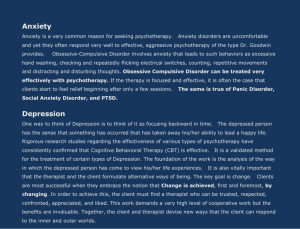
CBT for Anxiety & Depression: Evidence-Based Treatment
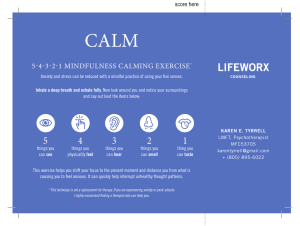
advertisement

EVIDENCE-BASED TREATMENT FOR ANXIETY DISORDERS AND DEPRESSION Written by internationally recognized experts, this comprehensive CBT clinician’s manual provides disorder-specific chapters and accessible pedagogical features. The cutting-edge research, advanced theory, and attention to special adaptations make this an appropriate reference text for qualified CBT practitioners, students in postgraduate CBT courses, and clinical psychology doctorate students. The case examples demonstrate clinical applications of specific interventions and explain how to adapt CBT protocols for a range of diverse populations. It strikes a balance between core, theoretical principles, and protocol-based interventions, simulating the experience of private supervision from a top expert in the field. Gillian Todd is a freelance CBT trainer, supervisor, and practitioner. She is a fellow of the British Association of Behavioural and Cognitive Psychotherapies (BABCP). Now retired, Gillian was affiliated with the University of Cambridge and University of East Anglia. She also coauthored two CBT self-help books and two CBT therapist manuals. Rhena Branch coauthored CBT for Dummies and is the clinical lead and director of a mental health charity (Fig Branch, reg no. 1189312). Now retired from lecturing, Rhena was affiliated with Goldsmith’s University London, Anglia Ruskin University, and University of East Anglia. Evidence-Based Treatment for Anxiety Disorders and Depression A COGNITIVE BEHAVIORAL THERAPY COMPENDIUM Edited by Gillian Todd Rhena Branch University Printing House, Cambridge CB2 8BS, United Kingdom One Liberty Plaza, 20th Floor, New York, NY 10006, USA 477 Williamstown Road, Port Melbourne, VIC 3207, Australia 314–321, 3rd Floor, Plot 3, Splendor Forum, Jasola District Centre, New Delhi – 110025, India 103 Penang Road, #05–06/07, Visioncrest Commercial, Singapore 238467 Cambridge University Press is part of the University of Cambridge. It furthers the University’s mission by disseminating knowledge in the pursuit of education, learning, and research at the highest international levels of excellence. www.cambridge.org Information on this title: www.cambridge.org/9781108420891 DOI: 10.1017/9781108355605 © Cambridge University Press 2022 This publication is in copyright. Subject to statutory exception and to the provisions of relevant collective licensing agreements, no reproduction of any part may take place without the written permission of Cambridge University Press. First published 2022 A catalogue record for this publication is available from the British Library. ISBN 978-1-108-42089-1 Hardback ISBN 978-1-108-43107-1 Paperback Cambridge University Press has no responsibility for the persistence or accuracy of URLs for external or third-party internet websites referred to in this publication and does not guarantee that any content on such websites is, or will remain, accurate or appropriate. Contents List of Figures page ix List of Tables xi List of Contributors 1 Introduction xiii . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1 Rhena Branch and Gillian Todd 2 The History and Philosophical Underpinnings of CBT: The State of the Art . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6 Jodie M. Paget PART I COGNITIVE BEHAVIORAL THERAPY FOR ANXIETY DISORDERS 3 CBT for Specific Phobias . . . . . . . . . . . . . . . . . . . . . . . . . . 29 Lina A. Gega and Barry J. D. Wright 4 CBT for Panic Disorder . . . . . . . . . . . . . . . . . . . . . . . . . . . 50 Robin D. Bailey 5 The Cognitive Behavioral Treatment of Agoraphobia . . . . . . . . . 75 Vijaya Manicavasagar and Derrick Silove 6 Cognitive Behavioral Therapy for Social Anxiety Disorder . . . . . . 93 Michaela B. Swee, M. Taylor Wilmer, and Richard G. Heimberg 7 CBT for Social Anxiety Disorder . . . . . . . . . . . . . . . . . . . . . 115 Henrik Nordhal and Adrian Wells 8 CBT for Somatic Symptom Disorder and Illness Anxiety Disorder . . 136 Lillian Reuman and Jonathan S. Abramowitz 9 Cognitive Behavioral Therapy for Generalized Anxiety Disorder: Targeting Intolerance of Uncertainty . . . . . . . . . . . . . . . . . . . 152 Cara R. Dunkley and Melisa Robichaud v vi Contents PART II COGNITIVE BEHAVIORAL THERAPY FOR POSTTRAUMATIC STRESS DISORDER 10 CBT for PTSD . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 177 Lily A. Brown and Edna B. Foa PART III COGNITIVE BEHAVIORAL THERAPY FOR OBSESSIVECOMPULSIVE DISORDER AND ASSOCIATED DISORDERS 11 Obsessive-Compulsive Disorder: An Updated Cognitive Behavioral Approach . . . . . . . . . . . . . . . . . . . . . . . . . . . . 197 Oliver Sündermann and David Veale 12 CBT for OCD: Evidence-Based Treatment for Contamination and Checking . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 222 Elizabeth A. Forrester 13 Obsessive-Compulsive Disorder: Treating Obsessions and Associated Behavioral Responses . . . . . . . . . . . . . . . . . . . . . 252 Gillian M. Alcolado 14 Other Specified and Unspecified Obsessive-Compulsive and Related Disorders . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 269 Jan van Niekerk and Kieron O’Connor 15 A Cognitive Behavioral Approach to Body Dysmorphic Disorder: Assessment, Treatment and New Developments . . . . . . . . . . . . . 295 Oliver Sündermann and David Veale 16 Comprehensive Behavioral Treatment for Trichotillomania (Hair Pulling Disorder) and Excoriation (Skin Picking) Disorder . . . 316 Charles S. Mansueto 17 Cognitive Behavioral Therapy for Hoarding Disorder . . . . . . . . . 341 Caitlin A. Stamatis, McKenzie K. Roddy, and Kiara R. Timpano PART IV COGNITIVE BEHAVIORAL THERAPY FOR DEPRESSION 18 Behavioral Activation . . . . . . . . . . . . . . . . . . . . . . . . . . . . 367 Courtney Colgan, Carl W. Lejuez, and Jessica F. Magidson 19 CBT for Persistent Depressive Disorder . . . . . . . . . . . . . . . . . 383 Anne Garland 20 Rumination-Focused Cognitive Behavioral Therapy . . . . . . . . . . 402 Edward R. Watkins 21 Cognitive Behavioral Therapy for Perinatal Depression Laura E. Sockol . . . . . . . . 418 Contents vii PART V COMPLEXITY AND COMORBIDITY IN ANXIETY DISORDERS AND DEPRESSION: CASE FORMULATION AND TREATMENT PLANNING 22 Case Formulation for Complexity and Comorbidity in Anxiety Disorders and Depression . . . . . . . . . . . . . . . . . . . . . . . . . 461 Simona Stefan and Daniel David 23 Treating Complexity and Comorbidity in Anxiety Disorders and Depression . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 475 Cory F. Newman PART VI SPECIALIST APPLICATIONS OF COGNITIVE BEHAVIORAL THERAPY FOR ANXIETY DISORDERS AND DEPRESSION 24 The Application of CBT for Adults with Learning Disabilities . . . . 507 Marc Serfaty, Matt Broadway-Horner, and Angela Hassiotis 25 Cognitive Behavioral Therapy for Children and Adults with Autism . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 533 Peter E. Langdon 26 Adapting CBT for Treating Anxiety Disorders and Depression in Adults with ADHD . . . . . . . . . . . . . . . . . . . . . . . . . . . 553 Laura D. Eddy, Laura E. Knouse, and Steven A. Safren 27 Adapting CBT for Children and Adolescents with Anxiety Disorders and Depression . . . . . . . . . . . . . . . . . . . . . . . . . 573 Taylor N. Stephens, Kimberly Blears, Erin E. Soares, Julia Rogers, and Eduardo L. Bunge 28 Adapting Cognitive Behavioral Therapy for Older Adults with Anxiety Disorders and Depression . . . . . . . . . . . . . . . . . . . . 599 Suma P. Chand and George T. Grossberg 29 Cross-Cultural CBT . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 620 Andrew Beck and Michelle Brooks-Ucheaga PART VII FUTURE DEVELOPMENTS 30 Definitions of Self-Esteem across CBT and REBT Literature . . . . . 643 Jodie Paget, Rhena Branch, and Michael Townend Appendices Index 667 681 Figures 2.1 ABC schematic diagram showing the possible interaction among As, Bs, and Cs 3.1 Three-systems model for specific phobia 3.2 Fear cycle for BII phobia 3.3 CBT cycle for BII phobia 3.4 Habituation and extinction 3.5 Overview of CBT process for specific phobias 4.1 Cognitive model of panic disorder 4.2 A cognitive model of panic with maintenance cycles added 4.3 Psychoeducation and socialization to the model 7.1 A cognitive model of social phobia 7.2 An idiosyncratic SAD case conceptualization for Jenny 9.1 Initial clinical model of GAD for CBT-IU 9.2 Expanded clinical model of GAD for CBT-IU model featuring negative beliefs about uncertainty 11.1 Eric’s case formulation, demonstrating how his contamination-related OCD developed and was maintained 12.1 Case formulation 14.1 Cognitive-behavioral formulation of obsessional jealousy 14.2 BFRB model 15.1 Case formulation 16.1 Kaitlyn’s progress in ComB treatment for two BFRBs 17.1 Etiological model of hoarding disorder 17.2 Blank copy of hoarding case conceptualization model 17.3 Ron’s case conceptualization 18.1 Behavioral model of depression 19.1 Case formulation for David 21.1 Rachel’s EPDS scores over the course of therapy 22.1 Stress-diathesis model as case formulation 22.2 The general model of integrative and multimodal CBT/IM-CBT 22.3 The ABC model for specific emotions 22.4 The behavioral ABC model 23.1 Cognitive conceptualization diagram (CCD) page 16 38 38 39 39 40 52 57 60 116 126 159 164 209 232 273 279 306 335 344 345 349 372 394 448 462 469 470 471 493 ix x List of Figures 24.1 Case study 1: Joe. Core belief focus formulation 24.2 Case study 2: Lisa. Belief focus formulation 30.1 Cognitive (bottom-up) model of self-esteem formation and maintenance 30.2 An affective (top-down) model of self-esteem formation and maintenance 523 525 647 648 Tables 3.1 Example of phobia-specific CBT assessment questions page 34 3.2 Behavioral approach task (BAT) examples 37 4.1 Examples of catastrophic misinterpretations and an alternative explanation 64 4.2 Panic thought record 65 4.3 Behavioral experiment record modeled with SPEAR 70 6.1 Commonly used self-report measures of social anxiety and related constructs 98 9.1 Examples of challenges to positive beliefs about the usefulness of worry 162 9.2 Example of behavioral experiment record form 166 10.1 Joyce’s baseline assessment scores 183 10.2 Session content 187 10.3 Joyce’s in vivo hierarchy 190 11.1 A cognitive-behavioral assessment and treatment protocol for OCD 202 11.2 Worksheet for Theory A/Theory B with example of client suffering from sexual obsessions about children 206 11.3 Assessment measures for OCD 215 12.1 Examples illustrating the range of contamination and checking concerns 223 12.2 A picture paints a thousand words 235 12.3 Theory A/Theory B 237 12.4 OCD/non-OCD way 238 12.5 OCD/non-/anti-OCD 244 14.1 Overview of reasoning errors in IBT 283 15.1 A cognitive behavioral therapy protocol for BDD 300 15.2 Worksheet for Theory A/Theory B with example of client suffering from a preoccupation with balding hair 303 15.3 Assessment measures for BDD 310 16.1 Five domains of the ComB model 324 16.2 Weekly self-monitoring form 329 16.3 Intervention ideas list 332 17.1 Example sorting: Rules for Ron 355 xi xii List of Tables 19.1 DSM-5 diagnostic criteria for persistent depressive disorder 21.1 Assessment questions addressing characteristics and concerns of perinatal patients 21.2 Measures of psychological symptoms and related outcomes for perinatal populations 21.3 Example three-column thought record 25.1 Suggested changes to the process of cognitive behavioral therapy for people with autism 27.1 Developmental framework to consider: Piaget’s theory of cognitive development 27.2 Assessment measures 28.1 Age-specific examples of maladaptive avoidance 28.2 Age-specific examples of maladaptive safety behaviors 28.3 Cognitive distortions 28.4 Modifications in CBT for late life depression 28.5 Modifications in CBT for late-life anxiety and depression 29.1 The main differences between culturally adapted and culturally responsive CBT 30.1 DSM-5 references to self-esteem across disorders 30.2 ICD-10 references to self-esteem and self-worth across disorders 30.3 Definitions of self-esteem across CBT and REBT literature 386 428 431 446 542 576 579 605 605 610 612 612 627 651 652 660 Contributors JONATHAN S. ABRAMOWITZ, Department of Psychology and Neuroscience, University of North Carolina at Chapel Hill, USA GILLIAN M. ALCOLADO, Department of Clinical Health Psychology, University of Manitoba, Canada ROBIN D. BAILEY, School of Psychology, Liverpool John Moores University, Liverpool, UK ANDREW BECK, East Lancashire Child and Family Service, UK KIMBERLY BLEARS, Children and Adolescents Psychotherapy and Technology (CAPT) Research Lab, Palo Alto University, Palo Alto, California, USA RHENA BRANCH, University of East Anglia, Norwich, UK, formerly affiliated with Goldsmiths University of London, Anglia Ruskin University and the University of East Anglia. MATT BROADWAY-HORNER, University of Chester, UK MICHELLE BROOKS-UCHEAGA, University of Derby, UK LILY A. BROWN, Perelman School of Medicine, Department of Psychiatry, University of Pennsylvania, Philadelphia, USA EDUARDO L. BUNGE, Children and Adolescents Psychotherapy and Technology (CAPT) Research Lab, Palo Alto University, Palo Alto, California, USA SUMA P. CHAND, Department of Psychiatry and Behavioral Neuroscience, Saint Louis University School of Medicine, Missouri, USA COURTNEY COLGAN, Boston College, Counseling Psychology Program, Lynch School of Education and Human Development, Massachusetts, USA DANIEL DAVID, Department of Clinical Psychology and Psychotherapy, International Institute for the Advanced Study of Psychotherapy and Applied Mental Health, Babes-Bolyia University, Romania xiii xiv List of Contributors CARA R. DUNKLEY, Department of Psychology, University of British Columbia, Vancouver, Canada LAURA D. EDDY, ADHD Clinic at UNC Greensboro, University of North Carolina Greensboro, Greensboro, USA EDNA B. FOA, Perelman School of Medicine, Department of Psychiatry, University of Pennsylvania, Philadelphia, USA ELIZABETH A. FORRESTER, chartered clinical psychologist in independent practice, Orpington, UK ANNE GARLAND, Nottingham Psychotherapy Unit, School of Health Sciences, Medical School, Queen’s Medical Centre, Nottingham, UK LINA A. GEGA, Department of Health Sciences and Hull York Medical School, University of York, UK GEORGE T. GROSSBERG, Department of Psychiatry and Behavioral Neuroscience, Saint Louis University School of Medicine, Missouri, USA ANGELA HASSIOTIS, Faculty of Brain Sciences, Division of Psychiatry, University College London, UK, and Camden Learning Disability Service, London, UK RICHARD G. HEIMBERG, Department of Psychology, Temple University, Philadelphia, USA LAURA E. KNOUSE, Department of Psychology, University of Richmond, Virginia, USA PETER E. LANGDON, Centre for Educational Development Appraisal and Research (CEDAR), University of Warwick, UK, and Coventry and Warwickshire NHS Partnership Trust, UK CARL W. LEJUEZ, Department of Psychology, University of Connecticut, USA JESSICA F. MAGIDSON, Maryland, USA Department of Psychology, University of VIJAYA MANICAVASAGAR, School of Psychiatry, University of New South Wales, Kensington, Sydney, Australia CHARLES S. MANSUETO, Behavior Therapy Center of Greater Washington, Silver Spring, Maryland, USA CORY F. NEWMAN, Perelman School of Medicine, University of Pennsylvania, Philadelphia, USA HENRIK NORDAHL, Department of Psychology, Norwegian University of Science and Technology, Trondheim, Norway List of Contributors KIERON O’CONNOR, Research Center of the Mental Health University Institute at Montreal, Canada, and Department of Psychiatry, University of Montreal, Canada JODIE M. PAGET, Department of Clinical Psychology, University of East Anglia, Norwich, UK LILLIAN REUMAN, Department of Psychology and Neuroscience, University of North Carolina at Chapel Hill, North Carolina, USA MELISA ROBICHAUD, Vancouver CBT Centre, and Department of Psychology, University of British Columbia, Vancouver, Canada McKENZIE K. RODDY, Department of Psychology, University of Miami, USA JULIA ROGERS, Children and Adolescents Psychotherapy and Technology (CAPT) Research Lab, Palo Alto University, Palo Alto, California, USA STEVEN A. SAFREN, Department of Psychology, University of Miami, USA MARC SERFATY, Department of Epidemiology and Applied Clinical Research, Division of Psychiatry, University College London, and Priory Hospital, North London, UK DERRICK SILOVE, School of Psychiatry, University of New South Wales, Kensington, Sydney, Australia ERIN E. SOARES, Children and Adolescents Psychotherapy and Technology (CAPT) Research Lab, Palo Alto University, Palo Alto, California, USA LAURA E. SOCKOL, Psychology Department, Davidson College, North Carolina, USA CAITLIN A. STAMATIS, Department of Psychology, University of Miami, USA SIMONA STEFAN, Department of Clinical Psychology and Psychotherapy, International Institute for the Advanced Study of Psychotherapy and Applied Mental Health, Babes-Bolyia University, Romania TAYLOR N. STEPHENS, Children and Adolescents Psychotherapy and Technology (CAPT) Research Lab, Palo Alto University, Palo Alto, California USA OLIVER SÜNDERMANN, Clinical and Health Psychology Centre (CHPC), Department of Psychology, National University of Singapore, Singapore MICHAELA B. SWEE, Department of Psychology, Temple University, Philadelphia, Pennsylvania, USA KIARA R. TIMPANO, Department of Psychology, University of Miami, USA xv xvi List of Contributors GILLIAN TODD, University of East Anglia, Norwich, UK, formerly affiliated with the University of Cambridge and the University of East Anglia. MICHAEL TOWNEND, Department of Health and Social Care, University of Derby, UK JAN VAN NIEKERK, Beechwood Centre, Cambridge, UK, and Cambridge Clinical Research Centre for Affective Disorders, Addenbrooke’s Hospital, Cambridge, UK DAVID VEALE, The Institute of Psychiatry, Psychology and Neurosciences, King’s College London, UK EDWARD R. WATKINS, Sir Henry Wellcome Building for Mood Disorders Research, and University of Exeter, UK ADRIAN WELLS, School of Psychological Sciences, Faculty of Biology Medicine and Health, University of Manchester, UK M. TAYLOR WILMER, Department of Psychology, Temple University, Philadelphia, USA BARRY J. D. WRIGHT, Hull York Medical School and Child Oriented Mental Health Intervention Centre (COMIC), University of York, UK 1 Introduction Rhena Branch and Gillian Todd In 2015, it was estimated that in excess of 300 million people globally suffered with depression (WHO, 2017). Roughly the same number were estimated to suffer from a range of anxiety disorders. Considering that many people experience comorbidity, simply adding these figures together to arrive at a total for common mental health disorders is not sufficient. Depression was ranked as the single largest contributor to global disability (7.5% of all years lived with a disability in 2015) with anxiety disorders ranked sixth largest contributor (3.4% of all years lived with a disability in 2015). Cognitive behavioral therapy (CBT) is a therapeutic tradition that also refers to a range of interventions sharing the basic premise that psychological and emotional distress are maintained by cognitive factors. Early pioneers Albert Ellis (Ellis, 1962) and Aaron Beck (Beck, 1970) posited that maladaptive cognitions including core beliefs (also referred to as ‘schemas’) about self, others, and the world/future, when triggered by particular conditions or situations, give rise to related negative automatic thoughts, associated negative emotions, and behaviors. In essence, CBT holds that interventions and strategies aimed at changing maladaptive cognitions ultimately lead to therapeutic change in both emotional distress and dysfunctional behavior. Since the emergence of CBT, much research has been carried out demonstrating its efficacy with specific anxiety disorders and depression. A plethora of metaanalytic studies, considered to be the gold standard of research methodology, have examined the effectiveness of CBT for anxiety disorders and depression, quantified in terms of the effect size, that is, a quantitative measure of statistical significance of an observed specific treatment effect when compared with other treatments or with a control condition. The larger the effect size, the greater the difference is between two groups. Watts et al. (2015) conducted a meta-analysis of randomized controlled trials (RCTs) that compared CBT with treatment as usual (TAU) in the treatment of anxiety disorders and depression. The meta-analysis demonstrated a media effect size favouring CBT over TAU. Cuijpers et al. (2013) in their meta-analysis support the efficacy of CBT for depression. The generalizability of delivering evidence-based treatment protocols derived from RCTs into healthcare settings is often questioned by clinicians in the setting 1 2 Rhena Branch and Gillian Todd itself. Researchers are often regarded as cherry picking participants for their studies, recruiting a stable of talented therapists who are rigorously trained and closely supervised; however, the evidence suggests otherwise. Otte (2011) conducted a meta-analysis of meta-analyses of CBT for anxiety disorders and concluded that both placebo-controlled trails and trials within a naturalistic setting supported the efficacy and effectiveness of CBT as a treatment intervention for anxiety disorders. Stewart and Chambless’s (2009) meta-analysis of effectiveness studies in real-world circumstances found CBT to be effective. In recent years, numerous disorder-specific protocols have been developed to address specific cognitive and behavioral elements which are key components of a disorder’s maintenance. As such, disorder-specific protocols demonstrate some considerable differences in treatment techniques from those typically found in ‘standard’ CBT. Despite these differences in assessment and treatment focus, as well as the use of distinctive interventions, the core theory and general approach to treatment remains consistent. The roll-out of the UK government initiative Improving Access to Psychological Therapies (IAPT) in 2008, based on the premise that CBT can be delivered effectively and economically (Layard and Clark, 2014), has increased the number of trainees learning from a protocol-based curriculum. However, initiatives to roll out CBT training to the masses, thereby affordably and speedily developing an army of therapists to provide evidence-based therapy, may have observable limitations. Brief, rapid-fire, protocol-based training means that most trainees will learn a maximum of two protocols per common disorder. The majority of these brief courses include little or no training on core theoretical and philosophical CBT principles. Moreover, lack of emphasis on basic transdiagnostic skill acquisition, coupled with a paucity of time to focus on developing and demonstrating overarching clinical competency, leaves newly trained clinicians dependent on dogged obedience to protocols. CBT theoretically consistent ‘eclecticism’, or deviation from protocol, is clinically justifiable and is expected among seasoned clinicians with adequate training. CBT clinicians taught only the bare minimum of protocols on an intensive course may, therefore, be likely to drift away from CBT altogether when a single protocol proves insufficient. It has been observed that therapists easily slip into being eclectic in their therapeutic stance, offering a pick and mix approach to therapy, which has no empirical or theoretical basis. Not all patients who think they are having CBT actually receive the evidence-based version they rightfully expect. Waller has extensively examined the issue of therapist drift (Waller, 2009). For a detailed analysis of factors leading to therapist drift, see Waller and Turner (2016). In addition to disorder-specific protocols (i.e., obsessive-compulsive disorder [OCD], generalized anxiety disorder, panic disorder), CBT increasingly comprises a number of specific approaches for identified populations (i.e., older adults, people with intellectual disabilities) and ‘third wave’ approaches (i.e., mindfulness-based CBT, acceptance, and commitment therapy). Introduction The aim of this compendium is to provide a framework so clinicians can follow evidence-based CBT protocols for treating their patients with anxiety disorders and depression that have proven efficacy. Experts in their field from around the world have shared their protocols and wisdom to enable the reader to (1) develop a knowledge base of current research, (2) understand the phenomenology of psychological disorders, (3) learn idiosyncratic additions to the assessment process, (4) follow a step-by-step guide to treatment, (5) identify and overcome common problems in treatment, and (6) effectively evaluate treatment progress. While anxiety, depression, and other common mental health disorders are the main focus of this compendium, some disorders such as OCD have more than one chapter devoted to them, with more than one model or protocol represented. More complex and nuanced disorders like OCD, as well as more newly understood disorders such as body dysmorphic disorder (BDD), require variation in focus with respect to assessment and treatment. Knowledge of more than one protocol and recent research findings will prove invaluable to the clinician. Specialist approaches of CBT focus on the treatment of anxiety disorders and depression in distinct populations. Based on clinical presentation and need, adaptations to protocols need to be made and implemented flexibly. Leading authorities in their field have contributed chapters on adapting CBT for common mental health problems in diverse communities. Chapters on specialist applications of CBT for older adults and for youth are included. CBT for mental health problems in patients with neuro-cognitive-biological disorders, including autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD), and identity disorder (ID), is covered. And a chapter is included on cultural adaptations of CBT where the authors consider the need for an understanding of ethnicity and cultural variations. The clinician will be enlightened in their understanding of the nuances observed in clinical presentations and will gain knowledge in how to work effectively with complex and highly comorbid clinical presentations. A strength of this compendium is its international focus: chapters have been contributed from around the world, including the United Kingdom, United States, Canada, Australia, Singapore, Norway, and Romania. All chapters are consistent with the American Psychiatric Association’s Diagnostic and statistical manual of mental disorders (5th ed.) (DSM-5). This compendium assumes a degree of reader knowledge and therefore suits an intended audience of qualified clinicians. However, it is also likely to be useful for post-graduate trainees and students. Book Overview This compendium is divided into six parts. The state of CBT today is explored and its historical and philosophical underpinnings are reviewed in Chapter 2, which examines how CBT has developed, transformed, and, to an extent, migrated from its early roots (Beck 1976; Ellis, 1962). 3 4 Rhena Branch and Gillian Todd Part I, includes seven chapters focusing on DSM-5 anxiety disorders, offering specific models as well as providing transdiagnostic interventions. There are two protocols offered for the treatment of social anxiety. Part II is comprised of a chapter on the treatment of posttraumatic stress disorder (PTSD) by pioneer in the field Edna Foa and specialist Lily Brown. Part III includes seven chapters dealing with OCD and related disorders, including BDD, trichotillomania, hoarding, and excoriation disorder. Part IV features four comprehensive chapters on CBT for depressive disorders, including behavioral activation (BA) for moderate to severe depression, targeting depressive rumination, and chapters dealing with the treatment of persistent depression and depression within the perinatal population. Part V hosts two chapters, the first dealing with case formulation of complex and comorbid cases and the second discussing the treatment of complexity and comorbidity. Part VI consists of six chapters dealing with specialist CBT applications to distinct patient populations. We hope readers will agree that the result of the editors’ collaboration with internationally recognized expert clinicians, trainers, academics, and researchers is a comprehensive compendium that is highly relevant to all cognitive behavioral practitioners. We would like to thank all our esteemed contributors for their hard work and cooperation. REFERENCES American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association. Beck, A. T. (1970). Cognitive therapy: Nature and relation to behavior therapy. Behavior Therapy, 1, 184–200. (1976). Cognitive therapy and the emotional disorders. Penguin Group. Cuijpers, P., Berking, M., Andersson, G., Quigley, L., Kleiboer, A., & Dobson, K. (2013). A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Canadian Journal of Psychiatry, 58(7), 376–385. Ellis, A. (1962). Reason and emotion in psychotherapy. Stuart. (1994). Reason and emotion in psychotherapy: A comprehensive method of treating human disturbances. Citadel. Layard, R., & Clark, D. M. (2014). Thrive: The power of evidence-based psychological therapies. Allen Lane. Otte, C. (2011). Cognitive behavioral therapy in anxiety disorders: Current state of the evidence. Dialogues in Clinical Neuroscience 13(4), 413–421. Stewart, R. E., & Chambless, D. L. (2009). Cognitive-behavioral therapy for adult anxiety disorders in clinical practice: A meta-analysis of effectiveness studies. Journal of Consulting and Clinical Psychology, 77(4), 595–606. Waller, G. (2009). Evidence-based treatment and therapist drift. Behaviour Research and Therapy, 47(2), 119–127. Introduction Waller, G., & Turner, H. (2016). Therapist drive redux: Why well-meaning clinicians fail to deliver evidence-based therapy, and how to get back on track. Behaviour Research and Therapy, 77, 129–137. Watts, S. E., Turnell, A., Kladnitskj, N., Newby, J. M., & Andrews, G. (2015). Treatment-asusual (TAU) is anything but usual: A meta-analysis of CBT versus TAU for anxiety and depression. Journal of Affective Disorders, 175, 1152–1167. World Health Organization. Depression and other common mental disorders: Global health estimates. (2017). World Health Organization. License: CC BY-NC-SA 3.0 IGO. 5 2 The History and Philosophical Underpinnings of CBT: The State of the Art Jodie M. Paget You don’t need to go out and buy pop psychology self-help books. When you read the classics in the humanities, you become aware that the big ideas have been around for a long time, despite the fact they are often served up today in modern psychological explanations of human action as novel and scientific. —James Stockdale (1995, p. 24) Cognitive therapies are often attributed to Albert Ellis and Aaron Beck, who created rational emotive behavior therapy (REBT) and cognitive therapy (CT), respectively. This chapter discusses the historical development, philosophical underpinnings, and current state of CBT. ‘Third wave’ approaches, and what these have in common with ‘second wave’ theoretical concepts and protocol-driven CBT, are discussed alongside possible implications for quality of CBT training (i.e., Improving Access to Psychological Therapies [IAPT] training courses in the United Kingdom). Commonalities between REBT and ‘new developments’ are highlighted, asking the question of how it is that third wave CBT such as ACT (Hayes et al., 2012), and dialectical behavior therapy (DBT) (Linehan, 1993), for example, give little credence to Ellis, when those practicing REBT, or who have an understanding of it, are keenly aware of the commonalities (Malkinson, 2011). Furthermore, are concepts such as ‘self-compassion’ (Neff, 2003), ‘clinical perfectionism’ (Egan et al., 2014), and ‘intolerance of uncertainty’ (Dugas and Robichaud, 2007) a reinvention of core aspects of REBT? The idea that some of these new developments were posited by early theorists will be explored. First Wave Behavioral Therapies Classical CBT (REBT and CT) are commonly referred to as ‘second wave’ cognitive behavior therapies. It is important to note that during the 1950s and 1960s ‘first wave’ behavior therapies were also developing and great efforts were made to have them empirically validated. Briefly stated, behavior therapy can trace its genesis to the work of Pavlov (1955), whose research in classical conditioning theory paved the way 6 The History and Philosophical Underpinnings of CBT for the study of abnormal behavior, in particular, research pertaining to fear acquisition and de-conditioning (Wolpe, 1958). The Institute of Psychiatry and the Maudsley Hospital in London were home to several pioneering psychologists (such as Cyril Franks, Hans Eysenck, and Stanley Rachman), who each made significant contributions to behavioral research during World War II and afterwards. In 1956, H. S. Jones, a clinical psychologist at the Maudsley, wrote, ‘The Application of Conditioning of Learning Techniques to the Treatment of a Psychiatric Patient’, considered the first published article on behavior therapy. In 1965, Eysenck and Rachman wrote the first behavioral therapy textbook, considered one of the single most significant developments within the field at that time (Marks, 2012). In 1966 whilst at Middlesex Hospital in London, Dr Victor Meyer applied some of the techniques he had acquired (and achieved success with) during his time at the Maudsley, towards treatment of OCD. At that time there was little to offer sufferers of OCD, but through the application of exposure and response prevention (ERP) significant improvements were made. Over the next decade the treatment was refined and made available to outpatients to good effect (see Rachman et al., 1979). Rachman (2015) provides a detailed history of behavior therapy. He states that in the 1970s attention to cognitive factors occurred in part due to Bandura’s (1969, 1977) research into social-cognitive factors, and success was seen in the treatment of social anxiety and generalized anxiety. Due to the success of these approaches, behavior therapists became open to incorporating cognitive concepts, and began using cognitive techniques alongside behavioral components, in part due to a need to develop an effective therapy for depression. Rachman adds that the inclusion of behavioral experiments within Beckian CT was reassuring to behavioral therapists and, in part, paved the way for a cognitive behavioral form of therapy. The combining of these two approaches was further solidified by Clark’s (1986) cognitive therapy for panic disorder and Barlow’s (1988) panic control therapy. Second Wave Cognitive Behavioral Therapies REBT In the 1950s Ellis created what is now known as rational emotive behavior therapy (REBT) and described it as a cognitive-experiential-behavioral system of therapy that has strong philosophical underpinnings and an active focus on disputing dysfunctional self-defeating beliefs (Ellis, 2001). REBT was the first form of cognitive behavioral therapy and Ellis’s ABC(DE) model is not only the foundation of REBT, but also a core theoretical construct of all subsequent versions of CBT (David et al., 2005). It is well documented that the creation of REBT was born primarily out of Ellis’s scepticism of the efficiency of psychoanalysis, the therapeutic orientation Ellis had originally trained in (Ellis, 1962): I went back to my hobby since the age of 16 . . . the philosophy of the ancients, largely of Epictetus, Marcus Aurelius, and in the east of Confucius and Lao Tsu and Buddha, and 7 8 Jodie M. Paget amalgamated it with behavior therapy, which I had used on myself at the age of nineteen to get myself over my phobia of public speaking and of approaching young females. (Interview with Ellis in Ellis, 2010) Ellis overcame his fear of rejection from potential dating partners via philosophically informed interventions. He exposed himself to feared situations, deliberately challenging his pre-existent belief systems and deliberately adopting more functional ways of thinking and behaving. Ellis gave his first presentation of REBT, then known as rational therapy, in the late 1950s, and shortly after changed the name of the approach (due to an accusation of rationalism) to rational emotive therapy (Yankura and Dryden, 1994). Rationalism deems thought superior to other senses when determining the validity of knowledge, and that distinct boundaries exist between mental and physical processes (see DiGiuseppe and Linscott, 1993, for a detailed review). Whilst it is not surprising for such a misunderstanding to occur, perhaps partly due to common misunderstandings of the underpinning philosophy of Stoicism, Ellis (1958) states that human emotion and creativity are not controlled (nor should they be) by reason and intellect alone. It is evident here that although REBT does stress that if one is to achieve significant reduction in emotional distress, one must alter the associated belief system. This does not mean, however, that psychological intervention is limited to or should only focus on work at a cognitive level. Throughout the 1950s, 1960s, and 1970s REBT grew in popularity, and in 1959 the Albert Ellis Institute was established in New York. In 1993 the second (and most current) rebranding of rational emotive behavior therapy was undertaken. This was done in part due to Ellis insisting the ‘between session tasks’ and behavioral work undertaken in therapy be acknowledged (Yankura & Dryden, 1994). In 1994, the second edition of Reason and Emotion in Psychotherapy was published, containing an updated and revised version of Ellis’s conceptual model of human disturbance, known as the ABC(DE) model (see Figure 2.1). This model is still widely used within CBT, in both its original and updated forms (Dryden, 2013a; Dryden & Branch, 2008). Simplified versions that may neglect or incorrectly present core philosophical and theoretical constructs also exist currently (e.g., Skinner & Wrycraft, 2014). Yankura and Dryden (1994) state that during the 1980s, REBT had developed an international presence and treatment manuals were developed for couples therapy (Ellis et al., 1989), individual counselling (Dryden, 1987), and family therapy (Huber & Baruth, 1989). A study conducted by Smith (1982) found that Ellis was placed between Carl Rogers and Sigmund Freud as the second most influential psychologist (Aaron Beck was seventh) by a vote of over 400 American psychologists. Despite the undeniable contributions Ellis made to psychology and psychotherapy, many CBT therapists are unaware of the origins of CBT, or credit it primarily to Aaron Beck. So, what happened? Why is REBT regarded as ‘the disturbed child in the family’ (Malkinson, 2011, p. 259)? REBT Current Status. When Ellis developed his theory of personality (Ellis, 1978b) and put forward a conceptual model that accounted for psychological The History and Philosophical Underpinnings of CBT disturbance, it offered an explanation for emotional distress as opposed to advancing specific disorders. This could be considered one of the failings of REBT, in that unlike CT it has done little to advance understanding of specific psychiatric disorders. This was highlighted by David (2014), who states REBT research tends not to be related to specific psychiatric conditions and that there is a lack of rigorous research that is necessary for a therapeutic approach to be considered evidencebased. REBT interventions are primarily aimed at challenging evaluative beliefs, rather than inferences (i.e., negative automatic thoughts [NATs]), and its interventions are transdiagnostic. Knowing why a psychological intervention works is just as important as the theory that attempts to explain the phenomena; therefore, welldesigned research aimed at examining the efficacy of REBT is well overdue (David and Montgomery, 2011). A criticism of REBT put forward by Padesky and Beck (2003) is that it is it philosophically based whilst CT is empirically based. Ellis (2005a) argues, however, that both therapies are philosophically and empirically based, but REBT is more philosophical and CT currently has more empirical support. When Isaac Newton felt the apple hit his head, this was empirical evidence that apples fall from trees. Seeing an apple fall does not explain why it fell, but it does provide validation for the theory of the law of universal gravitation. Both Ellis (2005a) and Padesky and Beck (2005) welcome the recommendation that REBT become more empirically validated, yet there is still a significant lack of well-designed studies to examine its empirical status. Qualitative studies have shown that REBT is effective for both clinical and non-clinical populations, that the efficacy of individual and group therapy is broadly similar, that a higher number of sessions produces greater results, and that the more well trained the therapist, the better the results (Dryden, 2012a). A meta-analysis by David et al. (2005) concluded REBT interventions are efficacious for a wide range of conditions, regardless of how interventions were delivered and the clinical status or mean age of the sample. When analyzing presumed mechanisms of change, REBT is deemed to be efficacious. However, due to the diversity of outcomes and reporting and the quality of measures utilized, more research is needed that includes transdiagnostic and diagnostic categories. Philosophy of CBT Stoicism The philosophical underpinnings of cognitive behavioral therapies can trace their origins to ancient Greek and Roman Stoic philosophers, such as Marcus Aurelius and Epictetus, as well as Asian philosophers such as Buddha, Confucius, and Lao Tsu. Both Ellis and Beck cite Stoicism as a primary philosophical foundation in the development of their approaches, yet this fact is seldom acknowledged by many therapists (Robertson, 2018). Stoicism is a school of thought founded by Zeno of Citium (330 BCE) that existed as a philosophical movement for around 500 years. Its main assertions are not limited to what we can know, or what is right and wrong, 9 10 Jodie M. Paget but concerns itself more with how one should live. Whilst not unique in this idea – the same can be said for Epicureanism – Stoic philosophy insists happiness can be achieved through virtue alone (Sellars, 2010). Stoicism is commonly, and erroneously, considered to be synonymous with repression of emotion. Stoic philosophy does not advocate suppression of affect, but rather endeavours to determine what are natural human feelings and what affective responses one would have if one were free from false belief. The aim, therefore, is to avoid feeling what is false, as opposed to eradicating negative affect (Graver, 2007). Epicureanism The Stoic concept of faulty judgement and its link to affective distress clearly mirrors the core theory of REBT: rigid absolutism as a primary cause of human distress. However, this is not the only Hellenistic school of philosophy that Ellis deemed informative when it came how one should live. Ellis advocated responsible hedonism, and suggested limiting short-term indulgences, a key theme in Epicurean philosophy (Ellis et al., 2009). Epicurus argued that the primary motivators that underpin almost every action are the pursuit of pleasure and avoidance of pain, and that providing our beliefs are under control, hedonism need not be a threat to our freedom (Warren, 2009). Ellis frequently highlights the philosophic emphasis REBT has over CT. He proposes humans are natural born philosophers with an innate biological tendency to be irrational; humans create meaning, have the ability to predict the future via rational means, and are natural scientists (Yankura & Dryden, 1994). It is the role of the REBT therapist, therefore, to facilitate profound philosophical change within the client that will ease both current and future emotional distress (Ellis, 1980). In addition to the ancient philosophies mentioned, REBT also has current influences, such as Karl Popper and Bertrand Russell, and aligns itself well with Christian values, ethical humanism, and a humanistic-existential view of life (Dryden, 2012a). History of Cognitive Therapy Similarly to Ellis, Aaron Beck also practiced as a psychoanalyst and had endeavoured to put to empirical testing theories such as depression being the result of unreleased aggression. He found that dream studies and many other psychoanalytic concepts did not stand up to empirical testing, yet did fit with cognitive explanations (Beck, 1991). In 1967 Beck wrote the pioneering and comprehensive text Depression: Clinical, Experimental and Theoretical Aspects, a first look at cognitive therapy for depression (Beck, 1967). This text outlined the cognitive model of depression and its proposed treatment recommendations. The model proposes three concepts that explain the proposed psychological mechanisms of depression, these being the cognitive triad, schemas, and cognitive errors. The cognitive triad is comprised of three cognitive patterns that create an idiosyncratic experience for the person, these being negative views of self, experiences (world), and the future. The The History and Philosophical Underpinnings of CBT lack of motivation common in people with depression is viewed as a consequence of cognitions that result from these mechanisms. Suicidal ideation is viewed as an escape strategy, dependency a consequence of views of self as helpless/ ineffective, and psychomotor inhibition a result of assuming all is futile (Beck, 1970; Beck et al., 1979). Schemas are described as enduring attitudes that influence the content of cognitions. They screen, code, and evaluate stimuli that impinge on the person, enabling them to interpret experiences in a meaningful way. Schemas can be inactive, meaning they are asymptomatic at times, but can be activated and energized by external factors. When schemas are activated in depression, thoughts are quickly saturated with depressed content, and are more easily evoked by external triggers (Beck, 1970). Cognitive distortions, the third concept, are the frequently articulated thoughts of the depressed individual. These thoughts deviate from logical thinking and can be classified as paralogical (arbitrary inference, selective abstraction, and overgeneralization), stylistic (exaggeration), or semantic (inexact labelling) (Beck, 1970). Modification of schemas should therefore lead to changes in how one interprets and organizes experiences and how one goes about setting and achieving goals (Beck et al., 1979). In 1991 Beck published a subsequent edition of Cognitive Therapy and the Emotional Disorders where he cites Ellis’s contributions as a major development in the field of cognitive therapy and goes on to state that upon discovering the similarities in techniques and formulations between both approaches, he gained confidence he was traveling in the right trajectory (Beck, 1991). Beck’s relentless pursuit of researching depression and anxiety disorders has culminated in a variety of validated measurement tools (e.g., Beck Depression Inventory [BDI-II, Beck et al., 1996], Beck Hopelessness Scale [BHS, Beck and Steer, 1993a], Beck Anxiety Inventory [BAI, Beck and Steer, 1993b]) used as gold standards for research, and a sound body of research demonstrating the efficacy of CBT for common mental health problems. In 1994, Beck and his daughter Judith Beck set up the Beck Institute for Cognitive Therapy in Philadelphia, which provides training and supervision in CBT. Subsequently, CBT, under its broad heading, has been found to be efficacious for a wide range of disorders, and research into the proposed change mechanisms responsible for symptom reduction within disorders is vast (see Hofmann et al., 2012, for a detailed meta-analysis of CBT efficacy). Third Wave Cognitive Behavioral Therapy Having provided a brief overview of first wave behavioral approaches of the treatment of psychological problems and the influence and contribution these had on the development of second wave approaches (specifically REBT and CT), this section outlines the basic principles of acceptance and commitment therapy (ACT; Hayes et al., 2012), arguably the only form of third wave CBT. The concept of selfcompassion (Neff, 2003) is also discussed (but as to whether these legitimately fall 11 12 Jodie M. Paget into second wave or third wave therapies is beyond the scope of this chapter). Briefly put, Hayes et al. (2006) state that metacognitive therapy (MCT; Wells, 2009), dialectical behavior therapy (DBT; Linehan, 1993), and mindfulness-based cognitive therapy (MBCT; Segal et al., 2001) can be considered third wave approaches; however, David and Hofmann (2013) claim the respective authors do not share this view). Discussion of ACT (Hayes et al., 2012) and self-compassion (Neff, 2003) are included not to provide a detailed account of their developments or current standing within the field, but rather to discuss similarities in core principles that have been overlooked, often due to comparisons occurring between CT and various third wave approaches. Acceptance and Commitment Therapy (ACT) Hayes and Hofmann (2017) claim third wave CBT began approximately in 2004 and was primarily defined by a set of contextual concepts that paid attention to how a person relates to thoughts and emotions, as opposed to the actual content of thoughts. They propose that ACT, DBT, and MCT can be defined as third wave versions of CBT and add that these approaches emphasize emotions, metacognition, and acceptance. In 2012, Hayes et al. outlined the main principles of ACT, a psychotherapeutic approach based on radical behaviorist principles, in particular, relational frame theory (RFT) (see Hayes, 2004, for a detailed account). Despite its close link to first wave approaches, it is referred to as a third wave modality due to that fact that interventions target the way people relate to thinking and feeling, rather than direct challenging of specific cognition or experience (Morris & Oliver, 2012). ACT is based on functional contextualism, a pragmatic philosophy of science that aims to predict and influence behavior. Biglan and Hayes (1996) argue behavioral problems may be prevented or ameliorated if behavioral scientists focus on developing empirically based concepts that enable behavioral phenomena to be predicted and influenced. A central aim within ACT is to increase psychological flexibility, defined as enhancing the ability to make contact with the present moment, based on what is possible in that moment, and to behave in ways that are in accordance with one’s chosen values. In order to achieve this end, ACT incorporates mindfulness, acceptance, and cognitive defusion skills (Hayes et al., 2012). A key difference often acknowledged between ACT and CBT is ACT’s rejection of cognitive restructuring (CR) as an intervention, due to the assumption it encourages suppression. This is discussed in detail by Arke and Craske (2008), who state that the labelling of some thoughts as ‘faulty’ may increase a desire to suppress such content, and that thought challenging may lead to reduced sense of control; however, they do conversely state the distress-reducing effects of CR and highlight a great number of similarities between ACT and CBT (specifically, CT). A common oversimplification of CR is the identification and labelling of thoughts as ‘faulty’ and this is often equated to using empirical-based disputing techniques as a primary intervention. Testing whether a thought (most likely a negative automatic thought The History and Philosophical Underpinnings of CBT [NAT]) stands up to empirical challenging is ubiquitous throughout CBT textbooks (e.g., Greenberger et al., 2015) and to many disorder specific protocols to the neglect of more advanced disputing methods (see DiGiuseppe, 1991; Ellis, 1993; Neenan and Dryden, 1999). Arguably, skilled CR necessitates going beyond empirical-based arguments to challenge cognition (whether via verbal discussion or thought records); however, sophisticated CR methods are too seldom represented within protocol-driven CBT. Defusion Defusion is a core component of ACT which aims to reduce the believability and/or attachment to thoughts without direct challenging of thought content. Defusion is intended to counteract cognitive fusion, defined by Hayes et al. (2012) as the inability to distinguish between awareness and the cognitive narrative of one’s mind, due to the inextricable binding of thoughts and meaning. David and Hofmann (2013) claim a fundamental weakness of ACT is the idea that it is possible to have cognition (thought) without simultaneously passing some kind of judgement (evaluation). Furthermore, they argue this assumption can be counter-argued by the Spinoza model of mental representation, which lends credence to this criticism (see Appendix 2.1). This model argues that in order for one to understand, one simultaneously and automatically attributes a value of true (or false) to a specific thought. In other words, the idea that it is possible to change dysfunctional cognition via ACT interventions (acceptance, cognitive defusion, and mindfulness) into ‘neutral’ thoughts is potentially flawed. The view that people automatically, unconsciously, and quickly evaluate cognition and assign a value of true or false to it is anecdotally endorsed by many REBT and CBT clinicians. David and Hofmann (2013) propose that taking a look at the differences between CT and REBT may help in clarifying the issue of whether one can have cognition and decide what to do with it without simultaneously evaluating it. Briefly stated, Abelson and Rosenberg (1958) define cold cognition as that which reflects the process of representation, knowing, and description, whereas hot cognitions are indicative of the process of an evaluation or appraisal. CT views cold cognitions as a proximate cause of distress, whereas REBT views them as distal causes and views hot cognitions as proximate to distress (Hyland & Boduszek, 2012). Hence, a fundamental research difference between these two approaches is CT’s focus on cognitive distortions (e.g., selective abstraction, arbitrary influence, absolutistic thinking; see A. Beck, 1970; J. Beck, 2011) and REBT’s focus on evaluations and appraisals in the form of irrational beliefs (i.e., rigid demands and their derivatives; awfulizing, low frustration tolerance, and self/other/world depreciation; Dryden & Branch, 2008). REBT is consistent with Lazarus’s (1991) appraisal theory of emotions, which proposes that despite representational cognitions contributing to appraisal, it is the process of appraisal itself that gives rise to emotions (Hyland & Boduszek, 2012). Therefore, ‘neutralizing’ (defusing) of cognition can occur, but probably does so due 13 14 Jodie M. Paget to changing an underlying evaluation (an irrational belief/evaluative assumption), meaning ‘defusing’ may occur in part due to a form of CR (David & Hofmann, 2013). Acceptance In addition to developing defusion skills, ACT promotes developing acceptance, defined by Hayes et al. (2012) as an ongoing process – an alternative to avoidance and a function, rather than a technique. For a discussion of similarities between CBT (Beckian CT, in particular) and ACT, see Arch and Craske (2008), who claim CBT may contain elements of acceptance. However, if CBT also included REBT in such comparisons, it would be hard to ignore that acceptance is a core principle, explicitly defined and deeply rooted in REBT’s underpinning philosophy. It is postulated that lack of acknowledgement of CBT’s advocacy of acceptance is in part due to (1) current literature defining CBT solely as Beckian CT and omitting REBT and (2) a faulty assumption that REBT and CT hold a shared view on acceptance and self-esteem. Indeed, Beck’s pursuit to empirically validate CT for depression occurred whilst Ellis was forcefully promoting attitudes of self, other, and world acceptance (Ellis, 2005b, 2007). Ellis (2005b) (and subsequent REBT theorists such as Windy Dryden, Ray DiGiuseppe, Janet Wolfe, and Paul Hauck, to name a few) consistently promotes the adoption of acceptance-based beliefs, and of behaving in accordance with new healthy attitudes (rational beliefs). Though perhaps not as explicit as ACT’s focus on value-directed action, rational beliefs that are fair, compassionate, and pragmatic tend to be highly concordant with an individual’s values, thereby promoting valuedriven behavior. Thus, although Ellis and other early theorists have not put specific emphasis on values per se, it seems reasonable to assume that one’s values are considered both important and intrinsic to meaningful therapy. A final note regarding philosophical similarities between ACT and components of REBT is that both make reference to sharing aspects of Buddhist philosophy. Hayes (2002) highlights that ACT shares several key notions with Buddhism that are relevant to human distress, namely, attachment and its role in suffering, and mindfulness. Ellis indicates that irrational and therefore unaccepting (self/others’/ world) beliefs greatly contribute to distress, and that in order to be less distressed, one better become less attached to such ideas. He advocates adopting flexible accepting preferences that reflect strongly held ideals but allow for philosophical acceptance when life falls short of one’s ideals. In summary, the ACT intervention of cognitive defusion seems unlikely to occur without some kind of change in the associated belief system that is, in part, causative of such cognitive content. Whilst it may be true that CT does not explicitly advocate acceptance, this has been a core principle of REBT since its inception. Therefore, accuracy would be promoted if comparative analyses more clearly stated to which school of CBT they referred. Whilst ACT provides a valued contribution in the continued development of CBT, it may be worthwhile taking stock of how similar some of the key change methods The History and Philosophical Underpinnings of CBT are to REBT, giving due acknowledgement and continuing research into these mechanisms of change. Self-Compassion Neff (2003) claims the concept of self-compassion arose due to problems with the concept of self-esteem, an ill-defined psychological phenomenon, yet a concept widely endorsed within CBT literature (see Beck, 2011; Fennell & Jenkins, 2010; Wilding & Palmer, 2010). Self-compassion differs from self-esteem in that is does not advocate rating the ‘self’ as good or bad (Neff, 2009). Self-compassion is comprised of (1) self-kindness, as opposed to harsh self-criticism, (2) common humanity and one’s connectedness to others, and (3) mindfulness (Neff and Lamb, 2009). Ellis rejects the concept of self-esteem and instead advocates unconditional self-acceptance (USA), endorsing principles of self-compassion (Ellis, 2005b). Encouraging clients to develop unconditional self-acceptance (USA) and unconditional other-acceptance (UOA) is a key aspect of REBT. Essentially, this means viewing others as fallible, complex, and in a state of flux. When USA and UOA are implemented via consistent and deliberate practice, this increases one’s interconnectedness (Dryden, 2013b). Therefore, self-kindness has much in common with USA, and the connectedness to others can be seen within UOA. Mindfulness, however, is as not seen as a necessary component in USA, but rather a likely by-product that is a consequence of USA (Ellis, 2005b). For a detailed discussion on the differences between self-compassion and USA and how these concepts can be integrated, see Dryden (2013b), who provides a model for how USA and self-compassion can be utilized concomitantly towards the reduction of psychological distress. When looking for alternative or innovative ways of working with low selfesteem or distressing emotions such as guilt and shame, CBT therapists who are trained primarily in protocol-driven CBT might understandably search for new developments within second or third wave CBT literature. However, a wealth of literature addressing interventions for emotional problems exists within REBT (e.g., anger, Dryden, 1993; guilt, Dryden 1994; shame, Dryden, 1997; jealously, Dryden, 2005; hurt, Dryden, 2007). Self-compassion and REBT have long been bedfellows and are happy in their relationship. The (D)Evolution of the ABC Model When attempting to put forward a conceptual model derived from theory, complex ideas are often simplified and presented as partial versions of the greater phenomenon. Although models are useful guides, a map of the territory should not be confused with the territory itself (Korzybski, 1958). In 1962 Ellis put forward a conceptual model of human disturbance, which was later updated and illustrated diagrammatically in the second edition of Reason and Emotion (Ellis, 1994). For a detailed account of earlier models that existed, influenced, and shaped this model, see Korzybski (1958). This model was simple, yet profound: ‘A’ represents Activating 15 16 Jodie M. Paget stimulus energy transmitted by external happening sensory system response A activity in sensory area of the brain (sensation experienced) activity in sensory association area (sensation interpreted) B cortical area (experience tied in with belief systems and evaluated) C -emotional and behavioral reactions Figure 2.1. ABC schematic diagram (as cited in Ellis, 1994, p. 84) showing the possible interaction among As, Bs, and Cs. The forward progression of the event extends from the top to the bottom of the diagram, and the interactional feedback is indicated by the arrows. Events, ‘B’ beliefs systems, and ‘C’ emotional and behavioral consequences (see Figure 2.1). What is significant about this model is the acknowledgement of its interactional nature and the proposition that Bs are inherently emotionally laden (for a full discussion, see Ellis, 1994, p. 87). REBT ‘Bs’ differ greatly from Meichenbaum’s ‘self-statements’ and Beck’s ‘automatic thoughts’. Beliefs at B are comprised of evaluations and musts (often omitted in the formulations of Meichenbaum and Beck). Overt evaluations of good or bad, desirable or undesirable, are clearly stated at ‘B’, as such overt evaluation renders them emotionally laden. This point is stressed by Dryden (2012b), who states that in order to correctly present theory, REBT theorists make a conscious effort to avoid stating ‘B’ causes ‘C’, and will instead use terms such as ‘B’ largely determines ‘C’, or ‘B’ is at the core of ‘C’. Yet this significant point is too frequently omitted in examples across CBT literature, resulting at times in reproduction of diluted constructs. Moreover, cognitive consequences are not indicated at ‘C’. Whilst this is true of Ellis’s original model, the Dryden framework acknowledges that cognition occurs at each part of the ABC, and specifically that cognitive consequences (of ‘B’) occur at ‘C’ (see Dryden, 2012b). The omission of cognitive consequences is significant, as this is what many REBT theorists would label worry or rumination (e.g., ‘I’ll always be alone, no one will ever like me’), which some CT theorists might label NATs. When discussing theoretical comparisons between approaches, the use of the word ‘belief’ can at times be problematic. The word ‘belief’ in some CBT literature is not always evaluative, as it is in REBT, which can cause theoretical confusion. For example, in Westbrook et al. (2012, p. 198), they state, ‘If I become very anxious The History and Philosophical Underpinnings of CBT I will lose control and go mad.’ Some textbooks may label this a prediction or a predictive NAT as opposed to a belief. REBT activating events can be internal or external; past, present, or future; real or imagined (Cristea et al., 2015), meaning the above prediction, if one is utilizing the ABC, is best placed at A, rather than B. This may result in different interventions depending on where the CBT therapist places this level of cognition. In order for complex psychological concepts to be understood and communicated accurately, it would be ideal that any form of psychotherapy that places itself under the umbrella of CBT would make consistent use of CBT nomenclature. A typical example of the dilution of the ABC model can be seen in Skinner and Wrycraft (2014)’s CBT textbook (recommended for those training within IAPT), where ‘A’ is an exam, ‘B’ is meaning (I might fail), and ‘C’ is anxiety. ‘I might fail’ is not overtly evaluative, nor stated clearly as a rule/demand, but rather is a predictive NAT indicating the possibility or prospect of failing. As such, the prospect of failing belongs at A, the meaning of which we can infer is negative due to its associated feelings of anxiety. Kuyken et al. (2009, p. 176) make use of an ABC model, and refer to it as an ABC functional analysis. A refers to antecedents, B refers to behaviors, and C refers to consequences (see Figure 2.2). Cognition – beliefs, in particular – are not clearly labelled nor are they given indication of where one should place relevant cognition. In the B (behavior) of their example, they place ‘Thought about all the work I had not done and how useless I am.’ Whilst thinking is a cognitive behavior, this statement contains an evaluative label, so some CBT therapists may have identified the ‘I’m useless’ and would label this a belief. A therapist utilizing this ABC model would therefore have to put evaluative cognition within a behavioral heading. Whilst Kuyken et al. (2009) do not refer to the origin of the ABC model in their text, this example demonstrates how some CBT therapists make use of an ABC model that differs greatly from how other CBT therapists may utilize an ABC model, such as Skinner and Wrycraft (2014, see above). Having a B within an ABC model labelled ‘behavior’ in a CBT textbook demonstrates how the use of ABC models within CBT varies greatly, arguably creating theoretical confusion. These points demonstrate that the ABC model is not always represented accurately or consistently within CBT literature. Consequently, recent REBT developments are not always acknowledged within CBT literature or are presented in a manner that neglects core theoretical principles. Potential consequences can include a theoretical minefield across literature and possibly the implementation of superficial interventions that result from theoretical inconsistencies in the presentation of terminology (for more detail on the definitions of self-esteem within CBT, see Chapter 30). Protocol-Driven CBT Protocol-based CBT or empirically supported treatment (EST) protocols are a set of specific interventions, used within a set time period for a specific disorder that have 17 18 Jodie M. Paget been shown to be efficacious. These are often compared to a case-formulation approach, which arguably provides greater flexibility over treatment, enables work with more complex presentations, and allows clinicians to make treatment decisions based on continued assessment and their clinical acumen that stems from a sound understanding of core theory (Persons, 2006). There is now a wealth of manuals available to therapists for the treatment of both common and more complex mental health problems (e.g., PTSD, Foa et al., 2007; social anxiety disorder, Hope et al., 2010). The efficacy of protocols for specific disorders is beyond this chapter (see Addis et al., 2006, for a detailed discussion), but what is known is that the efficacy of CBT for depression appears to be decreasing. A meta-analysis conducted by Johnsen and Friborg (2015) found CBT is not quite as potent as it once was. It is no great surprise that they found that patients who received CT for depression from experienced psychologists achieved better results than those receiving it from student therapists. They propose the decline in treatment efficacy may in part be due to a misconception that CBT is easy to learn, and highlight the need for high-quality training and supervision that is conducted by appropriately qualified therapists. In 1979 Beck outlined the prerequisites for psychotherapists conducting CT for depression and stated that the aspiring cognitive therapist should be, at first, a competent psychotherapist. He found fewer than 25% of trainees (consisting of psychiatrists and psychologists) met minimum competency in CT after three months of training in the delivery of CT for depression (Beck et al., 1979). Considering that many training courses in the United Kingdom require competency in delivering CBT for depression, in addition to a wide range of mental health problems within an academic year, it may be worth researching whether increasing duration of training facilitates a wider range of competencies, to help ensure the efficacy of CBT remains as high as it once was. Whilst empirically supported protocols (ESPs) and manuals are useful, patients rarely fit neatly into one diagnostic criterion. Hayes and Hofmann (2017) claim that evidence-based practitioners can enhance their efficacy by employing methods from all generations of CBT and add that there is increased recognition of the importance of philosophical assumptions to methods of treatment interventions. Moreover, they state that upon recognition of this, the inter-organizational task force on cognitive and behavioral psychology doctoral education insists that CBT training include philosophy of science training. Comorbidity is common, and patients can experience a great deal of distress that does not have an associated DSM-5 diagnosis (e.g., meet criteria for a major depressive episode but also struggle with jealously or anger). CBT training that includes teaching of core theoretical concepts, in addition to disorder-specific protocols, may go some way to ensuring that CBT therapists are better equipped to work with the wide variety of presentations they will no doubt encounter. Emotional Disorders and Transdiagnostic CBT In addition to manuals that guide treatment of specific disorders, protocols are beginning to surface that provide guidance for working with emotional disorders The History and Philosophical Underpinnings of CBT and transdiagnostic processes. CT is known for its diagnostic orientation, specifically for treatment of depression, with only a recent move towards process-oriented or transdiagnostic CBT (Mansell et al., 2012). Although Beck (1991) outlined some of the cognitive themes for anger, depression, and sadness, cognitive theory and interventions for emotional disorders has been refined and further developed since the early 1990s, primarily by REBT theorists (see DiGiuseppe & Tafrate, 2010; Dryden, 1993, 1994, 1997; Dryden & Branch, 2008). REBT is inherently transdiagnostic, and does not introduce specific models to explain disorders; rather, it indicates what beliefs and derivatives should be the target for intervention. In generalized anxiety disorder (GAD), for example, beliefs related to uncertainty are the focus of therapy, as well as awfulizing and low frustration tolerance (LFT) derivatives (Cristea et al., 2015). ‘Intolerance of uncertainty’ (IOU) is a central feature in Dugas and Robichaud’s (2007) cognitive model and treatment manual for GAD. They state that GAD sufferers view uncertainty as stressful and upsetting, see uncertain future events as unfair, attempt to avoid unexpected events, and believe uncertainty can interfere with one’s ability to function. Theoretically, these concepts are similar to the REBT ‘demands’ that would be a target of intervention within this disorder (i.e., ‘I need to know I’ll be able to support my family’) and associated derivatives (i.e., ‘It’s horrible that I do not know, I can’t stand not knowing, the uncertainty of life is unfair’). Both CT and REBT help clients to relieve their ego anxiety (self-deprecation when one acts or performs less than ideal or is disapproved of ). The concept of discomfort anxiety, or low frustration tolerance (LFT), however, is specific to REBT, yet aspects of this concept can be seen within Dugas and Robichaud’s (2007) intolerance of uncertainty model (IUM) of GAD. IUM is defined as negative beliefs about uncertainty which impede an individual’s ability to effectively manage situations, resulting in ineffective problem solving and increased worry in an attempt to prevent negative events from occurring (Bottesi et al., 2016). Discomfort anxiety, or LFT, is a state that arises when a person decides or finds (1) their comfort is threatened, (2) they should not have to experience such discomfort, and (3) it is awful to feel such discomfort, as opposed to being merely uncomfortable (Ellis, 1978a, 1980). Ellis conceptualizes LFT as a key factor of poor life function that leads to avoidance, stagnation, impulsivity, abandonment of goals, numbing pain in unhealthy ways, and so on. When discomfort anxiety is evident, the pursuit on behalf of the REBT therapist is to elicit and dispute beliefs that perpetuate it, reconstructing beliefs to be in line with developing high frustration tolerance (HFT), that is, hard to bear versus unbearable, uncomfortable versus intolerable, unfortunate versus completely awful. Furthermore, Ellis claims that the healthy individual, one who demonstrates emotional maturity and stability, will be successful in confronting frustration and proficient in the practice of delayed gratification (responsible hedonism) (Ellis et al., 2009). Ellis (1980, 1994) makes specific reference to REBT’s focus on helping clients manage their discomfort anxiety and notes that therapists should also help patients work on their ‘secondary symptoms of disturbance’ (and tertiary disturbance if 19 20 Jodie M. Paget necessary), specifically, patient anxieties about anxiety. Thus, there are salient points of the IUM put forward by Dugas and Robichaud (2007) that share aspects of Ellis’s concept of discomfort anxiety, a feature that sets it apart from Beckian CT. ‘Clinical perfectionism’ has been identified as a concept within CBT and there are many CBT manuals available that provide guidance for treatment. ‘Perfectionism’ is ubiquitous in the sense that people experience it to varying degrees, as opposed to having or not having it, whereas clinical perfectionism can result in functional impairment due to self-worth being contingent on achieving selfimposed high standards of performance (Egan et al., 2014). Similarly, REBT theory provides a rationale for interventions aimed at changing rigid rules/demands to more healthy standards of performance, and refraining from attaching one’s overall worth to a specific domain (e.g., career). Ellis’s identification of demands is acknowledged by Egan et al. (2014) and they include an example of a completed thought diary set out in an ABC format (see Appendix 2.2). Whilst it is positive to see protocols emerging that further develop or refine CBT interventions, there are aspects of these ‘new developments’ that share much in common with the psychological interventions first put forward by Ellis. As previously discussed, it is not uncommon for CBT nomenclature to be used inconsistently with CBT texts. In the example ABC provided by Egan et al. (2014), some of the cognitions under the ‘beliefs’ section are not evaluative (e.g., ‘the whole presentation was ruined, I may lose my job’) but are inferences/predictive NATs, creating theoretically muddy waters. Moreover, it demonstrates how the ABC has morphed into a format that at times inaccurately displays theoretical principles. Protocol-Driven CBT in IAPT Protocols provide therapists with an overview of evidenced-based treatment interventions and a session-by-session therapy plan for specific disorders, thus are well suited to the psychological services of the UK National Health Service (NHS). In 2008, the English IAPT service began and from its inception was an impressive and radical initiative aimed at providing government-funded evidence-based psychological treatments for adults with depression and anxiety disorders. The three defining features of IAPT are: (1) evidence-based psychological therapies, (2) routine outcome monitoring, and (3) regular outcomes-focused supervision. Its current aim is to increase services to support 1.9 million people by 2024, an increase of 380,000 patients (NHS England, 2019). In order to reach these targets, continued recruitment of trainees is vital as well as the ongoing training, development, and supervision of those working within the service. Unfortunately, according to the British Association for Behavioural and Cognitive Psychotherapies (BABCP), IAPT funding difficulties has resulted in a lack of training places, meaning fewer therapists, long wait times, and ‘patchy’ provision for those who would benefit from these services (BABCP, 2018). Despite IAPT’s good intentions, the cuts imposed by funding Clinical Commissioning Groups (CCGs) have resulted in session limits set below guidelines The History and Philosophical Underpinnings of CBT recommended by the National Institute for Health and Care Excellence (NICE) (e.g., a maximum of six sessions despite guidelines suggesting 12–20). Roscoe (2019) states that IAPT trainees describe a number of restrictions imposed on them by the services in which they work, including a need to rigidly apply disorder-specific protocols (EST protocols) despite this not always being appropriate, not being allowed outside the therapy room to undertake in vivo exposures, and active discouragement from talking about core beliefs due to fear of patient suicides. Moreover, there is an increasing gap between recommended guidelines and what services provide, resulting in sub-therapeutic doses of diluted CBT and culminating in patients returning to therapy for multiple episodes of treatment with different therapists (perhaps partly due to insufficient number of sessions and/or a lack of topup sessions having been offered from the outset). Roscoe further states that this situation is likely to strengthen the misconception that CBT is a superficial treatment. When protocols are taught in isolation there is a danger that therapists, in particular, IAPT therapists, are throwing interventions at ‘problems’ because manuals advise them to, as opposed to using their own clinical judgement based on a sound understanding of theory. Due to the short duration of courses and the necessary adherence to IAPT curriculum, there is little time to teach core theoretical concepts in sufficient detail. Swiftly taught protocols might be less problematic if newly qualified therapists had a sound understanding of core theory, were well supported within service, and were reviewed for competency regularly and meaningfully by experienced and highly trained CBT supervisors. However, this is too often not the case as highlighted by Isabel Clarke, a clinical psychologist within the NHS, who states that it suits managers to regard CBT as a simple, technical fix that can be applied by any of their existing staff, with minimal training and inadequate supervision (Clarke, 2018). The current level of clinical supervision provided by most services to qualified IAPT therapists is one hour (per week) for 20–24 contact hours (per week). Assuming this one hour were only used to discuss how to work with the most difficult presentations (as opposed to being taken up with risk management, referrals, etc.), does this workload/supervision ratio permit therapists time to review sessions, and to appropriately prepare for supervision? Are IAPT therapists consistently supervised by highly qualified, highly experienced, and well-supervised supervisors? Even if the answer to these questions is ‘yes’, it seems improbable that one hour per week is a sufficient amount of time to adequately (and ethically) support fledgling therapists in their continued clinical development. The BABCP insists that newly qualified trainees complete one year of clinical practice before granting full accreditation (BABCP, 2019). Currently, however, newly qualified IAPT therapists are able to become BABCP-accredited cognitive behavior psychotherapists, the same level of accreditation given to those who have studied for many years outside IAPT training courses (i.e., master’s and doctorate courses). This creates the opportunity for IAPT-trained therapists to leave the NHS 21 22 Jodie M. Paget fairly quickly after training and set up private practices, despite limited CBT knowledge, training, and experience. This constitutes a concern for both the reputation of CBT and the NHS staff retention rate. Considerations If funding and/or a dire need for qualified therapists imposes brevity of training, high caseloads, and minimal supervision, then the selection criteria need to be robust enough to ensure that prospective trainees are well suited to post-graduate academic study and demonstrate characteristics suitable for a CBT therapist (i.e., a scientific and curious mind and the ability to apply CBT theory and practice to themselves). It is evident that some of the new developments within CBT have evolved from Ellis’s original model of psychological disturbance. Yet despite the importance and contribution of REBT, its core principles are all too frequently reproduced inaccurately or are diluted versions of what is a sound psychological principle. In an age where the need for instant gratification has never been more present, and selfesteem is so fragile one must be given an award just for showing up, perhaps it is time to focus on increasing one’s discomfort anxiety in addition to fostering healthy self-esteem. When attempting to advance or build on CBT principles, it might be sensible to resurrect such early principles in their entirety, give credence to where they came from, and work on what adaptations need to be made for current presentations and future developments. RECOMMENDED READING David, D. (2014). Rational emotive behavior therapy. Oxford University Press. Dryden, W. (Ed.). (2012). Cognitive behaviour therapies. Sage. Ellis, A. (1994). Reason and emotion in psychotherapy: A comprehensive method of treating human disturbances. Citadel. Robertson, D. (2018). The philosophy of cognitive-behavioural therapy (CBT): Stoic philosophy as rational and cognitive psychotherapy. Routledge. REFERENCES Abelson, R. P., & Rosenberg, M. J. (1958). Symbolic psycho-logic: A model of attitudinal cognition. Behavioural Science, 3(1), 1–13. Addis, M. E., Cardemil, E. V., Duncan, B. L., & Miller, S. D. (2006). Does manualization improve therapy outcomes? In J. C. Norcross, L. E. Beutler, & R. F. Levant (Eds.), Evidence-based practices in mental health: Debate and dialogue on the fundamental questions (pp. 131–160). American Psychological Association. Arch, J. J., & Craske, M. G. (2008). Acceptance and commitment therapy and cognitive behavioural therapy for anxiety disorders: Different treatments, similar mechanisms? Clinical Psychology: Science and Practice, 15(4), 263–279. BABCP. (2018). IAPT therapist funding and stated mental health policy. www.babcp.com/ About/Press/IAPT-therapist-funding-and-stated-mental-health-policy.aspx (2019). Accreditation. www.babcp.com/Accreditation/Accreditation.aspx The History and Philosophical Underpinnings of CBT Bandura, A. (1969). Principles of behaviour modification. Holt, Rinehart and Winston. (1977). Social learning theory. Prentice-Hall. Barlow, D. H. (1988). Anxiety and its disorders. Guilford Press. Beck, A. T. (1967). Depression: Clinical, experimental and theoretical aspects. Hoeber Medical Division. (1970). Depression: Causes and treatment. University of Pennsylvania Press. (1991). Cognitive therapy and the emotional disorders. Penguin. Beck, A. T., Brown, G. K., & Steer, R. A. (1996). Beck Depression Inventory®-II (BDI®-II). www.pearsonassessments.com/ Beck, A. T., Rush, J. A., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of depression. Guilford Press. Beck, A. T., & Steer, R. A. (1993a). Beck Anxiety Inventory® (BAI®). www.pearsonassess ments.com/ (1993b). Beck Hopelessness Scale® (BHS®). www.pearsonassessments.com/ Beck, J. (2011). Cognitive behavior therapy: Basics and beyond. Guilford Press. Biglan, A., & Hayes, S. C. (1996). Should the behavioral sciences become more pragmatic? The case for functional contextualism in research on human behaviour. Applied and Preventive Psychology, 5(1), 47–57. Bottesi, G., Ghisi, M., Carraro, E., Barclay, N., Payne, R., & Freeston, M. H. (2016). Revising the intolerance of uncertainty model of generalized anxiety disorder: Evidence from UK and Italian undergraduate samples. Frontiers in Psychology, 7, 1723. Clark, D. M. (1986). A cognitive approach to panic. Behaviour Research Therapy, 24(4), 461–470. Clarke, I. (2018). The case for CBT: A practical perspective from the NHS frontline. In D. Loewenthal & G. Proctor (Eds.), Why not CBT? Against and for CBT revisited (pp. 362–373). PCCS Books. Cristea, I. A., Stefan, S., David, O., Mogoase, C., & Dobrean, A. (2015). REBT in the treatment of anxiety disorders in children and adults. Springer International Publishing. David, D. (2014). Rational emotive behavior therapy. Oxford University Press. David, D., & Hofmann, S. (2013). Another error of Descartes? Implications for the ‘third wave’ cognitive-behavioural therapy. Journal of Cognitive and Behavioral Psychotherapies, 13(1), 111–121. David, D., & Montgomery, G. H. (2011). The scientific status of psychotherapies: A new evaluative framework for evidence-based psychosocial interventions. Clinical Psychology: Science and Practice, 18(2), 89–99. David, D., Szentagotai, A., Eva, K., & Macavei, B. (2005). A synopsis of rational-emotive behaviour therapy (REBT): Fundamental and applied research. Journal of RationalEmotive & Cognitive-Behaviour Therapy, 23(3), 175–221. DiGiuseppe, R. (1991). Comprehensive cognitive disputing in RET. In M. Bernard (Ed.), Using rational-emotive therapy effectively: A practitioner’s guide (pp. 173–195). Plenum. DiGiuseppe, R., & Linscott, J. (1993). Philosophical differences among cognitive behavioral therapists: Rationalism, constructivism, or both? Journal of Cognitive Psychotherapy, 7 (2), 117–130. DiGiuseppe, R., & Tafrate, R. C. (2010). Understanding anger disorders. Oxford University Press. Dryden, W. (1987). Counselling individuals: The rational emotive approach. Taylor and Francis. (1993). Overcoming anger: When anger helps and when it hurts. Sheldon. (1994). Overcoming guilt. Sheldon. (1997). Overcoming shame. Sheldon Press. (2005). Overcoming jealously. Sheldon Press. 23 24 Jodie M. Paget (2007). Overcoming hurt. Sheldon. (2012a). Rational emotive behaviour therapy. In W. Dryden (Ed.), Cognitive behaviour therapies (pp. 189–215). Sage. (2012b). The ‘ABCs’ of REBT I: A preliminary study of errors and confusions in counselling and psychotherapy textbooks. Journal of Rational-Emotive & Cognitive-Behaviour Therapy, 30(3), 133–172. (2013a). The ABCs of REBT revisited: Perspectives on conceptualization. Springer. (2013b). Unconditional self-acceptance and self-compassion. In M. Bernard (Ed.), The strength of self-acceptance: Theory, practice and research (pp. 107–120). Springer. Dryden, W., & Branch, R. (2008). The fundamentals of rational emotive behaviour therapy: A training handbook (2nd ed.). Wiley. Dugas, M., & Robichaud, M. (2007). Cognitive behavioural treatment for generalised anxiety disorder: From science to practice. Routledge. Egan, S. J., Wade, T. D., Shafran, R., & Antony, M. M. (2014). Cognitive behavioural treatment of perfectionism. Guilford Press. Ellis, A. (1958). Rational psychotherapy. The Journal of General Psychology, 59(1), 35–49. (1962). Reason and emotion in psychotherapy. Citadel Press. (1978a). Discomfort anxiety: A new cognitive-behavioral construct. BMA Audiotapes. (1978b). Rational-emotive theory. In R. J. Corsini (Ed.), Readings in current personality theories (pp. 297–311). F. E. Peacock. (1980). Rational-emotive therapy and cognitive behaviour therapy: Similarities and differences. Cognitive Therapy and Research, 4(4), 325–340. (1993). Better, deeper, and more enduring brief therapy: The rational emotive behaviour therapy approach. Routledge. (1994). Reason and emotion in psychotherapy: A comprehensive method of treating human disturbances. Citadel. (2001). Behaviour psychotherapy: Rational and emotive. In N. J. Smelser & P. B. Baltes (Eds.), International encyclopaedia of the social and behavioural sciences (pp. 1072–1076). Pergamon. (2005a). Discussion of Christine A. Padesky and Aaron T. Beck, ‘Science and Philosophy: Comparison of Cognitive Therapy and Rational Emotive Behaviour Therapy’. Journal of Cognitive Psychotherapy, 19(2), 181–185. (2005b). The myth of self-esteem: How rational emotive behaviour therapy can change your life forever. Prometheus Books. (2007). Unconditionally accepting yourself. Albert Ellis Institute. (2010). A guide to rational living [Film]. Thinking Allowed Productions. Ellis, A., Abrams, M., & Abrams, L. (2009). Personality theories: Critical perspectives. Sage. Ellis, A., Sichel, J. L., Yeager, R. J., Dimattia, D. J., & DiGiuseppe, R. (1989). Rationalemotive couples therapy. Pergamon Press. Fennell, M., & Jenkins, H. (2010). Low self-esteem. In J. Bennett-Levy et al. (Eds.), Oxford guide to behaviour experiments in cognitive therapy (pp. 413–430). Oxford University Press. Foa, E. B., Hembree, E. A., & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences. Therapist Guide. Oxford University Press. Graver, M. R. (2007). Stoicism and emotion. University of Chicago Press. Greenberger, D., Padesky, C. A., & Beck, A. (2015). Mind over mood: Change how you feel by changing the way you think (2nd ed.). Guilford Press. Hayes, S. C. (2002). Buddhism and acceptance and commitment therapy. Cognitive and Behavioural Practice, 9(1), 58–66. The History and Philosophical Underpinnings of CBT (2004). Acceptance and commitment therapy, relational frame theory, and the third wave of behavioural and cognitive therapies. Behaviour Therapy, 35(4), 639–665. Hayes, S. C., & Hofmann, S. G. (2017). The third wave of cognitive behavioural therapy and the rise of process-based care. World Psychiatry, 16(3), 245–246. Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (2012). Acceptance and commitment therapy: The process and practice of mindful change (2nd ed.). Guilford Press. Hofmann, S. G., Asnaani, A., Vonk, I. J. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioural therapy: A review of meta-analyses. Cognitive Therapy and Research, 36(5), 427–440. Hope, D. A., Heimberg, R. G., & Turk, C. L. (2010). Managing social anxiety: A cognitive behavioural therapy approach. Therapist Guide. Oxford University Press. Huber, C. H., & Baruth, L. G. (1989). Rational-emotive family therapy: A systems perspective. Springer. Hyland, P., & Boduszek, D. (2012). Resolving a difference between cognitive therapy and rational emotive behaviour therapy: Towards the development of an integrated CBT model of psychopathology. Mental Health Review Journal, 17(2), 104–116. Johnsen, T. J., & Friborg, O. (2015). The effects of cognitive behavioural therapy as an anti-depressive treatment is falling: A meta-analysis. Psychological Bulletin, 141(4), 747–768. Korzybski, A. (1958). Science and sanity: An introduction to non-Aristotelian systems and general semantic. International Non-Aristotelian Library Publishing Company. Kuyken, W., Padesky, C. A., & Dudley, R. (2009). Collaborative case conceptualisation: Working effectively with clients in cognitive-behavioural therapy. Guilford Press. Lazarus, R. (1991). Emotion and adaptation. Oxford University Press. Linehan, M. (1993). Cognitive-behavioural treatment of borderline personality disorder. Guilford Press. Malkinson, R. (2011). REBT: Past, present and future. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 29(4), 257–262. Mansell, W., Carey, T. A., & Tai, S. J. (2012). A transdiagnostic approach to CBT using method of levels therapy: Distinctive features. Routledge. Marks, S. (2012). CBT in Britain: Historical and present. In W. Dryden (Ed.), Cognitive behaviour therapies (pp. 1–24). Sage. Morris, E., & Oliver, J. (2012). Acceptance and commitment therapy. In W. Dryden (Ed.), Cognitive behaviour therapies (pp. 70–92). Sage. Neenan, M., & Dryden, W. (1999). Rational emotive behaviour therapy: Advances in theory and practice. Whurr. Neff, K. (2003). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2(2), 85–101. (2009). Self-compassion. In M. R. Leary & R. H. Hoyle (Eds.), Handbook of individual differences in social behaviour (pp. 561–573). Guilford Press. Neff, K. D., & Lamb, L. M. (2009). Self-compassion. In S. Lopez (Ed.), The encyclopedia of positive psychology (pp. 864–867). Blackwell. NHS England. (2019). Adult improving access to psychological therapies programme. www .england.nhs.uk/mental-health/adults/iapt/ Padesky, C. A., & Beck, A. T. (2003). Science and philosophy: Comparison of cognitive therapy and rational emotive behaviour therapy. Journal of Cognitive Psychotherapy, 17(3), 211–224. 25 26 Jodie M. Paget (2005). Response to Ellis’ discussion of ‘Science and Philosophy: Comparison of Cognitive Therapy and Rational Emotive Behaviour Therapy’. Journal of Cognitive Psychotherapy, 19(2), 187–192. Pavlov, I. P. (1955). Selected works. Foreign Languages Publishing House. Persons, J. B. (2006). Case formulation-driven psychotherapy. Clinical Psychology: Science and Practice, 13(2), 167–170. Rachman, S. (2015). The evolution of behaviour therapy and cognitive behaviour therapy. Behaviour Research and Therapy, 64, 1–8. Rachman, S., Cobb, J., Grey, S., McDonald, B., Mawson, D., Sartory, G., & Stern, R. (1979). The behavioural treatment of obsessional-compulsive disorders, with and without clomipramine. Behaviour Research and Therapy, 17(5), 467–478. Robertson, D. J. (2018). The philosophy of cognitive therapy (CBT): Stoic philosophy as rational and cognitive psychotherapy. Routledge. Roscoe, J. (2019, February). Has IAPT become a bit like Frankenstein’s monster? CBT Today. Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2001). Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. Guilford Press. Sellars, J. (2010). Stoicism. Acumen. Skinner, V., & Wrycraft, N. (2014). CBT fundamentals: Theory and cases. McGraw-Hill. Smith, C. A. (1982). Trends in counselling and psychotherapy. American Psychologists, 37, 802–809. Stockdale, J. B. (1995). Thoughts of a philosophical fighter pilot. Hoover Institution Press. Warren, J. (2009). The Cambridge companion to epicureanism. Cambridge University Press. Wells, A. (2009). Metacognitive therapy for anxiety and depression. Guilford Press. Westbrook, D., Kennerley, H. & Kirk, J. (2012). An introduction to cognitive behaviour therapy: Skills and applications. Sage. Wilding, C., & Palmer, S. (2010). Teach yourself: Beat low self-esteem with CBT. Hodder. Wolpe, J. (1958). Psychotherapy by reciprocal inhibition. Stanford University Press. Yankura, J., & Dryden, W. (1994). Albert Ellis (Key Figures in Counselling and Psychotherapy Series). Sage. PART ONE COGNITIVE BEHAVIORAL THERAPY FOR ANXIETY DISORDERS 3 CBT for Specific Phobias Lina A. Gega and Barry J. D. Wright Introduction to Specific Phobias Fear takes centre stage in phobias. It is an emotion fuelled by our body’s ‘fight-orflight’ response to a threat, whether it is a sabre-toothed cat in the Ice Age or an enclosed windowless office in the Digital Age. Our feared consequences may have evolved – from ‘Will I eat today, or will I be eaten?’ to ‘Will I escape from this office?’ – but the fear cycle remains the same: we spot a threat, we feel anxious, we run away from it, or we use tactics to keep ourselves safe, and we learn that we have escaped once more, till the next time – and the cycle of fear goes on. Diagnosis Fear has an important role in keeping us safe, and although fear is here to protect us from harm and prepare for danger, disproportionally extreme fear can become harmful because it interferes with people’s lives and with their mental well-being. For a diagnosis of specific phobia according to the DSM-5 (First et al., 2015) the following criteria must be met over a minimum period of six months: 1. 2. 3. 4. Marked fear of a specific object or situation Exposure to the specific object or situation leading to marked anxiety Avoidance of the feared object or situation whenever possible Impact on functioning or daily life. There are the following five diagnostic subtypes of specific phobias: 1. Living creature type: fear of dogs, snakes, spiders, mice, birds, insects, or other creatures 2. Natural environment type: fear of phenomena such as water or storms or of heights 3. Blood-injection-injury type (BII): fear of seeing blood, receiving an injection, or watching or receiving invasive dental or medical procedures 4. Situational type: fear of flying, tunnels, bridges, elevators, or enclosed spaces 29 30 Lina A. Gega and Barry J. D. Wright 5. Other type: fears that do not fit into one of the other categories, such as fear of choking or vomiting, of inanimate objects (e.g., buttons), or of specific people (e.g., clowns, costumed characters). The Curious Case of Blood-Injury-Injection (BII) Phobia Blood-injury-injection (BII) phobia is characterized by intense fear when thinking about or seeing blood, needles, or medical procedures. Individuals tend to avoid any situation connected with blood, for example, going to the dentist or the doctor, watching films with scenes of blood or injury. The sight of blood can cause someone with BII phobia to faint, something which happens very rarely with other types of phobias. The physiological mechanism behind fainting in BII phobia, known as vasovagal syncope, is due to the activation of the parasympathetic nervous system (some theories link this with disgust), which causes the blood pressure to drop and the pulse to slow down (for a review, see Ayala et al., 2009). This is very different from other phobias where the heart rate increases. Vasovagal syncope has implications for CBT as it often necessitates the use of applied tension to increase blood pressure and prevent fainting during treatment (discussed later in the chapter). Case example 1 gives a typical picture of BII phobia. Differential Diagnosis To be certain of a diagnosis of a specific phobia, the fear (or the avoidance and safety behaviors associated with the fear) must not be better explained by another condition, especially agoraphobia/panic disorder and social phobia, or obsessive-compulsive disorder (OCD) and posttraumatic stress disorder (PTSD). The key differentiator between specific phobias and other conditions is the feared consequences (e.g., that the worst thing the individual fears may happen CASE EXAMPLE 1: CHRIS (BII PHOBIA) Chris is a 47-year-old woman who has been recently diagnosed with multiple sclerosis (MS) and needs to start on injectable medication, which she will either administer herself daily or have done weekly by a nurse. She currently refuses the medication because of an extreme fear of injections: she faints as the needle approaches her arm, or she gets so anxious that she starts trembling and has muscle spasms. She is worried about the pain that the injections may cause. She is less worried about watching other people having injections except at times that it looks painful or when people wince with a sharp pain. She also avoids seeing the doctor or dentist, and she avoids watching medical dramas on the TV. On previous occasions when she needed to have an injection, she managed her fear by distraction, by either holding her breath or digging her nails into her palms. She pretended that her arm was an orange and that she was someone else observing this (almost like a feeling of depersonalization). She is more fearful of having an injection than having blood taken, because she says it is the idea of having something injected into her body that makes her worried. CBT for Specific Phobias CASE EXAMPLE 2: MARY (VOMIT PHOBIA) Mary is a 20-year-old woman with fear of vomiting. She sought treatment because her phobia is now restricting her life at the university; for example, she avoids socializing because her fellow students often get drunk on a night out and vomit. Also, she cannot eat food from the student canteen as it is served in open booths that she fears may have been exposed to germs. She avoids watching medical TV series in case someone vomits. She is vigilant for signs of someone being unwell (e.g., looking clammy, pale, and complaining of feeling sick). When she and her family or friends go out to restaurants, she never orders chicken, meat, or dairy products because she worries about contracting gastroenteritis or getting other bacterial infections. She washes her hands several times before she eats; if her fingers or anything else touch her food (e.g., a wrapped sandwich on a plate), then she discards it. She never eats until she is full when she is in a public place (e.g., she leaves half of her meal at a restaurant) because she worries that if she vomits, the more food she has in her stomach, the more horrible it will be; in fact, she has an image in her mind of her ‘projectile vomiting’ on the table and everyone looking at her with disgust. When asked about what the worst thing is that she fears may happen, she says that it would be so awful to vomit or watch someone else vomit that she will be traumatized, and that this is not worth the risk. She remembers when her little brother was violently sick with gastroenteritis and he nearly choked while vomiting. in certain situations). Let’s take the example of Mary, who has vomit phobia, in case example 2. In case example 2, could the diagnosis for Mary be anything other than vomit phobia? How could we make sense of her feared consequences to help us exclude other diagnoses? For example, could it be social anxiety (fear of embarrassment), health anxiety (fear of becoming ill), PTSD (recalling a traumatic incident), or OCD (fear of contamination, repeated hand washing, and not touching food)? In Mary’s case, it is most likely that her fear, avoidance, and safety behaviors are due to vomit phobia because the overriding feared consequence is the ‘awfulness’ of vomiting itself. Social anxiety would have been likely if Mary was worried about vomiting only when she was in a public place, but not worried if she were at home. If Mary’s fear was about becoming ill with conditions involving vomiting (e.g., cancer, heart conditions, sexually transmitted infections), then health anxiety might have been an alternative diagnosis. Finally, if she was worried about contamination from things other than food (e.g., using public bathrooms, touching doors, sitting on public transport), then a diagnosis of OCD also could have been plausible. Background on CBT for Specific Phobias Behavior therapy, the earliest form of CBT, was introduced when Freudian psychotherapy dominated psychiatry, in the 1950s. While Freudian analysis sought to 31 32 Lina A. Gega and Barry J. D. Wright probe the unconscious roots of a phobia, as in the case of Little Hans (a boy who had a fear of horses; Freud, 1909), behavior therapy viewed fear as a learned association (classical conditioning) between a stimulus (the horse) and a response (fear). If Little Hans had received behavior therapy at the time, the strategy would have been to pair the phobic stimulus with a pleasant stimulus (e.g., food) to ‘counter-condition’ the fear response with a more neutral or pleasant response. This was the basis for ‘systematic desensitization’ (Wolpe, 1961), the first CBT variant for specific phobias. Systematic desensitization has evolved into what is now known as ‘exposure therapy’ (established widely by Marks, 1997), in which an individual confronts their feared situation until fear subsides over time (‘habituation’). Through repeated experiences of the feared situations, the association between the stimulus and the fear response weakens until it disappears (‘extinction’). During exposure therapy, the individual must remain focused on the physical and emotional manifestations of their fear (e.g., focus on the heart pounding) and must refrain from engaging in ‘safety behaviors’ to mask or reduce fear (e.g., seeking reassurance or trying to relax). Exposure therapy does not try to counteract a person’s fear responses, as systematic desensitization does; instead, fear in exposure therapy is regulated by grading the feared situations from the least to the most feared, thereby generating a ‘fear hierarchy’. The only meta-analysis available to date of randomized controlled trials on specific phobia treatments (Wolitzky-Taylor et al., 2008) concluded that exposurebased treatments have large effects relative to no treatment, and they also outperform placebo conditions and non-exposure treatment. Still, the same meta-analysis found that non-exposure treatments can have a large effect compared with no treatment. The advent of cognitive therapy in the 1970s (Beck, 1976) influenced CBT for phobias by highlighting that exaggerated negative predictions and unhelpful beliefs about the feared situation fuel fear responses (emotional and physical) and drive safety behaviors. These predictions and beliefs relate to how likely, catastrophic, or awful the consequences of a feared situation are expected to be and how limited the individual’s ability will be to cope with these (‘feared consequences’). Examples of feared consequences in specific phobias relate to coping (‘It will be too much to deal with’), harm (‘I may choke and die’); emotional consequences (‘I hate being out of control of my feelings,’ ‘Vomiting is too awful’), sensory consequences (‘The injection will be painful,’ ‘I hate the big furry body of spider, it makes me cringe and feels like something is crawling on me’), and social consequences (‘If I vomit, people will think am disgusting’). While traditional exposure therapy uses habituation and extinction to reduce fear, cognitive techniques use exposure-based behavioral experiments (BennettLevy et al., 2004) to test key negative predictions that are central to the maintenance of the phobia and to generate and reinforce more realistic beliefs about the feared consequences. These exposure-based behavioral experiments involve some incremental experiences of the feared situation to facilitate new learning and revision of exaggerated predictions; however, these experiments do not need to be repeated or prolonged to achieve habituation and extinction as in traditional exposure therapy. Wolitzky-Taylor et al.’s (2008) meta-analysis of randomized controlled trials on specific phobia treatments drew on five studies that were available at the time to CBT for Specific Phobias compare exposure plus cognitive techniques compared with exposure alone. They concluded that ‘contrary to prediction, exposure augmented with cognitive procedures did not outperform exposure treatment alone. The overall composite effect size was not significant, and comparisons of the two treatments for each assessment domain separately revealed no significant advantage for combining exposure with cognitive techniques’ (p. 1031). CBT Assessment for Specific Phobias Assessment Interview A good starting point for a phobia-specific CBT assessment is to explore a recent occasion when an individual experienced extreme fear. The therapist can start by asking the individual to describe this occasion (what happened, what made them feel scared) and what their particular emotional and physical responses were. For example, some people commonly describe fear with expressions such as ‘being terrified’ or ‘freaking out’, whereas others experience ‘disgust’, feel worried or uncomfortable, or feel like fainting in response to fear. It is important to understand how fear manifests within an individual and thereafter use their own words while referring to their fear responses during formulation and treatment. Other than a recent incident, the therapist can also ask about the first remembered incident or the most severe episode, to form a picture about the phobia’s development and fluctuations over time. A clinical assessment should gather information about an individual’s general mental state, risk factors, serious physical conditions, medication, and social circumstances. A CBT assessment for specific phobias should also gather information about three important topics that relate to formulation and treatment: (1) triggers, (2) feared consequences, and (3) avoidance and safety behaviors. Table 3.1 gives examples of questions to assess each topic. When asking these questions, the therapist gathers information about not only phobia-specific maintenance factors, but also contextual factors that may influence the fear response are identified (e.g., with whom, where, and when it is better or worse) and any adaptive coping methods (e.g., time management to cope with stress). The last part of the assessment is about understanding the impact that the phobia has on different domains of the individual’s life: studies/work, friends/family, hobbies, perception of self, aspirations for the future. This will also be a stepping-stone for setting the end-of-treatment goals, that is, statements about what a person would be able to do and under what circumstances to know that their phobia has improved. Questions that can help the therapist elicit such goals are the following: • What made you decide to come for help now? • Why is it important for you that you stop being afraid of/worry about . . .? • What would you like to do in the future that you cannot do now because of your phobia? • If you woke up tomorrow and were 100% free of your fear/worry, what would be the first thing that you like to do? 33 34 Lina A. Gega and Barry J. D. Wright Table 3.1. Example of phobia-specific CBT assessment questions Phobia-specific information 5Ws What (triggers) Example questions • • • • • • • • • Can you think of a recent incident when you felt really scared of . . . (e.g., heights)/worried about . . . (e.g., vomiting)? Can you think back to the very first time that you felt extreme fear/worry about . . . ? Can you remember any time when you had the worst experience of . . . (e.g., seeing a spider, having an injection)? Looking back, can you pick a situation that was particularly frightening/ overwhelming/stays vivid in your mind? Could you tell me what it was and what makes this situation stand out in your memory? Could you tell me more about what happened? Can you tell me how you felt at the time? What was the first thing you noticed in your body when you started getting worried? What was the most intense feeling that you noticed in your body when you felt extremely scared? Where (better/worse) Are there any places where: • the phobia gets better/worse? • you find it easier to cope with the phobia? • you feel safer/at ease? • you feel more at ‘risk’ or ‘exposed’? With Whom (better/worse) • • • Are there any people that make the phobia better/worse? Who is most helpful when you feel really scared/worried? How do other people (friends, family) help you with the phobia? When (better/worse) • • • Do you remember any times when your phobia got worse? Do you remember any times when your phobia got better? Does your fear of/worry out . . . (e.g., enclosed spaces) change at all over the course of the day/week/year? Why (feared consequences) • What is the worst thing you worry may happen if you had to face up to the things you are most scared of? What is the worst thing you fear may happen if you stopped yourself from scanning the environment for the things that make you anxious/scared? When you are in a situation where you feel anxious/scared, what sort of things go through your mind? • • Avoidance • • • • • Is there anything that you avoid doing because you are scared of/about . . . or because it makes you uncomfortable/worried? What does the phobia stop you from doing? Are there activities you would like to do or places you would like to go or people you would like to see, but you can’t because of your phobia/fear? Is there anything than you don’t do as much as you would like to, because of fear or worry? Is there anything you used to do but now have stopped doing because you feel scared? CBT for Specific Phobias 35 Table 3.1. (cont.) Phobia-specific information Example questions • • Safety behaviors • • • • If you had no fear or worry, what more would you have done differently in the last week or would do differently each day? If you woke up tomorrow and you were no longer scared of/about . . . (e.g., heights, vomiting), how could you family or friends tell? What would they notice you doing differently in your day-to-day life? Is there anything that you do more of/excessively because you are scared of/ worry about . . .? What do you do when you come across (e.g. a spider)/when you find yourself in a situation where (e.g., you have to have an injection), in order to cope? Is there anything that you tell yourself or that you have to do discreetly/in your head when you are faced with situations that trigger your phobia? Is there anything that your family/friends do for you to help you cope with your phobia? Standardized Assessment Tools Diagnostic Tools The specific phobia subsections of the Structured Clinical Interview for DSM-5 (SCID-5; First et al., 2015) and the Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5; Brown & Barlow, 2014) are considered to be the gold standard for establishing a diagnosis through a clinical interview. These diagnostic tools can be used as outcome measures before and after treatment to establish whether an individual has ‘recovered’ from their phobia. The tools collect information about the type of specific phobia (e.g., animal/insect, small spaces, blood/injection phobias), the level of fear, the degree of avoidance, and the extent of interference with daily life. Phobia-Specific Self-Report Questionnaires Standardized self-report questionnaires can measure treatment outcomes for individual specific phobias, such as the following: Spider Phobia: Fear of Spiders Questionnaire (FSQ) and Spider Phobia Questionnaire (SPQ) (Muris & Merckelbach, 1996) Claustrophobia: Claustrophobia Scale (CS) (Öst et al., 2007), Claustrophobia Questionnaire (CLQ) (Radomsky et al., 2001) Fear of Flying: Flight Anxiety Situations (FAS) questionnaire and Flight Anxiety Modality (FAM) questionnaire (Van Gerwen et al., 1999). Fear of Heights: Heights Interpretation Questionnaire (HIQ) (Steinman & Teachman, 2011) BII Phobia: The Blood-Injection Symptom Scale (BISS) (Page et al., 1997) 36 Lina A. Gega and Barry J. D. Wright Vomit Phobia: Emetophobia Questionnaire (EmetQ) (Boschen et al., 2013), Specific Phobia of Vomiting Inventory (SPOVI) (Veale et al., 2013) Generic Phobia Self-Report Questionnaires: Two seminal self-report questionnaires that assess fear and avoidance (including but not limited to specific phobias) are the Fear Questionnaire (FQ) (Marks & Mathews, 1979) and the Fear Survey Schedule (FSS) (Wolpe & Lang, 1964). Since their development decades ago, they have been through multiple iterations, revisions, adaptations, and validations and have been used in hundreds of studies. A more recently developed self-report measure, the Phobic Stimuli Response Scales (PSRS) (Cutshall & Watson, 2004) assesses the cognitive and emotional factors of five fears: social, animal, physical confinement, bodily harm, and blood injection; however, like the FQ and the FSS, the PSRS does not focus on specific phobias and its items do not correspond to the five specific phobia diagnostic subtypes. The only outcome measure designed for specific phobias that covers all subtypes is the recently validated Specific Phobia Questionnaire (SPQ) (Ovanessian et al., 2019). The SPQ assesses the extent of fear and its interference with daily life for a broad range of objects and situations. It consists of 43 items, each rated using a five-point Likert scale on two dimensions – level of fear and interference with daily life – with scores ranging from 0 (no fear/interference) to 4 (extreme fear/interference). The SPQ is scored by combining fear ratings of each specific phobia subtype to create five different composite scores: animals, natural environment, situational, blood-injection-injury, and other. Behavioral Approach Task (BAT) A behavioral approach task (BAT), also known as behavioral avoidance task/test, is a measurement technique in which an assessor observes and rates how far an individual can approach their feared object or enter their feared situation in successive steps. It starts with a simple instruction: I’d like to understand how you react around [the stimulus, e.g., blood/needle, dog, vomit]. What I would like you to do is to open the door, go inside, sit in the chair, and stay until it’s time to leave after several minutes. However, you don’t have to do any more of this than you want to. You don’t even have to open the door. The number of steps is the main unit of measurement for the BAT; that is, scores correspond to the steps that the individual completes, for example, 0 for the first step, 1 for the second, through to 10 for the 11th step. Subjective units of distress (SUDs) are also included at the start and end of the BAT by asking: ‘Using an 8-point scale where 0 is none and 8 is the most, how anxious/scared are you right now?’ The BAT has been introduced by Öst et al. (1991) and subsequently has been widely used with adults (Vernon, 2007) and children (Silverman & Ollendick, 2005). BATs need to be devised for different phobic stimuli (e.g., a spider phobia BAT is CBT for Specific Phobias 37 Table 3.2. Behavioral approach task (BAT) examples Score BAT 1: Vomit phobia BAT 2: Height phobia 0 1 2 3 Does not agree to proceed with BAT Opens door Enters room (passes through doorway) Enters approximately ¼ way into room (about 3–4 feet from doorway) Enters at least ½ way into room (about 6–7 feet from doorway) Enters at least 3/4 way into room (about 9–10 feet from doorway) Stands/comes within 3 feet of transparent container with fake vomit Stands/comes within 6 inches of container Touches or holds container Opens container Sits down beside container for final step (20 seconds) Does not agree to proceed with BAT Presses button to call elevator Enters elevator (passes through doorway) Allows elevator doors to close while inside 4 5 6 7 8 9 10 Rides elevator to top floor Exits elevator Stands more than 6 feet away from railing Stands more than 3 feet away from railing Stands within 6 inches of railing Looks down over railing for < 15 seconds Looks down over railing without using hands for 30 seconds different to a claustrophobia BAT) and may vary in the number of steps included, the way the steps are constructed (e.g., by grading the stimulus or the time spent with the stimulus), the way the steps are scored (e.g., from 0 to 1, or from 0 to 100) and how the instructions are given by the assessor. Table 3.2 illustrates two different BATs for vomit phobia and for fear of heights. CBT Formulation for Specific Phobias Maintenance Cycle A CBT mini-formulation is a way of demonstrating how a phobia is maintained through an interaction between thoughts, feelings, and behaviors that are specific and meaningful to that individual. The three-systems model (Figure 3.1) (introduced by Lang, 1968), although decades old, is a CBT icon that conveys aptly and parsimoniously the ‘maintenance cycle’ of phobias. It does so by demonstrating the links between feared consequences (thoughts), avoidance and safety behaviors, and fear-associated feelings (emotions and physical symptoms). For example, Figure 3.2 illustrates the fear cycle for Chris in case study 1 (BII phobia). The added advantage of a simple visual model is that it can be readily used to explain CBT to children for whom specific phobias are common and debilitating, more so than in adults. Working Hypothesis The three-systems mini-formulation of a specific phobia is the stepping-stone for CBT interventions, because it highlights that a change in any one corner of the triangle can lead to changes in the other two. CBT aims to break the ‘maintenance 38 Lina A. Gega and Barry J. D. Wright Fear response (how or what we feel) Emotions and Physical Symptoms Behaviors (what we do or avoid doing because of fear) Thoughts (what we think may happen in a feared situation) Figure 3.1. Three-systems model for specific phobia. Feelings Feeling worried and scared, muscles tense and have spasms Behaviors Avoid watching medical programs Avoid doctor check-up Digging nails in hands Thoughts ‘I will faint’ ‘ It will be very painful’ ‘I won’t be able to cope’ Image of needle breaking the skin Figure 3.2. Fear cycle for BII phobia. cycle’ of fear by creating a ‘alternative cycle’ in which avoidance is replaced by graded experiences of the feared situation, safety behaviors are removed, and feared consequences are replaced by new ideas about the feared situation. The aim is to replace extreme fear with more neutral and proportionate emotional and physical responses. The individual may never feel happy when they find themselves face-to-face with a situation that they used to dread, but our aim is to replace fear with boredom, and to change the feeling of dread to a sense of readiness and confidence. CBT for Specific Phobias 39 FEAR Figure 3.3. CBT cycle for BII phobia. TIME Figure 3.4. Habituation and extinction. Figure 3.3 illustrates an alternative cycle for case example 2 (Chris, BII phobia) which includes confronting feared situations and reinforcing alternatives to her feared consequences of pain and not being able to cope. Socialization to the Model Habituation and extinction are the proposed mechanisms that explain how graded exposure works (Figure 3.4). Fear is the body’s natural response to excessive adrenaline production when a person is faced with a situation which is threatening or is perceived as threatening. Adrenaline prepares the body for a fight-or-flight response. Fear increases until it reaches a point when the person cannot tolerate it anymore, so the person runs away or uses safety behaviors to cope; by so doing, fear goes down rapidly. As soon as the person comes across the same situation again, fear reappears with the same or greater intensity. If the person remains in this situation a little longer than usual, and most importantly passes the point when they would normally run away or use safety behaviors, the excess adrenaline in the body is gradually depleted and the anxiety symptoms eventually subside. Over repeated and prolonged exposure to the same or similar situations, the peak fear brought on by a situation reduces until it is no longer a feared situation. 40 Lina A. Gega and Barry J. D. Wright Box 3.1 The Principles of Exposure Therapy • Graded: Start from the easiest task and build up to the most dreaded one with increments in between. • Focused: Experience fully the physical and emotional aspects of fear without trying to mask it or avoid it with safety behaviors. • Repeated: Carry out the same exposure task until the peak fear decreases (due to extinction). • Prolonged: Stay with the fear long enough to allow habituation to take place. CBT Methods for Specific Phobias For specific phobias, treatment duration can be shortened by delivering a single threehour session (introduced by Öst, 1989) or with the use of digital media such as virtual reality (Freeman et al., 2018). Irrespective of the duration of treatment or the form by which it is delivered, CBT for specific phobias includes constructing a fear hierarchy, dropping all safety behaviors, exposure practice, and cognitive restructuring. Figure 3.5 gives an overview of the CBT process from assessment to formulation and treatment. Constructing a Fear Hierarchy Constructing a fear hierarchy involves making a list of situations that can cause fear/ anxiety and attaching a rating of distress to each of them on a 0–10 Likert scale, where 0 = not at all distressing and 10 = extremely distressing. The questions asked during the assessment would have elicited some information to help the therapist populate the hierarchy; however, the situations in the hierarchy have to be strategically selected to be directly linked to the feared stimulus and the feared consequence, so that they can be engineered and tested during the treatment process. For example, in spider phobia, ‘sitting in the garden’ or ‘going into the shed’ are not helpful in the fear hierarchy; instead, statements like ‘looking for spider webs in the Assessment Triggers Feared Avoidance and safety behaviors Impact and goals Formulation Treatment Maintenance cycle Construct fear Working hypothesis Drop safety behaviors Socialization to model Exposure practice Cognitive restructuring Figure 3.5. Overview of CBT process for specific phobias. CBT for Specific Phobias garden and the shed and putting my hand through these webs’ or ‘finding a small spider in the garden, putting it in a glass jar and holding the jar’ are more specific and directly linked to the stimulus (spider) and feared consequence (‘touching it’). An easy way to start constructing a fear hierarchy is by using cards or an standard-sized piece of paper cut into eighths. Each card describes a task that involves entering a feared situation/approaching a feared object in various incremental steps. The increments may be of the feared object or of the exposure task. For example, increments of a spider will be ‘small, big, dead, live, toy, picture’, whereas increments of a task will be ‘handling the spider, handling a jar with a spider in it, looking at a spider’. The following is how the relevant hierarchy would look like (the number in parentheses is the predicted fear score): 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Handle small realistic toy spiders. (3) Look at a dead small spider. (4) Handle a jar with a small dead spider inside. (4.5) Handle a jar with a small live spider inside. (5) Touch a small live spider with a short stick. (6) Handle a small live spider. (6.5) Handle a jar with a medium-sized dead spider inside. (7) Handle a jar with a medium live spider inside. (8) Touch a medium-sized live spider with a short stick. (9) Handle a medium-sized live spider. (10) The following is another example of a fear hierarchy for case study 1, Chris (BII phobia), starting from the least difficult and building up to the final goal and most dreaded task, with ratings of predicted anxiety for each task: 1. Handle a syringe without a needle attached and touching my arm with it. (3) 2. Handle a syringe with a needle attached and hold it against the inside of my arm. (4) 3. Watch a nurse prepare all the injection instruments. (4) 4. Have a tourniquet strapped around my upper arm and watch my vein bulge. (5) 5. Watch a video of someone having an injection. (6.5) 6. Watch someone having an injection live. (7) 7. Give an injection to a ‘medical arm’ (a realistic dummy used by doctors to practice injections). (8) 8. Have blood taken (needle draws something out rather than putting something in). (9) 9. Have an injection done to me by a nurse. (9.5) 10. Give an injection to myself. (10) Dropping Safety Behaviors In cognitive behavioral therapy, safety behaviors are discouraged because the individual may attribute the fact that their feared consequences did not happen 41 42 Lina A. Gega and Barry J. D. Wright (or were not as bad as expected) to the safety-seeking behavior (Salkovskis, 1991), rather than take it as evidence that their feared consequence was unlikely to happen (at least to the expected severity) in the first place. In the context of learning theories, using safety behaviors during exposure may get in the way of habituation (because the person does not learn to tolerate distress) and of extinction (because the person does not make new stimulus-response associations) (for a review, see Blakey & Abramowitz, 2016). Safety behaviors can be overt (physical, observable actions) or covert (mental actions, often subtle, that can go unnoticed). Examples of overt safety behaviors include asking for reassurance or for help from someone we trust, holding on to someone or something that makes us feel safe, closing our eyes, or looking away. Examples of covert safety behaviors include imagining that the phobic object is something different (e.g., instead of our arm receiving an injection, pretending it is an orange), having an internal dialogue that takes our focus away from the feared situation (e.g., this is not real, we are dreaming), or counting or reciting things in our minds to feel safe (e.g., a poem or a prayer). When it comes to safety behaviors in CBT, it is important do three things: (1) identify them, (2) understand how they maintain a phobia and how they can obstruct therapy, and (3) eliminate them before, during, and after exposure. Sometimes it is difficult for people to give up their safety behaviors. Children are a good example of this, as they often hold on to objects that make them feel more comfortable, such as a blanket or a teddy. Adolescents and adults hold on to their mobile phone instead of a comfort blanket, or they bring along to therapy their parent or partner instead of a teddy. This may work in the short term but may serve as an ‘emotional crutch’ without which the individual cannot function. We have to be careful not to unintentionally collude with safety behaviors; some therapists may get this wrong by encouraging the graded use of safety behaviors. During exposure therapy, our aim is to engineer an incremental approach to the feared situation so that each increment can be completed without any safety behaviors. In case example 3 below (Kevin, fear of heights), a potential fear hierarchy could involve Kevin going up a staircase, looking out of a window from a high building, or crossing a bridge. Increments for ‘going up a staircase’ could be for Kevin to climb up one step and then turn and walk back down, then climb up two steps, turn and walk back down, and so on. Kevin needs to complete each step (climb up, turn, walk down) until he is ready to move up. Each step needs to be taken as close to the railings as possible (to counteract the safety behavior of walking in the middle of the staircase) but without holding on to the railings (we can suggest that Kevin carries two cups of water while going up the stairs, which makes it impossible to hold on to the railings). Similarly, Kevin can take one step closer to a window or across a bridge and describe how far down is the ‘drop’ he can see (the further he is from the window, the less ‘drop’ he can see), and stay there until his anxiety subsides. The increment here is the distance travelled towards the window or across the bridge, but also the sense of ‘drop’ while looking down. Rachman et al. (2008) introduced the concept of ‘judicious use of safety behaviors’ to overcome obstacles and improve the acceptability and tolerance of exposure CBT for Specific Phobias CASE EXAMPLE 3: KEVIN (FEAR OF HEIGHTS) Kevin is a 19-year-old man with height phobia. He does not use open escalators while he is in a shopping mall, and although he can use a closed elevator, he will not go into a glass one. When he has to walk up the stairs, he would either walk in the centre of the staircase or on the side, holding tightly onto the railings. Kevin avoids going into any building taller than two floors, and if he has to approach a window, he never looks down. He refuses to go walking with his family as this involves going over some hills and bridges in the nearby countryside. When he has to approach any ‘edge’ with a drop beneath it, he freezes and starts shaking. The latest incident happened at a train station when he would not cross the bridge above the platforms to get to a train. When he is asked what the worst thing is that he imagines may happen if he stands at the edge of a cliff or a building or a bridge, he says that he is worried he will fall. When asked why he will not go into a glass elevator or look out of a closed window from a tall building, despite having a barrier that protects him from falling, he says that he feels dizzy and wants to avoid this unpleasant sensation. therapy. Hood et al. (2010) took this further to suggest that safety behaviors could in fact enhance exposure therapy because they can expedite progression through the fear hierarchy and enable people to ‘go the extra mile’ with their final exposure task. Some authors argue strongly for the identification of and eradication of unhelpful safety behaviors (Helbig-Lang & Petermann, 2010). A recent high-quality randomized controlled trial in specific phobias did not find any difference between abstaining completely from safety behaviors or introducing them at first and then systematically fading them out over the course of multiple exposure sessions (Blakey et al., 2019). In summary, empirical findings are mixed as to whether safety behaviors are good, bad, or indifferent when it comes to exposure therapy: their effect seems to depend on how they are used. Safety behaviors tend to have a positive or neutral effect when used selectively for some people at the beginning of exposure, but they are counterproductive when used indiscriminately and throughout exposure. In practice, it is important to weigh both the positive and negative consequences of encouraging the use of safety behaviors. As a rule of thumb, safety behaviors should be dropped at the first opportunity, but their strategic use at the earlier stages of exposure therapy may be helpful. Sometimes it is helpful to carry out behavioral experiments to demonstrate that safety behaviors maintain fear and that these behaviors can become obsolete as the person confirms their fear, as in case example 4 (Susan, claustrophobia and the ‘comforting pendant’). Exposure Practice Repeated practice of an exposure task needs to take place as many times as needed until the task is performed with relative ease. During each exposure task, we monitor an individual’s distress/fear by asking, ‘On a scale from 0 to 10, how 43 44 Lina A. Gega and Barry J. D. Wright CASE EXAMPLE 4: SUSAN (CLAUSTROPHOBIA AND THE ‘COMFORTING PENDANT’) Susan is a 22-year-old woman with claustrophobia. She does not remember how her fear of being trapped somewhere and suffocating started, but she remembers that even as a child she would never lock the toilet door, nor would she sleep on the ‘inside’ of the bed when she had to share a bed with her sister. Her family and friends know about her phobia and accommodate it; for example, they do not use elevators but use the stairs instead when they go to a shopping mall; they also let Susan sit near the door when they are in a new place (e.g., a restaurant) or when using public transport. Susan wears a pendant with a religious symbol on it that gives her a sense of protection if she feels trapped. She always has to wear it when she goes out and has to take public transport. When she feels trapped, she will hold and stroke the pendant between her fingers. During therapy we discussed what would happen if she forgot her pendant at home or lost it. We also talked about how she would feel if she managed to stay in an enclosed space without wearing her pendant. When we constructed the fear hierarchy, we agreed that Susan would do the first few exposure tasks first with the pendant and then without it. Before the exposure task, Susan’s anticipatory anxiety was higher when she did not wear the pendant than when she did. In both occasions, Susan’s anxiety faded away anyway after the exposure task, with or without the pendant. Although the pendant helped her start exposure therapy, once we were able to move up the hierarchy, Susan realized that the pendant did not really make a difference, so she no longer needed it. uncomfortable/worried/scared do you feel at the moment?’ Distress and discomfort are part of exposure, and although they are unpleasant, they are not harmful. However, discomfort should not be so great as to make exposure practice traumatic or disheartening if the individual cannot achieve the task and considers they have failed. The pace of exposure should be negotiated with the individual who carries it out; tasks are fine-tuned throughout the exposure practice and do not have to adhere strictly to the fear hierarchy. An important aspect of exposure is modelling. Once we describe the exposure step (what to do and how), then we show the exposure task without the individual participating, then we do it together with the individual, and finally we encourage them to do it independently. Positive reinforcement should be specific and explicit during each step; for example, not only saying, ‘Well done’, but saying, ‘Well done for moving two steps forward towards this jar of vomit’ or ‘Well done that in the last 10 minutes you focused on this frame of a videoclip of someone vomiting.’ It is expected that many individuals will face difficulties when they try to complete their exposure tasks or will report failure of the exposure to produce the desired effects. The following are some examples and ways to overcome these difficulties. CBT for Specific Phobias ‘I faint when I see blood; how can I do exposure when I am unconscious?’ Applied tension (Ost & Sterner, 1987) (note: different to applied relaxation) aims to stop blood pressure dropping and to increase heart rate. It is carried out by tensing groups of large body muscles (arms, legs, stomach) simultaneously for 10–15 seconds at a time and then releasing them gradually. This is repeated up to five times until faintness subsides. In children it is often difficult to use applied tension because of the speed with which they faint. In this case, using other strategies to increase the blood pressure, such as running on the spot while sitting down or doing star-jumps as the child is standing up are useful ways of keeping the heart pumping and preventing the blood pressure from dropping. ‘I could look out of a window from a tall building, but I could not go up the escalator.’ Exposure tasks should have enough variance in them to address all the feared consequences; for example, fear of heights may relate to escalators (fear of falling) and looking down a window from a tall building (fear of feeling dizzy). The individual may use some covert safety behaviours during exposure which are easy to apply in some tasks but not to others, for example, knowing that they can quickly move away from the window but not easily once they are on an escalator. ‘I was comfortable doing one exposure task but could not move up the hierarchy.’ We may need to grade down the task (develop an intermediate task between two existing tasks in the hierarchy) or choose a different task with similar fear/anxiety rating or use shaping (successive approximation) to help the individual move incrementally towards the next step. Cognitive Restructuring Exposure-based activities are important learning experiences that can be used to restructure exaggerated or unhelpful ideas about a feared situation. Behavioral experiments can be set up in different ways. For example, an experiment may be open-ended to test what might happen if an individual stopped doing their safety behaviors. On the other hand, an exposure-based behavioral experiment could have two or three possible predictions to test which one is likely to happen. Behavioral experiments should ultimately be designed to target key predictions about coping, harm, and aversive emotional, sensory, and social feared consequences. Key questions after successful exposure-based behavioral experiments can help make experiential learning explicit, correct myths about the feared situation, and challenge false assumptions about the feared consequences and about the person’s ability to cope. Examples of such questions are the following: • What have you learnt from this? • What does this tell you about how dangerous/painful/awful . . . (dogs, spiders, heights, injections, etc.) are? • What does this tell you about yourself when you have to . . . (e.g., go into a lift, have an injection)? 45 46 Lina A. Gega and Barry J. D. Wright • Before we started, you thought that you would become very dizzy and not be able to go on an escalator; how do you explain that you can now do it? • What do you expect to happen next time you . . . (e.g., have to go on an escalator)? In between therapy sessions, and after therapy ends, it is important for the individual to carry out self-directed exposure-based activities for three reasons: first, so that the gains from therapy sessions generalize to everyday life and to a variety of feared situations; second, so that avoidance and safety behaviors do not creep back in; and third, so that the individual accumulates positive memories of coping and evidence to reinforce helpful new beliefs about the feared situation. The activities should be designed with specificity and detail. A suggested format is this: ‘to be able to do (observable, measurable behavior) . . ., when/where/with whom (what conditions) . . ., without doing . . . (safety behaviors), for . . . (duration), every . . . (frequency)’. Self-directed behavioral experiments can be used to lay down new memories of coping and success. An individual with a specific phobia can easily forget their positive experiences and selectively attend to evidence that supports their previously held beliefs about the awfulness of their feared situations. To reinforce memories of positive/coping experiences during behavioral experiments, a useful strategy is to create ‘self-talk’ flashcards based on these experiences (e.g., ‘I have done this ten days in a row, I am not looking back’) and by keeping diaries of the behavioral experiments (e.g., when they took place, what the prediction was, what actually happened, what the person learnt). Smartphones, tablets, or laptops can be used to produce idiosyncratic electronic equivalents of flashcards to read, diaries to make notes in, and self-talk recordings to listen to; this may be less cumbersome and fit in better with people’s day-to-day habits (e.g., making notes on their tablet or listening to music and podcasts on their phone), rather than creating paper documents that need to be carried around discreetly, filled in by hand, and kept somewhere privately. Conclusion The application of CBT techniques may vary according to the practitioner’s theoretical orientation, working environment, and level of competence. Practitioners may offer traditional graded exposure therapy or cognitive behavior therapy via exposure-based behavioral experiments. Some may offer multiple, individual CBT sessions; others may offer brief CBT sessions supplemented by self-help materials (guided self-help); and others may deliver a one-session treatment. Irrespective of the format that CBT takes, practitioners should draw on their core skills of engaging an individual, and their family as appropriate, building a trusting working relationship, considering comorbid problems and risks, communicating clearly the treatment process and giving the individual CBT skills and self-confidence to overcome their fear beyond therapy sessions. CBT for Specific Phobias Summary CBT for specific phobias has its roots in behavior therapy but evolved through cognitive therapy. We have discussed two key therapeutic techniques for specific phobias under the CBT umbrella: exposure therapy and cognitive restructuring. Both techniques aim to help people overcome their fear by changing the way they think about, and respond to, their feared situation. Cognitive restructuring for specific phobias focuses on identifying and changing key predictions about coping, harm, and aversive emotional, sensory, and social consequences associated with someone’s fear. Exposure therapy focuses on getting used to a feared situation by letting the fear response subside with time and by weakening the association between the feared situation and the fear response. Both techniques involve working through a fear hierarchy and refraining from using safety behaviors. FURTHER RECOMMENDED READING Davis, T. E., III., Ollendick, T. H., & Ost, L. G. (2012). Intensive one-session treatment of specific phobias. Springer-Verlag. This is the definitive guide on CBT for specific phobias. The first part of the book gives an extensive background on the phenomenology and assessment of specific phobias; it also gives an overview of the evidence for various treatments for specific phobias. The second part of the book focuses on one-session treatment for specific phobias with adults and children. It gives detailed instructions and treatment plans and materials on how to conduct one-session treatments. The last part of the book addresses special topics in CBT for specific phobias, including how to train therapists and assess their competence, how to adapt the treatment for specialist populations (e.g., people with learning or developmental difficulties), ethical issues, research evidence, and use of technologies. Öst, L.-G., & Reuterskiöld, L. (2013). Specific phobias. In S. Gregoris & S. G. Hofmann (Eds.), CBT for anxiety disorders: A practitioner book (pp. 107–133). Wiley Online Publishing. This chapter summarizes the state of the art for specific phobias, including diagnosis and differential diagnosis. It gives an overview of key characteristics of specific phobias, such as age of onset, gender, focus of fear, neurobiology and physiology, comorbidity, impairment, risk factors, and treatment response. The chapter also gives a broad overview of the variants of CBT for specific phobias and discusses evidence of their efficacy. It concludes with a case example of CBT for a complex specific phobia. REFERENCES Abramowitz, J. S., Deacon, B. J., & Whiteside, S. P. H. (2011). Exposure therapy for anxiety: Principles and practice. Gilford Press Ayala, E. S., Meuret, A. E., & Ritz, T. (2009). Treatments for blood-injury-injection phobia: A critical review of current evidence. Journal of Psychiatric Research, 43(15):1235–1242. Beck, A. T. (1976). Cognitive therapy and the emotional disorders. International Universities Press. Bennett-Levy, J., Butler, G., Fennell, M., Hackmann, A., Mueller, M., & Westbrook, D. (Eds). (2004). Oxford guide to behavioural experiments in cognitive therapy. Oxford University Press. 47 48 Lina A. Gega and Barry J. D. Wright Blakey, S. M., & Abramowitz, J. S. (2016). The effects of safety behaviors during exposure therapy for anxiety: Critical analysis from an inhibitory learning perspective. Clinical Psychology Review, 49, 1–15. Blakey, S. M., Abramowitz, J. S., Buchholz, J. L., Jessup, S. C., Jacoby, R. J., Reuman, L., & Pentel, K. Z. (2019). A randomized controlled trial of the judicious use of safety behaviors during exposure therapy. Behaviour Research and Therapy, 112, 28–35. Boschen, M. J., Veale, D., Ellison, N., & Reddell, T. (2013). The emetophobia questionnaire (EmetQ-13): Psychometric validation of a measure of specific phobia of vomiting. Journal of Anxiety Disorders, 27(7), 670–677. Brown, T. A., & Barlow, D. H. (2014). Anxiety and related disorders interview schedule for DSM-5 (ADIS-5): Client interview schedule. Oxford University Press. Butler, G. (1989). Phobic disorders. In K. Hawton, P. M. Salkovskis, J. Kirk, & D. M. Clark (Eds.), Cognitive behaviour therapy for psychiatric problems: A practical guide (pp. 97–128). Oxford University Press. Cutshall, C., & Watson, D. (2004). The phobic stimuli response scales: A new self-report measure of fear. Behaviour Research and Therapy, 42, 1193–1201. Davis, T. E., III, Ollendick, T. H., & Ost, L. G. (2012). Intensive one-session treatment of specific phobias. Springer-Verlag. First, M. B., Williams, J. B. W., Karg, R. S., & Spitzer, R. L. (2015). Structured clinical interview for DSM-5: Research version. American Psychiatric Publishing. Freeman, D., Haselton, P., Freeman, J., et al. (2018). Automated psychological therapy using immersive virtual reality for treatment of fear of heights: A single-blind, parallel-group, randomised controlled trial. Lancet Psychiatry, 5(8), 625–632. Freud, S. (1909). Analysis of a phobia of a five-year old boy. In Case Histories, vol. 8 (pp. 169–306). Pelican Library. Helbig-Lang, S., & Petermann, F. (2010). Tolerate or eliminate? A systematic review on the effects of safety behavior across anxiety disorders. Clinical Psychology: Science and Practice, 17(3), 218–233. Hood, L., Fenwick, J., & Butt, J. (2010). A story of scrutiny and fear: Australian midwives' experiences of an external review of obstetric services, being involved with litigation and the impact on clinical practice. Midwifery, 26(3), 268–285. Lang, P. J. (1968). Fear reduction and fear behavior: Problems in treating a construct. In J. M. Shiler (Ed.), Research in psychotherapy (Vol. 3) (pp. 90–102). American Psychological Association. Marks, I. M. (1987). Fears, phobias and rituals. Oxford University Press. (1997). Behaviour therapy for obsessive-compulsive disorder: a decade of progress. Canadian Journal of Psychiatry, 42(10), 1021–1027. Marks, I. M., & Mathews, A. M. (1979). Brief standard self-rating for phobic patients. Behaviour Research and Therapy, 17, 263–267. Muris, P., & Merckelbach, H. (1996). A comparison of two spider fear questionnaires. Journal of Behavior Therapy and Experimental Psychiatry, 27(3), 241–244. Öst, L. G. (1989). One-session treatment for specific phobias. Behaviour Research and Therapy, 27(1), 1–7. Öst, L. G. (2007). The claustrophobia scale: A psychometric evaluation. Behaviour Research and Therapy, 45(5), 1053–1064. Öst, L. G., Salkovskis, P. M., & Hellstrom, K. (1991). One-session therapist-directed exposure vs self-exposure in the treatment of spider phobia. Behavior Therapy, 22(3), 407–422. Ost, L. G., & Sterner, U. (1987). Applied tension: A specific behavioural method for treatment of blood phobia. Behaviour Research and Therapy, 25, 25–30. Ovanessian, M. M., Fairbrother, N., Vorstenbosch, V., McCabe, R. E., Rowa, K., & Antony, M. M. (2019). Psychometric properties and clinical utility of the specific phobia CBT for Specific Phobias questionnaire in an anxiety disorders sample. Journal of Psychopathology and Behavioral Assessment, 41, 36–52. Page, A. C., Bennett, K. S., Carter, O., Smith, J., & Woodmore, K. (1997). Assessing a structure of phobic symptoms elicited by blood and injections. Behaviour Research and Therapy, 35(5), 457–464. Rachman, S., Radomsky, A. S., & Shafran, R. (2008). Safety behaviour: A reconsideration. Behaviour Research and Therapy, 46(2), 163–173. Radomsky, A. S., Rachman, S., Thordarson, D. S., McIsaac, H. K., & Teachman, B. A. (2001). The Claustrophobia Questionnaire. Journal of Anxiety Disorders, 15(4), 287–297. Salkovskis, P. M. (1991). The importance of behaviour in the maintenance of anxiety and panic: A cognitive account. Behavioural Psychotherapy, 19(1), 6–19. Silverman, W. K., & Ollendick, T. H. (2005). Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34(3), 380–411. Steinman, S., & Teachman, B. (2011). Cognitive processing and acrophobia: Validating the Heights Interpretation Questionnaire. Journal of Anxiety Disorders, 25, 896–902. Van Gerwen, L. J., Spinhoven, P., Van Dyck, R., & Diekstra, R. F. W. (1999). Construction and psychometric characteristics of two self-report questionnaires for the assessment of fear of flying. Psychological Assessment, 11(2), 146–158. Veale, D., Ellison, N., Boschen, M. J., Costa, A., Whelan, C., Muccio, F., et al. (2013). Development of an inventory to measure specific phobia of vomiting (emetophobia). Cognitive Therapy and Research, 37(3), 595–604. Vernon, L. L. (2007). Specific phobia. In M. Hersen & J. C. Thomas (Eds.), Handbook of clinical interviewing with adults. Sage Publications, 247–270. Wolitzky-Taylor, K. B., Horowitz, J. D., Powers, M. B., & Telch, M. J. (2008). Psychological approaches in the treatment of specific phobias: A meta-analysis. Clinical Psychology Review, 28, 1021–1037. Wolpe, J. (1961). The systematic desensitization of neurosis. Journal of Nervous Mental Disorder, 132(March), 189–203. Wolpe, J., & Lang, P. J. (1964). A fear survey schedule for use in behaviour therapy. Behaviour Research and Therapy, 2, 27–30. 49 4 CBT for Panic Disorder Robin D. Bailey Introduction Panic disorder is an anxiety disorder where people experience recurrent, unexpected panic attacks. According to the DSM-5 (American Psychiatric Association, 2013) panic attacks are defined as a period of intense fear in which a minimum of four out of 13 defined physiological symptoms are experienced, for example, palpitations, breathlessness, sweating, and shaking. Panic attacks can also be experienced as ‘unexpected’ or ‘expected’. Unexpected panic attacks appear without an obvious cause, whilst expected panic attacks are often brought on by external stressors, for example, taking a test or in response to a phobia. Although panic attacks are common, to meet diagnostic criteria the individual needs to have a minimum of one panic attack, which is followed by at least one month of persistent concern and worry about having more attacks, and/or maladaptive behavior related to the attacks (e.g., cognitive and behavioral avoidance). Although panic attacks are an essential component of panic disorder, they are not unique to this disorder. Individuals with a wide range of mental health problems may experience panic attacks (which may be considered a key criterion of a disorder), such as the full range of anxiety disorders, including phobia, social anxiety disorder, and generalized anxiety disorder (Goodwin & Gotlib, 2004); depression (Goodwin et al., 2004a); psychotic disorders (Goodwin et al., 2004b); personality disorders (Goodwin et al., 2005); and substance use disorders (Bernstein et al., 2006). The DSM-5 acknowledges this by making panic attacks a generic symptom specifier for all DSM-5 disorders. Before a diagnosis of panic disorder can be made, it is recommended that patients have a medical examination to rule out organic causes that might better explain their anxiety symptoms and panic attack. Direct physiological effects of a substance need to be considered (e.g., excessive alcohol consumption or alcohol withdrawal; medication that has stimulant properties, e.g., corticosteroids, asthma medication, caffeine and caffeine-based medication; medication discontinuation; illicit drugs such as amphetamines). Significant medical conditions of the respiratory (e.g., asthma), 50 CBT for Panic Disorder cardiovascular (e.g., hypertension, cardiac arrhythmia, tachycardia, coronary heart disease), endocrine (e.g., hyperthyroidism, hypoglycaemia, pregnancy), hepatic (anaemia), neurological (e.g., epilepsy), and aural (e.g., vertigo, labyrinthitis, otitis media) systems that might better explain panic symptoms need to be ruled out. Panic disorder is a common mental health problem, with a cross national lifetime prevalence of 1.7% (De Jonge et al., 2016). In an international crosscultural sample, lifetime mental health comorbidity was 80.4%, with anxiety and mood disorders. In primary care settings, panic disorder has been detected in 10.3% of women and 8.8% of men (King et al., 2008). Cognitive Behavioral Model of Panic Disorder and Evidence Base A number of different cognitive and behavioral models of conceptualizing and treating panic disorder have been developed over the last 35 years; these include behavioral models based on the principles of classical conditioning (Wolpe & Rowan, 1988). The key principle of classical conditioning in relation to panic disorder is the process of paired association: the anxiety symptoms of an uncued panic attack are paired with a neutral stimulus (e.g., going on a train). Anxiety then becomes associated with the neutral stimulus. Models based on cognitive, learning, and biological elements (Barlow, 1988) and expectancy theory (Vroom, 1964) put the concept of anxiety sensitivity at the forefront of the development of anxiety disorders. Anxiety sensitivity is based on the theory that bodily sensations arise from beliefs that physical sensations are harmful (Reiss & McNally, 1985). Recently mindfulness-based approaches have begun to explore and treat panic disorder (Beck et al., 1985). The dominant evidence-based CBT model of panic disorder was developed by Clark (1986), which was based on Beck’s (Beck et al., 1985) generic cognitive theory of anxiety and the expectancy model of Reiss and McNally (1985). Wells (1997) revised this model, to give emphasis to the role of safety behaviors as an additional maintenance factor. Clark’s model (see Figure 4.1) revolves around a key theme that people with panic disorder ‘catastrophically misinterpret’ the experience of specific bodily sensations and mental events. According to the Clark model, a panic attack is triggered by either external or internal events. External events can be environments associated with the first or subsequent panic attacks (paired associations), for example, supermarkets. Other external triggers can be hearing or reading words associated with feared symptoms. More often internal experiences act as more powerful triggers for a panic experience. These could be common low-level bodily sensations, such as heart palpitations and light-headedness that arise from normal daily activities (i.e., waking up, exercise, or tiredness). They can also stem from non-anxiety-related emotional states, such as excitement, anger, and happiness. When these triggers arise, people with panic disorder will tend to selectively attend to a particular bodily sensation that is perceived as threatening; for example, a person may worry, ‘This rapid heartbeat could mean I am having a heart attack’. Additionally, the fear of having a panic attack (particularly if one is anxious in anticipation of panic itself ) tends to result in a state of apprehension (‘What if 51 52 Robin D. Bailey TRIGGER STIMULUS (internal or external) Perceived threat Interpretation of sensations as catastrophic Apprehension Body sensations Figure 4.1. Cognitive model of panic disorder (Clark, 1986). I . . .?) and further anxiety. This heightened state of anxiety produces a range of physiological and cognitive symptoms, which the individual will selectively attend to and monitor closely. These symptoms of panic are perceived as dangerous and threatening (i.e., indicating imminent physical or psychological harm). When these symptoms are perceived in a catastrophic way, the patient interprets their physical/ cognitive symptoms as indicative of ‘immediate, impending disaster’ (Clark, 1986; 1988, p. 73). The model assumes that cognition is key to the aetiology and maintenance of panic disorder. Once the symptoms are misinterpreted in this catastrophic way, a negative feedback cycle occurs whereby anxiety perpetuates further increases, physical/cognitive symptoms intensify, and conviction in the belief becomes stronger. In this vicious cycle, the individual becomes motivated to reduce the perceived threat and associated anxiety symptomology. This can include further selective attention to bodily symptoms as a means either to ‘monitor’ the level of threat or to control or stop the anxiety. This can result in increased intensity of symptoms and decreased perceived ability to cope with symptoms and sensations. Ultimately, the patient engages in a range of idiosyncratic safety behaviors intended to prevent the feared catastrophe from occurring and to regulate the associated anxious response (Salkovskis, 1991; Wells, 1997). For example, a person who believes they are going to choke during a panic attack may excessively swallow to clear their throat, or, as a preventive safety behavior, they may carry a bottle of water with them at all times. Paradoxically, the employment of such strategies CBT for Panic Disorder results in the individual feeling less safe as the use of safety behaviors serves to exacerbate physical and cognitive symptoms (e.g., excessively forcing swallowing can mimic the experience of throat constriction), thereby reinforcing the believability of the catastrophic misinterpretation (‘I’m choking’). According to the model, safety behaviors are also problematic as they both prevent disconfirmation of the feared catastrophe and become associated with stopping the feared catastrophe from occurring. Hence, the patient attributes carrying a bottle of water as a preventative strategy for the feared consequence (choking), thereby preventing disconfirmation (they were never going to choke in the first instance). Evidence for the Model For any psychological treatment to be effective, it must have a theory which is well supported. A number of studies over the years have provided evidence for the main tenets of Clark’s model of panic. Findings have supported the assumption that catastrophic misinterpretations of bodily symptoms is a key factor in the development and maintenance of panic disorder (Casey et al., 2004; Hoffart, 2016). It has also been identified that targeting these beliefs in treatment is associated with a reduction in symptoms, including the frequency of panic attacks and the intensity of panic symptoms and associated distress (Hoffart et al., 2008; Teachman et al., 2010) When exploring the role of selective of attention in panic disorder, it has been found that individuals with panic disorder have an attentional bias towards panicrelated stimuli (Pergamin-Hight et al., 2015; Reinecke et al., 2011). In early tests of the model an increased use of safety behaviors has been shown to prevent change in the catastrophic misinterpretations and reduction in levels of anxiety when compared with participants who reduced such behaviors (Salkovskis et al., 1996; Salkovskis et al., 1999). CBT is recommended in the NICE guidelines (NICE, 2011) as the first line of treatment for people with panic disorder. Although other treatments exist (i.e., pharmacotherapy, psychodynamic therapy, and supportive therapy), CBT has the strongest evidence base (Pompoli et al., 2016). In this Cochrane review it should be noted that, although CBT was deemed superior to other treatments, the authors conclude the evidence was not unequivocal. When different variations of cognitive and behavioral therapies were compared, CBT had statistically significant superiority over behavior therapy and cognitive therapy. Evidence also exists that a combination of medication and therapy in the treatment of panic disorder is more effective than medication alone, both during treatment and at 24 months followup (Furukawa et al., 2007). Components of Treatment Theoretical models of psychological disorder, on which treatment is based, should have a strong evidence base to support the key treatment components used to target specific aspects of the theory. Within CBT and BT there is a range of techniques and 53 54 Robin D. Bailey interventions which have been developed to treat panic disorder, including cognitive restructuring, interoceptive exposure, breathing retraining, muscle relaxation, in vivo exposure, and virtual reality exposure. What has also emerged is how these specific interventions, and importantly the combinations and sequence of these interventions, impact on treatment efficacy. In a component network meta-analysis (Pompoli et al., 2018), it emerged that a combination of interoceptive exposure and cognitive restructuring produced the most efficacious form of CBT. The combination of these components (behavioral experiments) are used in both Clark’s (1986) and the modified version of Clark’s treatment protocol for panic (Wells, 1997). Treatments that combine breathing retraining, muscle relaxation, in vivo exposure, and virtual reality exposure in their treatment protocol are less efficacious. It is also worth noting that breathing retraining has a specific low impact on positive outcomes in the treatment of panic, and relaxation is associated with worse outcomes in treatment (Pompoli et al., 2018). This corresponds with the idea that relaxation and breathing retraining may act as a safety behavior that paradoxically prevents disconfirmation of the catastrophic misinterpretation (Wells, 1997). This may explain why CBT may be superior to BT in the treatment of panic disorder (Pompoli et al., 2016). Interpersonal Skills and Therapeutic Alliance It has been shown that patient engagement and perception of the therapeutic alliance may be a contributing factor to positive outcomes in the treatment of panic disorder and low attrition rates (Huppert et al., 2014). These findings highlight the importance of collaboration between the therapist and patient in areas such as goal setting, understanding the model based on the patient’s own experiences of panic, accepting treatment rationale, and a sense of working together towards the amelioration of symptoms. Adherence to the treatment protocol is important in the successful application of CBT for panic disorder. This is particularly important with treatment-resistant patients, as evidence suggests that adherence to protocol can decrease with such patients (Zickgraf, 2016). Treatment resistance may be responded to through re-evaluating the formulation or exploring beliefs about the patient’s fears regarding exposure-based behavioral experiments or concerns about reducing safety behaviors. Ultimately, maintaining adherence to the protocol in a skilled and sensitive manner is key. Patients are generally seen weekly for between five and 15 sessions. Successfully treating panic patients in as few as five sessions is best supported with guided selfhelp materials (Clark et al., 1999). Measurement and Assessment of Panic Disorder Session 1 Assessment should begin with the completion and review of panic-specific outcomes measures. A useful measure is the Panic Disorder Severity Scale (PDSS; Shear CBT for Panic Disorder et al., 1997), which is both a screen for panic disorder (Houck et al., 2002) and measure of severity. This measure also captures pertinent information that can inform and guide the assessment, such as frequency and levels of distress, worry about reoccurring panic attacks, avoidance, fear of physiological symptoms, and impact related to the disorder. The PDSS is repeated and reviewed on a weekly basis since the measure has shown both sensitivity to change and the ability to capture a reduction in panic symptoms over the full course of CBT treatment (Barlow et al., 2000; Shear et al., 1997). Other measures that capture aspects of panic disorder include the Mobility Inventory (Chambless et al., 1985), which assesses agoraphobic avoidance. The Agoraphobic Cognitions Questionnaire assesses the frequency and believability of panic-related thoughts (Chambless et al., 1984). Additionally, in session belief ratings can and should be used before and after any intervention, where 0 is ‘do not believe at all’ to 100 ‘completely believe it to be true’. Often the physiological effects of a panic attack can be a similar to a range of other conditions, including asthma, angina, irregular heartbeat, benign paroxysmal positional vertigo (BPPV), migraine, and thyroid issues. It is important to explore in the assessment whether the panic is linked to any of these conditions or if the patient has had their symptoms checked by a general practitioner; if not, such considerations should be discussed. Patients may have some of these conditions as well as panic disorder; however, it is not within the scope of this chapter to address comorbidity and the reader is advised to read research/treatment manuals that deal with treating panic disorder alongside physical health conditions. Current issues with substance misuse, such as amphetamines, benzodiazepines, and cocaine, which can be associated with panic disorder, need to be addressed during the assessment. Practitioners sometimes find it difficult to differentiate between panic disorder and health anxiety. In both panic disorder and illness anxiety disorder (IAD), individuals misinterpret bodily symptoms as the sign of illness threat, attend to bodily symptoms, and respond with disproportionate levels of fear (Deacon & Abramowitz, 2008). Equally, individuals with both these conditions have a tendency to overutilize healthcare services as a means of explaining the symptoms and gaining medical reassurance (Olatunji et al., 2007). A good starting point in differentiating between these two disorders is to refer to diagnostic criteria such as the DSM-5 as a guide. Additionally, a number of studies have found clear differences between the two disorders (Deacon & Abramowitz, 2008). In panic disorder, the sudden onset of bodily sensations leads to the ‘catastrophic misinterpretation’ that is considered imminent, for example, having a heart attack, whereas with IAD the illness is perceived as more protracted and existing in the future, with more concern being placed on the future significance of symptoms (Noyes et al., 1986; Salkovskis & Clark, 1993). Studies have found that individuals with IAD rate their symptoms as more distressing and tend to have poorer relationships with their general practitioner (Deacon & Abramowitz, 2008; Hiller et al., 2005) than patients with panic disorder. Furthermore, with IAD 55 56 Robin D. Bailey perceived medical symptoms may not be the direct response of anxiety, for example, someone finding a blemish on their skin, unlike panic disorder where symptoms directly arise from autonomic arousal (Williams, 2004). If a patient presents with both panic disorder and IAD, CBT focuses on targeting the same maintaining factor of catastrophic misinterpretations; however, IAD may need more specific interventions due to the chronological occurrence of the perceived illness. (See Chapter 8 for further information on IAD.) Other areas to explore during the assessment can include health-related attitudes and behavior of significant others (family, colleagues, and doctors), current alcohol and drug use, previous medical and psychological treatment, personal strengths, and social and financial circumstances to obtain a wider perspective of panic disorder. Assessment and Formulation (Sessions 1 and 2) Assessment and formulation of panic disorder requires a thorough exploration of the key components of the model that are specific to the patient’s own experience of the disorder. This requires having a template of the model when carrying out the assessment, which can be used for formulation, psychoeducation, and treatment. The panic model is in essence cross-sectional in nature so a detailed evaluation of longitudinal factors may be unnecessary, outside the initial onset of panic symptoms, that is, the first panic attack. Using the template as a guide (see Figure 4.2), ask the patient to think of a recent example of panic that is typical of how they experience the disorder. It is important to do this as it will be fresh in the patient’s memory; it also keeps the assessment focussed and enables the therapist to walk with the patient through the model. The use of Socratic questioning is essential as it enables the development of the therapeutic alliance and helps raise the patient’s insight into the model and how their panic is being maintained. At the end of the assessment it is important to check that all the information gleaned is congruent with the patient’s own experience of their panic. If this is not ascertained, it will have a detrimental effect on both socialization and treatment. Assessment Stages Using the Cognitive Model of Panic Disorder (see Figure 4.1) Internal/External Trigger. Once you ascertain the situational specific aspects of the panic attack, begin by focusing on component number 1 in the model (Internal/ External Trigger). The patient may generate a number of triggers; therefore, it is important to ascertain which of these is most problematic for the patient. Therapist/Patient Dialogue Therapist: Patient: So when you were walking into the lecture theatre, which symptom did you notice first? I just started sweating, my head was racing, I was dizzy. CBT for Panic Disorder 57 INTERNAL/EXTERNAL 1. TRIGGER PERCEIVED THREAT 3. ANXIETY 2. MISINTERPRETATION 5. PHYSICAL/COGNITIVE SYMPTOMS 4. AVOIDANCE & SAFETY BEHAVIORS (Including Selective Attention) 6. Figure 4.2. A cognitive model of panic disorder with maintenance cycles added. From Wells (1997, p. 102). Copyright 1997 by John Wiley & Sons Limited. Reprinted by permission Therapist: Patient: OK that sounds scary, which of these symptoms concerned you most? Feeling dizzy. Anxiety. Then move to component number 2 in the model, to ascertain the emotional experiences. Again, it is important to remember that the patient may have many different ways to describe anxiety, so it is always worth clarifying their terminology. It also worth ascertaining a baseline rating of intensity for the level of emotion using a 1–10 Likert scale. Therapist: And when you noticed the dizziness, how did you feel? Patient: I was like, oh no. Therapist: As a feeling how would you describe ‘oh no’? Patient: It was like pure fear. Therapist: So you were feeling fearful? Scared? Patient: Yes, both. Therapist: On a scale of 0 to 100, how high would you rate your fear, with 0 being none, to 100 being the worst? Patient: Erm, about 70%. 58 Robin D. Bailey Perceived Threat. At component 3 the therapist elicits thoughts that moderate the relationship between the initial trigger and the emotional response. At this stage the catastrophic misinterpretation is not elicited, but more the anticipatory thought about what the patient thought was about to happen. Therapist: Patient: Therapist: Patient: OK, so it sounds like when you went into the lecture you noticed yourself feeling dizzy and as a result you are started to feel yourself getting fearful and scared. Is that correct? Yes, it was horrible. It sounds like it; at that point what was worrying you about these symptoms starting? It just didn’t feel right. I just knew something bad was going to happen. Physical/Cognitive Symptoms. At component 4 the physical and cognitive symptoms experienced in a panic attack are assessed. The aim here is to elicit all the physiological and cognitive symptoms the patient experienced during this panic episode and further establish which of these caused most concern. This can often indicate what the feared catastrophe might be. Therapist: Patient: Therapist: Patient: Therapist: Patient: So when you were feeling really anxious, and you thought something bad was going to happen, did you experience any more physical sensations? Yes, my breathing got worse, I was even dizzier, my legs felt really heavy and wobbly, and then my mind started racing. OK, so which of these symptoms concerned you most? At that moment all of them, though the dizziness was scaring the hell out of me. So as these symptoms escalated what happened to your anxiety? It was going through the roof. It was sky high. Catastrophic Misinterpretation. At component 5 the aim is to elicit the catastrophic misinterpretation. The patient may be able to identify this readily or it may require additional Socratic exploration. It also worth ascertaining a baseline rating of believability in the catastrophic misinterpretation. Therapist: Patient: Therapist: Patient: Therapist: Patient: Therapist: So when you were having these feelings, what was going through your mind? I was just really scared and needed to get out. Ok, so what would have happened if you didn’t get out at that point? Something awful. So something awful like what? Like . . . erm . . . collapsing. So what might have made you collapse? CBT for Panic Disorder Patient: Therapist: Patient: Therapist: Patient: The anxiety was getting so bad I thought it was going to make me pass out. So it sounds like you thought the anxiety could have made you pass out? Yes, it was awful. In that moment in time, how much did you believe that thought to be true, with 0 being not at all to 100 being completely convinced it would happen? Oh, definitely 90%. Safety Behaviors. Initially, it is important to establish any in situ safety behaviors that may be used to prevent the feared catastrophe from occurring or as a means to control the symptoms of anxiety. Therapist: Patient: Therapist: Patient: Therapist: Patient: Therapist: Patient: Therapist: Patient: Therapist: Patient: Therapist: Patient: So, when you were in the lecture theatre is there anything you tried to do to prevent yourself from passing out? I just tried to do some breathing exercises that I read about online. So what did that involve? Breathing in and out quickly into a paper bag. Did this reduce your dizziness? I am not sure, but it might have helped me not pass out. How much do you believe doing these techniques stopped you passing out? Probably about 80% because I did not pass out. Did you do anything to try to control your anxiety in that moment in time? Well I always have my phone ready and have emergency services on speed dial. OK, how does that help reduce your anxiety? Well, if I know I can contact them before I pass out, then they may be able to find and help me. Did this help reduce your anxiety on that day? It did a little, but I was still scared. It is also important to assess any behaviors that may be employed as a way to prevent panic attacks recurring in the future; this can include forms of avoidance. Therapist: Patient: Therapist: Patient: So, at other times maybe when you are not having a panic attack is there anything you do or maybe don’t to prevent another panic attack occurring? I have stopped drinking caffeine. OK, so why is that? I just do not like the feeling it gives, makes me feel dizzy and shaky, which scares me. Even the smell has a negative effect. 59 60 Robin D. Bailey Therapist: Patient: So you avoid caffeine, as you feel it may increase your anxiety and lead to you passing out? Yes. Psychoeducation and Socializing to the Model: (Sessions 2 and 3) Once all the information is gathered after assessment, the therapist should then use psychoeducation to show how all the components of the model fit together to explain the patient’s experience of panic. It is imperative that this is carried out using the patient’s own idiosyncratic experiences of panic, coupled with a clear connection to the theory expressed in a language that is easily understood by the patient. It is important this balance is achieved; otherwise, it can result in a theoretical didactic lecture which may have no relevance to the patient and may potentially rupture the alliance. Alternatively, if it is overly simplistic this may prevent the patient understanding and grasping the theory. This process can be achieved through both verbal and visual presentation of the labelled model with the patient’s own experiences included (see Figure 4.3). INTERNAL/EXTERNAL TRIGGER Lecture 1. theatre/dizzy PERCEIVED THREAT 3. Something bad! ANXIETY 2. Fear/scared 70% MISINTERPRETATION 5. Going to pass out! 90% PHYSICAL/COGNITIVE SYMPTOMS 4. Dizzy, racing mind, wobbly legs AVOIDANCE & SAFETY BEHAVIORS (Including Selective Attention) 6. Breathing exercises, avoid coffee Figure 4.3. Psychoeducation and socialization to the model. CBT for Panic Disorder It is always important at this stage (and throughout therapy) to check that what is presented is congruent and relevant to the patient’s experience; otherwise, this can lead to a breakdown in alliance and interventions that target the wrong processes. The rationale of socializing the patient to the model is to provide patients with a better understanding of what maintains their panic disorder and how working on these processes can lead to symptom relief. Psychoeducational interventions help the patient understand the problem and also increase the patients’ sense of agency, which can lead to a reduction of catastrophic thoughts and emotions. In panic disorder, socialization is a powerful therapeutic intervention in its own right. The key to socializing the patient to the model is to pick important connective components of the model to illustrate experientially how they cause a maintaining effect. In-Session Socialization Exercises The Effect of Thought on Emotion and Physical Sensations A way for patients to see how thinking about specific symptoms is linked to increased anxiety is to get them to complete the paired associates task (Clark, 1988). This activity involves reading a list of words related to physical symptoms, paired with a catastrophic misinterpretation. The aim of this exercise is to enable the patient to discover the true cause of the sensations that occur in panic attacks. In the original version of this task, when patients with panic disorder were presented with a series of associated word pairs referring to catastrophic interpretation (e.g., palpitations-dying), 83% experienced panic symptoms. In a more up-to-date version of the paired associates task, two categories of paired words are used: 10 panicrelated words and 10 neutral words (De Cort et al., 2013). Neutral words are used to help patients understand that only panic-specific words elicit anxiety and not other words. Before beginning the exercise, it is important to get a rating of the patient’s anxiety so this can be compared with levels of anxiety post-exercise. It is important that the patient is not told that this exercise may induce panic, as they may avoid or disengage from reading. Patients should be encouraged to read the words out loud and think about the meaning of the words. After completing the exercise, if there is an increase in anxiety, ask the patient why that might be. In addition, what does that tell them about the role thinking plays in relation to anxiety and increase in physical symptoms? The patient’s specific formulation can be used to further explain how this component of the model maintains anxiety. Paired Association Words (De Cort et al., 2013) Headache – Brain tumour Bookcase – Installation Shortness of breath – Suffocation Flowers – Picking 61 62 Robin D. Bailey Purchase – Shopping Newspaper – Reading Dizziness – Fainting Lemonade – Drinking Shaking – Lose control Shaking – Paralysis Meal – Cooking Weeds – Pull out Tingling – Stroke Rocking chair – Wiggling Chest pain – Heart attack Television – News Nausea – Vomit Garden table – Summertime Racing thoughts – Going crazy The Role of Attention on Thinking and Physical Symptoms Using the exercise above you can highlight how selective attention plays a role in panic disorder. Ask the patient how many catastrophic words they can recall from the list, then ask them to recall how many neutral words they can recall. As patients with panic disorder tend to display strong attentional biases towards panic-related stimuli compared with neutral stimuli (Reinecke et al., 2011), they will be more likely to recall more panicogenic words than neutral words. Another technique used to highlight the role of selective attention is the body focus task. This involves asking the patient to monitor a neutral part of their body, for example, their toes or fingers, to identify as many physical sensations as they can. After a few minutes ask the patient what they noticed. Once the patient reports what sensations they noticed, then ask them how aware they were of the same sensations prior to completing the exercise. This enables the patient to connect that focusing on symptoms increases both the awareness and intensity of the symptoms. This experiment can be expanded upon, to highlight how body focusing may also be an ineffective safety-seeking behavior. Often patients report that if they focus or ‘keep their eye’ on the symptoms, they can either stop or control them. This can be tested by asking the patient to repeat the exercise, but this time, whilst focusing on the sensations, ask them to try to stop or control the sensations by focusing more intensely on them. This tends to result in an increase in sensations and a sense of decreased control. Again, help the patient see how safety behaviors and selective attention can increase and enhance physical sensations, and strengthen belief in the feared catastrophe. The Role of Safety Behaviors The role of safety behaviors in panic disorder can be particularly problematic for two reasons. First, it maintains and exacerbates symptoms, and second, prevents CBT for Panic Disorder disconfirmation of the feared catastrophe. To socialize the patient to this idea the use of metaphors and allegories maybe useful. The following is an example. 1. Some children (and adults) believe scary monsters exist under the bed. Each night when they go to bed, they may get anxious and worry that the monster will get them. To prevent this from happening, they may hold a teddy, sleep with the light on, cover the gap between the bed and floor, or get someone else to check. To date no child has been taken by a scary monster. Because of this the child may believe two things: that if they look under the bed the monster will get them and that teddies, night lights, and so on keep children safe from monsters. A question to help the patient make the connection may be: ‘How can the children discover that their belief is false and that monsters don’t exist?’ One way to highlight further the role of safety behaviors is for the patient to complete a behavioral experiment whilst engaging in and even increasing their safety behaviors, to prove that catastrophe does not occur. This principle is explored later when we look at behavioral experiments. Treatment Discussion Techniques (Sessions 3–13) The aim of treatment is to help the patient to challenge their catastrophic misinterpretation and recognize the benign nature of anxiety symptoms, ultimately becoming less fearful of the unpleasant symptoms. As stated earlier in the chapter, two optimal CBT techniques can be utilized to achieve this: cognitive restructuring and exposure to bodily symptoms. Optimal improvements may be obtained when cognitive and exposure techniques are integrated to the modification of specific misinterpretations (Salkovskis et al., 2007). Cognitive Restructuring The aim of verbal reattribution techniques is to weaken the patient’s belief in the likelihood of the catastrophic misinterpretation (CM) occurring and to strengthen the belief that physical sensations are not inherently dangerous and that it is the meaning assigned to them that makes them frightening. Completing verbal reattribution prior to behavioral experiments is a beneficial way to help loosen conviction in the CM. As always in CBT, the aim is to teach the patient how to challenge their own CM independently. The following standard principles of verbal reattribution are applied: 1. The belief in the catastrophic misinterpretation is identified and rated. 2. Evidence for and against the catastrophic interpretations is reviewed and challenged. 3. Alternative cognitive accounts of the patient’s panic attacks are explored. 63 64 Robin D. Bailey Table 4.1. Panic thought record Emotion and % of intensity Situation Going into lecture and feeling dizzy Anxiety and fear 70% Catastrophic misinterpretation (CM) and % of belief Was going to pass out. 90% Evidence for CM Evidence against CM Alternative explanation Felt dizzy. Was scared. Felt hot. I didn’t pass out. I have never passed out and felt like this lots of times. Feeling these symptoms does not lead to passing out. To pass out, blood pressure needs to drop; when people panic, their blood pressure rises. Lots of other people feel anxious and do not pass out. New belief rating 40% 4. Rating of belief in the alternative response and re-rating of belief in the catastrophic interpretation are carried out. Completion of Cognitive Restructuring for Homework A panic thought record (see Table 4.1) to illustrate how to complete cognitive restructuring may be a useful tool to facilitate practicing this technique and enhance homework practice. Some patients find the use of the paper redundant in this technological age, so adaptation through electronic means (completion on an electronic device) may be more relevant. Identification of Catastrophic Misinterpretation. This will have been identified during assessment; however, it is always worth rechecking with the patient: Is it still the same or are there other additional beliefs? Evidence for and Against. At step 2 of cognitive restructuring, the therapist questions and challenges the evidence for the patient’s catastrophic misinterpretation(s), and substitutes these ideas with more realistic interpretations of the symptom(s). It is quite common for patients with panic disorder to neglect objective evaluation of CM-supporting thoughts. The following questions may be helpful. If you have experienced at least 20 panic attacks, what do you think are the reasons you have never passed out? If you didn’t believe that you were going to pass out, how anxious would you be? How does anxiety lead to, for example, having a heart attack? (questioning the mechanism) If anxiety caused (stroke/madness/heart attack), how many people in a day would suffer these illnesses? How many people do you know who have experienced anxiety but have not had a heart attack/fainted/had a stroke/gone blind? CBT for Panic Disorder 65 Table 4.2. Examples of catastrophic misinterpretations and an alternative explanation Catastrophic misinterpretation ‘I am going to pass out’ ‘I am going to have a heart attack’ ‘I am going to suffocate’ ‘I am going blind’ ‘I am having a stroke’ ‘I’m going crazy’ Alternative explanation To pass out, blood pressure needs to drop; when people panic, their blood pressure rises. Police officers, ambulance drivers, and firefighters when attending to an emergency feel anxious and don’t pass out. There are situations where people can pass out, specifically if someone has a blood-injury-injection phobia. The role of adrenaline when anxious is to keep us safe rather than kill us. Panic is about fear of our bodily sensations and where they might lead. Our reaction to the fear is the same as if we came face to face with a lion. Suffocation can occur only if your airways are blocked by something. Breathing is an automatic process and not something we need to think about controlling; our bodies self-regulate. Airways do not spontaneously close when anxious. Blindness is primarily caused by age-related eye diseases that include macular degeneration, cataracts, diabetic retinopathy, and glaucoma. These diseases are progressive and develop over a long period of time. It is not something that is caused or happens through experiencing emotion. A stroke is when the circulation of blood to the brain declines. Decreased blood flow and lack of oxygen results in loss of brain cells. Strokes can be caused by either a blockage of blood flow to the brain or bleeding into the brain. Anxiety does not clot blood. Feeling frightened of symptoms of anxiety and the fear of what it means and where it might lead, that is, to uncontrollable anxiety and losing one’s mind or the fear that your brain is not working properly, serves to increase anxiety. When in a heightened state of anxiety, it is normal to feel detached and disconnected from ourselves, like walking on cotton wool or when hearing the echo of our voice, which adds to our worry and fears and at the time feels very real. It is not possible to ‘go crazy’ through panic. How often have you been convinced that (CM) will happen and it hasn’t happened? What reasons do you have to believe that (CM) is unlikely to happen in a panic attack? Alternative Explanations. At step 3 the aim is to explore and strengthen alternative explanations for the symptom other than the CM. This involves providing the patient with some further psychoeducation and counter-evidence to the CM. It is important that this be facilitated through guided discovery and Socratic questioning. Some examples of alternative explanations are shown in Table 4.2. Modifying Images (Sessions 3–13) Although patients often verbalize their feared catastrophic misinterpretation, for some this may represent itself more as an image or variety of images. In much 66 Robin D. Bailey the same way as above, these images can be challenged using verbal-based techniques. In some situations, working with imagery may be of additional benefit to weaken belief and reduce the associated affect. One such technique proposed in Clark and Salkovskis (2009) is image restructuring with the aim of generating an alternative image to the feared image. This involves, first, helping the patient make the distinction between imagery and reality. Second, ask the patient to bring to mind a negative catastrophic image and hold it in mind until they feel anxious. Third, once they feel an increase in anxiety, they transform all aspects of the image into something more positive. This transformation enables to patient to observe and experience affective change through manipulation of an image. Fourth, the image may require changing in stages, with the most distressing components being chosen for transformation first. The patient is encouraged to practice this over the course of a week for homework, to further reduce frequency and believability. Behavioral Experiments (Sessions 3–13) A natural follow on from any form of verbal reattribution is to further test out the patient’s specific predictions through behavioral experiments. Although cognitive restructuring may bring around some belief change at a logical and intuitive level, the strength of the belief can be further reduced through gathering experiential evidence (Bennett-Levy, 2003). In essence, patients may understand theoretically that they may not pass out; however, it becomes indisputable only when they see that they do not. Additionally, behavioral experiments are a very powerful tool in enabling the patient to find out that safety behaviors do not prevent feared catastrophes and in fact can maintain emotion and physiological effects. For a full review on behavioral experiments, see the Oxford Guide to Behavioral Experiments (Bennett-Levy et al., 2004). One of the main forms of behavioral experiments used in panic disorder are symptom induction experiments. The aim of these types of experiments is to enable the patient to experience the emotional/physical/cognitive symptoms that closely resemble those experienced when having a panic attack. From this they can find out the non-catastrophic cause of the symptoms and that the sensations that accompany panic attacks are not dangerous. The following specific steps are among those that need to be considered before setting a behavioral experiment. 1. Ensure the patient understands and buys into the rationale for the experiment; this is linked to the formulation and any verbal reattribution that has occurred. 2. Make sure the induction exercise is specific to the patient’s CM. 3. Rate the believability in the CM before and after the experiment, and through all future experiments. 4. Make sure the patient is not engaging in any overt or covert safety behaviors when doing the experiment. 5. This should be practiced for homework to accrue real in situ disconfirmation CBT for Panic Disorder Note that assessment of any diagnosed physical conditions is important and that it is advisable to seek assurance from the patient’s doctor that it is safe to use interoceptive exposure. For further information, it is worth reading Bennett-Levy et al.’s work on self-reflection and self-practice (Bennett-Levy et al., 2001) Below are some examples of experiments that may be beneficial in testing out and challenging specific catastrophic misinterpretations. Catastrophic Misinterpretation: ‘I am going to faint/pass out/collapse’ The hyperventilation provocation task (HVPT) is the most useful behavioral experiment to use with this belief. Hyperventilation on its own is not necessary or sufficient to induce panic; it is the patient’s misinterpretation of somatic symptoms that are the issue. 1. The therapist models HVPT by breathing in and out as deeply and as quickly as they can. 2. The patient and therapist stand together and breathe deeply and rapidly for a few minutes (time duration may need to be graded depending on the patient’s level of fear). 3. If safety seeking behaviors are being used, the patient is prompted nonverbally to desist. 4. At the end of the HVPT, the patient is informed they should stay standing, resume normal breathing for the next few minutes, and further desist from using any safety-seeking behaviors. 5. The patient is then asked to re-rate their belief in the CM and comment on what happened to the physical symptoms when left alone (these will have decreased). 6. Repeat until the belief in the CM is significantly reduced. These experiments can be repeated with variations to help strengthen belief in the non-occurrence of the catastrophe, and that the sensations that accompany panic attacks are not dangerous. During the experiments it is worth asking the patient to make predictions about what they think will happen and then assess whether these predictions are correct. If the patient believes they will pass out due to dizziness or derealization, the above experiment can be carried out with the addition of asking the patient to spin around three times. Spinning can mimic the symptoms of dizziness and derealization; however, the patient can learn that these symptoms do not lead to the feared catastrophe of passing out. Catastrophic Misinterpretation: ‘I am going to have a heart attack’ Inducing physical activity to enhance cardiac awareness can be used to challenge this CM. This should include enough physical exercise to get the blood flowing and the heart speeded up, which can bring on other feared physical sensations, such as breathlessness, sweating, or dry mouth. Activities can be sitting to standing exercises, running on spot, walking up and down stairs, and so on. 67 68 Robin D. Bailey Catastrophic Misinterpretation: ‘I am going to suffocate/choke/stop breathing’ In this behavioral experiment you can get the patient to engage in some paradoxical experiments, through the ‘holding the breath test’. This involves asking the patient to intentionally stop breathing (i.e., hold their breath) to see what happens. Patients discover that it impossible to volitionally hold their breath for long periods of time. After a while the brain will automatically start the breathing rhythm again, even if they try very hard to hold their breath. Catastrophic Misinterpretation: ‘I am going to lose my mind/go crazy’ This can be tested using the HVPT with the addition of instructing the patient to intentionally worry about going crazy whilst doing the exercise. This can be further modified if the patient has specific behaviors which they associate as a sign of losing one’s mind, such as running around in circles or screaming. Again, the patient completes the HVPT and during the exercise carries out the behaviors to see if they actually go crazy/lose their mind. Catastrophic Misinterpretation: ‘I am having a stroke’ In this experiment, first, we get the patient to compare the difference between the specific symptoms experienced when someone is having a stroke (using the established acronym of FAST [see below]; Flynn et al., 2014) compared with when someone is having a panic attack, to find out the symptoms are completely different. Then, the patient can complete a HVPT and test out whether they have any of the symptoms of a stroke. F (Face): Because the face may have dropped to one side during a stroke, test whether they are able to smile. A (Arms): Because of weakness and numbness in the arm during a stroke, test whether they are able to lift both arms and keep them there. S (Speech): Because speech becomes slurred and garbled during a stroke, test whether they can speak a number of sentences clearly.1 These are just some examples of behavioral experiments; therapists should be creative when working with patients to devise and develop idiosyncratic behavioral experiments. If the patient has a pre-existing physical condition such as cardiac issues or chronic obstructive pulmonary disease, use a specific treatment manual (Livermore et al., 2010; Tully et al., 2017) that incorporates safe interoceptive exposure. Behavioral Experiments and Safety Behaviors It is important to reinforce with the patient that safety behaviors can often be part of the problem in panic disorder rather than a solution. During the completion of all 1 The final ‘T’ in the acronym stands for time, which is of the essence in a real stroke situation. CBT for Panic Disorder behavioral experiments patients are encouraged to actively desist from engaging in overt and covert safety behaviors. To highlight the problematic nature of safety behaviors, patients can complete the above behavioral experiments and actively try to control or stop symptoms by increasing their use of safety behaviors. For example, patients who believe they are going to go insane when panicking can try actively suppressing their thoughts, resulting in a paradoxical rebound effect. Or patients who believe that they will stop breathing during panic attacks can try deliberately focusing on/controlling their breathing, making breathing seem irregular/unnatural and increasing anxiety. Behavioral Experiments as Homework It is important and a more powerful learning experience for the patient to carry out behavioral experiments away from the therapy room and on their own. This has a number of therapeutic effects, such as the following. 1. Patients can believe that the security of a therapy room and the presence of a professional are factors preventing the CM from happening. Practicing experiments on their own (at home and in feared situations) helps them find out that feared catastrophes do not occur and that the sensations are not dangerous. 2. It strengthens beliefs in the ability to choose to respond differently to symptoms of panic, reduces the perception of threat, and increases belief in their ability to cope. 3. It facilitates long-term learning whereby the patient becomes more self-reliant and less dependent upon the therapist and therapy. All behavioral experiment homework should follow logically from the session work and be collaboratively devised. Review of homework should always be explored at the start of the next session. This can all be facilitated by using a behavioral experiment record and the acronym SPEAR (Situation, Prediction, Experiment, Actual Outcome, Review) (see Table 4.3), with the first three components of the acronym (SPE) completed in session, and the last two components (AR) completed after the experiment and reviewed in the next session (see below). Relapse Prevention and Blueprint for Therapy (Sessions 5–15, Depending on How Well Patient Responds to Therapy) Once the patient has reported a reduction in panic symptoms and severity and is below the clinical cut-off on the outcome measures used, then therapy should move into relapse prevention. To facilitate relapse prevention, some detailed questioning regarding how the person will manage post-treatment is needed. This enables the therapist to assess for any residual beliefs or behaviors that may still be problematic, currently or in the future. It also addresses whether the patient has fully understood what maintains their panic and whether they are clear on the strategies they need to continue using. 69 70 Robin D. Bailey Table 4.3. Behavioral experiment record modelled with SPEAR (situation, prediction, experiment, actual outcome, review) SITUATION Where and when. Going into lecture theatre. PREDICTION What is your feared prediction? (Belief rating 0–100%) If I go and there are lots of people, I will get so anxious I will pass out. EXPERIMENT What will you do to test the prediction? What will you not do to test the prediction (safety behaviors)? Go into lecture theatre with the knowledge that anxiety is not dangerous and cannot make me faint. Avoid looking at phone and do not do breathing exercises (these make me worse). Actually listen to the lecture. ACTUAL OUTCOME What really happened? Did the outcome match the prediction? I did not pass out. I did feel a bit anxious to begin with, but this seemed to disappear. I felt quite proud of myself. REVIEW What have you learned? Re-rate belief. How can apply this for the future? Anxiety really does not make me pass out. I learned more in the lecture than I ever have. Next time I will try and not sit close to an exit. 10% This can be achieved by asking the patient some hypothetical questions such as the following: What happens in the future if you begin to feel some of the old symptoms? What would you do? If you begin to have thoughts that you may ‘pass out’, how can you respond to that thought? In the future, do you think it would be helpful to start using your old (safety) behaviors again? It is also worth normalizing with the patient that experience of panic and anxiety may be something that will occur, as it does for many people. It is important to view this not as a relapse but as a good chance to practice and develop skills learned. It is also worth giving the patient copies of the formulation and treatment techniques to review in the future if any issues arise. What may be even more beneficial is giving the patient the option of recording each session, so that they have an actual copy of everything that has occurred throughout the treatment. This enables the patient to re-listen and strengthen their understanding post-treatment. Key Learning Points • Assessment of panic disorder requires detailed analysis of the key components that maintain the disorder. Use the model to guide assessment. • Formulation and socialization to the model are essential to help the patient understand how panic disorder is maintained. It is also a powerful change mechanism in itself. CBT for Panic Disorder (cont.) • Both cognitive and behavioral change methods should be derived from the idiosyncratic case formulation and be specific to the patient’s presentation. • Homework is essential to help the patient discover that feared catastrophes do not occur in their own environment. • If residual beliefs exist towards the end of therapy, relapse prevention should focus on modifying these before therapy ends. RECOMMENDED READING Bennett-Levy, J. E., Butler, G. E., Fennell, M. E., Hackman, A. E., Mueller, M. E., & Westbrook, D. E. (2004). Oxford guide to behavioral experiments in cognitive therapy. Oxford University Press. Bennett-Levy, J., Turner, F., Beaty, T., Smith, M., Paterson, B., & Farmer, S. (2001). The value of self-practice of cognitive therapy techniques and self-reflection in the training of cognitive therapists. Behavioral and Cognitive Psychotherapy, 29(2), 203–220. Clark, D. M. (1996). Panic disorder: From theory to therapy. In P. M. Salkovskis (Ed.), Frontiers of cognitive therapy. Guilford Publications, 318–344. Hackmann, A. (1998). Cognitive therapy with panic and agoraphobia: Working with complex cases. In N. Tarrier, A. Wells, & G. Hoddock (Eds.), Treating complex cases. Wiley, 27–43. Livermore, N., Sharpe, L., & McKenzie, D. (2010). Panic attacks and panic disorder in chronic obstructive pulmonary disease: A cognitive behavioral perspective. Respiratory Medicine, 104(9), 1246–1253. Tully, P. J., Sardinha, A., & Nardi, A. E. (2017). A new CBT model of panic attack treatment in comorbid heart diseases (PATCHD): How to calm an anxious heart and mind. Cognitive and Behavioral Practice, 24(3), 329–341. Wells, A. (1997). Cognitive therapy of anxiety disorders: A practice manual and conceptual guide. John Wiley and Sons. REFERENCES American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.) (DSM-5). American Psychiatric Association. Barlow, D. H. (1988). Anxiety and its disorders. Guilford Press. Barlow, D. H., Gorman, J. M., Shear, M. K., & Woods, S. W. (2000). Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. JAMA, 283(19), 2529–2536. Beck, A. T., Emery, G., & Greenberg, R. L. (1985). Anxiety disorders and phoblas: A cognitive perspective. Basic Books. Bennett-Levy, J. (2003). Mechanisms of change in cognitive therapy: The case of automatic thought records and behavioral experiments. Behavioral and Cognitive Psychotherapy, 31(3), 261–277. Bennett-Levy, J. E., Butler, G. E., Fennell, M. E., Hackman, A. E., Mueller, M. E., & Westbrook, D. E. (2004). Oxford guide to behavioral experiments in cognitive therapy. Oxford University Press. Bennett-Levy, J., Turner, F., Beaty, T., Smith, M., Paterson, B., & Farmer, S. (2001). The value of self-practice of cognitive therapy techniques and self-reflection in the training of cognitive therapists. Behavioral and Cognitive Psychotherapy, 29(2), 203–220. 71 72 Robin D. Bailey Bernstein, A., Zvolensky, M. J., Sachs-Ericsson, N., Schmidt, N. B., & Bonn-Miller, M. O. (2006). Associations between age of onset and lifetime history of panic attacks and alcohol use, abuse, and dependence in a representative sample. Comprehensive Psychiatry, 47(5), 342–349. Casey, L. M., Oei, T. P., & Newcombe, P. A. (2004). An integrated cognitive model of panic disorder: The role of positive and negative cognitions. Clinical Psychology Review, 24(5), 529–555. Chambless, D. L., Caputo, G. C., Bright, P., & Gallagher, R. (1984). Assessment for fear of fear in agoraphobics: The Body Sensations Questionnaire and the Agoraphobia Cognitions Questionnaire. Journal of Consulting and Clinical Psychology, 52, 1090–1097. Chambless, D. L., Caputo, G. C., Jasin, S. E., Gracely, E. J., & Williams, C. (1985). The mobility inventory for agoraphobia. Behavior Research and Therapy, 23, 35–44. Clark, D. M. (1986). A cognitive approach to panic. Behavior Research and Therapy, 24(4), 461–470. Clark, D. M. (1988). A cognitive model of panic attacks. In S. Rachman & J. D. Maser (Eds.), Panic: Psychological perspectives (pp. 71–89). Lawrence Erlbaum Associates. (1996). Panic disorder: From theory to therapy. In: P. M. Salkovskis (Ed.), Frontiers of cognitive therapy. Guilford Publications, 318–344. Clark, D. M., & Salkovskis, P. (2009). Cognitive therapy for panic disorder: Manual for IAPT high intensity therapists. Clark, D. M., Salkovskis, P. M., Hackmann, A., Wells, A., Ludgate, J., & Gelder, M. (1999). Brief cognitive therapy for panic disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 67(4), 583. De Cort, K., Hermans, D., Noortman, D., Arends, W., Griez, E. J., & Schruers, K. R. (2013). The weight of cognitions in panic: The link between misinterpretations and panic attacks. PloS One, 8(8). De Jonge, P., Roest, A. M., Lim, C. C., Florescu, S. E., Bromet, E. J., Stein, D. J., & AlHamzawi, A. O. (2016). Cross-national epidemiology of panic disorder and panic attacks in the world mental health surveys. Depression and Anxiety, 33(12), 1155–1177. Deacon, B., & Abramowitz, J. S. (2008). Is hypochondriasis related to obsessive-compulsive disorder, panic disorder, or both? An empirical evaluation. Journal of Cognitive Psychotherapy, 22(2), 115–127. Flynn, D., Ford, G. A., Rodgers, H., Price, C., Steen, N., & Thomson, R. G. (2014). A time series evaluation of the FAST national stroke awareness campaign in England. PLoS One, 9(8). Furukawa, T. A., Watanabe, N., & Churchill, R. (2007). Combined psychotherapy plus antidepressants for panic disorder with or without agoraphobia. Cochrane Database of Systematic Reviews, (1). Goodwin, R. D., Brook, J. S., & Cohen, P. (2005). Panic attacks and the risk of personality disorder. Psychological Medicine, 35(2), 227–235. Goodwin, R. D., Fergusson, D. M., & Horwood, L. J. (2004a). Panic attacks and psychoticism. American Journal of Psychiatry, 161(1), 88–92. (2004b). Panic attacks and the risk of depression among young adults in the community. Psychotherapy and Psychosomatics, 73(3), 158–165. Goodwin, R. D., & Gotlib, I. H. (2004). Panic attacks and psychopathology among youth. Acta Psychiatrica Scandinavica, 109(3), 216–221. Hiller, W., Leibbrand, R., Rief, W., & Fichter, M. M. (2005). Differentiating hypochondriasis from panic disorder. Journal of Anxiety Disorders, 19(1), 29–49. Hoffart, A. (2016). Cognitive models for panic disorder with agoraphobia: A study of disaggregated within-person effects. Journal of Consulting and Clinical Psychology, 84(9), 839. CBT for Panic Disorder Hoffart, A., Sexton, H., Hedley, L. M., & Martinsen, E. W. (2008). Mechanisms of change in cognitive therapy for panic disorder with agoraphobia. Journal of Behavior Therapy and Experimental Psychiatry, 39(3), 262–275. Houck, P. R., Spiegel, D. A., Shear, M. K., & Rucci, P. (2002). Reliability of the self-report version of the panic disorder severity scale. Depression and Anxiety, 15(4), 183–185. Huppert, J. D., Kivity, Y., Barlow, D. H., Gorman, J. M., Shear, M. K., & Woods, S. W. (2014). Therapist effects and the outcome–alliance correlation in cognitive behavioral therapy for panic disorder with agoraphobia. Behavior Research and Therapy, 52, 26–34. Kim, Y. W., Lee, S. H., Choi, T. K., Suh, S. Y., Kim, B., Kim, C. M., . . . & Song, S. K. (2009). Effectiveness of mindfulness-based cognitive therapy as an adjuvant to pharmacotherapy in patients with panic disorder or generalized anxiety disorder. Depression and Anxiety, 26(7), 601–606. King, M., Nazareth, I., Levy, G., Walker, C., Morris, R., Weich, S., . . . & Rifel, J. (2008). Prevalence of common mental disorders in general practice attendees across Europe. The British Journal of Psychiatry, 192(5), 362–367. Lewis-Fernández, R., Hinton, D. E., Laria, A. J., Patterson, E. H., Hofmann, S. G., Craske, M. G., . . . & Liao, B. (2011). Culture and the anxiety disorders: Recommendations for DSM-V. Focus, 9(3), 351–368. Livermore, N., Sharpe, L., & McKenzie, D. (2010). Panic attacks and panic disorder in chronic obstructive pulmonary disease: A cognitive behavioral perspective. Respiratory Medicine, 104(9), 1246–1253. NICE. (2011). Common Mental Health Disorders: Identification and Pathways to Care. Clinical Guideline 123. National Institute for Health and Care Excellence. Noyes, R., Reich, J., Clancy, J., & O’Gorman, T. W. (1986). Reduction in hypochondriasis with treatment of panic disorder. The British Journal of Psychiatry, 149(5), 631–635. Olatunji, B. O., Deacon, B. J., Abramowitz, J. S., & Valentiner, D. P. (2007). Body vigilance in nonclinical and anxiety disorder samples: Structure, correlates, and prediction of health concerns. Behavior Therapy, 38(4), 392–401. Pergamin-Hight, L., Naim, R., Bakermans-Kranenburg, M. J., van IJzendoorn, M. H., & BarHaim, Y. (2015). Content specificity of attention bias to threat in anxiety disorders: A meta-analysis. Clinical Psychology Review, 35, 10–18. Pompoli, A., Furukawa, T. A., Efthimiou, O., Imai, H., Tajika, A., & Salanti, G. (2018). Dismantling cognitive-behavior therapy for panic disorder: A systematic review and component network meta-analysis. Psychological Medicine, 48(12), 1945–1953. Pompoli, A., Furukawa, T. A., Imai, H., Tajika, A., Efthimiou, O., & Salanti, G. (2016). Psychological therapies for panic disorder with or without agoraphobia in adults: A network meta-analysis. Cochrane Database of Systematic Reviews, (4). Reinecke, A., Cooper, M., Favaron, E., Massey-Chase, R., & Harmer, C. (2011). Attentional bias in untreated panic disorder. Psychiatry Research, 185(3), 387–393. Reiss, S., & McNally, R. J. (1985). The expectancy model of fear. In S. Reiss & R. R. Bootzin (Eds.), Theoretical issues in behavior therapy (pp. 107–122). Academic Press. Salkovskis, P. M. (1991). The importance of behavior in the maintenance of anxiety and panic: A cognitive account. Behavioral and Cognitive Psychotherapy, 19(1), 6–19. Salkovskis, P. M., & Clark, D. M. (1993). Panic disorder and hypochondriasis. Advances in Behavior Research and Therapy, 15(1), 23–48. Salkovskis, P. M., Clark, D. M., & Gelder, M. G. (1996). Cognition-behavior links in the persistence of panic. Behavior Research and Therapy, 34(5–6), 453–458. Salkovskis, P. M., Clark, D. M., Hackmann, A., Wells, A., & Gelder, M. G. (1999). An experimental investigation of the role of safety-seeking behaviors in the maintenance of panic disorder with agoraphobia. Behavior Research and Therapy, 37(6), 559–574. 73 74 Robin D. Bailey Salkovskis, P. M., Hackmann, A., Wells, A., Gelder, M. G., & Clark, D. M. (2007). Belief disconfirmation versus habituation approaches to situational exposure in panic disorder with agoraphobia: A pilot study. Behavior Research and Therapy, 45(5), 877–885. Shear, M. K., Brown, T. A., Barlow, D. H., Money, R., Sholomskas, D. E., Woods, S. W., . . . & Papp, L. A. (1997). Multicenter collaborative panic disorder severity scale. American Journal of Psychiatry, 154(11), 1571–1575. Teachman, B. A., Marker, C. D., & Clerkin, E. M. (2010). Catastrophic misinterpretations as a predictor of symptom change during treatment for panic disorder. Journal of Consulting and Clinical Psychology, 78(6), 964. Tully, P. J., Sardinha, A., & Nardi, A. E. (2017). A new CBT model of panic attack treatment in comorbid heart diseases (PATCHD): How to calm an anxious heart and mind. Cognitive and Behavioral Practice, 24(3), 329–341. Vroom, V. H. (1964). Work and motivation. Wiley & Sons. Wells, A. (1997). Cognitive therapy of anxiety disorders: A practice manual and conceptual guide. John Wiley and Sons. Williams, P. G. (2004). The psychopathology of self-assessed health: A cognitive approach to health anxiety and hypochondriasis. Cognitive Therapy and Research, 28(5), 629–644. Wolpe, J., & Rowan, V. C. (1988). Panic disorder: A product of classical conditioning. Behavior Research and Therapy, 26(6), 441–450. Zickgraf, H. F., Chambless, D. L., McCarthy, K. S., Gallop, R., Sharpless, B. A., Milrod, B. L., & Barber, J. P. (2016). Interpersonal factors are associated with lower therapist adherence in cognitive-behavioral therapy for panic disorder. Clinical Psychology and Psychotherapy, 23(3), 272–284. 5 The Cognitive Behavioral Treatment of Agoraphobia Vijaya Manicavasagar and Derrick Silove Although many people may experience periods of anxiety and avoidance behaviors in response to situational stressors, only a minority develops agoraphobia, a chronic condition involving widespread avoidance of places such as shopping centres, bridges, tunnels, and crowds. Despite these lifestyle limitations, most people with agoraphobia seek treatment only when their symptoms become highly restrictive or they become overly dependent on others to pursue everyday activities (Greenberg et al., 1999; Lepine, 2003). The development of agoraphobia often reflects a downward spiral characterized by a ‘fear of fear’, in which the anticipation of anxiety leads to increasing avoidance behaviors and vice versa, creating a vicious circle. The key concern amongst people with agoraphobia is a fear that they will develop severe physical symptoms in certain situations where escape or obtaining help from others is impossible. In some instances, the presence of a trusted companion can contain or lessen their fears (American Psychiatric Association, 2013 [DSM-5]). In order to receive a full DSM-5 diagnosis of agoraphobia, a person must experience significant psychosocial distress or disability related to their symptoms and the problem must persist for at least six months. Once entrenched, agoraphobia is associated with diminished quality of life and increased use of healthcare services. These core features distinguish agoraphobia from the other anxiety disorders that share superficial similarities. For example, in separation anxiety disorder, core fears revolve around being separated from or harm befalling key attachment figures, or being away from places of security such as the home (Bowlby, 1973); in social phobia, feelings of embarrassment and negative appraisal by others leads to avoidance of social interactions; and in obsessive-compulsive disorder, fears of contamination or contagion may lead to avoidance of public places. In posttraumatic stress disorder, people avoid places which remind them of their original trauma and/or which trigger traumatic memories (flashbacks). People experiencing severe depression may avoid leaving home because they feel hopeless or lack motivation and the energy to do so; and persons with psychotic illnesses may be fear persecution or harm by others when venturing away from the house. 75 76 Vijaya Manicavasagar and Derrick Silove Historical Context The term ‘agoraphobia’, first coined by Westphal in the 1870s (Kuch & Swinson, 1992), was applied to people who experienced unexpected and situation-specific panic attacks in public places, empty streets, bridges, and crowds. They typically experienced anticipatory anxiety (‘fear of fear’) and sudden physical incapacitation (such as gastrointestinal upset, dizziness, and difficulty breathing) in these situations (Kuch & Swinson, 1992). In the 1970s, the focus turned to panic disorder which then was regarded as the primary cause of agoraphobic symptoms, a model reflected in the third edition of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 1980) (Barlow, 2002). Since then, debate has persisted regarding the relationship of the two disorders. In DSM-5 (American Psychiatric Association, 2013) and the eleventh edition of the International Classification of Diseases (ICD-11; World Health Organization, 2018), agoraphobia and panic disorder are classified as separate categories. Nevertheless, in clinical practice, it is common to trace the onset of avoidant symptoms of agoraphobia to pre-existing fear of experiencing panic attacks or at least panic-like symptoms when approaching or entering the relevant locations. Prevalence The aforementioned serial changes in the classification of agoraphobia and its association with panic disorder has contributed to the variability in prevalence rates identified for the two disorders over time. Population studies prior to DSM-5 suggested that a third of people with panic disorder develop agoraphobia, whereas agoraphobia without a history of panic attacks appeared to be relatively uncommon (Sanchez-Meca et al., 2010). For example, a national epidemiological study in the United States (Kessler et al., 2006) found a lifetime prevalence for panic disorder with agoraphobia of 1.1%, whereas only 0.5% of participants reported agoraphobia alone (Robins & Regier, 1991). The peak age of expression of agoraphobia is between 20 and 30 years; woman make up three quarters of cases (Yonkers et al., 1998) and also tend to develop more severe forms of the disorder (Turgeon et al., 1998). Relatives of persons with agoraphobia are more likely to develop the disorder (Crowe et al., 1983), a pattern not seen in panic disorder alone (Rapee & Murrell, 1988). Causes and Pathways Most people with agoraphobia who seek treatment can recall a clear point of onset of anxiety (Aronson & Logue, 1987). At first, symptoms are commonly misinterpreted as indicating serious physical illness, generating further anxiety (Clark, 1986), a spiral that contributes to avoidance of situations in which symptoms occur. Cognitive Behavioral Treatment of Agoraphobia Cognitive Distortions Cognitive processes, or the way people think about and interpret events, can play a key role in the maintenance of agoraphobia. In particular, the belief about the meaning and implication of symptoms may be instrumental in generating anticipatory anxiety and avoidance. Extreme or catastrophic cognitions, such as a conviction that the person will die, go mad, soil themselves, vomit, faint, or collapse if they enter a certain place, can exacerbate symptoms. An important cognition that adds to the spiral of avoidance is that the person will not be able to control themself, resulting in chaotic or embarrassing behavior (Cox et al., 1995; Craske & Barlow, 1988; Craske et al., 1988; Telch et al., 1989). Evidence from experimental studies suggests that cognitive distortions are more common amongst persons with agoraphobia; for example, persons with the disorder are more likely to interpret ambiguous physical sensations and novel situations as threatening and anxiety-provoking than those who do not experience anxiety (McNally & Foa; 1987). In summary, the types of cognitions that maintain agoraphobia include the following: Expecting negative outcomes if the person approaches or enters a particular situation, including fear of becoming overwhelmingly distressed, experiencing a catastrophic illness, or acting in an embarrassing way Fear of uncontrollable anxiety symptoms, leading to collapse or madness A conviction that the person will not be able to manage or cope with anxiety, often associated with characteristics such as low self-confidence, poor coping strategies, and an impaired sense of self-efficacy. Conditioning to Situational Cues Classical conditioning, in which repetitive exposure to environmental stimuli becomes paired with adverse experiences such as anxiety, can lead to associative learning. The consequence is that returning to the same or a similar situation can provoke a fear reaction, even if there is no objective danger in that location. For example, an individual who experienced severe anxiety symptoms at work in response to a situational stress (e.g., an altercation with a manager) may develop a conditioned learnt response in which neutral cues, such as the journey to work or the physical workplace itself, trigger anxiety and avoidance. Clinical Assessment and Tools When assessing a person with suspected agoraphobia, it is important to obtain precise information about the core symptoms including timing of onset, progression, and the pattern of fear, anxiety, and avoidance as it evolved over time. Differentiating agoraphobic from other forms of avoidance observed in other anxiety subtypes is essential to making an accurate diagnosis. A detailed account 77 78 Vijaya Manicavasagar and Derrick Silove should be elicited of factors that contribute to the onset and perpetuation of the symptoms, including life stressors at work, home, and the wider environment. The developmental history should also include inquiry into the style of parenting experienced in childhood, including evidence of overprotectiveness or neglect. Sensitive inquiry should also be made into past experiences of trauma and abuse. A detailed, chronological history of how avoidance behaviors developed, unfolded, and fluctuated, and how they relate to situational cues and life stressors, may provide useful insights into what approaches and possible lifestyle modifications may be worth pursuing to change the associated maladaptive responses and behaviors. Assessment of the impact of avoidance is made in relation to all aspects of the person’s life, that is, in the personal, social, work, study, and leisure domains. Physical symptoms of anxiety need to be differentiated from those of organic disorders which may be independent of or contribute to anxiety. Special attention should be given to conditions known to cause or mimic anxiety, such as thyroid or other endocrine diseases, cardiac arrhythmias or other heart conditions (such as mitral valve disease), and drug withdrawal syndromes. A history of alcohol and drug use (both prescribed and non-prescribed) is important to determine whether these substances may be contributing to anxiety and/or providing relief to the person. Up to a third of men and one in 10 women with agoraphobia misuse drugs or alcohol (Markowitz et al., 1989). These substances and the complications from their use can be a factor in the causal pathway to agoraphobia or represent an attempt at ‘selfmedication’, that is, to reduce anxiety. Invariably, the early transient anxietyreducing effect is lost, and, instead, escalating use of the drug or alcohol exacerbates or complicates avoidant tendencies. Comorbidity needs to be assessed, in relation to both past and concurrent disorders. Agoraphobia commonly is comorbid with a range of other anxiety or depressive disorders and, as indicated, with drug and alcohol misuse. If possible, causal links should be identified amongst comorbid disorders, that is, which disorder appears to have preceded and triggered the other, and identification of the disorder that is dominant at the time of assessment. Psychiatric complications, such as the onset of depressive symptoms or disorder and especially suicidal feelings/urges, require close attention and may demand urgent intervention. Assessing personality characteristics is important, including features of perfectionism, dependency, or borderline behaviors, given that these traits are likely to play a role in determining the prognosis and in the capacity of the person to engage in and adhere to treatment. When a high level of diagnostic reliability and validity is required, such as in epidemiological studies and clinical trials, structured diagnostic interviews may be used. The Structured Clinical Interview for DSM-5 (SCID-5; First et al., 2015) is one of the most commonly used comprehensive assessment tools. Self-report measures may also be used as an adjunct to the clinical interview or to gauge varying levels of agoraphobic avoidance and the frequency and intensity of physical symptoms and dysfunctional negative thoughts. Some of the more frequently used measures that are specific to the assessment of agoraphobia are listed as follows: Cognitive Behavioral Treatment of Agoraphobia Agoraphobic Cognitions Questionnaire (ACQ) (Chambless et al., 1984) comprises 14 items (plus an open question) rated on a five-point Likert-type scale measuring the frequency of catastrophic thoughts. Body Sensations Questionnaire (BSQ) (Chambless et al., 1984) has 18 items rated on a five-point Likert-type scale measuring fear of physical sensations. Mobility Inventory for Agoraphobia (MIA) (Chambless et al., 1985) is a 27-item scale which includes two agoraphobic avoidance scales measuring the severity of phobic avoidance and the frequency of panic attacks depending on whether the participant is alone (MIA-Alone) or accompanied (MIA-Accompanied). Other measures that are frequently used tend to focus on panic attacks and include the Panic Agoraphobia Scale (PAS; Bandelow, 1997) and the Anxiety Sensitivity Index (ASI; Reiss, et al., 1986). The Panic and Agoraphobia Scale (P&A; Bandelow, 1995) is a short clinician- or client-rated scale that covers panic frequency, severity, and duration; panic-related phobias; anticipatory anxiety; impairment and general quality of life; and global problem severity. A similar measure is the clinician-scored diary the Panic-Associated Symptoms Scale (PASS; Scupi et al., 1992). Evidence-Based Treatments for Agoraphobia Cognitive behavioral therapy (CBT) is the mainstay of therapy for agoraphobia. This approach generally offers lower treatment costs and greater access than other treatment modalities. An extensive body of research has shown that CBT, whether individually delivered or group-based, is generally effective in treating agoraphobia (Barlow et al., 2000; Hahlweg et al., 2001). In summary, CBT interventions typically include a package of inter-related components, including psychoeducation, normalizing symptoms and experiences of anxiety, cognitive restructuring, slow breathing exercises, strategies to reduce general physical symptoms of anxiety, exposure to interoceptive stimuli (e.g., rapid heart rate or sweating), and gradual in vivo exposure to avoided situations. Ultimately, CBT aims to encourage people with agoraphobia to utilize more adaptive thought patterns and behaviors (Craske et al., 2008) as the foundation for recovery. Psychoeducation Understanding the nature of agoraphobia and the pathways leading to and maintaining the problem helps the person to gain a sense of mastery in coping with the disorder. Psychoeducation about the physical manifestations of anxiety can help to alleviate unrealistic and catastrophic fears while helping the person with anxiety to understand the specific triggers and stressors that contribute to anxiety and avoidance behaviors. This assists in anticipating and using pre-emptive strategies to 79 80 Vijaya Manicavasagar and Derrick Silove manage stressful situations (Craske & Barlow, 1988; Goldstein & Chambless, 1978; Zarate et al., 1990). Cognitive Therapy Cognitive therapy helps people to address dysfunctional thoughts that lead to or exacerbate symptoms, giving them confidence in their ability to cope with panic and anxiety symptoms and to curb negative thoughts about themselves regarding their capacity to overcome lifestyle restrictions and to reduce their dependence on others. Thought challenging and cognitive restructuring can be used at various points in therapy, for example, to re-appraise thoughts around anticipatory anxiety and resistance to engage in exposure, and to address any negative thoughts regarding their performance and progress in therapy. Addressing Arousal A key focus of treatment is to reduce high levels of autonomic arousal and acute anxiety symptoms. Commonly used methods include hyperventilation control, meditation or mindfulness, and relaxation exercises. These techniques relieve symptoms and facilitate the implementation of the exposure hierarchy by providing a method to achieve de-arousal which can be used in vivo. Exposure Therapy Graded exposure to feared situations is a key component of CBT for agoraphobia (Mattick et al., 1990; Teusch and Boehme, 1999). Exposure therapy is grounded on the principles of habituation and extinction of learned fear responses. The assumption is that intrinsically non-harmful situations or places cannot continue to evoke fear or anxiety if the person is repeatedly exposed to these conditions without any adverse consequences. A hierarchy of situations is developed with the person in which feared or avoided situations are ranked according to the severity of the anxiety they provoke. It can be useful to apply a simple numerical rating scale to identify the order of the hierarchy (e.g., on a visual analogue scale ranging from 0 to 10). Additional questions that can guide anxiety ratings may include ‘What would make this worse?’ and ‘What would make this better?’ The person then is guided through a systematic program aimed at reducing anxiety and avoidance in a progressive manner by graduated and repeated exposure to the designated places or conditions listed in the hierarchy, starting with the least anxiety-provoking items and moving serially up to the most severe. Remaining in the feared situation long enough for the fear response to dissipate is important to reverse conditioning. Ideally, the person should be there long enough for the anxiety rating to reduce by at least 2 or 3 points during exposure exercises, a process which may take 20–30 minutes to achieve. If in vivo exposure is not possible or can be undertaken only infrequently, then exposure in imagination can be used Cognitive Behavioral Treatment of Agoraphobia (imaginal exposure) as a first step. Therapist-guided in vivo exposure, where the professional initially accompanies the patient to coach and guide them through specific situations (Gloster et al., 2011), remains a mainstay of therapy. In some situations, a trusted companion can substitute for the therapist, but it is important to gauge whether this strategy may increase dependency and how and when the companion should withdraw from the process to ensure that the person becomes autonomous in confronting the feared situation. Increasingly, virtual reality–based treatments can be used, which are time-efficient and safe and allow direct monitoring of physiological arousal (Botella et al., 2004). Throughout the process, the challenge for the person and the therapist is to overcome in a sustained manner the initial discomfort incurred by confronting the feared situation(s) on the hierarchy. The participant needs to be prepared for possible setbacks and periods in which the task feels overwhelming to avoid feeling discouraged and giving up by retreating to safe but maladaptive behaviors such as finding reasons to stay at home or insisting on having a companion accompany them on outings. These forms of resistance should be anticipated, discussed, and monitored from the outset to avoid treatment failure or dropout. Other Strategies Initially, the use of safety behaviors can facilitate the first stages of exposure, for example, resorting to sipping water, carrying anxiolytic medication in a bag, or talking to a friend on a mobile phone. Later in therapy, these behaviors should be discussed and gradually withdrawn once the person’s confidence in managing anxiety has consolidated. Otherwise, improvements in mobility may be transitory. Engaging in structured problem-solving to address specific impediments to pursuing the exposure program and goal-setting to help maintain motivation to work through the hierarchy can be used throughout the treatment process. Homework tasks include practicing in vivo exposure and thought-challenging. Again, engaging family members or friends in the process can facilitate motivation and progress as long as clear instructions are given to these persons concerning the extent and limitations of assistance that should be provided. Evidence In combination, cognitive therapy (Fava et al., 2001; Gloster et al., 2011) and exposure (Barlow et al., 1984; Hahlweg et al., 2001; Michelson et al., 1985) appear to achieve the best outcomes for agoraphobia (Mattick et al., 1990; Michelson et al., 1985). The prognosis is less favourable if there is a pattern of comorbidity with other common mental disorders related to depression, anxiety, and substance use; where traits of personality disorder are evident and interfere with regular practicing of skills; and/or where there are social or environmental barriers to focusing on therapy, for example, in the presence of an unsupportive partner or family (Gloster et al., 2015). 81 82 Vijaya Manicavasagar and Derrick Silove In general, although most persons with agoraphobia respond positively to CBT, a quarter gain only limited symptom relief (McPherson et al., 1980; Munby & Johnston, 1980). For these people, other treatment approaches may be worth trying, including acceptance and commitment therapy (Gloster et al., 2015) or psychodynamic approaches (Keefe et al., 2014) that address the factors that impede motivation or generate resistance to engaging in CBT. At the same time, chronic, treatment-resistant cases encountered in clinical practice usually involve persons with long-term entrenched symptoms and a combination of the poor prognostic factors listed above. Medications Used to Manage Agoraphobia Anxiety-reducing medications (tranquilizers) such as the benzodiazepines (diazepam, alprazolam) can help to reduce both state anxiety and anticipatory anxiety and are frequently used in the treatment of agoraphobia. Some patients find that simply having a tablet of diazepam in their bag helps them to have the confidence to go out. Others take a benzodiazepine strategically, that is, just as they are anticipating leaving the house. Problems of addiction, tolerance, and withdrawal symptoms caution against using these medications for prolonged periods of time. Their use should be restricted to the short term where the person’s anxiety or distress is so overwhelming that they cannot engage in psychological interventions, or, for patients with no risk of addiction, on an occasional basis (not more than twice a week) for insomnia or to deal with specific anxiety-provoking situations. The main classes of drugs used (loosely referred to as antidepressants) are the selective serotonin reuptake inhibitors (SSRIs) such as sertraline, paroxetine, and fluoxetine, or serotonin and noradrenalin (also known as norepinephrine) reuptake inhibitors (SNRIs) such as mirtazapine, venlafaxine, and duloxetine, especially where depression is a comorbid feature. In situations where there is a restriction on availability of psychotropic medications, first-generation tricyclic medications (doxepin, imipramine, nortriptyline) and, less commonly, the monoamine oxidase inhibitors, such as phenelzine, can be used. Or these latter classes of drugs may be trialled in treatment-resistant cases. Although CBT and medication offer similar short-term outcomes, the former appears to result in longer-term maintenance of gains, whereas discontinuation of medication is often associated with higher relapse rates (Fava et al., 2001; Gould et al., 1995). Although various chemical augmentation methods have been trialled to improve the treatment response to CBT techniques, particularly exposure therapy, there is little evidence as yet that these approaches are useful for agoraphobia. Concerns have been raised that the use of psychotropic medications may impede learning when CBT methods are used, but so far the evidence remains slender (Basoglu et al., 1994). Clinical judgement therefore needs to be applied in deciding whether or not to prescribe medication on an individual basis, taking into account the severity of the problem, the capacity of the person to engage in CBT given their level of anxiety, the preferences of the patient, and the risk of adverse effects. Cognitive Behavioral Treatment of Agoraphobia Case Vignette ND was a 46-year-old married woman employed in a government service but currently on leave following a workplace incident in the year prior to seeking treatment. She had consulted a psychiatrist and a counsellor in the previous four months. ND had lost confidence in herself and in her abilities, had experienced repeated panic attacks, and, increasingly, agoraphobic avoidance. She was developing a pattern of avoiding driving, shopping, and even walking to the front gate to collect her mail. ND had been married for almost 20 years and had three adult sons who lived elsewhere but whom she saw on a weekly basis. She was also involved in the care of her elderly mother. She had been treated for cancer on two separate occasions several years prior to the work incident and had made a full recovery. Her agoraphobic avoidance had increased her reliance on her husband to take her to appointments and to go shopping. ND’s husband worked long hours involving variable timing of shifts which made it difficult to plan ahead, leading to arguments and considerable strain in their previously stable marriage. Although there was no previous history of formal psychiatric disorder, it became evident that ND had an obsessional personality style manifesting in controlling behaviours (such as keeping track of her husband’s whereabouts and closely monitoring her adult sons’ activities). Associated features were intolerance of uncertainty and unrealistic expectations of herself and others to behave in a what she considered to be a ‘highly moral’ way at all times. Nevertheless, prior to the development of her anxiety, ND was a highly independent woman holding a responsible job. Outline of ND’s Treatment Phase 1: Setting the Stage for Change After a clinical history was obtained, the next step was to examine and address the interpersonal factors that could be contributing to her anxiety and avoidance behaviors, such as uncertainty regarding her husband’s availability. Attention was given to planning and regularizing activities requiring her husband’s help such as shopping and keeping appointments with medical specialists. Other issues related to her concerns about her diet, lack of exercise, and interpersonal difficulties. Some of these could be addressed with simple problem-solving and encouraging ND to discuss these issues with her husband. ND’s pride in maintaining a healthy organic diet for herself and her family was also a source of tension given that shopping for these specialized groceries required her husband to accompany her. ND was reasonably fit and healthy prior to the development of her agoraphobia but had reduced her level of exercise because she could not drive to the gym or go for walks. She had also developed high blood pressure, headaches, and severe muscle tension in her neck. Her sleep was poor and she found herself unable to relax even 83 84 Vijaya Manicavasagar and Derrick Silove while at home when her husband was at work. Her other stresses mainly involved looking after her elderly mother and providing emotional support to her sons, who were both in the process of changing jobs. Although she had some close friends with whom she met on a regular basis prior to the development of her agoraphobia, ND had stopped calling them and declined invitations to meet up with them. Problem solving was used to assess and, where possible, resolve or lessen these obstacles and problems with the aim of allowing ND to return to a more fulfilling and satisfying life. During this phase, ND was instructed in some basic anxiety management skills, including progressive muscle relaxation, mindfulness meditation, and slow breathing. Moreover, the process of challenging her extreme cognitions was commenced, particularly her critical appraisal of herself as a failure because she could not leave the house. ND was guided in recording a hierarchy of anxiety-provoking situations, using the 0–10 rating system. She found this task helpful as it organized her experiences of anxiety and assisted in compartmentalizing the steps involved in addressing them in sequence. Her list of anxiety-provoking situations was further refined by discussing actions that increased or decreased the fear ratings, that is, the strategies she could use to minimize anxiety prior to or on entering these situations. ND also was encouraged to document the negative thoughts she experienced that were associated with those anxiety-provoking situations. In addition to her selfcritical thoughts, she became frustrated with the time it was taking to recover, challenging herself as to why she could not simply exert control over her anxiety. She was encouraged to examine how these cognitive-driven frustrations actually hampered the process of therapy, thereby reinforcing a vicious cycle of maintenance of symptoms. Suggestions were offered to substitute rigidly negative thoughts with more helpful and realistic appraisals of her progress in therapy. Once ND had learned some anxiety management skills such as slow breathing, she was encouraged to increase her exercise again given that physical activity in itself could contribute to improving her mental health. ND was at first hesitant to engage in activities that would lead to a perceptible increase in her heart rate or shortness of breath. She came to recognize the contextual differences in her bodily responses to physical activity as compared with the physiological arousal related to acute anxiety, allowing her to resume practicing yoga at home. Phase 2: Implementing Cognitive and Behavioral Techniques In phase 2, when ND had completed planning her program of exposure and had gained skills in cognitive restructuring, she commenced the task of confronting the problem of shopping (rated around 5 or 6). She practiced exposure in imagination while controlling her level of arousal with a slow-breathing exercise. The scene was repeated up to three times in each session and ND was instructed to remain in the imagined situation for as long as it took for her anxiety ratings to decrease. After each imaginal exposure session, ND was encouraged to discuss the effectiveness of Cognitive Behavioral Treatment of Agoraphobia the exercise in controlling her anxiety, any unhelpful thoughts that occurred during the exposure session, and her anxiety rating during the process. Once she achieved a reasonable level of confidence, she began to practice exposure in vivo, her husband being briefed to provide the necessary support by being physically present in the first stages. ND was encouraged to practice this scenario as many times as possible between therapy sessions and to report back to her therapist on the processes and outcomes of that activity. Phase 3: Working through the Exposure Hierarchy Subsequent sessions focused on each of the items in the hierarchy, in imagination during the session if necessary, then in vivo. Subjective ratings of anxiety were obtained pre- and post-activity in order to monitor progress, ensure motivation was maintained, and offer enough time to troubleshoot problem areas. In phase 3, with practice, ND was eventually able to drive short distances on her own to the gym and to appointments for herself or her mother. She rated her anxiety before and after these events, noting the anxiety management techniques that worked best for her in each situation. Over a period of time, the frequency of her therapy sessions was reduced as ND increasingly worked on overcoming her anxieties on her own. Her therapy sessions began to focus on troubleshooting situations that remained problematic for her. During this time the tensions in her relationship with her husband lessened as her ability to drive short distances resulted in fewer arguments about his availability. Over a period of 18 months, ND began to regain a sense of control over her life and engage in activities that she had been avoiding. She began exercising regularly and joined several group programmes, both recreational and therapeutic. Her husband’s involvement in her treatment programme was tapering off. Her therapy sessions focussed on supporting her positive change in self-image as an increasingly independent and confident person. However, ND’s perfectionistic character traits continued to limit her progress and affect other areas of her life, such as her frustration over her mother’s increasing frailty, intolerance over her friends’ perceived unreliability in attending social engagements, and her compulsive need to source specific types of foodstuffs despite the difficulties in obtaining them far from her home and thus having to rely on her husband to drive her. Comments about This Model for Treatment In vivo exposure during treatment should resemble the real situations avoided by individuals as much as possible. Furthermore, patients need to be guided to confront these situations as frequently and as long as possible until the anxiety subsides. Partners and other family members may be initially included in the exposure-based program, but their involvement should be gradually tapered off if the patient is to become more independent. 85 86 Vijaya Manicavasagar and Derrick Silove After working through several items on the exposure hierarchy, some patients may become ‘stuck’ and reach a point where they believe that they cannot proceed because the next item on the list seems too difficult. If this happens, exploration of the reasons for the resistance together with reversion to imaginal exposure may be required. In some cases, specific difficulties associated with that particular situation may need to be re-analyzed and addressed before attempting in vivo exposure. Exposure to feared situations can bring about positive cognitive changes, and these changes should be discussed during therapy sessions as they can facilitate further improvements in avoidance behaviors and serve as a reminder to patients when they become ‘stuck’ again. The presence of the therapist during the early stages of in vivo exposure may assist in initiating change when there is hesitation to do so. The therapist can alert patients to the use of positive rather than maladaptive ‘safety signals’ and ‘safety behaviors’ in real time while the provision of immediate feedback through modelling and verbal guidance can assist patients through challenging situations. Whilst some (see Bandura, 1977) have cautioned against the use of safety behaviors, it may be prudent to allow this practice early in the treatment program rather than to risk discontinuation. However, the excessive presence of the therapist as a safety signal for the patient ultimately can inhibit progress, so that timely withdrawal by the therapist allowing the patient to attempt the same situations on their own is vital. Facilitators of Therapy Progress during therapy can be affected by several factors, including the extent to which a person is willing to confront their anxiety during treatment (Perreault et al., 2014). Other issues include patient expectations (whether realistic or not) about the procedures, technique, format, and duration of treatment, as well as a commitment to make a sustained effort. These issues can be related to personality characteristics and the strength of family and social supports (Constantino, 2012). Patients also may have idiosyncratic expectations about their prognosis (either excessively optimistic or pessimistic) and the overall degree and speed of recovery (Constantino, 2012). These issues were discussed with ND prior to the commencement of treatment and were revisited throughout the program. Flexibility in the choice and timing of each intervention depends on the overall formulation of the patient’s clinical presentation, capacities, and supports (familial, environmental). If applied rigidly, manualized treatments, although popular, may overlook individual differences in patient characteristics, which may complicate treatment. However, if they are used with discretion, manuals can provide general guidance and practical information for patients and clinicians alike. Apart from general therapist factors, such as empathy and warmth, therapists treating agoraphobia need to be skilled and experienced in CBT and familiar with the medications used to treat both anxiety and depressive disorders, given the high levels of comorbidity between these two disorders. The therapist must have a capacity to assess and, if necessary, refer for other mental health problems (such Cognitive Behavioral Treatment of Agoraphobia as drug and alcohol misuse), social assistance, and medical assessment and intervention where necessary. Where treatment outcomes are unsatisfactory, consideration should be given to referral to therapists using other approaches (Barlow et al., 2000). For example, Gloster et al. (2015) have reported success in using acceptance and commitment therapy (ACT) in the treatment of agoraphobia with treatmentresistant patients. Engaging other health professionals, such as physiotherapists, dietitians, and general practitioners, as part of a multidisciplinary team may also help to facilitate change especially where physical and social factors may be impacting on the illness course. Inhibitors to Recovery Inhibitors to recovery should be addressed explicitly during assessment, in the collaborative development of a management plan, and in the initial stages of treatment. Although partners and family members can play a vital role in facilitating recovery, they may also constrain progress during the therapy process. For example, families may be critical of the patient for not being able to overcome their avoidance behaviors within a short time frame. In other situations, families may collude inadvertently with the person in justifying or compensating for avoidant behaviors. For example, the network of dependency that occurs when one member of the household experiences agoraphobia may lead to changes in family dynamics. Where these factors are present, it is essential to hold special sessions with partners and other family members (if the patient agrees) in order to ensure a shared understanding of the disorder, the type of family support needed to facilitate the treatment plan, and the expected pace of progress (Cerny et al., 1987). Gently but consistently confronting a sick-role attitude is vital to ensure that the person is motivated to recover. This involves acknowledging the gravity of agoraphobia and the genuine difficulties in overcoming avoidance but, at the same time, reinforcing the principle that recovery is possible as long as there is a sustained and concerted effort from all contributors (the person with agoraphobia, their family, and the therapist) in working in the same direction. It may also be important to discuss the gains and ‘losses’ relating to recovery with the person and their support network, in order to ensure that the losses, such as the sick role, are worth giving up for the gains, such as a greater sense of independence. A further complexity arises from multiple treatment providers and/or insurers involved in situations where patients experience chronic anxiety problems, especially when compensation for work-related stressors is involved. Various professionals may inadvertently contradict each other, and adversarial medico-legal issues (e.g., compensation-seeking) can retard recovery. Post-therapy Complications Agoraphobia often needs prolonged treatment, commencing with more intensive and frequent sessions at the outset but tapering off to infrequent visits over several 87 88 Vijaya Manicavasagar and Derrick Silove years. An attachment may form between patients and their therapists fostering dependency, which is clearly problematic given that the aim of therapy is to encourage independence and self-confidence. This issue can be addressed by estimating the ‘blocks’ of sessions that may be required at each phase of treatment, regularly reviewing progress, issuing a mutually agreed-upon treatment completion date, and anticipating the changes that the person will experience once therapy is concluded. As with people experiencing any long-term anxiety disorder, those with agoraphobia often develop other forms of emotional problems in their lives. For example, a study has reported that people with agoraphobia frequently develop depression following improvements in their anxiety symptoms and avoidance behaviors, possibly because they become more aware of the psychosocial costs incurred as a consequence of their previous level of disability (Gloster et al., 2011). Furthermore, their relationships with the people around them may change and, if not adequately managed, may result in increased interpersonal stress. Dropout from Treatment Treatment attrition rates for agoraphobia range from 10% to 55% (Issakidis & Andrews, 2004; White et al., 2010). Contributing factors include symptom severity at outset and the presence of comorbidities such as depressive illness (Issakidis & Andrews, 2004; White et al., 2010), sociodemographic variables such as lower household income and education (Swift & Greenberg, 2012), negative attitudes to past or ongoing treatment (Perreault et al., 2014), and difficulties in intimate relationships (El-Baalbaki et al., 2010; Marcaurelle et al., 2005). Remedial factors that need to be assessed if there appears to be a risk of dropout include the patient’s lack of understanding of the nature, procedure, and intended duration of the treatment program, especially feelings of being overwhelmed by the pace of treatment; motivational factors which may be reflected in the personality of the patient; and factors within the family and social environment that inhibit recovery or maintain avoidant behaviors. Maintenance and Relapse Prevention Relapse (i.e., return of fear and avoidance) after successful situational exposure is usually related to the recurrence of anxiety symptoms (Arnow et al., 1985). Booster sessions can be especially helpful to prevent full relapse, especially if they are scheduled as soon as early warning signs are detected (such as increasing feelings of tension or hesitancy in approaching situations after regaining the capacity to do so). If possible, booster sessions can be tentatively scheduled during the course of therapy. The availability of these sessions can be very reassuring to patients and can always be cancelled if they are not required. Cognitive Behavioral Treatment of Agoraphobia Future Developments in Agoraphobia Treatments There are several online programs and apps, based on manualized CBT principles, to assist the recovery of people with agoraphobia. These may be useful for mild to moderate levels of avoidance. It is likely, however, that people who have more severe or complex presentations will still require face-to-face therapist contact and intervention. Virtual reality platforms may replicate real-life situations more effectively than imagination, and these technologies may become affordable in office practice. Finally, neurobiological assessments may assist in predicting individual responsiveness to therapies such as CBT, but, as yet, they depend on specialist investigations such as advanced brain imaging which are costly and may carry risk. Significant numbers of patients continue to suffer from agoraphobia following treatment. Further investigation needs to be given to the use of second and third wave therapies for people who do not respond to CBT alone. Training of therapists to diagnose and treat is also a critical feature, as the more accurate the initial assessment, the greater the likelihood that treatment can be tailored to suit individual patient needs. REFERENCES American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders (3rd ed.). American Psychiatric Publishing. (2013). Diagnostic and statistical manual of mental disorders (5th ed.) (DSM-5). American Psychiatric Publishing. Arnow, D. A., Taylor, C. B., Agras, W. S., & Telch, M. I. (1985). Enhancing agoraphobia treatment outcome by changing couple communication patterns. Behavior Therapy, 16, 452–467. Aronson, T. A., & Logue, C. M. (1987). On the longitudinal course of panic disorder: Development history and predictors of phobic complications. Comprehensive Psychiatry, 28, 344–355. Bandelow, B. (1995). Assessing the efficacy of treatments for panic disorder and agoraphobia: II. The Panic and Agoraphobia Scale. International Clinical Psychopharmacology, 10, 73–81. (1997). Panic and Agoraphobia Scale (PAS). Hogrefe & Huber. Bandura, A. (1977). Self efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84, 191–205. Barlow, D. H. (2002). Anxiety and its disorders: The nature and treatment of anxiety and panic. Guilford Press. Barlow, D. H., O’Brien, G. T., & Last C. G. (1984). Couples treatment of agoraphobia. Behavior Therapy, 15, 41–58. Barlow, D. H., Gorman, J. M., Shear, M. K., & Woods, S. W. (2000). Cognitive behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. Journal of the American Medical Association, 283, 2529–2536. Basoglu, M., Marks, I. M., Kilic, C., Brewin, C. R., & Swinson, R. P. (1994). Alprazolam and exposure for panic disorder with agoraphobia attribution of improvement to medication predicts subsequent relapse. British Journal of Psychiatry, 164, 652–659. 89 90 Vijaya Manicavasagar and Derrick Silove Botella, C., Villa, H., Garcia Palacios, A., Quero, S., Banos, R. M., & Alcaniz, M. (2004). The use of VR in the treatment of panic disorders and agoraphobia. Studies in Health Technology and Informatics, 99, 73–90. Bowlby, J. (1973). Attachment and loss, vol. 2: Separation: Anxiety and anger. Penguin Books. Cerny, J. A., Barlow, D. H., Craske, M. G., & Himadi, W. G. (1987). Couples treatment of agoraphobia: A two-year follow-up. Behavior Therapy, 18, 401–415. Chambless, D. L., Caputo, G. C., Bright, P., & Gallagher, R. (1984). Assessment of fear in agoraphobics: The Body Sensations Questionnaire and the Agoraphobic Cognitions Questionnaire. Journal of Consulting and Clinical Psychology, 52, 1090–1097. Chambless, D. L., Caputo, G. C., Jasin, S. E., Gracely, E. J., & Williams, C. (1985). The Mobility Inventory for Agoraphobia. Behaviour Research and Therapy, 23, 35–44. Clark, D. M. (1986). A cognitive approach to panic. Behaviour Research and Therapy, 24, 461–470. Constantino, M. J. (2012). Believing is seeing: An evolving research program on patients’ psychotherapy expectations. Psychotherapy Research, 22, 127–138. Cox, B. J., Endler, N. S., & Swinson, R. P. (1995). An examination of levels of agoraphobic severity in panic disorder. Behaviour Research and Therapy, 33, 57–62. Craske, M. G., & Barlow, D. H. (1988). A review of the relationship between panic and avoidance. Clinical Psychology Review, 8, 667–685. Craske, M. G., Kircanski, K., Zelikowsky, M., Mystkowski, J., Chowdhury, N., & Baker, A. (2008). Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy, 46(1), 5–27. Craske, M. G., Rapee, R. M., & Barlow, D. H. (1988). The significance of panic-expectancy for individual patterns of avoidance. Behavior Therapy, 19, 577–592. Crowe, R. R., Noyes, R., Pauls, D. L., & Sylmen, D. (1983). A family study of panic disorder. Archives of General Psychiatry, 40, 1065–1069. El-Baalbaki, G., Bélanger, C., Perreault, M., Fredman, S. J., & Baucom, D. (2010). Marital interactions in predicting treatment outcome in panic disorder with agoraphobia. International Journal of Humanities and Social Science, 5, 671–681. Fava, G. A., Rafanelli, C., Grandi, S., Conti, S., Ruini, C., Mangelli, L., & Belluardo, P. (2001). Long-term outcome of panic disorder with agoraphobia treated by exposure. Psychological Medicine, 31, 891–898. First, M. B., Williams, J. B. W., Karg, R. S., & Spitzer, R. L. (2015). Structured Clinical Interview for DSM-5 Disorders, Clinician Version (SCID-5-CV). American Psychiatric Association. Gloster, A. T., Sonntag, R., Hoyer, J., Meyer, A. H., Heinze, S., Strohle, A., Eifert. G., & Wittchen, H.-U. (2015). Treating treatment-resistant patients with panic disorder and agoraphobia using psychotherapy: A randomized controlled switching trial. Psychotherapy and Psychosomatics, 84, 100–109. Gloster, A. T., Wittchen, H.-U., Einsle, F., Helbig-Lang, S., Hamm, A. O., Richter, J., Gerlach, A. L., Kircher, T., Zwanzger, P., Lang, T., Fydrich, T., Fehm, L., Alpers, G. W., Ströhle, A., Deckert, J., Höfler, M., & Arolt, V. (2011). Psychological treatment for panic disorder with agoraphobia: A randomized controlled trial to examine the role of therapist-guided exposure in situ in CBT. Journal of Consulting and Clinical Psychology, 79(3), 406–420. Goisman, R. M., Warshaw, M. G., Peterson, L. G., Rogers, M. P., Cuneo, P., Hunt, M. F., Tomlinalbanese, J. M., Kazim, A., Gollan, J. K., Epsteinkaye, T., Reich, J. H., & Keller, M. B. (1994). Panic, agoraphobia, and panic disorder with agoraphobia: Data from a multicenter anxiety disorders study. Journal of Nervous & Mental Disease, 182(2), 72–79. Goldstein, A. J., & Chambless, D. L. (1978). A reanalysis of agoraphobia. Journal of Behavior Therapy and Experimental Psychiatry, 1, 305–313. Cognitive Behavioral Treatment of Agoraphobia Gould, R. A., Otto, M. W., & Pollack, M. H. (1995). A meta-analysis of treatment outcome for panic disorder. Clinical Psychology Review, 15, 819–844. Greenberg, P., Sisitsky, T., Kessler, R., & Finkelstein, S. (1999). The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychiatry, 60(7), 427–435. Hahlweg, K., Fiegenbaum, W., Frank, M., Schroeder, B., & von Witzleben, I. (2001). Shortand long-term effectiveness of an empirically supported treatment for agoraphobia. Journal of Consulting and Clinical Psychology, 69 (3), 375–382. Issakidis, C., & Andrews, G. (2004). Pretreatment attrition and dropout in an outpatient clinic for anxiety disorders. Acta Psychiatrica Scandinavica, 109, 426–433. Keefe, J. R., McCarthy, K. S., Dinger, U., Zilcha-Mano, S., & Barber, J. P. (2014). A metaanalytic review of psychodynamic therapies for anxiety disorders. Clinical Psychology Review, 34, 309–323. Kessler, R., Chiu, W., & Jin, R. (2006). The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Archives of General Psychiatry, 63(4), 415–424. Kuch, K., & Swinson, R. P. (1992). Agoraphobia: What Westphal really said. Canadian Journal of Psychiatry, 37(2), 133–136. Lepine, J.-P. (2003). The epidemiology of anxiety disorders: Prevalence and societal costs. Journal of Clinical Psychiatry, 63(Suppl. 14), 4–8. Marcaurelle, R., Bélanger, C., Marchand, A., Katerelos, T. E., & Mainguy, N. (2005). Marital predictors of symptom severity in panic disorder with agoraphobia. Journal of Anxiety Disorders, 19, 211–232. Markowitz, J. S., Weissman, M. M., Quellette, R., Lish, J. D., & Klerman, G. L. (1989). Quality of life in panic disorder. Archives of General Psychiatry, 46, 984–992. Mattick, R. P., Andrews, G., Hadzi-Pavlovic, D., & Christensen, H. (1990). Treatment of panic and agoraphobia: An integrative review. Journal of Nervous and Mental Disease, 178, 567–576. McNally, R. J., & Foa, E. B. (1987). Cognition and agoraphobia: Bias in the interpretation of threat. Cognitive Therapy and Research, 11, 567–582. McPherson, F. M., Brougham, L., & McLaren, S. (1980). Maintenance of improvement in agoraphobic patients treated by behavioral methods: Four year follow-up. Behaviour Research and Therapy, 18, 150–152. Michelson, L., Mavissakalian. M., & Marchione, K. (1985). Cognitive and behavioral treatments of agoraphobia: Clinical, behavioral and psychophysiological outcomes. Journal of Consulting and Clinical Psychology, 53, 913–925. Munby, J., & Johnston D.W. (1980). Agoraphobia: Long-term follow-up of behavioural treatment. British Journal of Psychiatry, 135, 418–427. Perreault, M., Julien, D., White, N. D., Bélanger, C., Marchand, A., Katerelos, T., & Milton, D. (2014). Treatment modality preferences and adherence to group treatment for panic disorder with agoraphobia. Psychiatric Quarterly, 85, 121–132. Rapee, R. M., & Murrell, E. (1988). Predictors of agoraphobic avoidance. Journal of Anxiety Disorders, 2, 203–218. Reiss, S., Peterson, R. A., Gursky, D. M., & McNally, R. J. (1986). Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy, 24, 1–8. Robins, L. N., & Regier, D. A. (1991). Psychiatric disorders in America. Macmillan. Sanchez-Meca, J., Rosa-Alcazar, A. I., Marin-Martinez, F., & Gomez-Conesa, A. (2010). Psychological treatment of panic disorder with or without agoraphobia: A meta-analysis. Clinical Psychology Review, 30, 37–50. Scupi, B. S., Maser, J. D., & Uhde, T. W. (1992). The National Institute of Mental Health Panic Questionnaire: An instrument for assessing clinical characteristics of panic disorder. Journal of Nervous and Mental Disease, 180, 566–572. 91 92 Vijaya Manicavasagar and Derrick Silove Swift, J. K., & Greenberg, R. P. (2012). Premature discontinuation in adult psychotherapy: A meta-analysis. Journal of Consulting and Clinical Psychology, 80, 547–559. Telch, M. J., Brouillard, M., Telch, C. F., Agras, W. S., & Taylor, C. B. (1989). Role of cognitive appraisal in panic-related avoidance. Behaviour Research and Therapy, 27, 373–383. Teusch, L., & Boehme, H. (1999). Is the exposure principle really crucial in agoraphobia? The influence of client-centered ‘nonprescriptive’ treatment on exposure. Psychotherapy Research, 9, 115–123. Turgeon, L., March, A., & Dupuis, G. (1998). Clinical features in panic disorder with agoraphobia: A comparison of men and women. Journal of Anxiety Disorders, 12, 539–553. White, K. S., Allen, L. B., Barlow, D. H., Gorman, J. M., Shear, M. K., & Woods, S. W. (2010). Attrition in a multicenter clinical trial for panic disorder. Journal of Nervous and Mental Disease, 198, 665–671. World Health Organisation. (2018). International Statistical Classification of Diseases and Related Health Problems (11th Revision). https://icd.who.int/browse11/1-m/en Yonkers, K. A., Zlotnick, C., Allsworth, J., Warshaw, M., Shea, T., & Keller, M. B. (1998). Is the course of panic disorder the same in women and men? American Journal of Psychiatry, 155, 596–602. Zarate, R., Craske, M., & Barlow, D. H. (1990). Situation exposure treatment versus panic control treatment for agoraphobia: A case study. Journal of Behaviour Therapy and Experimental Psychiatry, 21(3), 211–224. 6 Cognitive Behavioral Therapy for Social Anxiety Disorder Michaela B. Swee, M. Taylor Wilmer, and Richard G. Heimberg Introduction Social anxiety disorder (SAD), also known as social phobia, is one of the most commonly occurring anxiety disorders, with an estimated lifetime prevalence of 12% (Kessler et al., 2005). SAD is characterized by significant and persistent fear of social situations, such as initiating a conversation, giving a presentation, or speaking up at a meeting (American Psychiatric Association [APA], 2013). Individuals with SAD experience excessive fear of being negatively evaluated by others, which often results in avoidance of social situations and causes significant distress and impairment in social, occupational, and personal domains. SAD commonly occurs with other anxiety disorders as well as substance use disorders, mood disorders, and personality disorders (Aderka et al., 2012; Grant et al., 2005; Ruscio et al., 2008). SAD often develops in early adolescence and runs a chronic course if untreated (Bruce et al., 2005; Kessler et al., 2005). Fortunately, there are several evidencebased psychotherapeutic interventions for SAD, with cognitive behavioral therapy (CBT) garnering the most evidence in its support (Gordon et al., 2014). This chapter presents an overview of an individual CBT protocol for SAD, developed by Hope et al. (2010a, 2010b) and evaluated in randomized controlled trials (RCTs) (e.g., Goldin et al., 2012; Ledley et al., 2009). We first discuss the theoretical model on which this treatment is based and review relevant efficacy and effectiveness research. We follow with discussion of methods and measures for diagnosing SAD and assessing symptom severity before, during, and after treatment. We then discuss how treatment is introduced to clients, as well as the socialization process and strategies for forming an initial case conceptualization. Finally, we outline the therapy protocol and describe the core aspects of the sessions. 93 94 Swee, Wilmer, and Heimberg Previous Research A Model of Social Anxiety Disorder Multiple models of SAD exist (e.g., Clark, 2001; Heimberg et al., 2014; Hofmann, 2007). The Hope et al. (2010b) protocol was developed in tandem with the model of SAD proposed by Rapee and Heimberg (Heimberg et al., 2014; Rapee & Heimberg, 1997), which proposes that a primary driver of SAD is the discrepancy between a person’s perception of the demands of the social world and their perceived ability to meet those demands. Individuals with SAD hold a highly negative view of themselves, and they spontaneously generate negative self-images in social situations based on how they imagine other people see them (Hackmann et al., 1998; Wells & Papageorgiou, 1999). This third-person viewpoint is particularly problematic for individuals with SAD, because they believe that others (the ‘perceived audience’; Rapee & Heimberg, 1997) hold the same excessively high standards for social performance that they hold for themselves. Individuals with SAD believe that they are unable to meet these high expectations and thus overestimate the probability and consequences of negative evaluation by others. Cognitive, physiological, and behavioral symptoms of SAD emerge as consequences of this process. Individuals with SAD also engage in negative and distorted thoughts before, during, and after social situations (Kaplan et al., 2017). These negative thoughts often reflect the individual’s concern that they will be unable to meet the high expectations held by others in social situations (e.g., “I won’t have anything interesting to say”; “I’ll make a fool of myself”) or that others will judge them negatively (e.g., “They will think I’m an idiot”; “They don’t want to spend time with me.”). Individuals with SAD tend to accept these thoughts as fact, focusing on them as they approach social situations and engaging in perseverative thinking afterward. They also exhibit negative interpretation biases, making negative interpretations about neutral or ambiguous social events and interpreting negative social outcomes as catastrophic (Amir et al., 1998; Hertel et al., 2008; Stopa & Clark, 2000). This biased cognitive processing may increase the tendency to ignore or discount positive social outcomes (Alden et al., 2008; Hirsch & Mathews, 2000; Weeks, 2010), reinforcing negative thought patterns and maintaining social anxiety. In response to these negative thoughts and resulting anxiety, individuals with SAD engage in avoidance and escape behaviors. Sometimes social situations are completely avoided; other times, individuals with SAD exhibit more subtle forms of avoidance, known as safety behaviors (Clark, 2001; Piccirillo et al., 2016; Wells et al., 1995). Safety behaviors are typically employed to minimize negative evaluation or reduce anxiety when complete evasion of the situation is undesirable or impossible. For instance, socially anxious individuals may go to a party but speak only to familiar people, or they may attend class but avoid participating. Although avoidance and safety behaviors serve to reduce anxiety in the moment, they prevent socially anxious individuals from gathering disconfirmatory evidence related to their CBT for Social Anxiety Disorder negative thoughts, reinforce beliefs about social incompetence, and increase anxiety about future social situations (Clark, 2001; Heimberg et al., 2014; McManus et al., 2008). Thus, these behaviors perpetuate the cycle of anxiety and play an important role in maintaining SAD symptoms. Core Components of CBT for SAD CBT protocols commonly incorporate three core components: cognitive restructuring, exposure to feared social situations, and between-session homework. Cognitive restructuring helps individuals identify and challenge maladaptive thoughts and reframe them in ways that are more realistic and helpful. Exposures are utilized to confront anxiety-provoking situations, challenge the accuracy of anxious cognitions, and foster self-efficacy. Exposures can take many forms, including imaginal exposures, in-session role-play, and exposure to real-life social situations during or between therapy sessions (i.e., in vivo exposures). Cognitive restructuring and exposure activities are often used in tandem because cognitive restructuring aids in more realistic thinking, which facilitates effective coping and adaptive behavior. Additionally, experiencing successful behavioral outcomes provides powerful evidence to challenge maladaptive thoughts. Finally, regular homework assignments allow clients to independently practice skills learned during therapy and apply them to a diverse range of everyday situations. As clients approach the termination of formal sessions, therapists encourage them to continue applying their newly acquired skills in everyday life to lower the chance of relapse and to maintain treatment gains. Evidence Base of CBT for SAD Heimberg and colleagues first developed and evaluated a cognitive behavioral group therapy (CBGT) for the treatment of SAD (Heimberg & Becker, 2002). The initial efficacy study compared CBGT with an educational-supportive group psychotherapy control condition (Heimberg et al., 1990). CBGT yielded greater improvements in SAD from pre- to post-test and at six-month follow-up than did the control condition, and gains were maintained approximately five years later (Heimberg et al., 1993). CBGT has also performed well relative to other treatments for SAD. When compared with mindfulness-based stress reduction, CBGT produced lower post-treatment scores for SAD, greater response and remission rates (Koszycki et al., 2007), and greater decreases in safety behaviors (Goldin et al., 2016). Thus, evidence points to CBGT as an efficacious treatment for SAD, even when compared with credible placebo and active treatment conditions. Heimberg and colleagues adapted the protocol for use in individual treatment, resulting in a manualized and workbook-driven individual CBT for SAD, now in its second edition (Hope et al., 2010b). RCTs have demonstrated lowered client- and clinician-rated severity of social anxiety after 20 weeks of treatment, with gains maintained at three-month (Ledley et al., 2009) and one-year follow-ups (Goldin 95 96 Swee, Wilmer, and Heimberg et al., 2012). Additionally, individuals who received CBT experienced improvement in comorbid mood and anxiety disorders. Individual CBT, based largely on this protocol, is also efficacious compared with acceptance and commitment therapy (ACT), producing equivalent symptom reduction across 12 weeks of treatment and outperforming a wait-list control (Craske et al., 2014). Meta-analyses provide further support for the efficacy of CBT for SAD, yielding strong within-person treatment effects at post-treatment (d = 0.77) and at follow-up (d = 0.95; Gil et al., 2001). Average post-treatment effect sizes were also strong when compared with wait-list control groups (e.g., d = 0.71, Acarturk et al., 2009; g = 0.84, Barkowski et al., 2016; d = 1.19, Mayo-Wilson et al., 2014). The Heimberg model of CBGT (d = 0.80) and individual CBT (d = 1.02) showed effect sizes comparable to other CBT models (Mayo-Wilson et al., 2014). Moreover, multiple meta-analyses suggest that CBGT is as efficacious as individual CBT for SAD (Acarturk et al., 2009; Barkowski et al., 2016; Gil et al., 2001; Powers et al., 2008). When compared with pharmacotherapy, CBT has been shown to be as efficacious at reducing SAD symptoms. Some studies suggest that CBT yields better longterm outcomes and lower relapse rates than pharmacotherapy (e.g., Liebowitz et al., 1999). An RCT comparing CBGT with the monoamine oxidase inhibitor phenelzine found that participants who received phenelzine improved more rapidly and reported lower social anxiety after 12 weeks, but they also showed greater relapse during the follow-up period, suggesting that CBGT conferred greater protection against relapse (Heimberg et al., 1998; Liebowitz et al., 1999). More recent research demonstrated a synergistic effect, with combined CBGT and phenelzine producing a steeper rate of improvement, higher remission rates, and higher response rates than CBGT alone, phenelzine alone, or placebo (Blanco et al., 2010). However, Nordahl et al. (2016) recently demonstrated superior efficacy of CBT to paroxetine pharmacotherapy at post-treatment and one-year follow-up. CBT was also superior to combination treatment at follow-up. Meta-analyses suggest that individual and group CBT are just as efficacious as pharmacotherapy for SAD in terms of symptom reduction and response rates (Barkowski et al., 2016; Mayo-Wilson et al., 2014). CBT for SAD has also produced positive outcomes in effectiveness trials, demonstrating that CBT for SAD is both feasible and acceptable to individuals in routine clinical care. Across four treatment clinics in Germany, clients receiving individual CBT for SAD experienced a significant reduction in social anxiety, as well as general anxiety and depression, after only six weeks (Lincoln et al., 2003). CBGT for SAD in a community clinic produced similar results, yielding significant decreases in social anxiety and depression after only seven sessions (McEvoy, 2007). Longitudinal research has further indicated that social anxiety symptom reduction is maintained up to 12 months following CBT in a routine clinical setting (McCarthy et al., 2013). Direct comparisons have demonstrated that CBT for SAD administered in an outpatient clinic produces symptom reduction equivalent to administration in a research laboratory, even when the clinic sample had more severe social anxiety, more comorbid disorders, and lower educational attainment than the CBT for Social Anxiety Disorder research sample (Gaston et al., 2006; McEvoy, Nathan et al., 2012). Taken together, CBT (individual or group) appears to be both efficacious and effective in reducing symptoms of SAD, with gains maintained up to five years later. Methods of Assessment Diagnostic Interviews Diagnostic interviews are particularly useful tools for identifying SAD, differentiating SAD from other anxiety disorders, and capturing a broad diagnostic picture, including comorbidity. Our clinicians administer the Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5; Brown & Barlow, 2014), which focuses on assessment of anxiety and related disorders. Although psychometric data for the ADIS-5 have not yet been published, the ADIS-5 was closely modeled on the ADIS for DSM-IV (Brown et al., 1994), which demonstrated substantial inter-rater reliability for SAD (κ = 0.77; Brown et al., 2001). The ADIS-5 takes approximately three hours to administer and can provide a wealth of information about the experience of SAD, including symptom severity, perceived causes and triggers, age of onset, and current interference in functioning. Other interviews that can be used to assess the presence of SAD include the Structured Clinical Interview for DSM-5 (SCID-5; First et al., 2015) and the Mini International Neuropsychiatric Interview for DSM-5 (M.I.N.I. 7.0; Sheehan, 2015). Clinician-Administered Measures A clinician-administered measure can be a helpful supplement to a full diagnostic interview or useful when completing a diagnostic interview is difficult or unnecessary. The Liebowitz Social Anxiety Scale (LSAS; Liebowitz, 1987) was the first clinician-rated scale to assess social anxiety and remains widely used today. It is a 24-item measure that assesses feared and/or avoided social situations. The measure addresses social interaction situations (11 items; e.g., talking to people in authority) and performance situations (13 items; e.g., working while being observed). For each item, the evaluator asks for ratings of fear and avoidance on Likert-type scales, with fear ranging from 0 (none) to 3 (severe) and avoidance ranging from 0 (never, 0%) to 3 (usually, 68–100%). The evaluator may adjust ratings based on clinical judgment. Fear and avoidance ratings are summed to create a total score. The LSAS has demonstrated excellent internal consistency (Cronbach’s α = 0.96), good convergent validity with other measures of social anxiety, and sensitivity to treatment-related changes (Heimberg et al., 1999). The LSAS performs well in identifying individuals who meet criteria for SAD, with a clinical cutoff score of 30 providing the best balance of sensitivity and specificity (Mennin et al., 2002). The LSAS has also been validated as a self-report measure (Fresco et al., 2001; Table 6.1). The Brief Social Phobia Scale (Davidson et al., 1991, 1997) is another psychometrically sound clinician-administered measure of social anxiety. 97 98 Downloaded from https://www.cambridge.org/core, on subject to the Cambridge Core terms of use, available at https://www.cambridge.org/core/terms. https://doi.org/10.1017/9781108355605.007 Table 6.1. Commonly used self-report measures of social anxiety and related constructs Measure name Domain Items Item score range Total score range Clinical cutoff Reference Brief Fear of Negative Evaluation Scale (BFNE) Liebowitz Social Anxiety Scale Self-Report Versionb (LSAS-SR) Fear of negative evaluation and judgment from other people Fear and avoidance of social interaction and performance situations 12a 1–5 12–60 n/a 24 0–144 30 Social Interaction Anxiety Scale (SIAS) Fear of interaction in social situations involving dyads or groups 20c 0–3 for fear 0–3 for avoidance 0–4 Leary (1983) Fresco et al. (2001) 0–80 34 Social Phobia and Anxiety Inventory (SPAI) Cognitive, somatic, and behavioral dimensions of social fear 45 1–7 60 (Social Phobia Subscale only) Social Phobia Inventory (SPIN) Fear, avoidance, and physiological symptoms characteristic of social anxiety Fear at the prospect of being observed or watched by other people 17 0–4 0–192 (Social Phobia Subscale) 0–78 (Agoraphobia Subscale) 0–68 19 Connor et al. (2000) 20 0–4 0–80 24 Mattick & Clarke (1998) Social Phobia Scale (SPS) Mattick & Clarke (1998) Turner et al. (1989) Note: n/a, not applicable. a Recent research suggests that scoring of only the eight straightforwardly worded Brief Fear of Negative Evaluation (BFNE) items provides a more valid score (see Rodebaugh et al., 2011). b The LSAS-SR is psychometrically equivalent to the clinician-administered LSAS (Fresco et al., 2001). c Recent research suggests that scoring of only the 17 straightforwardly worded SIAS items provides a more valid score; a clinical cutoff score of 28 would be more appropriate with that scoring (see Rodebaugh et al., 2011). CBT for Social Anxiety Disorder Self-Report Measures Because a full diagnostic interview or clinician-administered measure is not always feasible, much attention has been devoted to the assessment of social anxiety via self-report. Self-report measures are quick to administer and a useful supplement to clinician-gathered information. Although a full discussion of all self-report measures is beyond the scope of this chapter, we provide a summary table that describes the most commonly used self-report measures of social anxiety and related constructs (Table 6.1). Measuring Progress in Treatment Continued monitoring of social anxiety is a useful process. Tracking progress on a week-to-week basis can alert the clinician to client improvement or relapse and help clients recognize and acknowledge incremental changes. Here we highlight the Social Anxiety Session Change Index (SASCI; Hayes et al., 2008), a four-item self-report measure that asks about change in four areas: (1) anxiety in anticipation of and/or during social situations, (2) avoidance of social situations, (3) concern about doing something embarrassing or humiliating in front of others, and (4) functional interference. Each item is rated relative to the start of treatment on a Likert-type scale ranging from 1 (much less than the start of treatment) to 7 (much more than the start of treatment), and the SASCI is scored by summing the four items. The SASCI has been shown to have good validity and internal consistency (α = 0.84–0.94) and correlates positively with session-by-session changes in the Brief Fear of Negative Evaluation Scale (Leary, 1983; Table 6.1). The SASCI offers a brief assessment of subjective improvement in social anxiety symptoms that can be useful in both treatment and research settings (Hayes et al., 2008). Case Formulation and Conceptualization For the remainder of this chapter, we discuss case conceptualization, socializing the client to treatment, introducing the treatment model and rationale, and delivering treatment content using the Hope et al. (2010a, 2010b) protocol. This is demonstrated through the case of Kayla, a 30-year-old Black heterosexual female who grew up in Southern California with her biological parents and elder sister. At the time of treatment initiation, she was enrolled as a full-time student in business school and worked part-time as a server at a local restaurant. Initial Diagnostic Assessment During the ADIS-5, Kayla reported that she struggled with social anxiety since early childhood; depression followed in middle school when she became keenly aware of feeling as if she did not “fit in.” She stated that her depression would worsen when she perceived that a social situation had gone poorly or worried that others viewed 99 100 Swee, Wilmer, and Heimberg her as a failure, triggering feelings of hopelessness. Results from the interview suggested that Kayla met DSM-5 criteria for SAD and major depressive disorder, recurrent episode, in partial remission. SAD was determined to be her primary diagnosis. Kayla recognized fear and avoidance of numerous social situations, including participating in her business school classes, speaking with people in authority (e.g., professors, her restaurant manager), refusing requests of dissatisfied customers at work, and interacting with fellow students in class. She worried that she would embarrass herself by saying something stupid, that her professors or manager thought she was incompetent, and that her peers thought poorly of her. Kayla reported that these fears interfered with her ability to perform effectively as a server in the restaurant, making her highly nervous about interacting with customers and hesitant to ask her manager for help. Historically, she reported that social anxiety caused significant distress and interference in school. She felt unable to make friends or network with peers, and her grades suffered because she rarely participated in class and turned papers in late due to fear of negative evaluation by her professors. Kayla identified goals for treatment as connecting with her classmates, improving her confidence at work, and being able to network in preparation for applying to jobs in line with her career interests. Psychoeducation and Client Socialization Process The first therapy session was primarily aimed at socializing the client to treatment. This process ensured that Kayla had an accurate understanding of SAD, how her own experiences were related to SAD, and how CBT for SAD could be helpful. During the session, Kayla’s therapist initiated a discussion about the universality and dimensionality of social anxiety by presenting three case vignettes (Hope et al., 2010b), which vary in the severity of social anxiety and associated impairment. The therapist explained that mild symptoms of social anxiety are normal and experienced by most people (e.g., public speaking situations, job interviews). However, when symptoms are sufficiently distressing and interfere with day-to-day life, treatment is warranted. The therapist then briefly summarized empirical evidence supporting the positive outcomes and long-term effects of CBT for SAD to emphasize the potential value of treatment for Kayla. Introduction to the Treatment Model and Rationale The therapist introduced an abbreviated treatment model to Kayla through a discussion of the three principal components of SAD: physical symptoms, thoughts, and behaviors.1 Kayla then practiced identifying these components in her own life. 1 We suggest that therapists familiarize themselves with the full Rapee-Heimberg (1997) model of SAD, but we find that this simplified model is more intuitive and relatable for clients. CBT for Social Anxiety Disorder Engaging in this exercise helped Kayla learn ways in which physical, cognitive, and behavioral symptoms interact with each other in a process we call the “downward spiral.” For example, Kayla became cognizant of how anxious thoughts increased her physical symptoms and behavioral avoidance. She noted that these relationships functioned bidirectionally. The therapist then introduced and described the three key components of CBT for SAD: cognitive restructuring, exposures, and homework. Kayla was offered the opportunity to ask questions and clarify her understanding throughout these discussions. Therapy Session Outline Sessions 1–4: Psychoeducation, Tracking Components of SAD, and Developing the Fear and Avoidance Hierarchy Session 1. A priority for the first four sessions was rapport building. This created a foundation of trust between Kayla and her therapist, allowing Kayla to feel safe and supported when confronting anxiety-provoking material. Much of this was achieved through psychoeducation, which helped Kayla to develop a framework and vocabulary for SAD. Through this process, the therapist also had an opportunity to better understand Kayla’s past and current experiences and they together developed collaborative goals for therapy. The remainder of session 1 was devoted to a motivational exercise. Kayla identified pros and cons of working versus not working on her SAD “right now.” This exercise was intended to increase investment in treatment, proactively identify potential barriers to engagement, and encourage adherence, particularly when therapy would become more exposure-focused. The session concluded with a discussion of specific ways to maximize treatment gains and effectiveness, including completing between-session homework and approaching rather than avoiding anxiety-provoking situations. Session 2. Kayla explored the three components of social anxiety in a recent interaction with a complaining customer. Kayla described her physiological experience of heart palpitations, lightheadedness, and sweaty palms when confronted by the customer. She identified the thoughts “He thinks this is my fault” and “He thinks I am incompetent at my job.” Regarding behavioral symptoms, Kayla remembered avoiding eye contact with the customer and leaving the table as quickly as possible. Kayla and her therapist discussed how these different symptoms interacted to create a downward spiral of anxiety. Attending to her physical symptoms affirmed her thoughts about appearing nervous or foolish, which intensified her physical symptoms, leading to further thoughts of incompetence and the inclination to escape. Kayla’s therapist emphasized that although avoidance/escape reduces anxiety in the short term, it increases feelings of guilt, shame, and depression; prevents learning; and reduces feelings of self-efficacy in social situations in the long term. 101 102 Swee, Wilmer, and Heimberg Next, the therapist introduced the three main components of treatment, which together serve as valuable tools for interrupting the downward spiral of social anxiety. The therapist explained that Kayla would first learn cognitive restructuring, the process of identifying maladaptive negative thoughts and modifying them to become more neutral, or less anxiety-provoking. The second component of treatment, which would begin after learning and practicing cognitive restructuring skills, is exposure. The therapist explained that exposure gives Kayla evidence with which to challenge her negative thoughts and gain confidence in her ability to persevere through anxiety-provoking social situations. Finally, Kayla was introduced to the third major component of treatment, between-session homework. Homework would be utilized throughout treatment to continue momentum between sessions and provide the opportunity to practice using cognitive restructuring and exposure skills in her everyday life.2 Session 3. This session was devoted to creating the “fear and avoidance hierarchy,” an important step prior to beginning exposures. For homework, Kayla generated eight to ten feared social situations that varied in level of anxiety evocation. Hierarchy items ranged from specific social scenarios (e.g., talking to her supervisor at work) to more general categories of social situations (e.g., networking with peers at business school events). Kayla and her therapist examined factors that made each situation more or less distressing. For example, one item on Kayla’s hierarchy was “sharing personal information.” The therapist asked if there were people with whom Kayla was more or less comfortable speaking about herself. Kayla reported that sharing personal information with her professors was more difficult than sharing with fellow students, which was more difficult than sharing personal information with coworkers at the restaurant. All of these situations were included on the hierarchy. Next, Kayla rated each situation on two dimensions: anxiety and avoidance (both on a scale from 0 to 100, where 0 is no anxiety or avoidance, and 100 is the worst anxiety or avoidance imaginable). To evaluate anxiety, the therapist described the Subjective Units of Distress Scale (SUDS; Wolpe & Lazarus, 1967). Kayla used her SUDS levels to rank the situations on her hierarchy from most to least difficult. Her therapist explained that they would monitor SUDS ratings throughout exposures to track symptom change over time. Session 4. This session focused on etiology and included a discussion of factors involved in the development of Kayla’s SAD. The therapist described ways in which genetics, family environment, and formative life experiences can influence SAD. The therapist used Kayla’s homework, an exploration of where her SAD came from, to guide the discussion. Kayla shared that there was a family history of social anxiety on her father’s side. Specifically, she observed that her paternal uncle and 2 It should be noted that the first portion of every session is devoted to a check-in on homework completion, as well as a review of highlights from the worksheets that were completed for homework. This serves as a way to regularly monitor clients’ compliance and investment in therapy, as well as an opportunity to ensure that material from the previous week’s session was appropriately and effectively integrated and implemented before moving on to new material. CBT for Social Anxiety Disorder cousin always seemed shy and withdrawn when she spent time with them. When she was a child, her father impressed upon her the importance of “staying under the radar” and encouraged Kayla to stay home if she was feeling nervous about attending school functions or birthday parties. Additionally, Kayla’s mother was strict and demanding, keeping Kayla and her sister from spending time with other children if their grades were not high enough or they had not finished their household chores. Thus, Kayla identified genetics and family environment as having the biggest impact on her development of SAD. Sessions 5 and 6: Automatic Thoughts and Cognitive Restructuring Session 5. The therapist opened this important phase of treatment with two vignettes in which an objectively neutral social situation leads to two entirely different outcomes for two individuals based on how they interpret the situation. The pair of vignettes illustrated that people with SAD become anxious because of their beliefs about a social situation, others involved, and themselves, not because of the situation itself. The therapist explained that negative thoughts about oneself, others, and the world can be labeled as automatic thoughts (ATs). ATs are frequently erroneous and/or unhelpful and have significant consequences for behaviors and emotions. Hence, learning to evaluate and challenge them, rather than automatically accepting them as fact, is fundamental to SAD treatment. Kayla and her therapist reviewed her ATs (recorded in previous homework assignments) and noted several important commonalities: they were emotionally based, largely negative, sometimes irrational, and often future-oriented. Kayla’s therapist next introduced the concept of thinking errors (Beck, 2011), which are common dysfunctional thinking patterns that underlie ATs.3 Strengthening Kayla’s ability to identify thinking errors in her own ATs was the first step in helping her question their validity and challenge them. Kayla practiced identifying thinking errors in the ATs of a case vignette, then some of her own ATs. Using the thought, “People will not like me when they meet me,” Kayla identified thinking errors such as mind reading and fortune telling. With the thought, “My writing is awful,” she identified all-or-nothing thinking, labeling, catastrophizing, and emotional reasoning (Beck, 2011). Kayla’s therapist pointed out that an individual AT may involve multiple thinking errors (as many of Kayla’s ATs did). Next, the therapist guided Kayla toward an awareness of emotions triggered by her ATs. For example, when Kayla experienced the thought that her writing was awful, she noticed feeling angry, hopeless, and ashamed. Kayla’s therapist emphasized the interconnections between thoughts and feelings – thoughts affect emotions and vice versa. Session 6. Before Kayla began exposures, she learned the final steps of cognitive restructuring. The therapist reminded Kayla that the aim was to act like a scientist by studying her thoughts and examining their validity and helpfulness. Kayla learned to challenge her ATs through the use of an anxious-self/coping-self 103 104 Swee, Wilmer, and Heimberg (AS/CS) dialogue. With this technique, Kayla would first identify an AS (anxious self ) thought, then pose a disputing question (coping self ), next answer the question expressing honest concern or disbelief in the response (anxious self ), then again pose a question to address that response (coping self ), and so on. Finally, a CS (coping self ) response is reached that Kayla could accept as tenable. Kayla’s AS/CS dialogue concerning the AT “People will not like me when they meet me” follows: Anxious self: Coping self: Anxious self: Coping self: Anxious self: Coping self: Anxious self: Coping self: Anxious self: Coping self: Anxious self: People will not like me when they meet me. How do you know that people will not like you when they meet you? Because there have been times when I have gotten the strong feeling that someone does not like me. When were these times? Once in fifth grade when I met that girl, Brianna, and once in high school with my teacher, Mr. Mattingly. Any other times? No, those are the two main ones I can think of. How many people have you met in your life? Over the course of my whole life? Oh, I don’t know if I can even count. Hundreds. Do you think Brianna and Mr. Mattingly’s possible dislike for you is representative of most people’s first impressions of you? No, I think most people feel positively, or at least neutral, when they meet me. By thoroughly examining these questions and answers, Kayla and her therapist noticed an eventual shift in her original anxious self perspective. Kayla realized that most people do not dislike her when they meet her. Next, the therapist asked Kayla to take a step back from the dialogue and summarize the take-home message. Kayla reported, “There have been a couple of people in my life who have not liked me, but I have met many people in my life and most people have had no negative feelings toward me at all; in fact, their reactions have been positive.” The therapist coached Kayla to generate a rational response from this summary point. Effective rational responses are typically short, concise, positive, or neutral statements that can be used to counter negative ATs in the heat of an anxiety-provoking situation. When the therapist asked Kayla for a rational response based on the conclusion of the AS/ CS dialogue, Kayla replied, “Most people I meet like me.” Kayla was encouraged to use this and other helpful rational responses during exposures and future anxietyprovoking situations. Sessions 7–11: First and Continued Exposures These sessions focus on conducting exposures to feared social situations. Exposures are perhaps the most important and impactful component of CBT for social anxiety, CBT for Social Anxiety Disorder particularly when paired with cognitive restructuring skills introduced in sessions 5 and 6. Kayla and her therapist discussed exposures several times prior to session 7, including when the treatment model was introduced and during the development of the fear and avoidance hierarchy. Session 7. The therapist reviewed key aspects of exposures, explaining that they would start with easier situations and steadily advance toward more anxietyprovoking situations. The rationale behind exposures was also reviewed, namely, that exposures would allow Kayla to experience habituation to feared social situations. She would also be able to practice specific social skills, learn to cope with anxiety while remaining in social situations, and gather additional evidence to challenge ATs, ultimately building self-efficacy. Kayla and her therapist collaboratively selected a situation from the lower portion of Kayla’s hierarchy for the first in-session exposure (one that triggered a SUDS level of 40–50 in real life). The chosen situation was relevant to Kayla’s treatment goals and could feasibly be conducted within the therapy session. Kayla selected “small talk at a business school networking event,” which she and her therapist role-played for the first exposure. The therapist guided Kayla through preexposure cognitive restructuring, in which Kayla identified her ATs and selected a specific thought for restructuring, in this case: “I won’t have anything interesting to say.” Kayla rated her belief in the AT at 80%. The therapist helped Kayla pinpoint thinking errors in the AT (e.g., all or nothing thinking, fortune telling, and catastrophizing), challenge the AT using an AS/CS dialogue, and develop a rational response: “All I have to do is talk about my favorite business school class.” Kayla rated her belief in the rational response at 40%. Kayla and her therapist then worked out the details of the exposure and, importantly, identified achievable behavioral goals. The therapist explained that such goals are attainable, observable, measurable, and focused on behaviors (i.e., how Kayla could act against SADrelated ATs) rather than oriented toward feelings (e.g., wishing to speak without feeling any anxiety). Kayla identified a behavioral goal of making one statement about her favorite class and asking at least two questions. The therapist reminded Kayla that she would be prompted to share her SUDS level and repeat her rational response throughout the exposure. Kayla and her therapist then completed the exposure. The therapist prompted Kayla to rate her SUDS level at one-minute intervals throughout the exposure and recorded each rating. Kayla was also prompted to state her rational response aloud whenever she gave a SUDS rating. After the exposure was completed, Kayla noted that she was able to share more than one piece of information and she asked four questions during the conversation. She stated that the conversation was easy because she already felt comfortable with the therapist, and the therapist pointed out the disqualifying the positive thinking error in that statement. The therapist and Kayla discussed her pattern of SUDS ratings, which peaked at 65 and eventually decreased to 20 by the end of the five-minute conversation. Kayla re-rated her belief in the AT at 50% and the rational response at 60%. Kayla also noticed one additional AT during the conversation, “This silent pause is so awkward.” The 105 106 Swee, Wilmer, and Heimberg therapist reflected that she did not notice any long pauses during the conversation, and she and Kayla used this information to challenge this AT. The therapist helped Kayla celebrate the completion of her first exposure and praised her for her effort. Finally, they collaborated on planning an out-of-session homework exposure. Kayla decided that she would say “Hello” and ask one question (e.g., “How was your weekend?”) to a classmate. Sessions 8–11. The following four sessions continued with in-session exposures, following a similar format and proceeding up Kayla’s hierarchy as appropriate. Sessions 12–15: Advanced Cognitive Restructuring and Core Beliefs Session 12. After conducting five in-session exposures, the skills of which were reinforced through in vivo, out-of-session exposures, sessions 12–15 turn to advanced cognitive restructuring techniques, with a particular focus on core beliefs. Core beliefs are the central and enduring beliefs one holds about oneself, others, the world, or the future (Beck, 2011). Individuals with SAD often hold negative core beliefs with typical themes of being unlovable, defective, helpless, or worthless. Because core beliefs are so fundamental and deeply held, they are often unarticulated prior to engaging in treatment. Thus, session 12 was aimed at helping Kayla explore and verbalize her negative core belief(s). The therapist guided Kayla to delve deeper into her ATs to examine her underlying beliefs about herself, using a downward arrow technique called “peeling the onion.” The therapist explained that the ATs Kayla had challenged in prior sessions were like the outer layers of an onion, and the goal for the session would be to “peel back” these layers and identify negative underlying beliefs that might be at the onion’s “core.” Kayla gathered her worksheets from previous exercises and homework assignments and reviewed her previously recorded ATs. She and the therapist examined the list for emergent themes, and she selected the one that seemed most important to how she thought about herself. She then addressed the theme with the following questions: (1) Why is that important?, (2) What does it mean if this is true?, and (3) What would be so bad about that? Similar to the AS/CS dialogue, she answered the question, questioned the answer, answered the question, and so on, until she reached a statement that she had believed for a long time, one that seemed very personal and true, and that evoked strong emotion. A transcript of this dialogue follows: Therapist: Kayla: Therapist: Thinking back to the automatic thoughts you challenged before and after your exposures, did you notice any that came up over and over again? Well, I usually had thoughts like, “I won’t have anything interesting to say” or “Everyone thinks I’m an idiot.” Okay, let’s focus on those “outer layer” automatic thoughts and see if we can peel back a few layers of the onion. First, do you notice any common themes in those thoughts? CBT for Social Anxiety Disorder Kayla: Therapist: Kayla: Therapist: Kayla: Therapist: Kayla: Therapist: Kayla: Therapist: Kayla: Therapist: Kayla: Well, I guess there seems to be a theme about other people not liking me because I’m not interesting or smart enough. And what would be so bad about that, if other people thought you were not interesting or smart enough? It would mean that I’m less than them in some way. It’s been like this my whole life. I’ve been working as hard as I can to keep up with everyone else, but I feel like I’ll never measure up. So, one related thought you have is, “I’ll never measure up.” It’s important to you to succeed in most, if not all, areas of your life. What does it mean to “measure up” to other people? I think of it as doing things really well or getting what you want, like the grades you want, the friends you want, the promotion you want. So, when you set a goal for yourself, you feel like you should meet or exceed that goal every time? Well it sounds a little extreme when you put it like that, but yeah. I don’t want to fall short, especially if I know I can do better. How does it feel when you think you’ve fallen short of your goals? It feels terrible. I have this sinking feeling in my stomach, and I feel really sad and ashamed. I get that way sometimes even if I do well. I don’t want to tell anyone about successes I have because I worry that they’re going to expect me to do even better the next time. So, you have the thought that even when you do something well or reach your goals, you’ll still fall short or disappoint people? Yeah, it’s like nothing I do will ever be good enough. I think you may have reached the core of the onion. Does “I’m not good enough” sound like it could be a core belief for you? Yeah, I guess so. It’s like I’ll never be smart enough, fun enough, or attractive enough, especially compared to my sister and my law school classmates. I think “I’m not good enough,” captures all of those. Kayla identified the core belief, “I am not good enough.” The therapist then explained that Kayla could approach the core belief like any other AT, by challenging and restructuring the belief using the same skills practiced since session 5. The therapist explained how in vivo exposures could help Kayla gather additional realworld evidence against this core belief. During the sessions that followed, Kayla used cognitive restructuring to identify and elaborate on past accomplishments. She reflected on the strength of her friendships from college and engaged in “perspective-taking” about her mother’s criticism. She also completed in vivo exposures of creating a resumé that highlighted her achievements, speaking to two recruiters at a networking event, and inviting one of her classmates to get coffee with her. Over 107 108 Swee, Wilmer, and Heimberg time, she chipped away at the belief that she was not good enough and gained strong evidence in opposition to this belief. Session 13 and Termination. A typical course of CBT for SAD runs 16–20 sessions, although some clients require more exposures or attention to core beliefs to achieve their treatment goals. The final sessions are focused on evaluating progress, establishing post-treatment goals, and discussing relapse prevention. Kayla terminated therapy in 19 sessions. She had made good progress toward her original goals and indicated that she felt comfortable applying her new skills independently. At the final session, Kayla and her therapist reviewed her SASCI scores, which had dropped by 50% since the beginning of treatment. Kayla also re-rated her fear and avoidance hierarchy and noted that her avoidance scores were considerably lower and her fear scores were moderately lower, especially for situations directly targeted in therapy. Kayla wondered aloud whether she had worked hard enough in her exposure sessions. The therapist again pointed out disqualifying the positive and helped Kayla remember how she overcame the challenges of her early exposures. Kayla also identified ways in which her day-to-day life had changed since beginning treatment. In addition to feeling less depressed, Kayla acknowledged that she now felt comfortable speaking in class and talking to her professors and was more confident in her ability to handle difficult customers at work. She further noted that she recently made a friend in one of her classes and attended two business school networking events. Kayla pointed out that the situations at the top of her hierarchy, including dating and job interviews, still evoked high levels of anxiety, but she felt more able to confront them without avoidance or safety behaviors. She and her therapist used these situations to set behavioral goals for Kayla’s first month following treatment. Kayla planned to create an online dating profile and apply to at least three jobs by the end of the month. Her therapist offered the option of booster sessions if Kayla were to get a job interview and wanted to refresh her CBT skills beforehand. The therapist congratulated Kayla on her hard work, her progress in treatment, and her openness to learning skills to manage her social anxiety, and they concluded their treatment together. Key Summary Points Social anxiety disorder (SAD) is characterized by excessive fear of negative evaluation and avoidance of social situations, which results in significant distress and impairment in social, occupational, and personal domains. Heimberg and colleagues developed a cognitive behavioral therapy (CBT) protocol for SAD that has been shown to be efficacious when compared with credible placebo and active treatment conditions, including pharmacotherapy, and effective when administered in routine clinical settings. Careful assessment of social anxiety and related symptomatology is essential to treatment planning, case conceptualization, and symptom monitoring. A variety CBT for Social Anxiety Disorder of clinician-administered (e.g., ADIS-5, LSAS) and self-report measures (e.g., SIAS, SPS) are available for these purposes (Table 6.1). The Heimberg CBT protocol is designed to be administered in 16–20 sessions. Primary treatment components include cognitive restructuring, exposure to feared social situations, and between-session homework. Sessions 1–4 focus on psychoeducation for SAD, socializing clients to treatment, and fostering treatment engagement. Clients are introduced to the treatment model and rationale; practice identifying the physical, cognitive, and behavioral symptoms of SAD; and create a hierarchy of feared social situations. Sessions 5 and 6 target the cognitive restructuring component of treatment. Clients learn to identify automatic thoughts, label thinking errors in the thoughts, and challenge the thoughts using disputing questions and an anxious-self/coping-self dialogue. Sessions 7–11 are devoted to conducting exposures to feared social situations, based on the clients’ “fear and avoidance hierarchy.” Successful in-session exposures are reinforced through cognitive restructuring beforehand, debriefing afterward, and in vivo exposures between sessions. Sessions 12–16 focus on advanced cognitive restructuring skills and continued exposures. Clients identify their core beliefs through a downward arrow exercise, and they work to challenge those beliefs through in-session restructuring and out-of-session exposure homework. Treatment termination may be considered when clients make progress toward their original goals and feel comfortable applying CBT skills independently in their own lives. The final session is devoted to evaluating progress, establishing post-treatment goals, and discussing strategies for relapse prevention. RECOMMENDED FURTHER READING Clark, D. M., & Wells, A. (1995). A cognitive model of social phobia. In R. Heimberg, M. Liebowitz, D. A. Hope, & F. R. Schneier (Eds.), Social phobia: Diagnosis, assessment, and treatment (pp. 69–93). Guilford Press. Gordon, D., Wong, J., & Heimberg, R. G. (2014). Cognitive-behavioral therapy for social anxiety disorder: The state of the science. In J. W. Weeks (Ed.), The Wiley-Blackwell handbook of social anxiety disorder (pp. 477–497). Wiley-Blackwell. Heimberg, R. G., Brozovich, F. A., & Rapee, R. M. (2014). A cognitive-behavioral model of social anxiety disorder. In S. G. Hofmann & P. M. DiBartolo (Eds.), Social anxiety: Clinical, developmental, and social perspectives (3rd ed., pp. 705–728). Academic Press. Heimberg, R. G., & Magee, L. (2014). Social anxiety disorder. In D. H. Barlow (Ed.), Clinical handbook of psychological disorders: A step-by-step treatment manual (5th ed., pp. 114–154). Guilford Publications. Hofmann, S. G. (2007). Cognitive factors that maintain social anxiety disorder: A comprehensive model and its treatment implications. Cognitive Behaviour Therapy, 36, 193–209. Hope, D. A., Heimberg, R. G., & Turk, C. L. (2010a). Managing social anxiety: A cognitivebehavioral therapy approach (Therapist Guide, 2nd ed.). Oxford University Press. 109 110 Swee, Wilmer, and Heimberg (2010b). Managing social anxiety: A cognitive-behavioral therapy approach (Client Workbook, 2nd ed.). New York: Oxford University Press. Kaplan, S. C., Swee, M. B., & Heimberg, R. G. (2018). Psychological treatments for social anxiety disorder. In O. Braddic (Ed.), Oxford research encyclopedia of psychology. Oxford University Press. Mayo-Wilson, E., Dias, S., Mavranezouli, I., Kew, K., Clark, D. M., Ades, A. E., & Pilling, S. (2014). Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. The Lancet Psychiatry, 1, 368–376. Powers, M. B., Sigmarsson, S. R., & Emmelkamp, P. M. G. (2008). A meta-analytic review of psychological treatments for social anxiety disorder. International Journal of Cognitive Therapy, 1, 94–113. REFERENCES Acarturk, C., Smit, F., de Graaf, R., van Straten, A., ten Have, M., & Cuijpers, P. (2009). Economic costs of social phobia: A population-based study. Journal of Affective Disorders, 115, 421–429. doi:10.1016/j.jad.2008.10.008 Aderka, I. M., Hofmann, S. G., Nickerson, A., Hermesh, H., Gilboa-Schechtman, E., & Marom, S. (2012). Functional impairment in social anxiety disorder. Journal of Anxiety Disorders, 26, 393–400. doi:10.1016/j.janxdis.2012.01.003 Alden, L. E., Taylor, C. T., Mellings, T. M. J. B., & Laposa, J. M. (2008). Social anxiety and the interpretation of positive social events. Journal of Anxiety Disorders, 22, 577–590. doi:10.1016/j.janxdis.2007.05.007 American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. Amir, N., Foa, E. B., & Coles, M. E. (1998). Automatic activation and strategic avoidance of threat-relevant information in social phobia. Journal of Abnormal Psychology, 107, 285–290. doi:10.1037/0021-843x.107.2.285 Barkowski, S., Schwartze, D., Strauss, B., Burlingame, G. M., Barth, J., & Rosendahl, J. (2016). Efficacy of group psychotherapy for social anxiety disorder: A meta-analysis of randomized-controlled trials. Journal of Anxiety Disorders, 39, 44–64. doi:10.1016/j. janxdis.2016.02.005 Beck, J. S. (2011). Cognitive behavior therapy: Basics and beyond (2nd ed.). Guilford Press. Blanco, C., Heimberg, R. G., Schneier, F. R., Fresco, D. M., Chen, H., Turk, C. L., . . . & Liebowitz, M. R. (2010). A placebo-controlled trial of phenelzine, cognitive behavioral group therapy, and their combination for social anxiety disorder. Archives of General Psychiatry, 67, 286–295. doi:10.1001/archgenpsychiatry.2010.11 Brown, T. A., & Barlow, D. H. (2014). Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5L): Client interview schedule. Oxford University Press. Brown, T. A., Di Nardo, P. A., & Barlow, D. H. (1994). Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV): Client interview schedule. Oxford University Press. Brown, T. A., Di Nardo, P. A., Lehman, C. L., & Campbell, L. A. (2001). Reliability of DSMIV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology, 110, 49–58. doi:10.1037/0021-843X.110.1.49 Bruce, S. E., Yonkers, K. A., Otto, M. W., Eisen, J. L., Weisberg, R. B., Pagano, M., . . . & Keller, M. B. (2005). Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: A 12-year prospective study. American Journal of Psychiatry, 162, 1179–1187. doi:10.1176/appi. ajp.162.6.1179 CBT for Social Anxiety Disorder Clark, D. M. (2001). A cognitive perspective on social phobia. In W. R. Crozier & L. E. Alden (Eds.), International handbook of social anxiety: Concepts, research and interventions relating to the self and shyness (pp. 405–430). John Wiley & Sons. Connor, K. M., Davidson, J. R. T., Churchill, L. E., Sherwood, A., Foa, E., & Weisler, R. H. (2000). Psychometric properties of the Social Phobia Inventory. British Journal of Psychiatry, 176, 379–386. doi:10.1192/bjp.176.4.379 Craske, M. G., Niles, A. N., Burklund, L. J., Wolitzky-Taylor, K. B., Vilardaga, J. P., Arch, J. J., . . . & Lieberman, M. D. (2014). Randomized controlled trial of cognitive behavioral therapy and acceptance and commitment therapy for social phobia: Outcomes and moderators. Journal of Consulting and Clinical Psychology, 82, 1034–1048. doi:10.1037/ a0037212 Davidson, J. R. T., Miner, C. M., De Veaugh-Geiss, J., Tupler, L. A., Colket, J. T., & Potts, N. L. S. (1997). The Brief Social Phobia Scale: A psychometric evaluation. Psychological Medicine, 27, 161–166. doi:10.1017/s0033291796004217 Davidson, J. R. T., Potts, N. L. S., Richichi, E. A., Ford, S. M., Krishnan, K. R. R., Smith, R. D., & Wilson, W. H. (1991). The Brief Social Phobia Scale. Journal of Clinical Psychiatry, 52 Suppl., 48–51. doi:10.1037/t07672-000 First, M. B., Williams, J. B. W., Karg, R. S., & Spitzer, R. L. (2015). Structured Clinical Interview for DSM-5 Disorders, clinician version (SCID-5-CV). American Psychiatric Publishing. Fresco, D. M., Coles, M. E., Heimberg, R. G., Liebowitz, M. R., Hami, S., Stein, M. B., & Goetz, D. (2001). The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine, 31, 1025–1035. doi:10.1017/S0033291701004056 Gaston, J. E., Abbott, M. J., Rapee, R. M., & Neary, S. A. (2006). Do empirically supported treatments generalize to private practice? A benchmark study of a cognitive-behavioural group treatment programme for social phobia. British Journal of Clinical Psychology, 45, 33–48. doi:10.1348/014466505x35146 Gil, P. M., Carrillo, F. M., & Meca, J. S. (2001). Effectiveness of cognitive-behavioural treatment in social phobia: A meta-analytic review. Psychology in Spain, 5, 17–25. Goldin, P. R., Morrison, A., Jazaieri, H., Brozovich, F., Heimberg, R., & Gross, J. J. (2016). Group CBT versus MBSR for social anxiety disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 84, 427–437. doi:10.1037/ccp0000092 Goldin, P. R., Ziv, M., Jazaieri, H., Werner, K., Kraemer, H., Heimberg, R. G., & Gross, J. J. (2012). Cognitive reappraisal self-efficacy mediates the effects of individual cognitivebehavioral therapy for social anxiety disorder in a randomized controlled trial. Journal of Consulting and Clinical Psychology, 80, 1034–1040. doi:10.1037/a0028555 Gordon, D., Wong, J., & Heimberg, R. G. (2014). Cognitive-behavioral therapy for social anxiety disorder: The state of the science. In J. W. Weeks (Ed.), The Wiley-Blackwell handbook of social anxiety disorder (pp. 477–497). Wiley-Blackwell. Grant, B. F., Hasin, D. S., Blanco, C., Stinson, F. S., Chou, S. P., Goldstein, R. B., . . . & Huang, B. (2005). The epidemiology of social anxiety disorder in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry, 66, 1351–1361. doi:10.4088/JCP.v66n1102 Hackmann, A., Surawy, C., & Clark, D. M. (1998). Seeing yourself through others’ eyes: A study of spontaneously occurring images in social phobia. Behavioural and Cognitive Psychotherapy, 26, 3–12. Hayes, S. A., Miller, N. A., Hope, D. A., Heimberg, R. G., & Juster, H. R. (2008). Assessing client progress session by session in the treatment of social anxiety disorder: The Social Anxiety Session Change Index. Cognitive and Behavioral Practice, 15, 203–211. doi:10.1016/j.cbpra.2007.02.010 111 112 Swee, Wilmer, and Heimberg Heimberg, R. G., & Becker, R. E. (2002). Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. Guilford Press. Heimberg, R. G., Brozovich, F. A., & Rapee, R. M. (2014). A cognitive-behavioral model of social anxiety disorder. In S. G. Hofmann, & P. M. DiBartolo (Eds.), Social anxiety: Clinical, developmental, and social perspectives (3rd ed., pp. 705–728). Academic Press. doi:10.1016/B978-0-12-394427-6.00024-8 Heimberg, R. G., Dodge, C. S., Hope, D. A., Kennedy, C. R., Zollo, L. J., & Becker, R. E. (1990). Cognitive behavioral group treatment for social phobia: Comparison with a credible placebo control. Cognitive Therapy and Research, 14, 1–23. doi:10.1007/ bf01173521 Heimberg, R. G., Horner, K. J., Juster, H. R., Safren, S. A., Brown, E. J., Schneier, F. R., & Liebowitz, M. R. (1999). Psychometric properties of the Liebowitz Social Anxiety Scale. Psychological Medicine, 29, 199–212. doi:10.1017/S0033291798007879 Heimberg, R. G., Liebowitz, M. R., Hope, D. A., Schneier, F. R., Holt, C. S., Welkowitz, L. A., . . . & Klein, D. F. (1998). Cognitive behavioral group therapy versus phenelzine therapy for social phobia. Archives of General Psychiatry, 55, 1133–1141. doi:10.1001/ archpsyc.55.12.1133 Heimberg, R. G., Salzman, D., Holt, C. S., & Blendell, K. (1993). Cognitive behavioral group treatment of social phobia: Effectiveness at 5-year follow-up. Cognitive Therapy and Research, 17, 325–339. doi:10.1007/BF01177658 Hertel, P. T., Brozovich, F., Joormann, J., & Gotlib, I. H. (2008). Biases in interpretation and memory in generalized social phobia. Journal of Abnormal Psychology, 117, 278–288. doi:10.1037/0021-843x.117.2.278 Hirsch, C. R., & Mathews, A. (2000). Impaired positive inferential bias in social phobia. Journal of Abnormal Psychology, 109, 705–712. doi:10.1037/0021-843x.109.4.705 Hofmann, S. G. (2007). Cognitive factors that maintain social anxiety disorder: A comprehensive model and its treatment implications. Cognitive Behaviour Therapy, 36, 193–209. doi:10.1080/16506070701421313 Hope, D. A., Heimberg, R. G., & Turk, C. L. (2010a). Managing social anxiety: A cognitivebehavioral therapy approach (Therapist Guide, 2nd ed.). Oxford University Press. doi:10.1093/med:psych/9780195336689.001.0001 (2010b). Managing social anxiety: A cognitive-behavioral therapy approach (Client Workbook, 2nd ed.). Oxford University Press. doi:10.1093/med:psych/ 9780195336696.001.0001 Kaplan, S. C., Morrison, A. S., Goldin, P. R., Olino, T. M., Heimberg, R. G., & Gross, J. J. (2017). The Cognitive Distortions Questionnaire (CD-Quest): Validation in a sample of adults with social anxiety disorder. Cognitive Therapy and Research, 41, 576–587. doi:10.1007/s10608-017-9838-9 Kessler, R., Chiu, W., Demler, O., Merikangas, K., & Walters, E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 617–628. doi:10.1001/archpsyc.62.6.617 Koszycki, D., Benger, M., Shlik, J., & Bradwejn, J. (2007). Randomized trial of a meditationbased stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behaviour Research and Therapy, 45, 2518–2526. doi:10.1016/j. brat.2007.04.011 Leary, M. R. (1983). A brief version of the Fear of Negative Evaluation Scale. Personality and Social Psychology Bulletin, 9, 371–375. doi:10.1177/0146167283093007 Ledley, D. R., Heimberg, R. G., Hope, D. A., Hayes, S. A., Zaider, T. I., Dyke, M. V., . . . & Fresco, D. M. (2009). Efficacy of a manualized and workbook-driven individual treatment for social anxiety disorder. Behavior Therapy, 40, 414–424. doi:10.1016/j. beth.2008.12.001 CBT for Social Anxiety Disorder Liebowitz, M. R. (1987). Social phobia. Modern Problems in Pharmacopsychiatry, 22, 141–173. doi:10.1159/000414022 Liebowitz, M. R., Heimberg, R. G., Schneier, F. R., Hope, D. A., Davies, S., Holt, C. S., . . . & Klein, D. F. (1999). Cognitive-behavioral group therapy versus phenelzine in social phobia: Long-term outcome. Depression and Anxiety, 10(3), 89–98. PMID: 10604081. Lincoln, T. M., Rief, W., Hahlweg, K., Frank, M., von Witzleben, I., Schroeder, B., & Fiegenbaum, W. (2003). Effectiveness of an empirically supported treatment for social phobia in the field. Behaviour Research and Therapy, 41, 1251–1269. doi:10.1016/s00057967(03)00038-x Mattick, R. P., & Clarke, J. C. (1998). Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy, 36, 455–470. doi:10.1016/s0005-7967(97)10031-6 Mayo-Wilson, E., Dias, S., Mavranezouli, I., Kew, K., Clark, D. M., Ades, A. E., & Pilling, S. (2014). Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. Lancet Psychiatry, 1, 368–376. doi:10.1016/s2215-0366(14)70329-3 McCarthy, O., Hevey, D., Brogan, A., & Kelly, B. D. (2013). Effectiveness of a cognitive behavioural group therapy (CBGT) for social anxiety disorder: Immediate and longterm benefits. The Cognitive Behaviour Therapist, 6. doi:10.1017/S1754470X13000111 McEvoy, P. M. (2007). Effectiveness of cognitive behavioural group therapy for social phobia in a community clinic: A benchmarking study. Behaviour Research and Therapy, 45, 3030–3040. doi:10.1016/j.brat.2007.08.002 McEvoy, P. M., Nathan, P., Rapee, R. M., & Campbell, B. N. C. (2012). Cognitive behavioural group therapy for social phobia: Evidence of transportability to community clinics. Behaviour Research and Therapy, 50, 258–265. doi:10.1016/j.brat.2012.01.009 McManus, F., Sacadura, C., & Clark, D. M. (2008). Why social anxiety persists: An experimental investigation of the role of safety behaviours as a maintaining factor. Journal of Behavior Therapy and Experimental Psychiatry, 39, 147–161. doi:10.1016/j. btep.2006.12.002 Mennin, D. S., Fresco, D. M., Heimberg, R. G., Schneier, F. R., Davies, S. O., & Liebowitz, M. R. (2002). Screening for social anxiety disorder in the clinical setting: Using the Liebowitz Social Anxiety Scale. Journal of Anxiety Disorders, 16, 661–673. doi:10.1016/ S0887-6185(02)00134-2 Nordahl, H. M., Vogel, P. A., Morken, G., Stiles, T. C., Sandvik, P., & Wells. A. (2016). Paroxetine, cognitive therapy or their combination in the treatment of social anxiety disorder with and without avoidant personality disorder: A randomized clinical trial. Psychotherapy and Psychosomatics, 85, 346–356. doi:10.1159/000447013 Piccirillo, M. L., Dryman, M. T., & Heimberg, R. G. (2016). Safety behaviors in adults with social anxiety: Review and future directions. Behavior Therapy, 47, 675–687. doi:10.1016/ j.beth.2015.11.005 Powers, M. B., Sigmarsson, S. R., & Emmelkamp, P. G. (2008). A meta-analytic review of psychological treatments for social anxiety disorder. International Journal of Cognitive Therapy, 1, 94–113. doi:10.1521/ijct.2008.1.2.94 Rapee, R. M., & Heimberg, R. G. (1997). A cognitive-behavioral model of anxiety in social phobia. Behaviour Research and Therapy, 35, 741–756. doi:10.1016/s0005-7967 (97)00022-3 Rodebaugh, T. L., Heimberg, R. G., Brown, P. J., Fernandez, K. C., Blanco, C., Schneier, F. R., & Liebowitz, M. R. (2011). More reasons to be straightforward: Findings and norms for two scales relevant to social anxiety. Journal of Anxiety Disorders, 25, 623–630. doi:10.1016/j.janxdis.2011.02.002 113 114 Swee, Wilmer, and Heimberg Ruscio, A. M., Brown, T. A., Chiu, W. T., Sareen, J., Stein, M. B., & Kessler, R. C. (2008). Social fears and social phobia in the USA: Results from the National Comorbidity Survey Replication. Psychological Medicine, 38, 15–28. doi:10.1017/s0033291707001699 Sheehan, D. V. (2015). Mini International Neuropsychiatric Interview 7.0. Medical Outcomes Systems. Stopa, L., & Clark, D. M. (2000). Social phobia and interpretation of social events. Behaviour Research and Therapy, 38, 273–283. doi:10.1016/s0005-7967(99)00043-1 Turner, S. M., Beidel, D. C., Dancu, C. V., & Stanley, M. A. (1989). An empirically derived inventory to measure social fears and anxiety: The Social Phobia and Anxiety Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 1, 35–40. doi:10.1037/1040-3590.1.1.35 Weeks, J. W. (2010). The Disqualification of Positive Social Outcomes Scale: A novel assessment of a long-recognized cognitive tendency in social anxiety disorder. Journal of Anxiety Disorders, 24, 856–865. doi:10.1016/j.janxdis.2010.06.008 Wells, A., Clark, D. M., Salkovskis, P., Ludgate, J., Hackmann, A., & Gelder, M. (1995). Social phobia: The role of in-situation safety behaviors in maintaining anxiety and negative beliefs. Behavior Therapy, 26, 153–161. doi:10.1016/s0005-7894(05)80088-7 Wells, A., & Papageorgiou, C. (1999). The observer perspective: Biased imagery in social phobia, agoraphobia, and blood/injury phobia. Behaviour Research and Therapy, 37, 653–658. doi:10.1016/s0005-7967(98)00150-8 Wolpe, J., & Lazarus, A. A. (1967). Behavior therapy techniques: A guide to the treatment of neuroses. Pergamon Press. 