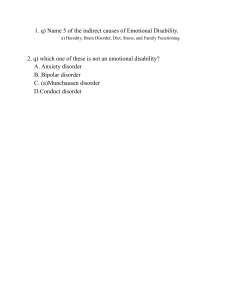
ABNORMAL PSYCHOLOGY PSYCHOPATHOLOGY - Scientific study of psychological disorders ➢ 3 Concepts • Clinical Description - Unique combination of behaviors, thoughts and feelings that make up a specific disorder. - [we based our diagnosis in DSM – V] - Clinical Judgement, as a practitioner you should know how to diagnose the client - Clinical Eyes, we tend to be observant to our clients • Etiology - Origins and cause which include biological, psychological and social dimensions. - Biopsychosocial Model, one of the things we used that is etiology or theory when it comes to knowing what the roots or the cause of a disorders. • Treatment and Outcome - Pharmacology, Psychological or combined - Pharmacology, (medicines, medication for depression etc.) - Psychological, (therapy or counseling) » Difference between psychologist and psychiatrist? - Psychiatrists (Are doctor of medicine, with specialized training in psychiatry and they can provide medication or can prescribe medication - Psychologist cannot prescribe medication but focus mostly on psychotherapy or talk therapy. - Based on research, the best treatment is the combination of both. ➢ Clinical Description • Presenting Problem - Why the person came to the clinic - What are their concerns • Prevalence - How many people in the population have the disorder Example: 1 person out of 100 people have a schizophrenia • Incidence - How many new cases occur during a given period. - How many people in the population Example: How many people had depression during the pandemic. • Course - Individual pattern of a disorder ▪ Chronic – last a long time (Example: Schizophrenia) ▪ Episodic – recover and suffer a recurrence at a later time (Example: mood disorders, depressive disorders) ▪ Time – limited – it will improve without treatment (distress, depressive symptoms) • Onset - Start of the disorder ▪ Acute – begin suddenly (depression due to triggers [anxiety disorder or phobias]) ▪ • ▪ ▪ • • • • • - • • ▪ ▪ ▪ - Insidious – develop gradually over an extended period. Most dangerous and poorer prognosis (Example: schizophrenia) Prognosis Anticipated course of a disorder (looking at the history and case formulation of an individual) “The prognosis is good” – therefore there will have a good outcome “The prognosis is guarder” – there will be a poor prognosis PSYCHOLOGICAL DISORDER A psychological dysfunction within an individual that is associated with distress or impairment in functioning and a response that is not typical or culturally expected. Psychological Dysfunction [Internal] Breakdown in cognitive, emotional, or behavioral functioning [you are unable to perform your usual action] Personal Distress Situation is extremely upsetting Can’t tolerate by simple coping mechanisms Atypical or Not Culturally Expected [Deviance] It deviates from the average (norms) Violation of social norms Disability [external are affected] Impairment in some important areas of life Danger To self and others Not all people who have psychological disorders are dangerous. MODELS IN EXPLANING ABNORMALITY Diathesis – Stress Model Individuals inherit tendencies to express certain traits or behaviors, which may then be activated under conditions of stress. Diathesis, inherited tendencies [you are predisposed to have psychological disorders] + Stress, [stressors] = Disorder [when you are high in inherited tendencies and even have a low stress, you are predisposed or predicted to have a disorder. On the other hand, if you don’t have or have low inherited tendencies and even have a high stress, there is a possibility that you will not develop a disorder.] Gene – Environment Correlation Model Also known as Reciprocal Gene – Environment Model in different references. Genetic endowment may increase the probability that an individual will experience stressful life events. “Influence of Genes” Even if stress is not present, it is the gene that leads us to stressful situations to have disorders. • - Neuroscience Model How the brain works is central to any understanding of our behaviors, emotions, and cognitive processes. - Neurotransmitters Selective serotonin reuptake inhibitors (SSRIs) are the most prescribed antidepressants. They are given most with people having major depressive disorder. • Psychological • BioPsychoSocial ❖ How do biological, psychological, and sociocultural factors interact in the development of complex patterns of abnormal behavior? - They interact with each other, and they contribute into a specific disorder. - In studies, it is proven that Anxiety disorders and depression have evidences from biopsychosocial model. CLINICAL ASSESSMENT AND DIAGNOSIS • Clinical Assessment - Systematic evaluation and measurement of psychological, biological, and social factors in an individual presenting with a possible psychological disorder - [looking for different factors, perspective in diagnosing disorder] ▪ Physical examination - Medical condition ▪ Behavioral assessment - Direct observation - Rating scales ▪ Psychological Testing - Projective test - Personality inventories - Intelligence testing - Neuropsychological testing ➔ Symptoms - Subjective - From the client/patient’s perspective ➔ Signs - Objective - From the psychologist/psychiatrist - Can be measured by assessment tools • Diagnosis - Process of determining whether the particular problem afflicting the individual meets all criteria for a psychological disorder, as set forth in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, or DSM – 5. • ▪ ▪ ▪ ▪ 1. 2. 3. 4. 