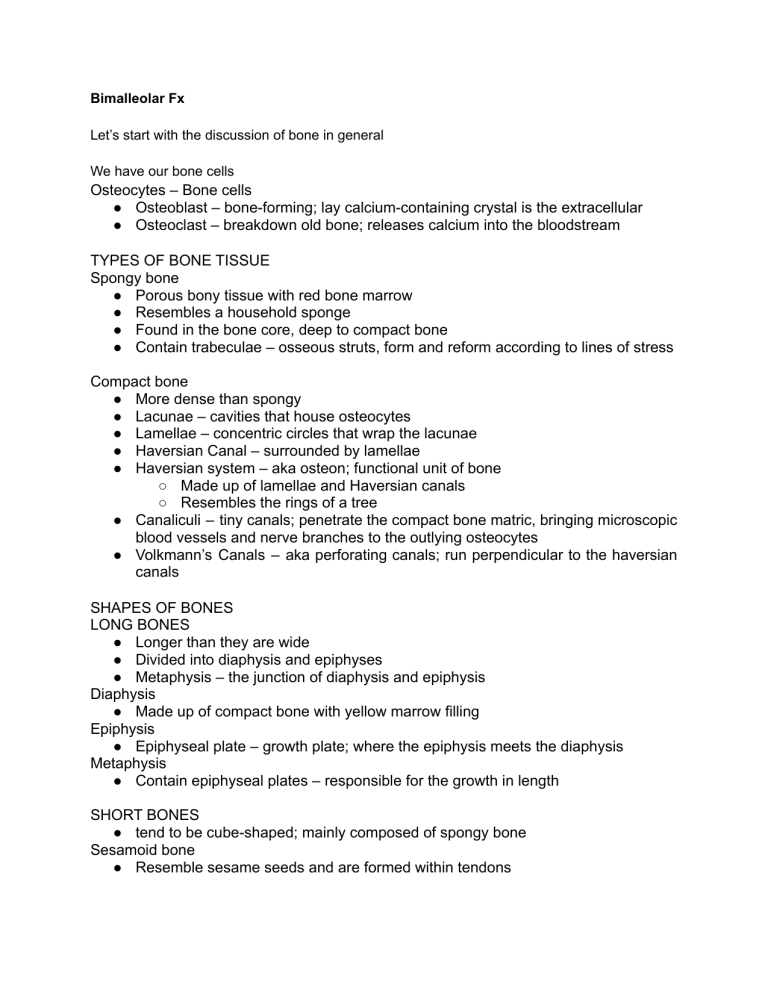
Bimalleolar Fx Let’s start with the discussion of bone in general We have our bone cells Osteocytes – Bone cells ● Osteoblast – bone-forming; lay calcium-containing crystal is the extracellular ● Osteoclast – breakdown old bone; releases calcium into the bloodstream TYPES OF BONE TISSUE Spongy bone ● Porous bony tissue with red bone marrow ● Resembles a household sponge ● Found in the bone core, deep to compact bone ● Contain trabeculae – osseous struts, form and reform according to lines of stress Compact bone ● More dense than spongy ● Lacunae – cavities that house osteocytes ● Lamellae – concentric circles that wrap the lacunae ● Haversian Canal – surrounded by lamellae ● Haversian system – aka osteon; functional unit of bone ○ Made up of lamellae and Haversian canals ○ Resembles the rings of a tree ● Canaliculi – tiny canals; penetrate the compact bone matric, bringing microscopic blood vessels and nerve branches to the outlying osteocytes ● Volkmann’s Canals – aka perforating canals; run perpendicular to the haversian canals SHAPES OF BONES LONG BONES ● Longer than they are wide ● Divided into diaphysis and epiphyses ● Metaphysis – the junction of diaphysis and epiphysis Diaphysis ● Made up of compact bone with yellow marrow filling Epiphysis ● Epiphyseal plate – growth plate; where the epiphysis meets the diaphysis Metaphysis ● Contain epiphyseal plates – responsible for the growth in length SHORT BONES ● tend to be cube-shaped; mainly composed of spongy bone Sesamoid bone ● Resemble sesame seeds and are formed within tendons ● Strengthen the tendon and improve the traction mechanics of the corresponding muscle Flat Bones Spongy bone of flat bones is the location for hematopoiesis. ● Cranial bones, sternum, scapula, clavicle, ribs, ilium IRREGULAR BONES ● Have unique shapes ● Examples: vertebrae, ischium and pubis WORMIAN BONES ● Aka intrasutural bones/ sutural bones ● Small, irregular bones found along sutures of the cranial bones ● OS INCAE & PTERION OSSICLE TYPES OF FRACTURE There are many types of fractures, but the main categories are: 1. Displaced or non-displaced – refers to the alignment of the fractured bone 2. Open fracture or closed fracture Displaced or Complete fracture-The bone snaps into two or more parts and moves so that the two ends are not lined up straight. ● Transverse: the break is in a straight line across the bone. ● Spiral: the break spirals around the bone. ● Oblique: the break is diagonal across the bone. ● Impacted: compression of two bones driven to each other. The fragments are jammed tightly together and the fracture line is indistinct. ● Comminuted: the bone fragments into several different pieces. Displacement: ● Translation (shift) – The fragments may be shifted sideways, backward or forward ● Angulation (tilt) – The fragments may be tilted or angulated in relation to each other. ● Rotation (twist) – One of the fragments may be twisted on its longitudinal axis; Length – The fragments may be distracted and separated, or they may overlap, due to muscle spasm, causing shortening of the bone Non-displaced or Partial fracture- The bone cracks either part or all of the way through, but maintains its proper alignment. ● Greenstick fracture: the bone is bent, but not broken all the way through; Compression: the bone is crushed and flattens in appearance. Mostly seen in adults, mainly in vertebral bodies, calcaneum and tibial plateau. Open fracture- The bone breaks through the skin. This is an important difference from a closed fracture because with an open fracture there is a risk of a deep bone infection. Other types of fracture: ● Avulsion: a fragment of bone is pulled off, often by a tendon or ligament. ● Stress fracture: or “hairline fracture,” is like a crack and may be difficult to see with regular X-rays. ● Pathologic fracture: caused by a disease that weakens the bone. ● Growth plate fracture: at the joint that can result in shorter bone length; present only in children. STAGES OF BONE HEALING There are three stages of bone healing: the inflammatory, reparative, and remodeling stages. 