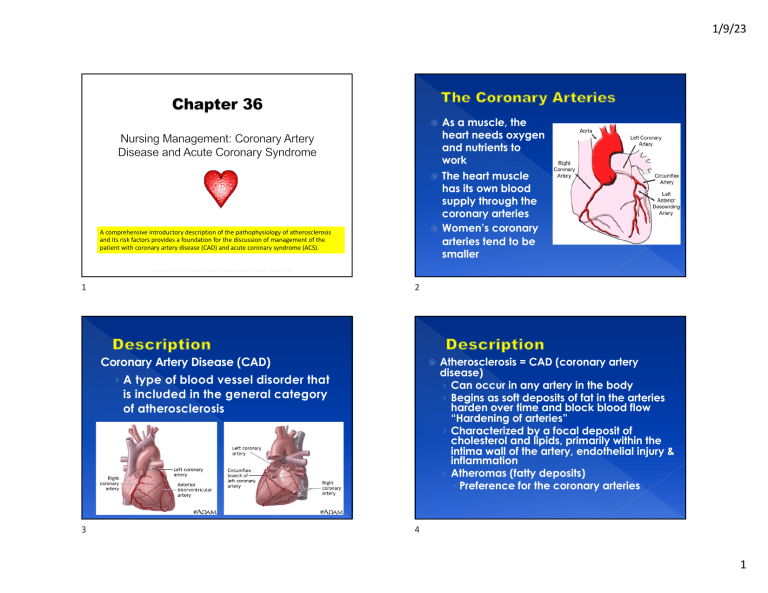
1/9/23 As a muscle, the heart needs oxygen and nutrients to work The heart muscle has its own blood supply through the coronary arteries Women’s coronary arteries tend to be smaller A comprehensive introductory description of the pathophysiology of atherosclerosis and its risk factors provides a foundation for the discussion of management of the patient with coronary artery disease (CAD) and acute coronary syndrome (ACS). Copyright © 2019 Elsevier Canada, a division of Reed Elsevier Canada, Ltd. 1 2 Coronary Artery Disease (CAD) › A type of blood vessel disorder that is included in the general category of atherosclerosis 3 Atherosclerosis = CAD (coronary artery disease) › Can occur in any artery in the body › Begins as soft deposits of fat in the arteries harden over time and block blood flow “Hardening of arteries” › Characterized by a focal deposit of cholesterol and lipids, primarily within the intima wall of the artery, endothelial injury & inflammation › Atheromas (fatty deposits) Preference for the coronary arteries 4 1 1/9/23 Arteriosclerotic heart disease (ASHD) Cardiovascular heart disease (CHD) Ischemic heart disease (IHD) CAD 5 6 Figure 36-01. Pathogenesis of atherosclerosis. A, Damaged endothelium. B, Fatty streak and lipid core formation. C, Fibrous plaque. Raised plaques are visible: some are yellow; others are white. D, Complicated lesion: thrombus is red; collagen is blue. Plaque is complicated by red thrombus deposition. Over time ….a series of events within the artery › A fatty streak (permanent)– can start in young children › Fat – ( lipid) deposits throughout the years › Narrowing and impaired blood flow occurs with the gradual occlusion as plaque thickens and blood clots form 7 7 8 2 1/9/23 Healthy endothelium is nonreactive to platelets & leukocytes and fibrin Endothelial lining injury (damage) is the major cause of atherosclerotic disease Damage/Injury from: › › › › › Hyperlipidemia › Hypertension › Diabetes › Infections › Immune Reactions › Tobacco use 9 Produced by the liver Nonspecific marker of inflammation Increased in many patients with CAD Chronic exposure to CRP triggers the rupture of plaques 10 Endothelial alteration ® › Platelets are activated › Growth factor stimulates smooth muscle proliferation & thickening of the arterial wall 11 Bacteria and/or viruses may have role in damaging endothelium by causing local inflammation C-reactive protein (CRP) › Cell proliferation entraps lipids, which calcify over time and form an irritant to the endothelium on which platelets adhere and aggregate › Thrombin is generated › Fibrin formation and thrombi occur causing further narrowing or total occlusion Collaterals are tiny “extra” blood vessels Same as “detours” around atherosclerotic plaques – Think of EC Row construction! Occur normally in coronary circulation Collaterals increase in the presence of chronic ischemia When occlusion occurs slowly over a long period, there is a greater chance of adequate collateral circulation developing 12 3 1/9/23 Copyright © 2019 Elsevier Canada, a division of Reed Elsevier Canada, Ltd. Copyright 2023 Elsevier Inc. All rights reserved. 13 13 14 Prescribed Meal Plan (Dietitian) Home Blood Glucose monitoring Regular exercise – at least 150 min/wk Medications – pills or Insulin or both Ongoing Education- Diabetes classes Support – family and friends Physician follow-up or Specialist referral Target is HgbA1C <7% 15 ANGINA AND ACUTE CORONARY SYNDROME (ACS) 16 4 1/9/23 Principles Ischemia = DECREASED blood flow to tissue When myocardial oxygen demand exceeds the ability of the coronary arteries to supply the heart tissue with oxygen – ischemia occurs – result is damage to the heart muscle Occurs with narrowing (plaque build up- atherosclerosis) of Coronary Arteries 17 Principles Infarction = ABSENT blood flow to tissue Results of sustained ischemia, causing irreversible myocardial cell death (necrosis) 80-90% due to formation of a thrombus Oxygenated blood is unable to flow distal to the occlusion 18 Factors Determining Myocardial Oxygen Needs (p.807) Assessment of Chest Pain (p. 807) Thorough and accurate assessment is vital Copyright 2023 Elsevier Inc. All rights reserved. 