5. • ▪ ▪ ▪ ▪ ▪ - Provisional diagnosis, if the criteria is not meet but you as a clinician based on your clinical judgement believe that they will meet it. Assessment Reliability Consistency Validity Measures what it designed to measure Standardization Application of certain standards to ensure consistency across different measurements. Mental Status Exam Appearance and Behavior Overt behavior (seen) Attire Appearance, posture, expressions Thought Processes Rate or flow of speech Delusions Hallucinations Mood and Affect Down, elated, depressed Inappropriate, blunted, or flat Intellectual Functioning Vocabulary Memory Sensorium General awareness Person, place, time Case Formulation Presenting problem Chief complaints [What client present experience] Precipitating factors Triggers Actual events Predisposing factors Vulnerabilities Perpetuating factors Maintaining factors [What maintain the presenting problems] Protective factors Areas of competency, skill, talents, interest, and supportive elements. [Where clinician based for the prognosis of the client] It protects the individual - Where the clinician based their intervention for the client. DIAGNOSTIC AND STATISTICAL MANUAL OF MENTAL DISORDERS (DSM – 5) » About the DSM – 5 ➢ Publish last 2013 by the American Psychiatric Association ➢ Removed the Five – Axis Diagnosis System [because misdiagnosis and overdiagnosis happens] ➢ Inclusion of new assessment measures ➢ 20 Chapters Describing Mental Disorders (Section II) ➢ Other Specified Disorder - Clinician records the specific reason a particular client does not meet the criteria for a specific diagnosis. ➢ Unspecified Disorder - Clinician cannot specify or choose not to specify • DSM – 5 – TR ➢ Released on March 2022 ➢ Addition of Prolonged Grief Disorder (PGD) to Section II – a new disorder for diagnosis ➢ Someone close to the bereaved person has died within at least 6 months for children and adolescents, or within at least 12 months for adults. ➢ Prolonged Grief Disorder (Criteria) » Gain major criticism because… - This disorder is under trauma and stress related disorders. - Cannot measure grief [cannot know when to move on or move forward from the death of someone] • MENTAL DISORDERS » Some terms to remember… ➢ Ego Syntonic - Actions that are aligned/acceptable to the self [“I’m normal, there is nothing wrong with me” (Example: Personality Disorders, Anorexia Nervosa)]. ➢ Ego Dystonic - Actions that are inconsistent with your ego - (Example: - Majority of disorder is ego dystonic [both ego syntonic and dystonic is rooted in psychoanalysis] ➢ Alloplastic - Individual attempts to change the environment or situation - [others should adjust] ➢ Autoplastic - Changing oneself when confronted by a problem or stressful situation - [accept the problem and start the change] ➔ NEURODEVELOPMENTAL DISORDERS - Commonly diagnose during developmental period [usually before child enters grade school or during grade school - Cannot diagnose a child until they can interact with people. • Intellectual Disability (Intellectual Developmental Disorder) - The following three criteria must be met: A. Deficits in intellectual functions (problem solving, abstract thinking) - We can say that it has a deficit if it is in 2 standard deviations (30) below the mean (70 and below). B. Deficits in adaptive functioning that result in failure to meet developmental and sociocultural standards for personal independence and social responsibility. - [difficulty in academic, self-management (basic hygiene can’t be done), thoughts (inappropriate in age level)]. C. Onset of intellectual and adaptive deficits during the developmental period. - [during childhood and adolescence] • Communication Disorders ➢ Language Disorder - Difficulties in the acquisition and use of language across modalities - [Differential diagnosis: has a reduce vocabularies (Example: Selective mutism – instances that a child is not talking in a specific situations)] ➢ Speech Sound Disorder - Difficulty with speech sound production that interferes with speech intelligibility - [having a difficulty or change the way it pronounces words] ➢ Childhood – onset Fluency Disorder (stuttering) - Frequent repetitions or prolongations of sounds or syllables and by other types of speech dysfluencies - [broken words, words pronouns and whole word repetitions] ➢ Social (Pragmatic) Communication Disorder - Primary difficulty with pragmatics or the social use of language and communication - [has a difficulty in the use of language in social context] • Autism Spectrum Disorder ➢ Persistent impairment in reciprocal social communication and social interaction (Criterion A), and - [there’s a tendency to have difficulty on interacting with others and to have eye contact.] ➢ Restricted, repetitive patterns of behavior, interests, or activities (Criterion B) - [preoccupied in certain behavior or object] ➢ Symptoms are present from early childhood and limit or impair everyday functioning (Criteria C and D). • Attention – Deficit/Hyperactivity Disorder (ADHD) ➢ A persistent pattern of inattention and/or hyperactivity – impulsivity that interferes with functioning or development. ➢ Inattention manifest behaviorally in ADHD as wandering off task, lacking persistence, having difficulty sustaining focus, and being disorganized and is not due to defiance or lack of comprehension ➢ Hyperactivity refers to excessive motor activity (such as a child running about) when it is appropriate, or excessive fidgeting, tapping, or talkativeness. ➢ Impulsivity refers to hasty actions that occur in the moment without forethought and that have high potential for harm to the individual (e.g., darting into the street without looking)/ ➢ Specify whether (for 6 months): - Combined presentation - Predominantly inattentive presentation - Predominantly hyperactive/impulsive presentation • Specific Learning Disorder ➢ Persistent difficulties learning keystone academic skills (Criteria A), with onset during the years of formal schooling (i.e., the developmental period – 6 months) ➢ Impairment in reading – Dyslexia ➢ Impairment in mathematics – Dyscalculia - Having low IQ is not require in having a specific learning disorder, because it focuses on the keystone academic skill. • Motor Disorders ➢ Developmental Coordination Disorder - The acquisition and execution of coordinated motor skills is substantially below that expected given the individual’s chronological age and opportunity for skill learning and use. - [too clumsy, dropping or dumping into objects, difficulties in catching object and using scissors] ➢ Stereotypic Movement Disorder - Repetitive, seemingly driven, and apparently purposeless motor behavior - [Example: clapping or running] – paulit ulit na ginagawa ng bata ➢ Tic Disorder - Presence of motor and/or vocal tics before 18 years old. - A tic is sudden, rapid, recurrent, nonrhythmic motor movement or vocalization ▪ Tourette’s Disorder - Both multiple motor and one or more vocal tic - More than 1 year ▪ Persistent (Chronic) Motor or Vocal Tic Disorder - Only motor or vocal tics are present - More than 1 year ▪ Provisional Tic Disorder - Motor and/or vocal tics may be present [both] - Less than 1 year ➔ » ✓ ▪ ▪ ▪ ▪ ▪ ▪ SCHIZOPHRENIA SPECTRUM AND OTHER PSYCHOTIC DISORDERS Key features that define the psychotic disorders Delusions – fixed belief that are not amenable to change in light of conflicting evidence. Persecutory – one is going to be harmed [oneself or others] Jealous – spouse or lover is unfaithful Grandiose – exceptional abilities, wealth, or fame [excessive belief about oneself] Erotomania – another person is in love with him or her [believe that someone like her/him] Somatic – problem in health and organ function Referential – gestures, comments, environmental cues are directed at oneself. [anything is directed to them] ▪ Nihilistic – major catastrophe will occur [having earthquake etc.] • Bizarre Delusion – implausible and not understandable to same – culture peers and do not derive from ordinary life experiences. ▪ Thought Withdrawal - One’s thought have been “removed” by some outside force ▪ Thought Insertion - Alien thoughts have been put into one’s mind [inject] ▪ Delusion of Control - One’s body or actions are being acted on or manipulated by some outside forces ✓ Hallucinations – perception – like experiences that occur without an external stimulus - Illusions have external stimulus but having different perception. ▪ Visual - Involve seeing things that aren’t there. ▪ Auditory - Most common type of hallucination. - Someone might hear someone speaking to them or telling them to do certain things. ▪ Tactile - Involve the feeling of touch or movement in the body which aren’t there or not present. ▪ Proprioceptive – flying or floating » 2 Kinds of Hallucinations that is normal ▪ Hypnagogic – while falling asleep ▪ Hypnopompic – upon waking up ▪ Broca’s Area - Responsible for the production of speech [scientist prove that there is an increase of blood flow and activity when there is an auditory hallucination in Broca’s area which means that the person experiencing auditory hallucination is hearing his or her own thoughts] - Most active during auditory hallucination Delusion ▪ Wernicke’s Area - Comprehension of speech Hallucination ✓ Disorganized Thinking (speech) – formal thought Disorganized thinking (speech) disorder Grossly Disorganized or Abnormal Motor Behavior ▪ Derailment or Loose Association (including catatonia - Switch from one topic to another - These are Positive symptoms (should not be present but it is present). ▪ ▪ ✓ ▪ ▪ ▪ ▪ ✓ - Rabbit to hair to jacket etc. Tangentiality Answers to questions may be obliquely related or completely unrelated Incoherence or “Word Salad” Severely disorganized that it is nearly incomprehensible Grossly Disorganized or Abnormal Motor Behavior (including Catatonia) Catatonia – marked decrease in reactivity to the environment Negativism – resistance to instructions Mutism and Stupor – lack of verbal and motor responses Catatonic Excitement – purposeless and excessive motor activity without obvious cause Negative Symptoms [dapat meron pero nawawalan] Decline Examples: ▪ ▪ ▪ ▪ ▪ ✓ • ➢ ➢ ➢ ➢ • ▪ ▪ ▪ - Diminished emotional expression – reductions in the expression of emotions Avolition – decrease in motivated self – initiated purposeful activities Alogia – diminished speech output Anhedonia – decrease ability to experience pleasure (Ex: Major Depressive Disorder) Asociality – lack of interest in social interactions Positive symptoms [dapat wala naman pero nag kakaroon] what makes them the same with each other Adding symptoms Delusional Disorder One or more delusions for 1 month or longer Not met the criteria for schizophrenia (have delusion and hallucination and more) Impairment in psychosocial functioning Subtypes: ▪ Erotomania ▪ Grandiose ▪ Jealous ▪ Persecutory ▪ Somatic ▪ Mixed ▪ Unspecified Psychotic Disorders Brief Psychotic Disorders Disturbance and sudden onset of positive symptoms 1 day to less than 1 month Schizophreniform Disorder Symptoms of schizophrenia 1 month to 6 months Schizophrenia At least 6 months or more than 6 months ➢ ➢ Two or more of the following: Delusion Hallucinations Disorganized speech Grossly disorganized or catatonic behavior Negative symptoms Impairment in functioning ➢ Phases of Schizophrenia - • ➢ ➢ ➢ ➢ ▪ Prodromal – experience but seems normal ▪ Active – positive symptoms are noticeable Negative symptoms might also happen ▪ Residual – manifest the negative symptoms [ people who undergo medication based on research]. Schizoaffective Disorder There is a major mood episode (major depressive or manic) concurrent with Criterion A (delusion, hallucination etc) of schizophrenia Delusions or hallucinations must be present for at least 2 weeks in the absence of a major mood episode (depressive or