1. The Inflammatory Stage ● This tells the body to stop using the injured part so it can heal. ● Other cells that come to the area during this stage form a hematoma (blood clot) around the broken bone. This is the first bridge between the pieces of the broken bone. ● Inflammation is at its peak 48 hours after a fracture. 2. The Reparative Stage ● The reparative stage starts within about a week of the injury. A soft callus (a type of soft bone) replaces the blood clot that formed in the inflammatory stage. The callus holds the bone together, but isn't strong enough for the body part to be used. ● Over the next few weeks, the soft callus becomes harder. ● By about 2–6 weeks, this hard callus is strong enough for the body part to be used. ● The repair phase persists for several months; it can be divided into two distinct phases: soft and hard callus formation. 3. The Remodeling Stage ● The remodeling stage starts around 6 weeks after the injury. ● In this stage, regular bone replaces the hard callus. If you saw an X-ray of the healing bone, it would look uneven. But over the next few months, the bone is reshaped so that it goes back to looking the way it did before the injury ○ Stage of clinical union- -when the fracture site is firm enough that it no longer moves, it is clinically united. ○ Stage of radiologic union: when temporary callus has been replaced by mature lamellar bone Introduction When people talk about ankle fractures, they are usually referring to an injury to the bones of the tibia and fibula, The ends of these bones commonly called the medial malleolus (end of the tibia) and lateral malleolus (end of the fibula) are the bony bumps that you feel on the inner and outer side of the ankle, are the bony bumps that you feel on the inner and outer side of the ankle. There are different types of ankle fractures that can occur ● When a bimalleolar ankle fracture occurs, there is an injury to both the medial malleolus (inner side of the ankle) and the lateral malleolus ● One special subset of these fractures is called a bimalleolar equivalent fracture ○ This typically occurs when there is a fracture of the lateral malleolus and a ligament injury on the inner side of the ankle (the deltoid ligament) ○ While this particular injury does not involve a bone injury on the inner side of the ankle, the ligament injury that has occurred causes the ankle joint to become unstable and requires surgical treatment to stabilize the joint ● People who sustain a trimalleolar ankle fracture also have a bone injury at the back of the tibia called the posterior malleolus Simply put, the more bones that are broken, the more unstable the ankle becomes Anatomy and physiology Three bones make up the ankle joint: ● Tibia - shinbone ● Fibula - smaller bone of the lower leg ● Talus - a small bone that sits between the heel bone (calcaneus) and the tibia and fibula The tibia and fibula have specific parts that make up the ankle ● Medial malleolus - inside part of the tibia ● Posterior malleolus - back part of the tibia ● Lateral malleolus - end of the fibula Two joints are involved in ankle fractures: Ankle joint - where the tibia, fibula, and talus meet ● The ankle joint is composed of 2 joints ○ The true ankle joint contains the tibia (medial wall), fibula (lateral wall), and talus (the floor upon which the tibia and fibula rest) ○ The true ankle joint allows dorsiflexion and plantar flexion ○ The subtalar joint consists of the talus and the calcaneus. The subtalar joint allows the foot to be inverted or everted Syndesmosis joint - the joint between the tibia and fibula, which is held together by ligaments these can also be called as the high ankle sprain Ligaments The lateral collateral ligament complex has three components: the anterior talofibular (ATFL), posterior talofibular (PTFL), and calcaneofibular ligaments The medial collateral ligament (MCL) complex lies deep to the medial flexor tendons and is divided into four components: the anterior and posterior tibiotalar, tibionavicular, tibiospring, and tibiocalcaneal ligaments The syndesmotic ligament complex comprises the anterior-inferior tibiofibular (AITFL), posteroinferior tibiofibular (PITFL), and transverse tibiofibular ligaments and the interosseous membrane. Tendons of the Lateral