19 20 5 1/9/23 Relationships Among CAD, Stable Angina, and MI Assessment Cont’d Classic symptoms: “crushing”, “elephant sitting on my chest”, “heaviness”, radiating down left arm or up into the jaw, diaphoresis, “ashen” skin Locations: substernal, retrosternal or epigastric Non-classic symptoms: weakness, “heartburn”, shortness of breath, N &V 21 22 COMPARISON OF MAJOR TYPES OF when the lack of oxygen supply is ANGINA (p.808) Results temporary and reversible **ISCHEMIA Type Etiology Characteristics Chronic stable angina Myocardial ischemia, usually secondary to CAD • Episodic pain lasting 5–15 min Prinzmetal's angina Coronary vasospasm Microvascular angina Myocardial ischemia secondary to microvascular disease affecting the small, distal branches of the coronary arteries • More common in women Unstable angina Rupture of thickened plaque, exposing thrombogenic surface • New-onset angina • Provoked by exertion • Relieved by rest or nitroglycerin • Occurs primarily at rest • Triggered by smoking and increased levels of some substances (e.g., histamine, epinephrine, cocaine) • May occur in presence or absence of CAD • Triggered by activities of daily living (e.g., shopping, work) vs. physical exercise (exertion) • Treatment may include nitroglycerin • Chronic stable angina that increases in frequency, duration, or severity • Occurs at rest or with minimal exertion • Pain refractory to nitroglycerin 23 Chronic Stable Angina Ischemia of the myocardial tissue – REVERSIBLE Due to increased demand of oxygen to tissue or a lack of sufficient blood flow Chest pain occurs intermittently over a long period with the same pattern of onset (predictable), duration, and intensity of symptoms Predictable activities result in chest pain ie. Climbing stairs, sexual activity, lifting heavy objects Can be controlled with medications on an outpatient basis – Nitroglycerine (see Acute Coronary Syndrome for pt teaching) Pain is brief (3-5 min) Subsides when the precipitating factor is relieved Pain at rest is unusual Pressure, aching, squeezing, heavy (not usually sharp or stabbing), indigestion Substernal mostly (May radiate to jaw, shoulders, down arms, between shoulder blades) 24 6 1/9/23 Silent Ischemia Prinzmetal’s Angina Occurs without clinical symptoms such as chest pain. Noted by ST-segment changes only and may place a patient at higher risk for adverse outcomes and even death. Individuals with diabetes are especially at risk Occurs at rest usually due to spasm of a major coronary artery Spasm may occur in the absence of CAD Rare form of angina More common in clients with a hx of migraines and Raynaud’s phenomenon Why? 25 26 Interprofessional Management: Drug Therapy (p. 808) Nitroglycerine (short & long- acting) 27 A.K.A. Variant Angina Dilates coronary arteries to increase blood flow Dilates peripheral blood vessels to decrease SVR, decrease venous blood return, decrease myocardial o2 demand Sublingual for acute attacks (spray or tabs) Transdermal- long-acting (small amount released over 12/24 hours) **Headache, dizziness due to significant drop in BP – take when laying or sitting down – never standing up (orthostatic hypotension) Flushing and tingling sensation normal 1 metered spray or 1 tab SL q5min x3 prn- if symptoms unchanged or worse = CALL 911 Do not mix with erectile disfunction meds Interprofessional Management: Drug Therapy Cont’d See TABLE 36.11 Page 810 1. 2. 3. 4. 