARcPSD|3413111 NON-ODONTOGENIC TUMORS DISEASE I. Benign Tumors 1. Ossifying Fibroma OTHER TERM/S CAUSE - Cementifying fibroma, Cementoossify ing fibroma Psammomatoi d ossifying fibroma - bony islands in these lesions have a round or spheroidal shape. 2. Fibrous Dysplasi a LOCATION AGE SEX CLINICAL head and neck jaws craniofaci al bones mandible – premolarmolar regions 3rd and 4th decade of life female - slow-growing tumor - asymptomatic - expansile lesion – causing thinning of buccal and lingual cortical plates - is a condition in w/c normal medullary bone is replaced by an abnormal fibrous connective tissue proliferation in which new nonmaturing bone is formed. - nature of this condition has not been firmly established - more often in the maxilla than in the mandible - may extend to involve the maxillary sinus, zygoma, sphenoid bone and floor of the orbit 1st or 2nd decade of life - variant: 1. juvenile ossifying fibroma - children and young adult - involves paranasal sinuses and periorbital bones - asymptomatic - slow enlargement - present as a unilateral swelling - as the lesion grows, facial asymmetry becomes evident and may be the initial presenting complaint displacement of teeth, malocclusion, interference with tooth eruption may occur HISTOPATH RADIOGRAPH DIFFERENTIAL DIAGNOSIS TREATMENT PROGNOSIS composed of fibrous connective tissue with welldifferentiated spindled fibroblast most important radiographic feature of this lesion is the well circumscribed, sharplydefined border (lucent) 1. fibrous dysplasia ossifying fibroma has a wellcircumscribed radiographic appearance and the ease of separating it from the bone 2. osteoblastoma 3. focal cementoosseous dysplasia 4. focal osteomyelitis surgical removal using curettage or enucleation Good - consist of slight to moderate cellular fibrous connective tissue stroma 1. appearance ranges from a radiolucent lesion to a uniformly radiopaque mass 2. radiopaque change that imparts a “ground glass” or “peau d‟ orange” effect (not pathognomonic) 3. most commonly seen in patient with long-standing disease, is a mottled radiolucent and radiopaque appearance 4. fingerprint bone pattern and superior displacement of the mandibular canal in mandibular lesion - important distinguishing feature is the poorly defined radiographic and clinical margins of the lesion ossifying fibroma chronic osteomyelitis - small lesion – no treatment other than biopsy confirmation and periodic follow-up - large lesion – surgical recontouring - en bloc resection for complete removal is contraindicated malignant transformation is rare (fewer than 1% of cases) Good prognosis 2 Forms of Fibrous dysplasia Downloaded by Micheal KL (up828456@myport.ac.uk) lOMoARcPSD|3413111 1. Monostotic fibrous dysplasia - involves one bone - much more common ( 80%) than polyostotic form - jaw involvement is common – body of the mandible - other bones: ribs and femur - equal gender predilection - laboratory values: within normal range – serum calcium, phosphorous, and alkaline phosphatase 2. Polyostotic fibrous dysplasia - involves more than one bone - diseases that involve this form: - Mc-CuneAlbright Syndrome - JaffeLichtenstein Syndrome - occurs more commonly in females 3. Osteobla stoma / Osteiod Osteoma - arise most often in vertebrae and long bones - less common in the jaws and other craniofacial bones - posterior toothbearing regions of the maxilla and mandible are the usual sites of jaw involvement - 2nd decade of life - 90% of lesions presenti ng before the age of 30 years Males (2:1) - pain, often quiet severe, is usually associated with osteoid osteoma - localized swelling may occur - nocturnal pain is relieved by aspirin - duration of signs and symptoms of osteoblastoma ranges from weeks to years composed of irregular trabeculae of osteoid and immature bone within a stroma - may arise in maxilla and mandible 2nd to 5th decade males - usually solitary, except in patients 2 distinct variants - well circumscribes and have a mixed lucent-opaque pattern - a thin radiolucency may be noted surrounding a calcified central tumor mass - cementoblastoma - ossifying fibroma - fibrous dysplasia - osteosarcoma Conservative surgical approach (curettage or local excision) Good - exostoses of the jaws - osteoblastoma Surgical excision Good Osteoblastom a - uncommon primary lesion of bone - lesion greater than 1.5 cm in diameter Osteoid osteoma - represent a smaller version - lesion less than 1.5 cm in diameter 4. Osteoma - cause is unknown (trauma, 1. composed of Downloaded by Micheal KL (up828456@myport.ac.uk) lOMoARcPSD|3413111 infection, and developmental abnormalities) - facial and skull bones - within the paranasal sinuses with Gardner‟s syndrome s of life - headaches, recurrent sinusitis and opthalmologic complaints have been noted (depending on the lesion location) relatively dense, compact bone with sparse marrow tissue - osteoid osteoma - odontoma 2. consist of lamellar trabeculae of cancellous bone with abundant fibrofatty marrow Periosteal osteoma – asymptomatic - slow-growing - bony (hard masses) - asymmetry (when lesions enlarge) Endosteal osteoma – discovered during routine radiographic