7 CBT for Social Anxiety Disorder Henrik Nordahl and Adrian Wells Introduction Social anxiety disorder (SAD) is characterized by a marked fear or anxiety concerning one or more social situations in which the individual may be scrutinized by others (DSM-5; American Psychiatric Association [APA], 2013). Individuals with SAD are concerned with their social performance and fear that others will perceive them negatively, for example, as anxious, boring, stupid, weak, or unlikeable and that this will lead to embarrassment, humiliation, rejection, or loss of self-worth. These concerns can be so pronounced that the individual avoids most social situations or endures them with intense discomfort. SAD is one of the most common mental health disorders, with a 12-month prevalence estimate of 7% and a lifetime estimate of 12% in the United States (Ruscio et al., 2008). The disorder often has an early onset with a median of 13 years of age, and 75% of individuals with SAD have an onset between 8 and 15 years (APA, 2013). In addition, SAD is considered a relatively chronic disorder if left untreated and is associated with lower quality of life. It is also considered to be a major risk factor for developing major depressive disorder, other anxiety disorders, substance abuse/addiction, and work-related problems (APA, 2013; Wittchen & Fehm, 2003). Effective clinical management and treatment of the disorder is therefore of great importance. The Cognitive Model of SAD Building on Beck’s schema theory (Beck, 1976) and the self-regulatory executive function (S-REF) model of psychological disorder (Wells & Matthews, 1994), Clark and Wells (1995) advanced a cognitive model of SAD that has received substantial empirical support. Central to the model is the view that individuals with SAD engage in an information processing style characterized by self-focused attention. Self-attention is not capable of providing unambiguous disconfirmation of social fears and concerns in feared social situations, as the primary source of information comes from feelings and sensations rather than external information which has the 115 116 Henrik Nordahl and Adrian Wells Social Situation Activates assumptions Perceived social danger (negative automatic thoughts) Processing of Self as a Social Object Safety Behaviors Somatic and cognitive symptoms Figure 7.1. A cognitive model of social phobia. From Wells (1997, p. 169). Copyright 1997 by John Wiley & Sons Limited. Reprinted by permission potential to correct distorted beliefs. Hence, the Clark and Wells model accounts for the persistence of SAD with reference to a number of specific cognitive-behavioral mechanisms involving vicious circles that are responsible for maintaining the problem. This model is depicted in Figure 7.1. Assumptions and Beliefs Resulting from past experience, individuals with SAD hold negative assumptions and beliefs about social situations and the social self that are activated when entering or anticipating a social situation. These beliefs contribute to negative appraisals of social situations and the vicious cycles that maintain SAD. The following three types of assumptions and beliefs are identified in the model: 1. Conditional assumptions (e.g., “If I show signs of anxiety, people will think I am weak”; “If people like me they will begin the conversation first”) 2. Unconditional beliefs about the social self (e.g., “I am boring”; “I am unlikeable”) 3. High standards and rules for social performance (e.g., “I must always get everyone’s approval”; “I have to appear intelligent and relaxed”) CBT for Social Anxiety Disorder Activation of such assumptions and beliefs leads to a perception of potential social danger, which is evident as anticipatory worry or negative automatic thoughts – for example, “What if I shake?”; “They will notice I’m anxious”; and “I’ll babble and talk funny” – which increase the sense of threat and anxiety. Furthermore, the somatic and cognitive symptoms that accompany anxiety are themselves subject to negative appraisal and may be interpreted as evidence of failure and impending social humiliation. Processing of the Self as a Social Object Negative automatic thoughts about the social self not only are associated with an increase in anxiety symptoms but also are accompanied by a shift in attention in which the individual becomes self-conscious and engages in self-processing with a specific focus toward how they think they appear to others. The socially anxious individual uses internal information in the form of feelings or an image of the self in their mind’s eye to infer how they must appear. The image of the self typically consists of an “observer perspective,” meaning that it entails seeing oneself as if from someone else’s vantage point. In images of this type, anxiety symptoms and personal inadequacies are seen as highly conspicuous, and the socially anxious person assumes that the negative observer image accurately reflects what other people can see in them. This process in turn reinforces negative self-appraisals of performance and negative thoughts about evaluation by others. Safety Behaviors In order to prevent feared social outcomes, such as showing anxiety or failed performance, safety behaviors are used. For example, individuals fearful of saying something that others will judge as stupid will often say little or mentally rehearse sentences before talking. Contrary to their intended effect, safety behaviors are problematic and maintain social anxiety in several ways. They contribute to heightened self-focused attention, prevent disconfirmation of negative beliefs and assumptions, increase feared symptoms, can draw attention toward the individual, and have the potential to contaminate the social situation by, for example, making the person with SAD appear withdrawn or unfriendly. In addition to the safety behaviors that are used during a social encounter, avoidance of social situations is a problem because it prohibits experiences that could disconfirm assumptions and beliefs. It is therefore crucial to deal with in order to maximize treatment effects. Post-Mortem and Anticipatory Processing There are two other strategies that individuals with SAD use to deal with social concerns that occur before or after social encounters. Before exposure to situations, anticipatory worry and planning are used to try to deal with and avoid social threat, 117 118 Henrik Nordahl and Adrian Wells for example, mentally rehearsing conversations. This is a negative process that heightens the sense of danger and anxiety. On leaving the social situation the individual may also engage in a “post-mortem” that consists of rumination, analyzing their performance, and recalling what might have gone wrong. This process can transform a relatively positive experience into a sense of failure to perform well. Each of these processes contributes to emotional distress and negative selfprocessing even in the absence of direct social threat. Research Supporting CBT for SAD There is substantial empirical support for the key aspects of the Clark and Wells model such as the role of observer perspective imagery (e.g., Wells, Clark & Ahmad, 1998) and reviews of self-focused attention (Ng et al., 2014), safety behaviors (Piccirillo et al., 2015), and dysfunctional self-beliefs (Gregory & Peters, 2017). In terms of treatments for SAD, findings are summarized in a systematic review and network meta-analysis by Mayo-Wilson and colleagues (2014) that aimed to compare interventions for SAD and identify which were the most effective in adults. They included 101 trials which explored 41 interventions or control conditions. Compared with wait-list control, several classes of medications (monoamine oxidase inhibitors, benzodiazepines, selective serotonin-reuptake inhibitors, serotoninnorepinephrine reuptake inhibitors, and anticonvulsants), individual CBT, group CBT, exposure and social skills training, self-help with support, self-help without support, and psychodynamic psychotherapy were efficacious. However, individual CBT was found to be most effective, and the authors concluded that, in particular, individual CBT that was based on the Clark and Wells (1995) model provided large effects (standardized mean difference compared with wait-list reported to be 1.56, with 95% confidence interval for recovery from 1.85 to 1.27 based on three included studies). This finding is in line with the most updated clinical guidelines for adults with SAD, for example, by the National Institute for Health and Care Excellence (NICE, 2013); however, the meta-analysis has also been criticized for being biased in favor of CBT in drawing its conclusions (Wampold et al., 2017). The efficacy of CBT based specifically on the Clark and Wells (1995) model and treatment manuals (e.g., Wells, 1997) has been evaluated in several randomized controlled trials. Clark et al. (2003) reported that CBT was superior to fluoxetine combined with self-exposure, and superior to placebo combined with self-exposure. The effect size for CBT pre- to post-treatment on social anxiety symptoms was large (Cohen’s d = 1.31). In a different study, Clark and colleagues (2006) demonstrated that CBT was superior to exposure plus applied relaxation. The effect size for CBT was reported to be large from pre- to post-treatment (Cohen’s d = 2.63) and 86% of patients were classified as recovered at post-treatment. In this study, 78% of the patients who met criteria for avoidant personality disorder at pretreatment no longer met the criteria at one-year follow-up. Both these studies reported that treatment effects were maintained at follow-up one year after treatment. Moreover, CBT was also associated with large effect sizes on secondary outcome measures such as depression. CBT for Social Anxiety Disorder Stangier and colleagues (2003) compared individual with group CBT and found that the treatment was most efficacious in the individual format with a large mean effect size for social anxiety measures at post-treatment (Cohen’s d = 1.17) and at six-month follow-up (Cohen’s d = 1.57). In a similar study, Mörtberg and colleagues (2007) reported individual CBT to be more efficacious than group and intensive group CBT. The individual CBT was associated with a large mean effect size for social anxiety measures post-treatment (Cohen’s d = 1.62) and at one-year follow-up (Cohen’s d = 1.89). CBT has been compared with interpersonal therapy (IPT) in two studies. Stangier et al. (2011) reported that CBT was superior to IPT and that the response rate for CBT was 65.8% and largely maintained at one-year follow-up. CBT was associated with large controlled effect sizes on measures of social anxiety and medium controlled effect sizes for depression symptoms. In another study, CBT was evaluated against IPT in a residential setting: Borge and colleagues (2008) reported a medium effect size for CBT from pre- to post-treatment (Cohen’s d = 0.76) and that only 31% of patients were classified as recovered post-treatment. However, the effects of CBT were not statistically different from those of residential interpersonal therapy. Leichsenring et al. (2013) conducted a large RCT where they compared CBT to psychodynamic therapy. They found CBT to be the superior intervention and reported a remission rate for CBT of 36%. The effect size for CBT from pre- to post-treatment was large (Cohen’s d = 1.32). However, it is important to note that Leichsenring and colleagues delivered CBT over a mean of 25.7 sessions, suggesting that the treatment manual was not adhered to. To summarize, CBT based on the Clark and Wells model is associated with moderate to large effects on primary and secondary outcome measures, which are largely maintained at follow-up. The efficacy of the treatment seems to be reliant on adherence and competence factors. Moreover, the treatment has been found to be superior to other psychological treatments and medications in most direct comparisons. Clinical Management of SAD In the remainder of this chapter, we will describe the clinical management of SAD from a CBT orientation in terms of issues related to assessment, formulation, and intervention. A more extensive and detailed description of this CBT for SAD can be found in the treatment manual by Wells (1997, pp. 167–199). Effective interventions for SAD such as CBT may not be accessed due to poor recognition and inadequate assessment. Often, individuals with primary SAD present in the clinic with other problems such as depression or substance dependence, and will reveal their problem with social anxiety only on direct questioning. In addition, many patients with various disorders present with social evaluative concerns and anxiety in social situations that are not manifestations of SAD. For example, patients with paranoid personality problems can present social anxiety 119 120 Henrik Nordahl and Adrian Wells due to suspiciousness and mistrust in others, while patients with body dysmorphic disorder can present social anxiety related to their obsessive belief about the conspicuousness of a “flawed body part.” Thus, an initial and crucial step in the successful formulation and treatment of these patients is a thorough clinical assessment and accurate diagnosis of the presenting problem. Two of the most commonly used semi-structured interviews for diagnosing SAD are the Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV; Brown et al., 1994) and the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-IV; First et al., 1996). Both instruments are based on the diagnostic criteria outlined in DSM-IV, but recent revisions of these instruments have been published following the publication of DSM-5 (APA, 2013): ADIS-5 (Brown & Barlow, 2014) and SCID-5-RV (First et al., 2015). Assessment Following a thorough general clinical assessment and accurate diagnosis of SAD, more SAD-specific assessment and measurement will serve several aims. These include assessing severity of the problem, identifying which situations are associated with most fear and/or avoidance, elicitation of information about the maintaining mechanisms for case conceptualization, and monitoring treatment outcome. Measurement should be used to determine progress in meeting treatment goals and as a guide to modifying components of treatment in a way that maximizes the probability of cognitive behavioral change. For example, the continuation of counterproductive safety behaviors and avoidance should be monitored throughout treatment as they prohibit necessary disconfirmation of social fears and the acquisition of new information. There is a range of clinical assessment tools that can be used to assess social anxiety and the components thought to maintain it. These have recently been summarized in a review by Wong et al. (2016), which the interested reader can consult for more detailed information. A brief overview of scales frequently used in research and with good utility for clinical practice are outlined. Clinician-Administered Outcome Measures In addition to the ADIS-IV/ADIS-5, commonly used clinician-administered scales include the Liebowitz Social Anxiety Scale (LSAS; Liebowitz, 1987) and the Brief Social Phobia Scale (BSPS; Davidson et al., 1997). All these assessment tools provide separate ratings of fear and avoidance for different social situations. Thus, these instruments can be of great use in planning treatment as they provide information about the severity and breadth of social anxiety and which situations are associated with the most fear and/or anxiety for the patient. Self-Report Outcome Measures There is a range of self-report measures that are established and widely used to assess social anxiety. Although these measures overlap, there are slight differences CBT for Social Anxiety Disorder in terms of what they assess. The Liebowitz Social Anxiety Scale has also been developed as a self-report version (LSAS-SR; Baker et al., 2002) and assesses fear and avoidance across 24 different social situations. The Social Interaction Anxiety Scale (SIAS; Mattick & Clarke, 1998) measures distress related to interaction with others. The Social Phobia Scale (SPS; Mattick & Clarke, 1998) assesses anxiety related to being observed or watched by others. The Social Phobia and Anxiety Inventory (SPAI; Turner et al., 1989) assesses symptoms, cognitions, and behavior in a range of social situations. The Social Phobia Inventory (SPIN; Connor et al., 2000) assesses fear, avoidance, and physiological discomfort related to social situations. Moreover, shortened versions have been developed for several of the most commonly used scales to reduce administration times, which can be an important factor in clinical settings. For a comprehensive overview of these measures, the interested reader should consult Wong et al. (2016). Self-Report Measures of SAD-Maintenance Factors Cognitive and behavioral factors that maintain social anxiety are usually assessed with self-report measures. The Social Phobia Rating Scale (SPRS; Wells, 1997) was published together with the original treatment manual and was designed as a clinical assessment tool for assessment and monitoring of social anxiety and its cognitive behavioral maintenance components when treating SAD patients with CBT. The SPRS has 32 items and five subscales that assess distress, avoidance, selfconsciousness, use of safety behaviors, and negative beliefs characterizing SAD. In addition, several measures more specifically assess cognitive and behavioral components of the cognitive model that we briefly mention below. Negative beliefs characterizing social anxiety can be assessed with the Social Cognitions Questionnaire (SCQ; Wells et al., 1993). In addition, the Self-Beliefs Related to Social Anxiety Scale (SBSA; Wong & Moulds, 2009; Wong et al., 2014) was developed to assess high standards, unconditional beliefs, and conditional beliefs based on the Clark and Wells (1995) model. Anticipatory processing can be assessed with the Anticipatory Social Behaviours Questionnaire (ASBQ; Hinrichsen & Clark, 2003), and post-event processing can be assessed with the Post-Event Processing Questionnaire (PEPQ; Rachman et al., 2000). Self-attention can be assessed with the Self-Consciousness Scale (SCS; Fenigstein et al., 1975), and, in particular, one of its subscales (public self-consciousness) is relevant to the Clark and Wells (1995) model. Safety behaviors can be assessed with the Social Behaviours Questionnaire (SBQ; Clark et al., 1995). Avoidance of social situations is best assessed with the previously described outcome measures. Cognitive Behavioral Therapy for Social Anxiety Disorder Structure of Treatment A course of CBT treatment for SAD (Wells, 1997) is typically implemented over 12–14 sessions, in which sessions are held weekly and each session is normally 121 122 Henrik Nordahl and Adrian Wells 60 minutes in duration. Moreover, the treatment should follow a particular sequence in maximizing the efficiency of cognitive behavioral change. It is a logical derivation from the model to use strategies early in treatment that reconfigure the patient’s behaviors and focus of attention in a way that maximizes subsequent change in negative thoughts and beliefs. More specifically, if behavioral experiments involving exposure proceed without modifying the use of maladaptive safety behaviors and reducing self-focused attention, the effectiveness of such strategies may be impaired. Sessions 1–3 of treatment usually consists of case formulation, socialization, and cognitive preparation for restructuring, involving manipulations of safety behaviors and of attention. Treatment sessions 4–6 typically focus on a continuation of behavioral experiments, often involving exposure to test negative appraisals and predictions, and video feedback methods to correct the distorted self-image. Sessions 7–9 continue with cognitive and behavioral reattribution methods, and introduce bandwidth maneuvers aimed at further interrogating the environment and discovering that social catastrophes (e.g., everyone staring at you) are unlikely, even in the event of failed performance. Finally, sessions 10–12 involve consolidation of material learned, relapse prevention, and a continuation of work on the remaining issues (i.e., residual negative beliefs and avoidance). Clearly, there is flexibility in the number of sessions devoted to these phases of treatment, but it serves here to provide a basic conceptual structure for planning specific interventions. Formulation In the following, we present a fictional but realistic case of Jenny to illustrate the process from assessment to case formulation and socialization. First, we provide some background information about Jenny. Background Information Jenny is a single, 32-year-old architect with no children. After graduating from university three years ago, Jenny moved to a new city a long way from her family and childhood friends to work for a medium-sized construction company. This was a large step for Jenny as she had always been a cautious person and most comfortable in safe and well-known surroundings. However, the construction company had a great reputation, and Jenny was excited that she was offered a job there as a newly qualified architect. After three years in the city, Jenny did not know anyone outside work, and she rarely spent time with colleagues outside the office. Most of her spare time was spent going for walks, doing yoga, or just sitting in front of the TV. Jenny felt lonely and depressed, and she also struggled at work. She very much enjoyed working by herself on, for example, designing houses, but she found teamwork challenging as it nearly always had her feel very anxious; she avoided eating lunch with her colleagues; and she hated attending meetings and other formal settings. Sometimes CBT for Social Anxiety Disorder Jenny found it difficult to ask her manager for help, even when she needed supervision to do her job effectively. On some occasions, typically before meetings where she had to present some of her design drawings to several spectators, Jenny would drink wine before presenting. During the past three years, Jenny had been on several periods of short-term sick leave due to depression and fatigue, and her general practitioner had prescribed antidepressant medications that had helped somewhat. However, in her latest encounter with her general practitioner, Jenny agreed to be referred to a mental health professional for assessment and treatment as the problems with depression and fluctuating work performance endured. Jenny’s therapist initially conducted a standardized diagnostic interview and concluded that Jenny met the diagnostic criteria for social anxiety disorder and recurrent depressive disorder. Jenny reported avoidance of performance situations and concerns about being negatively evaluated since adolescence. She agreed with the therapist that depression would be less of a problem if she could have a richer social life and be more relaxed when interacting with others during the work day. The therapist questioned Jenny about her worst fears in social situations at work. The main problem as Jenny saw it was trembling in her whole body and in her voice, and she was certain that others would think she was a stupid and weak person if they noticed it. Therefore, she avoided as many performance situations as she could. However, when she was left with no choice other than confronting her feared situations, Jenny reported that she tried to control her body and voice with the aim of concealing her anxiety. Eliciting Information for Case Formulation When working with SAD, there are two basic approaches that can be used to elicit data for conceptualization. The first option is reviewing one or more recent episodes in which the patient felt socially anxious by direct questioning. However, for some individuals where avoidance of feared situations is a prominent problem, it might be necessary to conduct a behavioral assessment test where the individual is exposed to a feared situation constructed in session. Depending on the nature of the patient’s fear, this will typically involve introducing a type of performance situation for the patient such as making conversation with a stranger. For an example of a behavior test to elicit data for conceptualization, the reader can consult Wells (1997, p. 180). Four types of information are required to make an idiosyncratic case formulation. The therapist aims to identify (1) main negative automatic thoughts, (2) anxiety symptoms, (3) contents of self-consciousness/inner image, and (4) safety behaviors. Negative Automatic Thoughts. Negative automatic thoughts occur in anticipation of and within social situations. Two types of content are relevant to problem maintenance: (1) the meaning and significance that other people might attach to symptoms and (2) an individual’s own appraisal of the significance of symptoms such as overestimation of conspicuousness and implications for self-concept. Useful questions to elicit negative automatic thoughts include (1) “What were you thinking before you entered the situation/in the situation/when you noticed symptom X?” 123 124 Henrik Nordahl and Adrian Wells (2) “What was the worst you thought could happen in the situation?” and (3) “What did you think people would think or see?” Anxiety Symptoms. Anxiety takes the form of cognitive and somatic symptoms. They are maintained by negative appraisals, but are also a focus of negative appraisals. Individuals with SAD are often most troubled by symptoms that can be witnessed by others, such as shaking, sweating, blushing, crying, or their mind going blank. In constructing the idiosyncratic formulation, it is useful to determine the extent to which appraisals of symptoms contribute to negative automatic thoughts and dysfunctional self-processing. The following questions can be used: (1) “Which symptoms bother you most?” (2) “When you felt anxious in the situation, what symptoms did you notice?” (3) “How conspicuous do you think the symptoms are?” and (4) “If people did notice your symptoms what would that mean?” Contents of Self-Processing. There are three main ways to explore the content of an individual’s self-processing: (1) exploring the content of heightened selfconsciousness, (2) questioning the appraised level of conspicuousness of symptoms, and (3) determining if safety behaviors are linked to a particular self-perception. The initial marker for self-processing in patients’ accounts of situations is a report of increased self-consciousness. The therapist should specifically ask about the point in time at which the patient became highly self-conscious, either through direct exploration of the content of processing in this state (e.g., “What aspect of yourself were you most aware of?”) or by questioning the subjective impression of the self for periods when symptoms were intense (e.g., “When you felt anxious, how do you think you appeared?”). Moreover, some patients utilize safety behaviors to conceal symptoms, and this provides an opportunity to determine the content of selfperception in two ways: (1) explore self-processing associated with implementing safety behaviors (e.g., “When you try to conceal your symptoms, what is your impression of how you look to others?”) and (2) explore self-processing in the hypothetical absence of safety behaviors (e.g., “If you did not engage in your safety behavior when you felt anxious, how would you look to others then?”). It is important to try to determine the content of self-processing in as detailed and precise a way as possible, and the therapist should ask about imagery, as the selfimpression often occurs as an image from the “observer perspective” (e.g., “Did you have an image of the way you thought you looked when you were in the situation? Can you describe the image”?). Safety Behaviors. Safety behaviors can be overt or covert. It is important that the therapist works to elicit all kinds of safety behaviors, which can be a challenge when there is low awareness by the patient. In addition to questioning about safety behaviors, exposure to feared situations in conjunction with questioning from the therapist may be warranted. Examples of typical question to elicit safety behaviors are: (1) “When you thought (feared event) was happening, did you do anything to prevent it?” (2) “Do you do anything to control your symptoms/improve your performance/hide your problem?” and (3) “Do you do anything to avoid drawing attention to yourself?” CBT for Social Anxiety Disorder Collecting Data for Jenny’s Formulation In the case of Jenny, reviewing a recent episode of social anxiety was chosen to elicit data for her idiosyncratic case formulation. Below we have provided a description of the conversation between Jenny and her therapist from the process of generating her formulation. The formulation arising from the dialogue is presented in figure 2. Therapist: Jenny: Therapist: Jenny: Therapist: Jenny: Therapist: Jenny: Therapist: Jenny: Therapist: Jenny: Therapist: Jenny: Therapist: Jenny: Therapist: Jenny: Therapist: In today’s session, I would like to explore a recent social situation in which you felt anxious and uncomfortable. In doing this we can explore factors that are keeping your social anxiety going and begin to examine ways that you can overcome your anxiety. When was the last time you were anxious and distressed in a social situation? It was on Monday. I went to a meeting with two of my colleagues to talk to some customers about a new project. I am going to ask you some questions about your feelings and thoughts in that situation. Is it clear in your memory? Yes. Just before you went to the meeting, were you feeling anxious? Very much so, I did not really want to go, but it was an important meeting and I did not want to let my colleagues down. What were your anxious thoughts? I was worried that I had to take the lead in the conversation, and that my anxiety would lead to trembling in my voice and body. I do not want others to see me shaking and being anxious for nothing. So, your thoughts were something like “What if I shake and everybody will notice?” Is that right? Yes, that is right. When you entered the situation, how did you feel? I felt anxious, tense, hot, and shaky. When you felt anxious in that situation, what thoughts went through your mind? I thought, “They will notice the shaking and think I am an incompetent person.” It sounds like you think others will perceive you as an incompetent person if they saw you shaking. How conspicuous do you think your symptoms are? I think it is quite easy to notice that I am nervous and uncomfortable. If I could have seen you in that meeting, what would I see? You would see a shivering wreck. It felt like my whole body was shaking. When you felt that your whole body was shaking, did you do anything to prevent it? 125 126 Henrik Nordahl and Adrian Wells Situation: Meeting at work NAT: “They will notice the shaking and think I am an incompetent person” Self-Conscious Image of self as a “shivering wreck” Safety Behaviors Tense legs Hide arms Deep breaths Control shaking Say little Anxiety Anxious Tense Hot Shaky Figure 7.2. An idiosyncratic SAD case conceptualization for Jenny. Jenny: Therapist: Yes, I tried to tense my legs to control the shaking. I hid my arms behind my back, and I took deep breaths to calm down. I usually say very little to avoid attracting attention. Thank you for answering these questions, Jenny. Now, let us have a look together at a diagram [Figure 7.2] I have mapped out to see some important factors and cycles that help us understand the causes of your anxiety problem. Socialization When the idiosyncratic formulation has been developed, the therapist presents the model using guided discovery to begin to share an understanding of the factors maintaining the problem. A goal in the socialization process is to engage the patient in the treatment and to demonstrate that social anxiety is linked to negative selfevaluation based on internal information. In particular, the effect of self-focused attention and use of safety behaviors on symptoms and performance is discussed and illustrated by in-session experiments. Behavioral Experiments in Socialization Typically, a socialization experiment involves social performance under two conditions where the engagement in and disengagement from safety behaviors and/or CBT for Social Anxiety Disorder self-focused attention are contrasted. The first condition usually involves full engagement in self-focus/safety behaviors, and this is followed by a second condition where the patient is instructed to reduce these strategies as much as possible. Several socialization experiments are usually required in order to demonstrate the key elements in the model and the interactions between them. For examples and further discussion, the reader should consult Wells (1997). In the case of Jenny, one of the socialization experiments aimed to explore the effects of her safety behaviors. She was asked to participate in two interactions with a small group of the therapist’s colleagues. In the first interaction, Jenny was instructed to engage all of her typical safety behaviors (e.g., tensing her legs, hiding her arms, taking deep breaths, trying to control shaking, and saying little). In the second interaction, Jenny was instructed to drop all safety behaviors, and focus attention externally on other people in the situation. When the two conditions were contrasted with appropriate questioning by the therapist, Jenny discovered that her self-consciousness was greater and her trembling more noticeable in the first condition. She also felt more at ease in the second condition and experienced that participating in the conversation felt more natural. The experiment had the effect that Jenny was more curious about the role of safety behaviors and self-attention; this increased her motivation for therapy and to reduce these responses. Modifying Self-Processing with Video Feedback Following socialization and successful work in reducing safety behaviors, the next stage of treatment consists of modifying the content of self-processing, as it is the main source of evidence used by the socially anxious individual to make negative self-appraisals and inferences about the content of other people’s appraisals. Video feedback provides an effective technique for correcting distorted self-images and beliefs concerning the conspicuousness of anxiety symptoms, and can help patients obtain a more realistic view of how they appear to other people. This procedure should be managed in a particular way to prohibit adverse effects and maximize change in self-image and negative beliefs. Clinical guidelines detailing a range of procedures for successful implementation of the procedure have been published elsewhere (Warnock-Parkes et al., 2017; Wells, 1997). Video feedback can be used in a variety of different ways during a course of CBT for SAD. Normally, a video of the behavioral experiment with two contrasting conditions is used as part of the socialization process where the patient likely experienced high levels of anxiety as described above. This experiment was originally set up to evaluate the effect of self-focused attention and safety behaviors, and patients usually discover that they feel less anxious and think they came across more favorably in the second condition. In the case of Jenny, watching the videos helped her discover that her trembling was barely noticeable and that she came across more favorably in both conditions than she thought. For Jenny, this insight meant that her feelings are not a reliable judge of how she appears to others and that even when 127 128 Henrik Nordahl and Adrian Wells feeling shaky it is barely noticeable to others. In addition, Jenny realized that the safety behavior of tensing her legs likely contributed to the felt shakiness. Verbal Reattribution Throughout therapy, verbal reattribution techniques are used with a view to modifying negative self-appraisals and thoughts concerning other people’s reactions and thoughts in social situations. In addition to video feedback, there are several strategies that can be used for challenging the patient’s belief in their negative automatic thoughts, of which we present some of the most commonly used techniques here. Questioning the Evidence A typical strategy to use is to review the evidence that the socially anxious individual has for their belief. A central aim in doing so is to help the patient discover that the evidence mostly stems from internal information such as feelings/symptoms and self-appraisal rather than objective sources. Thinking Errors Educating patients to identify thinking errors is a good approach as a means of helping the patient gaining distance from their negative appraisals and objectively evaluating their validity. Common thinking errors in SAD include mind reading (e.g., “She thinks I am stupid”), catastrophizing (e.g., “I won’t be able to say anything”), and personalization (e.g., “No one is talking to me because I am boring”). Some also engage in an error of projected self-appraisal (Wells, 1997) in which they assume their own negative beliefs are held by others (e.g., “I sound really boring; they must think I am boring”). Dealing with Anticipatory Processing and the Post-mortem These cognitive types of safety behaviors are typically dealt with by asking patients to ban or reduce the time spent on these processes. To make this easier for the patient, an analysis of the advantages and disadvantages of such processing is usually undertaken with the aim to show how the disadvantages outweigh the advantages. In the case of Jenny, her therapist made a list of all the advantages and disadvantages of planning what to say (i.e., anticipatory processing) that Jenny could think of. According to Jenny, the advantage with this coping strategy was that it could help her come across as a competent person. The disadvantage was that she became more self-focused and anxious when engaging in this strategy. In addition, Jenny’s therapist helped her see other disadvantages with using the strategy, for example, that her planning seldom fitted with how meetings and conversations actually turn out and that the strategy had not helped her overcome her social anxiety problem. In reviewing the advantages and disadvantages, Jenny concluded that the disadvantages by far outweighed the advantages and that anticipating potential negative social consequences contributed to her social anxiety problem. CBT for Social Anxiety Disorder She agreed to ban the activity as homework and to spend time on evaluating her experiences from this in the next treatment session. Using Rational Self-Statements When more rational statements have been generated and/or validated by verbal retribution and behavioral strategies during the course of treatment, these can be used as self-statements in feared situations as a means of preventing full activation of self-processing and of maintaining stability of the self-concept. For example, Jenny was instructed to use a rational self-statement (“I look calm even when I don’t feel it”) based on corrective video feedback in challenging social situations. Behavioral Experiments Behavioral experiments consisting of exposure to social situations with concurrent dropping of safety behaviors and processing of external information are a crucial component of CBT for SAD. They complement verbal reattribution procedures and provide one of the most powerful means of modifying distorted appraisals and beliefs by enabling testing of other people’s reactions and by evaluating the consequences of showing signs of anxiety or failed performance in feared social situations. We recommend implementing behavioral experiments in accordance with the P-ET-S protocol described by Wells (1997), which consists of four phases: (1) preparation (P), (2) exposure to social situations (E), (3) testing the predictions based on negative beliefs (T), and (4) a final summarizing (S) of the results. Examples of test (T) phases in such experiments include deliberately focusing on other people to determine their reactions, dropping safety behaviors, deliberately showing signs of anxiety, producing “failures in performance,” or behaving in an “unacceptable” manner and observing if predicted outcomes occur. Such testing usually requires that the patient maintain an external focus of attention as a means to gather objective information about other people’s reactions. After the testing phase, the experiences are interpreted and summarized in light of the cognitive formulation, and belief in negative thoughts and predictions is reassessed in light of these results. Experiments conducted in session are normally repeated for homework in order to test the predictions in more naturalistic settings for the patients with means to further challenge negative thoughts and beliefs. In the case of Jenny, she did an experiment in a meeting at work where she deliberately shook her arms while carefully observing her colleagues’ reactions. To her surprise, Jenny discovered that only one of her colleagues noticed, but this person did not seem to react to it in any negative may. This discovery was used by the therapist to help Jenny discover that even in the event of “failed performance,” strong negative reactions from others are unlikely. Dealing with Underlying Assumptions and Beliefs In the Clark and Wells model, individuals with SAD hold underlying negative assumptions and beliefs (“schemas”) that are activated when entering or 129 130 Henrik Nordahl and Adrian Wells anticipating a social situation and contribute to negative appraisals of social situations and the vicious cycle that maintains SAD. These schemas can be divided into conditional assumptions, unconditional beliefs about the social self, and high standards and rules for social performance, and should be addressed and modified in the later stages of the treatment. To accomplish this successfully, it is important to generate a clear definition of concepts represented in the assumptions and to operationalize them in a testable format. A good strategy in working with conditional assumptions is to review evidence and counterevidence for the assumptions, as individuals with SAD often fail to process disconfirmatory information. This can be followed up with a mini-survey to gather information about other people’s thoughts and beliefs, and it may be useful to run behavioral experiments to test the validity of the assumption. When the therapist aims to modify high standards and rigid rules for social performance, it is useful to explore the effects of behaving in ways that break these personal rules. For example, the patient may be asked to deliberately “make mistakes” or spill a drink in a social situation to test the reactions of others. With unconditional negative self-beliefs, which often consist of dichotomous concepts, continua work offers a means of introducing a more nuanced perspective on the self. The positive data log and flashcards provide a means of accumulating evidence in support of replacement positive beliefs with the aim of counteracting negative cognitive bias in feared situations. In some cases, identifying early events and images that might explain how a negative self-belief arose can also be helpful, and either encouraging the patient to treat their negative self-beliefs as prejudice against themselves or using elements from trauma interventions such as exposure or memory rescripting to process the traumatic event and thus overcome the negative belief. Relapse Prevention Toward the end of therapy, a central part of the treatment is relapse prevention. Patients are typically asked to write a detailed summary of the information learned during the course of treatment, a task that the therapist should supervise to make sure most of the important learning points and experiences are included. In addition, several examples of the patient’s formulation that highlight the more specific components responsible for maintaining social anxiety are included in the summary. It is also typical to include a list of strategies that have been used in overcoming social anxiety. Furthermore, booster sessions are normally scheduled at two and six months after treatment and provide an opportunity to consolidate treatment gains and reinforce the implementation of treatment strategies. Recent Developments and Advances Although it has been nearly 25 years since the Clark and Wells model and the treatment derived from it was published, it is still considered the benchmark model CBT for Social Anxiety Disorder and treatment of SAD. In more recent years, treatment based on the model has successfully been adapted to children and adolescents (Ingul et al., 2014; Leigh & Clark, 2016, 2018) and to different formats such as delivery through the Internet (see Carlbring et al., 2018, for a review of controlled trials) with promising results. A Return to Theoretical Influences: The Metacognitive Approach. A conceptual feature of the Clark and Wells model (1995) is that it draws on different theoretical frameworks in an integrative way that may create upper limits to what can be achieved. For example, it places the content of cognition in center stage and argues that schemas or negative beliefs give rise to self-processing and social anxiety. However, the S-REF model (Wells & Matthews, 1994) that partially informed its development emphasizes the failure to adaptively regulate processing such as worry and attention as the main features of disorder. This effect is thought to emerge from metacognitive beliefs, and together these are the targets of metacognitive therapy (Wells, 2009). In line with this idea, recent studies have shown that metacognitive (e.g., “I cannot control my worry”) rather than cognitive beliefs (e.g., “I am boring”) are more reliable predictors of social anxiety (Gkika et al., 2017; Nordahl & Wells, 2017). Moreover, change in metacognitive rather than cognitive beliefs is associated with symptom improvement in individuals undergoing treatment for SAD (Nordahl et al., 2017). Metacognitive but not cognitive beliefs are statistical predictors of depression symptoms in patients with SAD (Nordahl et al., 2018), and of work status among high socially anxious individuals (Nordahl & Wells, 2017). Two studies (Nordahl et al., 2016; Wells & Papageorgiou, 2001) have shown that a briefer and more metacognitive-focused intervention can be highly effective and time efficient for patients with SAD. Furthermore, Vogel and colleagues (2016) isolated and tested two techniques: the attention training technique (ATT: Wells, 1990) and situational attentional refocusing (SAR: Wells & Papageorgiou, 1998) often used in metacognitive therapy applications, and found that 46% of patients no longer met diagnostic criteria for SAD after receiving them. Nordahl and Wells (2018) have presented preliminary evidence suggesting that full metacognitive therapy is associated with positive outcomes for patients with different presentations of SAD. These emerging data support the idea that moving toward a greater metacognitive-focused implementation of treatment may contribute positively to further treatment developments. Key Points Social anxiety disorder (SAD) is among the most common mental disorders, with a lifetime prevalence of approximately 12%. Building on Beck’s schema theory (Beck, 1976) and the self-regulatory executive function model of psychological disorder (Wells & Matthews, 1994), Clark and Wells (1995) advanced a cognitive model of SAD. The cognitive model emphasizes schemas/negative automatic thoughts, selfattention, and safety behaviors as the key maintenance factors of social anxiety. 131 132 Henrik Nordahl and Adrian Wells (cont.) Wells (1997) developed the CBT manual for SAD based on the Clark and Wells (1995) model. Individual CBT is considered the most efficacious treatment of SAD and is recommended as the treatment of choice in NICE guidelines. Refinements of the model and treatment may be possible, as shown by recent research on metacognitive factors. RECOMMENDED READING Clark, D. M., & Wells, A. (1995). A cognitive model of social phobia. In R. G. Heimberg, M. R. Liebowitz, D. A. Hope, & F. R. Schneier (Eds.), Social phobia: Diagnosis, assessment, and treatment (pp. 69–93). Guilford Press. Mayo-Wilson, E., Dias, S., Mavranezouli, I., Kew, K., Clark, D. M., Ades, A. E., & Pilling, S. (2014). Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. The Lancet Psychiatry, 1, 368–376. Wells, A. (1997). Cognitive therapy of anxiety disorders: A practice manual and conceptual guide. John Wiley & Sons. (2007). Cognition about cognition: Metacognitive therapy and change in generalized anxiety disorder and social phobia. Cognitive and Behavioral Practice, 14, 18–25. (2009). Metacognitive therapy for anxiety and depression. Guilford Press. REFERENCES American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. Baker, S. L., Heinrichs, N., Kim, H. J., & Hofmann, S. G. (2002). The Liebowitz social anxiety scale as a self-report instrument: A preliminary psychometric analysis. Behaviour Research and Therapy, 40, 701–715. Beck, A. T. (1976). Cognitive therapy and the emotional disorders. International Universities Press. Borge, F. M., Hoffart, A., Sexton, H., Clark, D. M., Markowitz, J. C., & McManus, F. (2008). Residential cognitive therapy versus residential interpersonal therapy for social phobia: A randomized clinical trial. Journal of Anxiety Disorders, 22, 991–1010. Brown, T. A., & Barlow, D. H. (2014). Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5L): Lifetime Version. Client interview schedule. Oxford University Press. Brown, T. A., Di Nardo, P. A., & Barlow, D. H. (1994). Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV). Psychological Corporation. Carlbring, P., Andersson, G., Cuijpers, P., Riper, H., & Hedman-Lagerlöf, E. (2018). Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: An updated systematic review and meta-analysis. Cognitive Behaviour Therapy, 47, 1–18. Connor, K. M., Davidson, J. R., Churchill, L. E., Sherwood, A., Weisler, R. H., & Foa, E. (2000). Psychometric properties of the Social Phobia Inventory (SPIN): New self-rating scale. The British Journal of Psychiatry, 176, 379–386. Clark, D. M., Butler, G., Fennell, M., Hackmann, A., McManus, F., & Wells, A. (1995). Social behaviour questionnaire [Unpublished manuscript]. CBT for Social Anxiety Disorder Clark, D. M., Ehlers, A., Hackmann, A., McManus, F., Fennell, M., Grey, N., . . . & Wild, J. (2006). Cognitive therapy versus exposure and applied relaxation in social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 74, 568–578. Clark, D. M., Ehlers, A., McManus, F., Hackmann, A., Fennell, M., Campbell, H., . . . & Louis, B. (2003). Cognitive therapy versus fluoxetine in generalized social phobia: A randomized placebo-controlled trial. Journal of Consulting and Clinical Psychology, 71, 1058–1067. Clark, D. M., & Wells, A. (1995). A cognitive model of social phobia. In R. G. Heimberg, M. R. Liebowitz, D. A. Hope, & F. Schneier (Eds.), Social phobia: Diagnosis, assessment, and treatment (pp. 69–93). Guilford Press. Connor, K., Davidson, J., Churchill, L., Sherwood, A., Weisler, R., & Foa, E. (2000). Psychometric properties of the Social Phobia Inventory (SPIN): New self-rating scale. British Journal of Psychiatry, 176(4), 379–386. doi:10.1192/bjp.176.4.379 Davidson, J. R., Miner, C. M., De Veaugh-Geiss, J., Tupler, L. A., Colket, J. T., & Potts, N. L. S. (1997). The brief social phobia scale: A psychometric evaluation. Psychological Medicine, 27, 161–166. Fenigstein, A., Scheier, M. F., & Buss, A. H. (1975). Public and private self-consciousness: Assessment and theory, Journal of Consulting and Clinical Psychology, 43(4), 522–527. First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. (1996). User’s guide for the Structured Clinical Interview for DSM-IV axis I disorders. SCID-I: Clinician version. American Psychiatric Publishing. First, M. B., Williams, J. B. W., Karg, R. S., & Spitzer, R. L. (2015). Structured clinical interview for DSM-5: Research version (SCID-5 for DSM-5, research version; SCID-5RV). American Psychiatric Association. Gkika, S., Wittkowski, A., & Wells, A. (2017). Social cognition and metacognition in social anxiety: A systematic review. Clinical Psychology & Psychotherapy, 25, 10–30. Gregory, B., & Peters, L. (2017). Changes in the self during cognitive behavioural therapy for social anxiety disorder: A systematic review. Clinical Psychology Review, 52, 1–18. Hinrichsen, H., & Clark, D. M. (2003). Anticipatory processing in social anxiety: Two pilot studies. Journal of Behavior Therapy and Experimental Psychiatry, 34, 205–218. Ingul, J. M., Aune, T., & Nordahl, H. M. (2014). A randomized controlled trial of individual cognitive therapy, group cognitive behaviour therapy and attentional placebo for adolescent social phobia. Psychotherapy and Psychosomatics, 83, 54–61. Leichsenring, F., Salzer, S., Beutel, M. E., Herpertz, S., Hiller, W., Hoyer, J., . . . & Ritter, V. (2013). Psychodynamic therapy and cognitive-behavioral therapy in social anxiety disorder: A multicenter randomized controlled trial. American Journal of Psychiatry, 170, 759–767. Leigh, E., & Clark, D. M. (2016). Cognitive therapy for social anxiety disorder in adolescents: A development case series. Behavioural and Cognitive Psychotherapy, 44, 1–17. (2018). Understanding social anxiety disorder in adolescents and improving treatment outcomes: Applying the cognitive model of Clark and Wells (1995). Clinical Child and Family Psychology Review, 21, 388–414. Liebowitz, M. R. (1987). Social phobia. In D. F. Klein (Ed.), Anxiety. Karger, 141–173. Mattick, R. P., & Clarke, J. C. (1998). Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy, 36, 455–470. Mayo-Wilson, E., Dias, S., Mavranezouli, I., Kew, K., Clark, D. M., Ades, A. E., & Pilling, S. (2014). Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. The Lancet Psychiatry, 1, 368–376. 133 134 Henrik Nordahl and Adrian Wells Mörtberg, E., Clark, D. M., Sundin, Ö., & Åberg Wistedt, A. (2007). Intensive group cognitive treatment and individual cognitive therapy vs. treatment as usual in social phobia: A randomized controlled trial. Acta Psychiatrica Scandinavica, 115, 142–154. National Institute for Health and Care Excellence. (2013). Social anxiety disorder: recognition, assessment and treatment of social anxiety disorder (Clinical guideline 159). http:// guidance.nice.org.uk/CG159 Ng, A. S., Abbott, M. J., & Hunt, C. (2014). The effect of self-imagery on symptoms and processes in social anxiety: A systematic review. Clinical Psychology Review, 34, 620–633. Nordahl, H., Nordahl, H. M., Hjemdal, O., & Wells, A. (2017). Cognitive and metacognitive predictors of symptom improvement following treatment of social anxiety disorder: A secondary analysis from a randomized controlled trial. Clinical Psychology and Psychotherapy, 24(6), 1221–1227. Nordahl, H., Nordahl, H. M., Vogel, P. A., & Wells, A. (2018). Explaining depression symptoms in patients with social anxiety disorder: Do maladaptive metacognitive beliefs play a role? Clinical Psychology and Psychotherapy, 25, 457–464. Nordahl, H. M., Vogel, P. A., Morken, G., Stiles, T. C., Sandvik, P., & Wells, A. (2016). Paroxetine, cognitive therapy or their combination in the treatment of social anxiety disorder with and without avoidant personality disorder: A randomized clinical trial. Psychotherapy and Psychosomatics, 85, 346–356. Nordahl, H. M., & Wells, A. (2017). Social anxiety and work status: The role of negative metacognitive beliefs, symptom severity and cognitive-behavioural factors. Journal of Mental Health, 29(6), 665–669. (2018). Metacognitive therapy for social anxiety disorder: An A-B replication series across social anxiety subtypes. Frontiers in Psychology, 9, 540. Piccirillo, M. L., Dryman, M. T., & Heimberg, R. G. (2015). Safety behaviors in adults with social anxiety: Review and future directions. Behavior Therapy, 47, 675–687. Rachman, S., Grüter-Andrew, J., & Shafran, R. (2000). Post-event processing in social anxiety. Behaviour Research and Therapy, 38, 611–617. Ruscio, A. M., Brown, T. A., Chiu, W. T., Sareen, J., Stein, M. B., & Kessler, R. C. (2008). Social fears and social phobia in the USA: Results from the National Comorbidity Survey Replication. Psychological Medicine, 38, 15–28. Scheier, M. F., & Carver, C. S. (1985). The Self-Consciousness Scale: A revised version for use with general populations. Journal of Applied Social Psychology, 15, 687–699. Stangier, U., Heidenreich, T., Peitz, M., Lauterbach, W., & Clark, D. M. (2003). Cognitive therapy for social phobia: Individual versus group treatment. Behaviour Research and Therapy, 41, 991–1007. Stangier, U., Schramm, E., Heidenreich, T., Berger, M., & Clark, D. M. (2011). Cognitive therapy vs interpersonal psychotherapy in social anxiety disorder: A randomized controlled trial. Archives of General Psychiatry, 68, 692–700. Turner, S. M., Beidel, D. C., Dancu, C. V., & Stanley, M. A. (1989). An empirically derived inventory to measure social fears and anxiety: The Social Phobia and Anxiety Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 1, 35–40. Vogel, P. A., Hagen, R., Hjemdal, O., Solem, S., Smeby, M. C. B., Strand, E. R., Fisher, P., Nordahl, H. M., & Wells, A. (2016). Metacognitive therapy applications in social phobia: An exploratory study of the individual and combined effects of the attention training technique and situational attentional refocusing. Journal of Experimental Psychopathology, 7, 608–618. Wampold, B. E., Flückiger, C., Del Re, A. C., Yulish, N. E., Frost, N. D., Pace, B. T., . . . & Hilsenroth, M. J. (2017). In pursuit of truth: A critical examination of meta-analyses of cognitive behavior therapy. Psychotherapy Research, 27, 14–32. CBT for Social Anxiety Disorder Warnock-Parkes, E., Wild, J., Stott, R., Grey, N., Ehlers, A., & Clark, D. M. (2017). Seeing is believing: Using video feedback in cognitive therapy for social anxiety disorder. Cognitive and Behavioral Practice, 24, 245–255. Watson, D., & Friend, R. (1969). Measurement of social-evaluative anxiety. Journal of Consulting and Clinical Psychology, 33, 448–457. Wells, A. (1990). Panic disorder in association with relaxation induced anxiety: An attentional training approach to treatment. Behavior Therapy, 21, 273–280. (1997). Cognitive therapy of anxiety disorders: A practice manual and conceptual guide. John Wiley & Sons. (2009). Metacognitive therapy for anxiety and depression. Guilford Press. Wells, A., Clark, D. M., & Ahmad, S. (1998). How do I look with my mind’s eye?: Perspective taking in social phobic imagery. Behaviour Research and Therapy, 36, 631–634. Wells, A., & Matthews, G. (1994). Attention and emotion: A clinical perspective. Erlbaum. Wells, A., & Papageorgiou, C. (1998). Social phobia: Effect of external attention on anxiety, negative beliefs and perspective taking. Behavior Therapy, 29, 357–370. (2001). Brief cognitive therapy for social phobia: A case series. Behaviour Research and Therapy, 39, 713–720. Wells, A., Stopa, L., & Clark, D. M. (1993). Social cognition questionnaire [Unpublished manuscript]. Department of Psychiatry, University of Oxford, Warnerford Hospital. Wittchen, H. U., & Fehm, L. (2003). Epidemiology and natural course of social fears and social phobia. Acta Psychiatrica Scandinavica, 108, 4–18. Wong, Q. J., Gregory, B., & McLellan, L. F. (2016). A review of scales to measure social anxiety disorder in clinical and epidemiological studies. Current Psychiatry Reports, 18, 38–53. Wong, Q. J., & Moulds, M. L. (2009). Impact of rumination versus distraction on anxiety and maladaptive self-beliefs in socially anxious individuals. Behaviour Research and Therapy, 47, 861–867. Wong, Q. J., Moulds, M. L., & Rapee, R. M. (2014). Validation of the self-beliefs related to social anxiety scale: A replication and extension. Assessment, 21, 300–311. 135 8 CBT for Somatic Symptom Disorder and Illness Anxiety Disorder Lillian Reuman and Jonathan S. Abramowitz Introduction According to the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; American Psychiatric Association, 2013), the essential feature of somatic symptom disorder (SSD) and illness anxiety disorder (IAD) is a preoccupation with one or more physical symptoms that are attributed to a non-psychiatric disease. This preoccupation is often distressing and results in significant disruptions of daily life. For example, SSD or IAD may be characterized by worry about stomach pains that are not consistent with a medical diagnosis or by the persistent fear that frequent “chest tightening” is indicative of a heart attack despite no evidence of cardiac disease. This preoccupation is accompanied by inaccurate and persistent thoughts about the seriousness of the perceived symptoms, a high level of anxiety related to one’s health, and excessive time and energy devoted to thinking about or responding to the perceived symptoms and health concerns. Accordingly, an individual preoccupied with concerns about stomach pains or chest tightening may devote hours to researching medical treatments online, spend excessive amounts of money pursuing unnecessary medical tests and procedures, and enlist family members and doctors to provide reassurance regarding worrisome symptoms. In addition to maladaptive cognitions and unhelpful accompanying behaviors, bodily sensations play a large role in the development and maintenance of SSD. For example, physical discomfort or shifts in body sensations (internal triggers) are often interpreted as signs of serious disease (e.g., the sensations that accompany a headache indicate a brain tumor). Individuals may also experience anxiety as a result of external triggers (e.g., reading about an illness) that cue thoughts about one’s own risk of illness and selective attention to benign (yet perceptible) bodily perturbations. The emotional response of anxiety further evokes (or exacerbates) bodily sensations (e.g., racing heart) that may be misinterpreted as signs of serious illness. This perception of intensifying bodily sensations can then lead to a vicious cycle of selective attention toward the perceived threat, misinterpretation of the nature and severity of bodily sensations, and maladaptive coping. 136 CBT for Somatic Symptom Disorder and Illness Anxiety Disorder Somatic sensations may result from normal “bodily noise,” the experience of general stress (including stress related to worrying about one’s health), and a heightened awareness of the body. Given the conceptualization of SSD and IAD as conditions having to do with maladaptive thinking patterns and accompanying repetitive behaviors, the literature on the treatment of SSD and IAD supports the use of cognitive behavioral therapy (CBT) for reducing symptomatology and improving physical functioning and quality of life. In this chapter we summarize the research base for CBT for somatic concerns and provide a clinical guide to formulating, assessing, and implementing CBT for clients with such concerns. Clinical Case Formulation, Assessment, and Treatment Case Formulation and Treatment Implications The cognitive behavioral formulation of SSD/IAD explains why health-related anxiety persists despite no good evidence of ill health. This conceptualization includes environmental and learning factors, as well as a range of cognitive and behavioral mechanisms (Abramowitz & Braddock, 2008). From this perspective, dysfunctional beliefs about bodily sensations and illnesses (e.g., “My body is weak, and I am vulnerable to illness”) and the inability to tolerate uncertainty and anxiety (e.g., “Not having a guarantee about my health is unbearable”) increase the likelihood of catastrophic misinterpretations of benign bodily sensations and perturbations (i.e., normal “body noise”), as well as ambiguous health-related information, as indicators of illness. Such misinterpretations trigger anxiety, an increased sense of uncertainty, and increased vigilance for signs of illness, as well as the urge to gain assurances about health to reduce the subjective discomfort. The catastrophic misinterpretations are then maintained (despite contradictory information and repeated reassurance of good health from medical professionals) by maladaptive strategies used to cope with illness-related anxiety. These strategies include exaggerated attempts to prevent the feared illness or its consequences (e.g., staying near a hospital), avoidance (e.g., of triggers or illness cues), and attempts to attain certainty about health status (e.g., checking medical resources, body checking). Such safety behaviors prevent individuals with SSD/IAD from disconfirming their mistaken beliefs about being ill and learning that they can in fact manage uncertainty and anxiety. This approach to understanding SSD/IAD, which is partially derived from conceptualizations of other anxiety-related problems, provides the foundation for cognitive behavioral interventions discussed later in this chapter, which generally have the aim of helping the individual develop healthier responses to the ubiquitous internal and environmental cues, as well as uncertainty, related to one’s health. One such intervention is psychoeducation, which involves providing the individual with information about the nature of their presenting concerns and potential strategies for addressing them. Exposure and response prevention (ERP) is a set of procedures 137 138 Lillian Reuman and Jonathan S. Abramowitz used to help health anxious individuals confront fear triggers (external and internal) to learn that they can manage such cues, as well as the anxiety and uncertainty they provoke, without the use of safety behaviors or other strategies for trying to gain reassurance. In some instances, cognitive restructuring might be used to identify and challenge inaccurate beliefs about the meaning of bodily sensations. Assessment The cognitive behavioral model also informs what is necessary to assess when working with clients affected by SSD/IAD. We recommend using the following instruments and approaches to gain an understanding of SSD/IAD severity and related behavioral and cognitive features that will help inform a treatment plan and assess treatment response. The Yale-Brown Obsessive Compulsive Scale The Yale–Brown Obsessive Compulsive Scale (Y-BOCS; Goodman et al., 1989) is a semi-structured interview developed to assess obsessive-compulsive symptoms and also serves as a measure of illness anxiety severity. It includes 10 items (healthrelated thinking, items 1–5; compulsions, items 6–10) that assess the following five parameters: (a) time, (b) interference, (c) distress, (d) efforts to resist, and (e) perceived control. Each item is rated on a 0–4 scale, and the item scores are summed to produce a total score ranging from 0 (no symptoms) to 40 (extreme). Behaviors such as checking, reassurance seeking, or consulting with doctors are scored on the compulsions (safety behaviors) subscale. Scores of 0–7 represent subclinical symptoms, 8–15 represent mild symptoms, 16–23 relate to moderate symptoms, 24–31 suggest severe symptoms, and scores of 32 or greater imply extreme symptoms. The Short Health Anxiety Inventory The Short Health Anxiety Inventory (SHAI; Salkovskis et al., 2002) is an 18-item instrument that assesses health anxiety independent of physical health status. For each item the respondent chooses from a series of four statements (ranging in severity from 0 to 3) that best reflects their feelings over the past several months. Items address worry about health, awareness of bodily sensations and changes, and feared consequences of having an illness. The Cognitions about Body and Health Questionnaire The Cognitions about Body and Health Questionnaire (CBHQ; Rief et al., 1998) is a 31-item self-report scale that assesses various domains of exaggerated and dysfunctional cognitions and assumptions about illness, bodily sensations, and health habits. The respondent rates each item (e.g., “My body can tolerate a lot of strain”) on a four-point Likert scale ranging from 0 (completely wrong) to 3 (completely right). CBT for Somatic Symptom Disorder and Illness Anxiety Disorder Functional Assessment of Illness-Related Anxiety We also suggest collecting detailed, patient-specific information about internal and external health anxiety cues and behavioral responses to these cues. As indicated by the conceptualization described previously, the key domains to assess include the following. Bodily Signs, Sensations, and Perturbations. Signs and sensations might be internal but can also be associated with the skin, hair, or products that are expelled from the body (e.g., “Which bodily signs and sensations are you concerned with?”). External Situations and Stimuli. Such triggers often include hospitals, doctors, seeing or hearing about sick people, reading about illnesses, and other stimuli that serve as reminders of health concerns. Being alone or “too far” from a hospital or medical center can also be situational triggers, as can seeing oneself naked or giving oneself an examination (e.g., breast or testicular) (e.g., “What situations trigger your health-related thoughts and concerns?” “What situations do you avoid because they might trigger your health concerns?”). Misinterpretations of Bodily Signs and Sensations. Beliefs concerning the presence and meaning of unexpected, unwanted, or disconcerting bodily sensations are common. For example, patients may believe “When my head hurts, I think I’m getting a brain tumor” or “When I feel a lump in my throat, it reminds me that I have a serious neck problem that no doctors have been able to figure out.” Therapists should query, “What do you think this sensation means?” and “What do you worry is causing you to have this feeling?” Feared Consequences. Beliefs about the probability and severity of becoming ill or dying must be assessed. Some individuals have fears of explicit disastrous consequences, whereas for others, the internal and external cues evoke only a vague sense that “something is wrong.” Others fear they cannot tolerate uncertainty associated with their health (i.e., not having a 100% guarantee that they are not ill). Avoidance. Avoidance patterns (usually related to external triggers) might include staying away from hospitals, people with certain illnesses or diseases, funerals, or cemeteries, or avoiding disease-related movies, TV shows, news articles, or other information in the media. Such avoidance can often be predicted from external triggers and feared consequences. Therapists can ask, “What kinds of things do you not do because of your health concerns?” and “What situations do you routinely avoid?” Checking, Reassurance Seeking, and Other Safety Behaviors and Safety Signals It is important to assess body checking, which might include examination of the body’s vital signs (using medical equipment) or the structure and function of a particular body part (e.g., probing bodily orifices, smelling certain body parts or bodily excretions). Individuals might also perform other forms of checking and reassurance seeking, such as scheduling extraneous doctor visits, repetitively reviewing medical test results and reports, and searching the internet for information about diseases of concern. Furthermore, therapists ought to inquire about 139 140 Lillian Reuman and Jonathan S. Abramowitz other strategies the person engages in to reduce health-related anxiety or fear, for example, the use of a cane to avoid putting “too much stress” on one’s “rotting” legs or being sure to get exactly eight hours of sleep. Finally, safety signals are situations or objects that are associated with safety, such as cell phones, medications, and medical alert bracelets. Many individuals do not recognize these behaviors, situations, or objects as part of their problems with SSD or IAD. Questions to help elucidate safety behaviors and signals are: “Are there things you do to protect yourself from illnesses?” and “What precautions do you take so that you are prepared if you should have a medical emergency?” Illustration of Assessment and Case Formulation Theo, a 37-year-old accountant, noticed a small discoloration of the skin on his left shoulder. At his routine biyearly physical exam, he asked his physician to evaluate the skin mark for possible skin cancer. The doctor measured its diameter and told Theo she believed the mark was a solar lentigo, a benign discoloration of the skin caused by sun exposure. The doctor suggested Theo wear sunscreen with zinc oxide to help prevent additional sun damage and felt there was no need at that time to biopsy or remove the lentigo. Theo was initially relieved by this diagnosis, yet a few months later, he began thinking about it again when a family friend was diagnosed with skin cancer. Theo examined the skin mark in the mirror, and for a few weeks, took pictures of it and compared them to see whether the lentigo was growing. Although there did not seem to be any worsening, Theo became preoccupied with checking the lentigo every day. He rubbed and picked at it to see if it was raised and noticed that it seemed to be looking redder and “angrier.” He had the sensation that it was itchy and sore, and he found himself searching other parts of his body for more signs of skin cancer, from which Theo now believed he was suffering. Theo’s next step was to be evaluated by a dermatologist, who provided the same diagnosis of benign lentigo and suggested that no follow-up was necessary. The irritation, she suggested, was due to Theo’s persistent rubbing and picking of the area. But Theo continued to press the dermatologist for a biopsy “just to be sure.” After his pleas were denied several times, Theo took to searching the internet for information about skin cancer. Every day, he examined images of benign and malignant discolorations and growths. He spoke with his family and friends about their knowledge of skin cancer and frequently asked for reassurance that the problem was benign, never believing the feedback he received. He was losing sleep, his appetite was reduced, and he was spending more time reading about skin cancer than with his wife and two children. At that point, Theo’s wife encouraged Theo to talk with a mental health professional, which is how he ended up in our treatment clinic. Theo’s therapist used the cognitive-behavioral framework (1) to generate a formulation of Theo’s illness anxiety complaints and (2) to assess his concerns to further refine the formulation and develop a treatment plan. Numerous triggers and cues to Theo’s health concerns were present in his environment, including looking CBT for Somatic Symptom Disorder and Illness Anxiety Disorder at himself in the mirror, seeing spots on his skin, talking about cancer, and relating to his family friend with cancer. Theo’s belief that he had undiagnosed skin cancer was thought to lead to anxiety, which maintained his excessive health concerns by causing him to feel stressed and fatigued. Theo’s safety behaviors were conceptualized as natural responses to anxiety aimed at reducing distress and leading to some degree of certainty about the nature of his “symptoms.” These behaviors often resulted in temporary or short-lived reductions in anxiety. However, they ultimately maintained Theo’s health anxiety. For example, excessive body-checking led Theo to become sensitive to any changes on his skin; picking and rubbing led to irritation of the lentigo, which seemed to confirm (to Theo) that it was cancerous; and reassurance seeking always left some degree of ambiguity about the actual nature of the skin mark, thus sustaining the belief that he had been misdiagnosed. Theo’s score on the Y-BOCS was 28, indicating somewhat severe illness anxiety. His responses on the CBHQ indicated all-or-nothing beliefs about health and illness, such as the belief that good health means having no symptoms whatsoever. Finally, functional assessment led to identifying a list of illness anxiety triggers and additional safety behaviors that would need to be addressed in treatment. Cognitive Behavioral Therapy CBT for somatic-related anxiety is an active intervention that includes components of psychoeducation, cognitive therapy, self-monitoring, exposure and response prevention, and relapse prevention (e.g., Abramowitz & Braddock, 2008; Barlow, 2014). Numerous studies suggest that multicomponent CBT treatment packages involving between 12 and 20 treatment sessions are efficacious for somatic symptoms; however, not all patients respond equally, and some do not achieve improvement at all. The primary treatment components are described in the following sections. Psychoeducation Psychoeducation involves providing information about bodily symptoms, the development and maintenance of SSD/IAD, and a rationale for using CBT. Therapists can offer statistics about the prevalence of health anxiety (up to 25% of patients in some medical clinics; Tyrer et al., 2011), as this can help clients to recognize that they are not alone in their suffering. Clinicians should also share that symptoms of SSD exist along a continuum of severity ranging from mild to severe distress and impairment. This can help clients recognize that a mild degree of illness-related anxiety is normal and adaptive but that increased levels of concern are maladaptive and impairing. Within this conversation, the client and therapist can discuss the ways in which mild to moderate anxiety may be beneficial (i.e., anxiety may motivate an individual to act and alert us to danger), whereas severe levels of anxiety can be costly and debilitating. 141 142 Lillian Reuman and Jonathan S. Abramowitz Importantly, clinicians should educate clients about the aforementioned model of the maintenance of illness worry. Important points to convey include that dysfunctional beliefs about bodily symptoms and illness increase anxiety and worry. Once anxious about the possibility of acquiring an illness, the individual exhibits heightened awareness for any signs of illness and seeks to reduce their worry by gaining certainty about their health. Dysfunctional beliefs are maintained by maladaptive strategies used to cope with health-related anxiety, as we have discussed. Therapists, for example, can explain how avoidance of anxiety-provoking situations prevents the disconfirmation of feared consequences and how seeking reassurance from health-related websites strengthens fears about the situation. This information is best delivered in a collaborative, interactive approach, and the clinician should also check with the client to gauge their understanding of the model by asking questions such as, “Can you describe to me how this model applies to your situation?” Once clients have a grasp of the processes implicated in the development and maintenance of SSD, they should receive the rationale for CBT, which aims to modify unhelpful behavioral and thinking patterns that maintain SSD. Cognitive restructuring techniques are used to address catastrophic thinking and beliefs about the need for certainty. Behavioral methods include refraining from engaging in actions that provide temporary reassurance (e.g., seeking medical advice, browsing the internet) while engaging in activities that facilitate engagement with daily living (e.g., attending school/work, engaging in pleasurable activities). Psychoeducation is different from providing reassurance in that the individual is presented with new information, rather than the repeated presentation of old information (e.g., repeating assurances of good health, unnecessary medical tests to placate concerns). Therapists should also ask clients to identify the ways in which moderate levels of health-related anxiety can be normal, safe, and adaptive. By understanding that anxious responses are common, not dangerous, and adaptive, individuals may be more likely to proceed with treatment. Self-Monitoring Self-monitoring involves recording instances of body-related sensations, any external triggers, and accompanying emotions, cognitions, and behaviors as they occur in real time between therapy sessions. Self-monitoring not only helps increase awareness of such episodes and their antecedents and sequalae, but also aids in identifying treatment targets and detecting patterns between sensations, cognitions, and emotions. Cognitive Restructuring Cognitive restructuring involves the systematic use of Socratic questioning to help patients identify and challenge mistaken thoughts, beliefs, and assumptions about health, illnesses, and their external and internal cues (e.g., “Anxiety will harm me”; CBT for Somatic Symptom Disorder and Illness Anxiety Disorder “Doctors can’t be trusted”), to arrive at more useful, healthy, and empirically or logically consistent beliefs and assumptions (e.g., “I have been anxious many times in the past and it has never harmed me”; “Doctors are very knowledgeable, and I can generally trust them”). Exposure Therapy Aims of exposure therapy for SSD/IAD are to help the individual (1) modify exaggerated estimates of probability and severity of feared outcomes and (2) learn that anxiety and uncertainty are tolerable and do not have to interfere with functioning. Exposure is conducted both during the treatment session and for homework. A repetition of exposure exercises in a variety of contexts (e.g., location, time of day) is essential to promote generalization of learning (e.g., Craske et al., 2008). Three types of exposure are discussed in turn. Interoceptive Exposure As bodily sensations are often cues for illness anxiety, interoceptive exposure (IE) represents an important treatment strategy. IE involves deliberately and repeatedly producing feared bodily sensations, focusing on the sensations without trying to bring them to an end, and trying to maintain the sensations for a period of time (Walker & Furer, 2008). Two main goals of IE for SSD/IAD are (1) to increase acceptance of such sensations and (2) to decrease associated distress. Exercises such as spinning, hyperventilation, and breathing through a straw are common fearinducing strategies; for a complete list of suggestions, see Huppert and BakerMorissette (2003). Before beginning interoceptive exposure exercises, the clinician should conduct a thorough assessment to determine which bodily sensations are most anxietyprovoking and which interoceptive activities bring about feared sensations. For exposure to such bodily sensations, the clinician and client jointly and repeatedly practice the activity in session. Interoceptive exposure might be produced by having the patient hyperventilate, move vigorously (e.g., jumping jacks), or spin in an office chair. The therapist should demonstrate the activity, intensify the activity as needed, encourage the client to note their reactions, and debrief following the exposure. The therapist can coach the client to “lean in” to the feared body sensations, and practice observing them without trying to change them (Walker & Furer, 2008). The clinician should encourage repeated IE practice for extended periods of time between sessions in order to promote generalization of learning that such sensations are safe and tolerable. Imaginal Exposure Imaginal exposure for SSD/IAD usually entails writing scripts or creating images (e.g., of one’s death) based on the client’s somatic concerns. Exposure to such stories via writing, reading, and listening allows the client to experience feared situations (e.g., getting a cancer diagnosis) that cannot be accessed through in vivo 143 144 Lillian Reuman and Jonathan S. Abramowitz or interoceptive exposure. Imaginal exposure can also be used to amplify feelings of uncertainty about feared illnesses to help the client learn that uncertainty is manageable. In practice, the therapist guides the client in creating stories or images that are detailed and individually tailored to the client’s concerns. Next, the client focuses on the written or visual material (i.e., reread the story for an extended period of time) as a cue to vividly imagine the scenario and adds details as necessary to intensify the experience. The client may wish to record the reading to listen to the scenario repeatedly for homework practice. The therapist encourages the client to note physical and emotional discomfort that arises as a result of the imaginal exposure. To intensify the experience, imaginal exposure may be combined with IE. In Vivo Exposure In vivo exposure involves repeatedly and systematically facing a fear-provoking situation until the individual learns that (1) the situation or cue is safe, (2) they can tolerate the discomfort associated with the trigger, and (3) anxiety does not persist indefinitely or spiral out of control. For example, individuals may read stories (or obituaries) of individuals with chronic illness, watch medical documentaries that depict medical suffering and disability, or visit sites of painful physical memories (e.g., a chemotherapy center). The procedures for conducting exposure are described in detail elsewhere (e.g., Abramowitz et al., 2012). Response Prevention Response prevention entails voluntarily refraining from reassurance seeking and other anxiety-reducing (safety) behaviors both during and after exposure exercises. This technique is used so the individual with SSD/IAD can learn that safety behaviors are not necessary for safety and for anxiety tolerance and that, moreover, health anxiety subsides naturally, even when safety behaviors are not performed. Specific response prevention guidelines for the patient to follow can be determined collaboratively, and whereas some patients are able to immediately stop all checking, reassurance seeking, and other safety behaviors, others require a gradual approach. It is important to discuss the negative effects of checking, reassurance seeking, and other safety behaviors as well as the rationale for stopping them when implementing response prevention. Patients are often surprised at how much less attention they pay to their bodies when they do not engage in these maladaptive behaviors. Therapists can emphasize that refraining from safety behaviors is a difficult choice and can work with the client to define guidelines for response prevention. If relatives or friends are involved in the patient’s symptoms, such individuals are also encouraged to refrain from “helping” with the performance of safety behaviors. The patient is to record violations of response prevention on a symptom record and bring these to the therapist so that areas in need of additional attention can be CBT for Somatic Symptom Disorder and Illness Anxiety Disorder addressed. Violations of the response prevention plan can be self-monitored and addressed. The following are some examples of response prevention plans and strategies for various types of safety behaviors often observed in individuals with SSD/IAD. Body Checking Patients are not to check bodily signs (e.g., pulse) or levels (blood sugar), or the skin. Inspecting or scrutinizing body fluids and excreta (aside from a simple glance) is also prohibited. Reassurance Seeking Medical appointments for previously evaluated symptoms are off-limits. Any “new symptoms” can be discussed with the therapist, but no doctor visits are to occur. Telephoning medical personnel or “help lines” is off-limits. Internet searches for medical information are also prohibited. If the patient must be online for work or school, they should avoid medical websites. It may be helpful to ask a partner or relative to monitor internet use. Reviewing one’s own medical records is also prohibited. Patients are also not to ask for reassurance about health matters from friends and family members and are not to discuss symptoms with others (e.g., “I have had this headache for two days now”). We suggest helping the patient draft a letter to friends and relatives explaining the detrimental effects of reassurance seeking and providing suggestions for how to respond if asked for reassurance. For example, “I’m sorry but I can’t answer your question because I agreed to help you with treatment.” Mental Analyzing Patients are not to mentally devote time to going over what doctors have told them or trying to analyze situations related to their health. Instead, they should purposely imagine being uncertain (as in exposure). Dietary Restrictions Patients are discouraged from taking dietary supplements, herbs, and other similar agents if their use reduces health anxiety or unexplained body sensations. Similarly, adhering to special diets because of health anxiety is prohibited. The therapist should be alert for additional safety behaviors and signals that will require response prevention rules. Homework Each stage of CBT for SSD includes homework components to practice skills and reinforce session content. To emphasize the central role of homework, the therapist should assign homework beginning with the first session. For example, homework during the psychoeducation stage might include reading handouts about the 145 146 Lillian Reuman and Jonathan S. Abramowitz patient’s particular problem and how the CBT approach addresses conceptualization and treatment. Homework during the self-monitoring phase is described above. For exposure homework assignments, it is important to explain that such tasks provide opportunities for the client to challenge their fear-provoking assumptions and form new beliefs about situations that are realistically safe and tolerable (e.g., “Even if I have a stomach ache before flying, I can still travel”). In explaining outof-session exposure practice, the therapist can emphasize the importance of repeated practice in various contexts to maximize treatment effects and enhance generalizability. Additionally, conducting exposure outside the medical setting and without the therapist present allows the patient to develop self-efficacy and learn that they can approach these situations even if help is not immediately available or if the bodily discomfort persists. More broadly, homework presents an opportunity to practice coping with anxiety and physical discomfort. It is important to consider that homework non-completion may occur for a variety of reasons. Huppert and colleagues (2006) posit that patients may misunderstand or refuse to complete a homework assignment due to beliefs about the utility of the assignment or low motivation to change. For example, patients with SSD may believe that a particular response prevention assignment (e.g., not consulting a doctor for a perceived uncomfortable body sensation) is harmful or irresponsible. Patients with SSD may also experience pain and exhaustion, effectively impairing their ability to complete their homework. In each situation, it is important to understand the patients’ reasons for non- or partial homework completion and integrate this information into the case formulation. The therapist and patient should work jointly during homework review to address and problem-solve any obstacles to homework compliance that arise. In the case of a misunderstanding, the therapist might explain the assignment in different terms, provide clear illustrations or examples, and/or check that the patient understands homework expectations by asking the patient to teach the therapist about the importance of homework. Cognitive therapy and motivational interviewing (e.g., identifying pros and cons) can be useful for addressing homework compliance barriers such as beliefs about safety (e.g., “conducting IE on my own is dangerous”) or low motivation for change. In the context of emotional barriers (e.g., fear, shame) to homework (non)compliance, psychoeducation about emotions (e.g., normalizing fear) can be useful. Given logistical barriers (e.g., little time to complete homework), the therapist and patient could work jointly to schedule a specific time of day to complete homework practice or identify an individual that can help the patient remain accountable. Treatment Outcome Abundant research supports the efficacy of CBT for SSD/IAD and their precursors in earlier editions of the DSM (i.e., hypochondriasis), and findings are well summarized in a meta-analysis of this literature by Olatunji and colleagues (2014). Considering 13 randomized controlled trials (RCTs) with a total sample size of CBT for Somatic Symptom Disorder and Illness Anxiety Disorder 1,081 participants, Olatunji and colleagues (2014) found that CBT for hypochondriasis outperformed control conditions (e.g., treatment as usual, wait-list) on primary symptom outcome measures at post-treatment and showed a large effect size. A follow-up analysis of seven studies revealed that CBT for patients with health anxiety also outperformed control conditions on secondary outcomes (i.e., exhibited significant reductions in symptoms of depression). This suggests that the acute therapeutic effects of CBT for patients with hypochondriasis/health anxiety may generalize to other symptoms. The researchers examined the extent to which effect size varied as a function of treatment factors (e.g., number of sessions) and participant characteristics (e.g., percentage of females, mean age). More sessions of CBT for hypochondriasis were associated with larger effect sizes at post-treatment. Higher pre-treatment hypochondriasis/health anxiety was found to be associated with an increase in CBT effect size at follow-up visits; however, participant demographics were not differentially associated with effect sizes. Although these findings are promising, additional research with longer follow-up intervals is necessary to offer more definitive conclusions regarding the strength of CBT for SSD/health anxiety. Recent Advances Although CBT for SSD/IAD is most commonly offered in an individual, in-person format, a number of recent advances lend empirical support to varied styles of treatment delivery such as group therapy, internet-based formats, and mindfulness-based approaches. Group Therapy Group therapy has been shown to be effective for a variety of psychiatric conditions, such as anxiety disorders (e.g., panic disorder) and hypochondriasis (Hedman et al., 2010). In comparison to individual therapies, a group approach for SSD/IAD offers support and advantages for participants in various ways. First, learning about fellow group members’ experiences can help to normalize the individual’s concerns. Second, working together in a group setting can provide a supportive, encouraging environment that motivates individuals to persist with out-of-session practice. Third, group members can collectively brainstorm and problem-solve treatment obstacles by providing a range of perspectives and first-hand accounts. Further, given that patients can be treated jointly, a group approach can facilitate scheduling by maximizing therapist availability and decreasing costs for the group members (Espejo et al., 2016). This is particularly important given that somaticizing patients exhibit increased utilization of medical services and incur higher costs by virtue of more specialist and emergency department visits as a function of perseverative worry (Barsky et al., 2005). In a recent open trial, Hedman and colleagues (2010) investigated the effectiveness and cost impact of a group CBT protocol in a psychiatric setting for individuals with somatic concerns. Using a CBT model, the treatment emphasized challenging 147 148 Lillian Reuman and Jonathan S. Abramowitz interpretations of bodily sensations as signs of serious illness and reducing avoidance and safety behaviors (Furer et al., 2007; Taylor & Asmundson, 2004). The groups included four to seven patients, and treatment consisted of 10 weekly group sessions. Each session lasted two hours, covered a particular theme (e.g., cognitive restructuring, interoceptive exposure, response prevention), and followed a structured format (e.g., agenda-setting, homework review, and psychoeducation). Results revealed large within-group effect sizes on self-report measures of health anxiety. At post-treatment, there was a significant reduction in the number of participants meeting diagnostic criteria for hypochondriasis following treatment. Treatment gains were maintained at follow-up on all measures, and participants continued to improve on measures of depression and anxiety sensitivity (i.e., the “fear of fear”). Taken together, findings suggest that group CBT can be delivered in a regular psychiatric healthcare context for individuals with SSD. The researchers also concluded that CBT for health-related worry can be highly cost-effective, as the intervention generated a total cost offset within one year, primarily because of a decrease in direct medical costs. Internet-Based Treatment Hedman and colleagues (2011) also investigated an internet-based treatment platform for somatic concerns (i.e., DSM-IV hypochondriasis). The 12-week CBT-based protocol, developed by their research team, included thematic modules (e.g., psychoeducation) and accompanying homework. Further, participants received online access to fellow study participants for group discussion/support and to a therapist who was available for online feedback and encouragement. Study findings lent support for the feasibility of providing online educational modules and therapeutic support for somatic concerns. The researchers noted that minimal therapist resources (approximately 10 minutes per patient per week) and the flexibility of internet-based CBT with respect to delivery make internet therapy a promising means for improving the availability of CBT for hypochondriasis. In particular, an online CBT protocol may be well suited to individuals with severe somatization symptoms who are unable to leave their home due to somatic complaints (e.g., pain) or time-consuming, debilitating worry and ritualistic behavior. Mindfulness-Based Approaches Mindfulness-based cognitive therapy (MBCT; Lovas & Barsky, 2010) represents another recent advance in treatment for somatic concerns. An emphasis on nonjudgment and relaxation may be particularly useful for reducing physiological arousal and interrupting cycles of unproductive worry that accompany somatic complaints among individuals with illness anxiety. Lovas and Barsky (2010) conducted a small pilot study of an eight-week group MBCT intervention for severe health anxiety. Educational in focus, the intervention was based on preexisting models of mindfulness-based stress reduction (MBSR) and MBCT, by Kabat-Zinn (1990) and Segal et al. (2002), respectively. Participants were taught mindfulness CBT for Somatic Symptom Disorder and Illness Anxiety Disorder meditation, including body scan, mindful breathing, and mindful movement practices. For homework, participants practiced the meditations for at least 30 minutes daily. Following treatment, participants exhibited significant improvements in measures of health anxiety, disease-related thoughts, somatic symptoms, and mindfulness, which were sustained at three-month follow-up. These preliminary findings simultaneously highlight the various cognitive behavioral options for treating SSD, as well as the need for exploring novel treatment options for this ill patient population. Key Points Assessment of SSD Rule out organic medical conditions. Assess external and internal triggers of SSD. Assess beliefs about internal body sensations. Assess safety behaviors associated with SSD. Use the functional assessment and self-monitoring to develop an idiosyncratic case conceptualization. Treatment of SSD Begin with psychoeducation about cognitive behavioral model and rationale for cognitive behavioral therapy. Incorporate cognitive restructuring to challenge beliefs about bodily sensations. Use a mix of interoceptive, in vivo, and imaginal exposure. Eliminate all safety behaviors. FURTHER RECOMMENDED READING Abramowitz, J. S., & Braddock, A. E. (2008). Psychological treatment of health anxiety and hypochondriasis. Hogrefe. Deacon, B., & Abramowitz, J. S. (2008). Is hypochondriasis related to obsessive-compulsive disorder, panic disorder, or both? An empirical evaluation. Journal of Cognitive Psychotherapy, 22(2), 115–127. Furer, P., Walker, J. R., & Stein, M. B. (2007). Treating health anxiety and fear of death: A practitioner’s guide. Springer. Olatunji, B. O., Kauffman, B. Y., Meltzer, S., Davis, M. L., Smits, J. A., & Powers, M. B. (2014). Cognitive-behavioral therapy for hypochondriasis/health anxiety: A metaanalysis of treatment outcome and moderators. Behaviour Research and Therapy, 58, 65–74. Reuman, L., & Abramowitz, J. S. (2015). Illness anxiety disorder. In K. A. Phillips & D. J. Stein (Eds.), Handbook on obsessive-compulsive and related disorders (pp. 225–246). American Psychiatric Publishing. Rief, W., Hiller, W., & Margraf, J. (1998). Cognitive aspects of hypochondriasis and the somatization syndrome. Journal of Abnormal Psychology, 107(4), 587. 149 150 Lillian Reuman and Jonathan S. Abramowitz Salkovskis, P. M., Rimes, K. A., Warwick, H. M. C., & Clark, D. M. (2002). The Health Anxiety Inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine, 32(5), 843–853. Taylor, S., & Asmundson, G. J. (2004). Treating health anxiety: A cognitive-behavioral approach. Guilford Press. REFERENCES Abramowitz, J. S., & Braddock, A. E. (2008). Psychological treatment of health anxiety and hypochondriasis. Hogrefe. Abramowitz, J. S., Deacon, B. J., & Valentiner, D. P. (2007). The Short Health Anxiety Inventory: Psychometric properties and construct validity in a non-clinical sample. Cognitive Therapy and Research, 31(6), 871–883. Abramowitz, J. S., Deacon, B. J., & Whiteside, S. P. (2012). Exposure therapy for anxiety: Principles and practice. Guilford Press. American Psychiatric Association. (2013). Diagnostic and statistical manual of Mental Disorders (5th ed.). American Psychiatric Association. Barlow, D. H. (Ed.) (2014). Clinical handbook of psychological disorders: A step-by-step treatment manual. Guilford Press. Barsky, A. J., Orav, E. J., & Bates, D. W. (2005). Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Archives of General Psychiatry, 62(8), 903–910. Craske, M. G., Kircanski, K., Zelikowsky, M., Mystkowski, J., Chowdhury, N., & Baker, A. (2008). Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy, 46(1), 5–27. Espejo, E. P., Castriotta, N., Bessonov, D., Kawamura, M., Werdowatz, E. A., & Ayers, C. R. (2016). A pilot study of transdiagnostic group cognitive-behavioral therapy for anxiety in a veteran sample. Psychological Services, 13(2), 162. Furer, P., Walker, J. R., & Stein, M. B. (2007). Treating health anxiety and fear of death: A practitioner’s guide. Springer Science & Business Media. Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., Hill, C. L., . . . & Charney, D. S. (1989). Yale–Brown Obsessive Compulsive Scale (YBOCS). Archives of General Psychiatry, 46, 1006–1011. Hedman, E., Andersson, G., Andersson, E., Ljótsson, B., Rück, C., Asmundson, G. J., & Lindefors, N. (2011). Internet-based cognitive-behavioural therapy for severe health anxiety: Randomised controlled trial. The British Journal of Psychiatry, 198(3), 230–236. Hedman, E., Ljótsson, B., Andersson, E., Rück, C., Andersson, G., & Lindefors, N. (2010). Effectiveness and cost offset analysis of group CBT for hypochondriasis delivered in a psychiatric setting: An open trial. Cognitive Behaviour Therapy, 39(4), 239–250. Huppert, J. D., & Baker-Morissette, S. L. (2003). Beyond the manual: The insider’s guide to panic control treatment. Cognitive and Behavioral Practice, 10(1), 2–13. Huppert, J. D., Roth Ledley, D., & Foa, E. B. (2006). The use of homework in behavior therapy for anxiety disorders. Journal of Psychotherapy Integration, 16(2), 128–139. Kabat-Zinn, J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Dell Publishing. Lovas, D. A., & Barsky, A. J. (2010). Mindfulness-based cognitive therapy for hypochondriasis, or severe health anxiety: A pilot study. Journal of Anxiety Disorders, 24(8), 931–935. Salkovskis, P. M., Rimes, K. A., Warwick, H. M. C., & Clark, D. M. (2002). The Health Anxiety Inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine, 32(5), 843–853. CBT for Somatic Symptom Disorder and Illness Anxiety Disorder Segal, Z. V., Teasdale, J. D., Williams, J. M., & Gemar, M. C. (2002). The mindfulness-based cognitive therapy adherence scale: Inter-rater reliability, adherence to protocol and treatment distinctiveness. Clinical Psychology and Psychotherapy, 9(2), 131–138. Taylor, S., & Asmundson, G. J. (2004). Treating health anxiety: A cognitive-behavioral approach. Guilford Press. Tyrer, P., Cooper, S., Crawford, M., Dupont, S., Green, J., Murphy, D., et al. (2011). Prevalence of health anxiety problems in medical clinics. Journal of Psychosomatic Research, 71, 392–394. Walker, J. R., & Furer, P. (2008). Interoceptive exposure in the treatment of health anxiety and hypochondriasis. Journal of Cognitive Psychotherapy, 22(4), 366–378. 151 9 Cognitive Behavioral Therapy for Generalized Anxiety Disorder: Targeting Intolerance of Uncertainty Cara R. Dunkley and Melisa Robichaud Despite being a relatively common disorder, generalized anxiety disorder (GAD) is known as one of the more challenging mental health conditions to accurately diagnose and treat. The diagnostic criteria for GAD in the current edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) include excessive and uncontrollable worry about a number of daily life events, accompanied by anxiety and somatic symptoms, occurring more days than not for a period of at least six months (American Psychiatric Association [APA], 2013). Among the general population, 12-month prevalence rates for GAD are between 2 and 4%, and lifetime prevalence rates are between 4 and 7% (Blazer et al., 1991; Hunt et al., 2002; Wittchen et al., 1994). The incidence of GAD is markedly greater among clinical populations, with GAD being the most common anxiety disorder and the second most common mental health concern within primary care facilities (Barrett et al., 1988; Wittchen et al., 2002). As GAD is associated with significant social, occupational, and functional impairment (e.g., Stein & Heimberg, 2004), there is a great need for a highly effective psychological treatment. In this chapter, we provide an overview of the research and evidence-based treatment protocol for a GAD-specific treatment, cognitive behavioral therapy targeting intolerance of uncertainty (CBT-IU). Within the theoretical model for CBT-IU, intolerance of uncertainty (IU) represents the underlying mechanism that drives the development and maintenance of excessive worry and contributes to additional model components that serve as maintenance factors in GAD. Relevant Research CBT-IU is a theoretically derived treatment protocol for GAD that has been refined and validated over 25 years of clinical research (see Robichaud et al., 2019, for review). Its central focus is to address GAD symptoms by targeting what underlies the development and maintenance of excessive worry, namely, intolerance of uncertainty. IU can be defined as a dispositional characteristic that results 152 CBT for Generalized Anxiety Disorder from a set of negative beliefs about uncertainty and its consequences (e.g., uncertainty is unfair, leads to negative and catastrophic outcomes, and is beyond one’s ability to cope) (Hebert & Dugas, 2018; Robichaud et al., 2019). Research related to CBT-IU for GAD has focused not only on the efficacy of the treatment itself but also on the processes targeted within the protocol and its corresponding theoretical conceptualization. CBT-IU Processes The four cognitive processes targeted in treatment include intolerance of uncertainty, positive beliefs about the function of worry, negative problem orientation, and cognitive avoidance. Each of these factors has been extensively researched with respect to its association to GAD symptoms, and is conceptualized as contributing to the development and maintenance of excessive and uncontrollable worry. IU, however, is viewed as a higher-order process that drives the worry cycle, and at least partially accounts for the associations between the remaining factors and GAD. That is, positive beliefs about worry, negative problem orientation, and cognitive avoidance can be explained, at least in part, by the level of intolerance of uncertainty in individuals with GAD. IU is thus the key feature of this theoretical model, and should be addressed at all phases of treatment. Intolerance of Uncertainty Given the primacy of IU in the CBT-IU protocol, a great deal of research has been conducted over the years to identify evidence for a potential causal relationship between IU and worry in GAD (e.g., Bomyea et al., 2015; Dugas et al., 2004b; Koerner & Dugas, 2006; Meeten et al., 2012). Evidence for this link comes from various sources, including longitudinal research, wherein variations in IU were found to predict increases in excessive worry over time (Dugas et al., 2012). A bidirectional relationship between IU and worry also emerged, whereby habitual worry predicted greater IU. In addition, research using an experimental design has found that heightening IU momentarily increases worry. Specifically, when the level of IU is experimentally manipulated, participants in the group who underwent IU manipulation reported higher levels of worry compared with those in the control condition who did not have an IU manipulation (Ladouceur et al., 2000; Meeten et al., 2012). Evidence in support of IU as a causal risk factor for GAD can also be found in the temporal sequence of change, with changes in IU preceding changes in worry during treatment (Dugas et al., 1998). It is worth noting that research has also linked IU to symptoms of many other disorders, including obsessive-compulsive disorder, social anxiety disorder, posttraumatic stress disorder, panic disorder, depression, and eating disorders (see Carleton, 2016, for review), making IU a transdiagnostic process. However, several studies have identified the association of IU to worry as stronger than its relationship to other anxiety and mood disorders (Dugas et al., 1997, 2004a; Ladouceur et al., 1999), as well as to conceptually related processes, such as perfectionism and 153 154 Cara R. Dunkley and Melissa Robichaud need for control over all facets of life (Buhr & Dugas, 2006). Moreover, a study examining whether the level of IU predicted GAD symptom severity found that clients with severe GAD had higher levels of IU than those with more moderate symptoms of GAD (Dugas et al., 2007). These findings suggest that despite its significant relationship to other mental health conditions, IU maintains a sensitive and specific association to the excessive, uncontrollable worry characteristic of GAD. Positive Beliefs about Worry Although most people view the process of worry as helpful to some degree on occasion, individuals with GAD appear to hold positive beliefs about the function of worry to a greater degree than nonclinical worriers (Ladouceur et al., 1998, 1999). Common positive beliefs include the notion that worry (1) aids in problem-solving, (2) represents a motivational force, (3) is a positive personality trait, (4) can prevent negative outcomes in and of itself, and (5) protects against negative emotions. The extent to which nonclinical individuals hold a combination of these beliefs is associated with problematic worry (Robichaud et al., 2003). Overall, the belief that worry is useful perpetuates the ongoing use of worry as a means of reducing uncertainty, and can lead to ambivalence about change with treatment. Negative Problem Orientation Problem orientation describes one’s attitude and confidence about problems and problem-solving ability. Individuals with a positive problem orientation view problems as normal challenges that can be effectively overcome, while individuals with a negative problem orientation view problems as insurmountable obstacles. Research into the relationship between problem-solving and worry suggests that individuals with GAD endorse a strong negative problem orientation via self-report, which is marked by the tendency to view daily life problems as threatening, to doubt their problem-solving ability, and to be pessimistic about the outcome of problem solving (Robichaud & Dugas, 2005a, 2005b). As daily life problems are inherently marked by uncertainty, it is not surprising that individuals with GAD view problems as threatening. Indeed, research has found negative problem orientation to predict GAD symptom severity (Dugas et al., 2007) and to be associated with worry above and beyond worry’s relationship to anxiety, depression, and IU (Dugas et al., 1997; Robichaud & Dugas, 2005b). Yet negative problem orientation in individuals with GAD does not reflect deficits in actual problem-solving ability; rather, having a negative problem orientation appears to lead to increased anxiety and avoidance when confronted with problems (Davey, 1994), which in turn interferes with the proper application of problem-solving skills (D’Zurilla & Nezu, 2006). As such, holding negative perceptions about problems and problem-solving, as well as mentally reviewing problems through worry, impedes individuals with GAD from engaging in active problem-solving. CBT for Generalized Anxiety Disorder Cognitive Avoidance Individuals with GAD tend to engage in a number of cognitive avoidance strategies as an attempt to cope with worry and avoid threatening cognitive and emotional content. Worry represents an implicit form of cognitive avoidance, in that it is a verbal-linguistic process that reduces physiological arousal and inhibits emotional processing (Borkovec et al., 2004). Cognitive avoidance of mental imagery involving disturbing events is therefore a particularly common process among individuals with GAD. A number of ineffectual cognitive avoidance strategies are associated with GAD, including thought suppression, substituting worries with positive thoughts, mental distraction, and situational avoidance (Sexton & Dugas, 2008). Research has shown that writing about feared hypothetical situations elicits vivid mental imagery, which promotes emotional processing of core fears and results in subsequent reductions in worry among pathological worriers (Fracalanza et al., 2014; Ovanessian et al., 2018). Repeated writing about core fears is thus theorized to reduce negative beliefs about emotion, as well as shift perceptions about feared hypothetical situations and coping ability. Treatment Efficacy Research The efficacy of the CBT-IU protocol in treating GAD has been demonstrated through several clinical trials. First, significant reductions in GAD symptoms from pre- to post-treatment have been observed in both individual and group formats when compared with wait-list controls (Dugas et al., 2003; Ladouceur et al., 2000). Specifically, treatment gains and diagnostic remission of GAD were maintained for 77% participants at one-year follow-up. CBT-IU has also been compared to wait-list controls and applied relaxation (AR) therapy in a randomized controlled trial (Dugas et al., 2010). CBT-IU emerged as being markedly superior to wait-list controls and marginally superior to AR. Treatment gains were largely maintained among those in the CBT-IU group, and diagnostic remission remained high in the majority of participants at two-year follow-up. Although AR was beneficial to those with GAD, only CBT-IU produced ongoing improvement over time in both symptom measures and diagnostic remission. Among individuals in the CBT-IU group, parallel decreases in IU and GAD symptoms were observed during treatment and follow-up. Further, reductions in IU predicted reductions in GAD symptoms above and beyond several other important therapy factors. A new single-component treatment that focuses entirely on behavioral experiments targeting IU has been developed in recent years. Preliminary testing of this treatment showed statistically and clinically significant improvements in GAD severity and associated symptoms, pathological worry, and IU, comparable to that observed in studies testing the efficacy of the entire CBT-IU protocol (Hebert & Dugas, 2018). Collectively, these findings provide additional evidence for the importance of targeting IU in treating GAD and suggest that CBT-IU leads to substantial short- and long-term improvements in GAD symptoms. 