manic) at some point during the lifetime duration of the illness. [preceded for or followed by a mood episode (mood episode then psychotic episode), should not be present during in the same time] Major Depressive Disorder with psychotic features (occurs during the mood episodes) Experience manic then at the same time hallucination, then it is Bipolar Disorder I with psychotic features. Note: - Major depressive disorder and bipolar disorder with psychotic features occurs during the mood episode. While in Schizoaffective Disorder, mood episode and Criterion A of schizophrenia should not be present at the same time. ➔ BIPOLAR AND RELATED DISORDERS • Bipolar Disorders ▪ Bipolar I Disorder - It is necessary to meet the criteria for a manic episode - The manic episode may have been preceded by and may be followed by hypomanic or major depressive episodes. ▪ Bipolar II Disorder - It is necessary to meet the criteria for a current or past hypomanic episode and for the current or past major depressive episode • Cyclothymic Disorder ➢ 2 years (at least 1 year in children and adolescents) ➢ Numerous periods with hypomanic symptoms that do not meet criteria for a hypomanic episode ➢ numerous periods with depressive symptoms that do not meet criteria for a major depressive episode. - Suicide mostly present in depressive episode of bipolar disorder ➔ • ➢ ➢ ➢ ➢ » » DEPRESSIVE DISORDERS (present of sad, irritable, and angry mood) Disruptive Mood Dysregulation Disorder Chronic, severe persistent irritability This severe irritability has two prominent clinical manifestation: Frequent temper outburst Chronic, persistent irritable or angry mood that is present between the severe temper outbursts Present for 12 or more months Age of onset of the symptoms is before 10 years DMDD is made because there is an overdiagnosis of bipolar disorder to children Unipolar [consistent] » Individuals diagnose with DMDD, can be diagnose in turn in a longitudinal study they can be diagnose and they have higher risk developing major depressive disorder. • Major Depressive Disorder ➢ Five or more symptoms for 2 weeks (5 symptoms over 9) ▪ Feeling sad ▪ Loss of interest or pleasure ▪ Changes in appetite – weight loss or gain unrelated to dieting ▪ Trouble sleeping or sleeping too much ▪ Loss of energy or increased fatigue ▪ Increase in purposeless physical activity or slowed movements and speech ▪ Feeling worthless or guilty ▪ Difficulty thinking, concentrating, or making decisions ▪ Thoughts of death or suicide ✓ Suicide ▪ Suicidal ideation – thinking seriously about suicide ▪ Suicidal plan – formulation of a specific method for killing oneself ▪ Suicidal attempt – the person survives ▪ Completed suicide – the suicide has been made ✓ Types of Suicide by Emile Durkheim ▪ Altruistic – killing oneself will serve a greater societal good (sacrificing oneself) ▪ Egoistic – loss of social support (older adults are vulnerable to suicide because they loss social supports) ▪ Anomic – sudden and unexpected changes in situations (such as financial loss) ▪ Fatalistic – loss of control over one’s own destiny. (Example slave) • Persistent Depressive Disorder (Dysthymia) ➢ Depressed mood for most of the day, for more days than not, for at least 2 years or at least 1 year for children and adolescents ➢ Two or more of the following: ▪ Poor appetite or overating ▪ Insomnia or hypersomnia ▪ Low energy or fatigue ▪ Low self – esteem ▪ Poor concentration or difficulty making decisions ▪ Feeling of hopelessness • Premenstrual Dysphoric Disorder ➢ Expression of mood lability, irritability, dysphoria, and anxiety symptoms that occur repeatedly during the premenstrual phase of the cycle and remit around the onset of menses or shortly thereafter. ➢ These symptoms may be accompanied by behavioral and physical symptoms. ➢ Symptoms must have occurred in most of the menstrual cycles during the past year and must have an adverse effect on work or social functioning. ➔ ✓ ✓ • ➢ ➢ ➢ ➢ ➢ • ➢ ➢ ➢ ➢ ANXIETY DISORDERS Fear – is the emotional response to real or perceived imminent threat Stimulus is present Present Anxiety – is anticipation of future threat Stimulus is not present Future Separation Anxiety Disorder Excessive fear or anxiety concerning separation from home or attachment figures. They experience recurrent excessive distress when separation from home or major attachment figures is anticipated or occurs They worry about the well-being or death of attachment figures, particularly when separated from them, and they need to know the whereabouts of their attachment figures and want to stay in touch with them they also worry about untoward events to themselves, such as getting lost, being kidnapped, or having an accident, that would keep them from ever being reunited with their major attachment figure At least 4 weeks in children and adolescents; 6 month or more in adults Selective Mutism Consistent failure to speak in specific social situations in which there is an expectation for speaking (e.g., at school) despite speaking in other situations. The disturbance interferes with educational or occupational achievement or with social communication. The duration of the disturbance is at least 1 month (not limited to the first month of school). The failure to speak is not attributable to a lack of knowledge of, or comfort with, the spoken language required in the social situation. - Can be comorbid with PTSD • Specific Phobia Marked fear or anxiety about a specific object or situation (e.g., flying, heights, animals, receiving an injection, seeing blood). The phobic object (phobic stimulus) or situation almost always provokes immediate fear or anxiety. The phobic object or situation is actively avoided or endured with intense fear or anxiety. The fear or anxiety is out of proportion to the