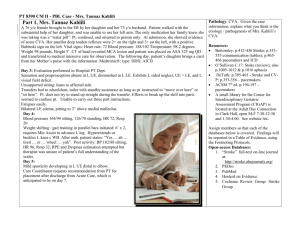
CVA and ICP Case Study & content N232 2022 CVA learning outcomes Identify risk factors, signs & symptoms, and nursing care for CVA Describe the prevention and early recognition of a TIA and an evolving CVA Compare the differences between an ischemic and hemorrhagic CVA Develop a plan of care for a patient in the recovery phase of a CVA (case study) Who is at risk? •Non-Modifiable Risk Factors •Age •Male •Race • •Modifiable • Risk Factors HTN, •A-Fib, •Hyperlipidemia, •Obesity •Smoking, •Diabetes What is a CVA/Stroke ? A stroke occurs when blood flow to the brain is interrupted by a blocked (ischemic – 80%) or burst (hemorrhagic – 20%) blood vessel The duration, severity, and location of cerebral ischemia determine the extent of brain function and thus the severity of stroke. Hot Stroke Code Stroke: Time is Brain YouTube CLIC K HERE This Photo by Unknown author is licensed under CC BY-SA-NC. Types of Strokes Ischemic Stroke – Blood clot or blockage of Large flow arteryto blood thrombotic brain tissue Small penetrating artery thrombotic Cardiogenic embolic Cryptogenic Other Hemorrha gic stroke How do the symptoms differ? ISCHEMIC MAIN PRESENTING SYMPTOMS • NUMBNESS OR WEAKNESS OF THE FACE, ARM, OR LEGESPECIALLY ON ONE SIDE OF THE BODY HEMORRHAGIC MAIN PRESENTING SYMPTOMS • “EXPLODING HEADACHE” • DECREASED LEVEL OF CONSCIOUSNESS Transient Ischemic Attack (TIA) What assessme nt do you do if you suspect a CVA? Suspected stroke priority interventions on the ward Get help and assess the patient• Vital Signs, BG, GCS, and neurological symptoms • Note the Last Time Normal (LTN)- when last seen without symptoms/are they on anticoagulants? • Physician must be notified immediately (SBAR) • What diagnostic test will they be sent for? Treatment for hemorrhagic stroke Emergency treatment of hemorrhagic stroke focuses on controlling the bleeding and reducing pressure in the brain caused by the excess fluid. Tissue Plasminogen Activator (TPA) AKA Alteplase Tissue plasminogen activator is a protein involved in the breakdown of blood clots. It catalyzes the conversion of plasminogen to plasmin, the major enzyme responsible for clot breakdown. • Rapid diagnosis of ischemic CVA and initiation of TPA within 3-4.5 hours leads to a decrease in the size of the stroke and an overall improved functional outcomes. TPA questions In an ischemic stroke, when would it be contraindicated to administer TPA? What is the priority assessment during and postadministration? Diagnostics for CVA CT Scan • A computed tomography scan is a medical imaging technique used to obtain detailed internal images of the body. The personnel that perform CT scans are called Angiography • Cerebral angiography is a procedure that uses a special dye (contrast material) and x-rays to see how blood flows through the brain. • What procedure could they do here to return Angiograph y Magnetic Resonance Imaging (MRI) A magnetic resonance imaging (MRI) is an imaging test that uses powerful magnetic forces, radiofrequency (RF) waves and a computer to make detailed 3-dimensional pictures of the organs, bones and tissues inside your body. Some MRI scans require a. contrast medium. MRI scanning can be challenging to obtain urgently in an Emergency Department setting. This must be considered in decision-making and not delay decisions CVA diagnostics Carotid continued Ultrasound Carotid ultrasound is a safe, painless procedure that uses sound waves to examine the blood flow through the Carotid ultrasound and endarterectomy (CEA) Most common surgical procedure for patients with TIA’s and mild stroke that are caused by carotid artery stenosis Used to prevent stroke in patients with Pharmacological Interventions Antihypertensives Anticoagulants Platelet-inhibiting medications: clopidogrel All stroke patients should be assessed for their risk of developing venous thromboembolism (deep vein thrombosis and pulmonary embolism). Patients at high risk include those who are unable to move one or both lower limbs; those who are unable to mobilize independently; a previous history of venous thromboembolism; dehydration; and comorbidities such as cancer Stroke deficit Terminolog y • • Hemiplegia Hemiparesis Stroke Deficit Terminology con’t Ataxia Stroke deficit terminology con’t DYSPHAGIA Stoke deficit terminolo gy Con’t Dysphasia/Aph asia Hemianop sia Case study 76 years old admitted with CVA three day ago. Patient was at home sitting at the table about to eat breakfast when the patient suddenly couldn’t move the left arm, speech became slurred and had a facial droop. Patient's spouse noticed these changes and called 911. Upon arrival to ER, Patient had slurred gobbled speech, left facial droop, no movement to left arm and left leg. Vital Signs BP: 220/120, HR:89 irreg, RR:26 O2sat:94% R/A, Temp 36.5 Hyperlipidemia HTN Past medical history A-fib MI COPD smoked 1 pkg a day X 60 yrs Father had HTN, CAD and died of an MI at age 45. Family History Mother Type II Diabetes and HTN and died of stoke at age 70. Brother has HTN and CAD Medications Home Meds Hydrochlorothiazide (HCTZ) 25mg PO OD, Ramipril 2.5mg PO OD, Warfarin 1mg, Atorvastatin 10mg PO OD, Advair 2 puffs BID Hospital meds HCTZ 25mg OD, ASA 81mg OD, Metoprolol 25mg PO BID, Ramipril 5mg PO OD, Atorvastatin 10mg PO OD, Enoxaparin 60mg SC OD, Warfarin 3mg PO OD, Clopidogrel 75mg PO OD, Pantoprazole 40mg PO OD, Advair 2 puffs BID, Ventolin neb Q4hr PRN, Morphine 5-10mg SC Q4h PRN, Risperidone ODT 0.5mg TID PRN, Risperidone 