155 156 Cara R. Dunkley and Melissa Robichaud Assessment GAD is one of the more challenging anxiety disorders to accurately diagnose. There are several likely reasons for this. For example, clients with GAD are often reluctant to seek help as worry may not be viewed as a legitimate mental health complaint, and the main diagnostic criteria for GAD is ambiguous, given that the central feature of GAD is “excessive and uncontrollable worry” about daily life events. Furthermore, individuals with GAD largely report worrying about the same topics as nonclinical worriers. The content of worry is therefore less relevant in discriminating between clinical and nonclinical worry. Rather, it is the extent to which reported worries are experienced as frequent, excessive, and uncontrollable that distinguishes worry characteristic of GAD. As such, the frequency and severity of worry is the primary focus of the assessment. In order to accurately diagnose GAD, excessive worries relating to several life domains should be examined. Clients who meet diagnostic criteria for GAD will endorse at least two worry domains as frequent, excessive, and uncontrollable. In addition to excessive worry, at least three of the seven GAD-associated somatic and cognitive symptoms (i.e., restlessness, fatigue, irritability, muscle tension, sleep difficulties, concentration, and memory impairment) are required for diagnosis. Only muscle tension, however, is specific to a diagnosis of GAD, as the other associated symptoms can also be seen in various anxiety and mood disorders. GAD-associated somatic and cognitive symptoms should therefore not be a primary consideration when diagnosing GAD. Given the diagnostic challenges, GAD is best assessed using a structured diagnostic interview. The Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5; Brown & Barlow, 2014) and Structured Clinical Interview for DSM-5 Disorders, Clinician Version (SCID-5-CV; First et al., 2016) are the most common measures for the structured assessment of GAD. Therapists assessing for GAD should consider whether the presence of excessive worry is best accounted for by GAD or another diagnosis, and whether particular worry themes, such as those pertaining to social settings or one’s health, are best captured by GAD or indicative of an additional separate diagnosis. Structured diagnostic interviews can be augmented with a battery of self-report measures. The Intolerance of Uncertainty Scale (IUS; Buhr & Dugas, 2002) assesses negative beliefs about uncertainty, and the Penn State Worry Questionnaire (PSWQ; Meyer et al., 1990) assesses the tendency for excessive and uncontrollable worry; these can be administered across all sessions. Additional measures that may be employed include the Negative Problem Orientation Questionnaire (NPOQ; Robichaud & Dugas, 2005a), which assesses negative problem orientation); the Why Worry-II (WW-II; Hebert et al., 2014), which assesses positive beliefs about worry; and the Cognitive Avoidance Questionnaire (CAQ; Sexton & Dugas, 2008), which assesses the tendency to engage in cognitive avoidance. Administering these questionnaires before, during, and after treatment provides a means by which treatment efficacy and client gains can be measured. CBT for Generalized Anxiety Disorder Key Points Accurate identification and differential diagnosis of GAD can be challenging, and a comprehensive assessment is therefore recommended. The distinction between GAD and nonclinical worry is quantitative (frequent, excessive, and uncontrolled), rather than qualitative (content of worry). GAD is best assessed using a structured assessment tool alongside selfreport questionnaires. Formulation and Case Conceptualization An appropriate theoretical model for any clinical disorder should be able to account for the particular symptom presentation within that disorder. The CBT-IU model emphasizes the primary role of intolerance of uncertainty (IU) in developing and maintaining excessive and uncontrollable worry. As such, IU needs to account for the symptoms and phenomenology in GAD, specifically, its cardinal feature of frequent, excessive, and uncontrollable worry, as well as its dynamic and varied content over time. Why would IU account for the worry that is characteristic of GAD? In order to address this question, it is first important to clarify how worry in GAD is conceptualized. Worry can be viewed as an attempt to mentally plan and prepare for all potential negative outcomes prior to their occurrence (e.g., “What if X happened? Then I might do . . . But what if Y happened?”). However, this elaborate scenario building tends to generate further worry among individuals with GAD, as worries centers upon what could happen, which allows for infinite iterations of hypothetical outcomes that could occur. Moreover, worry is highly dynamic in GAD, as worry content tends to shift from day to day, typically involving daily life events such as finances, work or school, family, and health of self and loved ones. In fact, people with GAD often report worrying about “everything.” Within the CBT-IU model, it is posited that individuals with GAD worry excessively as an attempt to reduce, avoid, or otherwise circumnavigate uncertainty by thinking about and planning for all potential outcomes in an uncertain situation. However, given that daily life is inherently fraught with uncertainty, there is always something to worry about. In addition, given that the particular uncertainties that an individual might face can change daily, worry topics can be expected to shift accordingly; hence, worry can be about multiple daily life events. Although everybody occasionally worries, most people can tolerate some uncertainty in daily life without the urge to mentally plan and prepare as a result. This is because IU can be conceptualized as a dimensional construct, with individuals with GAD displaying higher levels of intolerance than low or moderate worriers, such that even a minute amount of uncertainty in a given situation has the potential to incite a worry episode. In other words, the threshold for uncertainty in daily life situations is much lower among individuals with GAD; as such, their 157 158 Cara R. Dunkley and Melissa Robichaud worries are more easily triggered than is the case with individuals with a higher tolerance or threshold for uncertainty. Although the fear of uncertainty is present in many anxiety disorders, it is likely that it is the “general state of uncertainty” that characterizes GAD, hence the presence of varied and changing worry themes in GAD. Much like the fear of negative evaluation typically represents the source of threat in social anxiety, the fear of uncertainty is posited as the theme of threat in GAD. For example, consider an individual who spends much of their day occupied by various worries, including concerns about the health and well-being of their children, finances, career, and social interactions. To cope with these worries, they might engage in a number of safety behaviors, such as repeatedly checking on their children via text, asking multiple people for their opinions when making decisions, overpreparing for work presentations, or rereading emails several times before sending them. The worries that they experience, as well as all of these disparate safety behaviors, represent cognitive and behavioral attempts to reduce or avoid uncertainty. As such, despite the varied content of their worries and associated behaviors, their thoughts and actions can be parsimoniously understood as strategies to manage the fear of uncertainty. With this in mind, CBT-IU centers on targeting IU by changing negative beliefs about uncertainty and its consequences, rather than focusing on the specific content of worry. Given the frequent change in worry topics from day to day that is seen in GAD, CBT interventions that target worries themselves, rather than the underlying process that drives worry, would be akin to chasing a moving target. CBT-IU therefore aims to indirectly reduce GAD symptoms by directly targeting the fear of uncertainty. Overview of CBT-IU The CBT-IU treatment protocol can vary in length from 12 to 16 sessions and encompasses multiple modules that can be flexibly applied according to clients’ particular presentation. Though all aspects of CBT for IU are helpful for individuals with GAD, the primary emphasis across therapy is increasing tolerance to uncertainty by developing more balanced beliefs about uncertainty and its consequences. The goal of CBT-IU is not to free clients entirely of worry but to help them worry less as a result of challenging negative beliefs about uncertainty. Module 1: Psychoeducation about GAD and the Cycle of Worry Psychoeducation The first module centers on providing psychoeducation about CBT and the meaning of a GAD diagnosis. The diagnostic characteristics of GAD are outlined, with emphasis being placed on the primary symptom of frequent, excessive, and uncontrollable worry about daily life events. The somatic symptoms associated with GAD are reviewed, and anxiety is described as the physiological CBT for Generalized Anxiety Disorder Figure 9.1. Initial clinical model of GAD for CBT-IU. result of excessive worry. GAD can be presented to clients as existing on a continuum, with everyone falling somewhere from low to high anxiety and worry. In this way, the diagnosis of GAD is conceptualized as a matter of degree, with individuals meeting diagnostic criteria if their worry is excessive and creates significant distress or impairment. The distinction between nonclinical and clinical worries is thus not qualitative in nature, as GAD is seen as an excessive manifestation of a normal phenomenon. Clients are presented with an initial pictorial model of GAD that describes the basic worry cycle (see Figure 9.1). Negative beliefs about uncertainty and its impact on model components are introduced in later sessions when IU is presented. The initial CBT-IU model begins with a triggering situation marked by novelty (e.g., going to a new restaurant), ambiguity (e.g., noticing an unclear ache in one’s body), or unpredictability (e.g., taking a test at school). Triggers lead to initial “what if” questions (e.g., “What if I fail my exam?”), which in turn lead to worry. Worry as a strategy is described as elaborate scenario building of potential negative outcomes and attempts at mental problem-solving (e.g., “What if I fail my exam? I could perhaps retake it, but what if the teacher refuses? Maybe I could do an extra credit assignment?”). Given that the predicted feared negative outcomes have not happened yet (and may never happen), there are endless permutations of what “could” occur. This process engenders further “what if” thoughts and further worries, resulting in a cycle of worry (e.g., “What if I do poorly on the extra credit 159 160 Cara R. Dunkley and Melissa Robichaud assignment? I could fail the class. What if I am unable to graduate?”). It is this elaborate mental process that ultimately leads to the physiological experience of anxiety. To cope with worry and anxiety, people typically engage in safety behaviors (e.g., excessively checking of the course syllabus to repeatedly reassure oneself that they’ve studied all of the test material). Safety behaviors are deliberate actions designed to reduce anxiety and feared outcomes in the short term; however, such actions prevent the acquisition of corrective information, as the nonoccurrence of feared negative outcomes is taken as evidence that they otherwise would have occurred if not for the use of safety behaviors. As a consequence, fears are maintained in the long term, thereby perpetuating the cycle of worry. Worry Awareness Training. Following the exposition of the initial GAD model, clients are presented with their first between-session exercise, which involves selfmonitoring. Clients are invited to record a worry episode three times day, noting (1) the internal (thought or physical sensation) or external (actual situation) triggering event, (2) the original “what if” thought, (3) the level of anxiety (on a 0–10 scale), and (4) any associated safety behaviors. Through worry awareness training, clients are encouraged to become more aware of the content of their thoughts, as well as the association between their worries, physical sensations, and behaviors. Worry monitoring forms can then be debriefed in subsequent sessions, with the therapist inquiring about specific worry themes, as well as potentially common safety behaviors. Key Points Psychoeducation involves providing clients with information about the principles of CBT, as well as normalizing information about GAD diagnostic criteria. Clients are introduced to an initial model of GAD, with an emphasis on the worry cycle, and the maintaining role of safety behaviors. Worry awareness training helps clients become more cognizant of the interrelationship between their worries, anxiety, and associated safety behaviors. Module 2: Reevaluation of the Usefulness of Worry Identifying Positive Beliefs about Worry As individuals with GAD tend to hold positive beliefs about the usefulness of worry, the primary goal of this module is to help clients identify and challenge their beliefs regarding the actual utility of worry. So long as worries are perceived as beneficial, there remains a potential barrier to working toward worry reduction. Yet because clients present for treatment in order to reduce their excessive worry, they may be CBT for Generalized Anxiety Disorder unaware of, or hesitant to discuss, any ambivalence they hold toward actually letting go of their worries and their perceived benefits. However, as clients have typically spent a debilitating amount of time occupied by worry, there is often a need to see worry as serving some benefit, even while acknowledging its problems. The therapist can normalize conflicting beliefs about worry through an analogy: Therapist: Let’s say that a student consistently studies all night before an exam, and they usually get good grades. Although they are exhausted because of their overnight cram sessions, and know that it probably isn’t a very good way to study, it nevertheless feels like a helpful strategy because they are getting good grades. So too with worry, people with GAD might find it exhausting and stressful to worry all the time, yet they still might think that it is useful to worry about their finances or their daily schedules, for example, as it keeps them organized and on track in daily life. Research has identified five main categories of positive beliefs about worry: (1) worry helps to find solutions to problems; (2) worry can serve as a motivating function; (3) worry can guard against negative emotions by helping to prepare for terrible outcomes, should they occur; (4) worry, in and of itself, can prevent negative outcomes; and (5) worrying is a positive personality trait. When introducing these beliefs to clients, it is best accomplished through guided discovery, by asking clients about the perceived benefits they derive from their specific worries (e.g., “What are the positives about worrying about the health and well-being of your children?”), rather than discussing worry in general (e.g., “Do you think worrying helps to motivate you?”). This addresses the conflicting beliefs clients have about worry in general (e.g., “It’s bad that I worry”), as opposed to their own particular worries (e.g., “It’s good that I worry about my children, as it shows that I’m a loving and caring parent”). Challenging Positive Beliefs about Worry Positive beliefs about worry are investigated through cognitive challenging to determine whether worry is indeed useful. One strategy to help reevaluate the function of worry is the lawyer/prosecutor role-play, wherein clients first take on the role of a lawyer tasked with convincing a jury about the usefulness of a specific worry (rather than a belief in general), and then as the prosecutor, convincing the jury that worry is not useful. Socratic questioning can be used to aid clients with this (see Table 9.1 for possible challenges according to worry belief ). Therapists can also ask clients to consider the overall cost of worry in their lives, such as time spent worrying and difficulties enjoying the present moment. Focusing on specific worries, as opposed to the positive beliefs about worries themselves, allows the case made for and against the usefulness of worry to be more concrete, and prevents the discussion from becoming overly intellectualized. 161 162 Cara R. Dunkley and Melissa Robichaud Table 9.1. Examples of challenges to positive beliefs about the usefulness of worry Positive belief Challenge Worry helps to find solutions to problems. Do you actually solve your problems when you worry, or are you just thinking a lot about the problem? Does worrying ever interfere with problem-solving? Does your worry really improve your performance? Are there times when you got so worried about something that you were less likely to follow through on it? Does worrying about things that might never occur actually make you feel better in the here and now? Has anything bad ever happened that you had worried about before? If so, did worrying beforehand make you less upset? Is your belief about worry preventing negative outcomes based on real evidence, or is it an assumption? Is it possible that you remember only instances that support this belief? Do you know any caring/conscientious/organized individuals who do not worry excessively? Have you suffered any negative consequences from friends and family (e.g., being seen negatively by others) because of your excessive worry? Worry can serve a motivating function. Worry can guard against negative emotions. Worry can prevent negative outcomes. Worry is a positive personality trait. Gathering evidence about the actual usefulness of worries also promotes insight into the potentially paradoxical nature of beliefs about worry. For example, an individual might believe worrying about their health is positive, thinking that it motivates them to exercise; however, worrying about health may also leave that individual so stressed that they end up avoiding exercise altogether. It is important to note that significant cognitive shifts are not expected at this phase. Rather, clients are encouraged to recognize the positive beliefs they hold about the utility of worry, and identify whether worry is providing any actual benefits that cannot be obtained through other means. Shifting Beliefs about Worry: Implications A secondary goal of this module is to allow clients to consider what it would truly mean to worry less. What would they do with all their time that was previously spent worrying? What would it say about them as a person if they were no longer “a worrier”? As many clients cannot remember a time without excessive worry, this can be an emotional experience. Exploring what it really means to worry less allows clients to address any fears or feelings of loss they might experience with respect to this change, as well as begin to conceive of a future free of excessive worry. It should be noted that not all positive beliefs about worry are mistaken or incorrect; rather, discussion on this topic is intended to assist clients in ascertaining whether or not their excessive worries are as helpful as they think, and whether it is possible to obtain any perceived uses of worry through alternative means if there are in fact benefits achieved through worry. CBT for Generalized Anxiety Disorder Key Points People with GAD tend to hold positive beliefs about the usefulness of worry that might lead to ambivalence toward the goals of treatment. Socratic questioning is encouraged to help clients identify the specific positive beliefs they hold about their own worries. Cognitive challenging using a lawyer/prosecutor role-play can help clients to challenge their positive beliefs about worry by identifying evidence for and against their beliefs and recognizing paradoxes within their evidence. Exploring what it would mean to worry less is a valuable exercise that can help clients prepare for a life after treatment without excessive worry as a backdrop. Module 3: Reevaluation of Negative Beliefs about Uncertainty IU and Negative Beliefs about Uncertainty Module 3 focuses on IU and negative beliefs about uncertainty, which are the basis of the GAD model and the primary component of treatment. IU is posited as the underlying source of the excessive worry characteristic of GAD, and is therefore directly targeted in this module. Clients are introduced to negative beliefs about uncertainty and their consequences within the GAD model, as well as their impact on the development and maintenance of GAD. Graduated behavioral experiments are the primary therapeutic strategy introduced in this section, and they are designed to directly test the accuracy of negative beliefs about uncertainty. Therapists are encouraged to devote time to explaining the relationship between negative beliefs about uncertainty and excessive worry. Specifically, people with GAD are susceptible to worry even in situations with small amounts of uncertainty, as their tolerance threshold for uncertainty is low. As a result, they engage in worry as a means of decreasing uncertainty and increasing their sense of control by mentally preparing for hypothetical eventualities. In fact, situations that initially trigger the worry cycle, that is, novel, unpredictable, or ambiguous situations, all share uncertainty as a common factor. However, uncertainty is not inherently threatening. For example, many people likely would not perceive going to dinner with friends at a new restaurant as particularly threatening. Rather, it is an individual’s beliefs about the consequences of uncertainty in triggering situations that are perceived as threatening, and ignite a worry cycle as a consequence (e.g., “What if I don’t like the food at the restaurant? What if I order something I don’t like, and waste time and money as a result?”). The basic model of GAD is expanded through the inclusion of negative beliefs about uncertainty, and its impact on worry and safety behaviors (Figure 9.2). There are four primary negative beliefs about uncertainty that individuals with GAD tend 163 164 Cara R. Dunkley and Melissa Robichaud Figure 9.2. Expanded clinical model of GAD for CBT-IU model featuring negative beliefs about uncertainty. to hold, each of which can contribute to perceptions of threat in uncertaintyinducing situations: 1. Events with ambiguous or unknown outcomes will turn out negatively. This belief involves the overestimation of the likelihood of threat, wherein individuals inflate the expectation that uncertain situations are highly likely to have negative outcomes. 2. Negative outcomes will be catastrophic. This belief involves the overestimation of the severity of threat. 3. Inability to cope with negative outcomes. This involves the tendency to greatly underestimate one’s ability to cope or act effectively in the face of a negative outcome. 4. Being uncertain is unacceptable, unpleasant, or unfair. This involves the belief that the general state of uncertainty is upsetting and unjust. CBT for Generalized Anxiety Disorder When introducing the expanded model, it is important to normalize the experience of excessive worry considering the client’s negative beliefs about uncertainty. Regardless of the accuracy of one’s beliefs about uncertainty, it makes sense that someone with these beliefs would view uncertain events as threatening. The goal of this module is therefore to develop more balanced beliefs about uncertainty and its outcomes, with the expectation that this would reduce threat perceptions toward uncertain situations, and reduce worry and anxiety as a result. Balanced beliefs about uncertainty and its consequences include (1) belief that uncertain events will probably turn out all right, (2) confidence in one’s ability to cope with negative outcomes should they arise, and (3) understanding that some uncertainty is a normal part of life. It is worth noting that individuals with balanced beliefs about uncertainty are not expected to never worry; rather, their tolerance threshold is increased, such that some uncertainty in daily life is viewed as less threatening overall. Safety Behaviors In order to challenge negative beliefs about uncertainty, it is necessary to help clients identify the various ways in which IU manifests through behavior. As noted earlier, safety behaviors maintain fears through the nonoccurrence of feared outcomes, and thereby prevent the acquisition of corrective information. In the case of GAD, individuals are prevented from learning about the actual outcome of uncertain situations and their correspondent coping ability due to the use of safety behaviors. GAD-related safety behaviors involve a host of actions that are designed to either avoid uncertainty altogether or reduce the uncertainty of the situation as much as possible. Common safety behaviors seen among clients with GAD include excessive information seeking, reassurance seeking, double-checking, avoidance of uncertainty-inducing situations, procrastination, refusal to delegate tasks to others, and the maintenance of a predictable routine. Behavioral Experiments In order to allow clients to directly test the accuracy of their beliefs about uncertainty and its consequences, behavioral experiments are introduced. Behavioral experiments involve deliberately refraining from engaging in a safety behavior, making a prediction about the feared outcome, and then observing the actual outcome. In this manner, clients have the opportunity to discover whether uncertainty-inducing situations do in fact consistently lead to negative outcomes, whether those outcomes are catastrophic, and whether they are able to cope with any negative outcomes, if any. The development of balanced beliefs therefore occurs through direct testing and the accrual of discomfirmatory disconfirmatory evidence through experience. However, given the anxiety-provoking nature of 165 166 Cara R. Dunkley and Melissa Robichaud behavioral experiments, it is helpful to provide clients with a compelling and logical rationale for their use, as in the following dialogue: Therapist: Client: Therapist: In general, we tend to change our beliefs when there is compelling evidence that contradicts our current beliefs and supports alternative beliefs. For example, if I supported a particular political candidate, and you wanted to convert me to support another candidate, how would you sway me? I would probably list the various platforms, credentials, and virtues of my candidate, and discuss your candidate’s weaknesses. Precisely. You would provide evidence that supports your belief and challenges mine. We approach negative beliefs about uncertainty in the same way. You are unlikely to change your mind about the consequences of uncertainty without direct evidence. Unfortunately, your safety behaviors prevent you from finding out what would actually happen if you allowed some uncertainty into your life. For example, if you always look up your exact route before driving somewhere new in order to be sure that you know the way, then you never have the opportunity to find out whether you would have gotten lost without advance directions, or what you would have done if you had lost your way. Behavioral experiments should be planned and intentional, with the client recording (1) the experiment they are conducting, (2) their feared outcome(s), (3) the actual outcome, and (4) how they coped with the situation if the outcome was negative. Table 9.2 provides an example of a behavioral experiment record form. Clients are encouraged to have an air of curiosity about the outcome of experiments, and debriefing within session should adopt the same exploratory tone. Clients can be queried about whether the actual outcome matched the feared Table 9.2. Example of behavioral experiment record form (What did you do?) Deliberately not overpreparing for a work presentation Ordering a meal that you have never tried before Feared outcome (What were you worried would happen?) Actual outcome (What actually happened?) Coping (If outcome was negative, how did you cope?) The presentation will be horrible, and I won’t be able to answer all of the questions. The presentation went well, and I was able to answer most questions without difficulty. No coping was necessary. I won’t like it, I will not be able to eat it, and my friend will judge me. I actually didn’t enjoy what I ordered. I told my friend and he suggested I order something else. I only ate a little bit of the meal I ordered. I asked the waiter for something else, and they gave it to me without any problem. CBT for Generalized Anxiety Disorder outcome; whether the outcome was negative, neutral, or positive; whether it was viewed as catastrophic if the outcome was negative, whether it was viewed as catastrophic; and how they handled a negative outcome if it occurred. Given that belief change is expected to occur only with a preponderance of evidence, it is recommended that multiple sessions be devoted to developing, and then debriefing, behavioral experiments. Every few sessions, the therapist can help the client examine all of the experiments completed to date with the goal of identifying the following overarching conclusions: How often were the outcomes of experiments negative? Neutral? Positive? When the outcomes were negative, how often were they catastrophic? How did you manage negative outcomes when they arose? How do you view your ability to cope when negative outcomes occurred? What conclusions can you draw so far about the accuracy of your negative beliefs about uncertainty? By engaging in this process over the course of several weeks, clients are encouraged to discover that negative outcomes are relatively infrequent, seldom catastrophic, and typically manageable. In addition, it is hoped that clients gain improved self-efficacy and confidence concerning their ability to cope with difficulty through direct experience. Key Points Individuals with GAD tend to hold several negative beliefs about uncertainty and its consequences, including an overestimation of the likelihood and severity of threat in uncertain situations, underestimating of coping with negative outcomes, and a tendency to view uncertainty as unacceptable and unfair. GAD-related safety behaviors designed to reduce or avoid uncertainty maintain negative uncertainty beliefs through the nonoccurrence of feared outcomes and the prevention of corrective information. A primary goal of treatment is to encourage clients to obtain direct evidence about the actual threat of uncertain situations in order to ultimately develop balanced beliefs about uncertainty. This can be accomplished through behavioral experiments. Module 4: Problem-Solving Training Modules 4 and 5 differ from earlier modules due to their treatment focus. Specifically, while previous modules have largely targeted what underlies and maintains excessive worry, the next sections involve interventions that address specific worry content. Each module offers strategies for worries that persist following an extensive focus on shifting negative beliefs about uncertainty. 167 168 Cara R. Dunkley and Melissa Robichaud Module 4 addresses worries about current problems over which clients have some degree of control. Clients are taught that problem-solving is a more practical alternative to worry and are encouraged to target excessive worries about current problems through the active strategy of problem-solving. Problem-solving training involves addressing an individual’s negative problem orientation, followed by education on the effective use of problem-solving skills. Negative Problem Orientation Problem orientation concerns how we view problems and view ourselves as problem solvers. Individuals with a negative problem orientation typically view problems as negative and threatening, anticipate negative outcomes irrespective of effort, and doubt their capacity to solve problems effectively. As a negative problem orientation can impede or block individuals from actually solving their problems, the goal is to improve their problem orientation. There are three main strategies recommended for improving problem orientation: (1) viewing problems as a normal part of life, (2) looking for benefits and opportunities within problems instead of focusing solely on the threatening aspects, and (3) recognizing problems early by using one’s emotions as a cue to be alerted to the presence of a problem in life, and developing a recurrent problems list as a result (see D’Zurilla & Nezu, 2006). Active Problem-Solving Active problem-solving describes the deliberate and rational process of effectively solving a problem through a series of steps, including (1) problem definition, (2) goal formulation, (3) generation of possible solutions, (4) decision making, and (5) solution implementation and verification (see D’Zurilla and Nezu, 2006, for a thorough description of the application of these steps). Individuals with GAD not only tend to have difficulty with the effective use of these skills when dealing with their own worries, but they also struggle with moving forward in the problemsolving process. An emphasis is thus placed on helping them complete each stage and move on to the next by seeking out the best solution given the information at hand, not the “perfect solution.” Key Points After targeting negative beliefs about uncertainty, some clients with GAD continue to experience residual excessive worries about current problems. These worries can be addressed by targeting negative problem orientation and engaging in the effective use of problem-solving skills. Negative problem orientation involves the tendency to view problems as threatening, to be pessimistic about the outcome of problem-solving, and to underestimate one’s problem-solving ability. Clients with GAD can learn to improve their problem orientation by identifying their problems early, CBT for Generalized Anxiety Disorder (cont.) recognizing them as a normal part of life, and shifting their perceptions of problems from threats to potential challenges or opportunities. Problem-solving is an active strategy for managing worries about current problems. Treatment at this stage focuses on teaching clients about the effective use of problem-solving skills. Module 5: Written Exposure This module provides a means of addressing residual excessive worries about hypothetical situations through written exposure. Research has shown that individuals with GAD tend to avoid feared thoughts and corresponding negative emotions in order to reduce distress. Yet attempts to avoid or neutralize distressing thoughts about hypothetical problems prevents clients from learning what would actually happen if they allowed themselves to think about and visualize the situations they fear. The futility of cognitive avoidance should be discussed prior to starting written exposure; specifically, clients are told that attempts to suppress or avoid distressing worries not only tend to be ineffective, but lead to a paradoxical increase in worries. By engaging in written exposure, clients can tackle cognitive avoidance of core fears. This method of exposure enables clients to test the accuracy of two negative beliefs: (1) thinking about worst-case scenarios is dangerous and can heighten the probability of the feared outcome occurring and (2) negative emotions brought on by feared outcomes are dangerous, in that they are overwhelming and will result in a loss of control. Through experiencing and emotionally processing hypothetical worries, clients are able to shift perspective about how realistic the threat of their feared worst-case scenarios actually is. It is worth noting that the goal of this module is not to eliminate worries about distressing feared outcomes (e.g., a loved one dying). Rather, by focusing on worst-case scenarios and reevaluating the actual threat of both the situation and the attendant emotions it engenders, clients are expected to shift their worries from the “front of the mind” (i.e., from a constant worry) to the “back of the mind” (i.e., an upsetting thought that occurs on occasion but is not ever-present). As written exposure targets core fears, it is typically unnecessary for clients to engage in this exercise more than once, since most hypothetical worries tend to from a single core fear. Therapists can help clients identify their worst-case scenario through the use of the following “downward arrow” technique (Provencher et al., 2000; Vasey & Borkovec, 1992): 1. Clients are asked to describe their worry in simple terms (e.g., “What if my partner is involved in a car crash?”). 2. They are then queried, “If your worry came true, what would that mean? What would happen next?” 169 170 Cara R. Dunkley and Melissa Robichaud 3. After the client has responded with the subsequent link in the worry chain (e.g., “He could be seriously injured”), therapists continue to repeat the same question with the intent of getting progressively closer to the worst-case scenario. Once the client is unable to provide an answer to the prompt, the core fear has likely been identified (e.g., “He could die, and I would be alone, overwhelmed with grief and unable to function”). After identifying the core fear, clients are asked to write about their worst-case feared scenario as concretely as possible in the first-person present tense, and to include as much sense imagery as possible (smell, touch, sight, sound, taste) in order to generate a vivid visual image. Clients are asked to complete this exercise consistently for at least a week (e.g., five to six times per week), for approximately 20 minutes on each occasion. After each written exposure session, clients are asked to record the following: (1) level of distress, (2) estimated probability of the feared outcome occurring, (3) estimate of how catastrophic the feared outcome would be, and (4) estimated ability to cope with the feared outcome. As this exercise is often anxiety-provoking for clients, it is helpful to normalize any anticipated distress, provide a cogent rationale, and emphasize the goal of bringing excessive worries about feared hypothetical situations to the back of the mind. Key Points Excessive worries about hypothetical situations can be addressed through written exposure. Clients with GAD tend to engage in cognitive avoidance strategies that not only are futile, but also allow for the maintenance of negative beliefs about their ability to cope with negative emotions and the overestimation of the dangerousness of feared outcomes. Through written exposure, clients can face core fears by repeatedly writing about their feared worst-case scenarios in vivid and concrete visual images. In addition to allowing for a reevaluation of the actual danger of feared scenarios, written exposure can help clients shift their worries about hypothetical situations to the “back of the mind” rather than being a frequent and recurrent worry theme. Module 6: Relapse Prevention The final sessions should focus on reviewing the skills gained throughout treatment and creating a relapse prevention plan. First, therapists can clarify the difference between a lapse and relapse, with a lapse being understood as the result of normal fluctuations in worry and anxiety, and a relapse as a return to pre-treatment symptom levels. A clients’ reaction to, or catastrophic interpretation of, a lapse can influence whether the lapse becomes a relapse; it is thus important to stress that CBT for Generalized Anxiety Disorder occasional increases in worry and anxiety are unavoidable and are not necessarily a sign of relapse. Additional skills to review in this module can include the following: 1. Check-ups for good mental health hygiene. It can be helpful for clients to get in the habit of routinely setting aside 20–30 minutes (weekly or monthly) to evaluate their overall mental health. Useful points to assess can include current level of worry and anxiety, progress with behavioral experiments targeting uncertainty beliefs, review of current exercises and generation of new ones, and evaluation of short- and long-term goals. 2. Identification of at-risk situations. To ensure long-term maintenance of treatment gains, therapists can assist clients in identifying “red flags” that might signal a return of problematic symptoms. This can include specific situations (e.g., sleep difficulties), stressors (e.g., increased work demands), or behaviors (e.g., increased use of safety behaviors). Recognizing warning signs early encourages clients to take action quickly to remediate the situation. 3. Preparation for at-risk situations. Once at-risk situations have been identified, it is helpful for clients to have a plan of action to address the situation. This plan may entail increasing the frequency of mental health check-ins, reengaging with various treatment modules, or getting in touch with their therapist. The overall goal of this module is to ensure not only that clients maintain the gains they have acquired in treatment, but that they also are able to build upon and consolidate those gains over the long term. In essence, by becoming “their own therapist,” clients are encouraged to normalize lapses and manage them independently over the long term. Key Points Relapse prevention involves both the maintenance of treatment gains and preparation for potential lapses in the future. The difference between a lapse and a relapse can be reviewed, with an emphasis on normalizing the occurrence of fluctuations in worry and anxiety over time. It is helpful for clients to have self-led sessions on a consistent basis to review their overall mental health, as well as identify and plan for potential atrisk situations. FURTHER RECOMMENDED READING Hebert, E. A., & Dugas, M. J. (2018). Behavioral experiments for intolerance of uncertainty: Challenging the unknown in the treatment of generalized anxiety disorder. Cognitive and Behavioral Practice, https://doi.org/10.1016/j.cbpra.2018.07.007 Koerner, N., Mejia, T., & Kusec, A. (2017). What’s in a name? Intolerance of uncertainty, other uncertainty-relevant constructs, and their differential relations to worry and generalized anxiety disorder. Cognitive Behavior Therapy, 46, 141–161. 171 172 Cara R. Dunkley and Melissa Robichaud Robichaud, M., & Dugas, M. J. (2015). The generalized anxiety disorder workbook: A comprehensive CBT guide for coping with uncertainty, worry, and fear. New Harbinger. Robichaud, M., Koerner, N., & Dugas, M. J. (2019). Cognitive-behavioral treatment for generalized anxiety disorder: From science to practice. Routledge. REFERENCES American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. Barrett, J., Oxman, T. E., & Gerber, P. D. (1988). The prevalence of psychiatric disorders in primary care practice. Archives of General Psychiatry, 45, 1100–1106. Blazer, D. G., Hughes, D., George, L. K., Schwartz, M., & Boyer, R. (1991). Generalized anxiety disorder. In L. N. Robins & D. A. Regier (Eds.), Psychiatric disorders in America. The Epidemiologic Catchment Area Study (pp. 180–203). Free Press. Bomyea, J., Ramsawh, H., Ball, T. M., Taylor, C. T., Paulus, M. P., Lang, A. J., & Stein, M. B. (2015). Intolerance of uncertainty as a mediator of reductions in worry in a cognitive behavioral treatment program for generalized anxiety disorder. Journal of Anxiety Disorders, 33, 90–94. Borkovec, T. D., Alcaine, O., & Behar, E. (2004). Avoidance theory of worry and generalized anxiety disorder. In R. G. Heimberg, C. L. Turk, & D. S. Mennin (Eds.), Generalized anxiety disorder: Advances in research and practice (pp. 78–108). Guilford Press. Brown, T. A., & Barlow, D. H. (2014). Anxiety and related disorders interview schedule for DSM-5 (ADIS-5) – Adult and lifetime version: Clinical manual. Oxford University Press. Buhr, K., & Dugas, M. J. (2002). The Intolerance of Uncertainty Scale: Psychometric properties of the English version. Behavior Research and Therapy, 40, 931–945. (2006). Investigating the construct validity of intolerance of uncertainty and its unique relationship with worry. Journal of Anxiety Disorders, 20, 222–236. Carleton, R. N. (2016). Into the unknown: A review and synthesis of contemporary models involving uncertainty. Journal of Anxiety Disorders, 39, 30–43. Davey, G. C. (1994). Worrying, social problem-solving abilities, and social problem-solving confidence. Behaviour Research and Therapy, 32, 327–330. Dugas, M. J., Brillon, P., Savard, P., Turcotte, J., Gaudet, A., Ladouceur, R., Leblanc, R., & Gervais, N. J. (2010). A randomized clinical trial of cognitive-behavioral therapy and applied relaxation for adults with generalized anxiety disorder. Behavior Therapy, 41, 46–58. Dugas, M. J., Buhr, K., & Ladouceur, R. (2004b). The role of intolerance of uncertainty in etiology and maintenance. In R. G. Heimberg, C. L. Turk, & D. S. Mennin (Eds.), Generalized anxiety disorder: Advances in research and practice. Guilford Press, 143–163. Dugas, M. J., Freeston, M. H., & Ladouceur, R. (1997). Intolerance of uncertainty and problem orientation in worry. Cognitive Therapy and Research, 21, 593–606. Dugas, M. J., Gagnon, F., Ladouceur, R., & Freeston, M. H. (1998). Generalized anxiety disorder: A preliminary test of a conceptual model. Behaviour Research and Therapy, 36(2), 215–226. Dugas, M. J., Laugesen, N., & Bukowski, W. M. (2012). Intolerance of uncertainty, fear of anxiety, and adolescent worry. Journal of Abnormal Child Psychology, 40, 863–870. Dugas, M. J., Ladouceur, R., Léger, E., Freeston, M. H., Langlois, F., Provencher, M. D., et al. (2003). Group cognitive-behavioral therapy for generalized anxiety disorder: Treatment outcome and long-term follow-up. Journal of Consulting and Clinical Psychology, 71, 821–825. CBT for Generalized Anxiety Disorder Dugas, M. J., Savard, P., Gaudet, A., Turcotte, J., Laugesen, N., Robichaud, M., Francis, K., & Koerner, N. (2007). Can the components of a cognitive model predict the severity of generalized anxiety disorder? Behavior Therapy, 38, 169–178. Dugas, M. J., Schwartz, A., & Francis, K. (2004a). Intolerance of uncertainty, worry, and depression. Cognitive Therapy and Research, 28, 835–842. D’Zurilla, T. J., & Nezu, A. M. (2006). Problem-solving therapy: A positive approach to clinical intervention (3rd ed.). Springer Publishing. First, M. B., Williams, J. B. W., Karg, R. S., & Spitzer, R. L. (2016). Structured Clinical Interview for DSM-5 Disorders – Clinician version (SCID-5-CV). American Psychiatric Association Publishing. Fracalanza, K., Koerner, N., & Antony, M. M. (2014). Testing a procedural variant of written imaginal exposure for generalized anxiety disorder. Journal of Anxiety Disorders, 28, 559–569. Hebert, E. A., & Dugas, M. J. (2018). Behavioral experiments for intolerance of uncertainty: Challenging the unknown in the treatment of generalized anxiety disorder. Cognitive and Behavioral Practice, https://doi.org/10.1016/j.cbpra.2018.07.007 Hebert, E. A., Dugas, M. J., Tulloch, T. G., & Holowka, D. W. (2014). Positive beliefs about worry: A psychometric evaluation of the Why Worry-II. Personality and Individual Differences, 56, 3–8. Hunt, C., Issakidis, C., & Andrews, G. (2002). DSM-IV generalized anxiety disorder in the Australian National Survey of Mental Health and Well-Being. Psychological Medicine, 32, 649–659. Koerner, N., & Dugas, M. J. (2006). A cognitive model of generalized anxiety disorder: The role of intolerance of uncertainty. In G. C. L. Davey & A. Wells (Eds.), Worry and its psychological disorders: Theory, assessment and treatment. Wiley, 201–216. Ladouceur, R., Blais, F., Freeston, M. H., & Dugas, M. J. (1998). Problem solving and problem orientation in generalized anxiety disorder. Journal of Anxiety Disorders, 12, 139–152. Ladouceur, R., Dugas, M. J., Freeston, M. H., Rhéaume, J., Blais, F., Boisvert, J.-M., et al. (1999). Specificity of generalized anxiety disorder symptoms and processes. Behavior Therapy, 30, 191–207. Ladouceur, R., Gosselin, P., & Dugas, M. J. (2000). Experimental manipulation of intolerance of uncertainty: A study of a theoretical model of worry. Behavior Research and Therapy, 38, 933–941. Meeten, F., Dash, S. R., Scarlet, A. L. S., & Davey, G. C. L. (2012). Investigating the effect of intolerance of uncertainty on catastrophic worrying and mood. Behavior Research and Therapy, 50, 690–698. Meyer, T. J., Miller, M. L., Metzger, R. L., & Borkovec, T. D. (1990). Development and validation of the Penn State Worry Questionnaire. Behavior Research and Therapy, 28, 487–495. Ovanessian, M. M., Koerner, N., Antony, M. M., & Dugas, M. J. (2018). A preliminary test of the therapeutic potential of written exposure with rescripting for generalized anxiety disorder [Manuscript submitted for publication]. Provencher, M. D., Freeston, M. H., Dugas, M. J., & Ladouceur, R. (2000). Catastrophizing assessment of worry and threat schemata among worriers. Behavioral and Cognitive Psychotherapy, 28, 211–224. Robichaud, M., & Dugas, M. J. (2005a). Negative problem orientation (part I): Psychometric properties of a new measure. Behavior Research and Therapy, 43, 391–401. (2005b). Negative problem orientation (part II): Construct validity and specificity to worry. Behavior Research and Therapy, 43, 403–412. Robichaud, M., Dugas, M. J., & Conway, M. (2003). Gender differences in worry and associated cognitive-behavioral variables. Journal of Anxiety Disorders, 17, 501–516. 173 174 Cara R. Dunkley and Melissa Robichaud Robichaud, M., Koerner, N., & Dugas, M. J. (2019). Cognitive-behavioral treatment for generalized anxiety disorder: From science to practice. Routledge. Sexton, K. A., & Dugas, M. J. (2008). The Cognitive Avoidance Questionnaire: Validation of the English translation. Journal of Anxiety Disorders, 22, 355–370. Stein, M. B., & Heimberg, R. G. (2004). Well-being and life satisfaction in generalized anxiety disorder: Comparison to major depressive disorder in a community sample. Journal of Affective Disorders, 79, 161–166. Vasey, M. W., & Borkovec, T. D. (1992). A catastrophizing assessment of worrisome thoughts. Cognitive Therapy and Research, 16, 505–520. Wittchen, H.-U., Kessler, R. C., Beesdo, K., Krause, P., Höfler, M., & Hoyer, J. (2002). Generalized anxiety and depression in primary care: Prevalence, recognition, and management. Journal of Clinical Psychiatry, 63, 24–34. Wittchen, H.-U., Zhao, Z., Kessler, R. C., & Eaton, W. W. (1994). DSM-III-R generalized anxiety disorder in the National Comorbidity Survey. Archives of General Psychiatry, 51, 355–364. PART TWO COGNITIVE BEHAVIORAL THERAPY FOR POSTTRAUMATIC STRESS DISORDER 10 CBT for PTSD Lily A. Brown and Edna B. Foa Research Supporting CBT for PTSD A handful of cognitive behavioral therapies (CBTs) for PTSD have achieved significant empirical support. The most studied CBTs are prolonged exposure (PE) therapy (Foa et al., 2007), cognitive processing therapy (CPT; Resick & Schnicke, 1992), and cognitive therapy (CT; Ehlers & Clark, 2000). While other evidence-based therapies for PTSD exist, including eye-movement desensitization and reprocessing (EMDR; Shapiro, 2001) and present-centered therapy (PCT; Schnurr et al., 2007), these therapies do not fall under the domain of CBT either because of therapeutic content (in the case of PCT) or because of preference from the treatment developer (in the case of EMDR). There have been several meta-analyses that have attempted to determine the efficacy of CBT on PTSD. One recent meta-analysis found that across all CBTs for PTSD, there was a medium effect on PTSD symptoms (Hedges’ g = 0.48, 95% CI: 0.26, 0.71) and a small effect on depression (Hedges’ g = 0.32, 95% CI: 0.18, 0.46), general anxiety (Hedges’ g = 0.38, 95% CI: 0.23, 0.54), and quality of life (Hedges’ g = 0.24, 95% CI: 0.02, 0.47) relative to placebo control (Carpenter et al., 2018). Individual CBT outperformed group CBT for PTSD; however, CBT was associated with significantly higher dropout (29%) compared with placebo (17%; Carpenter et al., 2018). Another meta-analysis separated effects by type of CBT for PTSD. This study found that exposure therapy, including PE (Cohen’s d = 1.27, 95% CI: 1.00, 1.54), CPT (Cohen’s d = 1.40, 95% CI: 0.85, 1.95), and CT (Cohen’s d = 1.33, 95% CI: 0.67, 1.99) each had strong reductions on PTSD symptoms (Cusack et al., 2016). Prolonged exposure outperformed relaxation for PTSD, but there were no other outcome differences among the CBTs (Cusack et al., 2016). These findings replicated an early study in which PE significantly outperformed control conditions in terms of both PTSD outcomes (Hedge’s g = 1.08; 95% CI: 0.69, 1.46) and secondary clinical characteristics (Hedges’ g = 0.77, 95% CI: 0.53, 1.01; Powers et al., 2010). A fourth meta-analysis found that internet-delivered CBT for PTSD outperformed treatment as usual (Hedges’ g = 0.71, 95% CI: 0.49, 0.93; Sijbrandij et al., 2016). Thus, there is sufficient evidence to conclude that CBT is associated with significantly greater 177 178 Lily A. Brown and Edna B. Foa reductions in PTSD symptoms and secondary targets compared with control conditions, and CBT can be effectively delivered in diverse contexts. The efficacy of CBT for PTSD has been established across a wide range of populations. In adolescents, PE is associated with significantly greater reductions in PTSD symptoms compared with supportive counseling (Foa et al., 2013b). Both PE and CPT have demonstrated efficacy in veteran (Acierno et al., 2017; Sloan et al., 2018) and military samples (Foa et al., 2018; P. A. Resick et al., 2017). Survivors of sexual assault respond well to both PE and CPT compared with minimal attention or supportive counseling (Foa et al., 1991; P. A. Resick et al., 2002). Similar results have emerged across various cultures and international locations (Asukai et al., 2010; Schiff et al., 2015; Valentine et al., 2017) There is also a growing evidence base to suggest that CBT for PTSD is effective for complex comorbidities. For example, PE and CPT are both associated with significant reductions in suicidal ideation over time (Bryan et al., 2016; Cox et al., 2016), though most randomized controlled trials for PTSD exclude participants with more than mild suicidal ideation. PE is also effective in patients with a concurrent alcohol use disorder (Foa et al., 2013a), substance use disorders (Ruglass et al., 2017), or a tobacco use disorder (Foa et al., 2017). Similarly, PE is effective in individuals with psychosis (Grubaugh et al., 2017). Both CPT and PE have preliminary efficacy for those with traumatic brain injury (Ragsdale & Voss Horrell, 2016; Wolf et al., 2015). The literature on CBT for PTSD and comorbid conditions is likely to grow in coming years, as several studies to this effect are already underway. Summary: There are several evidence-based treatments for PTSD, including prolonged exposure therapy (PE), cognitive processing therapy (CPT), and cognitive therapy (CT). These treatments consistently outperform control conditions, but there are few differences between active CBTs. KEY READING Cusack, K., Jonas, D. E., Forneris, C. A., Wines, C., Sonis, J., Middleton, J. C., . . . & Gaynes, B. N. (2016). Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychology Review, 43, 128–141. Carpenter, J. K., Andrews, L. A., Witcraft, S. M., Powers, M. B., Smits, J. A. J., & Hofmann, S. G. (2018). Cognitive behavioral therapy for anxiety and related disorders: A meta-analysis of randomized placebo-controlled trials. Depression and Anxiety. doi:10.1002/da.22728 Powers, M. B., Halpern, J. M., Ferenschak, M. P., Gillihan, S. J., & Foa, E. B. (2010). A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review, 30(6), 635–641. doi:10.1016/j.cpr.2010.04.007 Clinical Management of PTSD In the remainder of this chapter, we will discuss the clinical management of PTSD from a CBT orientation. We will discuss issues related to assessment and CBT for PTSD formulation, and we will provide an overview of the treatment. A vignette of a fictitious but realistic case is provided throughout to facilitate comprehension. While many similar chapters could be written from a CPT or CT approach, we base our discussion in the PE approach. However, many of the core concepts will be shared across variants of CBT for PTSD. Assessment Evidence-based assessment of PTSD is a required component of CBT for PTSD. In this section, we provide suggestions for administering state-of-the-science assessments of PTSD. We review considerations for conducting a standardized assessment to derive an initial PTSD diagnosis and provide recommendations for assisting in this diagnosis. In addition, we include a discussion of strategies for determining patient readiness for CBT. Finally, we discuss approaches to monitor progress throughout CBT. Preliminary Diagnosis The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2013a) and the PTSD Severity Scale Interview for DSM-5 (PSSI-5; Foa et al., 2016a) are two empirically supported and widely used clinical interviews for diagnosing PTSD in adults. Both the CAPS-5 and the PSSI-5 have strong psychometric properties (Foa et al., 2016a; Weathers et al., 2013a). Assessors using either measure consider intensity and frequency in evaluating each PTSD symptom. There are several important differences between the measures. First, the CAPS-5 provides a separate section to assess the dissociative subtype of PTSD, a new subcategory of PTSD that was introduced in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5; American Psychiatric Association, 2013), whereas the PSSI-5 includes only a single item to assess for dissociation. Second, the CAPS-5 is always administered in conjunction with the Life Events Checklist (Weathers et al., 2013b), a self-report questionnaire, in order to facilitate identification of the index trauma (i.e., the most distressing trauma at the time of assessment). In contrast, the PSSI-5 identifies the index trauma through several items at the beginning of the administration. Finally, whereas both measures have been developed for diagnosing current (i.e., past month) PTSD, the CAPS-5 also has a version to test for past week and worst point (lifetime) symptoms. Both measures are used across research and clinical settings alike and are available on request (CAPS-5: www.ptsd.va.gov/professional/assessment/ncptsd-instrumentrequest-form.asp; PSSI-5: email foa@pennmedicine.upenn.edu). While a formal standardized clinical interview is the ideal method for determining PTSD, many clinicians may be unable to administer these measures due to constraints on time or resources. In these cases, the PTSD Diagnostic Scale for DSM-5 (PDS-5; Foa et al., 2016b) and the PTSD Checklist for DSM-5 (PCL-5; Blevins et al., 2015) are two commonly used self-report screening measures to identify which patients that should receive a formal PTSD assessment. 179 180 Lily A. Brown and Edna B. Foa As mentioned above, the index trauma is the most distressing trauma at the time of the assessment. However, many patients with PTSD have been exposed to repeated trauma or to more than one type of trauma. In these cases, it may be helpful to validate that the patient is not being asked to make a judgment as to which trauma was the “worst.” Instead, the patient is asked to indicate which trauma is distressing them most at the time of the assessment. This can be facilitated by querying about whether the patient has been most bothered by particular intrusive thoughts or nightmares in the past month, or if there are places that they are avoiding due to reminders of a specific trauma memory. For patients who feel equally bothered by multiple trauma memories, choosing one to start with in therapy will likely result in a generalization of learning to their other memories. Therefore, choosing one trauma to assess is a suitable approach in these cases. Beyond assessing general symptoms of PTSD, it is often useful to formally assess negative post-trauma cognitions because they are critical mediators of change in PTSD symptoms in treatment (McLean et al., 2015a, 2015b). In other words, reductions in negative cognitions often precede and lead to reductions in PTSD symptoms. The Posttraumatic Cognitions Inventory (PTCI; Foa et al., 1999) is a measure of three types of negative post-trauma cognitions, namely, negative cognitions about the self, negative cognitions about the world, and self-blame. This measure has strong psychometric properties (Foa et al., 1999) and is available on request (email foa@pennmedicine.upenn.edu). Assessing Readiness for CBT for PTSD During CBT for PTSD trainings, clinicians commonly request guidelines for assessing whether a given treatment is appropriate for the patient. Despite the abundance of discussion in the literature on this topic, there are few studies well suited to address this empirical question; however, the literature base on the topic is growing (for relevant studies on suicide, see Cox et al., 2016; for relevant studies on alcohol use, see Foa et al., 2013a). The challenge with identifying robust moderators of treatment (the variables that dictate whether someone is likely to respond to treatment or not) is that randomized controlled trials often have exclusion criteria that limit variance in the sample. While we await the literature to expand in this area, we present a few key readiness indicators that are likely to be relevant for the average patient with PTSD. The first indicator of readiness for CBT for PTSD is a willingness to focus on PTSD, largely to the exclusion of other topic areas, for the duration of the treatment. Most CBT protocols are flexible to adapt to unexpected emergencies and atypical circumstances, such as the death of a loved one or the breakup of a romantic relationship. Deviation from the protocol is recommended as needed during these rare circumstances to provide support. However, patients should be willing to dedicate most of their treatment time to addressing PTSD. The second indicator of readiness for CBT is willingness to engage in the treatment components, which may become apparent only after discussing treatment expectations. CBT for PTSD All psychotherapy focused on treating PTSD, including CBT, can be emotionally challenging; however, most patients can decide whether they are ready for the treatment after they are provided with information about the treatment format, content, and about PTSD in general. The third indicator of readiness for CBT is whether the patient is reasonably unlikely to be retraumatized. This concern most frequently, though not exclusively, arises in cases of domestic violence or familial abuse. If there is a significant risk that the patient will be retraumatized regularly (e.g., the patient is still living with an abusive partner or family member), the patient’s immediate safety needs to be prioritized prior to engaging in CBT. However, the therapist need not wait until conditions of guaranteed safety are met, as this may be unachievable. For example, if a patient lives in an unsafe neighborhood but is at no greater risk of exposure to trauma than their neighbors, they could still be eligible for CBT. As untreated PTSD can increase risk-taking behaviors (American Psychiatric Association, 2013), it may be very important to proceed with treatment in such circumstances. Additional considerations are required for some comorbid behaviors and diagnoses in determining readiness for CBT for PTSD. In therapist workshops, clinicians frequently ask about two common comorbidities or secondary conditions: substance use and suicide risk. These are common concerns because individuals with PTSD are significantly more likely both to abuse substances (Yalch et al., 2018) and to report suicidal thoughts and behaviors (Brown et al., 2016, 2018) compared with individuals without PTSD. Therefore, therapists providing CBT for PTSD often need to consider the management of substance use and suicide risk. In terms of substance use, a medical evaluation may be useful for determining whether the patient requires medical detoxification prior to engaging in CBT. Otherwise, CBT may be appropriate for patients who are willing to abstain from substance use for at least two hours before and after engaging in therapy and homework practice. The period of required abstinence may be longer depending on the substance of use. In terms of suicide risk, patients who have engaged in nonsuicidal self-injurious behavior or have made a suicide attempt in the prior two months may be referred for treatment focused on abstaining from these behaviors, including dialectical behavior therapy (DBT; Linehan, 1993). Otherwise, therapists may consider generating a crisis response plan (Bryan et al., 2017) with patients at the beginning of treatment to identify sources of support, problem-solving, and distress tolerance skills to be used as needed. Monitoring Progress throughout CBT for PTSD As with any CBT treatment, the therapist should monitor progress throughout treatment. This typically involves assessment of PTSD symptoms, depression, and key secondary targets (e.g., suicide risk, substance use, interpersonal conflict) approximately every other session. Common measures that are used to this end are the PDS-5 or PCL-5 and the Beck Depression Inventory-II (Beck et al., 1996). Often, clinicians also assess negative post-trauma cognitions using the PTCI on a regular basis in treatment. The therapist asks patients to arrive 10–15 minutes early 181 182 Lily A. Brown and Edna B. Foa for session to complete the self-report measures, which the patient then scores and discusses at the outset of the session. Assessment Summary: Frequent, evidence-based assessment of PTSD and related symptoms is a critical component of CBT for PTSD. Commonly used measures include (1) for clinician interviews, the Clinician-Administered PTSD Scale for DSM-5 (CAPS) and the PTSD Severity Scale Interview for DSM-5 (PSSI-5); (2) for self-report measures, the PTSD Diagnostic Scale for DSM-5 (PDS-5) and the PTSD Checklist for DSM-5 (PCL-5); and (3) for related targets: the Beck Depression Inventory (BDI) and the Posttraumatic Cognitions Inventory (PTCI). Formulation To illustrate a CBT formulation of PTSD, we provide the realistic but fictional case vignette of Joyce. We present some background information, describe the process of assessment and conceptualization of a treatment plan, and provide an example of the socialization process to the therapeutic model. We opted to provide a formulation for a case that is appropriate for PE, though many features of this formulation would extend to other variants of CBT for PTSD. Background Information Joyce is a married, 35-year-old pharmacist with two children under the age of 10. She presented for treatment approximately three years following an armed robbery at her place of work. Joyce reported that one evening, a man and woman entered the pharmacy; about five minutes later, the customers brandished loaded guns and demanded opiates and money from the cash register. The perpetrators threatened to kill Joyce and her assistant, Bill, if their demands were not met. At some point during the robbery, Joyce attempted to press the emergency button under the counter to alert the police. The female perpetrator witnessed Joyce’s attempt to alert the authorities, and hit her over the head with a pistol. Joyce’s head bled profusely as she waited for the perpetrators to collect the money and pills. The robbers threatened Joyce and Bill that if they did not wait at least five minutes to call the police, the robbers would return on a later date and kill them. In addition to the pain of the assault, Joyce felt horrified and helpless. After the robbers left, she broke down sobbing on the floor of the pharmacy from terror and shock. Bill, who also appeared shocked and fearful, said nothing throughout the robbery; he ran to the emergency button to contact the police as soon as the robbers exited. Joyce remembered screaming, “What have you done?” to Bill as he pressed the button and the alarm sounded. She reported feeling even more panicked at this point for fear that the robbers would return to murder her and Bill in retaliation. CBT for PTSD 183 Table 10.1. Joyce’s baseline assessment scores Date: December 1, 2017 Score PTSD Severity Scale Interview for DSM-5 (PSSI-5) PTSD Severity Scale for DSM-5 (PDS-5) Beck Depression Inventory (BDI) Posttraumatic Cognitions Inventory (PTCI) 60 55 32 140 Joyce telephoned the PTSD clinic requesting to discuss the aftermath of this trauma. She reported that she was on medical leave from her job intermittently due to fears of being retraumatized. When she was at work, she visually scanned the store for signs of threat and positioned her workstation to be closer to the emergency response button. Joyce identified that the feeling of not being safe at work or other places was novel to her; this was a dramatic shift from her pretrauma expectations about danger and safety. Since the robbery, she struggled with feeling constantly anxious and had extreme sleeping difficulties, which motivated her to seek help. The therapist agreed to meet with Joyce for a formal evaluation. At the time of the evaluation, Joyce’s therapist described that they would complete a formal assessment to understand the ways in which Joyce’s life was affected by the trauma. The therapist completed the PSSI-5 with Joyce. On this measure, Joyce endorsed nearly every symptom. Beyond those already reported, Joyce avoided being in crowded places, doing the shopping for the family, and intimacy with her husband. She reported that there were times when she could not control her emotions at work, resulting her “breaking down crying” in front of customers and coworkers. She reported trying to distract herself constantly to avoid remembering the trauma and “how close she had come to dying.” When she slept, she was plagued by nightmares of the trauma and generally bad dreams. She also endorsed feelings of self-blame and negative post-trauma cognitions. These included beliefs that she should have acted more quickly to press the emergency button, that she should have known that the two customers were dangerous as soon as they entered the store. She also felt guilty for feeling angry with Bill for pressing the emergency response button as soon as the robbers left the store. Finally, she reported thinking that her perception of danger and safety had been warped since the trauma, and that nowhere felt safe. Considering these negative trauma-related cognitions, the therapist administered the PTCI to assess whether Joyce endorsed other key areas of cognition alterations. Joyce’s baseline assessment scores are provided in Table 10.1. Formulation From the perspective of emotional processing theory (EPT; Foa & Kozak, 1986), the theoretical model from which PE therapy was derived, the robbery and assault resulted in the formation of an emotional cognitive structure. This structure included negative associations between previously neutral stimuli (e.g., her 184 Lily A. Brown and Edna B. Foa place of work, being in stores in general) and a sense of danger. Her trauma structure also included negative self-perceptions stemming from her responses during and after the trauma. Joyce expected that if she was at work or at another store, she was very likely to be hurt again. This expectation contributed to her avoidance of scenarios where she felt unsafe. Unfortunately, continuing to avoid these situations also resulted in the maintenance of her fear and shame. According to EPT and PE, PTSD symptoms are maintained because avoidance (1) becomes habitual, (2) prevents learning that situations Joyce feels are dangerous are indeed safe, (3) prevents learning that anxiety will diminish over time, and (4) promotes negative trauma-related cognitions. Relatedly, Joyce described engaging in frequent avoidance of the memory of the trauma. Despite feeling that she wanted to think of anything else, she described being constantly preoccupied by thoughts of the robbery. As a result, Joyce attempted to distract herself with music, television, or browsing the internet – anything to keep her from remembering the trauma. As with avoidance of real-world situations, avoidance of the trauma memory prevents Joyce from emotionally processing the trauma. According to EPT and PE, avoidance of the trauma memory results in (1) a disorganized trauma memory, (2) confusion about the trauma recurring versus being remembered, (3) missed opportunities for anxiety to diminish over time, (4) the promotion of negative associations about the trauma and similar events that result in altered perceptions of danger and safety, and (5) the promotion of negative post-trauma cognitions. Socialization to PE When coming to a clear formulation of the factors that are maintaining Joyce’s symptoms of PTSD, it is important to share this formulation with the patient. In so doing, it is critical to provide a rationale justifying why the selected treatment, in this case PE, is ideal for her. Therapists should ensure that the patient understands the treatment model prior to formally beginning therapy. This can often be accomplished with a 15–20-minute conversation following the assessment, especially because psychoeducation and rationale are provided on an ongoing basis on beginning the treatment. The following is an example of such a socialization conversation between Joyce and her therapist. Therapist: Thank you for sharing the details of the robbery and the ways in which it affects you today. It is very brave for you to come in and talk about this. I know that you have told me how tempting it is to pretend as if the trauma never happened; today, you took an important first step in starting to process what happened to you. In fact, talking about what you have been through is an important component of prolonged exposure therapy, or PE, for PTSD. I am going to tell you a bit about PE so that you can decide if you are willing to give the therapy a try. Does that sound okay to you? CBT for PTSD Joyce: Therapist: Joyce: Therapist: 185 Yes, I would like that. I have already tried so many things to manage my PTSD, and none of it has worked. At this point, I am ready to try anything. It is very common for individuals to try to manage their PTSD on their own for some time before coming to therapy. I know that in your case, you have been suffering with this problem for over three years, and I am very pleased to hear that you are open to trying a new way of dealing with this. For you to decide whether you want to start this therapy, you first need to know what the therapy entails. I am going to give you an overview of PE today and I will give you plenty of time to ask any questions about it. You do not need to decide today whether this is a therapy that you want to pursue; we can even meet again to discuss it in more detail before you decide. If you do decide to start PE, we will revisit some of the information that I am about to share with you as we go through the treatment together. Today, I will just briefly introduce you to the therapy. PE is a time-limited therapy that is typically completed in eight to fifteen ninety-minute treatment sessions. Occasionally, some patients complete the treatment in fewer than eight sessions, and occasionally some patients complete the treatment in more than twelve sessions. To date, there are over twenty clinical trials that demonstrate PE reduces PTSD and related symptoms, including depression and relationship problems. Many of the people in PE studies had similar symptoms to yours and were survivors of assaults and robberies. For this reason, I am very hopeful that this treatment will be very helpful for you. I had assumed that most of the people that you have worked with would be combat veterans – that is really all that I knew about PTSD before the robbery. It is comforting to hear that people like me have been through this before too. Yes, I often hear that. In fact, PE was developed broadly for individuals with PTSD stemming from a variety of traumatic events. The treatment directly targets the core symptoms of PTSD, regardless of the type of trauma that initiated the PTSD. Throughout the treatment, you and I will work together to identify the ways in which your life has changed since the trauma, and we will plan for how to get your life headed in the direction that you want. For instance, you told me that since the trauma, there are many things that you no longer do, like going to work or shopping, because you fear being hurt again. This is very common for individuals with PTSD. In PE, you and I would use what we call “in vivo exposure exercises.” These exercises will assist you in 186 Lily A. Brown and Edna B. Foa approaching people, places, and situations that, despite being objectively safe, have made you feel anxious since the trauma. We will go at a pace that feels reasonable to you and I will guide you through the process. We would also use imaginal exposure exercises to help you to emotionally process the robbery. This is important because while you try very hard not to think of the robbery, you also told me that you find yourself having intrusive thoughts of it frequently throughout the day. Imaginal exposure will help digest the experience of the robbery, which is now unfinished business. Both in vivo and imaginal exposures will help to reduce anxiety, change negative beliefs that you have about yourself and the world, and help to regain a sense of empowerment. As we continue throughout the treatment, you will complete practice exercises between sessions, which will include listening to audio recordings of your therapy sessions and practicing in vivo exposure exercises on your own. You will also complete questionnaires every couple of sessions so that we can see how your symptoms are changing over time. Do you have any questions about this? In some circumstances, scheduling one to three pre-treatment sessions can provide an opportunity for rapport building, answering questions, or ensuring that appropriate clinical management strategies are in place. For instance, the therapist may consider using this time to construct a crisis response plan with a patient or to orient them to monitoring of substance use in treatment, as relevant. These preparatory sessions can facilitate a smooth introduction into the treatment and help patients decide whether they are interested and willing to participate in the treatment. Formulation and Socialization Summary. It is critical to link your formulation of the patient’s symptoms to the rationale for treatment. Provide a transparent but brief description of what the patient can expect should they decide to complete the treatment. Occasionally, it may be necessary to schedule one to three preparatory sessions to build rapport and ensure that the patient is ready for treatment. Overview of Therapy Joyce’s therapy overview is presented in Table 10.2; this table includes information about the session content, Joyce’s reaction to the content, and her progress. In total, Joyce attended nine 90-minute sessions of PE for PTSD. Throughout the treatment, which included a combination of psychoeducation, breathing retraining, imaginal exposure and processing, and in vivo exposure, Joyce reported significant habituation in PTSD symptom severity, depression, and negative post-trauma cognitions. CBT for PTSD 187 Table 10.2. Session content Session Content Assessments 1: December 27, 2017 Psychoeducation The therapist described that most individuals exposed to a trauma have symptoms of PTSD in the immediate aftermath of the trauma, but for many of them, those symptoms resolve on their own. Those who go on to develop PTSD are often experts at avoiding reminders of the trauma. Joyce’s examples include working, shopping, and thinking about the trauma in general, among others. Trauma history interview Joyce provided enough details about her traumatic event to determine the starting and stopping point of the trauma. She described the physical, emotional, cognitive, and legal consequences of the trauma. Breathing retraining The therapist taught Joyce how to slow down her breathing. Assigned homework PDS-5 = 56 BDI = 31 PTCI = 140 1. Listen to audio recording of the full session. 2. Read treatment rationale. 3. Practice breathing retraining. 2: January 3, 2018 Homework review Joyce listened to nearly the entire session audio recording and practiced the breathing retraining twice. She also read the assigned homework and asked a few questions about the material. Common reactions to trauma The therapist described the common reactions to trauma and discussed the ones of high relevance to Joyce’s experience. In vivo exposure rationale The therapist described an in-depth rationale for using in vivo exposure, drawing on examples from Joyce’s life experiences. Introduction to subjective units of distress (SUDs) The therapist explained the concept of SUDs to Joyce and identified key anchor points. These anchors reflected times when Joyce’s distress was at 100, 50, and 0. These anchor points are used to gauge future distress ratings. Construction of in vivo hierarchy Joyce and her therapist generated a list of 12 items for her hierarchy (see Table 10.3). The therapist queried about examples of strategies to make each of those exercises more or less difficult. After generating this list, Joyce and the therapist made SUDs ratings for each item on the list. They selected an item that was rated as a 40 – going to a small gift store in the early afternoon – to practice three times. They also selected a behavioral activation item of taking a walk three times. Assigned homework 1. 2. 3. 4. 5. Listen to audio recording of the full session. Read common reactions to trauma worksheet. Practice breathing retraining. Complete in vivo exposure homework exercise. Review hierarchy and make alterations as needed. 188 Lily A. Brown and Edna B. Foa Table 10.2. (cont.) Session Content Assessments 3: January 10, 2018 Homework review Joyce listened to the entire session audio recording and practiced the breathing retraining one. She completed her first in vivo exercise three times, and the second exercise twice. She reviewed her hierarchy and added two items to the list. She read through the common reactions to trauma worksheet. The therapist provided her with a lot of praise for completing the exercises as prescribed. Imaginal exposure rationale The therapist provided an in-depth rationale for imaginal exposure. Joyce asked questions about this and reported feeling very nervous but willing to try it. Imaginal exposure Joyce completed an imaginal exposure exercise for 41 minutes. She repeated the exposure three times. Her initial rendition was somewhat disconnected and devoid of emotional expression, but she became tearful throughout the second rendition. Her tearfulness subsided by the third rendition. Processing The therapist praised Joyce for her bravery in conducting the imaginal exposure. She asked open-ended questions to explore Joyce’s emotional reaction to the imaginal exposure. Joyce described feeling terrified during the robbery and angry at her coworker for not following the assailants’ orders. Core cognitions that emerged from the processing centered on beliefs such as “I am helpless” and “This could happen to me at any time.” Homework Assigned PDS-5 = 52 BDI = 31 PTCI = 137 Pre-imaginal SUDs = 88 Peak imaginal SUDs = 95 Post-imaginal SUDs = 80 1. 2. 3. 4. 4: January 17, 2018 Listen to audio recording of the full session. Practice breathing retraining. Complete in vivo exposure homework exercise. Listen to imaginal exposure daily. Homework review Joyce listened to the entire session audio-recording but did not practice her breathing retraining. She completed her assigned in vivo exercise four times: peak SUDs scores were 75, 70, 70, and 69. She listened to the imaginal exposure on two additional occasions beyond the full tape review, for a total of three times. Her peak SUDs ratings were 89, 88, 86, and 86. Imaginal exposure Joyce completed an imaginal exposure exercise for 40 minutes. As with session 3, she repeated the exposure three times. She was tearful throughout the first rendition, but less tearful during the second and third rendition. Processing The therapist praised Joyce again. As usual, she asked open-ended questions to explore Joyce’s emotional reaction to the imaginal exposure. Joyce reported some surprise that the exercise was not as difficult as on the prior session. Homework assigned See session 3. Pre-imaginal SUDs = 80 Peak imaginal SUDs = 85 Post-imaginal SUDs = 69 CBT for PTSD 189 Table 10.2. (cont.) Session Content Assessments 5: January 24, 2018 Homework review Joyce completed all her homework. For in vivo exposure, her peak SUDs scores were 65, 65, 60, and 59. For imaginal exposure, her peak SUDs scores were 80, 65, and 60. Imaginal exposure Joyce completed an imaginal exposure exercise for 40 minutes. As in prior sessions, she repeated the exposure three times. Processing Key themes discussed in processing included habituation of distress over time and Joyce’s shifting sense of threat versus safety. Homework assigned See sessions 3 and 4. PDS-5 = 35 BDI = 19 PTCI = 115 Pre-imaginal SUDs = 65 Peak imaginal SUDs = 75 Post-imaginal SUDs = 50 6: January 31, 2018 Homework review Joyce completed most of her homework. For in vivo exposure, her peak SUDs scores were 55 and 40. For imaginal exposure, her peak SUDs scores were 65, 40, and 35. Imaginal exposure: Hot spots Joyce completed her first hot spot imaginal exposure, wherein a select portion of the most difficult part of the trauma memory was repeated instead of the full trauma memory. She selected one portion of the memory that was approximately four minutes long and repeated it 10 times. Processing Key themes discussed in processing included beliefs about why she had not acted more quickly to press the emergency response button. Homework assigned See sessions 3–5. Pre-imaginal SUDs = 45 Peak imaginal SUDs = 65 Post-imaginal SUDS = 50 7: February 7, 2018 Homework review Joyce completed all her homework. For in vivo exposure, her peak SUDs scores were 40, 40, and 35. For imaginal exposure, her peak SUDs scores were 50, 40, and 30. Imaginal exposure: Hot spots Joyce completed her second round of hot spot imaginal exposure. Processing The key theme discussed in processing was the observation that she has moved on in her life in a positive direction. Homework assigned See sessions 3–6. PDS-5 = 15 BDI = 15 PTCI = 101 Pre-imaginal SUDs = 30 Peak imaginal SUDs = 35 Post-imaginal SUDs = 20 8: February 14, 2018 Homework review Joyce completed most of her homework. For in vivo exposure, her peak SUDs scores were 30, 20, and 15. For imaginal exposure, her peak SUDs scores were 30, 30, and 20. Imaginal exposure: Hot spots Joyce completed her third round of hot spot imaginal exposure. Processing The key theme for discussion was Joyce’s readiness to terminate therapy, and the evidence that she has made significant progress in her symptoms. Homework assigned See sessions 3–7. Pre-imaginal SUDs = 25 Peak imaginal SUDs = 30 Post-imaginal SUDs = 15 190 Lily A. Brown and Edna B. Foa Table 10.2. (cont.) Session Content Assessments 9: February 21, 2018 Homework review Joyce completed all her homework. For in vivo exposure, her peak SUDs scores were 20, 10, and 5. For imaginal exposure, her peak SUDs scores were 20, 15, and 15. Imaginal exposure Joyce completed one final rendition of the full trauma memory from start to finish. Processing Joyce reflected on the difference in emotional upset and negative cognitions from the beginning of treatment to this point in therapy. Progress review and thinking ahead Joyce reported that she feels ready to return to work and can live her life as though she had not been through the robbery/ assault. She reflected on strategies that she needs to continue practicing. Joyce and her therapist terminated therapy. PDS-5 = 9 BDI = 10 PTCI = 75 Pre-imaginal SUDs = 20 Peak imaginal SUDs = 25 Post-imaginal SUDs = 10 Table 10.3. Joyce’s in vivo hierarchy Item Exposure SUDs Session 1 2 3 4 5 5 6 7 8 9 10 Going to a small gift store, 2 p.m. Talking a walk around her neighborhood, noon Watching a TV show about a crime Going to a busy store in a safe neighborhood, 3 p.m. Sitting in a restaurant, in the middle of the room, during lunch Going to a pharmacy in a safe neighborhood, 2 p.m. Going to her work pharmacy at lunch Watching a video of a pharmacy robbery Taking a bus around town Going to her work pharmacy in the evening Going to a new pharmacy in the evening 40 45 50 55 60 60 70 70 80 90 95 2 2 3 3 4 4 5 5 6 6 7, 8 Summary: In following the PE manual, the therapist offered psychoeducation, breathing retraining, in vivo exposure, and imaginal exposure in the treatment of Joyce’s PTSD. Joyce reported significant symptom resolution throughout PE. FOR ADDITIONAL READING Foa, E. B., Hembree, E. A., & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences therapist guide (Treatments that work). Oxford University Press. CBT for PTSD REFERENCES Acierno, R., Knapp, R., Tuerk, P., Gilmore, A. K., Lejuez, C., Ruggiero, K., . . . & Foa, E. B. (2017). A non-inferiority trial of prolonged exposure for posttraumatic stress disorder: In person versus home-based telehealth. Behaviour Research and Therapy, 89, 57–65. doi:10.1016/j.brat.2016.11.009 American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. Asukai, N., Saito, A., Tsuruta, N., Kishimoto, J., & Nishikawa, T. (2010). Efficacy of exposure therapy for Japanese patients with posttraumatic stress disorder due to mixed traumatic events: A randomized controlled study. Journal of Traumatic Stress, 23(6), 744–750. doi:10.1002/jts.20589 Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the Beck Depression InventoryII. Psychological Corporation. Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. doi:10.1002/jts.22059 Brown, L. A. Armey, M. A., Sejourne, C., Miller, I. W., & Weinstock, L. (2016). Suicide risk in psychiatric inpatients with PTSD. Psychiatry Research, 243, 191–197. Brown, L. A., Fernandez, C., Kohn, R., Saldivia, S., & Vincente, B. (2018). Pre-disaster PTSD as a moderator of the relationship between natural disaster and suicidal ideation over time. Journal of Affective Disorders, 230, 7–14. Bryan, C. J., Clemans, T. A., Hernandez, A. M., Mintz, J., Peterson, A. L., Yarvis, J. S., & Resick, P. A. (2016). Evaluating potential iatrogenic suicide risk in trauma-focused group cognitive behavioral therapy for the treatment of PTSD in active duty military personnel. Depression and Anxiety, 33(6), 549–557. doi:10.1002/da.22456 Bryan, C. J., Mintz, J., Clemans, T. A., Leeson, B., Burch, T. S., Williams, S. R., Maney, E., & Rudd, M. D. (2017). Effect of crisis response planning vs. contracts for safety on suicide risk in U.S. Army Soldiers: A randomized clinical trial. Journal of Affective Disorders, 212, 64–72. Carpenter, J. K., Andrews, L. A., Witcraft, S. M., Powers, M. B., Smits, J. A. J., & Hofmann, S. G. (2018). Cognitive behavioral therapy for anxiety and related disorders: A metaanalysis of randomized placebo-controlled trials. Depression and Anxiety. doi:10.1002/ da.22728 Cox, K. S., Mouilso, E. R., Venners, M. R., Defever, M. E., Duvivier, L., Rauch, S. A., . . . & Tuerk, P. W. (2016). Reducing suicidal ideation through evidence-based treatment for posttraumatic stress disorder. Journal of Psychiatric Research, 80, 59–63. Cusack, K., Jonas, D. E., Forneris, C. A., Wines, C., Sonis, J., Middleton, J. C., . . . & Gaynes, B. N. (2016). Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychology Review, 43, 128–141. Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. doi:10.1016/S0005-7967(99)00123-0 Foa, E. B., Asnaani, A., Rosenfield, D., Zandberg, L. J., Gariti, P., & Imms, P. (2017). Concurrent varenicline and prolonged exposure for patients with nicotine dependence and PTSD: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 85, 862–872. doi:10.1037/ccp0000213 Foa, E. B., Hembree, E. A., & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences – Therapist guide. Oxford University Press. Foa, E. B., & Kozak, M. J. (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1), 20–35. 191 192 Lily A. Brown and Edna B. Foa Foa, E. B., McLean, C. P., Capaldi, S., & Rosenfield, D. (2013b). Prolonged exposure vs supportive counseling for sexual abuse–related PTSD in adolescent girls: A randomized clinical trial. JAMA, 310(24), 2650–2657. doi:10.1001/jama.2013.282829 Foa, E. B., McLean, C. P., Zang, Y., Rosenfield, D., Yadin, E., Yarvis, J. S., . . . & Peterson, A. L. (2018). Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel: A randomized clinical trial. JAMA, 319(4), 354–364. doi:10.1001/jama.2017.21242 Foa, E. B., McLean, C. P., Zang, Y., Zhong, J., Rauch, S., Porter, K., . . . & Kauffman, B. Y. (2016a). Psychometric properties of the Posttraumatic Stress Disorder Symptom Scale Interview for DSM-5 (PSSI-5). Psychological Assessment, 28(10), 1159–1165. doi:10.1037/pas0000259 Foa, E. B., McLean, C. P., Zang, Y., Zhong, J., Powers, M. B., Kauffman, B. Y., . . . & Knowles, K. (2016b). Psychometric properties of the Posttraumatic Diagnostic Scale for DSM-5 (PDS-5). Psychological Assessment, 28(10), 1166–1171. doi:10.1037/pas0000258 Foa, E. B., Rothbaum, B. O., Riggs, D. S., & Murdock, T. B. (1991). Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitivebehavioral procedures and counseling. Journal of Consulting and Clinical Psychology, 59(5), 715–723. Foa, E. B., Tolin, D. F., Ehlers, A., Clark, D. M., & Orsillo, S. M. (1999). The posttraumatic cognitions inventory (PTCI): Development and validation. Psychological Assessment, 11, 303–314. Foa, E. B., Yusko, D. A., McLean, C. P., et al. (2013a). Concurrent naltrexone and prolonged exposure therapy for patients with comorbid alcohol dependence and PTSD: A randomized clinical trial. JAMA, 310(5), 488–495. doi:10.1001/jama.2013.8268 Grubaugh, A. L., Veronee, K., Ellis, C., Brown, W., & Knapp, R. G. (2017). Feasibility and efficacy of prolonged exposure for PTSD among individuals with a psychotic spectrum disorder. Frontiers in Psychology, 8, 977. doi:10.3389/fpsyg.2017.00977 Linehan, M. (1993). Cognitive behavior treatment for borderline personality disorder. Guilford Press. McLean, C. P., Su, Y. J., & Foa, E. B. (2015b). Mechanisms of symptom reduction in a combined treatment for comorbid posttraumatic stress disorder and alcohol dependence. Journal of Consulting and Clinical Psychology, 83(3), 655–661. doi:10.1037/ccp0000024 McLean, C. P., Yeh, R., Rosenfield, D., & Foa, E. B. (2015a). Changes in negative cognitions mediate PTSD symptom reductions during client-centered therapy and prolonged exposure for adolescents. Behaviour Research and Therapy, 68, 64–69. doi:10.1016/j. brat.2015.03.008 Powers, M. B., Halpern, J. M., Ferenschak, M. P., Gillihan, S. J., & Foa, E. B. (2010). A metaanalytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review, 30(6), 635–641. doi:10.1016/j.cpr.2010.04.007 Ragsdale, K. A., & Voss Horrell, S. C. (2016). Effectiveness of prolonged exposure and cognitive processing therapy for U.S. veterans with a history of traumatic brain injury. Journal of Traumatic Stress, 29(5), 474–477. doi:10.1002/jts.22130 Resick, P. A. (1992). Cognitive treatment of crime-related post-traumatic stress disorder. In R. D. Peters, R. J. McMahon, & V. L. Quinsey (Eds.), Aggression and violence throughout the life span (pp. 171–191). Sage Publications. Resick, P. A., Nishith, P., Weaver, T. L., Astin, M. C., & Feuer, C. A. (2002). A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology, 70(4), 867–879. Resick, P. A., & Schnicke, M. K. (1992). Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology, 60(5), 748–756. CBT for PTSD Resick, P. A., Wachen, J. S., Dondanville, K. A., Pruiksma, K. E., Yarvis, J. S., Peterson, A. L., . . . & Young-McCaughan, S. (2017). Effect of group vs individual cognitive processing therapy in active-duty military seeking treatment for posttraumatic stress disorder: A randomized clinical trial. JAMA Psychiatry, 74(1), 28–36. doi:10.1001/jamapsychiatry.2016.2729 Ruglass, L. M., Lopez-Castro, T., Papini, S., Killeen, T., Back, S. E., & Hien, D. A. (2017). Concurrent treatment with prolonged exposure for co-occurring full or subthreshold posttraumatic stress disorder and substance use disorders: A randomized clinical trial. Psychotherapy and Psychosomatics, 86(3), 150–161. doi:10.1159/000462977 Schiff, M., Nacasch, N., Levit, S., Katz, N., & Foa, E. B. (2015). Prolonged exposure for treating PTSD among female methadone patients who were survivors of sexual abuse in Israel. Social Work Health Care, 54(8), 687–707. doi:10.1080/00981389.2015.1058311 Schnurr, P. P., Shea, M. T., Friedman, M. J., & Engel, C. C. (2007). Posttraumatic stress disorder and cognitive behavioral therapy – In reply. JAMA, 297(24), 2965. Shapiro, F. (2001). Eye movement desensitization and reprocessing (EMDR): Basic principles, protocols, and procedures (2nd ed.). Guilford Press. Sijbrandij, M., Kunovski, I., & Cuijpers, P. (2016). Effectiveness of internet-delivered cognitive behavioral therapy for posttraumatic stress disorder: A systematic review and metaanalysis. Depression and Anxiety, 33(9), 783–791. doi:10.1002/da.22533 Sloan, D. M., Marx, B. P., Lee, D. J., & Resick, P. A. (2018). A Brief exposure-based treatment vs cognitive processing therapy for posttraumatic stress disorder: A randomized noninferiority clinical trial. JAMA Psychiatry. doi:10.1001/ jamapsychiatry.2017.4249 Valentine, S. E., Borba, C. P., Dixon, L., Vaewsorn, A. S., Guajardo, J. G., Resick, P. A., . . . & Marques, L. (2017). Cognitive processing therapy for Spanish-speaking Latinos: A formative study of a model-driven cultural adaptation of the manual to enhance implementation in a usual care setting. Journal of Clinical Psychology, 73(3), 239–256. doi:10.1002/jclp.22337 Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013a). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). Available from the National Center for PTSD at www.ptsd.va.gov. (2013b). The Life Events Checklist for DSM-5 (LEC-5). Available from the National Center for PTSD at www.ptsd.va.gov. Wolf, G. K., Kretzmer, T., Crawford, E., Thors, C., Wagner, H. R., Strom, T. Q., . . . & Vanderploeg, R. D. (2015). Prolonged exposure therapy with veterans and active duty personnel diagnosed with PTSD and traumatic brain injury. Journal of Traumatic Stress, 28(4), 339–347. doi:10.1002/jts.22029 Yalch, M. M., Hebenstreit, C. L., & Maguen, S. (2018). Influence of military sexual assault and other military stressors on substance use disorder and PTS symptomology in female military veterans. Addictive Behaviors, 80, 28–33. doi:10.1016/j.addbeh.2017.12.026 193 PART THREE COGNITIVE BEHAVIORAL THERAPY FOR OBSESSIVECOMPULSIVE DISORDER AND ASSOCIATED DISORDERS 11 Obsessive-Compulsive Disorder: An Updated Cognitive Behavioral Approach Oliver Sündermann and David Veale Introduction Obsessive-compulsive disorder (OCD) is the fourth most common mental disorder with a lifetime prevalence of 2% (Kessler et al., 2005). The WHO ranks OCD among the 10 most debilitating disorders (2008); OCD affects all cultural groups and is associated with poor quality of life, unemployment, social exclusion, stigma, and suicide risk (Eisen et al., 2006; Hollander & Benzaquen, 1996). Onset tends to be in adolescence or early adulthood, and without adequate treatment, OCD usually takes a chronic course (Fineberg et al., 2013). OCD is poorly recognized, and on average people struggle for 10 years until they receive appropriate help (Hollander et al., 1997). Diagnostic Criteria and Changes in ICD11 and DSM-5 OCD is characterized by the presence of obsessions and/or compulsions, which are time-consuming or cause distress or impairment in various areas of functioning. Obsessions are defined as ‘recurrent and intrusive, urges, or images’, and compulsions are repetitive behaviors or mental acts aimed at preventing or reducing distress caused by the obsessions (DSM-5; American Psychiatric Association, 2013). Obsessions are usually ego-dystonic and recognized as the product of one’s own mind. Common obsessions refer to preventing harm to self and others from contamination (e.g., dirt, germs, bodily fluids, chemicals) or from making a mistake (e.g., not turning off the gas taps); intrusive sexual, religious, or violent thoughts; and obsessions of incompleteness, order, and symmetry. DSM-5 and ICD11 have ‘shifted’ OCD from the anxiety disorders to a new chapter, ‘Obsessive-Compulsive and Related Disorders’, grouped alongside other disorders with seemingly similar phenomenology of repetitive behaviors such as body dysmorphic disorder, trichotillomania, and hypochondriasis. We regard this regrouping as problematic because the groups consist of repetitive behaviors that are only superficially similar (e.g., tics, hair pulling, compulsive checking) but have very different functions. Other anxietyreduction strategies are not captured adequately (e.g., mental neutralizing, avoidance) (Abramowitz & Jacoby, 2014). 197 198 Oliver Sündermann and David Veale CBT Model of OCD A cognitive-behavioral approach to OCD is based on the observation that intrusive thoughts, urges, and images are normal experiences (Rachman & de Silva, 1978 that cause distress through appraisals of personal significance (‘Having bad thoughts means, I am bad’), control (‘I must control my thoughts’), and responsibility (‘I am responsible for preventing harm’) (Salkovskis, 1999). Hence, the difference between a normal intrusion and a clinical obsession lies in the way the person with OCD interprets these and responds to them. Compulsive rituals (covert and overt), avoidance, safety seeking, and neutralizing behaviors (e.g., removing/replacing a thought) are conceptualized as attempts to control or remove intrusions and to avert feared consequences, all of which maintain obsessional distress through negative reinforcement, preventing disconfirmation of threat beliefs, and increase frequency of obsessions because rituals and avoidance act as constant reminders of their occurrence. While environmental and biological factors may increase vulnerability to acquire obsessional concerns (Taylor & Jang, 2011), compulsive responding to them and cognitive biases maintain OCD and are therefore the target in CBT (Abramowitz, 2006). Outcome Research and New Avenues Selective serotonin reuptake inhibitors (SSRIs) are the recommended pharmacological treatment for OCD, but gains typically subside when discontinued (Soomro et al., 2008). The psychological treatment of choice for OCD remains CBT, which refers to exposure and response prevention (E/RP) either with or without cognitive interventions. A recent meta-analysis by Öst et al. (2015) (n = 37 RCTs) found CBT the only effective psychological treatment for OCD, with an overall moderate effect (0.57) on the Yale–Brown Obsessive Compulsive Scale (Y-BOCS) changes from pre- to post-treatment. There were very large effect sizes in favour of CBT compared with wait-list (1.31) and placebo conditions (1.33), with minimal or no differences between individual and group treatments. Findings are generally in line with previous meta-analyses (Abramowitz, 1996; Olatunji et al., 2013; Rosa-Alcázar et al., 2008). Long-term outcome data are limited but promising, with some studies showing that gains from E/RP can be maintained at one year (Olatunji et al., 2013) and at five years (van Oppen et al., 2005). While CBT clearly is an effective intervention for OCD, up to 50% of individuals with OCD do not benefit from CBT, drop out of treatment, or find treatment, especially E/RP, too challenging. Around 75% live with residual symptoms after completing treatment (Abramowitz et al., 2003; Foa et al., 2005; Rufer et al., 2006; Tolin et al., 2004). It also remains unclear how much comorbidity (Öst et al., 2015), heterogeneity of symptoms (Sookman & Fineberg, 2015), and complexity require treatment adaptations (Sündermann & Veale, 2017). CBT-related research has advanced significantly over the last 10 years, and we will briefly describe four areas that we consider promising in informing OCD treatment, namely, (1) an inhibitory Obsessive-Compulsive Disorder learning approach to exposure therapy, (2) disgust in OCD, (3) imagery in OCD, and (4) complex OCD and specialized care. Exposure Therapy and Inhibitory Learning For many years E/RP was theoretically underpinned by emotional processing theory (Foa & Kozak, 1986) according to which conditionally learned obsessional fears are negatively reinforced and perpetuated through avoidance and compulsions. Consequently, the focus in E/RP had been on fear habituation. However, the concept of fear habituation is scientifically problematic because successful habituation of non-OCD fears fails to predict long-term outcomes, and, conversely, positive long-term outcomes can occur in the absence of habituation during E/RP (Craske et al., 2012, 2014). Applying updated knowledge on basic learning and memory processes, inhibitory learning has been suggested as the core mechanism in extinction (Bouton, 1993; Bouton et al., 2006; Vervliet et al., 2013), according to which the originally learned associations between conditioned and unconditioned stimulus remains intact. Therefore, the goal of E/RP should be to enhance inhibitory learning, through maximizing the likelihood that non-danger associations (e.g., ‘Obsessions are meaningless’; ‘Uncertainty is tolerable’) inhibit access and retrieval of threat associations (e.g., ‘Obsessions are unacceptable’; ‘Uncertainty is intolerable’). Principles of inhibitory learning that facilitate extinction involve maximal violation of expectancies of feared outcomes, eliminating safety-seeking behaviors, including retrieval cues, varying the context and time of E/RP (e.g., exposures offsite and at different times), and reconsolidating memory of adverse events that relate to the onset of OCD (Craske et al., 2014). Optimizing E/RP for OCD using inhibitory learning principles is promising (Arch & Abramowitz, 2015) but requires further evaluation. Disgust in OCD Disgust is a central but understudied emotion in OCD, and generally E/RP outcome in disgust-OCD is poorer than in fear-OCD, with smaller, slower, and more temporary effects (Mason & Richardson, 2010; Olatunji et al., 2009). Disgust differs from fear with regard to phenomenology, acquisition, and maintenance. For example, a case series of 11 residential patients with contamination-related OCD found that exposure with disgust-inducing stimuli was associated with an increased vagal tonus (Duncko & Veale, 2016), contrary to the concept of adrenergic activation of heightened fear. Disgust-avoidance has also been conceptualized as a distinct motivational ‘core dimension’ to harm-avoidance (Melli et al., 2015) in contamination-related OCD. Disgust may be acquired through evaluative conditioning where the reference between conditioned and unconditioned stimulus is learned rather than the expectancy of the occurrence of the unconditioned stimulus (Schienle et al., 2001; Woody & Teachman, 2000). These functional differences between evaluative and fear conditioning may require alternative intervention 199 200 Oliver Sündermann and David Veale strategies, and it was recently proposed that counter-conditioning (pairing the conditioned stimulus with an unconditioned stimulus of opposite/pleasant valence) and unconditioned stimulus revaluation (pairing the unconditioned stimulus with another unconditioned stimulus of opposite/pleasant valence) may be more effective in reducing disgust (Ludvik et al., 2015). Disgust is also related to the experience of mental contamination, the feeling of pollution or dirtiness in the absence of a physical contaminant (Rachman, 1994, 2006). Cognitive interventions appear more effective than E/RP in treating mental contamination (Coughtrey et al., 2013). Mental contamination is often linked with past trauma, particularly those involving moral violation (humiliation, betrayal, sexual, physical, or emotional harm) (Rachman, 2010; Zysk et al., 2018); thus, trauma-focused approaches (e.g., imagery rescripting) may enhance outcome of CBT for OCD, particularly when past aversive experiences continue to affect the person. Imagery in OCD People with OCD experience intrusive images (Speckens et al., 2007), and these can be linked emotionally with past fear-, disgust-, or shame-based experiences that continue to haunt the person. For example, a person who developed mental contamination in response to childhood sexual abuse may continue to experience disgust-based memories and sensations that drive attentional processes to threat, avoidance, and decontamination rituals. When intrusive images or sensations are linked with earlier trauma, these need to be addressed in treatment, in addition to cognitive and behavioral interventions. A recent single-case experimental case series (n = 12; Veale et al., 2015) found that a single session of imagery rescripting in patients with images linked to aversive memories was associated with a drop on the Y-BOCS scale from 24.1 pre-treatment to 10.7 at three-month follow-up. Complex OCD and Specialized Services Clients with OCD often present with a multitude of difficulties, and are sometimes described as ‘complex’. Although the term ‘complex OCD’ is widely used, the literature lacks a clear definition and guidelines for treatment. We therefore recently described, in a case series, how complexity in OCD arises, the challenges various dimensions of complexity pose to therapy, how they are inter-linked, and how best to work with them (Sündermann & Veale, 2017). Complexity can be incurred through non-specific factors (language and culture barriers, unemployment, cognitive disabilities, etc.), and more specifically through comorbid problems, often in the context of personality and interpersonal difficulties, dissociation, and trauma. ‘Complexity’ is not the same as ‘severity’ or ‘chronicity’, but is more likely to occur in those with long-standing OCD with multiple treatment failures. Complex OCD does not require ‘complex’ treatment, but should be formulated by understanding and processing relevant past experiences, the context and the function of Obsessive-Compulsive Disorder OCD behaviors, and drawing on compassion-focused techniques, and will likely require a multidisciplinary approach. Clients with severe and/or complex OCD or those for whom adequate treatments have failed (CBT and/or SSRI) may require ‘stepping up’ to secondary or tertiary care services (see NICE, 2006). Residential or inpatient settings with specialized staff and the resources to provide intensive CBT may be indicated when there is risk of suicide, severe neglect, or low body weight or when rituals are found to be too debilitating (e.g., 24-hour shower rituals) or risky (e.g., drinking bleach) for outpatient services. Specialized residential and inpatient clinics should provide a caring and safe therapeutic community modelled on compassion-focused and social learning principles (Veale et al., 2014), encouraging clients to provide mutual support. Assessment and Treatment of OCD Assessment and treatment of OCD can take place in many different settings and contexts, and depends on various factors such as the nature, severity, complexity, and subtype of the OCD; the availability of resources; accessibility of treatment; and the client’s motivation for change (McKay et al., 2015). Therapy needs to be culturally sensitive, and although OCD themes tend to be similar across cultures and societies (Clark & Radomsky, 2014; Radomsky et al., 2014), religious and sexual intrusions in particular vary with regard to themes of homosexuality, selfpurification, premarital sex, and prescribed prayers (Sookman, 2015). Table 11.1 gives an overview of a CBT protocol for assessment and treatment of OCD, including core measures for each therapy stage. Assessment The main purpose of the assessment is to gain a shared understanding of how the client’s OCD developed and how it is maintained. Assessment should be developmentally adapted, multidimensional, and include self-reports of subjective experiences of obsessions and compulsion, corroborated by clinical interviews and standardized self-report measures, as applicable to the client’s presenting OCD (Sookman, 2015); for example, someone suffering from mental contamination could complete the Vancouver Obsessional Compulsive Inventory–Mental Contamination Scale (VOCI-MC) (Rachman, 2005). Screening for OCD The National Institute for Health and Clinical Excellence (NICE) provides the following guidance on questions for OCD screening: Do you wash or clean a lot? Do you check things a lot? 201 202 Oliver Sündermann and David Veale Table 11.1. A cognitive behavioral assessment and treatment protocol for OCDa Session Therapy stage Key elements and aims 1 and 2 Assessment and formulation Screening for OCD Clarify hopes, expectations, motivation, readiness for change Define the problem; set specific, measurable, attainable, realistic, and time-based (SMART) goals (short, medium, long) Obtain history and relevant early experiences Assess nature of obsessions and compulsions (content, context, distress, appraisals, emotions) Psychoeducation and normalization of unwanted thoughts, urges, images Assessment of OCD-related imagery Theory A/Theory B: build alternative understanding of the problem Formulation: Identify main appraisals of obsessions, emotions, imagery, and coping responses Home-based assessment (if indicated and feasible) Self-monitoring to enhance awareness of obsessions and compulsions (e.g., using diaries, tally counter) Involve key significant others (e.g., partner, parents) 3–6 Work phase 1 Therapy-assisted and modelled behavioral experiments and exposures in session, off-site, and home-based (if feasible) Rehearse E/RP principles, including ‘going beyond’ anti-OCD behaviors (i.e., not simply resisting rituals, but actively triggering OCD) Cognitive restructuring and Socratic dialogues to target obsessional appraisals and reflect on exposure outcomes Relate all therapy work to Theory A/Theory B and obtain regular belief ratings in both theories Use of metaphors is helpful (‘OCD as bully’; ‘Digging yourself out of a hole’; ‘Ghosts from the past’; etc.) Strong emphasis on homework tasks Imagery rescripting (if indicated) Home visits and in vivo off-site experiments (if indicated, do as quickly as possible) 7–10 Work phaseb Space out sessions to agreed frequency, e.g. biweekly, monthly More emphasis on independent planned exposures: ‘Client becoming their own therapist’ 11 and 12 Termination 13–15 Follow-up Review of progress a Generalization of experiments/exposures Review of treatment Dealing with setbacks Blueprint (‘Staying well plan’) Protocol can/should be adapted according to severity, complexity, heterogeneity of OCD, and availability of resources. b Consider specific-subtype measures if indicated, e.g., for VOCI-MC mental contamination; monitor mood/anxiety/ quality of life and other difficulties as required. Obsessive-Compulsive Disorder Is there any thought that keeps bothering you that you would like to get rid of but cannot? Do your daily activities take a long time to finish? Are you concerned about putting things in a special order or are you very upset by mess? Do these problems trouble you? If the client answers any of the above affirmatively, a more thorough clinical assessment should be conducted. Hopes, Expectations, and Problem Definition A good clinical assessment should start by clarifying the client’s hopes and expectations for treatment. The therapist should also inquire about any ambivalence about seeking help. Does the client feel pressured to seek treatment, for example, by their partner or family, or are they sent or referred by someone else, for example, their general practitioner? The therapist may consider asking why they are seeking help now, what they hope to gain, and how they feel about seeing a therapist. Clients may feel ashamed about their OCD, and find it difficult to discuss their obsessions or compulsions. Normalization and psychoeducation about the universality of intrusions is therefore key (Rachman & de Silva, 1978). The therapist should also discuss expectations of what is required in therapy of the client, for example, engaging in homework tasks, carrying out planned exposures independently, or keeping daily diaries of intrusions, interpretations, and responses. This will help to gain an understanding of the client’s motivation for treatment, which can depend on different factors such as insight into their problem, overvalued ideas (e.g., preferring things to be neat and clean), having different ideas about how treatment should work (e.g., by discussion of childhood instead of doing exposures), frequency and duration of treatment (e.g., wanting a quick fix), or comorbid problems that require addressing first (e.g., alcohol problems may not be seen as a problem). The concept of ‘becoming your own therapist’ should be conveyed, that is, the idea of the client taking more responsibility for their recovery as treatment progresses. Client and therapist should then agree on what the problem is, and this should be translated into specific, measurable, attainable, realistic, and time-based (SMART) goals to help monitor treatment progress. A client with contamination fears may want to work on reducing washing rituals; someone with concerns about incompleteness and symmetry may aim to reduce ordering rituals. History and Early Experiences The developmental history is key to understanding the client’s problem, and often helps the client to ‘feel understood’. The goal should be to understand the onset of the problem and make clear links between possible past aversive memories and their OCD. We find drawing out a timeline helpful as an aid to go through the client’s early childhood, adolescence, and adulthood while focusing on key events in the person’s life, including the family history of mental health problems, attachment 203 204 Oliver Sündermann and David Veale history and any traumatic experiences, bereavements, or experiences of discrimination. Parenting characterized by high levels of criticism, perfectionism, riskaversion, or overprotection is related to OCD and should be inquired about (Frost et al., 1994). The therapist should provide a rationale as to why it is important to have a good grasp of the past. We find the metaphor of ‘ghosts from the past’ helpful in explaining how unprocessed difficult events can continue to affect (‘haunt’) the person in the here-and-now by shaping their experiences and interpretations of events; for example, a client who soiled herself as a child in school and was teased for smelling may have developed disgust-based memories of the event that now drive disgust-avoidance and cleaning rituals. A childhood memory of being racially teased (e.g., ‘Your skin colour is dirty’) can fuel mental contamination in the present. Assessment of Obsessions and Compulsions The assessment of obsessions and compulsions should be guided and informed by the CBT model of OCD; that is, the therapist should gain a good understanding of the context in which the OCD arises, how obsessions are appraised, and what coping strategies the person employs. A good starting point is to ask about a recent episode or trigger when the client felt distressed by obsessions/compulsions, and elicit a typical sequence of triggerintrusion-interpretation-response. We recommend drawing out a maintenance model (‘vicious flower’) jointly with the client on a whiteboard to clarify content of intrusion(s), appraisals, and the underlying principles and responses to the intrusion, including compulsive ritualizing, neutralizing, reassurance seeking, and avoidance. It is usually helpful to provide examples of typical OCD appraisals to further elicit discussion about these, alongside normalizing them. For example, if the client suffers from contamination-related OCD with harm-avoidance, inquire about whether they feel responsible for preventing harm. The (unintended) consequences of each coping behavior should be examined, and how these possibly strengthen OCD appraisals and maintain their OCD. Rather than focusing on understanding the content of an intrusion, we recommend identifying the processes by which the client concludes that their thoughts are dangerous or confirm danger. Typical principles involve ‘acting on thoughts’ (e.g., fear of losing control can lead to loss of control), ‘thoughts cause harm’ (e.g., belief that presence of thought has power to make it happen), ‘moral equivalence’ (e.g., having an intrusion is morally the same as acting on it), and emotional reasoning (e.g., I feel dirty, hence I am contaminated). This will enable clients to be able to identify and label these processes when they occur. The therapist should identify a recent episode in which the intrusion occurred but the person was not or less bothered by it, and discuss the differences. For example, someone with harm-obsessions about killing his wife may be less distressed when not around his spouse; the therapist should discuss how distress results from appraisals (e.g., ‘I must avoid being near her to prevent accidentally killing her’), avoidance, and failed disconfirmation. In case of incompleteness or ‘just-right’ Obsessive-Compulsive Disorder obsessions characterized by sensory perceptions preceding rituals, appraisals may focus more on the ability to tolerate the discomfort (e.g., ‘If I don’t feel right I cannot walk through the door’) rather than the meaning of the urge to ritualize. OCD-Related Imagery Intrusive images are common in OCD and are often linked with past adverse experiences. A thorough assessment includes checking if the client experiences any visual images when triggered. Similar to imagery in social phobia or body dysmorphic disorder, images may be experienced as a ‘felt impression’, that is, the perception of their trigger or feared catastrophe. For example, someone with contamination OCD may have images of oversized bugs crawling over their skin after contact with contaminants. The therapist should clarify the perspective of how images are perceived, that is, whether they are experienced from an observer perspective (as if looking at oneself from another person’s perspective), which often relates to more distorted imagery and greater distress or field perspective (looking out of one’s own body). Images often provide an emotional (‘hot’) bridge to the onset of the difficulties, hence it is important to ask when they first experienced their images. The therapist should also ask how old they feel when they are triggered in the here-and-now. The meaning of any images and their current relevance should be carefully explored. Engagement into the CBT Approach to OCD: Theory A/Theory B A common technique to help clients build an alternative view of their difficulties and to engage them into a cognitive approach to obsessional problems is ‘Theory A/ Theory B’ (see Table 11.2) (Salkovskis, 1999). This can be introduced by first asking the client what they believe their problem is from the OCD perspective (e.g., ‘My problem is that I am at risk of contracting and spreading HIV, and it is my responsibility to prevent this’). If this were true, then the therapist should ask what the client would need to do (e.g., wear only ‘safe’ footwear, scan floor for needles, check body for pricks), followed by inquiring what the future would be like if Theory A was true. Subsequently, the therapist should propose a different view on their problem, namely, Theory B, which states that their problem is one of worry instead of being factual (e.g., ‘The problem is that I worry that I am at risk of contracting HIV and infecting my partner’). Discuss implications of what they would need to do if Theory B were true, which usually elicits answers of ‘doing the opposite’ to their compulsions and living in line with their values. Understandably, the outlook for a Theory B–led life is much brighter. The therapist should highlight that only one of the two theories can logically be correct and that therapy is about finding out which theory is a better, more accurate account of their experiences. Of course, the only way to test both theories is by acting in reverse to Theory A, and this can lead to a discussion of E/RP and behavioral experiments. Inquire whether the client would be prepared to act ‘as if their problem were Theory B’. Commonly, clients express doubts about Theory B, 205 206 Oliver Sündermann and David Veale Table 11.2. Worksheet for Theory A/Theory B with example of client suffering from sexual obsessions about children Theory A (OCD) My problem is that I am a pedophile and I am going to harm my children. Theory B (Worry problem) My problem is that I worry about being a pedophile. I am a caring person, who simply worries about causing harm to those I love the most. Evidence I have thoughts about hurting children. Evidence I have never caused any harm. Everyone tells me that I worry too much. I have OCD. What do I need to do if Theory A is true? Stay away from all children, including my own. Monitor sensations in my genitals. Seek reassurance from my wife and doctors. Suppress any thoughts about children through distraction, counting rituals, and alcohol. Avoid reading newspaper and watching TV to minimize risk of seeing children. Mentally review if I was aroused by the thought of children. Report myself to the police. What do I need to do if Theory B is true? I need to live my life in accordance with my values. This involves spending time with my wife and children, going to work, meeting friends, and engaging in my hobbies. I need to do all these activities without engaging in any rituals, compulsions, and avoidance behaviors. The future Dark, depressing; would not have a future The future Positive, optimistic or reluctance to ‘act in line with Theory B’. This should be normalized as an understandable response whilst stressing the importance of challenging and testing out OCD fears. It is also helpful is to ask the client if they have noticed how their solutions (Theory A behaviors) have in fact become their problem (time-consuming and distressing rituals) and keep them stuck. The therapist can also suggest ‘fake it, to make it’ in order to challenge Theory A, and that the client can always go back to Theory A, if they wish – after fully committing to treatment for a set period of time. Once both theories are drawn out, belief ratings should be obtained, and it should be explained that both theories provide the framework of therapy; that is, all therapy work will be related to Theory A/Theory B, and change in belief rating should be monitored. Cognitive Behavioral Treatment for OCD Overview Once therapist and client have reached a shared formulation of the OCD, the actual work phase begins. The main purpose of treatment is to build up evidence for Theory B through repeatedly testing out fears and expectations and building up tolerance of the client’s specific OCD distress (fear, disgust, just-so sensations) through planned exposures and behavioral experiments – while not engaging in Obsessive-Compulsive Disorder any compulsive or safety-seeking behaviors. We usually highlight that OCD treatment is very much a ‘doing’ treatment as opposed to a ‘talking’ treatment, requiring the client to take responsibility for homework assignments and becoming gradually independent in conducting and generalizing therapy tasks. Delivery of CBT The delivery of therapy – that is, the number, length, and frequency of sessions; their format (group vs. individual); and context (home-based, outpatient, residential, or inpatient) – depends on severity, complexity, and available resources. Usually, outpatient sessions occur weekly for up to 20 sessions (mild to moderate severity), and last between 45 and 90 minutes. Longer sessions for prolonged exposures (e.g., 2–3 hours) should be considered. In residential or inpatient settings, sessions can also be shorter and more frequent. Sessions should be audio recorded or videotaped for clients to listen to, and treatment progress should be monitored. The OCD protocol described here (Table 11.2) can and should be adapted according to presentation and setting. Formulation and Treatment To illustrate formulation and treatment for OCD, we present the case of Eric (who attended intensive inpatient treatment in a UK national specialist service for OCD) with reference to challenges, pitfalls, and learning points from his therapy. We chose Eric because we think his case is informative in terms of enhancing CBT with insights from recent OCD research (see Sündermann & Veale, 2017, for a more detailed description of Eric’s OCD). CASE STUDY: ERIC Eric is a 27-year-old single man with Bosnian Muslim origin who suffered from debilitating OCD characterized by disgust avoidance of his and other people’s semen. He was admitted to a UK national specialist clinic for OCD and his YBOCS score on admission was 40/40 (extremely severe). His main worry was that he might leak and spread semen. He was easily triggered by sexual thoughts, arousal, or anything vaguely related to, or perceived as, semen. When triggered, he experienced vivid images of spermatozoa, which were associated with high levels of disgust and shame, emotionally linked with childhood wet dreams, and related to appraisals of being dirty and responsible for preventing semen from spreading. He engaged in extreme decontamination rituals (showering for 30 hours) using hard cleaning products (bleach, scrubs) and stayed indoors (he had not left the house in seven years at admission). Eric mentally replayed events, checking for contact with contaminants, suppressing thoughts with mental counting rituals, seeking reassurance from his mother (‘Is this semen?’; ‘Have you been in contact with semen?’), and ridding himself of everything perceived contaminated. 