actual danger posed by the specific object or situation and to the sociocultural context. The fear, anxiety, or avoidance is persistent, typically lasting for 6 months or more. The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. ▪ Animal (e.g., spiders, insects, dogs). ▪ Natural environment (e.g., heights, storms, water). ▪ Blood-injection-injury (e.g., needles, invasive medical procedures). ▪ Situational (e.g., airplanes, elevators, enclosed places). ➢ ➢ ➢ ➢ ➢ ➢ ▪ Other (e.g., situations that may lead to choking or vomiting: in children, loud sounds or costumed characters). Note: - Specific phobia, one situation Agoraphobia, two or more situations • Social Anxiety Disorder (Social Phobia) ➢ Marked, or intense, fear or anxiety of social situations in which the individual may be scrutinized by others. ➢ When exposed to such social situations, the individual fears that he or she will be negatively evaluated. ➢ The social situations almost always provoke fear or anxiety ➢ The social situations are avoided or endured with intense fear or anxiety. ➢ The fear or anxiety is out of proportion to the actual threat posed by the social situation and to the sociocultural context. ➢ The fear, anxiety, or avoidance is persistent, typically lasting for 6 months or more. ➢ The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. • Panic Disorder ➢ Recurrent unexpected panic attacks (without triggers) ➢ A panic attack is an abrupt surge of intense fear or intense discomfort that reaches a peak within minutes, and during which time four or more of a list of 13 physical and cognitive symptoms occur. - (Palpitation, sweating, trembling, shortness of breath, feeling of choking, chest pain etc) - Avoid different situation because they fear having panic attack • Agoraphobia ➢ Marked, or intense, fear or anxiety triggered by the real or anticipated exposure to a wide range of situations where escape might be difficult, or help might not be available ➢ The diagnosis requires endorsement of symptoms occurring in at least two of the following five situations: ▪ Using public transportation, such as automobiles, buses, trains, ships, or planes. ▪ Being in open spaces, such as parking lots, marketplaces, or bridges. ▪ Being in enclosed spaces, such as shops, theaters, or cinemas. ▪ Standing in line or being in a crowd; or ▪ Being outside of the home alone. • Generalized Anxiety Disorder ➢ Excessive anxiety and worry (apprehensive expectation), occurring more days than not for at least 6 months, about a number of events or activities (such as work or school performance). ➢ The individual finds it difficult to control the worry. ➢ The anxiety and worry are associated with three (or more) of the following six symptoms (with at least some symptoms having been present for more days than not for the past 6 months); ▪ Restlessness or feeling keyed up or on edge. ▪ Being easily fatigued. ▪ Difficulty concentrating or mind going blank. Irritability. ▪ Irritability. ▪ Muscle tension. ▪ Sleep disturbance (difficulty falling or staying asleep, or restless, unsatisfying sleep). ➢ The anxiety, worry, or physical symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. ➢ The disturbance is not attributable to the physiological effects of a substance ➔ • ➢ ➢ - ➢ - ➢ ➢ • ➢ ➢ ➢ ➢ OBSESSIVE – COMPULSIVE AND RELATED DISORDERS Obsessive – Compulsive Disorder Presence of Obsession, compulsions, or both: Obsessions: Recurrent and persistent thoughts, urges, or images that are experienced, at some time during the disturbance, as intrusive and unwanted, and that in most individuals cause marked anxiety or distress. The individual attempts to ignore or suppress such thoughts, urges, or images, or to neutralize them with some other thought or action (i.e., by performing a compulsion) Compulsions: Repetitive Behavior (e.g., hand washing, ordering, checking) or mental acts (e.g., praying, counting, repeating words silently) The behavior or mental acts are aimed at preventing or reducing anxiety or distress, or preventing some dreaded events or situation; however, these behaviors or mental acts are not connected in a realistic way with what they are designed to neutralized or prevent or are clearly excessive. Thought Suppression (conscious forgetting) happens. The obsessions or compulsions are time – consuming (e.g., take more than 1 hour per day) or cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. Body Dysmorphic Disorder Preoccupation with one or more perceived defects or flaws in physical appearance that are not observable or appear slight to others At some point during the course of the disorder, the individual has performed repetitive behaviors (e.g., mirror checking, excessive grooming, skin picking, reassurance seeking) or mental acts (e.g., comparing his or her appearance with that of others) in response to the appearance concerns. The preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. The appearance preoccupation is not better explained by concerns with body fat or weight in an individual whose symptoms meet diagnostic criteria for an eating disorder. Note: - Body Dysmorphic Disorder differ from OCD since it is limited in body appearance. • Hoarding Disorder ➢ Persistent difficult discarding or parting with possession, regardless of their actual value. ➢ The hoarding causes clinically significant distress or impairment in social, occupational, or other important areas of functioning (including maintaining a safe environment for self and others). • Trichotillomania (hair – pulling disorder) ➢ Recurrent pulling out of one’s hair, resulting in hair loss. ➢ Repeated attempts to decrease or stop hair pulling ➢ The hair pulling causes clinically significant distress or impairment in social, occupational, or other important areas of functioning ➢ The