5. Antiplatelets (ASA, Aspirin) Adenosine Diphosphate Receptor Antagonists( Plavix) Nitrates (Nitroglycerin short and long acting) B-Adrenergic Blockers (Atenolol, Metoprolol) Calcium Channel Blockers (Diltiazem, Amlodipine, Verapamil) 6. ACE inhibitors (Enalopril) 7. Opioid analgesics (morphine) 28 7 1/9/23 Acute Coronary Syndrome (ACS) • Encompasses the spectrum of unstable angina, non–STsegment–elevation myocardial infarction (NSTEMI), and STsegment–elevation myocardial infarction (STEMI) • Both are unpredictable • *NOT immediately reversible • Myocardial cell damage and death are the result of decreased or absent blood flow TIME = MUSCLE DAMAGE • Cannot reverse myocardial cell death BUT can prevent further cell death with rapid treatment 29 30 Unstable Angina (UA) NSTEMI Angina that is: New in onset, occurs at rest, or has a worsening pattern Unpredictable Associated with deterioration of a once stable atherosclerotic plaque S/S: Chest pain or discomfort (due to ischemia) A strange feeling, pressure, or ache in the chest Constrictive, squeezing, heaving, choking, or suffocating sensation Fatigue, SOB, indigestion and anxiety 31 Myocardial Infarction (MI) • Sustained ischemia – results in myocardial cell death (NECROSIS) • 80-90% due to thrombus formation • No blood flow = myocardium can’t contract = decreased CO • Most common artery: Left coronary artery (feeds the left ventricle) • Described as the anatomical location of the affected artery • *Collateral circulation helps to supply the affected tissue • Who has a better prognosis? 25 year old or a 60 year old 32 8 1/9/23 M.I. Clinical Manifestations M.I. Clinical Manifestations Cont’d PAIN – Severe, immobilizing chest pain not relieved by rest, position change, or nitrate administration • Initially, elevated BP & HR • As cardiac output drops, BP may lower • If low BP, poor perfusion to organs including kidneys leading to low urine output • Right and left sided heart failure have different S & S • Abnormal heart sounds • Dysrhythmias are the most common cause of death with an MI • Can develop heart failure, cardiogenic shock • The hallmark of an MI • N&V • Sympathetic Nervous System Stimulation (clammy, diaphoretic, increased HR and BP (BP may drop later due to decreased CO) • Fever – within 1st 24 hours, last up to one week 33 34 Diagnostic Studies (UA & MI) Diagnostic Studies Cont.’d • ECG – looking for elevation or depression of ST segment Normal ST Elevation FIGURE 36-8 Collaborative care: chronic stable angina and acute coronary syndrome. ACE, angiotensin-converting enzyme; ARBs, angiotensin II receptor blockers; ASA, acetylsalicylic acid; CABG, coronary artery bypass graft; CBC, complete blood cell count; CK-MB, creatine kinase, muscle and brain; CT, computed tomography; ECG, electrocardiogram; IV, intravenous; O2, oxygen; PCI, percutaneous coronary intervention. *See Table 36-11. †See Table 36-5. ‡See Tables 36-2, 36-3, and 36-4. 35 36 9 1/9/23 Cardiac Markers Diagnostic Studies: Acute Coronary Syndrome (Cont.) CREATINE KINASE (creatine phosphokinase) (CK-MB) qIncreased in > 90% of MI patients. qBegins to rise 3-12 hours qPeaks 24 hours qReturns to normal in 2 - 3 days TROPONIN qMyocardial muscle protein released after an injury qTroponin T and Troponin I are cardiac specific indicators of an MI qNormal Troponin T (<0.1mcg/L), Troponin I (0.5mcg/L) qMuch more specific than CK-MB qRises quickly and remains elevated for 2 weeks 37 Copyright © 2019 Elsevier Canada, a division of Reed Elsevier Canada, Ltd. 38 38 Coronary Angiography (Cardiac Catheterization) Coronary Angiogram • A diagnostic test using x-rays to record the passage of a contrast dye in the heart • To identify the presence, location and nature of any coronary artery disease • The heart valves and heart muscle can also be assessed 39 40 10 1/9/23 Collaborative Care UA & MI Nursing Responsibilities • Pre-procedure: pedal pulses, allergies to shellfish, vitals for baseline, client education – “warm feeling” Emergency Treatment: M = morphine O = oxygen N = nitrates A = ASA (chewable, 160 mg) • Post-procedure: Check femoral site for bleeding, *mark shadowing, pressure bandage, distal pulses, vital signs, assess for dysrhythmias, lay flat 6 hours ¯ oxygen demand and/or ­ oxygen supply • Complications: bleeding from puncture site, dysrhythmias, infection 41 Nitrate therapy Stent placement 42 Collaborative Care Percutaneous Coronary Intervention (PCI) – Surgical intervention alternative – Same procedure as an angiography – but opens up artery – “reopens” artery – goal is to perform within 90 minutes – Can “clean out” the artery and/or place a stent – Performed with local anesthesia – Ambulatory 24 hours after the procedure – Nursing