207 208 Oliver Sündermann and David Veale His relationship with his mother was highly enmeshed to the point that she had entirely bought into his OCD belief system fearing contamination and experiencing disgust by the thought of semen. She started wearing gloves and kept the house microscopically clean even though Eric was in hospital. They had not been in direct contact with each other for seven years, and kept a ‘safety distance’ of one meter, with Eric worrying that semen would magically transfer between them. Eric’s OCD developed during his early teenage years when he started masturbating, secretly watching pornographic material, and experienced wet dreams, all of which caused feelings of guilt, shame, and dirtiness. He coped by showering in the middle of the night to feel clean. Past treatment courses of CBT with E/RP for his OCD were largely unsuccessful, and our shared understanding for treatment failure was that previous therapies had overly focused on E/RP without formulating the emotional origins of his OCD. This continued to affect Eric through vivid imagery of semen fused with past shame and disgust-based memories. Eric’s OCD was also tightly linked with anger and aggression. Irritation interfered with ritual completion, which fuelled his OCD, and often escalated his anger. On the other hand, aggression also provided relief from OCD distress, all of which made sense in the context of his violent upbringing. His uncle was physically abusive towards him and his mother; in school he was bullied for being foreign; and he observed that the most aggressive male peers appeared to be most popular among the female students – all of which contributed to warped ideas about masculinity and needing to be aggressive to survive and be attractive. Case Formulation in OCD Case formulation is an integral part of CBT for OCD, and it is crucial to first reach a shared understanding of the problem before embarking on interventions. Theory A/ Theory B socializes the client into the CBT model and provides the groundwork for the initial formulation with the elicited Theory A behaviors mapping onto the OCD vicious cycle. The therapist might start by pulling together the information they have gathered so far, including interview and questionnaire data, by jointly drawing out a diagram of the model on a whiteboard. Figure 11.1 shows an example of Eric’s formulation. We have adapted this OCD model from previous established CBT models of OCD (Salkovskis, 1999; Veale, 2007). Note that the model includes clear past-present links between early relevant incidences and current OCD characterized by a triangulated experience of OCD-related imagery, emotions, and appraisals, which drive idiosyncratic OCD behaviors and processes. Each OCD coping behavior is briefly described, alongside the specific unintended consequences. For example, Eric discovered that seeking reassurance from his mother increased his uncertainty and anxiety. Decontamination rituals, besides feeding his preoccupation with contamination of semen, incurred significant financial debt and feelings of guilt for ‘wasting money’ on cleaning products. Staying indoors and avoiding social life caused feelings of disconnection and loneliness, increasing depression. Obsessive-Compulsive Disorder 209 Relevant past experiences (2,3,6) • 3 years: Fled civil war in Bosnia with mother; father died in genocide • 3–15 years: Mother suffered from PTSD and was emotionally unavailable to him • 10–16 years: Wet dreams and other shame/disgust-based relevant experiences (e.g., being told that ‘masturbation is the work of the devil’ Trigger (1,2,3) Any sexual thought, being aroused or worrying about arousal, seeing white stains perceived as semen, actual semen, semen-like smell; suspecting other people of having had contact with semen (1, 4) My attention narrows to: Other ways of coping: (1, 2) Mum 'protects' me from contamination; buys me OCD products and smuggles them into hospital; entirely dependent on her. Engaging in mental counting rituals to block out any thoughts about semen. Anything that could be semen. Constantly scanning and monitoring environment for threat Unintended consequences: Unintended cosequences: Mum now suffers from OCD, feeling guilty; increases my anxiety, more preoccupied with semen Meaning or past associations: (3, 6) I am dirty. l must prevent semen from spreading I seek reassurance by: (2) Constantly asking mum to clarify if something is semen, if she came in contact with semen, and if I am safe Unintended consequences: I became more uncertain, and get more anxious Spotting 'semen' everywhere, more anxious and agitated Image or physical sensations: (3, 6) Images of semen, linked with early experiences I 'undo' the event by: (i.e., washing) (1, 2) Extreme showering rituals using hard cleaning products (bleach, sponges) to scrub myself for up to 30 hours, assisted by my mother Throwing away clothes, shoes, and everything perceived contaminated Unintended consequences: I get more agitated and hardly feel clean; getting stuck and losing sense of time Severe debt and distress, also on mum's part I avoid: (1, 2) Emotions: (3, 5, 6) Overwhelming disgust and anxiety Stay indoors in my room at all times; move as little as possible Unintended consequences: Missing out on life; becoming depressed and stuck in OCD (1, 4) I replay past events in my mind or physically check by: Meticulously rehearsing and trying hard to recall whether I came in contact with own or other people's semen Unintended consequences: Becoming more anxious and never getting clarity and certainty Figure 11.1. Eric’s case formulation, demonstrating how his contamination-related OCD characterized by disgust of semen developed and was maintained by compulsive rituals and avoidance, which all served the function of disgust-avoidance and brought about multiple unintended consequences. Adapted with permission from Sündermann & Veale (2017) 210 Oliver Sündermann and David Veale Confirmatory biases of narrowing his attention and ‘scanning’ for semen (often labelled as ‘looking for trouble’) substantially increased the frequency of obsessions, thus triggering anxiety, frustration, and agitation. Eric found two aspects of his formulation particularly helpful. First, after discussion of the function of each behavior and its unintended consequences, Eric felt he ‘finally got how my OCD works, and backfires’. We translated each OCD behavior from his formulation into a treatment goal and avoidance hierarchy. Second, a developmental understanding of his OCD, that is, contextualizing his early shame and disgust-based experiences and linking these with his current experiences of semen-related imagery and disgustavoidance, was a greatly normalizing experience and motivated him to work on processing the relevant memories. Exposure-Based Interventions Exposure and behavioral experiments are deliberate and planned activities that help clients experience the main emotion avoided (e.g., fear, disgust, sensations of just-so/ right, and incompleteness), test out their predictions and build the evidence as to whether their experience best fits with a worry problem (Theory B), and learn to tolerate their distress without any compulsions or safety-seeking behaviors. A common misconception is that exposures are ‘simple’, ‘uncomplicated’, and ‘easy to deliver’. However, successful exposure based-interventions depend on a multitude of factors (Bouton, 2002; Craske et al., 2014; McKay et al., 2015) concerning decisions about context, content, timing, and process of delivery, that is, what to do, when, how, and at what pace. The following principles briefly outline how to set up and deliver exposure tasks, which are informed by an inhibitory approach to exposure-based interventions and testing out expectations (Arch & Abramowitz, 2015; Craske et al., 2014): 1. Set up a hierarchy of exposure tasks with feared/avoided triggers/situations 2. Exposure should be graded, but we recommend ‘jumping’ around the hierarchy instead of working sequentially from the bottom of the list to the top. 3. The focus is on maximal expectancy violation of what the client predicts, rather than habituation. Similar to behavioral experiments, test beliefs about coping (‘I can’t tolerate the disgust, will lose control’), and always reflect on the outcome of specific predictions with regard to formulation and Theory A/ Theory B. Ask what was learned, and how the outcome best fits the theories. 4. Habituation during sessions is less important than extinction between sessions. 5. All tasks should be generalized across different times and contexts (e.g., on their own, in unfamiliar places, at home). 6. Labelling of emotions during exposure can be helpful. 7. Overcome all avoidance and compulsive/safety-seeking behaviors during and after exposures; if client ritualizes subsequently, retrigger (e.g., touch contaminant again). 8. Aim for daily exposures, and do not leave long gaps between exposures to avoid spontaneous reinstatement of OCD distress and responses. Obsessive-Compulsive Disorder Various pitfalls should be kept in mind when conducting exposure-based interventions. First, response/ritual delay is highly common, which refers to clients carrying out an exposure without a ritual but ‘storing it’ for later, for example, tolerating contaminant triggers with the therapist, but completing a decontamination ritual after the session. This is common, and clients should be encouraged to redo the exposure (e.g., re-contaminate). Self-monitoring (e.g., using tally counters) can help clients to keep track of rituals (and resist them) post-exposures. Second, termination criteria for rituals should be specific and objective, and not feeling-based; for example, specify the frequency of and duration of showering. Note that emotional termination criteria (e.g., having to feel comfortable, ‘just right’) are not abnormal but elevated criteria to normal routine; that is, they are relevant for important decisions (e.g., who to get married to) but take excessive amount of time when applied to rituals. Clients should be encouraged to stop rituals feeling not right or uncomfortable, and if completed feeling right or comfortable, they should do re-exposure until they can stop the ritual feeling not right. Third, often therapy overly focuses on response prevention, rather than planned exposures, for example, not carrying out a counting ritual when the impulse arises instead of actively triggering the impulse (e.g., by wishing their parents to die in an accident). Exposure interventions should always be carried out together with ritual prevention to maximize effectiveness. Fourth, while the aim of E/RP should be to eliminate all ritualized responses, judicious use of safety-seeking behaviors (or better termed as approachenhancing behaviours) can be helpful (Rachman et al., 2011). This could involve confronting contaminants with reduced rituals instead of eliminating them immediately. For example, Eric was initially unable to masturbate because of overwhelming feelings of disgust and fear of decontamination rituals. To help Eric approach exposures of masturbation, we agreed to several achievable exposure levels, including the use of judicious safety behaviors such as masturbating only in the shower (as opposed to his room), a five-minute shower afterwards (as opposed to hour-long showers), wiping the shower drainage hole, and flushing his semen (as opposed to keeping it for further exposures and to build up disgust tolerance). In line with inhibitory E/RP principles, we focused on violation of expectancies of his coping beliefs. For example, Eric predicted he would not be able tolerate the smell of semen, and was surprised that he could with a graded approach using many repetitions. He also scored his emotions during each exposure (0–100), and during most E/RP his disgust dropped below 30/100 after 10–15 minutes. Uncertainty about contact with semen was a particularly strong trigger; therefore, another line of experiments involved shaking hands with the therapist who had put his hand into a plastic cup out of his sight in the inside of his jacket (without him seeing the cup), and telling him that it ‘may or may not contain’ semen. Since physiology of disgust responses during exposures is associated with a decrease in heart rate (Duncko & Veale, 2016), we speculated that accelerating Eric’s heartbeat 211 212 Oliver Sündermann and David Veale immediately before E/RP may enhance effectiveness. We found some anecdotal evidence that his disgust habituation was several minutes faster when Eric sprinted for one minute right before exposure (compared with not sprinting or doing a relaxation exercise). Counter-conditioning has been suggested as potentially enhancing E/RP in disgust-OCD; and we recommend exploring (and researching) if pairing disgust-triggers with idiosyncratically identified pleasant stimuli during exposures is effective. Imagery Rescripting and Stimulus Discrimination Imagery rescripting aims to change the meaning of past childhood events that continue to shape the person’s experience (Arntz, 2011). This may be relevant to clients with OCD, particularly where current imagery is fused with shame or disgustbased memories. The protocol is based on Arntz’s manual (Arntz & Weertman, 1999) and is described in Chapter 15. In short, the stages include reliving the event as a child, re-entering as an adult, then reviewing and rescripting the event as a child once more to a less catastrophic outcome that focuses on the child feeling safe. Eric was able to revisit and rescript several key events that were associated with the emotional origins of his OCD. For example, he rescripted the memory of his first wet dream that continued to cause him great distress, as it was not normalized due to the absence of his father. He was able to imagine soothing his younger self (‘Little Eric’) as an adult by normalizing the experience. Another key incident he rescripted involved his uncle telling him that ‘masturbation is the work of the devil’ and that ‘a good Muslim does not masturbate’. Imagery rescripting seemed to help Eric in several ways: he experienced a sharp decrease in shame and disgust, which also boosted exposure work as he was better able to tolerate disgust and uncertainty of contamination; frequency of intrusive semen-related imagery was reduced; and masturbation became more enjoyable. Imagery rescripting also brought about feelings of sadness for the loss of his father and aided a delayed bereavement process, and he experienced anger and guilt towards his mother for not being emotionally available when his OCD developed. Stimulus discrimination can further aid ‘putting aversive memories to rest’. Eric learned to identify associative past-present links and was able to tell himself, in a compassionate voice, that he did not feel safe in his abusive home environment and that he had no one to turn to when he felt lonely, ashamed, and dirty. Through becoming aware of these emotional links, he was able to distance himself from these memories and contextualize them, which in turn facilitated courage in exposures. Cognitive Interventions and Reassurance-Seeking for OCD Cognitive interventions for OCD involve challenging misappraisals of obsessional thoughts and discussing evidence for and against key appraisals. Caution is warranted when discussing feared consequences that relate to unspecific or far distant Obsessive-Compulsive Disorder time points in the future (e.g., causing accidents at any time or going to hell in the afterlife). Rather than attempting to disprove appraisals, discussions should focus on the helpfulness and costs of these beliefs and drawing on Theory A/Theory B to examine how rituals are the problem and keep the person stuck. Salkovskis (1999) uses the metaphor of OCD rituals being an extremely costly insurance premium with the cost being greater than the risk justifies. Sometimes ‘experts’ such as religious leaders with more credibility than the therapist with regard to the clients’ belief system can be involved or consulted in therapy to normalize and refute unhelpful spiritual beliefs. Disconfirmation strategies work best when clients exhibit clear thought–action fusion (e.g., imagining harm causes harm), and these can be subjected to experiments where the client deliberately attempts to bring on the feared outcome; for example, encourage the client to repeatedly wish/imagine their parents dying in car accident the same afternoon (of course, the therapist should also wish a loved one dead to normalize and model the experiment). Clients may also learn meta-cognitive skills to distance themselves from obsessions and reappraise the process. For example, a client who believes that ‘thinking of stabbing a baby is as bad as killing it’ can learn to label these as moral–action fusion, thereby distancing themself from it. However, we advise against ‘labelling’ thoughts as obsessions (e.g., ‘It’s my OCD’) as this in itself can become a ritualized response and may encourage engagement with OCD thoughts. It is usually best to practice acknowledging and ignoring (without ‘fighting’ or attempting to control) thoughts. Instead of engaging with the content of the intrusion, it can be helpful to identify and label the emotion that accompanies the thought (e.g., anxious) (Craske et al., 2014). And it is helpful to seek or give oneself emotional support (e.g., ‘I’m feeling anxious; can I have a hug, or can we go for a walk?’). Many people with OCD seek reassurance with regard to their OCD fears, for example, asking their partner if they killed someone or whether something is safe to touch. Generally, we encourage replacing reassurance seeking with providing emotional support instead. For example, if a client asks their partner for reassurance (‘Can I touch this?’), the partner could say: ‘I can see that you are anxious, and I am here with you. Do you remember what you should be doing?’ or ‘What would Theory B behavior consist of?’, rather than giving a point-blank refusal to give reassurance. Of course, the tone of one’s own voice and of the other people supporting the client should always be compassionate, warm, and accepting. The courage of challenging OCD is best met with compassion, including self-compassion (Veale et al., 2014). A Note on the Therapeutic Relationship As with any treatment, the therapeutic alliance is pivotal, and CBT takes place within a context of a safe and compassionate alliance where the client feels understood and trusts the therapist and their abilities. Two therapist qualities are particularly important for effective delivery of CBT for OCD. First, the therapist needs to be able to tolerate and contain distress that is likely to arise during exposures. 213 214 Oliver Sündermann and David Veale Second, the therapist needs the ability to model helpful coping responses in moments of peak distress. The therapist must be careful not to collude with avoidance of necessary behavioral tasks that they may find unacceptable or ‘abnormal’ such as touching the inside of a toilet, smelling bodily fluids, wishing their partner to die, or voicing blasphemous insults. Some of Eric’s exposures involved him masturbating to pornographic material, which his therapist had to organize and normalize, and exposure to the smell of semen; his previous therapists were not comfortable with these exposures, thus possibly reinforcing disgust-avoidance. Family Involvement Family accommodation is common in OCD, with family members or loved ones often becoming a part of the client’s OCD system. Family accommodation can take many different forms, such as clients asking and receiving reassurance for obsessional fears, ritual participation, or assisting clients in avoidance. There are various assessment tools to assess family accommodation (see Table 11.3). Family accommodation predicts poorer outcomes, and clients whose family members received a short intervention to reduce family accommodation seemed to recover more quickly (Stewart et al., 2008; Thompson-Hollands et al., 2015). Hence, whenever indicated, relevant others should be included in therapy (with consent) as co-therapists. In Eric’s case, his mother’s involvement, most notably through providing constant reassurance, worrying herself about semen, and ‘assisting’ constant showers, required her own CBT for OCD. In less severe cases, it may be sufficient to build a shared understanding, joint exposures, and practice resisting provision of reassurance (instead providing emotional support). Recovery from OCD and Staying Well (‘Blueprint’) Mindfulness meditation should not be offered instead of CBT and E/RP but can aid the recovery process. Mindfulness can help to reduce responding to OCD thinking styles, such as emotional reasoning (‘I feel anxious, therefore I must be in danger’), thought–action fusion (‘If I think I am a pedophile, then I must be one’), and distancing from OCD urges; becoming more aware of them; and choosing not to carry out compulsions. Both therapist and client should be cautious that mindfulness exercises are not carried out compulsively, as happened with one client who was a diligent mindfulness practitioner and who responded to worries of being a pedophile with meditation. Although he reported that he found mindfulness useful, it was discovered that he had not been aware of his underlying belief that he needed to meditate to prevent him from harming children. His meditation had become a safety-seeking behavior. As with recovery from any mental disorder that has occupied the client pervasively for many years, recovery can be a daunting process. When Eric’s OCD improved, he became aware of how much OCD had consumed his life and expressed sadness about how little else there was in his life. Recovery should focus Downloaded from https://www.cambridge.org/core, on subject to the Cambridge Core terms of use, available at https://www.cambridge.org/core/terms. https://doi.org/10.1017/9781108355605.014 Table 11.3. Assessment measures for OCD Outcome / Severity Name of measure Type of measure Function of measure Yale–Brown Obsessive Compulsive Scale (Y-BOCS) Semi-structured Clinician-rated Severity of OCD Brown Assessment of Beliefs Scale (BABS) Semi-structured Clinician-rated Insight into OCD Obsessive Compulsive Inventory– Revised (OCI-R) Self-report Screening Symptom profiling Severity of OCD Dimensional ObsessiveCompulsive Scale (DOCS) Self-report Symptom profiling Severity of OCD Florida Obsessive-Compulsive Inventory (FOCI) – Severity Scale Self-report Severity of OCD Responsibility Interpretations Questionnaire (RIQ) Self-report Interpretation of intrusive thoughts Description Reference Ten items measuring OCD symptoms, severity, and response to treatment. Each item is scored from 0 to 4, with a maximum score of 40; higher scores indicating greater severity and symptomatology. Most widely used OCD outcome measure. Seven items assessing conviction of a belief, fixity of ideas, attempts to disprove, and insight on a scale from 0 (nondelusional) to 4 (delusional). First six items are summed with scores 12, indicating poor insight. Eighteen-item scale rated on four-point Likert scale, measuring six subscales: obsessions, checking, neutralizing, hoarding, ordering, and washing. Twenty items assessing four dimensions of OCD: concerns about (1) germs and contamination; (2) responsibility for harm, injury, or bad luck; (3) unacceptable thoughts; and (4) symmetry, completeness, just-right. Five items assessing presence and severity of obsessions and compulsions (obtained from the FOCI, a 20-item symptom checklist). Recommended for tracking treatment progress. Twenty-two items assessing the interpretation of intrusive thoughts about potential harm by rating their frequency of occurrence Goodman et al. (1989) Eisen et al. (1998) Foa et al. (2002) Abramowitz et al. (2010) Storch et al. (2007) Salkovskis et al. (2000) 215 216 Downloaded from https://www.cambridge.org/core, on subject to the Cambridge Core terms of use, available at https://www.cambridge.org/core/terms. https://doi.org/10.1017/9781108355605.014 Table 11.3. (cont.) Type of measure Function of measure Self-report Mental contamination Self-report Disgust University of São-Paulo Sensory Phenomena Scale (UP-SPS) Self-report Sensory phenomena Family Accommodation Scale (FAS) Clinician-rated Family accommodation and distress Family Accommodation Scale SelfRated (FAS-SR) Self-report Family accommodation and distress Name of measure Specific OCD measures Family participation Vancouver Obsessional Compulsive Inventory–Mental Contamination Scale (VOCI-MC) Disgust Emotion Scale (DES) Description Reference Twenty-item self-report assessing mental contamination and internal dirtiness; with a potential maximum score of 80 Thirty items measuring disgust sensitivity across various domains: (1) animals, (2) injections and blood draws, (3) mutilation and death, (4) rotting foods, and (5) smells. Five-point Likert scale from 0 (no disgust or repugnance at all) to 4 (extreme disgust or repugnance). Investigates presence and severity of different sensory phenomena occurring before or during repetitive behaviors, including ‘just-so’, ‘just-right’, and ‘urge only’ perceptions, feeling of incompleteness sensations, and ‘energy release’ sensations Thirteen items assessing extent of family members’ accommodating rituals, and family distress associated with participation. Higher scores indicate greater involvement. A parent-report version (FAS-PR) is available for children and adolescents with OCD (Flessner et al., 2011). A self-report version of the clinician-rated FAS; a valid, time-saving, and costeffective alternative Rachman, (2005) Olatunji et al. (2007) Rosario et al. (2009) Calvocoressi et al. (1995) Pinto et al. (2013) Obsessive-Compulsive Disorder on helping clients to move towards their valued goals – which often involves building meaningful relationships, occupational work, hobbies, and so on – while also acknowledging and helping clients process sadness about the losses OCD has incurred. Measurement of Outcome Outcome measures are an important part of every evidence-based intervention, including CBT for OCD. Treatment progress should be measured continually, using self-report measures, assessing adherence to homework tasks, progress during E/RP and behavioral experiments, and (with consent) reports from significant others (Sookman, 2015). Table 11.3 gives an overview of specific OCD self-report measures and interviews that can be administered at various points during the course of treatment. Ideally, OCD-self-reports (e.g., Florida Obsessive-Compulsive Inventory [FOCI]), alongside general mood and anxiety measures, are obtained at every point of contact, preferably filled out before the session, so that progress can be reviewed jointly with the client. Clinical judgement should complement quantitative measures; for example, the therapist should regularly review engagement with therapy tasks, and progress during exposures in and between sessions, including asking relevant others how they perceive the client’s progress. More comprehensive outcome measures should be obtained at the beginning and end of therapy. The most common clinician-led OCD measure is the Yale–Brown Obsessive Compulsive Scale (Y-BOCS), which is more likely to be conducted in specialist services, and may be required by funding panels. Summary and Conclusion CBT for OCD remains the treatment of choice, and E/RP with testing of expectations lies at the heart of every therapy course. Inhibitory learning principles should optimize exposure-based interventions, for example, by focusing on maximizing expectancy violation of predicted concerns (e.g., ‘I cannot tolerate disgust’), with frequent repetitions of varying exposures in different contexts, always dropping all coping behaviors. A thorough developmental formulation is key, making clear links between past relevant experiences and current OCD. Cross-sectional formulations should describe the context and the function of each coping behavior and its unintended consequences. Imagery rescripting should be considered when past shame- or disgust-based memories continue to affect the client (as described here in Eric’s case). Selfcompassion skills can de-shame the clients’ experiences and further help to disengage from threat monitoring and ‘self-attacking’ thinking. We emphasize to clients that while their OCD is not their fault, it is their responsibility to do something about it, and the concept of ‘becoming your own therapist’ is particularly useful in OCD recovery that requires the client to continue with planned exposures and align their lives with their values. 217 218 Oliver Sündermann and David Veale Key Learning Points Behavioral interventions to test out expectations remain the key ingredient in the treatment of OCD. Inhibitory learning principles should inform all behavioral tasks. Theory A/Theory B is a helpful and engaging framework to conceptualize the problem and helps to build an alternative, more benign view of the problem. The formulation should describe the context and function of each safetyseeking behavior and the related unintended consequences. Imagery rescripting and stimulus discrimination can be considered when past aversive events are meaningfully linked to the person’s OCD. Compassion-focused interventions may be a helpful adjunct to therapy. Relevant others should be involved in therapy where possible and indicated. REFERENCES Abramowitz, J. S. (1996). Variants of exposure and response prevention in the treatment of obsessive-compulsive disorder: A meta-analysis. Behavior Therapy, 27(4), 583–600. (2006). The psychological treatment of obsessive-compulsive disorder. The Canadian Journal of Psychiatry, 51(7), 407–416. Abramowitz, J. S., Deacon, B. J., Olatunji, B. O., Wheaton, M. G., Berman, N. C., Losardo, D., . . . & Adams, T. (2010). Assessment of obsessive-compulsive symptom dimensions: Development and evaluation of the Dimensional Obsessive-Compulsive Scale. Psychological Assessment, 22(1), 180. Abramowitz, J. S., Franklin, M. E., Schwartz, S. A., & Furr, J. M. (2003). Symptom presentation and outcome of cognitive-behavioral therapy for obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology, 71(6), 1049. Abramowitz, J. S., & Jacoby, R. J. (2014). Obsessive-compulsive disorder in the DSM-5. Clinical Psychology: Science and Practice, 21(3), 221–235. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. Arch, J. J., & Abramowitz, J. S. (2015). Exposure therapy for obsessive-compulsive disorder: An optimizing inhibitory learning approach. Journal of Obsessive-Compulsive and Related Disorders, 6, 174–182. Arntz, A. (2011). Imagery rescripting for personality disorders. Cognitive and Behavioral Practice, 18(4), 466–481. Arntz, A., & Weertman, A. (1999). Treatment of childhood memories: Theory and practice. Behaviour Research and Therapy, 37(8), 715–740. Bouton, M. E. (1993). Context, time, and memory retrieval in the interference paradigms of Pavlovian learning. Psychological Bulletin, 114(1), 80. (2002). Context, ambiguity, and unlearning: Sources of relapse after behavioral extinction. Biological Psychiatry, 52(10), 976–986. Bouton, M. E., Westbrook, R. F., Corcoran, K. A., & Maren, S. (2006). Contextual and temporal modulation of extinction: Behavioral and biological mechanisms. Biological Psychiatry, 60(4), 352–360. Calvocoressi, L., Lewis, B., Harris, M., & Trufan, S. J. (1995). Family accommodation in obsessive-compulsive disorder. The American Journal of Psychiatry, 152(3), 441. Obsessive-Compulsive Disorder Clark, D. A., & Radomsky, A. S. (2014). Introduction: A global perspective on unwanted intrusive thoughts. Journal of Obsessive-Compulsive and Related Disorders, 3(3), 265–268. Coughtrey, A. E., Shafran, R., Lee, M., & Rachman, S. (2013). The treatment of mental contamination: A case series. Cognitive and Behavioral Practice, 20(2), 221–231. Craske, M. G., Liao, B., Brown, L., & Vervliet, B. (2012). Role of inhibition in exposure therapy. Journal of Experimental Psychopathology, 3(3), 322–345. Craske, M. G., Treanor, M., Conway, C. C., Zbozinek, T., & Vervliet, B. (2014). Maximizing exposure therapy: An inhibitory learning approach. Behaviour Research and Therapy, 58, 10–23. Duncko, R., & Veale, D. (2016). Changes in disgust and heart rate during exposure for obsessive compulsive disorder: A case series. Journal of Behavior Therapy and Experimental Psychiatry, 51, 92–99. Eisen, J. L., Mancebo, M. A., Pinto, A., Coles, M. E., Pagano, M. E., Stout, R., & Rasmussen, S. A. (2006). Impact of obsessive-compulsive disorder on quality of life. Comprehensive Psychiatry, 47(4), 270–275. Eisen, J. L., Phillips, K. A., Baer, L., Beer, D. A., Atala, K. D., & Rasmussen, S. A. (1998). The brown assessment of beliefs scale: Reliability and validity. American Journal of Psychiatry, 155(1), 102–108. Fineberg, N. A., Hengartner, M. P., Bergbaum, C., Gale, T., Rössler, W., & Angst, J. (2013). Remission of obsessive-compulsive disorders and syndromes: Evidence from a prospective community cohort study over 30 years. International Journal of Psychiatry in Clinical Practice, 17(3), 179–187. Flessner, C. A., Freeman, J. B., Sapyta, J., Garcia, A., Franklin, M. E., March, J. S., & Foa, E. (2011). Predictors of parental accommodation in pediatric obsessive-compulsive disorder: Findings from the Pediatric Obsessive-Compulsive Disorder Treatment Study (POTS) trial. Journal of the American Academy of Child and Adolescent Psychiatry, 50(7), 716–725. https://doi.org/10.1016/j.jaac.2011.03.019 Foa, E. B., Huppert, J. D., Leiberg, S., Langner, R., Kichic, R., Hajcak, G., & Salkovskis, P. M. (2002). The Obsessive-Compulsive Inventory: Development and validation of a short version. Psychological Assessment, 14(4), 485. Foa, E. B., & Kozak, M. J. (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1), 20. Foa, E. B., Liebowitz, M. R., Kozak, M. J., Davies, S., Campeas, R., Franklin, M. E., . . . & Schmidt, A. B. (2005). Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessivecompulsive disorder. American Journal of Psychiatry, 162(1), 151–161. Frost, R. O., Steketee, G., Cohn, L., & Griess, K. (1994). Personality traits in subclinical and non-obsessive-compulsive volunteers and their parents. Behaviour Research and Therapy, 32(1), 47–56. Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., Hill, C. L., . . . & Charney, D. S. (1989). Yale–Brown Obsessive Compulsive Scale (Y-BOCS). Archives of General Psychiatry, 46, 1006–1011. Hollander, E., & Benzaquen, S. D. (1996). Is there a distinct OCD spectrum? CNS Spectrums, 1(1), 17–26. Hollander, E., Stein, D. J., Kwon, J. H., Rowland, C., Wong, C. M., Broatch, J., & Himelein, C. (1997). Psychosocial function and economic costs of obsessive-compulsive disorder. CNS Spectrums, 2(10), 16–25. Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. 219 220 Oliver Sündermann and David Veale Ludvik, D., Boschen, M. J., & Neumann, D. L. (2015). Effective behavioural strategies for reducing disgust in contamination-related OCD: A review. Clinical Psychology Review, 42, 116–129. Mason, E. C., & Richardson, R. (2010). Looking beyond fear: The extinction of other emotions implicated in anxiety disorders. Journal of Anxiety Disorders, 24(1), 63–70. McKay, D., Sookman, D., Neziroglu, F., Wilhelm, S., Stein, D. J., Kyrios, M., . . . & Veale, D. (2015). Efficacy of cognitive-behavioral therapy for obsessive-compulsive disorder. Psychiatry Research, 225(3), 236–246. Melli, G., Chiorri, C., Carraresi, C., Stopani, E., & Bulli, F. (2015). The two dimensions of contamination fear in obsessive-compulsive disorder: Harm avoidance and disgust avoidance. Journal of Obsessive-Compulsive and Related Disorders, 6, 124–131. Olatunji, B. O., Davis, M. L., Powers, M. B., & Smits, J. A. (2013). Cognitive-behavioral therapy for obsessive-compulsive disorder: A meta-analysis of treatment outcome and moderators. Journal of Psychiatric Research, 47(1), 33–41. Olatunji, B. O., Sawchuk, C. N., de Jong, P. J., & Lohr, J. M. (2007). Disgust sensitivity and anxiety disorder symptoms: Psychometric properties of the disgust emotion scale. Journal of Psychopathology and Behavioral Assessment, 29(2), 115–124. Olatunji, B. O., Wolitzky-Taylor, K. B., Willems, J., Lohr, J. M., & Armstrong, T. (2009). Differential habituation of fear and disgust during repeated exposure to threat-relevant stimuli in contamination-based OCD: An analogue study. Journal of Anxiety Disorders, 23(1), 118–123. Öst, L.-G., Havnen, A., Hansen, B., & Kvale, G. (2015). Cognitive behavioral treatments of obsessive-compulsive disorder. A systematic review and meta-analysis of studies published 1993–2014. Clinical Psychology Review, 40, 156–169. Pinto, A., Van Noppen, B., & Calvocoressi, L. (2013). Development and preliminary psychometric evaluation of a self-rated version of the Family Accommodation Scale for Obsessive-Compulsive Disorder. Journal of Obsessive-Compulsive and Related Disorders, 2(4), 457–465. Rachman, S. (1994). Pollution of the mind. Behaviour Research and Therapy, 2(3), 311–314. (2005). Vancouver Obsessional Compulsive Inventory Mental Contamination Scale (VOCIMC). Rachman Lab. (2006). The fear of contamination: Assessment & treatment. Oxford University Press. (2010). Betrayal: A psychological analysis. Behaviour Research and Therapy, 48(4), 304–311. Rachman, S., & de Silva, P. (1978). Abnormal and normal obsessions. Behaviour Research and Therapy, 16(4), 233–248. Rachman, S., Shafran, R., Radomsky, A. S., & Zysk, E. (2011). Reducing contamination by exposure plus safety behaviour. Journal of Behavior Therapy and Experimental Psychiatry, 42(3), 397–404. Radomsky, A. S., Alcolado, G. M., Abramowitz, J. S., Alonso, P., Belloch, A., Bouvard, M., . . . & Wong, W. (2014). Part 1: You can run but you can’t hide: Intrusive thoughts on six continents. Journal of Obsessive-Compulsive and Related Disorders, 3(3), 269–279. Rosa-Alcázar, A. I., Sánchez-Meca, J., Gómez-Conesa, A., & Marín-Martínez, F. (2008). Psychological treatment of obsessive-compulsive disorder: A meta-analysis. Clinical Psychology Review, 28(8), 1310–1325. Rosario, M. C., Prado, H. S., Borcato, S., Diniz, J. B., Shavitt, R. G., Hounie, A. G., . . . & Perin, E. A. (2009). Validation of the University of São Paulo sensory phenomena scale: Initial psychometric properties. CNS Spectrums, 14(6), 315–323. Rufer, M., Fricke, S., Moritz, S., Kloss, M., & Hand, I. (2006). Symptom dimensions in obsessive-compulsive disorder: Prediction of cognitive-behavior therapy outcome. Acta Psychiatrica Scandinavica, 113(5), 440–446. Salkovskis, P. M. (1999). Understanding and treating obsessive-compulsive disorder. Behaviour Research and Therapy, 37, S29–S52. Obsessive-Compulsive Disorder Salkovskis, P. M., Wroe, A. L., Gledhill, A., Morrison, N., Forrester, E., Richards, C., . . . & Thorpe, S. (2000). Responsibility attitudes and interpretations are characteristic of obsessive compulsive disorder. Behaviour Research and Therapy, 38(4), 347–372. Schienle, A., Stark, R., & Vaitl, D. (2001). Evaluative conditioning: A possible explanation for the acquisition of disgust responses? Learning and Motivation, 32(1), 65–83. Sookman, D. (2015). Specialized cognitive behavior therapy for obsessive compulsive disorder: An expert clinician guidebook. Routledge. Sookman, D., & Fineberg, N. A. (2015). Specialized psychological and pharmacological treatments for obsessive-compulsive disorder throughout the lifespan: A special series by the Accreditation Task Force (ATF) of the Canadian Institute for Obsessive Compulsive Disorders (CIOCD). Psychiatry Research, 227(1), 74–77. Soomro, G. M., Altman, D., Rajagopal, S., & Oakley-Browne, M. (2008). Selective serotonin re-uptake inhibitors (SSRIs) versus placebo for obsessive compulsive disorder (OCD). The Cochrane Database of Systematic Reviews, (1), CD001765. Speckens, A., Ehlers, A., Hackmann, A., Ruths, F., & Clark, D. (2007). Intrusive memories and rumination in patients with post-traumatic stress disorder: A phenomenological comparison. Memory, 15(3), 249–257. Stewart, S. E., Beresin, C., Haddad, S., Egan Stack, D., Fama, J., & Jenike, M. (2008). Predictors of family accommodation in obsessive-compulsive disorder. Annals of Clinical Psychiatry, 20(2), 65–70. Storch, E. A., Bagner, D., Merlo, L. J., Shapira, N. A., Geffken, G. R., Murphy, T. K., & Goodman, W. K. (2007). Florida Obsessive-Compulsive Inventory: Development, reliability, and validity. Journal of Clinical Psychology, 63(9), 851–859. Sündermann, O., & Veale, D. (2017). Complexity in obsessive-compulsive and body dysmorphic disorder: A functional approach to complex difficulties. The Cognitive Behaviour Therapist, 10. Taylor, S., & Jang, K. L. (2011). Biopsychosocial etiology of obsessions and compulsions: An integrated behavioral-genetic and cognitive-behavioral analysis. Journal of Abnormal Psychology, 120(1), 174. Thompson-Hollands, J., Abramovitch, A., Tompson, M. C., & Barlow, D. H. (2015). A randomized clinical trial of a brief family intervention to reduce accommodation in obsessive-compulsive disorder: A preliminary study. Behavior Therapy, 46(2), 218–229. Tolin, D. F., Maltby, N., Diefenbach, G. J., Hannan, S. E., Worhunsky, P., et al. (2004). Cognitive-behavioral therapy for medication nonresponders with obsessive-compulsive disorder: A wait-list-controlled open trial. Journal of Clinical Psychiatry, 65(7), 922–931. van Oppen, P., van Balkom, A. J., de Haan, E., & van Dyck, R. (2005). Cognitive therapy and exposure in vivo alone and in combination with fluvoxamine in obsessive-compulsive disorder: A 5-year follow-up. The Journal of Clinical Psychiatry, 66(11), 1415–1422. Veale, D. (2007). Cognitive-behavioural therapy for obsessive-compulsive disorder. Advances in Psychiatric Treatment, 13(6), 438–446. Veale, D., Gilbert, P., Wheatley, J., & Naismith, I. (2014). A new therapeutic community: Development of a compassion-focussed and contextual behavioural environment. Clinical Psychology & Psychotherapy, 22(4), 285–303. Veale, D., Page, N., Woodward, E., & Salkovskis, P. (2015). Imagery rescripting for obsessive compulsive disorder: A single case experimental design in 12 cases. Journal of Behavior Therapy and Experimental Psychiatry, 49, Part B, 230–236. Vervliet, B., Craske, M. G., & Hermans, D. (2013). Fear extinction and relapse: State of the art. Annual Review of Clinical Psychology, 9, 215–248. Woody, S. R., & Teachman, B. A. (2000). Intersection of disgust and fear: Normative and pathological views. Clinical Psychology: Science and Practice, 7(3), 291–311. Zysk, E., Shafran, R., & Williams, T. (2018). The origins of mental contamination. Journal of Obsessive-Compulsive and Related Disorders, 17, 3–8. 221 12 CBT for OCD: Evidence-Based Treatment for Contamination and Checking Elizabeth A. Forrester Introduction and Research Did I clean the toilet with my husband’s toothbrush? There are warnings on cleaning products to keep them away from children and pets for a reason. Am I really in love with my girlfriend? The cat could die in a fire if I’ve left the gas on. How can I be sure the marks on my car aren’t from clipping a cyclist without realizing? I might have contracted HIV by stepping on a discarded syringe. Despite the fact that any idea can become an obsession and any action a compulsion, contamination concerns and checking remain two of the most prevalent forms of presentation in OCD. Contamination fears are reported by 25–50% of OCD sufferers, with checking the most common compulsion (Ruscio et al., 2010). While washing, cleaning, and checking are the most prevalent behaviors in OCD, they cover a broad spectrum of concerns and complexity. How Widespread Is Checking as a Compulsion? It is difficult to envisage any forms of OCD devoid of checking in some shape or form. Checking is a consistent feature across the range of OCD presentations and can take a variety of forms, including the following: Overt checking, for example, physically checking doors and windows, feeling pockets for keys, retracing the route driven Visual checking, for example, looking at an object, rereading a letter Reassurance seeking, for example, asking others directly, surreptitiously watching what others do (or gauging their reactions), reviewing psychoeducational materials, doing internet research Covert checking, for example, mentally reviewing an action, checking an internal state (Does this feel right? Do I feel certain?) 222 CBT for OCD 223 Usually a combination of checking behaviors is used and would be carried out more than once. Frequently, repeating actions becomes part of the ritual used in an attempt to alleviate worry and reduce anxiety. If a person has concerns about faeces (i.e., contamination), checking will be a regular behavior, whilst someone whose key concerns are connected with home safety will not automatically have concerns about contamination. Yet often obsessional concerns can range across various domains. This is particularly the case when someone has struggled with OCD over a long period of time: the initial onset of the problem may begin with a specific intrusive thought or worry and generalize to other areas. OCD has a tendency to morph to reflect the concerns of the day. Further examples of the range of obsessions and compulsions involving worries about contamination and checking behaviors can be seen in Table 12.1. Table 12.1. Examples illustrating the range of contamination and checking concerns Contamination Checking Obsessional concerns Blood, bodily waste, or secretions Dirt or germs Illness or disease Chemicals, e.g., insecticides, medicines Environmental contaminants, e.g., asbestos, lead paint, bisphenol A (BPA) Household cleaners, e.g., bleach Animals or insects Mental contamination or tainted by association, e.g., not buying from cancer or learning disability charity shop Accidental or deliberate contamination, e.g., broken glass in food, mishandling medication Obsessional concerns Have I done something dangerous? Fear of being responsible for something bad happening due to not being careful enough, e.g., fire, burglary, illness Welfare of self or others (including pets) Responding to doubts Making a mistake Is my hair falling out? Throwing something away accidentally Have I committed a crime? Do I love my partner? Perfectionism, e.g., cleaning, making the bed, writing a report at work, decorating, dressing and grooming Compulsions Excessive or ritualized hand washing Excessive or ritualized showering or bathing routines Toileting rules, e.g., never sit on seat, wash clothes after opening bowels, avoid public toilets Excessive use (or avoidance) of cleaning products Frequent laundering (including items of apparel not usually washed regularly, e.g., coats, bags, footwear) Actions to prevent contact with contamination, e.g., keeping groceries in bags, separating ‘clean’ and ‘unclean’ clothing, keeping doors and windows closed at all times, wearing gloves for certain activities Careful cleaning of certain items, e.g., mobile phone, door handles Asking for reassurance Compulsions Checking doors, windows, gas, electric, appliances Taking photos that can be checked later Checking the car: Is it locked? Signs of damage? Wallet, keys, phone, valuable items, e.g., jewellery Driving route or retracing steps to check for signs of an accident Checking for signs of injury, e.g., puncture wounds from syringes Checking for possible dangers, e.g., contamination, trip hazards, sharp items, causing offence, making mistakes Bank statements, till receipts Repeated checking Rereading, e.g., books, letters, emails Counting whilst checking 224 Elizabeth A. Forrester The overlap is not necessarily immediately obvious: for example, checking for hair loss may not be due to a diagnosis of body dysmorphic disorder but the result of worrying whether parabens in a shampoo previously used regularly may be harmful. Similarly, someone who is driven to check repeatedly before throwing something away may be concerned that it is contaminated (e.g., with bodily waste from nappies), harmful (e.g., sharp items), or contain something of importance (e.g., jewellery or passport). What Do Checking and Contamination Have in Common? Key features of both checking and contamination are fears about harm, danger, and safety. This may be about harm to themselves or to others, either accidental or intentional. Furthermore, the consequences may be immediate or (more often) in the future or even historically: The bin man will cut himself if I’ve put broken glass in the rubbish (immediate). I will become ill if I use a supermarket trolley that had contained raw chicken (future). What if the building rubble removed from my first flat contained asbestos? (historical) Responsibility, Blame, and Harm A number of belief domains have been postulated, such as beliefs about being a dangerous or harmful person (Riskind et al., 2007) and ideas about one’s own vulnerability and fear of self (Melli et al., 2016). Initially proposed by Salkovskis et al. (2000), responsibility continues to play an important role (Romero-Sanchiz et al., 2015). Overestimation of Threat Overestimation of threat is a frequent clinical feature, although the more recent development of inference-based therapy (IBT) (O’Connor et al., 2009) proposes that the person with OCD develops a doubting narrative which increases the sense of danger: ‘Although it looks clean, the last person to use this toilet may have a sexually transmitted disease.’ Contamination and Disgust A growing body of literature suggests that disgust should be taken into consideration where contamination fears are present (Thorpe et al., 2011). Many studies have found that exposure-based treatments are less effective where disgust is a predominant feature (Ludwik et al., 2015). It is suggested that disgust is less amenable to habituation and there is a greater likelihood of behavioral avoidance, which makes it less likely that therapeutic gains are sustained. CBT for OCD Checking and Memory Beliefs about memory appear to be more important in OCD than actual poor memory. Tackling maladaptive beliefs has been demonstrated to reduce checking symptoms (Alcolado & Radomsky, 2016). Furthermore, repeated checking increases doubt and uncertainty. The detrimental effect it has on clarity and detail of memory has implications for memory confidence (Toffolo et al., 2016). Not Just Right Feelings While Fergus (2014) proposes that not just right feelings are not exclusive to OCD, there is substantive evidence that obsessive checkers use more objective and subjective criteria compared with anxious and non-clinical controls when making decisions to terminate checking (Coles & Ravid, 2016; Salkovskis et al., 2017). Mental Contamination Previously overlooked, mental contamination is now recognized as a distinct concept separate from direct contamination, although there are similarities A preliminary study found that 46% of participants felt dirty without direct physical contact with a contaminant (Coughtrey et al., 2012). According to Mathes et al. (2019), with mental contamination there is a greater propensity for feeling dirty inside, which is less likely to be ameliorated by washing. So, What Does This Mean for Treatment? It can seem that every variant of OCD needs a different approach. So far, cognitive theories fail to provide an adequate explanation why some intrusions are appraised as significant and distressing whilst others are not (Melli et al., 2016). At a more fundamental level, what needs to be addressed in therapy is the overvalued importance of intrusive thoughts, doubts, images, urges, and beliefs regarding their control as these are associated with obsessive-compulsive symptoms at all levels of severity (Kim et al. 2016). McCubbin and Sampson (2006) argue there is a parallel between the intolerance of unwanted thoughts and the intolerance of unwanted emotions in OCD. Low distress tolerance has been found to correlate with OCD symptoms (Robinson & Freeston, 2014). It has also been suggested that compulsions prevent confrontation of distressing emotion and inhibit access to alternative information (Calkins et al., 2013). Third Wave CBT and OCD Third wave CBT has led to interesting changes of emphasis on cognitive aspects of treatment and uses various methods which place this important distinction at their core. 225 226 Elizabeth A. Forrester Mindfulness Mindfulness proposes that obsessive thoughts should be observed simply as mental events rather than an accurate reflection of reality. Outcomes from studies into the use of mindfulness in OCD have so far been inconsistent: in experimental settings they appear to show promise (e.g., Wahl et al., 2013), but there is insufficient evidence of clinically important improvements compared with ERP (Strauss et al., 2018). Metacognitive Therapy (MCT) MCT for OCD focuses on beliefs about inner experiences such as thoughts and urges to carry out compulsions (Wells, 2009) rather than beliefs such as probability, blame, or responsibility. An important feature is the concept of exposure and response commission. This involves engaging in rituals but deliberately invoking unwanted thoughts, for example, showering in their usual meticulous fashion whilst repeatedly thinking, ‘I’m smeared in faeces.’ Acceptance and Commitment Therapy (ACT) ACT utilizes the concept of holding a thought lightly, being an observer of thoughts in the manner of mindfulness so they do not interfere with acting in accordance with the individual’s values rather than in the pay of OCD (Twohig et al., 2015). How Big Is the ‘B’ in CBT? Exposure is an essential component in treatment of all anxiety disorders. Getting the right balance between ‘cognitive’ and ‘behavioral’ in CBT can be tricky for even the most experienced therapists. Sometimes it is the result of therapist ‘drift’ or a preference for discussing cognitive matters (Waller, 2009). For those who have become therapists via the Improving Access to Psychological Therapies (IAPT) route, it is likely that their training has been based on Beck’s CBT approach. Without an adequate grounding in behavior therapy, behavioral interventions rely on behavioral experiments (a cognitive intervention intended to test the validity of beliefs and assumptions) rather than exposure (Binnie, 2015). Through a combination of observations and case examples from clinical practice this chapter will do the following: Take a fresh look at exposure and considers its focus and function Examine the role of thought processes in OCD Consider how changing relationships with thoughts and feelings can facilitate exposure Change our perspective on goals, processes, and defining success Move away from ‘experiments’ and ‘homework’ to living in the real world. CBT for OCD Assessment Although a structured interview protocol (such as the Structured Clinical Interview for DSM-5 [SCID-5] or the Anxiety and Related Disorders Interview Schedule for DSM-5 [ADIS-5]) can be useful, diagnostic tools are rather blunt objects and will not in themselves yield sufficient detail about the person’s lived experience of OCD. The publication of the American Psychiatric Association’s Diagnostic and Statistical Manual (DSM-5) (2013) has been controversial since it removed OCD from the anxiety disorders category and created a new listing of ‘ObsessiveCompulsive and Related Disorders’ which includes other loosely related problems such as hoarding and skin picking. This has spurred various debates. Without discussing the appropriateness of this decision, for the purpose of this chapter the assertion is that psychiatric diagnoses do not indicate which treatment options are beneficial. Psychiatric diagnosis systems have frequently been criticized, not least because they have little utility in the clinical setting since they do not indicate which treatment options are beneficial (Kinderman et al., 2015). They often fail to take into account psychological or sociological aspects. Finding the meaning in the individual’s experiences and responses through the use of formulation enables an understanding of what keeps the problem going (Johnstone, 2018). This is far more useful in clinical practice, particularly since the experience of OCD is unique to each person. It also helps to normalize rather than pathologize the problem. The formulation should be drawn up collaboratively, using the person’s own description and quite possibly their own words. For the OCD sufferer, these invariably include ‘I worry that . . .,’ I feel anxious when . . .,’ and so on. The treatment protocol described in this chapter is formulation driven. Use of Assessment Measures: 1 An objective measure of the severity of symptoms is helpful to enable progress to be monitored. As well as demonstrating validity and reliability as an outcome measure, the following are of therapeutic use to identify key areas of difficulty. Obsessive Compulsive Inventory – Revised (OCI-R) The OCI-R (Foa et al., 2002) continues to demonstrate good reliability as a selfreport screening measure (Wootton et al., 2015). Yale–Brown Obsessive Compulsive Scale (Y-BOCS) The Y-BOCS (Goodman et al., 1989) continues to be considered the ‘gold standard’ for OCD assessment, although a newer version has been developed (Rapp et al., 2016). Administered by the therapist, its checklist of obsessions and compulsions is particularly helpful as a prompt for less troublesome concerns that may go unreported. 227 228 Elizabeth A. Forrester Ratings of mood and anxiety are also helpful additions. While the Beck Anxiety Inventory (BAI) and Beck Depression Inventory (BDI) are excellent measures, they create an unnecessary burden as part of a wider battery of questionnaires. Therefore, brief measures are sufficient, unless clinically indicated (Kroenke et al., 2001; Spitzer et al., 2006). How Much? How Often? Measures should be kept to a minimum and do not need to be repeated each session. From clinical experience, a significant number of OCD patients have difficulties completing questionnaire measures; thus, there is a paucity of research on this topic. Many checkers, for example, may take a long time to fill in self-report measures due to urges to check or indecisiveness about how to score an item. Whilst beginning and end of therapy would be the minimum data set, consider using assessment measures at pivotal points during treatment where change has clearly occurred. If follow-up appointments are offered once active therapy has ended, measures can also be used to track maintenance. Use of Assessment Measures: 2 There may be occasions during treatment when other measures may be used to rate specific features of clinical presentation such as responsibility appraisals, the importance of thoughts, or thought-fusion. The following are useful measures: Responsibility Attitudes Scale (RAS) (Salkovskis et al., 2000) Metacognitions Questionnaire (MCQ-30) (Wells & Cartwright-Hatton, 2004) (in Wells, 2009) Thought Fusion Instrument (TFI) (Wells et al., 2001) (in Wells, 2009). Obtaining an Overview Without a feel for both the content and extent of the problem, treatment might miss some important aspects that could hamper progress. OCD is the most idiosyncratic of the anxiety disorders, with many subtleties and differences. Not all contamination fears are about dirt and germs, in the same way that not all checkers worry about leaving the gas on. A familiarity with the many different ways in which OCD presents and can affect a person’s life is essential in order to understand the most appropriate questions to ask to assist in making a rudimentary formulation. Case Vignette Ask any of his colleagues and they’d say that Matthew was a brilliant paramedic. Professional and knowledgeable, yet thorough and calm in a crisis. He never balked when called to an emergency, no matter how gory. Inside his head, however, and CBT for OCD especially away from work it was another story. His mind was constantly on alert for potential dangers from bodily fluids or unknown diseases of the people he ministered to. He would keep a mental track of everything he’d handled or stepped on, keep a close eye on what his colleagues touched, and was careful never to touch his face after he’d removed the surgical gloves until he’d been able to thoroughly wash them. At the end of a shift, he’d change into ‘civvies’ before going home to his wife and children, stowing all his work clothes (right down to socks and underwear) in a bag he kept specially for this purpose at the bottom of his locker. Once a week, he’d make a trip to a launderette a few miles away from the ambulance station. Although he had to make a special detour to get there, he figured it was worth it despite the cost. He admitted he spent a small fortune on cleaning products and replacing many items of clothing he’d simply got rid of because they seemed too dirty. Once he got home, only after a thorough shower with chlorhexidine gluconate in the downstairs shower room used exclusively by him, followed by a swift wipe-round with disinfectant wipes, was he ready to put his feet up and relax. After all, he couldn’t risk the well-being of his family by bringing any source of contamination into the house. The following provide the basis for useful lines of questioning: Are there particular ‘rules’ about the way you do things or have to follow certain rituals? How does it impact on your daily living? What other consequences does OCD cause? Is there anything you don’t do because of this problem? Rules and Rituals. An inability to vary routines or procedures is frequently a feature. For example, hand washing is carried out equally meticulously regardless of the activity that it follows (such as throwing a scrap of paper into an open waste bin, putting away groceries, changing the baby’s nappy). Similarly, checking routines are carried out thoroughly, whether it’s scribbling a note to remind themselves to buy some milk on the way home or preparing their tax return. In other words, actions taken do not reflect the individual needs of specific situations. Impact on Daily Living. The severity of impact on daily living may vary greatly. Subtle changes to routine or small avoidances have often crept in over time; the initial reason for these changes has been lost as these alterations become absorbed as the usual way of doing things, for example, using paper kitchen roll instead of a tea towel, keeping windows and doors locked when at home, storing cleaning products in a locked cupboard even though the ‘children’ are adults. Without over-pathologizing habits and practices, the therapist must develop an awareness of subtle behaviors that may need addressing as therapy progresses. Unwanted or Unintended Consequences. Contamination fears can unexpectedly lead to quite the opposite. Routine domestic chores are so terrifying or timeconsuming that they are avoided; for example, clutter accumulates when rubbish can’t be put out for fear of contamination or losing something. There may be financial costs. With contamination concerns, a lot of money may be spent on cleaning products and toiletries, or replacing items discarded as unclean 229 230 Elizabeth A. Forrester or simply worn out from over-cleaning. Vigorous checking can damage locks, handles, or taps, while worries about potential dangers from items (like domestic appliances) may mean they are regularly replaced for a newer version that promises enhanced safety features. Impact on Activities. OCD may restrict leisure and social life, leaving little scope for pleasure and enjoyment. With checking and contamination worries, activities such as leaving the house for any length of time, travel, or eating out are affected. Avoidance may not be deliberate: there may not be time to do anything beyond rituals and compulsions. Identifying Covert Compulsions. Because these happen internally, the individual may not recognize them as behaviors. These actions may not even seem to be conscious and often are not differentiated from the experience of thoughts. However, overlooking covert compulsions is often a major reason for treatment failure (Pence et al., 2010). Common covert strategies include the following: Counting whilst carrying out a compulsion ‘Should’ statements, for example, ‘It should be okay’ Repeating special words, images, or numbers Reviewing actions Mentally ‘erasing’ an unwanted thought or image (e.g., trying to picture something clean) Completing a mental check list (e.g., ‘I hung my bag on the back of the washroom door, tore off the first six sheets of toilet paper, covered the seat with toilet paper, didn’t touch the walls’) Create mental ‘paper trail’ tracking actions for future reference (to make them more memorable – different to reviewing actions, as this is either whilst activity taking place or very soon after) More detailed accounts of the clinical assessment can be found in Forrester (2015) and Van Niekerk (2018). From Assessment to Formulation A comprehensive clinical picture in cognitive behavioral therapy requires more than a list of symptoms. The effects of OCD are far-ranging and affect many aspects of the person’s life. As an initial between-sessions task, the therapist should ask for a (written) list of the following: Things you do too much Things you do too little of Anything you avoid. While there will inevitably be some replication of compulsions discussed during assessment, it also gives an idea of how the client’s world might have shrunk or be compromised by the problem. An effective intervention needs to take this into account. Whilst many behaviors are self-explanatory, others are less so. Lavinia CBT for OCD avoids listening to the radio so she would be able to hear if the dog was in difficulty. She prefers not to go out as she worries so much about leaving the dog at home (even though she puts him in a cage). In addition, she read that many things are toxic to dogs – such as certain flowers and food stuffs. This means she doesn’t like to cook at home and takes precautions after preparing meals. An awareness of the wider picture is useful when considering goals for therapy. Overview of Treatment CBT for OCD should be considered as a brief, time-limited intervention even when the problem is severe and/or chronic. This approach is generally delivered over 12–15 sessions of an hour’s duration. For optimal impact, the first few sessions should occur weekly while the patient is socialized into the model and developing an understanding of both what maintains the problem and what they need to change. Frequency of subsequent therapy sessions is at the discretion of the therapist; more time may be required for therapeutic tasks to be practiced between sessions and (towards the end of therapy especially) to foster autonomy and independence prior to discharge. Additional time may be necessary when in vivo tasks are carried out during a session. The approach can be condensed hours into a briefer time frame without compromising outcomes (Challacombe & Salkovskis, 2011; Oldfield et al., 2011). This may be particularly appropriate where timing of an intervention is an important factor, such as impending parenthood or physical health considerations. Structure of Treatment Following initial assessment, structure of treatment can be broadly considered as having the following five phases: 1. Formulation 2. Developing a less threatening view of the problem 3. Focusing on change using a combination of behavioural and cognitive interventions 4. Building on progress 5. Maintaining change and preventing relapse. Case Formulation OCD can seem so random and senseless to the patient that they’re left puzzling about what it all means. Case formulation (see Figure 12.1) is the key to developing a shared understanding of the problem. The following steps create a cohesive thread through what’s often nicknamed the ‘vicious flower’: 1. Can you recall a recent situation that triggered one of your worries (or intrusive thought)? 2. What thought did that trigger? 231 232 Elizabeth A. Forrester 2. Intrusive thought, urge, image or doubt • Image of houses on fire 1. Situation Leaving the house to take my daughter to school Did my routine check 5. Neutralizing • Checking • Use random word to make it memorable • Take photo of hob and door 4. Feelings • Anxious • Tearful • Feeling sick 3. What this thought meant to me e.g., Why I believed I shouldn’t ignore it • 6. Counterproductive safety-seeking behaviors • Try to feel completely certain • Try not to have any doubts ( or horrible images) • I can’t trust my judgment If something went wrong I couldn’t live with the guilt 7. Attention and Reasoning biases • Looking for trouble: I notice all kinds of potential dangers • Emotional reasoning: If it feels dangerous it must be dangerous Figure 12.1. Case formulation. 3. Why did the thought seem so important to you at that moment? What made it hard to ignore or dismiss it? 4. How did it make you feel? Did you notice any physical sensations? 5. What did you do to make yourself feel better? (Prompt for overt and covert rituals) 6. Is there anything that you did to help keep you safe? 7. Are there particular attention or reasoning biases? Situation. Although invariably the person may try to describe a number of situations (especially if they have a variety of obsessional concerns), emphasize the importance of just discussing a recent one. The rationale for this is that they will have a clearer recall for details, which will be helpful for the formulation. CBT for OCD Intrusive Thought. Thoughts may also occur in the form of doubts, urges, or images. Meaning. The meaning isn’t always readily accessible, often because the person immediately engages in safety behaviors to prevent the occurrence of beliefs such as being responsible for harm or being a dangerous person. Stopping or delaying a compulsion will usually elicit the meaning. Feelings. As well as emotion responses such as anxiety, anger, or even depression, include physical feelings (e.g., tense, hot) and any mental references such as stressed, doubtful, or a sense of something terrible about to happen. Although there is no research evidence to date, clinical observation suggests that, in a similar way in which panic results from catastrophic misinterpretations of normal bodily sensations, it is possible that a person with contamination OCD may misinterpret the sensations of their sweating palms (an anxiety response) as feeling dirty. Similarly, frequent washers often have extremely dry skin on their hands and become sensitized to changes to the feel of their skin. Neutralizing. Any action (i.e., compulsion) to counteract the thought or reduce anxiety is neutralizing. The link between the neutralizing action and the harm it is intended to prevent may not be a direct one, for example, superstitious behaviors such as touching wood, or other idiosyncratic actions. Overt compulsions such as cleaning, checking, or repeating are outwardly observable. Covert actions (such as mental debate or thinking a good thought after a bad one) may be overlooked as behaviors. Counterproductive Safety-Seeking Behaviors. Many safety-seeking behaviors are in fact counterproductive. Attempts to suppress thoughts lead to further intrusions. Striving to be perfectly clean, safe, or certain is attempting to achieve the impossible. Avoiding, say, cleaning the bathroom due to worries about toilet germs means the bathroom gets dirtier from neglect. Attention and Reasoning Biases. Attention is drawn towards things that have personal relevance or importance. Thus, the patient is more likely to notice threat cues, and reason that this is further evidence for how dirty or dangerous the world is. Reasoning bias plays a role in another way: feeling anxious can be misinterpreted as a sign of danger. More detailed guidance to developing the vicious flower formulation with the patient can be found in Forrester (2015) or Bream et al. (2017). Socialization to the Model So it isn’t the thought (doubt, image or urge) that’s the main problem, but what you believe it means – and what you do in response to it. While various illustrations of how thought suppression is ineffective (try not to think of a polar bear), the following helpfully demonstrates the interplay between thoughts, emotions, and behavior and where it is possible (as well as impossible) to intervene: Imagine a masked gunman bursts into the room and puts a pistol to your head and shouts, ‘Don’t have any scary thoughts!’ Would you be able to stop such thoughts? 233 234 Elizabeth A. Forrester I reckon not. And if they said, ‘And don’t feel frightened!’ could you prevent yourself from feeling afraid? Again, highly unlikely. But imagine they then demanded you sang a nursery rhyme and danced to the tune, could you do that? While it isn’t possible to control what comes into our mind or prevent our emotional response, we are able to make choices over our actions. Instead of trying to persuade yourself that things are safe or clean before changing what you do – change behavior and belief change follows. Features of Treatment Shared understanding of maintenance factors Changing relationship with thoughts and feelings Exposure third wave style Tackling rumination and overthinking Use of anti-OCD. Will There Be Homework? As all CBT therapists know, therapy doesn’t begin and end in the therapist’s office. What the patient does between sessions is even more important: Therapy for OCD is like going to a slimming club. It’s helpful to go along each week, get some helpful tips, recipes, and encouragement to help you lose weight. If you keep eating cakes, chips, and chocolate in between times, nothing will change – you might even gain more weight. It won’t always be easy, but we can work together to help you stick to the diet. The idea of ‘homework’ suggests a specific, discrete activity separate to activities of daily living (including those aspects defined by OCD). It’s often put off until the last minute. To continue the slimming club analogy, the process of therapy is akin to healthy eating and lifestyle rather than a crash diet. This is a more holistic approach which facilitates individuals to thrive, as opposed to focusing on the absence of symptoms or psychopathology (Hayes & Hofmann, 2017). In other words, there won’t be homework, but there will be something far more dynamic: a plan of action. Plan of Action: From Formulation to Treatment Since the formulation is based mainly on a specific occurrence of OCD, it is not certain whether it has explanatory power for other situations. Hence the patient is asked to draw up some further formulations before the next session when OCD occurs. This is particularly useful when there are other kinds of presentation. A helpful way to phrase it is: ‘Let’s see if it still makes sense when OCD affects you in other ways, with other kinds of concerns or if we need to revise it in any way.’ In addition to ascertaining that the person understands the maintenance cycle, the process of change can begin by suggesting they either resist a compulsion to gain CBT for OCD 235 further insight (it is possible they haven’t done this for a long while) or simply do something differently. A Picture Paints a Thousand Words Although particulars of routines, rituals, and compulsions will have been obtained at the initial meeting (and added to as further features emerge during treatment), direct observation provides a wealth of detail in a glance. It may be possible to carry out an exposure task in the consulting room, for example, touching something ‘dirty’, or at the very least to demonstrate how a particular ritual is carried out, for example, hand washing. A home visit can be invaluable (see Table 12.2). Of course, this is not always practicable, in which case a step-by-step breakdown (even ‘miming’ a routine) can be done. Developing a Less Threatening View of the Problem The key to understanding OCD and what keeps it going is the meaning attached to the occurrence of particular intrusive thoughts, and the implications this has in terms of what is required to prevent this dreaded outcome. By continuing to take Table 12.2. A picture paints a thousand words Presenting problem: Justyna describes significant worries about contamination, that dirt is brought into her home from outside; in particular, she fears insect infestation. ‘What really gets me down is that vacuuming takes hours. It’s really exhausting.’ Therapist’s mental picture: So, we have a spotlessly clean house with every room carefully vacuumed, right up to the edges. No wonder it’s exhausting if the furniture – including beds, sofas, and wardrobes – is moved every time in order to clean beneath and not a bit of fluff or dirt around the skirting boards. The reality: On a visit to the home, the therapist is ushered to the only chair that does not have things piled on it. Justyna explains that the plastic boxes on the other chairs and sofas contain items she fears may be contaminated, which (in time) she plans to deal with but she’s too stressed at the moment to take on the task. She moves one of the boxes so she can sit down. Embarrassed, she admits that another reason for putting stuff everywhere is so she can control where the therapist would be able to sit. She has also placed throws on every chair because they can be washed more easily than the upholstery. Prior to the visit, Justyna agreed that she would demonstrate how she did the vacuuming. The therapist observed that the carpet did not look clean, and there was a distinct border about 20–30 cm in breadth around the perimeter of the room and items on the floor which was thick with dust and fluff. Before commencing vacuuming, Justyna put on slippers she kept exclusively for the task – first wiping the soles with a disinfectant wipe which she then discarded. A fresh wipe was used to wipe down the vacuum cleaner, a precaution she always took just in case part of it had been in contact with something dirty (perhaps the cable had touched a ‘dirty’ patch of floor). Often she had to repeat this if a doubt came into her mind, or if she was interrupted while attending to disinfecting the appliance. She’d begin by vacuuming a small area of carpet, stretching only as far as she could reach so her feet would not encroach on the newly cleaned area. By wiping the soles of her slippers again, she could then proceed to the cleaned area and repeat the process on the next patch. Meticulous care was taken not to get too close to furniture, walls, or other potential sources of contamination, hence the unvacuumed margins. 236 Elizabeth A. Forrester precautions in an attempt to feel safe or reduce risk, we never discover how necessary these behaviors really are, which in turn reinforces the belief that they are necessary actions. Helga believed that her judgment was poor and she lacked ability to assess safety or cleanliness in everyday situations. Helga: The thing is, I’ve had this problem for so long I just don’t know whether or not things are clean enough, or if I’ve done something that could put others at risk in some way. I’ve no idea how to do things properly. Therapist: Is it that you consider that your judgment is poor? Helga: Yes. I’m constantly wondering if I’ve done something wrong or dangerous. I just couldn’t live with myself if I thought I had. Therapist: So, it sounds like you have a theory about what your problem is . . . that it would be dangerous or irresponsible to ignore the thoughts? Helga: That’s right. Theory A/Theory B Theory A/Theory B is a common and effective tool for introducing alternative explanations for OCD-driven thoughts and behavior (see Table 12.3). For more details about developing Theory A/Theory B, refer to Forrester (2015), Bream et al. (2017), or to Chapter 11. The Right Solution for the Problem? If the problem was indeed harm or danger, then all the actions the person has been taken would of course be sensible solutions. If something toxic had been spilled, it’s entirely reasonable to wipe it up and clean the area thoroughly. It’s appropriate to check whether any shards remained if some glass smashed on the floor. However, it’s the wrong solution if the problem is worry about danger. Ideas generated by asking, ‘What would we do if we were treating this as a worry problem?’ help form the basis of the intervention and aims of treatment. Already, change becomes a possibility. Previous precautions are no longer necessary. Debunking the Myth of Graded Hierarchies. To grade or not to grade? That is indeed the question. While exposure is the essential ingredient in any anxiety treatment, consideration is required to optimize its efficacy (Jordan et al., 2017). Reasons in support of not taking a stepped approach include the following: The stepped approach is time consuming, especially if habituation is required before moving to the next step. Habituation does not fit the traditional neat reduction shown in textbook graphs. Habituation may not occur (some things will always induce a degree of fear or discomfort). The stepped approach reinforces the idea that some situations are more dangerous than others. The stepped approach does not reflect real life. CBT for OCD 237 Table 12.3. Theory A/Theory B Theory A: My problem is that my judgement is poor and I wouldn’t be able to live with myself if I’d harmed someone (i.e., danger or harm problem) Theory B: My problem is that I worry that my judgement is poor and I wouldn’t be able to live with myself if I’d harmed someone (i.e., a worry problem) What I need to do Act on every thought about danger or harm. Identify all possible hazards or dangers. Clean everything thoroughly. Wash my hands a lot. Keep clean and dirty things apart. Use antibacterial products on everything to avoid spreading my germs. Give ‘dirty’ things a wide berth. If I have a doubt, treat it as dirty. Reduce/stop any potentially dangerous behaviours, e.g., driving, buying ‘hazardous’ gifts, cooking for others. Allow others to make decisions to reduce my responsibility. Lock myself in the house so I can be sure I haven’t done something. Do things slowly and methodically so I can remember exactly what I did. What I need to do Not do the things on Theory A list! Allow thoughts and worries to come and go without acting on them. Don’t think too hard about hazards and dangers. Clean and wash like most people do, e.g., just use a damp cloth to wipe kitchen counters after cooking, wash hands only when greasy or visibly dirty. Sit down in public places, walk past bins, etc. Mix things up at home, e.g., put shoes in the kitchen, put coats and bags on the bed. Drive, cook for the family, buy gifts such as glass, candles, or other ‘hazardous’ items. Make my own decisions even if they’re scary. Deliberately go out several times each day (and not lock myself in). Do things in a breezy and relaxed way. If I have a doubt, treat it as OCD! Evidence for Theory A Things are dirty and people get ill through contact with dirt. It feels dangerous. Checking and cleaning makes me feel better. I don’t know what good enough cleaning is like. There have been times when I can’t remember whether I’ve done something that could be harmful. Evidence for Theory B Others don’t take the precautions I do yet don’t seem to get ill more than me. I get more of these worries when I’m stressed for other reasons. The focus of my worry changes – it’s often specific and not logical. People move on after bad things happen, even if it’s something that they’ve done. Most importantly, if viewing OCD as a worry problem (Theory B), there is no need for it: a worry is a worry. Grading compulsions give them extra meaning and power. There is substantial evidence for the effectiveness of using random schedules of exposure (e.g., Craske et al., 2008). Similarly, by increasing the range of contexts in which new learning takes place, more retrieval cues are generated, which increase the likelihood of the person remembering to make a different (more helpful) response (e.g., Bjork & Bjork, 2006). Although grading is unnecessary, it is still important to have targets to help orientate the intervention. They provide a guide towards the patient’s desired outcome: put simply, being able to do things the way most people do. See Table 12.4 for an example. 238 Elizabeth A. Forrester Table 12.4. OCD/non-OCD way OCD way Non-OCD way Wash hands thoroughly before touching or feeding my dog. Read label on dog food carefully each time. Rinse her dishes (and ours) several times to ensure no detergent traces. Don’t allow her in the garden unless I’m with her. Keep cleaning products in cloakroom with the door shut or locked in under-sink cupboard. Check lights and appliances several times before leaving the house. Take a photo of the front door so I know it’s closed. Keep all receipts to check against bank statement each week. Wash hands only when necessary. Just pick up the can or packet and feed her. Wash and dry dishes without rinsing. Let her play in the garden while I’m at home, either indoors or outdoors. Leave door open to air the cloakroom, remove child-lock from kitchen cupboards. Switch things off as I go, don’t check (or only have a quick glance). No photos! Just lock and go. Keep receipts only for high value items. Check statement once a month only. Exposure starts by doing things differently, changing habits, and learning from those experiences. The advantages of approaching it in this way are the following: 1. 2. 3. 4. 5. It’s more naturalistic and fits in with daily life. It increases opportunities for exposure to other things. It moves away from the idea of ERP as a discrete ‘homework’ activity. There is always scope for doing something differently. It increases cognitive flexibility. The Role of Habit in OCD. ‘If you always do what you’ve done, you’ll always have what you’ve always had’ is a useful adage for tackling OCD. The role of habit in OCD has been widely investigated (e.g., Gillan et al., 2014). Such findings are consistent with frequent clinical observations that people with OCD often engage in compulsions ‘by accident’ rather than triggered by a threat appraisal or physiological arousal, when their intention had been to adhere to the treatment protocol of ERP. The implications for treatment are that alternative instructions are needed about how to respond in given situations. It is not always easy to differentiate between an OCD-driven behavior and habits, preferences, and conventions of individuals. It can be helpful to view everything we do on a continuum (e.g., Mataix-Cols et al., 2005). After all, an isolated thought or action is not by itself an indicator of OCD, but when thoughts and actions are observed in a cluster with other features, they can then be considered symptoms. The fixedness of certain characteristics can be an indicator. For example, repeated checking leads to it becoming an automatic response in OCD (Dek et al., 2015). Anything that is done regularly and repeatedly becomes habit and the default way of doing things. This applies not only to what we do but also to what we don’t do: I always Take a photo of the door when I go to work. Use a tissue to open the door in public places. CBT for OCD Check my car for signs of damage before and after a journey. Closely examine the pavement for signs of blood, vomit, faeces. I never Use the same towel twice or share my partner’s. Leave the kettle or microwave plugged in when not in use. Wear clothes that can’t be washed. Drive on motorways or dual carriage ways. Safety Behaviors and Effective Exposure. While all responses to reduce anxiety, suppress unwanted thoughts, or otherwise ‘feel better’ should be considered safety behaviors and therefore need to be targeted in therapy (e.g., Abramowitz, 2006), it can also be argued that any change in the right direction is good. Safety behaviors can play an important role in encouraging engagement in exposure as long as they do not interfere with learning that a feared situation is in fact innocuous (Levy & Radomsky, 2016; Milosovic & Radomsky, 2008): ‘Charlene would have been unable to take her child to a public toilet if she hadn’t been allowed to wash her own hands thoroughly afterwards, and would not have discovered that her child did not become ill as a consequence.’ Fears relate not only to external outcomes but also to the emotions the feared stimulus elicits (Van den Hout et al., 2012). In Charlene’s case, it also imbued a sense of control over her feelings of disgust but perhaps more importantly allowed her to discover that these feelings did not persist (or escalate) but receded over time. She discovered that she was able to cope with them. Rationality, Risk, and Cognitive Restructuring. The clinical efficacy of exposure therapy is enhanced by the addition of cognitive interventions (Rector et al., 2019). Cognitive restructuring within the context of CBT for contamination and checking is focused on appraisals of the likelihood of being able to cope with feelings of discomfort (whether that be intrusive thoughts, physical sensations of anxiety, or feelings of distress, doubt, or uncertainty). The primary aim of therapy is not to prove or disprove the likelihood of feared outcomes, although that may occur as a by-product of therapy. A major obstacle in attempting to do so is that such concerns are not always amenable to testing: ‘Just because I haven’t run someone over on this occasion doesn’t mean it won’t happen in the future.’ However, the person may coincidentally discover that they do not lie awake all night after resisting urges to check. Box: Risk versus Uncertainty Julia was uneasy about letting her son go on the school trip to London. Anything could happen: the coach could crash, maybe he’d be abducted, there could be a terrorist attempt. It couldn’t be guaranteed that they definitely wouldn’t – so there’s a risk. Equally, there’s no guarantee that something similar wouldn’t happen if he were kept at home for the day (or taken to an amusement park by his parents, as she’d suggested). She was asked to weigh that risk against the certainty of him feeling left out when his classmates chattered excitedly about their shared experience. 239 240 Elizabeth A. Forrester Dichotomous Thinking and Overestimation of Threat. A tendency to dichotomous thinking exacerbated obsessional worries. If it isn’t clean or hygienic, it must be dirty or even contaminated. If we’re not convinced a situation is safe, it must be dangerous. The notion of risk is exchanged for absolute certainty, where in reality a feared outcome is only one of many possibilities (the majority of which may well be benign). ‘Any human activity involves some risk to life or health. Although it is possible to reduce the existing risk of a particular activity, it is not possible to reach the “zero risk” or “absolute safety” that is often demanded. Once this general fact is recognized, it then becomes necessary to define an acceptable level of risk’ (Black & Niehaus, 1980). Constant striving for certainty is an attempt to achieve the impossible. Certainty research often fails to differentiate between pathological and normative contexts (Cougle & Lee, 2014). In an age of instant access to ‘facts’, intolerance of uncertainty is rife. Risk Isn’t Only about Bad Things Happening. Just because something can happen doesn’t mean it will happen. It’s also often overlooked that risk isn’t only about bad things happening: Shirley: Therapist: Shirley: Therapist: But what if I put the dirty laundry on the bed and I can’t get the worry out of my head and my anxiety gets worse and worse? Don’t forget that risk isn’t only about bad things happening. How about taking the risk that by doing this you find it quite a challenge and discover it’s not as hard as you think it’s going to be, that you can cope with it. How would that feel? Ha, you’re right. I know it’s just my glass-half-empty way of looking at things. When I stopped washing my clothes with disinfectant I thought I’d never be able to wear them and feel comfortable, but actually it wasn’t that bad. So, maybe it’s worth taking the risk that it could go well. Thoughts and Thinking Understanding the difference between thoughts (the event of having a thought) and thinking (the process or action one takes in response to that thought) is a key factor in overcoming obsessional concerns. Normalizing the occurrence of intrusive thoughts is essential, but it is equally important for the patient to develop an understanding of how thoughts come and go, ebb and flow without any apparent act of will or effort from them. It is interesting to note that higher reports of spontaneous mindwandering are associated with increased OCD symptomatology (Seli et al., 2017), yet participants in the study were less likely to make negative or threatening appraisals when they deliberately chose to allow their minds to wander. This is further evidence, in fact, that attempts to control thoughts are counterproductive. Thought Bingo Encouraging patients to take a step back to observe what they’re actually doing is crucial. It should not be overlooked that thinking is also a behavior, and one that is CBT for OCD often used in an attempt to reduce uncertainty or anxiety. An exercise called Thought Bingo (see Appendix 12.1) can help the person discover the different ways in which they typically get caught up in rumination – the different ways in which they think. Amongst many other possibilities, these are typical manifestations: Reasoning Analyzing Debating Problem-solving Imagining. Helping people to learn about and understand their own thinking enables them to gain a little critical distance from it, as well as an awareness of its role as a maintaining factor. Allowing Thoughts without Thinking While thought suppression is impossible, developing the skill of allowing thoughts to occur without thinking about them is essential. Overthinking leads to increased worry as illustrated in the following. My husband let the cat in last night. It just ran straight through the kitchen, into the hall and up the stairs. I shouted at him to go and catch Misty while I checked the kitchen floor. I couldn’t see anything obvious so I knelt down to have a closer look. There were a few dark spots – I wasn’t sure what they were, they could have been anything. You’ve no idea where they go when they’re outside. She goes to the toilet out there, other cats do too . . . and foxes.. . . There could be anything on her paws. It’s disgusting. I can’t believe he didn’t wipe her feet before letting her through. I cleaned the tiles with bleach and then some disinfectant, but it still bothers me. I wanted to clean the carpet with it too but my husband stopped me so I just scrubbed at it with a soapy cloth when he wasn’t looking. Maybe we should get rid of the carpet. It’s just not hygienic. When I eventually went to bed, I just couldn’t settle. What if Misty had been on the bed? She might have run across the pillows. There are mice in the garden, and bird poo.. . . What if some of the lawn fertilizer hadn’t dissolved? I put my pillows in the bath so they could be washed in the morning. At least the sheet underneath them would still be okay. The Role of Rumination In the context of OCD, rumination refers to (ego-syntonic) repeated mental acts (e.g., mental debate or argument) carried out in response to (ego-dystonic) intrusive thoughts, doubts, or images in an attempt to reduce anxiety. Depressive rumination dwells on causes, meanings, and implications of negative symptoms, feelings, and problems with attempts to make sense of why something happened Whilst for both it may be conceptualized as a mental habit, there is a strongly purposive element in OCD rather than a passive focus on negative content (Watkins & NolenHoeksema, 2014). 241 242 Elizabeth A. Forrester There is a growing body of evidence for rumination as a transdiagnostic feature of both anxiety and depression (e.g., McEvoy et al., 2013). Indeed, the processes have many similarities. However, in OCD the use of ‘thinking solutions’ is very much a part of the problem and is more prevalent and distressing (Wahl et al., 2011). Rumination Is Never about Now Rumination is more prevalent where concerns are connected with something that has not yet happened (i.e., an imagined event in the future) or that happened in the past that is not amenable to physically checking: If I’m concerned there might be a hazardous substance in my house, it’s possible to check – but if I have a doubt whether or not there was a hazardous substance in the house I lived in several years ago which has now been demolished, I can’t. That’s particularly true for doubts about abstract concepts, for example, ‘Do I really love my partner?’ These kinds of moral questions – or questions about the nature of ‘being’ – elicit strong feelings but, even more importantly, they have no absolute answer. These things are not ‘knowable’ in the ‘fact’ sense (Forrester, 2017). Rumination Increases Likelihood of Further Intrusions Rumination prevents the natural ‘decay’ of memories of actual events. Repetition creates memories of thoughts, whether or not the thought was factual. By regularly bringing to mind a specific event associated with their obsessional concerns (e.g., losing a packet of tablets on the bus), it won’t just fade away to become a distant memory (or even be forgotten about, as would happen with many autobiographical memories that we don’t attribute a special significance to). Someone who doubts whether they may have run someone over in their car pictures something that hasn’t happened while trying to make themselves certain that it didn’t, and will recall that image. Rumination Prevents the Mind Wandering Freely Selectively attending to and considering threat-related intrusions may prevent other kinds of thoughts – nice or interesting or creative thoughts –that might distract them from their thinking (e.g., Welz et al., 2018). I could have cleaned the toilet with my husband’s toothbrush.. . . When did I last clean it?. . . It was when Naomi popped in.. . . She’s so funny . . . what was that joke? Must ask her again soon. I wonder where she got her dress from . . . such a lovely color. Although it may seem as if they have no choice, they may be actively choosing to attend to thoughts they consider important. This internal focus reduces cognitive resources left for other tasks and has a detrimental effect on performance (Koch & Exner, 2015). CBT for OCD Thinking Is not Doing! Although rumination is universal, in OCD the tendency is to do only this and very little else. In addition to addressing cognitive processes, the emphasis needs to remain on behavioral change. Encouraging the question, ‘What could I do differently to challenge OCD?’ means every activity of daily living becomes an opportunity. It’s Not What You Do but How You Do It We all wash, we all check, we all take care not to step in dog mess or to run pedestrians down in the street. The difference between someone who struggles with OCD and someone who doesn’t is a matter of degree. Rules are often used to create certainty – although they are impossible criteria (what’s the perfect hand wash?). What is needed is a lightness of touch. Focusing too hard, too closely on what you’re doing is closely related to overthinking. Initially, however, some new rules are required. Using the list of non-OCD actions for guidance, these instructions might include: Dry the laundry outside instead of indoors. Cook a meal with chicken twice a week. Decline receipts for purchases under £5. Leave kitchen appliances plugged in and switched on at the wall. Guidelines, not Rules! Guidelines offer flexibility. Development of flexibility is encouraged: it’s nicer to be able to use a well-kept toilet, but if you need the toilet and the only one available has a floor swimming in goodness-knows-what it would be most people’s preference to hitch up their trouser hems and hover over the seat rather than the discomfort of trying to hold on (or the imminent likelihood of wetting themselves). On a less graphic level, at home we might choose to wash an apple before eating it, but when having fun at a picnic would just give it a quick ‘polish’ on our sleeve. Dichotomous thinking is a feature of rigid rules: if I don’t do it the ‘right’ way it must be ‘wrong’; if it’s not ‘safe’ it must be ‘dangerous’. Building on Progress Spending less time on rituals or compulsions can dramatically improve quality of life, but it leaves scope for OCD to creep back in. Doing things the way that most people do (i.e., the non-OCD way) is not enough. How Far Is Far Enough? In order to change unhelpful habits, it’s necessary to act as if the less threatening alternative is true, rather than wait until we believe it or feel confident. After all, confidence results from doing the kinds of things that lead to anxiety/distress. Not only does doing more extreme things expand the person’s comfort zone; it means they are taking a proactive role in tackling OCD. Rather than simply viewing the 243 244 Elizabeth A. Forrester absence of obsessive thoughts as desirable, it should be also viewed as a potential indicator that the patient needs to push themself to do more. A timely reminder may be needed that exposure to thoughts is what is required. Anti-OCD More intensive exposure leads to greater reductions in anxiety levels and fear beliefs (Norberg et al., 2018). While this does not mean doing more dangerous things (although, as previously stated, nothing is without risk), it requires exposure to more challenging thoughts. By introducing a modicum of playfulness in therapy, creative anti-OCD ideas can be generated (see Table 12.5). Initial resistance is often encountered with the patient concerned that they will have to do any of the things Table 12.5. OCD/non-/anti-OCD OCD way Non-OCD way Anti-OCD way Avoid walking near dog poo or even looking at it Walk in areas where dogwalkers go. Go for a picnic and sit on the grass. Unplug all appliances off before leaving the house. Leave the kettle, TV, alarm clock, and table lights plugged in all the time. Ask mum to check my mail before shredding it. Decide for myself what to throw out. Shred only bank statements. Read label on dog food carefully each time. Rinse her dishes (and ours) several times to ensure no detergent traces are left. Just pick up the can or packet and feed her. Wash and dry dishes without rinsing. Check if I get aroused by images of men or women. Avoid any films or TV that might feature homosexuality. Try not to notice anything that looks like male genitalia. Be friendly and chatty with both sexes without wondering if I fancy them. Watch whatever I want to. Deliberately step on dark marks on the pavement. Make some chocolate cakes that look like dog poo for my son. Print pictures of dog poo and put our shoes on them. Switch lights, TV, radio, oven, kettle, and toaster on and go out for the afternoon. Use an image of a burning house as a screensaver on my phone. Put some bank or credit card statements in recycling without tearing them. Write my bank account number on a piece of paper and leave it on the bus. Stick ‘Poison/toxic’ symbols on the packets. Deliberately leave a dollop of detergent froth on dishes. Leave a bleach bottle on the floor where she eats. Play ‘Glad to Be Gay’ on my MP3 . . . on repeat. Agree with my thoughts. Deliberately watch Broke Back Mountain and ‘Queer Eye’. Buy a phallic shaped cactus for my desk and call it Dick. CBT for OCD 245 they have suggested. While it is partly a brain-storming exercise, it serves an important function: Considering possibilities is in itself exposure Writing them down facilitates repeated exposure. Outcomes from agreeing to complete anti-OCD tasks can be surprising, for example, inability to eat a sandwich that had been placed on a picture of raw chicken which they had purposely printed moments earlier. Such difficulties indicate further need for discussion of the nature of thoughts; that is, thoughts about danger are not the same as actual danger. Are We Nearly There Yet? Throughout therapy, the concept of exposure is maintained as an ongoing process, that is, a series of steps towards a goal. The size of the steps taken can vary. Of course, if only smaller steps are taken, change will take longer, but it also means there is always something the person can do to take them in the right direction. A dialogue between therapist and patient is presented below. What Would You Do? Patient: Therapist: Patient: Therapist: Patient: I couldn’t imagine actually sitting on the seat in a café toilet! If that seems a bit too challenging at the moment, what could you do that would move you in the right direction? Well, I’m not sure . . . it’s just really hard. Maybe I could hover, or put some tissue on the seat? That sounds like a good compromise. Of course, if you’re able to just sit on it, that’s great. But if not, at least you’d still be using a public loo. It would be brilliant if I could do that. At the moment I can’t go out for more than a short time because I’m petrified I’ll need a wee Yet the goal of living life free from OCD does not have a clearly defined end. Earlier in this chapter, therapy was likened to going to a slimming club. To continue with this analogy would be to describe the process as a diet for life – hardly appealing! The following is a more palatable parallel. You join the gym because you would like to lose weight and get fitter. It isn’t always enjoyable – it’s often really hard work, it makes you hot, sweaty, and aching. Some days you’re slower on the treadmill than others. But you keep going because you accept that is what you need to do to keep trim and stay fit. When you’re feeling fitter and looking trimmer, would you stop going and stay at home watching TV whilst eating crisps and chocolate? 246 Elizabeth A. Forrester Maintaining Change and Preventing Relapse A therapy blueprint is generated over the last couple of sessions to summarize key learning points. It includes an example of the formulation, initial beliefs along with the less threatening alternative view of the problem, and a brief account of behavioral changes along with what the client learned. It includes what they need to do to maintain progress, how to detect signs of relapse, and how to deal with it. A copy of the blueprint is presented in Appendix 12.2. Further guidance can be found in Forrester (2015). OCD ‘Rules’ are shown in Appendix 12.3. Looking at the Problem from the Other Side of Therapy We’ll always have worries. To be human is to feel anxious sometimes. Some thoughts will always be horrible, scary, unpleasant. These thoughts are more likely to keep coming back if I try not to have them. It’s fine to feel anxious. We don’t need to ‘fix’ anxiety for it to go away. Coping doesn’t necessarily feel great. Confidence comes from doing things differently despite how I feel. The world may be a dirty and dangerous place, but it doesn’t matter as much as I used to think If I’m willing to accept doubts, worries, and discomfort, I can live my life how I please. Summary and Conclusion There is not just one truth but many. Theories abound over how contamination concerns develop, the role of disgust, factors that lead to prolonged checking, and so on. Research seeks to simplify, but in clinical practice we encounter multifaceted presentations; thus, the breadth of research findings can seem overwhelming. While theory should inform practice and provide a general direction, it should not constrain it. Therapists (like their patients) should avoid becoming absorbed in finding The Way. Inclusion of third wave therapy techniques allows the effective therapist to hold many thoughts (and theories) lightly. It allows us to hover above such details to achieve an overarching view of OCD, that is, that too much importance and attention are given to thoughts and feelings, and that behavior change is possible in their presence. The emphasis on change as a process is powerful: keep on living until you feel alive is a pithy adage, in the absence of continual checking of course. This chapter explored what is required for exposure to be really effective, why we should redefine goals and success, and how to utilize creativity and playfulness to help clients free themselves from the grip of OCD as part of evidencebased practice. CBT for OCD FURTHER READING FOR THERAPISTS Bream, V., Challacombe, F., Palmer, A., & Salkovskis, P. (2017). Cognitive behaviour therapy for OCD. Oxford University Press. van Niekerk, J. (2018). A clinician’s guide to OCD. New Harbinger Publications. FURTHER READING FOR PATIENTS Challacombe, F., Salkovskis, P. M., & Oldfield, V. B. (2011). Break free from OCD: Overcoming obsessive compulsive disorder with CBT. Vermilion. Forrester, E (2015). How to deal with OCD. John Murray Learning, Hodder & Stoughton. REFERENCES Abramowitz, J. (2006). Understanding and treating obsessive-compulsive disorder: A cognitive-behavioral approach. Lawrence Erlbaum. Abramowitz, J. S., & Arch, J. J (2014). Strategies for improving long-term outcome in obsessive-compulsive disorder: Insights from learning theory. Cognitive and Behavioral Practice, 21, 20–31. Alcolado, G. M., & Radomsky, A. S. (2016). A novel cognitive intervention for compulsive checking: Targeting maladaptive beliefs about memory. Journal of Behavior Therapy & Experimental Psychiatry, 53, 75–83. https://doi.org/10.1016/j.jbtep.2015.02.009 American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. Binnie, J. (2015). Do you want therapy with that? A critical account of working within IAPT. Mental Health Review Journal, 20(2), 79–83. https://doi.org/10.1108/MHRJ-112014-0044 Bjork, R. A., & Bjork, E. L. (2006). Optimizing treatment and instruction: Implications of a new theory of disuse. In L.