hair pulling or hair loss is not attributable to another medical condition (e.g., a dermatological condition). ➢ The hair pulling is not better explained by the symptoms of another mental disorder (e.g., attempts to improve a perceive defect or flaw in appearance in body dysmorphic disorder). ➔ • ➢ ➢ ➢ • ➢ ➢ » - • ➢ ➢ ➢ ➢ ➢ ➢ TRAUMA AND STRESSOR – RELATED DISORDER Disorders related to Attachment Reactive Attachment Disorder Child rarely or minimally turns preferentially to an attachment figure for comfort, support, protection, and nurturance. (no reaction or attachment with people around them) Absent or grossly underdeveloped attachment between the child and putative caregiving adults. Evident before age 5 years and has a developmental age of at least 9 months. Disinhibited Social Engagement Disorder Culturally inappropriate, overly familiar behavior with relative strangers (lapit ng lapit kahit hindi kilala yung tao) Developmental age of at least 9 months Why have they become part of trauma and stressor related disorder? Because these children experience: ▪ Social neglect or deprivation ▪ Repeated changes of primary caregivers ▪ Rearing in unusual settings Posttraumatic Stress Disorder Exposure (direct exposure, witnessing the event, learning that the event occur in family member, you are expose to the details of the event) to actual or threatened death, serious injury, or sexual violence. Presence of one (or more) intrusion symptoms (memories, dreams etc.) Persistent avoidance of stimuli associated with the traumatic events, beginning after the traumatic event(s) occurred. Negative alterations in cognition and mood associated with the traumatic events(s) Marked alterations in arousal and reactivity associated with the traumatic event(s) More than 1 month - Can also be delayed, if the full the diagnostic criteria are not meet until/at least 6 months. • Acute Stress Disorder ➢ Developed of characteristic symptoms lasting from 3 days to 1 month following exposure to one or more traumatic events. • Adjustment Disorders ➔ DISSOCIATIVE DISORDER • Dissociative Identity Disorder ➢ Disruption of identity characterized by two or more distinct personality states, which may be described in some cultures as an experience of possession. • Dissociative Amnesia ➢ An inability to recall important autobiographical information, usually of a traumatic or stressful nature, that is inconsistent with ordinary forgetting. ▪ Localized Amnesia - Failure to recall events during a circumscribed period of time. ▪ Selective Amnesia - Can recall some, but not all ▪ Generalized Amnesia - A complete loss of memory for one’s life history ▪ Systematized Amnesia - Memory for a specific category of information (a specific person for example) ▪ Continuous Amnesia - Forgets each new event as it occurs • Depersonalization/Derealization Disorder ➢ The presence of persistent or recurrent experiences of depersonalization, derealization or both. ▪ Depersonalization - Experiences of unreality, detachment, or being an outside observer with respect to one’s thoughts, feelings, sensations, body, or actions. ▪ Derealization - Experiences of unreality or detachment with respect to surrounding ➔ SOMATIC SYMPTOMS AND RELATED DISORDER • Somatic Symptoms Disorder - people with somatic disorder are having a physical manifestation of pain but does not have medical basis. • Illness Anxiety Disorder ➢ Preoccupation with having or acquiring a serious illness ➢ Somatic symptoms are not present or, if present, are only mild in intensity ➢ There is a high level of anxiety about health, and the individual is easily alarmed about personal health status. ➢ - Illness preoccupation has been present for at least 6 months “Hypochondriasis” Severe anxiety on having developed a serious disease. 3 Common behaviors in person with Illness Anxiety Disorder 1. Researching their sickness 2. Self – diagnosis 3. Hospital hopping • Conversion Disorder (Functional Neurological Symptoms Disorder) ➢ One or more symptoms of altered voluntary motor or sensory functions - Physical malfunctioning with no organic cause, means there are parts of their body which is not functioning without cause - People with conversion disorder happens when they experience traumatic event and it’s become a way for them to cope. ▪ La belle indifference - in different with themselves (being okay with the changes or to the sickness that happen to them) - Should not be used for the diagnosis of conversion disorder • Factitious Disorder ➢ Falsification of physical or psychological sign or symptoms, or induction of injury or disease, associated with identified deception. - Known as faking but because of primary gain (internal) such as attention, sympathy, and pity from other people - Also known as Munchausen syndrome ▪ Munchausen Syndrome by proxy (imposed on another (by proxy) - When there is a proxy, it means that you are faking other people’s sickness - Usually seen in close relationship like mother and child. ▪ Malingering (faking) - Known as faking but because of secondary gain (external) such as avoiding responsibilities in school or work, for financial reason etc. ➔ • ➢ - FEEDING AND EATING DISORDER Pica Persistent eating of nonnutritive, nonfood substances over a period of at least 1 month. Pica is an eating disorder in which people compulsively eat one or more nonfood items or non-nutritive substances, such as ice, clay, paper, ash, or dirt. - Pica disorder often occurs with disorders associated with impaired functioning according to DSM – V. - Usually seen in people with anorexia nervosa • Rumination Disorder ➢ Repeated regurgitation of food over a period of at least 1 month. Regurgitated food may be re-chewed, re-swallowed, or spit-out. • Avoidant/Restrictive Food Intake Disorder • Anorexia Nervosa ➢ Persistent