0.5mg PO TID PRN, Dimenhydrinate 50mg IV PO Q4hr PRN, Metoclopramide 10mg IV Q6hr PRN What needs to happen before our patient is allowed to eat or drink or take oral meds? What Diagnostic Test is priority in hot stroke? Why? CT of Head from case study indicates Small area of focal cerebral cortical infarction in posterior Right frontal vertex in pre-central gyrus. Patchy deep and subcortical white matter ischemic change in both cerebral hemispheres. A able to speak in one word answer with slurred speech Priority Assessmen t B chest expansion equal with SOB C radial pulses weak and irregular @ 76bpm D drowsy no complaints of pain Neuro: Confused, oriented only to person, drowsier than yesterday, PERLA, Lt arm very weak and no movement in Lt leg. RT arm and leg moderate. No pain at present. Patient is hard to understand, sounds like the patient is saying, “let me go home”. Res: Anterior/posterior chest auscultated Lt clear but decreased A/E to bases, Rt Coarse crackles Mid lobe posterior with decreased A/E to base. Productive wet cough – pt’s cough weak and not able to bring up sputum. Increased work of breathing, shown by use of abdominal muscles RR 28 O2 Sat 87% on R/A. CVS: Apex irregular rhythm, HR 76 BP 198/98, Rd +1, DP and PT via Doppler. Pitted edema +1 to bilateral ankles. Cap refill <2 seconds. Skin pale, feet and hands cool. Assessment data Assessment Data GI: LBM 1 day ago. Pt incontinent of stool. Bowel sounds present X4. Abdomen round, soft, non-tender to palpate, mucus membranes dry. Pt is on a thickened diet. GU: Foley catheter insitu draining clear amber urine. Musculoskeletal/Mobility: Left sided weakness, 2 PA with sitting at side of bed, OHL to chair Psychosocial: Lives with wife Lucy, two son’s live out of town. What are the actual and potential problems? Actual Problems Decreased O2 sat/ SOB/Increased RR R/T COPD, or possible aspiration pneumonia/chest infection Increased BP 198/98 R/T HTN Potential problems At risk for further stokes, MI R/T increased BP, Hx of stroke, hyperlipidemia At risk for bleed R/T Warfarin and Enoxaparin At risk for ICP R/T recent CVA At risk for UTI R/T Foley catheter At risk for systemic infection R/T possible lung or urinary infection At risk for delirium R/T infection, CVA, narcotic use, constipation, immobility At risk for aspiration pneumonia R/T swallowing deficit, drowsiness – not able to cough (weak) At risk for skin breakdown R/T decreased mobility, Left sided weakness At risk for nutritional deficit R/T inadequate nutritional intake At risk for constipation R/T decreased mobility and nutrition/fluid intake Based on the actual and potential problems, what lab/diag nostics do you think should be order? Ra tionale? At risk for bleed R/T Warfarin and Enoxaparin and clopidogrel What lab tests? Risk for ICP R/T CVA What diagnostics do we need? What assessments can we do? Signs and symptoms of ICP Risk for pneumonia/chest infection Which tests do we need? Risk for UTI R/T Foley catheter What diagnostic tests? What test to rule out sepsis? Risk the patient had another stroke? What test is priority? the nursing interventi ons for YOUR TOP ACTUAL PROBLEM S? Nursing interventions - Position John in a high fowlers position, apply O2 and pulse oximetry on finger to monitor --Take vitals & BG to rule out hypoglycemia/hyperglycemia - Ensure suction is set-up at the bedside - Use of suction to remove sputum/phlegm -Administer PRN Ventolin (bronchodilator) If deteriorating- have someone stay with him (if safe to leave-->bed alarm ON) -Call doctor – inform about respiratory status, decreased O2 sats, increased RR, high BP, increased WBC and Neutrophils- current drowsy LOC and confusion- receive orders for diagnostic tests/meds- Physician may want to come and see the patient Hold breakfast and move it out of way Our patient is now stable and will be transferred to neuro-rehab when a bed is available. What nursing interventions would be helpful for a patient who had a right sided CVA? How is this different from the left? Right vs Left Sided Stroke Right Hemispheric Stroke Left Hemispheric Stroke Paralysis/weakness L side=Left side neglect Left visual field deficit Spatial perceptual deficit (prob w depth perception up/down/front/back Inability to localize/recog body parts Inability to understand maps/find objects/clothing Impulsive behavior/poor judgment no concern about situations, inappropriate, depression Paralysis/weakness R side of body Behavior change, depression Right visual field deficit Aphasia (prob w speech/understanding language) -expressive/receptive/or global Increased distractibility Altered intellectual ability Deficits in math/organization/reason Deficits in reading/writing, learning new info Slow cautious behavior/hesitant Nursing priorities for patient recovering from stroke • • • • • • Impaired physical mobility Unilateral neglect Acute Pain (painful shoulder) Self-care deficits (hygiene/toileting/dres sing) Impaired sensory perception Impaired swallowing • • • • • • Impaired nutritional status Impaired urinary elimination Impaired bowel function Disturbed thought process Impaired verbal communication Impaired skin integrity Care planning continued Higher risk of injury to the weakened side- due to decrease in function and sensation -monitor bony prominences and L side limbs to get caught or squeezed in chair/bed/tight socks or anything that can cause damage to limb -refrain from IV/BP on L side Mentation: -Change in emotions, depression, impulsive, Next class ICP content