examination, as dense, wellcircumscribed radiopacities Periosteal osteoma – arise on the surface of the bone Endosteal osteoma – develop centrally within bone 5. Central Giant Cell Granulo ma ii. Malignant Tumors 1. Osteosarco ma Etiology: reparative response to intrabony hemorrhage and inflammation - once regarded as reactive lesion Osteogenic Sarcoma maxilla and mandible mandible – involves the jaws anterior to the permanent molars (few cases reported – facial bones, small bones of the hands and feet) children and young adults 75% presenti ng before the age of 30 years Female s ( 2:1) - mandible is more commonly - 2nd decade of life convent ional osteosa - produces a painless expansion or swelling of the affected jaws - cortical plates are thinned composed of uniform fibroblasts in a stroma containing collagen - presence of multinucleated giant cells consist of multilocular or unilocular radiolucency of bone - margins of the lesion are well demarcated. Often presenting scalloped border - “aggressive” CGCG - may cause pain and exhibit rapid growth, root resorption, perforation of cortical bone - ameloblastoma - odontogenic myxoma - odontogenic keratocyst - ameloblastic fibroma - ossifying fibroma - adenomatoid odontogenic tumor Excision or curettage followed by removal of the peripheral bone margins Good prognosis ( thru excision or curettage) - swelling and localized pain - loosening - all osteosarcomas have a - early osteosarcoma – localized - scleroderma - chronic osteomyelities Surgical procedure and chemotherapy for jaw osteosarcoma - mandibular Downloaded by Micheal KL (up828456@myport.ac.uk) For children – higher rate of recurrence lOMoARcPSD|3413111 classification (accdg. to the site of origin) 1. conventional type – arising within the medullary cavity 2. juxtacortical tumor – arising within the periosteal surface 3. extraskeletal osteosarcoma – arising rarely in soft tissue 2. Erwing’s Sarcoma cause is unknown Parosteal Osteosarcoma affected (7:1) - 60% arises in the body of the mandible - remaining sites: symphysis, angle of the mandible, ascending ramus, temporomand ibular joint - in maxilla, equal incidence in alveolar ridge and maxillary sinus - those arising from the jaws present 1 to 2 decade s later mean age: 35 years (8 to 85 ) commonly involves the distal femoral metaphysis peak inciden ce 39 years old rcoma – slight predilec tion for males - when long bones are affected :female predilec tion and displacement of teeth - paresthesia due to involvement of the inferior alveolar nerve - mucosal alteration – seen at latestage - average duration of symptoms - 3 to 4 months before diagnosis sarcomatous stroma that directly produces tumor osteoid - histologic patterns: 1. chondroblastic (most common) 2. osteoblastic 3. fibroblastic 4. telangiectatic widening of periodontal ligament space and resorption of the surrounding alveolar bone - slow-growing swelling or palpablemass well-differentiated radiodense and attached to the external surface of bone Treatment for Juxtacortical Osteosarcoma - either bloc resection or radical excision - composed of lobules of poorly differentiated malignant cartilage - the cortex of involved bone is intact and thickened - tumor is radiolucent - poorly defined periphery Treatment for Juxtacortical Osteosarcoma - either bloc resection or radical excision over-all 5-year survival rate: 80% proliferation of uniform, closely packed cells most common characteristic appearance is that of a moth-eaten destructive radiolucency of the medullary bone Multiple-method treatment - surgery and radiation Poor prognosis - clinical features presented before age 10 years - presence of metastatic disease and systemic symptoms - advance tumor – “moth-eaten” radiolucencies or irregular, poorly marginated radiopacities - metastatic carcinoma - calcifying epithelial odontogenic tumor (CEOT) - chondrosarcoma - fibrous dysplasia - malignant fibrous histiocytoma - “sun-ray” or „sunbursts” radioopaque appearance due to periosteal reaction - often accompanied by a dull, aching sensation tumor – better prognosis than maxillary - radical surgery – superior survival rate of 80% as compared with local or conservative surgery (25%) - osteosarcomas of the jaws - commonly recur (40% - 70%) with a metastatic rate of 25% to 50% - metastasizes to lung and brain than to regional lymph nodes - once the disease has become metastatic, the mean survival time is 6 months over-all 5-year survival rate: 80% - when jaws are affected :male predilec tion Periosteal Osteosarcoma commonly involve the upper tibial metaphysis peak age – 20 years old male predilec tion (2:1) 4% arises in the bones of the head and neck - 1% occurring in the jaws - most involve bones are the lower extremities and pelvis - jaws: ramus of the mandible betwee n 5 and 30 years – 90% Males – 60% Mean age: 11 years most common presenting symptoms -pain and swelling - facial deformity - destruction of alveolar Downloaded by Micheal KL (up828456@myport.ac.uk) lymphoma/leukemia - metastatic neuroblastoma - mesenchymal chondrosarcoma - for local control - chemotherapy - for systemic micrometastases lOMoARcPSD|3413111 (involvi ng the bone