energy intake restriction. ➢ Intense fear of gaining weights or of becoming fat, or persistent behavior that interferes weight gain; and ➢ Disturbance in self – perceived weight or shape. - Common method of losing weight utilized by people is rigorous physical exercise. o 2 types of Anorexia Nervosa ▪ Restricting type (dieting, fasting, and/or excessive exercise) - Exercising in order to lose weight and limiting calorie intake - Common type of anorexia nervosa ▪ Binge – eating – purging type (recurrent episode of binge eating or purging behavior) - Having binge eating and purging • Bulimia Nervosa ➢ Recurrent episode of binge eating - Eating large amounts of food (binge eating) - They feel guilty then engaged in Purging techniques through induced vomiting (pagpilit sumuka) - Also used laxatives and diuretics ➢ The binge eating and inappropriate compensatory behavior both occur, on average, at least once a week for 3 months. • Binge – eating Disorder ➢ Recurrent episode of binge eating without compensatory behaviors. ➢ Marked distress regarding binge eating is present ➢ The binge eating occurs, on average, at least once a week for 3 months. ➔ SEXUAL DYSFUNCTION Sexual Response Cycle ▪ ▪ ▪ ▪ ▪ • ▪ ▪ ▪ • ➢ Desire Phase – sexual urges occur in response to sexual cues or fantasies. Arousal Phase – Plateau Phase – brief period occurs before orgasm Orgasm Phase – Resolution Phase – decrease in arousal occurs after orgasm (particularly in men). Orgasmic Disorder Delayed Ejaculation Marked delay in ejaculation (for 6 months) Marked infrequency or absence of ejaculation Early Ejaculation Ejaculation that occur prior to or shortly after penetration (within 1 minute) for 6 months Female Orgasmic Disorder Marked delay in, marked infrequency of, or absence of orgasm (for 6 months) Markedly reduced intensity of orgasmic sensation Erectile Disorder • ➢ • ➢ - Female Sexual Interest/Arousal Disorder Lack of, or significantly reduced, sexual interest/arousal, as manifested by at least 6 months When a female doesn’t have sexual urges and fantasies Male Hypoactive Sexual Desire Disorder Persistently or recurrent deficit (or absent) sexual/erotic thoughts or fantasies and desire for sexual activity (minimum duration of approximately 6 months) When a male doesn’t have sexual urges and fantasies ➔ PARAPHILIP DISORDER Difference: • Paraphilia ➢ Intense and persistent atypical sexual interest. • Paraphilic Disorder ➢ Paraphilia that is currently causing distress or impairment to the individual or a paraphilia whose satisfaction has entailed personal harm or risk of harm, to others. • Voyeuristic Disorder ➢ Over a period of at least 6 months ➢ Recurrent and intense sexual arousal from observing an unsuspecting person who is naked ➢ At least 18 years of age • Exhibitionistic Disorder ➢ Over a period of at least 6 months ➢ Recurrent and intense sexual arousal from the exposure of one’s genitals to an unsuspecting person ➢ Exposing Genitals to: Prepubertal children, physically mature individual, or both. • Frotteuristic Disorder ➢ Over a period of at least 6 months ➢ Recurrent and intense sexual arousal from touching or rubbing against a nonconsenting person, as manifested by fantasies, urges or behavior. • Sexual Masochism Disorder ➢ Over a period of at least 6 months ➢ Recurrent and intense sexual arousal from the act of being humiliated, beaten, bound, or otherwise made to suffer as manifested by fantasies, urges or behavior. • Sexual Sadism Disorder ➢ Over a period of at least 6 months ➢ Recurrent and intense sexual arousal from the physical or psychological suffering of another person, as manifested by fantasies, urges or behavior. • Pedophilic Disorder ➢ Over a period of at least 6 months ➢ Recurrent and intense sexual arousing fantasies, sexual urges or behaviors involving sexual activity with a prepubescent child or children (generally age 13 years or younger) ➢ Caused marked distress or interpersonal difficulty ➢ The individual is at least age 16 years and at least 5 years older than the child or children in Criterion A. • Fetishistic Disorder ➢ Over a period of at least 6 months ➢ Recurrent and intense sexual arousal from either the use of nonliving objects or a highly specific focus on non – genital body part(s) as manifested by fantasies, urges or behavior. • Transvestic Disorder ➢ Over a period of at least 6 months ➢ Recurrent and intense sexual arousal from crossdressing, as manifested by fantasies, urges or behavior. ➔ ➢ o o o ➢ o - PERSONALITY DISORDER CLUSTER A: Odd or Eccentric Disorders Paranoid Personality Disorder Pervasive distrust and suspiciousness Schizoid Personality Disorder Detachment from social relationship People who isolate themselves Flat affect or having restricted emotions For them relationship is messy and undesirable. Schizotypal Personality Disorder Eccentricities of behavior Have magical thinking, or belief that only them believes and governs their behavior. CLUSTER B: Dramatic, emotional, or erratic Antisocial Personality Disorder Disregard for and violation of the rights of others Anti to social norms (don’t like to follow rules) Should be 18 years old and above Characterized by lack of remorse (they get satisfaction for disobeying the rules) and empathy, criminal minds of sociopath. - Also been referred to as psychopath, sociopath, or dissocial personality disorder. ▪ Asocial - it is the apparent lack of interest in social interactions but not also be a manifestation of limited opportunities for social interaction. - avoiding social interaction, inconsiderate and hostile to others - lack of social skills and relationships. ▪ Conduct disorder - Mostly seen in children, who disregard to follow rules and social standards. - May display pattern of disruptive and violent behaviors. - Children with conduct