care: same as coronary angiography (cardiac cath) 43 44 11 1/9/23 The Coronary Stent Procedure • Laser angioplasty – Performed with a catheter containing fibers that carry laser energy – Used to precisely dissolve the blockage – Same procedure as a PCI – but uses a laser • A coronary stent is a small tubular wire object inserted into a coronary artery at the time of angioplasty to keep the previously narrowed artery open 45 46 The animation referenced below can be viewed in the PowerPoint Animations asset. Coronary Artery Bypass Surgery (CABG) Myocardial revascularization (CABG) Primary surgical treatment for CAD Patient with CAD who has failed medical management or has advanced disease is considered a candidate • Is open heart surgery, which a bypass (detour) is made to go around an area of blockage in a coronary artery Used to treat abrupt or threatened abrupt closure and restenosis following PCI (percutaneous intervention) • Bypasses are usually taken from the leg veins or an artery from the inside of the chest wall • May be 1 or more cardiac arteries which are “bypassed” Angioplasty with Stent Copyright © 2019 Elsevier Canada, a division of Reed Elsevier Canada, Ltd. 47 47 48 12 1/9/23 Collaborative Care – Drug Therapy Inclusion/Exclusion Criteria – See Table 36-13, p. 816 • Fibrinolytic Therapy – Stops the infarction by dissolving the thrombus through an IV infusion – Needs to be given within 2-3 hours of the onset of chest pain, no greater than 12 hours – “Clot Busters” Tissue Plasminogen Activator (Alteplase) – But…..they dissolve ALL clots in the body – Major Complication: Hemorrhage 49 50 Collaborative Care – Drug Therapy Collaborative Care – Drug Therapy Anti-Ischemic Therapy – ACE Inhibitors (ex. ramipril) • Helps to prevent remodeling and prevent/slow heart failure – Beta Blockers • Decreases myocardial workload – prevents dysrhythmias • Initiate within 24 hours of a STEMI in patients with no contraindications Anti-Ischemic Therapy Nitroglycerine Dilates coronary arteries to increase blood flow Sublingual for acute attacks or IV Morphine Vasodilator Monitor for bradypnea or hypoxia 51 52 13 1/9/23 Antidysrhythmia medications – ex. Amiodarone Cholesterol-lowering drugs – ex. Lipitor; Zocor • Draw fasting lipid panel Stool softener • Bedrest, opioid administration, prevent vagal stimulation that cause bradycardia 53 Drug Therapy – Antithrombotic Therapy Antiplatelet – Aspirin, Clopidogrel Anticoagulant a. Unfractionated Heparin (IV Heparin) » Typically reversible with protamine sulfate » Lab test for PTT b. Low Molecular-Weight Heparin (ex. enoxaparin) » Has less of an effect on thrombin compared to Heparin » Lab test for Plt (normal range 150-400 x 109/L) – must be > 100 54 Nursing Care During Hospitalization Home Care • Pain assessment • Monitoring – BP, ECG, vitals, cardiac markers, hydration status • Rest & Comfort – promote rest = decreases myocardial oxygen demand – activity level will gradually increase • Anxiety – The entire family is your patient! Patient and family teaching are an integral part of the healing process • Cardiac rehabilitation • Client teaching – activities, new medications (ASA or antiplatelet, use of Nitro, Beta-Blockers, etc.) • Physical activity: Teach how to check pulse rate, engage is supervised physical activity initially through cardiac rehab • Sexual Activity: often neglected area of health teaching – assess the psychological status of patient and partner – take Nitro prophylactically – do not consume a heavy meal prior to sexual activity – sexual activity may resume on average 7-10 days post MI depending upon physical condition Emotional & Behavioural Reactions: – Denial – Anger – Anxiety and Fear – Dependency – Depression – Realistic Acceptance *Maximize social support systems 55 56 14 1/9/23 Sudden Cardiac Death • Risk of CAD • Lethal ventricular dysrhythmia • Occurs within 1st hour of acute symptoms (angina, palpitations) • First sign of illness in 25% of people who die from heart disease • V-tach, V-fibrillation are most common causes • Immediate treatment-CPR, defibrillate, epinephrine, amiodarone, 57 15