of the head and neck) bone with loosening of teeth - mucosal ulcer Downloaded by Micheal KL (up828456@myport.ac.uk) - high erythrocyte sedimentation rate - elevated serum lactate dehydrogenase value - thrombocytosis - mandibular tumors: more favorable overall survival than in other bone site lOMoARcPSD|3413111 ODONTOGENIC TUMORS DISEASE OTHER TERM/S 1. Basal Cell Carcinoma (Malignant) Basal Cell Epitheliom a CAUSE Rodent Ulcer LOCATION AGE SEX CLINICAL HISTOPATH -arises from basal cell of the skin -most prevalent cancer of the skin, head and neck - non-hairbearing skin older patients male (because of greater cumulative sun exposure) individuals at increased risks for the development of basal cell carcinoma 1. those with lighter natural skin pigmentation 2. those with long history of chronic sun exposure 3. those with one of several predisposing hereditary syndromes - presents as an indurated pearly papule or nodule with telangiectatic vessels coursing over its surface - the center of the tumor becomes ulcerated and crusted - generally slow growing - rarely metastasizes - nest and cords of cuboidal cells arise from the region of the salepidermal basal cells -occurs on sun-exposed skin 2. Leukoplaki a (Premalignant) a clinical term indicating a white patch or plaque of oral mucosa that cannot be rubbed off or scrapped off and cannot be characteri zed clinically as any other disease Pre- unknown cause RADIOGRAPH - patches are greyish in color - lesions are irregularly shaped - lesions can be flat but can also be rough and textured - patches are thick and hardened - may be sensitive to touch and to extreme temperatures or spicy food Downloaded by Micheal KL (up828456@myport.ac.uk) DIFFERENTIAL DIAGNOSIS TREATMENT PROGNOSIS lOMoARcPSD|3413111 disposing Etiologies : 1.Smoking 2. Alcohol 3. Syphilis 4. Sunlight 5. Virus – EpsteinBarr Virus (EBV) & Human Papilloma Virus (HPV) 6. Fungus – Candida Albicans 7. Trauma/Irr itation 8. Nutritional deficiencie s/Spices 9. Sepsis 10. Hormonal Imbalance 3. Oral Submucou s Fibrosis - typically affects the buccal mucosa, lips, retromolar areas and the soft palate. - occasional involvement of the pharynx and esophagus - early lesions present as a blanching of the mucosa, imparting a mottled, marble-like appearance - later lesions demonstrate palpable fibrous bands running vertically in the buccal mucosa and in a circular fashion around the mouth opening or lips - as the disease progresses the mucosa becomes stiff, causing difficulty in eating and considerably restricting the patient's ability to open the mouth (trismus). If Downloaded by Micheal KL (up828456@myport.ac.uk) - There is no effective treatment for oral submucous fibrosis and the condition is irreversible once formed - Plastic surgery may be required to allow for improved opening of the mouth lOMoARcPSD|3413111 the tongue is involved, it becomes stiff and has a diminished size. - mucosal petechiae are seen in more than 10% of cases and most patients complain of a burning sensation, often aggravated by spicy foods - salivary flow is diminished and blotchy melanotic mucosal pigmentation is often seen 4. Squamous cell carcinoma 5. Erythropla kia 6. Leukoede ma - The most frequent oral sites of involvement, in decreasing order of frequency, are the lips (vermilion), lateral and ventral tongue, oral floor and soft palate. In the larynx, almost all cases occur on the vocal cords. - the lesion may appear more prominen t in smokers. - typically bilateral and is most often reported on the buccal mucosa although it can involve the floor of the mouth. asymptomatic red macule or patch on a mucosal surface The reason for the red color is unclear, but could be related to a combination of dilation and engorgement of the subepithelial microvascular system and a thinning of the keratin layer or of the entire epithelium. - the mucosal change may begin as early as 3-5 years of age, but is not usually noticeable until adolescence - by the end of the teenage years, 50% of - the lesion appears graywhite and may be folded resulting in a wrinkled appearance - the lesion does not rub off - the lesion disappears or is greatly diminished - should always be removed or destroyed, A conservative surgical procedure such as mucosal stripping is usually performed, with minimal damage to deeper connective tissues. - The microscopic features show acanthosis and intracellular edema of the spinous layer. Rete ridges are broad and elongated. Downloaded by Micheal KL (up828456@myport.ac.uk) No treatment is required It has no malignant potential and does not change significantly after 25-30 years of patient age. Should the affected individual stop using tobacco products, the lesion will - hundreds of lesions have demonstrated a malignant transformation rate of 14-50% - clinical follow-up should be examined every 3 months for the first year and semi-annually for an additional 4 years. lOMoARcPSD|3413111 black children demonstrate the altered mucosa. when the buccal mucosa is stretched asymptomatic, bilateral, whitish gray, semitranspare nt macule of the buccal mucosa Downloaded by Micheal KL (up828456@myport.ac.uk) likely become less pronounced.