disorder eventually will developed having antisocial personality disorder. ▪ Sociopathy - Having a criminal mind. o Borderline Personality Disorder - Instability of interpersonal relationship o o ➢ o ❖ - o o ▪ ❖ - Fear abandonment from their caregivers They respond in rage aggression, self-mutilating behavior and feeling of loneliness and helplessness. Have a poor identity, roller coaster emotions, impulsivity, and instability in interpersonal relationship. Bordering the edge of having psychosis or neurotic tendencies Only personality disorder which is linked to mood disorder. Histrionic Personality Disorder Have a pervasive and excessive emotionality and attention – seeking behavior. They are extroverted, flirtatious, sexual seductive, not into intimate relationship, promiscuity and wants to be the center of attraction. Narcissistic Personality Disorder Pervasive pattern of grandiosity, need for admiration, and lack of empathy. Characterized by exaggerated sense of self – importance and self – entitlement. CLUSTER C: Anxious or Fearful Avoidant Personality Disorder Also have social inhibition Have a inferiority complex Characterized by shyness, avoidance, embarrassment, and low self – esteem. What is the difference between Schizoid P.D and Avoidant P.D? The difference is that people with schizoid personality disorder are loners by choice and don’t want to build relationship because for them it is messy and undesirable while people that have avoidant personality disorder wants to form relationship, they just could not make one because they fear rejection and humiliation. Dependent Personality Disorder Pervasive need to be taken care of Cannot survive with other people and depend to other for emotional and physical needs. Obsessive – Compulsive Personality Disorder Preoccupation with orderliness, perfectionism, and mental and interpersonal control at the expense of flexibility, openness, and efficiency. Individual with obsessive – compulsive personality disorder is primarily motivated by a need for control. Obsessive Compulsive Disorder Thinking/thoughts are irrational or severe to release that’s why it has compulsion (with psychological stressor). What is the difference between OCD and OCPD? People with OCD experience stress and anxiety because they are ego dystonic while people with OCPD are ego syntonic. Ego dystonic, behavior is incongruent with the image they have. (They know that they should not do the behavior they are doing that is why they become anxious and stress). Ego Syntonic, the behavior is congruent or inclined with the image they have to themselves. ➔ IMPULSE CONTROL DISORDER - People who experience high degree of tension and the only way to relive themselves is to do the act. (Have the urge to do it to feel relive) ➢ Kleptomania - Recurrent failure to resist urges to steal objects. - Another feature of kleptomania is that they may surreptitiously (secretly) return an object they have stolen. ➢ Intermittent Explosive Disorder - Acting out their aggressive impulses ➢ Pyromania - Irresistible urge to set fire • - Fragile X Syndrome Happens when X chromosomes is susceptible to damage. (X chromosomes is fragile or madaling masira). - People with Fragile X Syndrome have problems with their intellectual capacities because cognitive ability of an individual comes from the X chromosomes (which is from the mother because of their two X chromosomes). - Mostly seen in both male and female, but most common in men. - Men: have long and narrow face and large ears (shown in physical appearance in men) - Women: extreme shyness • Down Syndrome (Trisomy 21) - Down syndrome is a genetic disorder. It is also called trisomy 21. It includes certain birth defects, learning problems, and facial features. (a child is having an extra copy of chromosome 21). o Characteristics: ▪ Simian Crease - Hands have only one line in the palm ▪ They have flattened nose and face, and upward slanting eyes ▪ Hypotonia (floppiness) - Low muscle tone - Called floppy babies • Capgras Syndrome - They believe that someone they know has been replaced by a double or impostor. - The best way to talk to them was to hide the person they believed has been replaced and let them hear their voice, because they can distinguish its voice and can confirm that it is the person they know. - People with Capgras syndrome loss the sense of familiarity • Cotard’s Syndrome (Emil Regis) - They believe that they are dead. ▪ Another form of Cotard’s syndrome wherein they believe that they loss their organs or one type of organ in their body. • • - Gambling Disorder Gambling Disorder is not considered a type of Obsessive Compulsive Disorder because a person with gambling disorder derives direct pleasure from the behavior. Under substance abused and related disorders and not OCD. Hypersomnolence Disorder is a condition marked by excessive and chronic daytime and nighttime sleepiness but still feel tired after waking up. • • o o • o o o o • - Sleep inertia (natulog pero parang hindi natulog) is a symptom which is most likely to indicate the presence of Hypersomnolence disorder. Alzheimer’s Disease Episodic memory, is the type of memory does people with Alzheimer’s typically lose. Has an insidious onset, which means that Alzheimer’s disease progresses slowly over time. (At first the symptoms are not apparent until the advanced stages.) Types of Amnesia Anterograde Amnesia Individual loses his ability to create new memories Retrograde Amnesia Individual loses their past memories Kinds of Affect Blunted affect Significantly reduce of affect of the person. Restricted affect Affect is reduced but not as significant as the blunted one, Flat affect Without emotion Labile affect Inappropriate of emotions Cataplexy Sudden and brief loss of muscle control due to intense emotions.