Ankle ● Peroneus brevis ● Peroneus longus ● Both serve as the major everters of the ankle ● Also serve as plantar flexors Tendons (medial side) ● Major tendons ● Anterior tibialis (dorsi-flexor) ● Achilles tendon (plantar flexor) ● Medial tendons ● ● ● Posterior tibialis (inverter and plantar flexor) Flexor digitorum longus Flexor hallucis longus Summary ● Osseous structures: ○ Tibia, fibula, talus ● Ligaments: static stabilizers ○ Lat, med, syndesmotic ● Muscles/ tendons: Dynamic stabilizers ○ DF and PF ○ Inverters: post and ant tibialis ○ Everters: peroneals Pathophysiology Like what I have just said, The primary motion of the ankle at the true ankle joint (tibiotalar joint) is plantarflexion and dorsiflexion. Inversion and eversion occur at the subtalar joint Excessive inversion stress is the most common cause of ankle injuries for 2 anatomic reasons ● First, the medial malleolus is shorter than the lateral malleolus, allowing the talus to invert more than evert ● Second, the deltoid ligament stabilizing the medial aspect of the ankle joint offers stronger support than the thinner lateral ligaments. As a result, the ankle is more stable and resistant to eversion injury than inversion injury Lauge Hansen First Word: position of foot at time of injury 2nd word: force applied to foot relative at time of injury Types: ● SER (40-75% of all ankle fx) ○ ATFL lig tear → Spiral or oblique distal fib fx → PM fx or PTFL TEAR → Transverse MM fx or deltoid lig tear ● SA (10-20% of all ankle fx) ○ Low avulsion LM fx or Lat lig injury → MM fx ● PER (7-19%) ○ Maisonnueve fx (syndesmosis instability) ○ MM fx → ATFL tear → Fib fx above ankle of mortise ○ PM fx or PTFL tear ● PA (5-20%) ○ MM fx → ATFL tear → fib fx Etiology Doctors classify ankle fractures according to the area of bone that is broken ● According to the Lauge Hansen classification: supination and external rotation (SER) injury are the most common cause of bimalleolar fractures ● They often occur from ○ Twisting or rotating your ankle ○ Rolling your ankle ○ Tripping or falling ○ Impact during a car accident Clinical Manifestations Because a severe ankle sprain can feel the same as a broken ankle, every ankle injury should be evaluated by a physician Common symptoms for a broken ankle include ● Immediate and severe pain ● Swelling ● Bruising ● Tender to touch ● Cannot put any weight on the injured foot ● Deformity Intervention Like what I said, a complete and thorough examination of the involved extremity is needed to avoid misdiagnosis and prevent unnecessary radiographs Ankle X-ray is the best initial investigation, requiring three views: AP (subtle fx), Mortise (15-20 deg IR) (talus positioning and syndesmosis widening), Lat view Sometimes the tenderness is present in the proximal leg in addition to the widening of the syndesmosis, This presentation calls for an image for the tibia and fibula to diagnose this injury called Maisonneuve fracture To reiterate, the more bones that are broken, the more unstable the ankle becomes, hence, Most bimalleolar fractures are unstable fractures and require treatment with open reduction internal fixation Non operative ● Uses a below-knee cast for six weeks or a total contact cast for three months in patients with diabetes or when the patient cannot tolerate surgical fixation Operative ● ORIF is indicated when the fracture is unstable, such as in a talar shift. The technique is by fibula fixation using plates and screws (lateral malleolus) and medial malleolus fixation using cannulated screws ● If the posterior malleolus fracture is more than 25%, a CT scan is necessary, and it requires posterior fixation using cannulated screws Prognosis ● ● ● can have a poor prognosis, depending on the patient and operation, like the elderly, persons with diabetes, and especially those with comorbidities In general, full weight-bearing takes time and is usually only possible at 12 to 16 weeks, but it generally takes up to 6 months to achieve full weight-bearing with final functional recovery With operative intervention, the mortality at one year after the surgery is 12% in patients older than 65 years And that concludes my medical and surgical report thank you for listening