-G. Nilsson & N. Ohta (Eds.), Memory and society: Psychological perspectives (pp. 116–140). Psychology Press. Black, S. C., & Niehaus, F. (1980). How safe is ‘too’ safe? IAEA Bulletin, 22(1). Bream, V., Challacombe, F., Palmer, A., & Salkovskis, P. (2017). Cognitive behaviour therapy for OCD. Oxford University Press. Calkins, A. W., Berman, N. C., & Wilhelm, S. (2013). Recent advances in research on cognition and emotion in OCD: A review. Current Psychiatry Reports, 15, 357. https:// doi.org/10.1007/s11920–013-0357-4 Challacombe, F. L., & Salkovskis, P. M. (2011). Intensive cognitive-behavioural treatment for women with post-natal obsessive-compulsive disorder: A consecutive case series. Behaviour Research & Therapy, 49(6–7), 422–426. Coles, M. E., & Ravid, A. (2016). Clinical presentation of not-just right experiences (NJREs) in individuals with OCD: Characteristics and response to treatment. Behaviour Research and Therapy, 87, 182–187. https://doi.org/10.1016/j.brat.2016.09.013 Coughtrey, A. E., Shafran, R., Knibbs, D., & Rachmann, S. (2012). Mental contamination in obsessive-compulsive disorder. Journal of Obsessive-Compulsive and Related Disorders, 1(4), 244–250. Cougle, J. R., & Lee, H.-J. (2014). Pathological and non-pathological features of obsessivecompulsive disorder: Revisiting basic assumptions of cognitive models. Journal of Obsessive-Compulsive and Related Disorders, 3(1), 12–20. https://doi.org/10.1016/j.jocrd .2013.11.002 Craske, M. G., Kircanski, K., Zelikowsky, M., Mystkowski, J., Chowdhury, N., & Baker, A. (2008). Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy, 46(1), 5–27. https://doi.org/10.1016/j.brat.2007.10.003 247 248 Elizabeth A. Forrester Dek, E. C. P., Van den Hout, M. A., Engelhard, I. M., Giele, C. L., & Cath, D. C. (2015). Perseveration causes automisation of checking behaviour in obsessive-compulsive disorder. Behaviour Research & Therapy, 71, 1–9. https://doi.org/10.1016/j.brat.2015.05.005 Fergus, T. A. (2014). Are ‘not just right experiences’ (NJREs) specific to obsessivecompulsive symptoms? Evidence that NJREs span across symptoms of emotional disorders. Journal of Clinical Psychology, 70, 353–363. doi:10.1002/jclp.22034 Foa, E. B., Huppert, J. D., Leiberg, S., Langner, R., Kichic, R., Hajcak, G., & Salkovskis, P. M. (2002). The obsessive-compulsive inventory: Development and validation of a short version. Psychological Assessment, 14(4), 485–496. https://doi.org/10.1037//10403590.14.4.485 Forrester, E (2015). How to deal with OCD. Hodder & Stoughton. (2017). Working with obsessional ruminations in clinical practice. Invited paper. Getting stuck in repetitive negative thoughts: A transdiagnostic phenomenon illuminated from different perspectives: Symposium on Repetitive Negative Thinking (RNT). 30 March. University of Basel. Gillan, C. M., Morein-Zamir, S., Urcelay, G. P., Sule, A., Voon, V., Apergis-Schoute, A. M., Fineberg, N. A., Sahakian, B. J., & Robbins, T. W. (2014). Enhanced avoidance habits in obsessive-compulsive disorder. Biological Psychiatry, 75(8), 631–638. https://doi.org/10 .1016/j.biopsych.2013.02.002 Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., Hill, C. L., Henninger, G. R., Charney, D. S. (1989). The Yale–Brown Obsessive Compulsive Scale: Part I. Development, use, and reliability. Archives of General Psychiatry, 46, 1006–1012. Hayes, S. C., & Hofmann, S. G. (2017). The third wave of cognitive behavioral therapy and the rise of process-based care. World Psychiatry: Official Journal of the World Psychiatric Association (WPA), 16(3), 245–246. doi:10.1002/wps.20442 Johnstone, L. (2018). Psychological formulation as an alternative to psychiatric diagnosis. Journal of Humanistic Psychology, 58(1), 30–46. https://doi.org/10.1177/ 0022167817722230 Jordan, C., Reid, A. M., Guzick, A. G., Simmons, S., & Sulkowski, M. L. (2017). When exposures go right: Effective exposure-based treatment for OCD. Journal of Contemporary Psychotherapy, 47, 31–39. https://doi.org/10.1007/s10879–016-9339-2 Kim, S.-K., McKay, D., Taylor, S., Tolin, D., Olatunji, B., Timpano, K., & Abramowitz, J. (2016). The structure of obsessive-compulsive symptoms and beliefs: A correspondence and bi-plot analysis. Journal of Anxiety Disorders, 38, 79–87. https://doi.org/10.1016/j .janxdis.2016.01.003 Kinderman, P., Read, J., Moncrieff, J., & Bentall, R. P. (2013). Drop the language of disorder. Evidence-Based Mental Health, 16, 2–3. http://dx.doi.org/10.1136/eb-2012-100987 Koch, J., & Exner, C. (2015). Selective attention deficits in obsessive-compulsive disorder: The role of metacognitive processes. Psychiatry Research, 225(3), 550–555. https://doi .org/10.1016/j.psychres.2014.11.049 Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. Levy, H. C., & Radomsky, A. (2016). Are all safety behaviours created equal? A comparison of novel and routinely used safety behaviours in obsessive-compulsive disorder. Cognitive Behaviour Therapy, 45(5), 367–379. https://doi.org/10.1080/16506073.2016.1184712 Ludvik, D., et al. (2015). Effective behavioural strategies for reducing disgust in contamination-related OCD: A review. Clinical Psychology Review, http://dx.doi.org/10 .1016/j.cpr.2015.07.001 Mataix-Cols, D., Rosario-Campos, M. C., & Leckman, J. F. (2005). A multidimensional model of obsessive-compulsive disorder. American Journal of Psychiatry, 162(2), 228–238. CBT for OCD Mathes, B. M., McDermott, K. A., Okey, S. A., Vazquez, A., Harvey, M. J., & Cougle, J. R. (2019). Mental contamination in obsessive-compulsive disorder: Associations with contamination symptoms and treatment response. Behavior Therapy, 50(1), 15–24. McCubbin, R. A., & Sampson, M. J. (2006). The relationship between obsessive-compulsive symptoms and appraisals of emotional states. Journal of Anxiety Disorders, 20(1), 42–57. https://doi.org/10.1016/j.janxdis.2004.11.008 McEvoy, P. M., Watson, H., Watkins, E. R., & Nathan, P. (2013). The relationship between worry, rumination, and comorbidity: Evidence for repetitive negative thinking as a transdiagnostic construct. Journal of Affective Disorders, 151(1), 313–320. https://doi .org/10.1016/j.jad.2013.06.014 Melli, G., Aardema, F., & Moulding, R. (2016). Fear of self and unacceptable thoughts in obsessive-compulsive disorder. Clinical Psychology & Psychotherapy. 23(3), 226–235. https://doi.org/10.1002/cpp.1950 Milosovic, I., & Radomsky, A. S. (2008). Safety behaviour does not necessarily interfere with exposure therapy. Behaviour Research & Therapy, 46(10), 1111–1118. https://doi.org/10 .1016/j.brat.2008.05.011 Norberg, M., Newins, A., Jiang, Y., Xu, J., Forcadell, E., Alberich, C., & Deacon, B. (2018). The scarier the better: Maximizing exposure therapy outcomes for spider fear. Behavioural and Cognitive Psychotherapy, 46(6), 754–760. doi:10.1017/ S1352465818000437 O’Connor, K., Koszegi, N., Aardema, F., van Niekerk, J., & Tallon, A. (2009). An inferencebased approach to treating obsessive-compulsive disorder. Cognitive and Behavioural Practice, 16, 420–429. Oldfield, V., Salkovskis, P. M., & Taylor, T. (2011). Time-intensive cognitive behaviour therapy for obsessive-compulsive disorder: A case series and matched comparison group. British Journal of Clinical Psychology, 50(1), 7–18. Pence, S. L., Sulkowski, M. L., Jordan, C., & Storch, E. A. (2010). When exposures go wrong: Trouble-shooting guidelines for managing difficult scenarios that arise in exposure-based treatment for obsessive-compulsive disorder. American Journal of Psychotherapy, 64(1), 39–53. Rapp, A. M., Bergman, R. L., Piacentini, J., & McGuire, J. F. (2016). Evidence-based assessment of obsessive-compulsive disorder. Journal of Central Nervous System Disease, 8, 13–29. doi:10.4137/JCNSD.S38359 Rector, N. A., Richter, M. A., Katz, D., & Leybman, M. (2019). Does the addition of cognitive therapy to exposure and response prevention for obsessive compulsive disorder enhance clinical efficacy? A randomized controlled trial in a community setting. British Journal of Clinical Psychology, 58(1), 1–18. Riskind, Ayers & Wright (2007). Simulated interpersonal provocation and fears of a loss of impulse control as determinants of aggressive mental intrusions. Journal of Cognitive Psychotherapy, 21, 285–294. doi: 10.1891/088983907782638752 Robinson, L. J., & Freeston, M. H. (2014). Emotion and internal experience in obsessive compulsive disorder: Reviewing the role of alexithymia, anxiety sensitivity and distress tolerance. Clinical Psychology Review, 34(3), 256–271. https://doi.org/10.1016/j.cpr.2014.03 .003 Romero-Sanchiz, P., Nogueira-Arjona, R., Godoy-Ávila, A. Gavino-Lázaro, A., & Freeston, M. H. (2015). Narrow specificity of responsibility and intolerance of uncertainty in obsessive-compulsive behavior and generalized anxiety symptoms. International Journal of Cognitive Therapy, 8(3), 239–257. https://doi.org/10.1521/ijct_2015_8_04 Ruscio, A., Stein, D., Chiu, W., & Kessler, R. (2010). The epidemiology of obsessivecompulsive disorder in the National Comorbidity Survey Replication. Molecular Psychiatry, 15(1), 53–63. https://doi:10.1038/mp.2008.94 249 250 Elizabeth A. Forrester Salkovskis, P. M., Forrester, E., Richards, H. C., & Morrison, N. (1998). The devil is in the detail: Conceptualising and treating obsessional problems. In N. Tarrier, A. Wells, & G. Haddock (Eds.), Treating complex cases: The cognitive behavioural therapy approach (pp. 46–80). Wiley. Salkovskis, P. M., Millar, J., Gregory, J., & Wahl, K. (2017). The termination of checking and the role of just right feelings: A study of obsessional checkers compared with anxious and non-clinical controls. Behavioural and Cognitive Psychotherapy, 45(2), 139–155. doi:10.1017/S135246581600031X Salkovskis, P. M., Wroe, A., Gledhill, A., Morrison, N., Forrester, E., Richards, H. C., Reynolds, M., & Thorpe, S. (2000). Responsibility attitudes and interpretations are characteristic of obsessive-compulsive disorder. Behaviour Research & Therapy, 38(4), 347–372. https://doi.org/10.1016/S0005–7967(99)00071-6 Seli, P., Risko, E. F., Purdon, C., & Smilek, D. (2017). Intrusive thoughts: Linking spontaneous mind-wandering and OCD symptomatology. Psychological Research, 81, 392. https://doi.org/10.1007/s00426–016-0756-3 Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166, 1092–1097. Strauss, C., Lea, L., Hayward, M., Forrester, E., Leeuwerik, T., Jones, A., & Rosten, C. (2018). Mindfulness-based exposure and response prevention for obsessive compulsive disorder: Findings from a pilot randomised controlled trial. Journal of Anxiety Disorders, 57, 39–47. https://doi.org/10.1016/j.janxdis.2018.04.007 Thorpe, S. J., Barnett, J., Friend, K., & Nottingham, K. (2011). The mediating roles of disgust sensitivity and danger expectancy in relation to hand washing behaviour. Behavioural and Cognitive Psychotherapy, 39(2), 175–190. Toffolo, M. B. J, Van den Hout, M. A., Radomsky, A. S., & Engelhard, I. M. (2016). Check, check, double check: Investigating memory deterioration within multiple sessions of repeated checking. Journal of Behavior Therapy & Experimental Psychiatry, 53, 59–67. https://doi.org/10.1016/j.jbtep.2015.09.001 Twohig, M. P., Abramowitz, J. S., Bluett, E. J., Fabricant, L. E., Jacoby, R. J., Morrison, K. L., Reuman, L., & Smith, B. M. (2015). Exposure therapy for OCD from an acceptance and commitment therapy (ACT) framework. Journal of Obsessive-Compulsive and Related Disorders, 6, 167–173. https://doi.org/10.1016/j.jocrd.2014.12.007. van den Hout, M. A., Reininghaus, J. K., van der Stap, D., & Engelhard, I. M. (2012). Why safety behaviour may not be that bad in the treatment of anxiety disorders: The commitment to future exposures. Psicoterapia Cognitiva e Comportamentale, monograph supplement, 111–126. van Niekerk, J. (2018). A clinician’s guide to OCD. New Harbinger Publications. Wahl, K., Huelle, J. O., Zurowski, B., & Kordon, A. (2013). Managing obsessive thoughts during brief exposure: An experimental study comparing mindfulness-based strategies and distraction in obsessive-compulsive disorder. Cognitive Therapy and Research, 37, 752. https://doi.org/10.1007/s10608–012-9503-2 Wahl, K., Schönfeld, S., Hissbach, J., Küsel, S., Zurowski, B., Moritz, S., Hohagen, F., & Kordon, A. (2011). Differences and similarities between obsessive and ruminative thoughts in obsessive-compulsive and depressed patients: A comparative study. Journal of Behaviour Therapy & Experimental Psychiatry, 42(4), 454–461. https://doi .org/10.1016/j.jbtep.2011.03.002 Waller, G. (2009). Evidence-based treatment and therapist drift. Behaviour Research and Therapy, 47, 119–127. Watkins, E. R., & Nolen-Hoeksema, S. (2014). A habit–goal framework of depressive rumination. Journal of Abnormal Psychology, 123(1), 24–34. http://dx.doi.org/10.1037/ a0035540 CBT for OCD Wells, A. (2009). Metacognitive therapy for anxiety and depression. Guilford. Wells, A., & Cartwright-Hatton, S. (2004). A short form of the metacognitions questionnaire: Properties of the MCQ-30. Behaviour Research and Therapy, 42(4), 385–396. https://doi .org/10.1016/S0005-7967(03)00147-5 Wells, A., Gwilliam, P., & Cartwright-Hatton, S. (2001). The Thought Fusion Instrument. Unpublished self-report scale, University of Manchester, UK. Welz, A., Reinhard, I., Alpers, G. W. & Kuehner, C. (2018). Happy thoughts: Mind wandering affects mood in daily life. Mindfulness, 9, 332. https://doi.org/10.1007/ s12671–017-0778-y Wootton, B. M., Diefenbach, G. J., Bragdon, L. B., Steketee, G., Frost, R. O., & Tolin, D. F. (2015). A contemporary psychometric evaluation of the Obsessive Compulsive Inventory-Revised (OCI-R). Psychological Assessment, 27(3), 874–882. doi:10.1037/ pas0000075 251 13 Obsessive Compulsive Disorder: Treating Obsessions and Associated Behavioral Responses Gillian M. Alcolado Background Theory and Research Researchers and clinicians once considered “pure” obsessions difficult to treat because they did not necessarily have associated overt compulsions (see Clark, 2000, for a review). These obsessions are repugnant in nature and are highly distressing to the sufferer as they run contrary to personal values (e.g., aggressive, blasphemous, sexual, or amoral thoughts) (Rachman, 1997). Thankfully, experts now recognize that obsessions can be treated (for a review, see Shafran et al., 2013). This is particularly due to the development of cognitive therapy (CT) for beliefs regarding obsessions (e.g., Rachman, 2003) and because of the recognition that there are behavioral responses to these intrusive thoughts (e.g., avoidance behavior, neutralization attempts; Rachman, 1997). The latter can be targeted effectively through cognitive or traditional exposure and response prevention (ERP) techniques (e.g., Clark, 2004). This chapter will cover both CT and ERP for treating obsessions and their behavioral sequelae and will therefore take a cognitive behavioral therapy (CBT) approach. Definitions The terms “intrusive thoughts” and “obsessions” will be used throughout. These words can be used interchangeably with clients once they have been socialized to the treatment language and model. When clinicians explain how obsessions develop, however (which will form an integral part of the psychoeducation; see below), they must make the following important difference clear: most people experience intrusive thoughts from time to time (as first demonstrated by Rachman & de Silva, 1978). It is only once the thoughts become frequent, distressing, and impairing that they become clinically significant, and are therefore called obsessions (American Psychiatric Association, 2013). Universality of Intrusive Thoughts Intrusive thoughts are very common in the general population. In a sample of nonclinical individuals, the overwhelming majority of participants reported having 252 Obsessive-Compulsive Disorder experienced an intrusive thought (80%; Rachman & de Silva, 1978). Researchers replicated this finding in a worldwide representative sample, where 94% of nonclinical participants endorsed having had at least one unwanted intrusive thought in the previous three months (Radomsky et al., 2014). Research findings from several studies (e.g., Moulding et al., 2014; Rowa & Purdon, 2003) support the theory (Rachman, 1997) that it is not the experience, but the interpretation of the intrusion that causes it to become an obsession. From Intrusion to Obsession According to Rachman’s (1997, 1998) cognitive theory of obsessions, intrusive thoughts lead to obsession via the “catastrophic misinterpretation” of what it means to have these thoughts. This misinterpretation is the target for treatment, rather than the obsessional content itself (see Clark, 2004; Rachman, 2003). Individuals who make this type of misinterpretation are understandably highly vigilant for the potential presence of such thoughts. They also often develop rituals aimed at reducing and/or neutralizing the thought and associated distress. In clients with obsessions, these thoughts are therefore occurring much more frequently, repeatedly, and are accompanied by a great deal of anxiety. By contrast, a person who is not suffering from OCD makes no negative interpretation. These intrusive thoughts are therefore more likely be fleeting, largely unnoticed, and tend not to cause suffering (Rachman, 1997). As such, no ritual to neutralize the thought is needed (Rachman, 1997). Research aligns with these tenets. In a recent worldwide study of nonclinical individuals, the intrusive thoughts that were rated as most highly distressing were the ones that occurred most frequently, were interpreted most negatively, and were most strongly attempted to be controlled (Moulding et al., 2014). Hence, the person who is vigilant for the recurrence of these thoughts because a catastrophic misinterpretation has been made, and engages in a behavior to obtain relief from any associated anxiety or distress, will be more likely to turn to the same strategies the next time the thought recurs (Rachman, 1997). These behaviors may include avoidance of objects/environments that trigger the thoughts or attempts to stop or cancel the thoughts (“neutralizing” their effect) through behavioral or mental tactics (Rachman, 1997). This type of individual is therefore then more likely to develop a problem with obsessions over time (Rachman, 1997). Types of Misinterpretations There are various ways in which individuals with OCD may catastrophically interpret their intrusive thoughts, and all are potential targets for treatment (see below). Rachman described these beliefs as typically fitting into one of these categories, mainly, the fears that the thought means one is “immoral, evil, dangerous, insane, or . . . a combination of these qualities” (Rachman, 2003, p. 4). In the subsequent theoretical and research literature, these types of beliefs have been elaborated on and expanded. The belief that having a thought means something about one’s true 253 254 Gillian M. Alcolado values or that the thought is more likely to “come true” is a type of thought–action fusion (Rachman & Shafran, 1999). Another common (and erroneous) belief is that thoughts are controllable and that inability to control thoughts is a sign one might lose control or go crazy (Clark & Purdon, 1993). Indeed, the Obsessive Compulsive Cognitions Working Group (OCCWG) has developed three factors of belief domains thought to be central to OCD, one of which is “importance and control over thoughts.” Another cognitive theory of obsessive thoughts is the inferencebased theory (O’Connor & Robillard, 1999). It postulates that individuals with obsessions are bothered by them because they are making incorrect logic inferences regarding the meaning of the presence of these thoughts (O’Connor & Robillard, 1999). An entire treatment has been developed that focuses solely on this type of misinterpretation and has been shown to be effective (O’Connor et al., 2005). Interested readers are directed to its treatment manual (O’Connor & Aardema, 2011). Evidence-Based Interventions for Obsessions: ERP and CBT Exposure and response prevention (ERP) was the first successful psychological intervention for OCD (Meyer, 1966). The focus is behavioral: the client gradually engages with situations that would normally prompt compulsive rituals, but practices refraining from doing so (see Foa et al., 2012, for the definitive ERP practitioner treatment manual). ERP has long been considered the gold standard of psychological interventions for OCD (Chambless et al., 1998). Recent treatment research examining outcome by symptom dimension, however, has shown that primary obsessions are less responsive to ERP than are the more behaviorally based symptom dimensions (Williams et al., 2014). In interventions with a heavy ERP focus but that contain some mixed CBT techniques, researchers have also found that in individuals with both obsessions and compulsions, their obsessive symptoms responded less well to intervention (Chase et al., 2015; Farrell et al., 2016). Encouragingly, however, combined approaches that incorporate cognitive rationale and challenges to cognitive beliefs in conjunction with ERP techniques have exhibited good outcomes for individuals with primary obsessions (Freeston et al., 1997; O’Connor et al., 2005). Evidence-Based Interventions for Obsessions: CT The first successful case study of cognitive therapy (CT) for primary obsessions was published in 1994 (Van Oppen, 1994). A woman with harming obsessions was treated with cognitive interventions targeting her overestimation of negative consequences as well as the personal significance of what her thoughts meant. She made clinically significant change, which was maintained at follow-up. A case series study targeting the obsessive belief domains outlined by OCCWG (2005) found similarly promising results (Freeston et al., 2001). In 2010, Whittal et al. conducted a randomized controlled trial (RCT), using Rachman’s (2003) cognitive therapy protocol Obsessive-Compulsive Disorder for obsessions. They found robust decreases in symptoms with large effect sizes that were stable at 12-month follow-up. Cognitive therapy seems to have a superior effect on obsessions regarding unwanted intrusive thoughts (i.e., the repugnant obsessions that are the focus of this chapter) than for obsessions relating to traditional compulsions (e.g., contamination obsessions related to washing behavior; Belloch et al., 2010), suggesting it is particularly appropriate for use in this population. Why Evidence-Based Treatments Work All psychological interventions for OCD generally exhibit the same trajectory of treatment change, whereby the behavioral symptoms change before cognitions (Anholt et al., 2008). A rigorous outcome trial on exposure and response prevention (ERP) for OCD suggested that cognitive change is not the mechanism of change (Su et al., 2016). In CBT for OCD, by contrast, it appears that change in cognition is an important factor, although the direction of that relationship might not be as straightforward as hypothesized (e.g., Andersson et al., 2015). The same has been found for CBT specifically for obsessions (Woody et al., 2011). A review by Polman et al. (2010) concluded that there is evidence that both cognitive change and behavioral change can lead to improvement and that there is bidirectionality between them. The authors recommended that as process and mechanism research in OCD outcomes is still in its infancy, it should be conducted separately by specific symptom dimension in order to best understand the mechanisms of change (Polman et al., 2010). Despite the lack of such research, ERP and cognitive therapy (CT) are both effective (e.g., Chambless et al., 1998; Woody et al., 2011). Therefore, these approaches continue to be used to target obsessions (e.g., Clark, 2004; Rachman, 2003), even though the mechanisms remain unknown. Assessment of Obsessions and Associated Behaviors The clinician will first determine the nature, frequency, and triggers for the obsessions. It is also important to ascertain the appraisals that the sufferer is making about the intrusive thoughts and any underlying beliefs that are affecting these interpretations. Additionally, any neutralizing, avoidance, and/or reassuranceseeking behaviors need to be identified, as they maintain the obsessions. Together, this information helps guide the case formulation and provides points of intervention. Assessment of Symptoms Structured Interviews The Yale–Brown Obsessive Compulsive Scale (Y-BOCS; Goodman et al., 1989b) is the gold standard structured interview for assessing OCD (Kim et al., 1989). It exhibits good internal consistency and inter-rater reliability (Goodman et al., 1989b) 255 256 Gillian M. Alcolado as well as validity (Goodman et al., 1989a). It contains a checklist with multiple examples of aggressive, sexual, and religious obsessions that can be used as probes for the clinician. This is particularly helpful as clients may not be as comfortable spontaneously reporting repugnant obsessions as compared with more benign compulsions. A psychometrically sound self-report version of the Y-BOCS has also been developed (Steketee et al., 1996). Alternatively, Rachman’s (2003) treatment manual provides a semi-structured interview for assessing obsessions. Although not validated, it is comprehensive and highly clinically relevant. If OCD symptoms are to be assessed in the context of other disorders, the Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5; Brown & Barlow, 2014), a semi-structured interview, includes in its section on OCD a useful checklist of possible obsessions and compulsions. It does not yet have published reliability and validity statistics, but its predecessor, the ADIS for DSM-IV, on which it is modeled, has strong psychometric properties (Brown et al., 2001). Self-Report Measures A number of questionnaires exist that assess OCD symptomatology, with subscales pertaining to obsessions. These tools include the Vancouver Obsessional Compulsive Inventory (VOCI; Thordarson et al., 2004), which has an obsessions subscale (12 items), some of which are specific to repugnant obsessional domains (e.g., harm, sex, religion). A shorter measure, the Obsessive-Compulsive Inventory – Revised (OCI-R; Foa et al., 2002) contains three items pertaining to obsessive thoughts, although without specifying type. The Dimensional Obsessive Compulsive Scale (DOCS; Abramowitz et al., 2010, measure appended to the article) contains two subscales that address obsessions, one relating to harm (although this subscale also contains items relating to checking compulsions) and the other to unacceptable thoughts. Another group has since amended the DOCS to include a supplemental five-item scale that assesses sexually intrusive thoughts (Wetterneck et al., 2015; subscale appended in the article) that would be highly relevant for the clinician working with this type of obsession. For a recent and comprehensive review of all OCD symptom interviews, measures, and their psychometric properties, see Rapp et al. (2016). Unstructured Interviews Obsessions can also be explored using open-ended questions as part of a nonstructured diagnostic intake interview. First, information on presence and type of intrusion can be collected. These would be intrusive thoughts of aggression, sex, morality, and religion. This can be asked in a manner such as, “Have you ever had unwanted thoughts of harming someone even though you don’t want to?” and “Have you ever had unwanted intrusive thoughts that go against your religious beliefs, sexual preferences, or moral values?” If these statements are endorsed, it is important to always follow up by asking the client for examples, as it will be the clinician who ultimately makes the determination whether a thought is an obsession or not. For example, having the desire to “throttle” someone during an argument is Obsessive-Compulsive Disorder not typically an obsession, as this type of thought tends to be mood-congruent and nonintrusive. A more likely example of an obsession would be an intrusive thought or image of harming a loved one while holding a sharp implement. Similarly, feeling guilty about having sexual fantasies with someone outside a partnership would not typically fit the criteria for an unwanted intrusive thought. A more likely example of an obsession would be an intrusive thought or image of engaging in a sexual act with an inappropriate or undesirable figure (e.g., a stranger, family member). In either case, however, determining the intrusiveness, interpretation, and distress associated with the thought will clarify whether it is an obsession or some other type of negative thought process. It is important to include unstructured questions regarding neutralizing behaviors, as they are not necessarily well captured otherwise. The clinician can ask in an open-ended manner: “How do you respond to those thoughts?” and/or “Is there anything you do to try to make the thoughts go away?” In order to determine whether the action they are describing is indeed a neutralizing strategy, it is helpful to ascertain the goal of said behavior. For example, “What are you trying to accomplish when you engage in that behavior?” If the client is not sure what is meant, clarify by asking whether they are trying to neutralize/cancel the thought, get rid of the thought, or stop the thought. It is also very clinically useful to directly ask regarding the presence of behaviors associated with the obsessions, such as avoidance and reassurance seeking: “Do you ever avoid anything out of fear of having these thoughts?” and “Do you ever seek reassurance from others about what it means that you have these thoughts?” Assessment of Beliefs Structured Interview Once symptoms are understood, the underlying beliefs must be probed in order to complete the clinical formulation and understand the client. There are currently no validated structured clinical interviews that assess these beliefs. However, for the clinician wanting some practical guidelines for this type of questioning, Rachman’s (2003) interview is useful. Self-Report Measures The Interpretation of Intrusions Inventory (III; OCCWG, 2005) focuses solely on beliefs about intrusive thoughts. It contains 31 items that assess beliefs about control of thoughts, importance of thoughts, and responsibility. These items load onto a single factor, and the measure has strong psychometric properties (OCCWG, 2005). The Obsessive Beliefs Questionnaire (OBQ-44) is a validated 44-item questionnaire for which the “importance and control over thoughts” subscale would be relevant to this population (OCCWG, 2005; the questionnaire is appended within the research article). This subscale includes items such as “Having nasty thoughts means I am a terrible person” and “If I have aggressive thoughts or impulses about my loved ones, this means I may secretly want to hurt them” (OCCWG, 2005). 257 258 Gillian M. Alcolado The Responsibility Interpretations Questionnaire (RIQ; Salkovskis et al., 2000) assesses beliefs associated with whatever is the most commonly occurring obsession they experienced within the last two weeks. To make it relevant to the assessment of “pure” obsessions, the clinician directs the client to fill out the questionnaire thinking about those unacceptable blasphemous thoughts. Items are highly pertinent to obsessional treatment, as they include statements such as “I must regain control of my thoughts” and “Because these thoughts come from my own mind I must want them to happen.” This questionnaire also asks about the degree to which an individual endorses a more adaptive interpretation, such as “There’s nothing wrong with letting such thoughts come and go naturally” and “Thoughts cannot make things happen.” This measure has good psychometric properties and can be found in the appendix of the research article (Salkovskis et al., 2000). Shafran et al. (1996) developed a measure of one domain of catastrophic misinterpretation, thought–action fusion (TAF). The TAF scale exhibits sound psychometric properties and is comprised of three subscales: (1) moral TAF (e.g., “Having a blasphemous thought is almost as sinful to me as having a blasphemous action”), (2) likelihood TAF for self (e.g., “If I think of myself in a car accident, this increases the risk that I will have a car accident”), and (3) likelihood of TAF for others (e.g., “If I think of a relative/friend falling ill, this increases the risk that they will fall ill”) (Shafran et al., 1996). The items are appended in the article, and the authors recommend the TAF as a useful starting point for discussion rather than one strictly to be used to monitor strict score changes (Shafran et al., 1996). Finally, the Personal Significance Scale (PSS; Rachman, 2003) can be completed by clients in order to assist them in understanding their beliefs about their intrusions. In order to tailor this measure to the assessment of relevant obsessions, ask the clients to think of their blasphemous thoughts when answering the items. A copy of this measure, which has yet to be validated, can be found in Rachman’s (2003) manual. Unstructured Interview To ascertain the beliefs that underlie the distress associated with the obsessions, one can ask, “What is most upsetting to you about the fact that you are experiencing this thought?” Follow-up questions can be more direct as needed. These may include queries such as “What do you think the thought means about you?” and “What do you fear would happen if you could not stop the thought?” Case Formulation An individualized case formulation guides the intervention. The clinician develops this using the information from the assessment and solidifies it through discussion with the client. As with any CBT model, predisposing factors that make an individual vulnerable to having obsessions are considered. These include genetics, brain chemistry, environment, learning, and/or life stressors. Core beliefs predispose an Obsessive-Compulsive Disorder individual toward making catastrophic misinterpretations of intrusions in the moment. Framework for Understanding Obsessions The important distinguishing factor in the case formulation of the obsession is that the obsession is considered not to be the automatic thought but instead a trigger for such thoughts. Thus, the clinician does not target the obsession itself in treatment, but rather the client’s interpretation of the obsession. The maintenance factors of the model (i.e., thoughts, emotions, behaviors) are the responses to the presence of the obsession or a stimulus that elicits the obsession (the trigger). The catastrophic misinterpretation of the intrusive thought as dangerous and personally significant in some way and/or a belief about what such thoughts mean (e.g., that they should be controllable and/or should not occur) is the automatic thought. This interpretation of the obsession leads to an increase in the emotion of anxiety, physiological arousal, and a behavioral response aimed at neutralizing the thought and decreasing the anxiety. If the behavior is successful in decreasing the anxiety, it becomes reinforced and more likely to occur the next time the client has the obsessive thought. Specific to a model of obsessions, included in the behavioral component of the model are any physical or mental neutralizing rituals and/or reassurance seeking. In the long term, the behavioral response will likely also include any avoidance of triggers as a strategy to prevent the cycle from occurring. Case Vignette. Elena is a 30-year-old married woman who works in administration. She had a Catholic upbringing and an anxious mother. After the birth of her daughter, she began experiencing unwanted intrusive thoughts of harming her. She presented reporting difficulty caring for her independently out of fear of “going crazy” and acting on these harm thoughts. An intake assessment was conducted using a semi-structured interview to assess symptom domains, as well as self-report questionnaires and unstructured clinical interviewing for further clarification of her obsessions. Developing the Model: Vulnerability Factors Clients often want to understand “where the anxiety came from.” It is helpful to incorporate this information into the broader case formulation to satisfy this desire and to demonstrate that, regardless of the origin of the anxiety (or whether one can even ascertain such a root cause, which is not always possible), the maintenance factors can still be targeted to successfully treat the problem (see below). Elena may have a genetic predisposition to OCD as her mother also struggled with anxiety. Elena confirmed the clinician’s guess that modeling of OCD behaviors by her mother was observed from a young age. Further, Elena’s religious background influenced her belief about the immorality of “impure thoughts,” which contributed to the development of some of her core beliefs. These beliefs were assessed via the unstructured clinical interview and self-report measures. The TAF was administered, as it was suspected Elena held some TAF beliefs. It revealed that 259 260 Gillian M. Alcolado she felt that having a “bad” thought is as bad as committing an action, and also that having a thought means it is more likely to occur “in real life.” Her scores on the OBQ were elevated, in particular, on the importance and control of thoughts subscale, demonstrating that Elena also felt that she should have control over her thoughts. The life stressor that catalyzed the onset of the current episode of OCD was identifiable in her case as the birth of her child. Developing the Model: Maintenance Factors Details of the OCD symptoms, including obsessions and related behaviors that Elena experiences, are gathered through the tools described above, including the self-report measures and the semi-structured and unstructured interviews. She exhibited elevated scores on the OCI-R obsession items. Further open-ended follow-up questions were asked to determine her understanding of the meaning of the intrusive thoughts, what she did in response to these thoughts, and how effective these strategies were. In Elena’s case, her obsessive thoughts include harming her daughter by dropping her or stabbing her with sharp objects. Elena had no desire to harm her child, but did not know how to reconcile this with her experience of having these thoughts. She responded to the thought by putting distance between herself and her child as well as between herself and any potentially dangerous objects (e.g., scissors, knives). She tried to avoid handling such objects in front of her daughter, and preferred to have help with her when she could so that a second person could observe their interactions and “keep her daughter safe.” She also engaged in several rituals, including praying over and over again to protect her child as well as trying to mentally replace the thought with a “loving and safe” thought. She recognized these rituals as unnecessary, but she could not resist engaging in them, as completing the rituals resulted in a temporary decrease in anxiety. Socialization to the Model: Specific Techniques Once the CBT model above is explained, the therapist provides an explanation of OCD. The clinician can begin by asking “Who experiences intrusive thoughts?” The client may not be sure, but through discussion with the clinician will come to understand that all individuals experience intrusive thoughts. Some clients may appreciate learning that there is a wealth of research to support this assertion. Having the client review a handout listing typical intrusive thoughts endorsed by the general population can also be very powerful (see example in Rachman, 2003, extracted from Rachman & de Silva, 1978). The clinician can then ask the client to guess what kind of people listed these thoughts. The client is typically surprised and relieved to know that individuals without OCD experience these thoughts. The clinician may then ask the client in Socratic fashion, “So, if everyone has these thoughts but not everyone has OCD, what is the difference?” This can lead to a productive discussion about the difficulty in OCD being the interpretation of the obsessive thought, not the obsessive thought itself. Individuals without OCD also Obsessive-Compulsive Disorder have intrusive thoughts, but they interpret them as meaningless noise. Minimal anxiety is provoked, and therefore no ritual is necessary. The goal of examining the client’s thoughts and behavioral processes is to help them understand this type of reaction to the intrusion and subsequent lack of necessary behavior that is seen in the general population. A clear explanation of the CBT model of obsessions is a crucial step in engaging the client in treatment. The other important salient point to make at treatment outset is that the goal is not to stop the thoughts. This can be initially disappointing for the client. The therapist can also provide the more hopeful caveat that as clients become less distressed by the thoughts over time (as a result of the treatment) they will likely find that the intensity and frequency of the obsessional thoughts also gradually declines. Socialization to the Model: Addressing Resistance If the client is reluctant to adopt this model, a couple of techniques can be used. The clinician can start with Socratic questioning and discussion regarding how well efforts to suppress and eliminate these thoughts have gone so far. Many clients readily acknowledge that their existing strategies have not been effective. Second, evidence from studies on the ubiquity of intrusive thoughts in the general population can be summarized, and, as suggested above, a handout listing common intrusive thoughts that people without OCD endorse may also be helpful. Finally, the clinician can conduct the “white bear” behavioral experiment (see Wilhelm & Steketee, 2006, for more details) to further demonstrate that trying not to have certain thoughts has a paradoxical effect, and that is what we are trying to avoid in this treatment. The white bear experiment is typically done without explaining the purpose ahead of time. The client is asked to spend 30–60 seconds trying to think of the white bear as much as they can. The clinician times them and gets the client to count how many times they think of the white bear. Then this experience is discussed. The client often will find it was hard to stay concentrated on the white bear. Then the opposite task is assigned for another 30–60 seconds. The client is instructed that no matter what, they cannot think of a white bear, and again instructed to count how many times they think of the white bear. A debrief follows again. This exercise demonstrates to the client how trying not to have obsessive thoughts is likely achieving exactly the opposite result. Thus, the goal of treatment will be not to suppress the thoughts but to learn to respond to them differently. Therapy Overview Treatment consists of three phases: (1) psychoeducation, (2) therapeutic techniques (including cognitive restructuring, ERP, and behavioral experiments), and (3) relapse prevention. Most of the sessions are concentrated on phase 2. The number of sessions will vary based on the number of obsessive belief domains to work on. 261 262 Gillian M. Alcolado A minimum of 12–16 sessions is typical, with 1–2 sessions for phase 1, 8–12 sessions for phase 2, and 1–2 sessions for phase 3. During phase 2, clients may prefer to begin with cognitive interventions and/or behavioral experiments, as they may be less anxiety-producing than ERP. Furthermore, alternative interpretations generated from these exercises can be used as coping statements during exposures to increase engagement with them. Alternatively, if clients prefer to start with ERP to gain control over some of their behaviors and avoidance, treatment can begin here and cognitive elements can be woven into the intervention if and when the client struggles or plateaus. Phase 1: Psychoeducation Definitions of CBT and OCD are provided. Socialization to the model (described above) also occurs here. When discussing the role of behavioral responses to obsessions, it is important to probe for ambivalence that clients might have. Emphasize that this is understandable, given that in the short term the anxiety and the relief they produce is so high. A good between-session exercise for these introductory sessions may include a pro/con list of engaging in therapy. The client can refer to this list in the future if ambivalence resurfaces. Have the client monitor their symptoms for one week. These would include obsessions, interpretations, and associated rituals. This provides a more exact picture of what the pertinent obsessions are and which behaviors to work on. It often also reveals some symptoms that have been overlooked. Rachman (2003) has a sample daily record form for the frequency and distress associated with an obsession. Foa et al. (2012) have a form for monitoring rituals. Either may be used or a hybrid that captures both elements (see Wilhelm & Steketee, 2006), depending on the focus for that particular week. Measuring Outcome A weekly monitoring form (see above) tracks symptom change in the most personalized fashion. Given that the goal is not for the obsessions to decrease, it is important to include the intensity and distress associated with the occurrence of the intrusion. Avoidance and mental ritualizing should be explicitly tracked. The obsessions subscale from the OCI-R (Foa et al., 2002) is a general and brief alternative, although the information gleaned from this will not be as nuanced. The Personal Significance Scale (Rachman, 2003) tracks a range of the beliefs being targeted. Phase 2: Cognitive Interventions and Behavioral Experiments Choose a relevant automatic thought to begin with based on the formulation and/or monitoring form. If desired, a thought record to modify beliefs about thoughts (not the obsessive content itself ) can be used (see Wilhelm & Steketee, 2006). The behavioral experiment approach was originated by Beck et al., (1979). For more Obsessive-Compulsive Disorder examples of behavioral experiments in the context of OCD treatment, refer to Clark (2004) or Rachman (2003). Common interventions relevant to obsessions are discussed below. To target the likelihood of TAF (i.e., that the occurrence of a thought means it is more likely to happen in reality), a behavioral experiment can be designed to test this belief. The client can begin by purposefully thinking about a good thing happening to the therapist (e.g., winning the lottery) and check in to see if it happens. They can then progress to more negative thoughts (e.g., thinking of the therapist tripping while walking, getting parking tickets). The therapist may model the safety of this behavior by also engaging in the task. A behavioral experiment can be conducted in-session where both write out “I wish (loved one) would get in a car accident.” The take-home message is that although it might feel unpleasant to have such thoughts, they do not actually influence reality. If the person is still struggling with such thoughts, then one can move on to ERP where the target is to not respond to thoughts that trigger likelihood TAF beliefs (see below). Morality TAF (i.e., that having a bad thought is as bad as doing a bad thing) can be targeted through a cognitive exercise. The goal is to shift how evil the client concludes they are for having such thoughts. The client is asked to consider who is the worst person and the best person they can think of (typical anchors are Hitler and Mother Teresa). The client is then encouraged to add other people along the continuum, for example, murderers, rapists, but also more ambiguous examples such as individuals who cheat, lie, evade taxes, don’t pay library fines, and so on. As the last step, the client is asked to consider where they might place someone who has repugnant thoughts that go against their values. This helps the client begin to see how far they are from being a bad person. Relevant ERP exercises to cues that elicit morality TAF could then be designed. Discussion of control over thoughts will likely have been covered through socialization to the model (see above), but if not, the white bear behavioral experiment would be appropriate here. Additionally, clients can be asked to manipulate how much they attempt to control their own intrusions using alternate days of attempting control versus days of not attempting control and tracking how frequent and intense the obsessions are on these days. They will likely find the obsessions are actually much better on days in which they do not attempt any such control. To target beliefs about the importance of thoughts, the discussion from the socialization to the model can be reviewed here as well. A behavioral experiment can be conducted similar to the one for control of thoughts. The client can alternate days on which they attend very closely to the thought, and give it importance, versus attempting to let it go and rate how important the thought actually feels. The client will again likely find that paying less attention to the thoughts will make them feel less important. If the client believes the thought must be true because of their behavioral reaction to it, the following demonstration and discussion can be useful. The clinician shares a story of how they made homemade pasta sauce on the weekend. The clinician and client can then discuss the thoughts (e.g., “I’m hungry”) and physical reactions (e.g., “salivation”) this story caused. The clinician then 263 264 Gillian M. Alcolado reveals the story is false. The point to be discussed is that thoughts (even when not true) can elicit reactions and that this should not be taken as a marker of their importance. Phase 2: Behavioral Interventions (Sessions 3–10) ERP can also be very helpful in addressing obsessions. See Foa et al. (2012) for the definitive guide to this type of work and Grayson (2014) for sample hierarchies. The client generates a list of cues and situations that typically elicit obsessions. They engage with these in planned, controlled circumstances and are prompted to apply response prevention. Response prevention may at first be a brief delay in neutralizing behavior, avoidance, or reassurance seeking. They then may continue to reduce the number of behavioral strategies employed, and continue to refrain from any overt or covert behavioral or mental rituals that would typically neutralize the thought. Clients are encouraged to sit with the intrusion and the subsequent anxiety for as long as planned. This can be accomplished by setting a goal of staying in the exposure either until the anxiety reduces by a certain amount (e.g., subjective anxiety decreasing from 95/100 to 65/100), or for a predetermined length of time (e.g., 20 minutes). When targeting reassurance seeking it might be helpful to have loved ones attend a session (with the client’s permission). They can then be provided with psychoeducation and the best strategies for supporting the client. The clinician will remind the loved one that the client is in the control of how and when they are reducing the behavior. If there are certain catastrophic feared outcomes of the intrusive thought that are not alleviated through the aforementioned techniques, an imaginal exposure exercise may be appropriate. For example, fear of having an intrusion, losing control, and harming loved ones could be targeted in this way. The goal of the imaginal exposure is for the client to have a reduced anxious reaction to that scenario through explicitly confronting it. What often happens is that when clients write out the scenario, they begin to see how unlikely it would be to occur. Phase 3: Relapse Prevention (Sessions 11 and 12) Typical CBT relapse principles apply with this treatment approach to obsessions. Strategies such as coping statements, maintenance ERP exercises, and education on lapses versus relapses are all important. The clinician should ensure that the client recalls that it is not the intrusive thoughts but their interpretation that leads to distress. This same principle (and associated cognitive and behavioral strategies the client has learned) would apply to any new intrusions not targeted in the therapy that become upsetting in the future. ERP exercises would include the continued vigilance for and elimination of mental rituals in response to intrusive thoughts. A lapse would not be the occurrence of an obsession, but a reaction of distress and impairment to its presence. Obsessive-Compulsive Disorder Summary of Key Learning Points Intrusive thoughts are universal; it is misinterpretation of intrusive thoughts that converts them to obsessions. The goal of therapy is not to get rid of the obsessive thoughts but to interpret them more adaptively. Some rituals may be covert (i.e., mental) and must be assessed prior to treatment. Obsessions and related behaviors can be effectively targeted in CBT using cognitive techniques, behavioral experiments, and exposure and response prevention. FURTHER RECOMMENDED READING Clark, D. A. (2003). Cognitive-behavioural therapy for OCD. Guilford. Foa, E. B., Yadin, E., & Lichner, T. K. (2012). Exposure and response (ritual) prevention for obsessive-compulsive disorder: Therapist guide (Treatments that work) (2nd ed.). Oxford University Press. Grayson, J. (2014). Freedom from obsessive-compulsive disorder. Berkley. Rachman, S. (2003). The treatment of obsessions. Oxford University Press. Wilhelm, S., & Steketee, G. S. (2006). Cognitive therapy for obsessive-compulsive disorder: A guide for professionals. New Harbinger. REFERENCES Abramowitz, J. S., Deacon, B. J., Olatunji, B. O., Wheaton, M. G., Berman, N. C., Losardo, D., . . . & Hale, L. R. (2010). Assessment of obsessive-compulsive symptom dimensions: Development and evaluation of the Dimensional Obsessive-Compulsive Scale. Psychological Assessment, 22, 18019–8. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.) (DSM-5). American Psychiatric Association. Andersson, E., Ljotsson, B., Hedman, E., Hesser, H., Enander, J., Kalod, V., . . . & Ruck, C. (2015). Testing the mediating effects of obsessive beliefs in internet-based cognitive behaviour therapy for obsessive-compulsive disorder: Results from a randomized controlled trial. Clinical Psychology and Psychotherapy, 22, 722–732. Anholt, G. E., Kempe, P., de Haan, E., van Oppen, P., Cath, D. C., Smit, J. H., & van Balkom, A. J. L. M. (2008). Cognitive versus behavior therapy: Processes of change in the treatment of obsessive-compulsive disorder. Psychotherapy and Psychosomatics, 77, 38–42. Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of depression. Guilford Press. Belloch, A., Cabedo, E., Carrio, C., & Larsson, C. (2010). Cognitive therapy for autogenous and reactive obsessions: Clinical and cognitive outcomes at post-treatment and 1-year follow-up. Journal of Anxiety Disorders, 24, 573–580. Brown, T. A., & Barlow, D. H. (2014). Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5) – Lifetime Version. Oxford University Press. Brown, T. A., Di Nardo, P. A., Lehman, C. L., & Campbell, L. A. (2001). Reliability of DSMIV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology, 110, 49–58. 265 266 Gillian M. Alcolado Chambless, D. L., Baker, M. J., Baucom, D. H., Beutler, L. E., Calhoun, K. S., CristsChristoph, P., . . . & Woody, S. R. (1998). Update on empirically validated therapies. II. The Clinical Psychologist, 51, 3–16. Chase, T., Wetterneck, C. T., Bartsch, R. A., Leonard, R. C., & Riemann, B. C. (2015). Investigating treatment outcomes across OCD symptom dimensions in a clinical sample of OCD patients. Cognitive Behaviour Therapy, 44, 365–376. Clark, D. A. (2000). Cognitive behavior therapy for obsessions and compulsions: New applications and emerging trends. Journal of Contemporary Psychotherapy, 30, 129–147. (2004). Cognitive-behavioural therapy for OCD. Guilford. Clark, D. A., Abramowitz, J., Alcolado, G. M., Alonso, P., Belloch, A., Bouvard, M., . . . & Wong, W. (2014). Part 3. A question of perspective: The association between intrusive thoughts and obsessionality in 11 countries. Journal of Obsessive-Compulsive and Related Disorders, 3, 292–299. Clark, D. A., & Purdon, C. (1993). New perspectives for a cognitive theory of obsessions. Australian Psychologist, 28, 161–167. Farrell, N. R., Ouimet, A. J., Rowa, K., Soreni, N., Swinson, R. P., & McCabe, R. E. (2016). Who gets better when? An investigation of change patterns in group cognitive behavioral therapy for obsessive-compulsive disorder. Journal of Obsessive Compulsive and Related Disorders, 10, 35–41. Foa, E. B., Huppert, J. D., Leiberg, S., Lagner, R., Kichic, R., Hajcak, G., & Salkovskis, P. M. (2002). The obsessive-compulsive inventory: Development and validation of a short version. Psychological Assessment, 14, 485–495. Foa, E. B., Yadin, E., & Lichner, T. K. (2012). Exposure and response (ritual) prevention for obsessive-compulsive disorder: Therapist guide (Treatments that work) (2nd ed.). Oxford University Press. Freeston, M. H., Ladouceur, R., Gagnon, F., Thibodeau, N., Rhéaume, J., Letarte, H., & Bujold, A. (1997). Cognitive-behavioral treatment of obsessive thoughts: A controlled study. Journal of Consulting and Clinical Psychology, 1997, 405–413. Freeston, M. H., Léger, E., & Ladouceur, R. (2001). Cognitive therapy of obsessive thoughts. Cognitive and Behavioral Practice, 8, 61–78. Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Delgado, P., Heniger, R., et al. (1989a). The Yale–Brown Obsessive Compulsive Scale. II. Validity. Archives of General Psychiatry, 46, 1012–1016. Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleishman, R. L., Hill, C. L., et al. (1989b). The Yale–Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Archives of General Psychiatry, 46, 1006–1011. Grayson, J. (2014). Freedom from obsessive-compulsive disorder. Berkley. Kim, S. W., Dysken, M. W., & Katz, R. (1989). Rating scales for obsessive compulsive disorder. Psychiatric Annals, 9, 74–79. Meyer, V. (1966). Modification of expectations in cases with obsessional rituals. Behaviour Research and Therapy, 4, 273–280. Moulding, R. M., Coles, M. E., Abramowitz, J., Alcolado, G. M., Alonso, P., Belloch, A., . . . & Wong, W. (2014). Part 2. Do we all dislike intrusive thoughts for the same reasons? Links between appraisals, control strategies and intrusions across countries. Journal of Obsessive-Compulsive and Related Disorders, 3, 280–291. Obsessive Compulsive Cognitions Working Group [OCCWG]. (2005). Psychometric validation of the obsessive belief questionnaire and interpretations of intrusions inventory – Part 2: Factor analyses and testing of a brief version. Behaviour Research and Therapy, 43, 1527–1542. O’Connor, K., & Aardema, F. (2011). Clinician’s handbook for obsessive compulsive disorder: Inference based therapy. Wiley-Blackwell. Obsessive-Compulsive Disorder O’Connor, K. P., Aardema, F., Bouthillier, D., Fournier, S., Guay, S., Robillard, S., Pelissier, M. C., . . . & Pitre, D. (2005). Evaluation of an inference-based approach to treating obsessive-compulsive disorder. Cognitive Behaviour Therapy, 34, 148–163. O’Connor, K. P., Freeston, M. H., Gareau, D., Careau, Y., Dufour, M. J., Aardema, F., & Todorov, C. (2005). Group versus individual treatment in obsessions without compulsions. Clinical Psychology and Psychotherapy, 12, 87–96. O’Connor, K. P., Koszegi, N., Aardema, F., van Niekerk, J., & Taillon, A. (2009). An inference-based approach to treatment obsessive-compulsive disorders. Cognitive and Behavioral Practice, 16, 420–429. O’Connor, K. P. & Robillard, S. (1999). A cognitive approach to the treatment of primary inferences in obsessive-compulsive disorder. Journal of Cognitive Psychotherapy: An International Quarterly, 13, 359–375. Polman, A., Bouman, T. K., van Hout, W. J. P. J., de Jong, P. J., & den Boer, J. A. (2010). Progress of change in cognitive-behavioural treatment of obsessive-compulsive disorder: Current status and some future directions. Clinical Psychology and Psychotherapy, 17, 1–12. Rachman, S. (1997). A cognitive theory of obsessions. Behaviour Research and Therapy, 35, 793–802. (1998). A cognitive theory of obsessions: Elaborations. Behaviour Research and Therapy, 36, 385–401. (2003). The treatment of obsessions. Oxford University Press. Rachman, S., & de Silva, P. (1978). Abnormal and normal obsessions. Behaviour Research and Therapy, 16, 233–238. Rachman, S., & Shafran, R. (1999). Cognitive distortions: Thought–action fusion. Clinical Psychology and Psychotherapy, 6, 80–85. Radomsky, A. S., Alcolado, G. M., Abramowitz, J., Belloch, A., Bouvard, M., Clark, D. A., et al. (2014). Part 1. You can run but you can’t hide: Intrusive thoughts across 13 cities on 6 continents. Journal of Obsessive-Compulsive and Related Disorders, 3, 269–279. Rapp, A. M., Bergman, L., Piacentini, J., & McGuire, J. F. (2016). Evidence-based assessment of obsessive-compulsive disorder. Journal of Central Nervous System Disease, 8, 13–29. Rowa, K., & Purdon, C. (2003). Why are certain intrusive thoughts more upsetting than others? Behavioural and Cognitive Psychotherapy, 31, 1–11. Salkovskis, P. M., Wroe, A. L., Gledhill, A., Morrison, N., Forrester, E., Richards, C., . . . & Thorpe, S. (2000). Responsibility attitudes and interpretations are characteristic of obsessive compulsive disorder. Behaviour Research and Therapy, 38, 347–372. Shafran, R., Radomsky, A. S., Coughtrey, A. E., & Rachman, S. (2013). Advances in the cognitive behavioural treatment of obsessive-compulsive disorder. Cognitive Behaviour Therapy, 42, 265–274. Shafran, R., Thordarson, D. S., & Rachman, S. (1996). Thought action fusion in obsessive compulsive disorder. Journal of Anxiety Disorders, 10, 379–391. Steketee, G., Frost, R., & Bogart, K. (1996). The Yale–Brown Obsessive Compulsive Scale: Interview versus self-report. Behavior Research and Therapy, 34, 675–684. Su, Y.-J., Carpenter, J. K., Zandberg, L. J., Simpson, H. B., & Foa, E. B. (2016). Cognitive mediation of symptom change in exposure and response prevention for obsessivecompulsive disorder. Behavior Therapy,47, 474–486. Thordarson, D. S., Radomsky, A. S., Rachman, S., Shafran, R., Sawchuk, C. N., & Hakstian, A. R. (2004). The Vancouver Obsessional Compulsive Inventory (VOCI). Behaviour Research and Therapy, 42, 1289–1314. Van Oppen, P. (1994). Cognitive therapy for obsessive-compulsive disorder. Clinical Case Studies, 3, 333–349. 267 268 Gillian M. Alcolado Wetterneck, C. T., Siev, J., Adams, T. G., Slimcowitz, J., & Smith, A. H. (2015). Assessing sexually intrusive thoughts: Parsing unacceptable thoughts on the Dimensional Obsessive-Compulsive Scale. Behaviour Therapy, 46, 544–556. Whittal, M. L., Woody, S. R., McLean, P. D., Rachman, S. J., & Robichaud, M. (2010). Treatment of obsessions: A randomized controlled trial. Behaviour Research and Therapy, 48, 295–303. Whittal, M. L., Thordardson, D. S., & McLean, P. D. (2005). Treatment of obsessivecompulsive disorder: Cognitive behavior therapy vs. exposure and response prevention. Behaviour Research and Therapy, 43, 1559–1576. Wilhelm, S., Berman, N. C., Keshaviah, A., Schwartz, R. A., & Steketee, G. (2015). Mechanisms of change in cognitive therapy for obsessive compulsive disorder: Role of maladaptive beliefs and schemas. Behavior Research and Therapy, 65, 5–10. Wilhelm, S., & Steketee, G. S. (2006). Cognitive therapy for obsessive-compulsive disorder: A guide for professionals. New Harbinger. Williams, M. T., Farris, S. G., Turkheimer, E. N., Franklin, M. E., Simpson, H. B., Liebowitz, M., & Foa, E. B. (2014). The impact of symptom dimensions on outcome for exposure and ritual prevention therapy in obsessive-compulsive disorder. Journal of Anxiety Disorders, 28, 553–558. Woody, S. R., Whittal, M. L., & McLean, P. D. (2011). Mechanisms of symptom reduction in treatment for obsessions. Journal of Consulting and Clinical Psychology, 79, 653–664. 14 Other Specified and Unspecified ObsessiveCompulsive and Related Disorders Jan van Niekerk and Kieron O’Connor* Introduction The diagnosis of “other specified” obsessive-compulsive and related disorder (OCRD) is made when the clinician describes the features of the presenting condition, which has similarities to an OCRD, but does not meet the full diagnostic criteria. “Other unspecified OCRD” is diagnosed when the clinician does not describe the presenting symptoms. DSM-5 (American Psychiatric Association [APA], 2013) provides seven examples of conditions in this category: Body dysmorphic-like disorder with actual flaws Body dysmorphic-like disorder without repetitive behaviors Body-focused repetitive behavior disorder (including behaviors such as repetitive nail biting or lip chewing, but excluding trichotillomania, excoriation disorder, stereotypic movement disorder and nonsuicidal self-injury) Obsessional jealousy Shubo-kyofu (from an indigenous Japanese diagnostic system: excessive fear of having a bodily deformity) Jikoshu-kyofu (related to shubo-kyofo: fear of having an offensive body odor; the alternative term, olfactory reference syndrome, will be used hereafter) Koro (a diagnostic label with origins in South East Asia: an episode of sudden and intense anxiety that the penis, or the vulva and nipples in females, will recede into the body, which may lead to death). The Malay word koro means “to shrink”; alternatively, kura means “tortoise” – the “head of the tortoise” is often used as an expression for the penis by the Malays and Chinese (Cheung, 1998). * Sadly, Kieron O’Connor passed away on August 27, 2019, just after the final submission of this manuscript. We would like to acknowledge his huge contribution to the field of obsessive-compulsive and related disorders. He will be greatly missed by his colleagues and collaborators. 269 270 Jan van Niekerk and Kieron O’Connor However, the above-listed conditions are not meant to be exhaustive. We will discuss CBT interventions in the sections below for the following presentations more likely to be encountered by the clinician: Obsessional jealousy Body-focused repetitive behavior disorders – not otherwise specified Body dysmorphic disorder with a visual defect Olfactory reference syndrome. Where the presentation falls outside this range, the clinician will have to carefully consider the available OCRD psychological models and how these may need to be modified to address the underlying mechanisms of the presenting problem. Further, transdiagnostic protocols (e.g., Barlow et al., 2011) could provide a helpful background framework for guiding formulation and intervention. Obsessional Romantic Jealousy Jealousy is a normal, complex social emotion experienced from infancy into old age. It has been defined as “the negative emotional state generated in response to a threatened or actual loss of a valued relationship due to the presence of a real or imagined rival” (DeSteno et al., 2006, p. 627). It serves an adaptive purpose, channeling cognition and behavior toward attainment of social goals, with a benefit to health. When predicated on realistic data (e.g., one’s partner flirting with someone else), jealousy is a reasonable response. However, it evolves into a clinical disorder when the concern strays from having a bearing in objective reality, such as when there is a “preoccupation with a partner’s sexual unfaithfulness based on unfounded evidence” (Kingham & Gordon, 2004, p. 207) and where the concern is unresolved by rational discussion. We will call this pathological jealousy, but other terms have been used (e.g., morbid jealousy). Pathological jealousy can manifest in varying degrees of conviction that the jealous concerns are justified: as a delusion (high, stable conviction); within the nondelusional category, as overvalued ideation (moderate conviction); or as an obsession (lower conviction). The current discussion will mainly be restricted to nondelusional, obsessional romantic jealousy (OJ), in line with the chapter remit. Ecker (2012) lists the following criteria for distinguishing non-delusional OJ from ordinary jealousy: (1) more time-consuming and distressing, (2) greater functional impairment, (3) greater negative impact on the partner, and (4) irrationality of the fears (e.g., they persist despite contradictory evidence). Prevalence and Impact Pathological jealousy is considered a relatively common clinical problem; however, epidemiological data are lacking (Ecker, 2012). From Shakespeare (Othello) to Jimi Hendrix (“Hey Joe”), culture is replete with examples of its toxic impact – it impairs Other Specified and Unspecified Obsessive-Compulsive and Related Disorders psychological health and can culminate in suicide, physical aggression, and even homicide, directed against the partner or the rival. Clinical Model Cognitive-behavioral formulation requires assessment of the following: 1. Learning history. Past experience and the meanings derived from them (i.e., beliefs about the self or others, and about ways of coping) constitute the template for the information-processing biases that fire up OJ. Examples of relevant experience/beliefs include insecure childhood attachment, prior traumatic loss (belief: “The people I love can leave me at any moment”), previous exposure to infidelity (“People can’t be trusted”), low self-esteem, a perception of sexual inferiority, a catastrophic expectation of relationship breakdown, and rules for staying safe (“I won’t be caught napping”). 2. Immediate precipitants (or triggers). A wide variety of stimuli can trigger OJ, including internal (e.g., imagined events, memories, thoughts about diminished physical attractiveness) or external (self-comparison with rivals, a partner being friendly with a rival). 3. Cognition. Jealous interpretations ensue: that the partner favors someone else (a present rival or a previous partner), is engaged in infidelity, or is considering cheating. The form of thinking may entail repetitive automatic intrusive thoughts (similar to OCD obsessions), which may be resisted, and/or lengthy ruminations (“Why can’t I be ever be good enough?”) or worries. The anticipated catastrophe is interpersonal – a defining feature. 4. Emotion. This can be complex: anxiety, fear (of rejection and loss), or anger (at the partner or rival for moral transgression or betrayal, or about causing jealousy), and shame, embarrassment, and guilt (when reflecting on the experience and consequences of OJ). 5. Behavior. Varied verification or repetitive safety behaviors (again, similar to OCD compulsions) may be deployed to “find out what is really going on” or to disconfirm the jealous worries, entailing a narrowed focus on, and response to, the particular concern. Examples include aggressively interrogating the partner about their movements or about past sexual experiences, examining bed linen for sexual activity, checking the partner’s phone, or repetitive reassuranceseeking from the partner. Avoidant strategies may be used, for example, requiring the partner to break off contact with opposite-gender friends. These behaviors are negatively reinforced by a temporary reduction in jealousyrelated distress; however, given the typical omnipresence of jealousy-relevant cues, coping or problem-solving strategies have to be ritualistically repeatedly enacted (similar to OCD rituals). 6. Secondary feedback loops. Jealous interpretation may be fed by the consequent negative affect, via an emotional reasoning bias, or as a result of conflict with the partner (e.g., after the partner refuses to provide reassurance: “You’re hiding something!”). Or jealous attention may make the partner feel special or powerful, 271 272 Jan van Niekerk and Kieron O’Connor and thus, be encouraged. The OJ sufferer may appraise their symptoms as being out of control, increasing their distress and inviting the use of maladaptive coping strategies (e.g., thought suppression, which paradoxically may achieve the opposite, or substance abuse, spiraling into aggression); however, simultaneously, jealousy may be considered helpful for staying safe and preventing surprises. Worry and rumination, ostensibly toward valued ends (such as distress reduction), result in protracted jealous torment, achieving the opposite. Assessment The diagnosis will need to be carefully considered (e.g., delusional vs. nondelusional OJ will require a different strategy), as well as assessment and management of risk to self and others. The bulk of the data enabling formulation will derive from the clinical interview; however, helpful supplementary information can be gained from psychometric assessment scales (listed in Ecker, 2012) and situational diary keeping of symptom triggers, emotional distress, and mediating factors (interpretations and behaviors). Interviewing the partner can be particularly helpful, setting the stage for their possible involvement in treatment. Formulation and Therapy Socialization The building blocks for cognitive-behavioral formulation are described above. The aim is to present the client with an alternative account of their problems residing in their thinking patterns and behavioral response, rather than in their partner. Ecker (2012) stresses the helpful contribution of a historical formulation. This allows the alternative account to be emboldened by having a plausible developmental underpinning and dovetails with a goal of normalizing jealous feelings, but seeking to modify the response to them. An example of the formulation of a jealous client is provided in Figure 14.1. The following elements may be helpful for socializing the client to the model: Jealousy is a normal emotion – it helps humans to bond and maintain their alliances; however, it becomes a problem when it leads you incessantly to doubt your relationship, and causes you distress. This can happen when you have developed powerful, unhelpful misgivings and apprehensions about yourself and others on the basis of your past experience (list the relevant experiences). They lead you to look out for what you fear. You then connect the dots and worry that something could be horribly wrong. You try to investigate your suspicions and allay your fears, but your strategies backfire (list any identified cons of the coping strategies). Suspicions linger and fester and the cycle repeats itself. Your relationship suffers – you squeeze your partner to keep them close, but you end up squeezing all the life out of the relationship, pushing them away. Treatment Therapist Stance and Psychoeducation Because people who suffer from OJ frequently feel ashamed of or defensive about their problems, the standard guidelines for establishing rapport in clinical Other Specified and Unspecified Obsessive-Compulsive and Related Disorders Learning history Mother has affair in early childhood; parents divorced; father loses interest in parenting. Discovered teenage steady cheated after relationship ended. Core beliefs and assumptions You can’t trust your partner. I’m not physically attractive. I’m at risk if my partner finds anyone else attractive. Losing someone you love is a terrible thing. Hypervigilant for infidelityrelevant cues Situational trigger Partner unexpectedly back late from work. Emotion Jealous Anxious Angry Guilty Cognitive They have been distracted lately/they didn’t want to have sex last weekend - they’re seeing someone. I will lose them. They have been lying. I haven’t been trying hard enough. Outcome Disbelieve them. Argument with partner ® ruminate. I have to be certain ® worry. Anxious, angry, depressed, ashamed Hypervigilant Retreat/distancing Figure 14.1. Cognitive-behavioral formulation of obsessional jealousy. Behavior Interrogate them. Confront them with the evidence. Blame and threaten them. 273 274 Jan van Niekerk and Kieron O’Connor interviewing apply ten times over. The therapist reassures the client that jealousy is a normal, commonly experienced feeling. Whether it is damaging depends on how it is managed and responded to. Increasing Motivation Carefully explore the client’s likely ambivalence about change: list the perceived pros of jealousy (e.g., preventing the partner from straying, preventing surprises, getting the partner back in line) and the cons (protracted personal/partner distress, relationship conflict and stagnation). Then consider the pros and cons of change in light of the likely future relationship trajectory if the status quo prevails (“Will your relationship continue to grow?”). Seek to question and reframe any progresssabotaging pros of jealousy or cons of change (e.g., “Even if your partner has broken off contact with his friends of the opposite gender, does that leave him happier with you?”). Consider whether benefits can be pursued using a healthier strategy (“Could there be ways of keeping your partner close without restricting them?”). Use of strategies derived from motivational interviewing may also be helpful; for example, address ambivalence using autonomy-affirming open questions and reflective listening, rather than persuasion (see Simpson & Zuckoff, 2011). Cognitive Strategies A common area of focus is the OJ sufferer’s interpretation that there is a risk of infidelity which has to be acted on. Standard CBT strategies may be used for restructuring of situation-specific automatic thoughts and underlying beliefs: thought elicitation, downward arrow (e.g., “What would it mean if they were seeing someone and you did nothing?”), and evaluation of validity (evidence for and against) and utility (costs and benefits). The aim is to introduce dissonance with OJ interpretations and encourage consideration of alternatives, while not arguing that the (sometimes unfalsifiable) jealous thought could not be true. Educate the client about the pitfalls of thought distortions (e.g., mind-reading: “They have a connection with each other”; soothsaying: “They will make a pass at them”) and work on articulating simpler, more helpful perspectives from within the parameters set by the existing context-relevant data. Cognitive restructuring work can also find a useful application in reconsideration of catastrophic beliefs regarding relationship breakdown (e.g. “I won’t be able to survive without them”). Insights from Inference-based Therapy for OCD (IBT; O’Connor et al., 2009) may have an application; here the jealous cognition is conceptualized as a doubt (“doubting what you know”) which derives from reasoning with its origin in the faculty of the imagination (which deals with “what could be” versus perception which deals with “what is”). The aim is to guide the client back to the simpler, commonsensical reasoning approach that they use in other domains of functioning. It can be helpful to examine the selectivity of their reasoning to OJ-relevant themes: “You’re not doubting that your partner is stealing your money, or earning extra income by working as a sex worker – how do you approach things differently there?” Other Specified and Unspecified Obsessive-Compulsive and Related Disorders The rationale for any jealousy-focused or jealousy-guided dysfunctional coping strategies (cognitive, such as worry or rumination, or behavioral, such as challenging or restricting the partner) needs to be carefully considered. What is the evidence against the pros? Overall, does the strategy deliver? Is the outcome attainable, that is, is it realistic to demand complete certainty about your partner’s inner experience, or about their movements? How does the strategy deviate from a healthy approach to relationship building? What is a sounder alternative to worrying or ruminating? (This line of questioning may expose unhelpful metacognitive beliefs about lacking control over worry/rumination, which need to be addressed – see Wells, 2009.) Overlapping with OCD approaches (see Frost & Steketee, 2002; Van Niekerk, 2018), the interpretation of OJ intrusive thoughts may benefit from consideration. Rather than designating actual threat, or a responsibility to act, have the client cultivate a stance toward their thoughts and feelings which recognizes that these are frequently irrelevant, transient, subjective mental events. In the absence of “hard evidence” to support their validity, it is better to accept and mindfully observe them, rather than try to control or act on them. The person is encouraged “to make room” for contradictory thoughts and feelings (e.g., resentment, love, and ire), and recognize that they have a right to their experience, but then refrain from unhelpful responses. A view of trust as a desirable, relationship-building attitude is promoted, and this entails not demanding 100% certainty about a partner’s behavior. A model of trust and acceptance of uncertainty can be explored in other interpersonal domains (such as letting your best friend stay in your house while you are away). If this works for the client, it can be helpful to name an alternative, healthier identity, guiding and subsuming therapy change, for example, “wiser Pat.” Leahy and Tirch (2008) suggest that insights and techniques from acceptance and commitment therapy (ACT; Hayes et al., 2012) and metacognitive therapy (MCT; Wells, 2009) can be helpful in promoting decentering from jealous feelings. Such insights and techniques might include metaphors (e.g., “Passengers on a bus” – the mind is noisy; jealous feelings are best accepted and disregarded, rather than avoided or acted on; Hayes et al., 2012) and detached mindfulness technique, to practice a more adaptive way of relating to thoughts (Wells, 2005). These approaches are not incompatible with the occasional adjunctive use of emotional regulation strategies, such as distraction or self-soothing behaviors, when jealous distress is high and there is a high risk of lapsing into destructive behavior. Yet, ideally, the longer-term focus should be on increasing the ability to practice acceptance and mindful observation of distressed experience (or the more workaday alternative: to tolerate distress better and catastrophize about it less), while refraining from unhelpful action. Where there is evidence of dysfunctional reasoning in this domain, decatastrophizing about the meaning of actual infidelity and relationship breakdown can be productive: “Are you really worthless if your partner cheats on you?” “You’ve coped with failed relationships before, why should it be different this time?” Core belief/self-narrative interventions (e.g., with themes of being an unlovable or worthless person) require good therapy rapport and are important for increasing 275 276 Jan van Niekerk and Kieron O’Connor the likelihood of enduring therapeutic change. Follow guidelines outlined in Young et al. (2003) and Beck (2011). As suggested above, use of strategies from different CBT approaches, for example, cognitive therapy (CT), IBT, ACT, or MCT, holds much promise in the treatment of OCRDs, but care should be taken that their combined use is coherent in terms of the case formulation and does not confuse the client. “More” can sometimes be less – a simpler strategy could be more powerful and efficient. Possible unhelpful consequences of the sequencing of techniques need to be considered (e.g., Gkika & Wells, 2015). When considering whether to combine traditional CBT and third wave methods, it may be helpful to reflect on both commonalities (Mennin et al., 2013) and differences (e.g. Hayes et al., 2013; Herbert & Forman, 2013) in the treatment models, to ensure clinical alignment. Farmer and Chapman (2016) provide further guidance. Behavioral Strategies A core focus of behavioral experimentation is on testing predictions about actual and/or mental consequences of reduction of dysfunctional coping or problemsolving responses. Ecker (2012) suggests that a useful strategy for identifying suitable options entails collaborating with the partner, by asking in which ways they would be acting differently if the client did not have OJ. Using standard guidelines, a list of mutually agreed experiments can then be designed in which the partner modifies their behavior so as not to be encroached on by jealousy. The client then responds by refraining from unhelpful responses and instead introducing valueguided behavior (e.g., jointly watch an arthouse film with erotic content and afterward discuss the artistic merits of the film instead of jealous worries). Relevant predictions are tested (e.g., that distress will continue interminably or that the client will not be able to function). Ultimately, the range of experiments is limited by what the client is willing to engage in. Where the client’s agreement cannot initially be obtained, further preparatory cognitive work may be helpful; however, be careful not to risk treatment disengagement by being perceived by the client to be invalidating, resulting in polarization. Experimentation can follow a graded approach, similar to exposure and response prevention for OCD. Note the caveats regarding the use of some imaginal exposure techniques in OJ described in Cobb and Marks (1979). Couple Interventions Involving the client’s partner can be a helpful adjunct to individual therapy. Furthermore, couple-focused intervention may be useful where skill deficits become apparent, such as in communication or sexual functioning, or where existing skills are not brought to bear in the problematic domain. Focus on how couples can communicate constructively about the jealousy problem, for example, negotiating an agreed definition of their commitment, giving clear feedback about helpful responses, and embracing a compassionate attitude. Other Specified and Unspecified Obsessive-Compulsive and Related Disorders Body-Focused Repetitive Behavior Disorders The term “body-focused repetitive behaviors” (BFRBs) refers to a group of maladaptive, injurious, and nonfunctional behaviors directed toward the body, including hair-pulling, skin-picking, and nail-biting (O’Connor et al., 2005; Teng et al., 2004). Individuals with BFRBs report diminished control over their behavior (Schreiber et al., 2011) and a range of physical and psychological sequelae (Diefenbach et al., 2005). Pathological hair-pulling (HP) and skin-picking (SP) are included in DSM-5 as trichotillomania and excoriation disorder, respectively, and these disorders are discussed in Chapter 16. However, several other BFRPs are mentioned in the diagnostic category of “Other Specified” OCRD, such as nail-biting, lip-biting, and cheek-chewing. Nail-biting or chewing (also called onychophagia) involves recurrent biting past the nail bed and cuticles, often drawing blood, creating scarring, or resulting in red, sore, and infected fingers (Penzel, 1995). Other lesser known BFRBs include trichotemnomania (hair cutting), dermatophagia (compulsive skin biting), rhinotillexomania (nose picking), and scab eating disorder. Finally, there is neck and knuckle cracking, or crepitation, often also termed “over-manipulation syndrome,” where a person forces sudden movements up and down or left or right, to the neck or spine; this causes rapid torsion, thereby compromising cervical or spinal stability and potentially resulting in ligament damage. The negative physical and psychological consequences of BFRBs are considerable (Diefenbach et al., 2002). Chronic nail-biting can damage fingers (Salmon-Ehr et al., 1999), gums (Krejci, 2000), and teeth (Johansson et al., 1991). Individuals may have infected and scarred fingers (Penzel, 1995) and be self-conscious and reluctant to show their hands (Williams et al., 2007). Although occasional knuckle cracking can be harmless, frequent cracking may lead to arthritis and dislocation of joints. These torsions often break bubbles in the joints, making a snap, crackle, pop sound and giving some satisfaction. Neck cracking is more serious and can lead to torn cervical ligaments and even a stroke. Individuals with BFRBs may avoid seeing doctors or dentists out of shame or fear of discovery, exacerbating their problems. Clinical Model and Formulation BFRBs are painful and produce physical consequences that result in shame and distress (Bohne et al., 2002; Diefenbach et al., 2002, 2005; Woods et al., 2001), and seem to be a distraction and a waste of time. However, they also seem to satisfy an urge and deliver some form of gratification or reward (APA, 2000; Penzel, 1995). One model, receiving recent research attention, is the emotional regulation (ER) model. ER refers to the way in which individuals identify and respond to emotional experience (Diefenbach et al., 2008). ER can be further understood as the process through which individuals influence the presence, experience, and expression of emotions (Gross, 1998). The ER model for BFRBs proposes that 277 278 Jan van Niekerk and Kieron O’Connor BFRBs function as a maladaptive mechanism for regulating emotions. That is, individuals with problematic body-focused behavior have difficulty regulating emotions and engage in BFRBs in an effort to avoid, decrease, or attenuate negative affect. BFRBs persist despite aversive consequences because they are negatively reinforced by relief from unpleasant emotions (Roberts et al., 2013). The ER model has been supported by studies that demonstrate change in affective states over the course of BFRB episodes. In clinical and nonclinical samples, individuals with HP and SP consistently report that emotions such as boredom, anxiety, tension, and frustration are present prior to BFRB and decrease during or after episodes of HP or SP (Roberts et al., 2013). Guilt, shame, sadness, and anger may develop subsequent to an episode of BFRB, but feelings of satisfaction, indifference, and relief are often present as well (e.g., Bohne et al., 2002; Duke et al., 2009; Mansueto et al., 2007; Neal-Barnett & Stadulis, 2006; Wilhelm et al., 1999). O’Connor and colleagues (O’Connor et al., 2001; Pélissier & O’Connor, 2004) observed that many individuals with BFRBs demonstrate a style of planning characterized by unwillingness to relax and difficulty with appropriate pacing of tasks. Individuals with this maladaptive planning style often try to do too much at once and feel the need to always be productive. They are consequently susceptible to frustration, impatience, and dissatisfaction when standards are not met, and to boredom when productivity is impossible. The authors suggest that one of the functions of BFRBs may be to release the tension generated by frustrated action (O’Connor, 2002, 2005). That is, impatience, boredom, frustration, and dissatisfaction build, creating tension. Tension and negative emotions are subsequently released or diminished through BFRBs. This frustrated action model also ties in negative emotions with aspects of perfectionism. In particular, there is a strong link between aspects of perfectionism and emotional regulation (Roberts et al., 2015). Although there are various types of perfectionism, the perfectionist components linked with pathology tend to be high standards and self-criticism (Dunkley et al., 2006). Self-criticism seems to be the key dysfunctional element. According to Thompson and Zuroff (2004), there are two forms of selfcriticism: (1) comparative, where the person compares the self unfavorably to others and (2) internalized, where the person falls short of their own standards, resulting in feelings of shame, for example, “I’m ashamed to be me” or “I’m ashamed I cannot live up to my own high standards.” Gilbert and Procter (2006) postulated two types of shame: (1) internal shame, characterized by a devaluation of the self as inadequate and (2) external shame, when the person projects the thoughts and feeling of others on to the self. Noble (2012) found shame to be an important mediator between perfectionism and symptoms of HP. Shame is also frequently reported in BFRBs (Weingarden & Renshaw 2015), to the extent that these authors propose that shame is the principal trigger for BFRBs, particularly shame about the body. According to this model, BFRBs serve to neutralize the shame. But of course, the consequences of BFRBs (e.g., damaged nails) elicit further shame and so produce a negative reinforcement cycle. Other Specified and Unspecified Obsessive-Compulsive and Related Disorders Maladaptive cognitive emotion regulation strategies Perfectionism Self-criticism Shame BFRBs Figure 14.2. BFRB model. Hence the model shown in Figure 14.2 might further refine the mechanism of BFRB onset. Here perfectionism creates the core emotion of shame, mediated by self-criticism, and frustrated action is a side consequence. Treatment Current treatment approaches generally involve identification of multimodal triggers and implementation of stimulus and response control. But current treatments rarely directly address emotional regulation, although adjuncts of mindfulness and ACT may indirectly influence mood (Flessner et al., 2008). Habit reversal training (HRT) has been used to treat a wide variety of BFRBs and allows short-term improvement, although this was not sustained over the long term (Morris et al., 2013). Mansueto and colleagues (2007) developed the comprehensive behavioral (ComB) model, which adds to HRT by encompassing a wide range of cognitive, affective, motor, sensory, and environmental modalities. When doing HRT, the therapist and client conduct a functional analysis and identify triggers. They then implement the following: 1. Awareness exercises, involving monitoring the habit 2. Stimulus control (either internal or external stimuli, that is, state or signal control), for example, becoming aware that a certain activity provokes the habit and so avoiding it 3. A competing response, which does not necessarily need to be anatomically antagonist but should prevent the BFRB. Since most BFRBs start with the hand, or a manipulation of the hand, this initial move needs preventing by introduction of an opposing action, like keeping the hand on the knee or in contact with a hard surface. An alternative is the cognitive psychophysiological (CoPs) approach, which has proved effective on a range of specified and unspecified BFRBs (see O’Connor et al., 2015). This involves addressing the underlying emotions triggering BFRBs, as well as more multimodal stimulus control. Stages include increasing awareness of but also understanding the way trigger situations are evaluated. For this purpose, an adaptation of George Kelly’s construct theory (Blowers & O’Connor, 1996) is used, where evaluations are elicited specific to each situation. The way the person reacts in the situation is then addressed cognitively and behaviorally with the aim of introducing greater flexibility, in particular, transplanting approaches in low-risk situations to high-risk situations – so adding habit control and modifying 279 280 Jan van Niekerk and Kieron O’Connor tension-producing thoughts and the style of planning of actions. The latter refers to how people plan and approach action and whether they prepare in an adaptive or maladaptive manner. Meta-cognitions of judgment and self-blame are also addressed. (A complete manual can be found in O’Connor et al., 2017.) BFRB Case Study. The following case is of an atypical BFRB treated with the CoPs approach (described above). The client presented with repetitive biting of the inner lip and the skin around the fingernails, and then rubbing her arms up and down symmetrically, all in the same movement, accompanied by tension in her jaw and shoulders. She would repeat the habit in front of the mirror, observing herself for several minutes, several times per day. The habit developed at the age of 13 years when she claimed she became more self-conscious about comments at school about her exposed body parts (arms and face). Auto-observation revealed that she performed the habit about 20 times a day for several minutes. On evaluation, she had mild depression and she reported that she was very emotional and had problems controlling negative emotions, frequently ending up crying. She said she reacted emotionally very quickly and had problems regulating stress. She scored high on the personal standards and organization subscales of the Frost Multidimensional Perfectionism Inventory and was quite rigid in her planning and ordering of events. This was, she claimed, so as not to waste time. She found it difficult when routines were changed or things went wrong. She also judged her self-worth entirely on her appearance and presentation to others and was particularly concerned that her arms and hands should appear correctly groomed. She also walked with a posture where her hands were kept close to her face as though ready to correct some blemish. She showed a classic overactive style of planning (as measured on the Style of Planning Action Questionnaire; O’Connor et al., 2015), where she found it difficult to sit still, and she was constantly attempting to do too much. She was afraid of wasting time and would rapidly become impatient when, for example, her computer malfunctioned at work, or when engaged in what she considered unnecessary conversations and social events. Sometimes she dealt with stress by suddenly feeling very tired and then “tuning out” of the situation. In the initial stages of the 10-week treatment, she had problems completing the relaxation exercises since she felt that she was not tense and therefore she also felt that she was wasting her time. This response is not atypical since people with BFRBs often do not appreciate that their tension may be high. Eventually, she realized that she was tense and the relaxation and discrimination exercises helped her acknowledge tension and therefore enhance her ability to respond more flexibly. She recognized that her thoughts and attitude contributed to her high levels of impatience. Hence, she profited from cognitive restructuring to change her thoughts about conversations with others, her idea of how others perceived her, and the need to be and appear perfect. Rather than constantly dividing her attention between the task and the conversation at hand, and self-observation, she dropped the selfobservation in favor of immersion in the task. Other Specified and Unspecified Obsessive-Compulsive and Related Disorders At the eighth session, her habit intensity and duration were reduced, and at post-treatment, habit frequency was significantly reduced. At post-treatment, there was still some tension and she reported 70% control over the habit. At the sixmonth follow up, she said she had maintained the changes in her thinking and action, and claimed that she did not even think about the habit and controlled it unconsciously. She reported that the goals of therapy had been achieved, and this was supported by clinical and psychometric pre-post evaluations. Body Dysmorphic Disorder with Visible Defect Although most body dysmorphic disorder (BDD) is invisible and only the person sees the defect, sometimes there is a minimal defect. Typically, this may involve a mild facial blemish or, in men, a mild body asymmetry or muscle underdevelopment. In these cases, more than in regular BDD, there is frequently other underlying pathology – in particular, impaired social judgment, social phobia, overinvestment in appearance, and doubts about being generally unattractive, or having a general insecurity, such as about gender identity (Philips, 2009). The behaviors found in more typical BDD, such as mirror-checking, applying makeup, camouflaging, frequent clothes changing, avoidance, and reassuranceseeking, may have greater apparent justification due to the objective defect. Recourse to surgery may be more frequent, and greater family accommodation of dysfunctional responding is problematic and may sanction avoidance. Exposure is difficult to achieve without prior belief change. Standard CBT Approaches Veale and Neziroglu (2010) recommend several CBT strategies for BDD, some of which are listed below. In the first instance, offer the client psychoeducation and deal with ambivalence about change. Identify and present the self-sabotaging loops of coping behaviors such as staying at home and avoidance, and identify the best alternative options for moving toward goals. Although support groups can help, it is important to avoid Google chat groups and internet searches, which may feed BDD. Address unhelpful judgments and metacognitions (e.g., “Why can’t I be like everyone else? I shouldn’t be suffering like this”). Educate the client in addressing self-critical appraisals using rational responding. Alternatively, mindfulness training can help in promoting decentering from self-flagellating thinking. At the same time, it is important to learn to direct attentional focus outward/ externally, since it is so often fixated internally. Mirror retraining can be helpful and involves looking in a mirror for a specified period of time and not selectively overfocusing on specific features. Other exercises in attentional retraining involve listening and talking exercises where the person learns to switch attention and distract themselves. Gradually giving up off safety behaviors is a standard behavioral technique where the person eliminates self-attacking behaviors, hypervigilance, and 281 282 Jan van Niekerk and Kieron O’Connor disguising, and examines the results. For example, the person ceases comparing their present appearance with that in old photos. Instead, new photos can be taken and the person asked to judge them as a third person (Wilhelm et al., 2013). Other cognitive strategies involve examining the questionable utility of rumination and worry, and how they get in the way of solving the real problems. Imagery rescripting can be helpful – here the person replays a scene where they felt their body part was demeaned in the past and rescript it from a position of power. This involves reframing the demeaner, and replying to the criticism from the perspective of the adult self, who comes to the rescue. Further, behavioral activation is important since so many clients become inactive and restrict themselves to their homes as a mechanism of defense. Finally, if the BDD entails skin- or scab-picking, then habit reversal (see above) may be combined with other CBT techniques. An alternative is to introduce CoPs as a combined or standalone strategy, which is described above in the BFRBs section on treatment. Inference-Based Therapy Traditional cognitive-behavioral models propose that unwanted intrusive thoughts are a universal experience, but that if they are appraised as holding negative implications for the person (e.g., “People will reject me because I look hideous”), the person will become preoccupied and try to “neutralize” or otherwise suppress the thought, consequently maintaining the preoccupation. On the other hand, IBT conceptualizes obsessions as doubts that are supported by an inductively generated and purely idiosyncratic narrative. In fact, IBT considers that there is a subjective narrative that precedes and supports the obsessional doubt before the intrusion is even appraised. The reasoning process, hypothesized to be common to OCD and BDD, and to lead to obsessions, is termed inferential confusion (O’Connor et al., 2005). Those whose reasoning processes are characterized by inferential confusion tend to distrust their senses and common sense, and to invest in remote and often imaginary possibilities at the expense of reality. See Table 14.1 for a list of inferential reasoning errors with examples applied to BDD. The aim of IBT is to modify the reasoning narrative producing the doubt, and to return the person to the world of commonsense perception. In IBT, obsessions are conceptualized as a two-step process. The person first arrives at one or more primary doubts about imperfection through a subjective narrative (inferential confusion) that leads them to confuse reality in the here and now with subjective possibilities. In BDD, overvalued doubting beliefs are common, that is, doubting with high conviction that certain aspects of their appearance are normal, for example, “My body is weirdly shaped” or “My skin is too oily.” The primary inference (e.g., “My nose is ugly”) is generally followed by one or more secondary inferences, that is, the negative consequences that are expected to derive from the primary doubt, such as: Other Specified and Unspecified Obsessive-Compulsive and Related Disorders 283 Table 14.1. Overview of reasoning errors in IBT (from Taillon et al., 2013) Reasoning error Definition Example Category errors Confusing two logically distinct properties or objects Apparently comparable events Selective use of out-of-context facts Purely imaginary sequences Distrust of normal perception Inverse inference Confusing two distinct events separated by time or place My sister had a nose job and got a lot of compliments. This procedure is therefore also justified for me. Teenagers with acne get mocked, which means that I can also be laughed at if my skin is imperfect. Inappropriately applying abstract facts to specific personal contexts Actors with physical flaws don’t get as many contracts. Making up convincing stories and living them Disregarding the senses in favor of going deeper into reality When people look at me, I feel my nose grows even bigger and I become even uglier. People say I look okay but it doesn’t mean that I actually do. Inferences about reality precede rather than follow from observation People in the room have laughed, which might mean I look ugly. “Nobody will ever love me because of my hideous nose.” Contrary to traditional cognitive behavioral approaches, IBT therefore addresses the initial content of the BDD doubt by intervening in the process of inferential confusion that led to it, rather than focusing on the perceived negative consequences arising from its appraisal. The rationale behind IBT is that addressing the initial BDD doubt will ultimately remove the trigger for the secondary distressing appraisals (Aardema & O’Connor, 2003). All the other BDD maintenance factors ultimately have to be eliminated, for example, attentional hypervigilance, ritualistic behaviors, thought suppression, and avoidant strategies, but the primary focus is on eliminating inferential confusion. In the most elegant solution, when the primary doubt is invalidated, the need for the use of dysfunctional coping strategies is eliminated. The IBT formulation applies equally to BDD with and without visible defect. BDD Case Study 1. Joe was a 31-year-old single man who worked as a fireman. He presented complaints of disabling preoccupations concerning his muscle mass and bone structure that have been present for the past 18 years. Joe stated that he was scarred by experiences of being mocked as a child, when he remembered being called ugly and scrawny. In fact, his body shape was objectively asymmetrical and he was weaker on one side. Joe’s main obsession was that if he were not “bigger,” the consequence would be that he would be unable to find a girlfriend. Joe engaged in a series of compulsive and safety-seeking behaviors such as working out excessively (two hours per day, five days per week), eating large amounts of food, checking his appearance in the mirror (for approximately 20 minutes, four to five times per day), and comparing his 284 Jan van Niekerk and Kieron O’Connor appearance to people around him and people on the internet (approximately two to three hours per day). His social network and daily functioning were only mildly impaired – he had a few friends and was functional in most domains of his life. Joe avoided bars, discos, and gyms (he worked out at home) and had stopped weighing himself for eight years. Apart from a primary diagnosis of BDD (in his case, “muscle dysmorphia”), Joe also met criteria for social anxiety disorder and presented borderline and avoidant personality traits. He was not taking any medication. At baseline, before therapy, Joe’s total BDD–Yale–Brown Obsessive Compulsive Scale (BDD-Y-BOCS) score was 28, in the severe symptomatic range. Severity of obsessions and compulsions was equivalent, and insight was fair, with mild associated depressive and anxious symptoms. Joe’s therapist assessed him over four sessions. Obsessions and compulsions were listed and clarified (see above). Obsessions were then explored further and elaborated in terms of IBT’s primary and secondary inferences. The question: “What do you fear would happen if you were prevented from engaging in your compulsive and reassuring behaviors?” will often allow specification of the person’s secondary inference. In Joe’s case, he feared that if he did not perform his rituals (e.g., working out), then he “would not find a girlfriend” and “would be less attractive and popular.” Joe was 90% convinced that these consequences would be realistic if he did not perform his compulsions. Starting from the identified feared consequences, the therapist can then work back to the initial obsessional doubt by posing the question: “Which doubt would have to be eliminated for you to be able to resist the compulsions?” In Joe’s case, the primary initial BDD doubt was: “Perhaps I’m not big enough to get noticed/ respected/loved.” Joe rated his doubt as 100% probable. The first part of the treatment aims at clarifying the distinction between subjective and real doubt. Real doubt is justified by new sense-based information (e.g., wondering if it is cold outside after seeing people wearing jackets and scarves), whereas subjective/imaginary doubt is not based on any new information that signals problems in the here and now (e.g., when there is no realistic precipitant for Joe ruminating, when waking up in the morning, on whether he is attractive enough to be loved). There may be an external trigger (e.g., seeing one’s reflection in the mirror), but the content of the doubt does not rely on normal attention to new sense-based information in the present (e.g., someone telling Joe that he is ugly). Thus, Joe’s reaction to the doubt (e.g., mirror gazing) does not lead to further information which allows him to resolve the doubt, but rather pushes him to go beyond his senses and commonsensical interpretation, unproductively venturing into the imagination. The next stage of therapy reveals to the person the reasoning supporting their doubts. The justification can seem quite logical since the arguments supporting the doubt are not necessarily incorrect on their own (e.g., “People do sometimes get rejected because of their looks”). It is often not the content of the justification which renders the doubt “illogical” but rather the context in which it occurs. Joe came up with the following arguments Other Specified and Unspecified Obsessive-Compulsive and Related Disorders to justify his doubt: “In movies, it’s always the attractive guy that ends up with the pretty girl” and “There are always women lining up at male strip clubs, therefore this is the kind of man (attractive and muscular) that women are attracted to.” These arguments did not derive from realistic information in the present, but rather from previous experiences and his own logical calculations that were irrelevant to Joe’s own situation in the here and now. He was able to recognize this, but still found it difficult not to give credence to these justifications. The objective of IBT’s third stage is for the person to recognize that the BDD doubt originates from them rather than from their senses. IBT therefore does not rely on convincing the person of the unlikelihood of the doubt, but proposes its irrelevancy to the context in which it arises. This was illustrated in Joe’s case by using an OCD example which was neutral to him – someone doubting that their hands might be dirty without any sense-based information justifying such a doubt (e.g., seeing dirt on their hands or smelling a bad odor from their hands). The next stage of IBT highlights the power of the imagination and explains how convincing, subjective reasoning leads the person into the BDD doubt. The “story” behind the doubt is countered by developing an alternative story exclusively based on realistic information in the here and now. The aim is to come up with an alternative story, rather than to “disprove” the BDD story. Although Joe was able to recognize both stories as being equally possible, he still continued to invest more in the BDD story, as is normal at the start: Joe’s BDD story: Joe’s alternative story: Maybe I am not big enough to get noticed/respected/ loved. In the past, I have elicited positive reactions from women because I was in good shape. This proves that I must continue working out. The bigger I will be, the more I will get noticed, just like the dancers in the clubs. These men look good and there are always women lining up at clubs to see them. This is therefore the kind of man that attracts women. Also, in movies, it is always the guy with the good looks that ends up with the pretty girl. It is not surprising that men who are in shape feel better, have more confidence, and are more popular. I don’t need to be big to get noticed/respected/loved. I can very well be, noticed, respected, and loved regardless of my appearance or physical condition. I am a good listener, I have good communication skills, and I am respectful of others. I enjoy helping people; in fact, that’s what I chose to do as a job. I have a good sense of humor and I don’t take myself too seriously. I am easy to approach and I enjoy being with people, talking to them and reassuring them. I am more than a weight or a body. All these qualities contribute much more to the love and respect that people can have for me. 285 286 Jan van Niekerk and Kieron O’Connor IBT’s step 5 is to help the person create distance from their BDD doubt by learning to identify a cross-over point when they leave reality behind and get caught in a “BDD bubble,” where the imagination takes over. A metaphor of a bridge is useful here: the therapist asked Joe to visualize himself crossing a bridge. On one side was reality, his senses, and his normal everyday responses. On the other side was the BDD doubt. The therapist asked Joe to move across the bridge toward the doubt and identify the specific moment when the imagination started to jump in. Although Joe understood the principle, he had to reflect to identify a precise moment when his BDD took over. This exercise was repeated at home and in sessions before Joe mastered identifying the cross-over point. The next two steps of IBT cover the reasoning devices (see Table 14.1) in the person’s narrative, which invalidly convinces them to be invested in the doubt. In Joe’s case, the principal reasonings were category errors and selective use of out-ofcontext facts. Joe achieved a good understanding of this stage and participated well. In step 8, the therapist covers the selectivity of the BDD doubt by exploring situations where Joe did not experience such doubts. If the person can become aware of other situations where they adopt a “normal” style of reasoning, it will highlight the irrelevance of obsessional doubts in BDD situations. Joe’s therapist used the example of crossing the street to illustrate this point. Joe agreed that in this situation, he did trust reality to decide whether it was safe to cross the street (e.g., looking left and right, waiting for the green light). He did not invoke far-fetched possibilities such as, “A car may cross the corner suddenly,” which would stop him from ever crossing the street. Joe was able to appreciate that his reasoning differed in BDD and “neutral” situations and that he chose not to trust his senses when it came to BDD situations. The next stage of IBT probably was most productive for him. The aim of step 9 is to discover the person’s vulnerable self-theme by exploring why the person experiences doubts in one area, but not in others. Joe realized that his muscularity was directly linked to his desire to be strong and a “real man” and that the BDD doubt of not being big enough made him feel weak and lacking character. He was gradually able to develop a more realistic view of himself by exploring and challenging the meaning of being “strong” and by considering and listing his other personal attributes that illustrated strength of character. The objective of IBT’s last step is to train the person in the proper use of their senses in BDD situations. Joe spent a lot of time each day analyzing his reflection in the mirror. Rather than representing appropriate reasoning about the meaning of sensory feedback, these behaviors in fact reflect a distrust of sensory feedback. In order to help Joe understand a “proper use of the senses,” his therapist used the neutral example of combing his hair in the morning. However, as Joe gradually learned to see his body and trust his senses using the same method as he did when grooming his hair, he reported feeling that he was “not doing enough” or that he was “missing something.” People with BDD often report this feeling, but as Joe’s therapist told him, it was temporary and should disappear over time as he again learned to trust his senses and reacquaint himself with a commonsensical reasoning Other Specified and Unspecified Obsessive-Compulsive and Related Disorders approach. Trusting the senses involves just accepting what the senses say using a simple reasoning approach – therefore, not applying extra effort and invalidating the initial impression by trying to go “deeper” – in other words, using the senses exactly as the person does in other non-BDD walks of life. Overall, Joe collaborated well in therapy and was compliant with homework and session attendance. Although his symptoms improved consistently over the weeks, working on his vulnerable self-theme (IBT’s step 9) appeared to have had the biggest impact in reducing the strength of conviction in his obsession. In fact, Joe’s score on the Overvalued Ideas Scale went from 6 at pre-treatment to 2 at post-treatment. At the end of the therapy, a 79% reduction was observed in Joe’s total BDD-Y-BOCS score (which fell in the subclinical range), with obsessions slightly more severe than compulsions. Although already low at the beginning of treatment, depressive and anxiety symptoms also decreased considerably (from 14 to 3 on the Beck Depression Inventory-II, and from 12 to 3 on the Beck Anxiety Inventory). Treatment of cases other than Joe shows that there tend to be differences in the benefits derived from and the obstacles encountered at each treatment step (see further examples described in Taillon et al., 2013). The focus of IBT on faulty inferences and overinvestment in obsessional doubts fits with the recommendation of Labuschagne et al. (2010) to include techniques from models of delusional thinking in the treatment of BDD. This focus on reasoning processes occurring before – and leading to – overinvested primary inferences fundamentally differentiates IBT from traditional CBT interventions, which typically target the feared consequences derived from the initial doubts. Given the chronic nature of BDD, it is noteworthy that with IBT, therapeutic gains appear to be maintained – or in some cases even improved – six months following treatment, suggesting that changes in reasoning processes and inferences endure (Taillon et al., 2013). The protocol may benefit from adding a module addressing depression. This is highlighted by the case study described below, which considers some of the difficulties encountered when attempting to treat a somatic delusion of having a terrible appearance defect, in the context of a small, but objectively visible defect. BDD Case Study 2. Dor was a 25-year-old female who had suffered from severe BDD for seven years, during which she was confined to home. Her central concern was that she was disfigured because of her facial acne. She claimed that she quit school after numerous negative comments from peers, and with the acquiescence of her parents. There were no stated reasons other than the acne for discontinuing school. Hence, the first treatment obstacle: significant others are more likely to agree with, sympathize and accommodate clients with BDD with visible defect. Due to the accommodation of her parents, Dor had missed several years of schooling, which further complicated her recovery. The family dynamic was complex: Dor’s older sister had broken off contact with her, considering her a “fake.” Her mother and stepfather were very accommodating of her difficulties, agreeing to her requests to stay in her room and be left alone, not go on outings, disengage from prescribed 287 288 Jan van Niekerk and Kieron O’Connor home-based education, and not perform domestic tasks. If her stepfather insisted on her doing the tasks, Dor would express anger and throw tantrums until she got her way. Even when she became aggressive with her parents and had spent 28 days in self-isolation, no behavioral limits were imposed using strategies of either positive or negative reinforcement. When questioned, in addition to what was wrong with her facial complexion, Dor would identify another “60,000” things wrong with her, including hip size, breast size, height, and body shape. The second obstacle: The initial (objective) label of defect generalizes to multiple additional nondesired physical features. Dor scored high on perfectionism, in particular, on the Personal Standards Scale. She had poor to moderate insight on the Brown Assessment of Beliefs Scale, low resistance to the obsessions, and low control over the compulsions. The third obstacle: Despite some insight that her concerns might be unjustified, this did not translate into an ability to resist or control the responses to her obsessions. Dor admitted there was a psychological element in her BDD, but still wanted to change her features surgically. The fourth obstacle: Anticipation of social scrutiny was a large source of anxiety for Dor, and before going out she would heavily camouflage herself with makeup in order to hide her complexion – to a greater degree than is typical in BDD. Fifth, Dor would exacerbate the barely visible facial marks by rubbing and tweaking at her skin (also described in Veale & Neziroglu, 2010), hence exacerbating the signs and making them more visible – so confirming the defect. Finally, as well as clinical depression, and social anxiety in the moderate range, Dor had antisocial personality traits – this raises the possibility that a manipulative tactic may have been a factor in some of her BDD avoidance behavior. Thus, additional comorbidity presents an amplified treatment challenge. Treatment. Dor sporadically attended six CBT therapy sessions over four months. She admitted that she would not judge others by their complexion. She acknowledged that her views were selective and that her BDD did not present an objective impediment to pursuing her life goals. A large component of therapy time was focused on improving her mood by using behavioral activation strategies, aiming to introduce greater planning and structuring of her activities. Some exercise routines were established and Dor undertook more regular short trips outside her home; however, more intensive exposure work was refused despite Dor having benefited from brief exposure. The therapist also allocated considerable effort to addressing maintenance factors within the family system, such as improved parenting skills and negotiating a decrease in voluntary accommodation of problem behavior and using strategies of reinforcement in a consistent way to diminish symptom accommodation. Outcome. Dor’s parents decided, against cautionary advice, to fund her pursuit of surgery. She embraced this option and disengaged from therapy with a promise to return after having had laser surgery. She was convinced that surgery would be her salvation and would enable her to feel comfortable in society. With her parents’ agreement, she terminated therapy. Other Specified and Unspecified Obsessive-Compulsive and Related Disorders Olfactory Reference Syndrome Olfactory reference syndrome (ORS) is a form of dysmorphophobia where the person is afraid that they emit a body odor, either from a specific part of the body or generally. This can include bad breath, genital scent, anal odor, armpit smell, chemical or tainted aroma. In particular there is a belief that others can detect the smell even if they do not communicate this. The disorder verges on delusional and there may be a paranoiac element, where the person is extra-vigilant to any possible social signal of smell detection, without further proof (e.g., nose wrinkling, coughing, or sighing). Other compulsive behaviors include typical BDD safety behaviors and strategies of over-disguising smells, avoiding close gatherings or social occasions, and frequently checking for smells. The checking behavior, as with OCD, frequently increases the doubt that there is a smell. Phillips and Menard (2011) report the following ORS preoccupations: bad breath, bad-smelling armpit/genitals/anus/feet/skin, flatulence, odd non-body emissions (old tires, rubbish), with symptoms present for one hour or more. Compulsive responses included smelling oneself (80%), showering (68%), dietary modification (45%), brushing teeth (40%), scrubbing nails (40%), laundering clothes (30%), sniffing others for comparison (30%), and reassurance seeking: “Do I have bad breath?” Other problem behaviors include camouflage, professing embarrassment, social avoidance, drug use, quitting jobs or leaving situations abruptly, and even suicide attempts. Mood disturbance, social anxiety, shame, and low self-esteem are common. ORS prevalence is unknown. The person often mis-smells and is inaccurate partly due to repetition but also due to misinterpretation of normal body odors (www.katharinephillipsmd.com/). Phillips and Menard (2011) recruited 20 patients, 60% female. The majority developed ORS in their mid-twenties, with no remission at two-year follow-up. Their ORS-Y-BOCS score was in the severe range, with moderate to severe interference in daily living. They were smelling a mean of 2.9 (SD: 1.4) body locations. The Brown Assessment of Beliefs Scale score overall was in the delusional range, with no to poor insight; but not all were classified as delusional. Eighty-five percent reported they smelled their unwanted body odor; 95% that others did; 88% had ideas of reference; 55–70% masked the smell with powder, deodorant, perfume, or mints. Forty-four percent sought alternative treatments (e.g., prescription mouthwash, tonsillectomy), which may have displaced some ORS symptoms, but the disorder prevailed. People with ORS may actually hallucinate smells, but as stated above, not all are delusional; 15% seem to have poor to fair insight. Some medical problems can lead to bodily excretions such as fish malodor syndrome (trimethylaminuria), but there are no reports of overlap with ORS cases. ORS can culminate in suicidal and violent behavior associated with strong reactions to what patients see as deceptive responses by others. There is a strong comorbidity with both social phobia and major depressive disorder, which generally develop subsequent to ORS. For a screening test, see https://ocdla.com/olfactoryreference-syndrome-test. 289 290 Jan van Niekerk and Kieron O’Connor Treatment for ORS is the same CBT as applied in BDD, but addressing ORS. But there is a danger that unless the general theme of dysfunctional thinking regarding smelling is addressed, and the smells are just dealt with one by one, the person will replace the resolved body smell with another. Inference-based therapy (IBT), discussed above, which unravels the person’s narrative about their smell, could be of assistance here, as the following case study illustrates. ORS Case Study. Mel was a 39-year-old male who had suffered from ORS since early puberty. He traced the onset to concern about his grandfather, who lived with the family and often through negligent hygiene would smell of urine or stale clothes, details that were commented on by members of the family. Mel thought he himself might emit such smells and hence felt constantly embarrassed or shameful. Mel had comorbidities of depression and social anxiety. He had poor insight and also paranoid tendencies, which classified him as between BDD and a somatic delusion. He self-referred to our study on BDD. Among other compensatory behaviors, Mel would try to camouflage his smell with cologne, and frequently changed his clothes and left social situations and spaces. He frequently quit jobs. He would not board a crowded bus and would change carriages in the metro, convinced everyone could smell him. Interference with daily living was severe, and apart from occasional visits by his family, he was isolated. An important feature of his ORS, which mimicked a paranoid presentation, was his constant vigilance for the reactions of others. Any nose movement, sniffing, even change in breathing pattern or head movements was confirmation that the other person had smelled him. Reassurance from family members that he did not smell was met with distrust and even a suspicion of deception: “Oh, they would say that to make me feel better” or “They don’t want to admit the truth.’’ Mel was treated with IBT (protocol described in BDD section above) where the justifications for his doubt about smelling and the reasoning errors in the narrative were identified and replaced with trust in normal sense data as in other walks of life. Reasoning errors included jumping prematurely to conclusions, imaginings, and interpreting categories of events as similar when they were not associated. And of course, he distrusted his senses and deviated from commonsense interpretations of social signals. His ORS-Y-BOCS reduced to the mild range after 16 weeks of treatment, as did his Beck Depression Inventory and ratings of social anxiety. Some of his safety behaviors and vigilance were more difficult to eliminate, and here more conventional techniques of attentional refocusing, distraction, and strategies aimed at enhancing cognitive flexibility proved helpful additions to reinforce reality sensing and eliminating confirmation bias. Final Remarks The chapter aimed to provide an overview of the CBT treatment strategies on offer for addressing obsessional jealousy, body-focused repetitive behavior disorders, body dysmorphic disorder with a visible defect, and olfactory reference syndrome. Other Specified and Unspecified Obsessive-Compulsive and Related Disorders Strategies covered include earlier CBT and behavior therapy approaches and newer methods such as inference-based therapy, metacognitive therapy, and ACT. The heterogeneity of presentation and therefore the treatment approach required is considerable; in fact, the OCRD diagnostic category has been criticized as lacking coherence (see Abramowitz & Jacoby, 2015). We therefore provide a very cursory overview, but have made recommendations for further reading in the text. We hope that the chapter can make a useful contribution to helping clients presenting with these challenging problems. FURTHER READING Obsessional Jealousy Ecker, W. (2012). Non-delusional pathological jealousy as an obsessive-compulsive spectrum disorder: Cognitive-behavioural conceptualization and some treatment suggestions. Journal of Obsessive-Compulsive and Related Disorders, 1, 203–210. Leahy, R. L. (2018). The jealousy cure: Learn to trust, overcome possessiveness, and save your relationship. New Harbinger. Body-Focused Repetitive Behavior Disorders O’Connor, K. P., Lavoie, M. E., & Schoendorff, B. (2017). Managing tic and habit disorders: A cognitive psychophysiological approach with acceptance strategies. Wiley-Blackwell. Body Dysmorphic Disorder Wilhelm, S., Phillips, K. A., & Steketee, G. (2013). Cognitive-behavioral therapy for body dysmorphic disorder: A treatment manual. Guilford Press. Olfactory Reference Syndrome Phillips, K. A., & Menard, W. (2011). Olfactory reference syndrome: Demographic and clinical features of imagined body odor. General Hospital Psychiatry, 33, 398–406. REFERENCES Aardema, F., & O’Connor, K. (2003). Seeing white bears that are not there: Inference processes in obsessions. Journal of Cognitive Psychotherapy, 17, 23–37. Abramowitz, J. S., & Jacoby, R. J. (2015). Obsessive-compulsive and related disorders: A critical review of the new diagnostic class. Annual Review of Clinical Psychology, 11, 165–186. American Psychiatric Association [APA]. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). American Psychiatric Association. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association. Barlow, D. H., Farchione, T. J., Fairholme, C. P., Ellard, K. K., Boisseau, C. L., Allen, L. B., & Ehrenreich-May, J. (2011). Unified protocol for transdiagnostic treatment of emotional disorders. Oxford University Press. Beck, J. S. (2011). Cognitive behavior therapy: Basics and beyond (2nd ed.). Guilford Press. 291 292 Jan van Niekerk and Kieron O’Connor Blowers, G., & O’Connor, K. P. (1996). Personal construct psychology in the clinical context. University of Ottawa Press. Bohne, A., Wilhelm, S., Keuthen, N. J., Baer, L., & Jenike, M. A. (2002). Skin picking in German students: Prevalence, phenomenology, and associated characteristics. Behavioural Modifications, 26, 320–339. Cheung, F. M. (1998). Cross-cultural psychopathology. In A. S. Bellack & M. Hersen (Eds.), Comprehensive clinical psychology, vol. 10: Sociocultural and individual differences (pp. 35–51). Pergamon. Cobb, J. P., & Marks, I. M. (1979). Morbid jealousy featuring as obsessive-compulsive neurosis: Treatment by behavioural psychotherapy. British Journal of Psychiatry, 134, 301–305. DeSteno, D., Valdesolo, P., & Bartlett, M. Y. (2006). Jealousy and the threatened self: Getting to the heart of the green-eyed monster. Journal of Personality and Social Psychology, 91, 626–641. Diefenbach, G. J., Mouton-Odum, S., & Stanley, M. A. (2002). Affective correlates of trichotillomania. Behaviour Research and Therapy, 40, 1305–1315. Diefenbach, G. J., Tolin, D. F., Hannan, S., Crocetto, J., & Worhunsky, P. (2005). Trichotillomania: Impact on psychosocial functioning and quality of life. Behaviour Research and Therapy, 43, 869–884. Diefenbach, G. J., Tolin, D. F., Meunier, S., & Worhunsky, P. (2008). Emotion regulation and trichotillomania: A comparison of clinical and nonclinical hair pulling. Journal of Behavior Therapy and Experimental Psychiatry, 39, 32–41. Duke, D. C., Bodzin, D. K., Tavares, P., Geffken, G. R., & Storch, E. A. (2009). The phenomenology of hairpulling in a community sample. Journal of Anxiety Disorders, 23, 1118–1125. Dunkley, D. M., Zuroff, D. C., & Blankstein, K. R. (2006). Specific perfectionism components versus self-criticism in predicting maladjustment. Personality and Individual Differences, 40, 665–676. Ecker, W. (2012). Non-delusional pathological jealousy as an obsessive-compulsive spectrum disorder: Cognitive-behavioural conceptualization and some treatment suggestions. Journal of Obsessive-Compulsive and Related Disorders, 1, 203–210. Farmer, R. F., & Chapman, A. L. (2016). Behavioral interventions in cognitive behavior therapy: Practical guidance for putting theory into action. (2nd ed.). American Psychological Association. Flessner, C. A., Busch, A. M., Heideman, P. W., & Woods, D. W. (2008). Acceptanceenhanced behavior therapy (AEBT) for trichotillomania and chronic skin picking: Exploring the effects of component sequencing. Behavior Modification, 32, 579–594. Frost, R., & Steketee, G. (2002). Cognitive approaches to obsessions and compulsions: Theory, assessment and treatment. Elsevier. Gilbert, P., & Procter, S. (2006). Compassionate mind training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clinical Psychology and Psychotherapy, 13, 353–379. Gkika, S., & Wells, A. (2015). How to deal with negative thoughts? A preliminary comparison of detached mindfulness and thought evaluation in socially anxious individuals. Cognitive Therapy and Research, 39, 23–30. Gross, J. (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2, 271–299. Hayes, S. C., Levin, M. E., Plumb-Vilardaga, J., Villatte, J. L., & Pistorello, J. (2013). Acceptance and commitment therapy and contextual behavioral science: Examining the process of a distinctive model of behavioral and cognitive therapy. Behavior Therapy, 44, 180–198. Other Specified and Unspecified Obsessive-Compulsive and Related Disorders Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (2012). Acceptance and commitment therapy: The process and practice of mindful change (2nd ed.). Guilford Press. Herbert, J. D., & Forman, E. M. (2013). Caution: The differences between CT and ACT may be larger (and smaller) than they appear. Behavior Therapy, 44, 218–223. Johansson, A., Fareed, K., & Omar, R. (1991). Analysis of possible factors influencing the occurrence of occlusal tooth wear in a young Saudi population. Acta Odontologica Scandinavica, 49, 139–145. Kingham, M., & Gordon, H. (2004). Aspects of morbid jealousy. Advances in Psychiatric Treatment, 10, 207–215. Krejci, C. B. (2000). Self-inflicted gingival injury due to habitual fingernail biting. Journal of Periodontology, 71, 1029–1031. Labuschagne, I., Castle, D. J., Dunai, J., Kyrios, M., & Rossell, S. L. (2010). An examination of delusional thinking and cognitive styles in body dysmorphic disorder. Australian and New Zealand Journal of Psychiatry, 44, 706–712. Leahy, R. L. (2018). The jealousy cure: Learn to trust, overcome possessiveness, and save your relationship. New Harbinger. Leahy, R. L., & Tirch, D. D. (2008). Cognitive behavioral therapy for jealousy. International Journal of Cognitive Therapy, 1, 18–32. Mansueto, C. S., Thomas, A. M., & Brice, A. L. (2007). Hair pulling and its affective correlates in an African-American university sample. Journal of Anxiety Disorders, 21, 590–599. Mennin, D. S., Ellard, K. K., Fresco, D. M., & Gross, J. J. (2013). United we stand: Emphasizing commonalities across cognitive-behavioral therapies. Behavior Therapy, 44, 234–248. Morris, S. H., Zickgraf, H. F., Dingfelder, H. E., & Franklin, M. E. (2013). Habit reversal training in trichotillomania: Guide for the clinician. Expert Review of Neurotherapeutics, 13, 1069–1077. Neal-Barnett, A., & Stadulis, R. (2006). Affective states and racial identity among AfricanAmerican women with trichotillomania. Journal of the National Medical Association, 98, 753–757. Noble, C. L. (2012). The relationships among multidimensional perfectionism, shame and trichotillomania symptom severity. Dissertation Abstracts International: Section B: The Sciences and Engineer, 74(2-B(E)). O’Connor, K. (2002). A cognitive-behavioral/psychophysiological model of tic disorders. Behaviour Research and Therapy, 40, 1113–1142. O’Connor, K., Audet, J.-S., Julien, D., Aardema, F., Laverdure, A., & Lavoie, M. E. (2015). The style of planning action (STOP) questionnaire in OCD spectrum disorders. Personality and Individual Differences, 86(Supplement C), 25–32. O’Connor, K., Koszegi, N., Aardema, F., Van Niekerk, J., & Taillon, A. (2009). An inferencebased approach to treating obsessive-compulsive disorder. Cognitive and Behavioral Practice, 16, 420–429. O’Connor, K. P. (2005). Cognitive behavioral management of tic disorders. John Wiley & Sons. O’Connor, K. P., Aardema, F., & Pélissier, M.-C. (2005). Beyond reasonable doubt: Reasoning processes in obsessive compulsive disorder and related disorders. John Wiley & Sons. O’Connor, K. P., Brault, M., Robillard, S., Loiselle, J., Borgeat, F., & Stip, E. (2001). Evaluation of a cognitive-behavioural program for the management of chronic tic and habit disorders. Behaviour Research and Therapy, 39, 667–681. O’Connor, K. P., Lavoie, M. E., Robert, M., Stip, E., & Borgeat, F. (2005). Brain–behaviour relations during motor processing in chronic tic and habit disorder. Cognitive and Behavioral Neurology, 18, 79–88. O’Connor, K. P., Lavoie, M. E., & Schoendorff, B. (2017). Managing tic and habit disorders: A cognitive psychophysiological approach with acceptance strategies. Wiley-Blackwell. 293 294 Jan van Niekerk and Kieron O’Connor Pélissier, M.-C., & O’Connor, K. (2004). Cognitive-behavioural therapy of trichotillomania, targeting perfectionism. Clinical Case Studies, 3, 57–69. Penzel, F. (1995). Skin-picking and nail biting: Related habits. In Touch, 2, 1–10. Philips, C. B. (2009). Student portfolios and the hidden curricullum on gender: Mapping exclusion. Blackwell Publishing. Phillips, K. A., & Menard, W. (2011). Olfactory reference syndrome: Demographic and clinical features of imagined body odor. General Hospital Psychiatry, 33, 398–406. Roberts, S., O’Connor, K., Aardema, F., & Bélanger, C. (2015). The impact of emotions on body-focused repetitive behaviors: Evidence from a non-treatment-seeking sample. Journal of Behavior Therapy and Experimental Psychiatry, 46, 189–197. Roberts, S., O’Connor, K., & Bélanger, C. (2013). Emotion regulation and other psychological models for body-focused repetitive behaviors. Clinical Psychology Review, 33, 745–762. Salmon-Ehr, V., Mohn, C., & Bernard, P. (1999). Longitudinal melanonychia consecutive to nail biting. Annales de Dermatologie et de Vénéréologie, 126, 44–45. Schreiber, L., Odlaug, B. L., & Grant, J. E. (2011). Impulse control disorders: Updated review of clinical characteristics and pharmacological management. Frontiers in Psychiatry, 2, 1–11. Simpson, H. B., & Zuckoff, A. (2011). Using motivational interviewing to enhance treatment outcome in people with obsessive-compulsive disorder. Cognitive and Behavioral Practice, 1, 28–37. Taillon, A., O’Connor, K., Dupuis, G., & Lavoie, M. (2013). Inference-based therapy for body dysmorphic disorder. Clinical Psychology and Psychotherapy 20, 67–76. Teng, E. J., Woods, D. W., Marcks, B. A., & Twohig, M. P. (2004). Body-focused repetitive behaviors: The proximal and distal effects of affective variables on behavioral expression. Journal of Psychopathology and Behavioral Assessment, 26, 55–64. Thompson, R., & Zuroff, D. C. (2004). The Levels of Self-Criticism Scale: Comparative selfcriticism and internalized self-criticism. Personality and Individual Differences, 36, 419–430. Van Niekerk, J. (2018). A Clinician’s guide to treating OCD: The most effective CBT approaches for obsessive-compulsive disorder. New Harbinger. Veale, D., & Neziroglu, F. (2010). Body dysmorphic disorder: A treatment manual. Wiley. Weingarden, H., & Renshaw, K. D. (2015). Shame in the obsessive compulsive related disorders: A conceptual review. Journal of Affective Disorders, 15(171), 74–84. Wells, A. (2005). Detached mindfulness in cognitive therapy: A metacognitive analysis and ten techniques. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 23, 337–355. (2009). Metacognitive therapy for anxiety and depression. Guilford Press:. Wilhelm, S., Keuthen, N. J., Deckersbach, T., Engelhard, I. M., Forker, A. E., Baer, L., O’Sullivan, R. L., & Jenike, M. A. (1999). Self-injurious skin picking: Clinical characteristics and comorbidity. Journal of Clinical Psychiatry, 60, 454–459. Wilhelm, S., Phillips, K. A., & Steketee, G. (2013). Cognitive-behavioral therapy for body dysmorphic disorder: A treatment manual. Guilford Press. Williams, T. I., Rose, R., & Chisholm, S. (2007). What is the function of nail biting? An analog assessment study. Behavior Research and Therapy, 45, 989–995. Woods, D. W., Friman, P. C., & Teng, E. J. (2001). Physical and social impairment in persons with repetitive behavior disorders. In D. W. Woods & R. G. Miltenberger (Eds.), Tic disorders trichotillomania, and other repetitive behavior disorders: Behavioral approaches to analysis and treatment (pp. 33–52). Springer. Young, J. E., Klosko, J. S., & Weishaar, M. E. (2003). Schema therapy: A practitioner’s guide. Guilford Press. 15 A Cognitive Behavioral Approach to Body Dysmorphic Disorder: Assessment, Treatment, and New Developments Oliver Sündermann and David Veale Introduction Body dysmorphic disorder (BDD) is a condition that is characterized by a disabling preoccupation with a perceived defect in one’s normal physical appearance. BDD affects about 2% of the general population (Veale et al., 2016) with similar rates in men and women, but prevalence rates are much higher in clinical settings, particularly in dermatological clinics (11.3%), general cosmetic settings (13.2%), and rhinoplasty clinics (20%). The onset of BDD tends to be during adolescence, remains chronic if untreated, and is associated with poor quality of life, high risk, and significant impairment in school, interpersonal, and work domains (Angelakis et al., 2016; Bjornsson et al., 2013; Didie et al., 2012). Hospitalization is common, and clients often accumulate significant financial debt from cosmetic surgeries. Earlier onsets are associated with higher severity, comorbidity, and risk (Bjornsson et al., 2013). Suicidality is a grave concern (Angelakis et al., 2016) with rates of completed suicide around 45 times higher in BDD than in the general population (Phillips & Menard, 2006). BDD is both under-recognized and underreported. Shame and stigma are main treatment barriers (Marques et al., 2011), and those who seek help are often misdiagnosed (e.g., with social anxiety), have their difficulties minimized, or receive inappropriate and ineffective treatments. Diagnostic Criteria and Phenomenology The Diagnostic and Statistical Manual of Mental Disorders (DSM) lists in its fifth edition the following criteria for BDD: a preoccupation with one or more perceived flaws in physical appearance that are not or only slightly noticeable by others, for at least an hour a day; repetitive overt or covert compulsive behaviors (e.g., mirror checking, excessive grooming, reassurance seeking) or mental acts (e.g., comparing, rumination) in response to appearance concerns, causing significant distress or impairment, and appearance concerns are not better explained by concerns with body fat or weight. DSM-5 requires clinicians to specify whether the preoccupation 295 296 Oliver Sündermann and David Veale is better described as muscle dysmorphia, that is, a concern of too small or insufficient muscle mass, and to make a judgement about the person’s insight regarding the conviction of their BDD beliefs (e.g., ‘I am ugly’; ‘I am deformed’). Historically, BDD has been categorized as a somatoform disorder, because of its focus on the body. However, DSM-5 classifies BDD in a new chapter, ‘Obsessive-Compulsive and Related Disorders’ (OCRD), because of its similar comorbidity, family history, and phenomenology of obsessive-compulsive disorder and other difficulties that involve compulsive behaviors such as hoarding disorder or excoriation disorder. Other diagnostic changes include referring to the person’s ‘defects or flaws in appearance’ as ‘perceived’ and no longer as ‘imagined’ to better capture the person’s experience, and the inclusion of ‘repetitive behaviors’ as a characteristic BDD feature that describes the person’s response to the perceived defect. The focus here is on the form and content of the behavior rather than the function, and other typical BDD behaviors that are less compulsive and repetitive may not be adequately captured (e.g., seeking cosmetic surgery). Note that BDD is now also recognized as a separate disorder by the International Classification of Diseases (ICD) in its latest version ICD-11, linkcode 6B21 (https://icd.who.int/browse11/l-m/ en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f1321276661; see Veale & Matsunaga, 2014, for a description of the ICD-11 Working Group’s proposal on OCRD to revise the classification of BDD in ICD-11). All areas of the body can be the focus of concern, but usually people with BDD are most concerned about visible parts, especially their skin (e.g., perceived wrinkles, scarring, acne, or ‘too dark’), hair (e.g., perceived baldness, thinning, too straight, or ‘too curly’), and nose (e.g., shape and size) (Phillips et al., 2006), and the preoccupation is usually focused on several body parts. Other common concerns focus on body shape (e.g., hips, waist, stomach, or buttocks), size and structure of face (e.g., jaw or chin), or concerns of asymmetry (e.g., asymmetric eyes, jaw, or hairline); and sometimes complaints are non-specific (e.g., feeling ugly or ‘not right’). Although clinical features of BDD appear similar across different cultures and societies (Bohne et al., 2002; Cansever et al., 2003; Fontenelle et al., 2006), there is some indication that Asian people are more concerned with straight hair and dark skin, and have fewer body shape concerns than Caucasians (Marques et al., 2011), possibly reflecting ethnic differences in beauty ideals. However, there is a general lack of cross-cultural research of differences in phenomenology of appearance concerns, related coping, and prevalence rates in non-Western countries (Veale et al., 2016). Cognitive, Perceptual, and Attentional Processes in BDD Several processes and biases in attention and perception characterize BDD. For example, people with BDD tend to have a detailed rather than holistic processing of visual information (Deckersbach et al., 2000; Greenberg et al. 2014) and selectively attend to the perceived flaws and other people’s responses towards them. A key attentional process, albeit understudied, appears to be self-focused attention (Windheim et al., 2011) onto internal imagery of how the person feels they look A Cognitive Behavioral Approach to Body Dysmorphic Disorder to others. They are also more aesthetically sensitive to facial information than controls, similar to people in the art and design profession (Lambrou et al., 2011); have higher and more perfectionistic beauty standards (Buhlmann et al., 2002); and overvalue the importance of appearance and self-objectify more than those without BDD (Lambrou et al., 2012). People with BDD are more likely to misinterpret faces as contemptuous or angry in self-referent (‘He’s looking at me’) but not in otherreferent scenarios (‘He’s looking at someone else’) than controls (Buhlmann et al., 2006, 2004). Other distinct features involve the experience of frequent and more vivid intrusive body image–related imagery that is also more negatively judged (‘I’m ugly, disgusting’) compared with controls (Osman et al., 2004). Cognitive behavioral models of BDD propose that these biases contribute to appearance-related threat appraisals that drive safety-seeking behaviors (e.g., grooming and camouflaging), avoidance, and self-focused attention, which aim to reduce perceived appearance-related threats but maintain the disorder and are therefore the target in CBT. Evidence Base for Cognitive Behavioral Therapy Outcome research is limited, but an emerging evidence base supports CBT as the treatment of choice for BDD. A recent meta-analysis by Harrison et al. (2016; N = 7 RCTs) found CBT to be superior to wait-list or credible psychological placebo control groups in reducing BDD (d = 1.22), depressive symptoms, and insight/ delusionality (d = 0.56), with improvement of BDD likely to be maintained at least in the short term at 2–4 months follow-up, in line with previous meta-analyses (Ipser et al., 2009; Williams et al., 2006). No significant predictors of outcome were identified, and there is no clear empirical support for a particular modality of CBT. Only one RCT compared CBT with a credible psychological control condition, that is, anxiety management (Veale et al., 2014). Participants were largely white and Western; hence it is unclear if CBT is acceptable to other ethnic groups. Long-term outcome data are rare, but gains can be maintained for several years as shown in a recent naturalistic case series (Veale et al., 2015). Despite the growing evidence supporting CBT for BDD, there is an urgent need to improve and validate current treatment protocols. Many clients drop out of treatment or do not or only minimally benefit from CBT, and many continue to live with chronic symptoms (Veale et al., 2015). On average, only 40–54% of trial clients were classed as responders, with many still in the moderate to severe range posttreatment. Thus response rates to CBT for BDD are significantly lower than those found in CBT trials for OCD (Öst et al., 2015). Many clients find engaging with treatment too difficult, possibly due to poor insight into their BDD, low mood, or high risk (Harrison et al., 2016). Furthermore, it remains unclear for whom CBT works, how best to address comorbidity (Buhlmann et al., 2008), and how to adapt treatment for severe and complex cases (Sündermann & Veale, 2017). Finally, current CBT protocols for BDD predominantly focus on anxiety and therefore may be less efficacious in addressing other emotions such as shame, anger, or disgust (Cassiello-Robbins & Barlow, 2016; Sündermann et al., 2016). 297 298 Oliver Sündermann and David Veale Functional and Contextual Approach to BDD While the phenomenology of BDD is well described in terms of appearance-related belief content, attentional biases, and the nature of repetitive behaviors, less is understood about the function of BDD behaviors in relation to a perceived threat from distorted body imagery. Veale and Gilbert (2014) recently described the functional and contextual aspects of the phenomenology of BDD as part of threat-based strategies. Taking an evolutionary angle, the authors argue that all BDD processes and behaviors serve the function of averting social threat and keeping the person safe. For example, attentional biases and checking function as threat detection and monitoring; comparing with others and camouflaging appearance aim to monitor and avoid rejection, shame, and humiliation. Those who suffer from BDD have often experienced trauma and social threats in the form of shaming, bullying, humiliation, and rejection (Buhlmann et al., 2012; Weingarden et al., 2017), and therefore it is understandable that their thinking and coping styles are rooted and driven by these emotional aversive experiences. Veale and Gilbert (2014) suggest that CBT can be improved by developing a shared functional analysis of the functions and contexts of the person’s BDD and linking their body-related fears to more underlying fears of rejection, exclusion, and loneliness, as well as aversive relevant memories where appropriate. The authors consequently propose to complement CBT with compassion-focused interventions, but more research is needed to evaluate these. A Cognitive-Behavioral Model: The Self as an Aesthetic Object Veale and colleagues have developed a cognitive behavioral model of BDD that is centered on the concept of the self as an aesthetic object, which refers to the experience of extreme self-consciousness and self-focused attention on distorted images of their disliked features (Baldock & Veale, 2017; Veale, 2004). The model proposes that mental imagery in BDD is at least in part constructed from intrusive imagery based on past aversive experiences that is meaningfully linked with the person’s BDD, especially shame-based memories (e.g., of being bullied or being different). The ‘felt impression’ of how the person fears they look is predominantly visual, experienced from an observer perspective (Osman et al., 2004) and associated with negative appearance-related beliefs (e.g., ‘I am only acceptable if I look good’) and emotions, most notably, shame. It is proposed that the person becomes intensely self-focused on all aspects of this triangulated experience of appearancefocused imagery, beliefs, and emotions, which in turn leads the person to engage in safety-seeking and avoidance behaviors that serve the function of keeping the person safe through monitoring and averting appearance-related social threat (judgment, rejection) but that paradoxically maintain and often worsen their concerns through preventing disconfirmation of feared outcomes, increasing dissatisfaction, preoccupation, and isolation. The model has clinical implications and aims to help the person reframe their difficulties as a problem of preoccupation with appearance A Cognitive Behavioral Approach to Body Dysmorphic Disorder rather than actual appearance, stemming from mental imagery fused with past aversive memories conditioned to the person’s body image and maintained through their attempts to cope. Below we outline a CBT protocol for BDD, which is informed by the model of the self as an aesthetic object. Assessment and Treatment of Body Dysmorphic Disorder Overview The main aim, as with any CBT approach, is to gain a sound and shared understanding of how the person’s BDD developed and what maintains it. In most cases, CBT will be delivered on an outpatient basis for at least 16–20 weekly sessions, with sessions typically lasting between 45 and 90 minutes. More severe or complex cases may require ‘stepping up’ to specialist services. See Table 15.1 for a session-bysession breakdown. Screening for BDD People with BDD may not reveal the degree of their preoccupation unless asked directly because of shame about their appearance, which may also lead them to seek inappropriate help. Consider the following screening questions to identify appearance concerns: Some people are very bothered by the way they look. Is that a problem for you? If the answer is positive, explore further. What concerns do you have about your appearance? How noticeable do you think it is? (Is there a difference between their perceived defect and actual or between actual and their ideal?) On a typical day, how many hours per day is your appearance at the forefront of your mind? Do you think about your appearance a lot and wish you could think less about it? Do you have to check your appearance a lot? How many hours per day do you spend thinking about your appearance? Is it very distressing for you? Is there anything you avoid because of the way you feel about your appearance? Does it interfere with your ability to study or work? Does in interfere in dating or your relationship? Does it interfere in your social life? Brief validated self-report measures can also be helpful to screen for BDD (see Table 15.2), for example, the Body Image Disturbance Questionnaire (BIDQ) (Cash et al., 2004), the Dysmorphic Concern Questionnaire (DCQ) (Mancuso 299 300 Oliver Sündermann and David Veale Table 15.1. A cognitive behavioral therapy protocol for BDDa Session Therapy stage Key elements and aims 1–3 Assessment and formulation 4–10 Work phase 1 11–15 Work phase 2 Focus on engagement, be flexible about location (e.g., phone session, home visit) and allow camouflaging if required. Clarify hopes, expectations, motivation for treatment, readiness for change. Assess disliked feature, related beliefs, and coping behaviors (content, context, distress, appraisals, emotions). Provide psychoeducation and normalization of BDD experience (evolutionary functions, ‘better safe than sorry’). Assess BDD-related imagery. Theory A/Theory B: build alternative understanding of BDD as a problem with preoccupation (Theory B) rather than physical appearance (Theory A) Formulation: draw idiosyncratic version of client’s model: identify main trigger, appraisals, emotions, imagery, and coping responses and cognitive processes; discuss the function and unintended consequences of these; and, where possible, link to early experiences (e.g., bullying, overvaluation of appearance in family). Involve key significant others (e.g., partner, parents) where appropriate. Imagery rescripting (if indicated) of relevant early experiences. This is usually done at the beginning of treatment. Behavioral experiments and exposures in session, off-site (if feasible) with the aim to resist/reduce safety-seeking behaviors (SSBs). Conduct behavioral experiments with or without SSBs to determine the effect on self-consciousness and frequency of BDD thoughts. Relate all therapy work to Theory A/Theory B and obtain regular belief ratings for both theories. Functional analysis of cognitive processes (e.g., ruminating, comparing, self-focused attention) through building awareness and labeling of these; discuss function of these and their unintended consequences and develop alternatives to them (e.g., focusing outwards, self-compassion). Mirror retraining (identify motivation for mirror checking, criteria for termination, practice viewing holistically focusing on whole body from a distance). Practice refocusing of attention away from self (e.g., by attending/ listening to environmental cues). Target beliefs about appearance using CBT techniques (e.g., Big ‘I’, Little ‘i’, overidentification of self with appearance, etc.). Address perfectionism if person has unrelenting high standards; identify criteria for ‘perfect looks’ (often subjective feeling–based, ‘just right’). Compassion-focused interventions, e.g., safe imagery exercises, mindful breathing, compassionate letter writing. Space out sessions to agreed frequency, e.g., biweekly, monthly. More emphasis on independent planned exposures: ‘Client becoming their own therapist’. Generalization of experiments/exposures Review of treatment Dealing with setbacks Blueprint (‘Staying well plan’) Review of progress 16 and 17 Termination 18–20 a Follow-up Protocol should be adapted according to severity, complexity, heterogeneity of BDD, and availability of resources. A Cognitive Behavioral Approach to Body Dysmorphic Disorder et al., 2010), or the Cosmetic Procedure Screening Questionnaire (COPS) (Veale et al., 2012). Challenges in Engaging Clients in Assessment and Therapy Clinicians face a number of challenges when working with clients suffering from BDD, especially in the initial assessment phase. These commonly involve clients having poor insight into their BDD, and thus they may not be motivated to engage with a psychological way of working. Often clients are brought or sent for an assessment by someone else, such as a family member, friend, or cosmetic surgeon. Those with strong delusional and fixed ideas about their problem being physical in nature (rather than psychological) may not believe that the interviewer can understand their problem or help in a meaningful way. Compared with mental health assessments of other disorders, it is pivotal to spend extra time on rapport building, motivational interviewing to address ambivalence (e.g., about the pros and cons of treatment or their quality of life with no treatment), as otherwise the client may disengage. Clients should be allowed to camouflage during the assessment (e.g., to hide their face), and clinicians should be flexible about where and how to see the client (e.g., Skype or Zoom sessions if the client feels unable to leave their house). Be transparent about the diagnosis and provide this with a good psychological explanation of what the problem is, including the concept of ‘body image’, which we explain to clients as ‘not just being a photo on the back of your eye, but is constructed by our brain based on thoughts, feelings, and past aversive experiences’. The way the person uses mirrors to check their disliked feature also contributes to distorted body imagery, for example, by using a magnifying glass to check for pimples, or close-up examinations. Some professionals, especially when inexperienced with BDD or those with negative beliefs about the condition, can be dismissive of the client’s concerns (e.g., ‘You look fine’) and of course this is likely to aggravate the client’s distress. We strongly recommend not to argue or debate with clients about their disliked feature, overvalued ideas of appearance, or their diagnosis but instead maintain an ‘inquiring’ stance and focus on validating feelings of shame and distress. In the case of slight visible differences (e.g., mild acne), it can be helpful to acknowledge that their concern is minimally noticeable and the interviewer may emphasize that they can see what the client is describing only when ‘taking a very close up look and raising my aesthetic standards’. Assessment of Disliked Feature(s), Appearance-Related Beliefs, and Coping A good starting point is to ask the client to describe the features of their body they dislike or would like to improve. Ask specifically whether the client is motivated to seek a medical procedure such as dermatological treatment or cosmetic surgery. For example, if the concern is regarding the size or shape of the nose, ask whether the client is motivated to have rhinoplasty or has undergone surgery in the past. In case the client is preoccupied with several areas of their body, it is helpful to ask the 301 302 Oliver Sündermann and David Veale Box 1 Common safety-seeking behaviors in people with BDD Mirror gazing or avoiding mirrors Checking perceived defect, inspecting, touching or measuring it Comparing self with others or to old photographs Grooming behaviors, e.g., combing, smoothening, straightening, plucking, or cutting hair Camouflaging rituals (e.g., make-up, scarves, hats, oversized clothes) Skin cleaning, picking, face peeling, scrubbing, or bleaching Trying to convince others that defect exists Facial exercises, e.g., practicing showing the ‘best face’ Monitoring other people’s reactions and eye movement Controlling body posture to avoid showing ‘defect’ client to draw out a pie chart adding up the percentages of concern for each feature. Ask to estimate how much time they spend thinking on average about each feature during the day, how much distress their preoccupation causes them, and how much they are impaired in the various domains of functioning such as relationships, friendships, and work. If the client is not in a romantic relationship, assess the extent their condition has on potential future relationships, for example, would they avoid meeting someone new because of their appearance-related distress, or could not enjoy sexual activity because of their BDD. Elicit a detailed list of activities and situations the client avoids because of their preoccupation, and discuss all appearance-related coping behaviors, their function, and unintended consequences. Box 1 contains a list of typical safety-seeking behaviors. Self-report measures and observer-rated scales such as the BDD-YBOCS are recommended to complement the assessment (see Table 15.3 below). The therapist should also probe for typical coping behaviors if these are not volunteered (e.g., mirror checking) and normalize accordingly, that is, as an understandable response to appearance distress. A helpful way of capturing a sense of the client’s felt impression is by asking the client to draw a self-portrait of how they think their perceived defect appears to others. The emphasis is explicitly not on artistic skills, but instead the client is instructed to draw a portrait from the picture in their mind or impression that they have of their disliked feature. Pre- and post-treatment self-portraits of successful CBT for BDD can impressively visualize the change in the person’s experience of their body image (see Sündermann et al., 2016). Engagement: Theory A/Theory B The main purpose of the initial treatment stage is to socialize and engage the client into a psychological way of thinking about their problem. ‘Theory A/Theory B’ (see Table 15.2) is a helpful technique to introduce a psychological approach to BDD and proposes to the client two fundamentally different accounts of their difficulties. A Cognitive Behavioral Approach to Body Dysmorphic Disorder 303 Table 15.2. Worksheet for Theory A/Theory B with example of client suffering from a preoccupation with balding hair Theory A (appearance problem) ‘My problem is that I am balding and that my hairline is receding, which makes me look ugly and inferior to other men, and means that I’ll never be able to have a romantic relationship.’ Theory B (preoccupation problem) ‘My problem is that I am preoccupied with hair loss, which makes me excessively self-conscious and constantly worry that I am inferior.’ What do I need to do if Theory A is true? Camouflage, particularly through using my hat. Avoid all situations where I need to take off my hat. Avoid bright lights, and spend more time in low lights. Compare myself with others who have ‘better’ hair. Worry ‘what if’’ a hair transplant does not work. Focus attention on my hair and monitor people’s response to it. Drink alcohol to avoid thinking about my baldness. What do I need to do if Theory B is true? Live my life in accordance with my values, in particular: If this is true, what does it say about the future? The future would be dark and grim, and I will be lonely forever. If this is true, what does it say about the future? I would feel optimistic and hopeful. I would be able to have relationships, work, and live a meaningful life. Get a job. Pursue a relationship. Socialize with friends. Spend time outside in the sun. Do all of these activities without engaging in safetyseeking behaviors. Theory A encompasses their beliefs about BDD and states that their problem is an actual appearance problem (e.g., ‘My problem is that my nose is deformed, which makes me look disgusting’). As such, Theory A is the theory according to which they had been living their life, and which suggests to ‘solve’ the problem accordingly, for example, camouflage, avoid, seek cosmetic surgery. The therapist gently suggests that these ‘solutions’ have become their actual problem, because they keep them stuck and maintain a poor quality of life. Hence, if the client continued to live their life according to Theory A, the future is very grim. Subsequently, the therapist explains Theory B, an alternative account of their difficulties stating that the problem is one of preoccupation with appearance rather than an actual appearance flaw (e.g., ‘My problem is that I am preoccupied with my nose not being “right”, and that I worry others will not like me’), suggesting that the preoccupation with appearance may stem from an emotional issue (i.e., BDD). The therapist then discusses what the client needs to do if their problem were indeed one of preoccupation. This usually elicits responses of doing the ‘opposite’ to Theory A behaviors, and acting and living by their values. Of course, Theory B has more benign and hopeful implications for the client’s life and future. The clinician might also ask whether they noticed that solving their difficulties as an appearance problem actually increases their distress and preoccupation. Clients may be quick to express doubts about Theory B or may not be willing to engage with the idea of an alternative theory of their problem, particularly when appearance-related beliefs are fixed. The clinician should normalize any doubts as understandable responses arising from their BDD, while inviting the client to test out whether Theory B better 304 Oliver Sündermann and David Veale fits their experiences. The therapist may also propose to the client that they can always go back to Theory A if therapy does not work for them, while stressing that only by acting in reverse to Theory A can they truly test out and experience whether their difficulties fit better with the idea of a preoccupation problem. Once both theories are drawn out, belief ratings should be obtained. Theory A/Theory B should serve as a framework for discussing all therapy-related tasks and the resulting client’s experience in subsequent sessions. Cognitive Behavioral Treatment of BDD Overview CBT for BDD helps the client to build up evidence for Theory B through testing out fears and expectations without avoidance and safety-seeking behaviors. BDD behaviors that are performed in private (e.g., mirror checking, comparing) are usually targeted first. Early goals in therapy usually involve reducing self-focused attention and linking BDD behaviors with heightened preoccupation. If indicated, relevant early adverse experiences (e.g., appearance-related bullying) should be processed as soon as possible. We also recommend building up self-compassion and self-soothing skills. Similar to other CBT approaches, we emphasize therapy as a ‘doing’ treatment, with the client taking responsibility for their recovery through increasing independence in conducting experiments as treatment progresses. Treatment outcome should be monitored using BDD-specific self-report measures (e.g., Appearance Anxiety Inventory [AAI]; Veale et al., 2014). Formulation and Treatment To illustrate our treatment protocol, we present the case of Tom, who attended outpatient sessions with one of the authors. Case vignette: Tom. Tom was a 20-year-old student who suffered from severe BDD characterized by a preoccupation with height (‘being too short’), and his nose (‘too large’). He had received 24 therapy sessions, some of them remotely via Skype. His main preoccupation was about his height (50 700 ), which he felt made him unattractive, inferior, and less of a man. He was also preoccupied with his nose being too large in proportion to his face, and he worried that it would project too much especially on the side profile. His appearance distress severely affected his quality of life, interfered with romantic relationships, and impaired his academic performance. He was constantly triggered by his own intrusive thoughts of not being tall enough, catching a glimpse of himself in reflective surfaces (e.g., cycling past cars), and seeing taller men. When triggered he experienced a felt impression of a shrunken, dwarf-like man worthy of ridicule and pity from women. Tom engaged in numerous avoidance and safety-seeking behaviors, such as wearing insoles to increase his height, avoiding bright lights, monitoring his body posture and A Cognitive Behavioral Approach to Body Dysmorphic Disorder straightening his back to appear taller, binge drinking on social occasions, researching risky leg-lengthening surgical procedures, and performing mental surgery imagining a positive outcome of the procedure. He also relentlessly compared himself unfavourably to taller men and sought constant reassurance from his mother while simultaneously trying to convince her of the severity of his physical flaws. Tom constantly checked the shape of his nose with his finger, and recorded daily videos of himself, which he stored to ‘keep track of his progress’. From a young age Tom had unrelenting high and perfectionistic academic standards and always saw good grades as his main compensatory ‘asset’ (‘I’m short, but at least I’m smart’). His preoccupation ignited in early adolescence following a number of comments from his aunt, who compared Tom unfavourably with his ‘attractive’ brother. Various comments made by women about not wanting to be with ‘short’ men as well as some dating profiles stating ‘I would not date a man shorter than me’ seemed solid proof of his overvalued ideas about the importance of appearance, especially height. His BDD deteriorated when he felt rejected by a woman, after which he sought professional help. CBT Formulation for BDD Case formulation for BDD should comprise a developmental part, linking the client’s BDD to past adverse experiences, and a cross-sectional part, showing how the felt impression, related appraisals, and emotions drive coping behaviors that maintain the current preoccupation. The case formulation presented here is derived from Veale’s model of the self as an aesthetic object (Veale, 2004), and is shown in Figure 15.1. We have adapted the diagram from Baldock and Veale (2017) by including past-present links between relevant shame-based experiences and the client’s current felt impression. Each coping behavior is noted in one of the petals of the vicious flower, and the therapist should discuss the intended function of each behavior and the related unintended consequences. For example, Tom was constantly comparing himself with taller men, which served the function of monitoring threat and establishing his place in the social hierarchy, but it also increased his preoccupation, self-consciousness, and distress. Researching leg lengthening surgeries gave him momentary glimmers of hope but was quickly overridden with despair when realizing that he could not afford it, and also triggered guilt for considering ‘wasting money’. Self-recorded videos were driven by the hope of looking better than he thought, but usually made him feel worse about his appearance. Excessive alcohol consumption allowed him to socialize but included the cost of memory loss, triggering prolonged mental reviewing and self-doubt. Although Eric initially held firm beliefs about Theory A, he found several aspects of his formulation allowed him to think more flexibly about his BDD. First, he agreed that his coping strategies increased his preoccupation and as such were ‘the problem, instead of the solution’. Understanding his BDD developmentally as a plausible response to feeling body shame when he was bullied and received comments critical of appearance (e.g., a teacher called him ‘tiny’) made him doubt that he would have developed BDD without such experiences (suggesting his difficulties were emotional rather than 305 306 Oliver Sündermann and David Veale Relevant early experiences • 6 years: Overvaluation of appearance in family, compared unfavorably with brother • 13–15 years: Appearance-related bullying in school (‘you are tiny’, ‘short’) • 17–20 years: Overheard derogatory comments by women about male height Appearance-related beliefs ‘Only tall men are sexually attractive and will find a partner’ ‘I am short and laughable, and destined to be alone and ridiculed’ ‘Appearance is everything’ Avoidance Staying indoors, avoiding social situations: binge drinking when out to numb/avoid feelings of shame Trigger Social situations Taller men, Own reflections Self-focused attention Constant and intense self-focus on felt impression Unintended consequences: Relying on internal information on how I feel I look; feeling selfconscious and can’t engage with others Unintended cosequences: Feeling alienated and lonely Can’t disconfirm that people don’t joke about me Attempts to correct Researching and fantasizing about leg surgery and rhinoplasty Unintended consequences Heightened preoccupation, increased despair and hopelessness Meaning and past associations I am less of a man; laughable, powerless, and disgusting Image/felt impression Impression of self as a dwarf, with a crooked, oversized nose Cover/hide features Wearing insoles to gain height; carefully adjust posture to avoid showing profile Unintended consequences More self-conscious about my height; feel link a ‘fraud’, worry about ‘being found out’ Figure 15.1. Case formulation. Emotions Shame, sadness, anger (selfdirected for not being taller) Comparing/rumination Relentlessly comparing unfavorably will other men; constant rumination why I was born short Unintended consequences Fuels my preoccupation, makes me feel hopeless, inferior, and depressed Checking Check by touch (feeling nose); video-recording of self, uploading and storing it, and mirror checks driven by hope to look better than felt impression Unintended consequences Feeling more hopeless and preoccupied A Cognitive Behavioral Approach to Body Dysmorphic Disorder physical). The formulation should be reviewed regularly and adapted as new information emerges in therapy. For example, in Tom’s case we did not learn until session 10 that high academic achievements served as a powerful way of dealing with feeling ugly and inferior (‘at least I have good grades’). When his BDD interfered with university performance, this aggravated his vicious cycle of selfdepreciating hostile thoughts, preoccupation, and hopelessness. Cognitive Behavioral Work: Addressing Beliefs about Appearance Based on the formulation, therapist and client agree on a hierarchy of avoided situations, coping behaviors, and processes to target (e.g., comparing, rumination, self-focused attention), always with a view of testing out Theory B and building a more helpful perspective of the client’s distress. Similar to CBT for OCD, behavioral tasks should be designed according to inhibitory learning principles (Craske et al., 2014), that is, maximizing violation of expectancies, repetition, generalizing to different contexts, and affect labelling. Beliefs about being judged for one’s appearance are often not testable in a credible way (‘Others are too nice to tell me how ugly I am’) and, in fact, can be counterproductive; for example, the client asking others directly what they think about their looks is likely to backfire because it may evoke anger for feeling dismissed or not understood. Therefore, predictions of experiments tend to focus more on tolerance of distress and building up confidence in social situations. For example, Tom predicted that by going out without wearing his insoles, his friends (and also strangers) would pity or tease him for being short; however, he believed that while they would surely judge him, they would not reveal their true judgements. However, he agreed to test out whether he would be able to tolerate and ‘survive’ without them. To his surprise, he was able to attend a party without his insoles and – importantly – without drinking alcohol. He was convinced that he was negatively evaluated, but as the evening progressed he became less selfconscious and learned that he could be more confident than he thought. Clients can be judicious with their use of safety-seeking behaviors in the early stages of treatment. For example, while Tom was able to remove his insoles, he initially could do so only with his ‘safe’ shoes, namely, his boots with thicker soles. Clients should be encouraged to always reflect on their learning and stimulate alternative explanations (that usually fit better with Theory B). Even though Tom’s strong beliefs about the importance of height were initially unshakable, he was able to reflect that his fluctuating levels of preoccupation fitted better with Theory B, suggesting his problems were emotional in nature. Mirror Retraining Mirror retraining is a standard component of CBT for BDD, and has the purpose of helping the client to develop a healthier and more functional relationship with mirrors and reflective surfaces. First, therapist and client should discuss and understand the motivation for mirror checks. Mirror gazing is often driven by the hope of not looking as bad as the client fears, coupled with a belief that they would feel 307 308 Oliver Sündermann and David Veale worse if they resisted (Veale & Riley, 2001). Common BDD behaviors often performed in front of the mirror involve skin picking, cleaning or removing perceived blemishes, facial exercises, or make-up and camouflaging rituals. Many patients carry pocket mirrors with them or use magnifying mirrors, and should be encouraged to desist. The actual steps of mirror retraining involve cutting down on frequency and duration of mirror usage and addressing the way mirrors are used. Instead of zooming in on perceived flaws, which magnifies the felt impression, clients are encouraged to step back, using larger mirrors to view themselves briefly and holistically. They are encouraged to scan their whole body from a slight distance while purposefully focusing outwards on external reflections, rather than internal feelings. A helpful experiment can be for the client to compare their level of preoccupation when using the mirror in a dysfunctional way and in a healthy way. Results can be used to strengthen conviction in Theory B. Patients often dissociate or ‘get stuck’ in front of the mirror and lose sense of time. Sometimes skin-picking or other mirror-based rituals serve additional functions, such as purposefully bringing on dissociative states to tolerate difficult memories or to avoid difficult feelings. Imagery Rescripting Imagery rescripting (ImRs) is indicated when the person’s sense of threat is associated with aversive memories. ImRs aims to change the meaning of past childhood events that continue to shape the person’s experience (Arntz, 2011) through processing and re-evaluating them. The felt impression of a person with BDD is often fused with imagery arising from shame-based memories of being teased, bullied, or humiliated. This is also reflected in clients’ reporting that, when triggered, they feel as young as when they were shamed as a child about their appearance. It is not uncommon for clients to become less avoidant of social situations yet continue to feel ugly. Old feelings of shame become easily triggered despite knowing that others may not judge them. Clients who continue to be affected by ‘ghosts from the past’ should receive ImRs as early as possible in treatment. The protocol we use is briefly outlined in Box 2, and follows the steps originally described by Arntz and colleagues (Arntz & Weertman, 1999) and adapted by Willson et al. (2016) for BDD. Unlike trauma reliving, it is not necessary to go over moments of peak distress. Also, the therapist can ask the client to pause before the scene changes to its worst point. The rationale of ImRs should be discussed beforehand, using metaphors such Box 2 Imagery Rescripting for BDD Stage 1: The client relives the image from the child’s perspective, and describes their needs that were not met at the time. Stage 2: The client enters the scene as an adult to provide the child’s needs and provide a different perspective Stage 3: The client returns to the image as a child with the adult self present at the scene to determine if all needs have been met. A Cognitive Behavioral Approach to Body Dysmorphic Disorder as ‘mental time travel’ to gain a different view on their experience (rather than changing what happened). Metaphors from trauma-focused CBT can be used to explain the aim of processing memories to contextualize them (Stott et al., 2010). ImRs proved useful in Tom’s treatment. He rescripted several key events linked with the emotional origins of his BDD. For example, Tom’s aunt used to compare his appearance as a six-year-old child unfavourably to his older brother, which was deeply shaming. The body shame experienced back then conditioned his presentday body image. Through rescripting, Tom was able to ‘stand up to my aunt, tell her off and make my younger self feel safe’, thus successfully processing old feelings of shame. The benefits were clearly noticeable. Tom was less frequently triggered, and when he was, he felt older, was less focused on his internal impressions, and was more able to tolerate distress. ImRs should be conducted alongside stimulus discrimination to further contextualize past experiences. This involves focusing on as many details as possible that discriminate the past from the here and now. Tom learned to be more mindful when triggered and was able to compassionately remind himself that the present is very different from the past and that he was safe. Self-Soothing and Compassionate Therapy Interventions Clients with BDD commonly suffer from self-deprecating thoughts and rumination, with the emotional tone of their inner voice being hostile and threat-based (‘It’s your own fault that you are ugly’). Compassion-focused interventions are therefore recommended to complement CBT for BDD to help de-shame the client’s experience (Veale & Gilbert, 2014). A key compassion intervention is psychoeducation about how our brains have evolved and how they are designed to keep us safe (‘better safe than sorry’). The therapist can explain how our old brain and our new brain can get caught in tricky loops, with the old brain alerting to social threat, and the new brain ruminating in an effort to solve the ‘appearance problem’. The therapist highlights that the way brains process threat is a design problem, and therefore not the client’s fault (albeit the client is responsible for change). The therapist should not label the client’s thinking style as ‘distorted’ or ‘biased’ because clients may perceive it as blaming (‘It’s my fault that I am thinking wrongly’). Instead, the therapist may say, ‘It is very understandable that you became preoccupied with height when you were teased in school, and the impression has stayed with you.’ Hence, the emphasis is on responsibility for change, which includes empathic understanding of how their problems developed and are maintained, as well as the importance of testing out an alternative view. Many clients find this evolutionary explanation de-shaming and motivating. Furthermore, practical exercises are recommended to build skills in self-compassion and self-soothing. This includes safe imagery exercises, compassionate breathing, and compassionate letter writing. BDD Measures for Screening, Diagnosing, and Outcome A range of BDD assessment measures is available for screening purposes, aiding diagnosis, and monitoring treatment outcome. Table 15.3 gives an overview of a 309 310 Downloaded from https://www.cambridge.org/core, on subject to the Cambridge Core terms of use, available at https://www.cambridge.org/core/terms. https://doi.org/10.1017/9781108355605.018 Table 15.3. Assessment measures for BDD Type of measure Function of measure Body Dysmorphic Disorder Questionnaire (BDDQ) Self-report Screens for BDD Body Image Disturbance Questionnaire (BIDQ) Self-report Screens for BDD dimensional Cosmetic Procedure Screening (COPS) Self-report Screens for BDD severity Dysmorphic Concern Questionnaire (DCQ) Self-report Screens for BDD Structured Clinical Interview for DSM-5 (SCID-5), BDD module Body Dysmorphic Disorder Diagnostic Module Brown Assessment of Beliefs Scale (BABS) Semi-structured Clinician-rated Semi-structured Clinician-rated Semi-structured Clinician-rated Diagnoses BDD Yale–Brown Obsessive Compulsive Scale modified for BDD (BDD-YBOCS) Semi-structured Clinician-rated Severity of BDD Appearance Anxiety Inventory (AAI) Self-report Body Image Quality of Life Inventory (BIQL) Self-report Assesses BDDprocesses and behaviors Monitoring progress Quality of life Name of measure Screening Diagnostic Outcome / severity Diagnoses BDD Insight into BDD Description Reference One to four items of yes/no questions mapping DSM criteria for BDD; maximum score of 4 suggests likely diagnosis of BDD Seven items derived from BDDQ; five-point Likert scale, with higher scores indicating greater body image disturbance Nine items scored from 0 to 8, with high scores indicating severity of BDD. Scores above 40 reflect a likely diagnosis of BDD Seven items assessing cognitive and behavioral symptoms of BDD, sum scores ranging from 0 to 21, with scores above 9 indicating possible BDD Maps onto the DSM-5 criteria for BDD; also allows diagnosis of muscle dysmorphia Five-item measure, which also allows diagnosis of muscle dysmorphia Seven-item scale measuring the strength of conviction in a belief. Items are rated from 0 to 4, with scores of 18 or above indicating delusional BDD Twelve-item scale, ranging from 0 to 48, with higher scores indicating increased severity of BDD; widely seen as the ‘gold standard’ outcome measure for BDD Ten-item questionnaire ranging from 0 to 4, measures frequency of avoidance behavior and threat-monitoring that are characteristic of a response to a distorted body image; ideal for tracking progress Nineteen items measuring impact of body image concerns on various life domains, using a sevenpoint scale (3 to +3) ranging from negative to positive, with lower scores reflecting a more negative impact. K. A. Phillips (1996) Cash et al. (2004) Veale et al. (2012) Mancuso et al. (2010) First et al. 2002 K. A. Phillips (2005) Eisen et al. (1998) K. A. Phillips et al., 2014 Veale et al., 2014 Cash & Fleming, 2002 A Cognitive Behavioral Approach to Body Dysmorphic Disorder selection of measures we use in our services. Screening measures can help in identifying BDD and prompting further BDD-specific assessments. The diagnostic process should include the use of validated clinician-rated semi-structured interviews such as the Structured Clinical Interview for DSM-5 (SCID-5) for BDD. The Brown Assessment of Beliefs Scale (BABS) is commonly used to gauge the level of insight a person has into their BDD. The Yale–Brown Obsessive Compulsive Scale (Y-BOCS) modified for BDD remains the ‘gold standard’ outcome measure and is typically used pre- and post-therapy to ascertain severity of BDD. Specialist clinics are likely to use the Y-BOCS modified for BDD, as it is also required by many funding panels to determine eligibility for accessing higher-level care services. We strongly advocate using BDD-specific measures to monitor treatment progress. For example, the Appearance Anxiety Inventory (AAI) provides a brief 10-item measure of the most common BDD avoidance and threat monitoring processes and behaviors that are characteristic of a response to a distorted body image. Thus, the AAI provides a helpful process measure that enables effective monitoring of treatment progress, and should be used in conjunction with more generic mood, anxiety, quality of life, and function measures. We strongly recommend incorporating these actively into treatment and jointly reviewing them with the client. Conclusion CBT is the treatment of choice for BDD. This chapter has outlined the key principles of effective delivery of CBT for BDD. Key principles include formulating BDD as a body image problem that has developed in response to shaming experiences, is maintained through avoidance and threat, is further maintained through monitoring behaviors that aim to protect the person from rejection and judgement, but have the unintended consequences of increasing preoccupation. Conceptualizing BDD within a contextual and evolutionary framework can be normalizing, engaging, and de-shaming. Compassion-focused interventions can complement CBT and give the client courage to test out an alternative understanding of their problem (Theory B). Additionally, they can reduce the inner critique and aid development of competency in relating more compassionately to self and others. ImRs is indicated when past aversive memories continue to shape the person’s experiences. Key Learning Points BDD is a common but under-recognized and under-reported problem. The treatment of choice for BDD is CBT, but only 50% make a satisfactory recovery. Engagement into treatment can be challenging, particularly when insight is low. Theory A/Theory B provides a helpful framework to socialize clients into therapy. 311 312 Oliver Sündermann and David Veale (cont.) Treatment aims to build a more helpful perspective of appearance distress (Theory B) through exposure tasks and behavioral experiments. Understanding functional and contextual aspects of BDD may enhance engagement and treatment outcome. Imagery rescripting and compassion-focused techniques can help to process related past aversive experiences. RECOMMENDED READING Phillips, K. A. (2005). The broken mirror: Understanding and treating body dysmorphic disorder. Oxford University Press. (2017). Body dysmorphic disorder: Advances in research and clinical practice. Oxford University Press. Sündermann, O., & Veale, D. (2017). Complexity in obsessive-compulsive and body dysmorphic disorder: A functional approach to complex difficulties. The Cognitive Behaviour Therapist, 10. Veale, D., & Gilbert, P. (2014). Body dysmorphic disorder: The functional and evolutionary context in phenomenology and a compassionate mind. Journal of Obsessive-Compulsive and Related Disorders, 3(2), 150–160. Veale, D., Gilbert, P., Wheatley, J., & Naismith, I. (2014). A new therapeutic community: Development of a compassion-focussed and contextual behavioural environment. Clinical Psychology and Psychotherapy, 22(4), 285–303. Veale, D., & Neziroglu, F. (2010). Body dysmorphic disorder: A treatment manual. John Wiley and Sons. Veale, D., Willson, R., & Clark, A. (2009). Overcoming body image problems including body dysmorphic disorder. Constable Robinson. Wilhelm, S., Phillips, K. A., & Steketee, G. (2012). Cognitive-behavioral therapy for body dysmorphic disorder: A treatment manual. Guilford Press. REFERENCES Angelakis, I., Gooding, P. A., & Panagioti, M. (2016). Suicidality in body dysmorphic disorder (BDD): A systematic review with meta-analysis. Clinical Psychology Review, 49, 55–66. Arntz, A. (2011). Imagery rescripting for personality disorders. Cognitive and Behavioral Practice, 18(4), 466–481. Arntz, A., & Weertman, A. (1999). Treatment of childhood memories: Theory and practice. Behaviour Research and Therapy, 37(8), 715–740. doi:10.1016/S0005-7967(98)00173-9 Baldock, E., & Veale, D. (2017). The self as an aesthetic object: Body image, beliefs about the self, and shame in a cognitive-behavioural model of body dysmorphic disorder. In Body dysmorphic disorder: Advances in research and clinical practice. Oxford University Press. Bjornsson, A. S., Didie, E. R., Grant, J. E., Menard, W., Stalker, E., & Phillips, K. A. (2013). Age at onset and clinical correlates in body dysmorphic disorder. Comprehensive Psychiatry, 54(7), 893–903. A Cognitive Behavioral Approach to Body Dysmorphic Disorder Bohne, A., Keuthen, N. J., Wilhelm, S., Deckersbach, T., & Jenike, M. A. (2002). Prevalence of symptoms of body dysmorphic disorder and its correlates: A cross-cultural comparison. Psychosomatics, 43(6), 486–490. Buhlmann, U., Etcoff, N. L., & Wilhelm, S. (2006). Emotion recognition bias for contempt and anger in body dysmorphic disorder. Journal of Psychiatric Research, 40(2), 105–111. Buhlmann, U., Marques, L. M., & Wilhelm, S. (2012). Traumatic experiences in individuals with body dysmorphic disorder. The Journal of Nervous and Mental Disease, 200(1), 95–98. Buhlmann, U., McNally, R. J., Etcoff, N. L., Tuschen-Caffier, B., & Wilhelm, S. (2004). Emotion recognition deficits in body dysmorphic disorder. Journal of Psychiatric Research, 38(2), 201–206. Buhlmann, U., McNally, R. J., Wilhelm, S., & Florin, I. (2002). Selective processing of emotional information in body dysmorphic disorder. Journal of Anxiety Disorders, 16(3), 289–298. Buhlmann, U., Reese, H. E., Renaud, S., & Wilhelm, S. (2008). Clinical considerations for the treatment of body dysmorphic disorder with cognitive-behavioral therapy. Body Image, 5(1), 39–49. Cansever, A., Uzun, Ö., Dönmez, E., & Özşahin, A. (2003). The prevalence and clinical features of body dysmorphic disorder in college students: A study in a Turkish sample. Comprehensive Psychiatry, 44(1), 60–64. Cash, T. F., & Fleming, E. C. (2002). The impact of body image experiences: Development of the Body Image Quality of Life Inventory. International Journal of Eating Disorders, 31(4), 455–460. Cash, T. F., Phillips, K. A., Santos, M. T., & Hrabosky, J. I. (2004). Measuring ‘negative body image’: Validation of the Body Image Disturbance Questionnaire in a nonclinical population. Body Image, 1(4), 363–372. Cassiello-Robbins, C., & Barlow, D. H. (2016). Anger: The unrecognized emotion in emotional disorders. Clinical Psychology: Science and Practice, 23(1), 66–85. doi:10.1111/ cpsp.12139 Craske, M. G., Treanor, M., Conway, C. C., Zbozinek, T., & Vervliet, B. (2014). Maximizing exposure therapy: An inhibitory learning approach. Behaviour Research and Therapy, 58, 10–23. Deckersbach, T., Savage, C. R., Phillips, K. A., Wilhelm, S., Buhlmann, U., Rauch, S. L., . . . & Jenike, M. A. (2000). Characteristics of memory dysfunction in body dysmorphic disorder. Journal of the International Neuropsychological Society, 6(6), 673–681. Didie, E. R., Loerke, E. H., Howes, S. E., & Phillips, K. A. (2012). Severity of interpersonal problems in individuals with body dysmorphic disorder. Journal of Personality Disorders, 26(3), 345. Eisen, J. L., Phillips, K. A., Baer, L., Beer, D. A., Atala, K. D., & Rasmussen, S. A. (1998). The Brown Assessment of Beliefs Scale: Reliability and validity. American Journal of Psychiatry, 155(1), 102–108. First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. (2002). Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. SCID-I/P. Fontenelle, L. F., Telles, L. L., Nazar, B. P., De Menezes, G. B., Do Nascimento, A. L., Mendlowicz, M. V., & Versiani, M. (2006). A sociodemographic, phenomenological, and long-term follow-up study of patients with body dysmorphic disorder in Brazil. The International Journal of Psychiatry in Medicine, 36(2), 243–259. Greenberg, J. L., Reuman, L., Hartmann, A. S., Kasarskis, I., & Wilhelm, S. (2014). Visual hot spots: An eye tracking study of attention bias in body dysmorphic disorder. Journal of Psychiatric Research, 57, 125–132. Harrison, A., de la Cruz, L. F., Enander, J., Radua, J., & Mataix-Cols, D. (2016). Cognitivebehavioral therapy for body dysmorphic disorder: A systematic review and meta-analysis of randomized controlled trials. Clinical Psychology Review, 48, 43–51. 313 314 Oliver Sündermann and David Veale Ipser, J. C., Sander, C., & Stein, D. J. (2009). Pharmacotherapy and psychotherapy for body dysmorphic disorder. Cochrane Database of Systematic Reviews, (1). Lambrou, C., Veale, D., & Wilson, G. (2011). The role of aesthetic sensitivity in body dysmorphic disorder. Journal of Abnormal Psychology, 120(2), 443. (2012). Appearance concerns comparisons among persons with body dysmorphic disorder and nonclinical controls with and without aesthetic training. Body Image, 9(1), 86–92. Mancuso, S. G., Knoesen, N. P., & Castle, D. J. (2010). The Dysmorphic Concern Questionnaire: A screening measure for body dysmorphic disorder. Australian and New Zealand Journal of Psychiatry, 44(6), 535–542. Marques, L., LeBlanc, N., Weingarden, H., Greenberg, J. L., Traeger, L. N., Keshaviah, A., & Wilhelm, S. (2011). Body dysmorphic symptoms: Phenomenology and ethnicity. Body Image, 8(2), 163–167. doi:10.1016/j.bodyim.2010.12.006 Osman, S., Cooper, M., Hackmann, A., & Veale, D. (2004). Spontaneously occurring images and early memories in people with body dysmorphic disorder. Memory, 12(4), 428–436. Öst, L.-G., Havnen, A., Hansen, B., & Kvale, G. (2015). Cognitive behavioral treatments of obsessive-compulsive disorder. A systematic review and meta-analysis of studies published 1993–2014. Clinical Psychology Review, 40, 156–169. Phillips, K. (2017). Body dysmorphic disorder: Advances in research and clinical practice. Oxford University Press. Phillips, K., & Menard, W. (2006). Suicidality in body dysmorphic disorder: A prospective study. American Journal of Psychiatry, 163(7), 1280–1282. Phillips, K. A. (2005). The broken mirror: Understanding and treating body dysmorphic disorder. Oxford University Press. (1996). Instruments for assessing BDD: The BDDQ: A self-report screening instrument for BDD. The Broken Mirror, 321–333. Phillips, K. A., Didie, E. R., Menard, W., Pagano, M. E., Fay, C., & Weisberg, R. B. (2006). Clinical features of body dysmorphic disorder in adolescents and adults. Psychiatry Research, 141(3), 305–314. Phillips, K. A., Hart, A. S., & Menard, W. (2014). Psychometric evaluation of the Yale– Brown Obsessive-Compulsive Scale Modified for Body Dysmorphic Disorder (BDDYBOCS). Journal of Obsessive-Compulsive and Related Disorders, 3(3), 205–208. Stott, R., Mansell, W., Salkovskis, P., Lavender, A., & Cartwright-Hatton, S. (2010). Oxford guide to metaphors in CBT: Building cognitive bridges. Oxford University Press. Sündermann, O., & Veale, D. (2017). Complexity in obsessive-compulsive and body dysmorphic disorder: A functional approach to complex difficulties. The Cognitive Behaviour Therapist, 10. Sündermann, O., Wheatley, J., & Veale, D. (2016). ‘If you have good skin, you are god. If you have bad skin, you are a piece of rubbish.’ Mastery of shame and anger in treatmentresistant body dysmorphic disorder: A single case study. The Cognitive Behaviour Therapist, 9. Veale, D. (2004). Advances in a cognitive behavioural model of body dysmorphic disorder. Body Image, 1(1), 113–125. doi:10.1016/S1740-1445(03)00009-3 Veale, D., Ellison, N., Werner, T. G., Dodhia, R., Serfaty, M. A., & Clarke, A. (2012). Development of a cosmetic procedure screening questionnaire (COPS) for body dysmorphic disorder. Journal of Plastic, Reconstructive and Aesthetic Surgery, 65(4), 530–532. Veale, D., Eshkevari, E., Kanakam, N., Ellison, N., Costa, A., & Werner, T. (2014). The Appearance Anxiety Inventory: Validation of a process measure in the treatment of body dysmorphic disorder. Behavioural and Cognitive Psychotherapy, 42(5), 605–616. Veale, D., & Gilbert, P. (2014). Body dysmorphic disorder: The functional and evolutionary context in phenomenology and a compassionate mind. Journal of Obsessive-Compulsive and Related Disorders, 3(2), 150–160. A Cognitive Behavioral Approach to Body Dysmorphic Disorder Veale, D., Gilbert, P., Wheatley, J., & Naismith, I. (2014). A new therapeutic community: Development of a compassion-focussed and contextual behavioural environment. Clinical Psychology and Psychotherapy, 22(4), 285–303. Veale, D., Gledhill, L. J., Christodoulou, P., & Hodsoll, J. (2016). Body dysmorphic disorder in different settings: A systematic review and estimated weighted prevalence. Body Image, 18, 168–186. Veale, D., & Matsunaga, H. (2014). Body dysmorphic disorder and olfactory reference disorder: Proposals for ICD-11. Revista Brasileira de Psiquiatria, 36, 14–20. Veale, D., Miles, S., & Anson, M. (2015). Long-term outcome of cognitive behavior therapy for body dysmorphic disorder: A naturalistic case series of 1 to 4 years after a controlled trial. Behavior Therapy, 46(6), 775–785. Veale, D., & Neziroglu, F. (2010). Body dysmorphic disorder: A treatment manual. John Wiley and Sons. Veale, D., & Riley, S. (2001). Mirror, mirror on the wall, who is the ugliest of them all? The psychopathology of mirror gazing in body dysmorphic disorder. Behaviour Research and Therapy, 39(12), 1381–1393. Veale, D., Willson, R., & Clarke, A. (2009). Overcoming body image problems including body dysmorphic disorder. Constable and Robinson. Weingarden, H., Renshaw, K. D., Davidson, E., & Wilhelm, S. (2017). Relative relationships of general shame and body shame with body dysmorphic phenomenology and psychosocial outcomes. Journal of Obsessive-Compulsive and Related Disorders, 14, 1–6. Wilhelm, S., Phillips, K. A., & Steketee, G. (2012). Cognitive-behavioral therapy for body dysmorphic disorder: A treatment manual. Guilford Press. Williams, J., Hadjistavropoulos, T., & Sharpe, D. (2006). A meta-analysis of psychological and pharmacological treatments for body dysmorphic disorder. Behaviour Research and Therapy, 44(1), 99–111. Willson, R., Veale, D., & Freeston, M. (2016). Imagery rescripting for body dysmorphic disorder: A multiple-baseline single-case experimental design. Behavior Therapy, 47(2), 248–261. Windheim, K., Veale, D., & Anson, M. (2011). Mirror gazing in body dysmorphic disorder and healthy controls: Effects of duration of gazing. Behaviour Research and Therapy, 49(9), 555–564. 315 16 Comprehensive Behavioral Treatment for Trichotillomania (Hair Pulling Disorder) and Excoriation (Skin Picking) Disorder Charles S. Mansueto Scene in a brightly lit bathroom. A young woman lies in her bathtub, her knees pulled up near her face. She has lost track of time, but has been there for hours. With one hand her fingertips glide over legs that are riddled with scars and scabs. Beneath her tortured skin lie the objects of her consuming efforts – the tiniest of hairs – the new growth that barely breaks above the skin’s surface. Once detected her other hand, holding small silver tweezers, moves to the spot in a desperate effort to grip and extract that hair and every other hair that she can find. The sharp tweezers’ tips dig deep beneath the skin’s surface, but she hardly notices any pain. Digging and scratching at her once delicate skin, now raw and unsightly, is the seemingly endless cycle of picking and pulling that consumes untold hours of her young life. She stops to rest only when her fingers detect no hairs remaining to be pulled or scabs to be scratched off with her fingernails. Finally, when her fingers are too tired and aching she stops and the episode ends. She lies back, filled with shame and self-loathing, and cries, no longer noticing that the bathwater is spotted pink with her blood. Body-Focused Repetitive Behaviors (BFRBs) Repetitive behavior patterns involving hair pulling, skin picking, nail biting, cheek and lip biting, and other similar behavior patterns, when taken together, are referred to as body-focused repetitive behaviors (BFRBs).* Among these, hairpulling disorder (HPD), also called trichotillomania, and skin-picking disorder (SPD), also called excoriation disorder, have received the most attention from the psychological and psychiatric research and clinical communities. Both have been accepted within official psychiatric nomenclature of the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association (HPD in 1987 and SPD in 2013, while other BFRBs are not specifically included). Over the * The author wishes to thank David Keuler, Michael Lent, and Sherrie Vavrichek for their assistance in preparation of this chapter. 316 Trichotillomania and Excoriation Disorder past two decades professional attention paid to BFRBs has substantially increased as research has established that these conditions are neither rare nor benign. While milder forms of these behavior patterns are common in the general population, in many adults and children these rise to the level of legitimate clinical disorders. Still, HPD and SPD remain largely outside the awareness of the general public, the scientific community, and the majority of clinical practitioners. For that reason, this chapter will provide some detailed information about these disorders, since effective treatment requires an in-depth understanding of their nature. Diagnosis Both HPD and as SPD are categorized within “Obsessive-Compulsive and Related Disorders” in DSM-5 (APA, 2013). The diagnostic criteria for HPD include recurrent pulling out of hair resulting in hair loss; SPD criteria include recurrent skin picking resulting in skin lesions. Criteria for both disorders specify: repeated attempts to decrease or stop the behaviors, significant distress or impairment as a result of these behaviors, that they are not attributable to the other medical disorders or conditions, nor better explained as symptoms of another mental disorder. Epidemiology HPD and SPD are both considered more common than previously understood. Individuals with these disorders usually attempt to conceal the physical damage from others with makeup, clothing, hairpieces, and hairstyles and can live lives of secrecy and isolation. This probably contributes to the widespread view that these disorders are rare. While large-scale studies documenting their prevalence within the general population have not yet been conducted, reported rates for HPD have been as high as 4.4% (Grant et al., 2005). However, wide discrepancies between reported prevalence rates of HPD are notable across reports. Such discrepancies are probably due to methodological limitations, such as small sample sizes, and inconsistencies in operational definitions and diagnostic criteria applied by different researchers (Mansueto & Rogers, 2012). Reasonable estimates suggest that 1–2% of adolescents and young adults suffer from the disorder (APA, 2013). Regarding estimates of SPD prevalence rates, similar limitations apply. According to DSM-5 (APA, 2013) between 1.4 and 5.4% of the population are SPD sufferers. Among childhood hair pullers and skin pickers of all ages, incidence seems to be evenly distributed between sexes. However, in the case of adult BFRB sufferers, most clinical samples find females outnumbering males by substantial margins (Mansueto & Rogers, 2012; Odlaug & Grant, 2012). Course, Comorbidity, and Associated Problems HPD and SPD can appear at any age. Onset at adolescence appears to be most common with childhood onset being second most common. Variations in age of 317 318 Charles S. Mansueto onset have led researchers to question whether there are phenomenological differences such as increased symptom severity and persistence, increased treatment resistance, and increased comorbidity between early and later onset cases (Keuthen et al., 2001a, b; Walsh & McDougle, 2001). In most cases these disorders are chronic, fluctuate over time, and wax and wane in intensity during their course. For both disorders, diagnostic criteria require significant distress or impairment associated with the behaviors. Patients with these conditions often attempt to conceal physical damage from others using makeup, clothing, hairstyles, and hairpieces. Significant numbers of sufferers report decreased self-esteem, a diminished sense of attractiveness, shame and embarrassment, anxiety, and depression associated with their conditions. Many avoid common activities such as haircuts, sports, sexual intimacy, and social situations (Flessner & Woods, 2006; Mansueto, 1991; Stemberger et al., 2000; Woods et al., 2006). Clinical comorbidity is prevalent among HPD and SPD sufferers, with anxiety and mood disorders among the most common. Other less common but not infrequent disorders comorbid with BFRBs include obsessive-compulsive disorder, body dysmorphic disorder, and an additional BFRB such as the coexistence of skin picking and hair pulling (Flessner, 2012). Besides exacting psychological and social tolls, there are also economic and medical consequences associated with HPD and SPD. Time spent performing the BFRB can interfere with academic and occupational functioning. Sufferers spend hours each day (and money), in attempts to conceal resulting cosmetic damage (Flessner & Woods, 2006). In a subset of patients, HPD and SPD can result in several kinds of medical problems. Most obvious is the damage to the hair or skin at the site (or sites) targeted. Hair loss and skin lesions are predictable outcomes, but scarring, infections, and other medical complications are not unusual. Repeated trauma from repetitive hair pulling and digging at the targeted sites with the fingernails or implements such as tweezers and pins can produce degrees of tissue damage that result in changes to the appearance and ultimate health of the hair and skin. In more extreme cases of HPD, hair may not regrow, or regrowth may show color or textural changes. The ingestion of the products of hair pulling, that is, the eating of all or parts of the hair, can result in the development of trichobezoars, (hairballs). Trichobezoars can produce gastrointestinal complications and may require surgery. In rare cases, they can be fatal (Christenson & Mansueto, 1999). Skin picking often produces tissue damage such as swelling, bleeding, weeping, infections, and scarring. In more extreme cases of SPD, corrective medical procedures such as dermabrasion or plastic surgery may be required. Clinical Presentation of HPD and SPD While earlier reports of HPD and SPD emphasized their mechanistic simplicity, later descriptions have highlighted their heterogeneous nature and phenomenological complexity (O’Sullivan et al, 2000). Mansueto (1990) described an array of variables that comprised the complexity and heterogeneity which distinguishes one Trichotillomania and Excoriation Disorder HPD sufferer from another on the basis of sensory experiences, cognitive elements, affective states, motor habits, and situational variables. This view of the disorder was affirmed in later reports (Christenson at al., 1991, 1993). HPD today is widely regarded as diverse, idiosyncratic, and heterogeneous. With research interest increasingly focused on SPD, it is clear that similar conclusions can be drawn regarding that disorder as well (Grant & Odlaug, 2009). HPD Regarding HPD, Mansueto and colleagues (1997) acknowledged the wide variety of behaviors associated with HPD that go beyond those specified within the diagnostic criteria, and integrated them in a conceptual framework. Their conceptual model of HPD has become known as the comprehensive behavioral (ComB) model. A wide array of associative behaviors is seen most clearly when hair is pulled in what has been termed a “focused style.” Focused hair pulling occurs when an individual is highly conscious of pulling activities occurring. These activities tend to be accompanied by urges, thoughts about pulling, and feelings of discomfort. This can be contrasted with “automatic pulling” in which pulling is performed with little or no awareness, typically while the individual is engaged in some sedentary activity like watching TV or reading. While some individuals have one or another predominant style, most experience combinations of focused and automatic pulling (Christenson & Mackenzie, 1994). With the ComB model, the many potential activities associated with hair pulling are organized into three phases: preparatory behaviors, pulling behaviors, and disposal behaviors. Preparatory behaviors include such preliminary activities as seeking privacy, accessing implements (such as mirrors and tweezers), and selecting hairs to be pulled (such as thick, dark, rough, sharp, gray, or out-of-line hairs), either visually or by touch. During the pulling phase, hair is most commonly extracted from the scalp. However, eyebrows, eyelashes, and pubic hair are frequent sites as well. Less commonly, hair is pulled from arms, legs, face, armpits, or other body areas. While there may be only one exclusively targeted site, hair is often removed from more than one site. Individuals may remove only a few or hundreds of hairs at any given episode. An episode may last from seconds to hours at a time. During the disposal phase, what is done with the pulled hairs can be elaborate and idiosyncratic. Although quick disposal of the hair is a possibility, many individuals engage in activities with the hairs or hair root. It is not unusual for hair to be visually examined or physically manipulated. Typical activities include rubbing of the hair or its root between the fingers, on the face, or lips, and a variety of oral activities such as biting, nibbling, chewing, or swallowing the hair root, bits of the shaft, or, in some cases, entire hairs. Less commonly, hairs are saved for later inspection, manipulation, or collection (Mansueto, 1991). SPD The clinical presentation of SPD is remarkably similar to that of HPD. While the ComB conceptual model was developed for hair pulling, it is easily applied to skin 319 320 Charles S. Mansueto picking, with only minor adjustments. As with HPD, the focused, automatic, and combined styles also apply. While picking is mostly done with fingernails, in the cases of focused picking, implements such as scissors, tweezers, pins, and mirrors are also employed. Seeking of privacy and accessing implements are common preparatory activities for skin picking, As with HPD, suffers can spend minutes to hours per day engaged in the activity. The face is the most common site for picking. However, fingers, arms, legs, chest, back, shoulders, feet, and pubic areas may also be targeted. Most individuals pick from more than one site. Picking is usually directed at imperfections or anomalies of the skin such as acne pimples, bug bites, scabs, bumps, or dry, flaking, and rough patches of skin. Many individuals pick at healthy skin as well. Regarding disposal, it is not unusual for products of the picking, such as bits of skin or scabs, to be bitten and swallowed (Odlaug & Grant, 2012). BFRB Treatment A wide variety of therapeutic approaches drawing from various models of pathology has been employed in efforts to help BFRB sufferers. These include traditional psychotherapy, hypnosis, biofeedback, meditation, acupuncture, pharmacotherapy, and behavior therapy. Among these, the two considered most promising, based on results from limited clinical trials, are pharmacotherapy and behavioral treatments. In a recent review of pharmacotherapy for BFRBs (Grant et al., 2012), the authors deplored the shortage of adequate studies examining efficacy for these disorders. However, they concluded that there is probably sufficient evidence from randomized controlled trials to support the use of the opioid antagonist naltrexone, the atypical antipsychotic olanzapine, and the glutamatergic agent N-acetylcysteine for HPD, and the selective serotonin reuptake inhibitors (SSRIs) fluoxetine and citalopram for SPD (Chamberlain et al., 2012). While pharmacological agents may be helpful in treatment of BFRBs, particularly when significant comorbid disorders are present, there are no psychotropic medications approved by the US Federal Drug Administration for BFRBs. Currently, the best supported of contemporary therapy approaches is behavior therapy. In a meta-analysis of randomized controlled trials for HPD, McGuire and colleagues (2014) reported that behavior therapy had a large effect in reducing hair pulling severity, while SSRIs had a smaller effect. Similarly, Schumer et al. (2016) found behavioral treatments superior to pharmacotherapy for skin picking in their meta-analysis. Because behavioral approaches are currently considered treatments of choice for BFRBs (Golomb et al., 2011), the remainder of this chapter will focus on behavioral treatment. Behavioral Treatment Two behavioral treatment approaches stand out from others because of their association with BFRB treatment. These are habit reversal training (HRT), Trichotillomania and Excoriation Disorder developed by Azrin and Nunn (1973), and comprehensive behavioral (ComB) treatment developed by Mansueto and colleagues (1999). HRT was an early treatment and is still influential. Because it has the most empirical support of any single treatment for BFRBs (Bloch et al., 2007), a brief overview will be provided of HRT and its variants. Habit Reversal Training (HRT) Azrin and Nunn’s HRT viewed a mixed group of problematic repetitive behaviors, such as tics and nail biting, as “nervous habits”: tension-reducing motor behaviors that became largely automatic because, through frequent repetition, they became strengthened. Later, HRT was applied to hair pulling (Azrin et al.,1980). From their perspective, hair pulling and skin picking were viewed as well-practiced habits, embedded in chains of internal and situational cues and connected responses, through conditioning mechanisms, that could occur without conscious awareness. In accordance with this conceptual model, HRT consists of a varying number of components designed to compete with and eliminate the problem behaviors. The essential component of HRT is competing response intervention, in which a motor response that is incompatible with the undesired behavior, such as fist clenching, is practiced in place of the problem behavior. Various therapeutic components were added and deleted in later reports of HRT. These include awareness training, motivation-enhancing procedures, imaginal rehearsal, self-monitoring, relaxation training, and social support (e.g., Azrin & Nunn, 1977; Azrin et al.,1980). More recently, Bloch and colleagues (2007) described HRT as encompassing four components: (1) self-monitoring, (2) awareness training, (3) stimulus control, and (4) stimulus–response intervention (competing response training). Early reports of successful treatment of hair pulling using variations of HRT treatment (e.g., Rosenbaum & Ayllon, 1981; Miltenberger & Fuqua, 1985; Tarnowski et al., 1987) were promising. However, they were criticized for substantial methodological shortcomings (Keuthen et al., 1999). Later indications of treatment effectiveness were less favorable with problems of relapse still significant (Lerner et al., 1998; Mouton & Stanley, 1996; Van Minnen et al., 2003). Augmented HRT and Mixed CBT Approaches Recognition of the phenomenological complexity of BFRBs highlighted the possibility that Azrin’s behavioral model may have oversimplified the fundamental nature of BFRBs by failing to identify some of the critical factors that govern them. In efforts to increase treatment effectiveness, some researchers grafted other treatment components onto HRT that were designed to address factors not formally addressed by HRT. One such later addition was stimulus control. Environmental cues, such as the presence of a magnifying mirror in a brightly lit bathroom, that can trigger an individual’s BFRB are altered or removed (e.g., Rothbaum, 1992). Interest in possible cognitive contributions to BFRBs for individuals with strongly held ideas, such as “I’ve got to get rid of these gray hairs,” led to the addition of 321 322 Charles S. Mansueto cognitive therapy techniques, such as cognitive restructuring, to augment HRT treatment (Gluhoski, 1995, Lerner et al., 1998). In recognition of research evidence that BFRBs help modulate aversive emotions and other kinds of unwanted internal experiences (e.g., Arnold et al., 1998), researchers have included emotional regulation skills as adjunctive components to traditional HRT in BFRB treatment outcome studies. More recent efforts to bolster HRT with newer CBT formulations designed to target these presumed variables, and thereby to enhance treatment effectiveness, have included the addition of dialectical behavior therapy skills (Keuthen et al., 2010) and acceptance and commitment therapy elements (Flessner et al., 2008; Woods et al., 2006). In clinical practice, adult and pediatric BFRBs are likely to incorporate multiple intervention strategies that include any of the abovementioned treatment components, such as psychoeducation, reward systems, and relapse prevention techniques. The various components of such “package” treatments can be applied in a modular fashion; therefore, modifications to suit individual patient characteristics are possible (Gianoli & Tolin, 2012). It is generally accepted that the myriad forms of CBT, typically with HRT elements at their core, are reasonably effective in the short term (Bloch et al., 2007). However, the effectiveness of these approaches varied, and relapse was a significant problem (Keijsers et al., 2006; Lerner et al., 1998). In particular, the problem of failure to maintain gains indicates that there is room for improvement in treatments for BFRBs. The Comprehensive Behavioral (ComB) Model Possible shortcomings in HRT and similar approaches to BFRBs can be identified. First, there is an absence of a guiding, comprehensive, theoretical framework that encompasses and integrates the behavioral, affective, cognitive, and sensory variables. Also, the general use of “package” treatments may not be individualized enough to address the heterogeneity of BFRB presentations. Finally, treatment models may not provide adequate guidance through the therapeutic steps of assessment, case conceptualization, and clinical decision-making to provide for more effective treatment. The ComB conceptual model (Mansueto et al., 1997) was designed to describe and capture the complex and heterogeneous nature of HPD. While it is clear that CBT practitioners have utilized and tested a wide variety of treatment techniques for BFRBs, this range of options can present a dilemma for clinicians. From what can seem like a hodgepodge of available techniques derived from standard CBT approaches, how can a clinician provide the most efficient and effective treatment plan for any individual patient? This is the question that the ComB approach is designed to answer. The ComB treatment model was developed from the outset to address the complexity and heterogeneity of hair pulling and to guide clinical decision-making throughout the therapeutic process. Therefore, it is useful to be familiar with the ComB conceptual model on which it is based (Mansueto et al., 1997) in order to Trichotillomania and Excoriation Disorder comprehend and most effectively apply ComB treatment to HPD and other BFRBs. Extensive clinical experience suggests that ComB treatment, with minor modifications, can effectively address SPD. ComB Conceptual Model The ComB model of HPD was originally developed as a framework for organizing and analyzing hair pulling data for research and clinical purposes, that is, as a conceptual model. ComB described the broad array of variables associated with hair pulling and, by extension, skin picking and other BFRBs in a functional analytic (i.e., A-B-C) formulation, in which the antecedents (A) and consequences (C) by which behaviors (B) associated with hair pulling are instigated and maintained. These incorporate antecedents – cues that generate or otherwise facilitate impulses and urges to engage in the BFRB, the array of behaviors involved in performance of the BFRB, and the consequences that influence the repetition of those behaviors. These variables are described as linked in accordance with familiar cognitive behavioral principles. Thus, from the ComB perspective, BFRBs are a set of wellpracticed behaviors that are triggered by various cues, occurring internally or externally to the individual. These are maintained by positive and negative reinforcing experiences. In other words, the performance of the BFRB behaviors is a function of factors that immediately precede and follow them. The ComB model specifies five categories (domains) in which variables functionally related to BFRBs can be identified. In this regard ComB has features in common with the multimodal therapy of Arnold Lazarus (1981). There are significant differences, however. While multimodal therapy employs a seven-modality framework to guide assessment and treatment of a wide range of disorders, ComB specifies five categories of variables that are derived from BFRB research (Mansueto, 1990) and are functionally relevant to these disorders. The five domains comprise sensory, cognitive, affective, motor, and place (environmental) variables. Note that sensory and cognitive variables are uniquely highlighted in combination with other, familiar behavioral components. The anagram SCAMP provides a convenient memory aid for recalling the five critical domains for patients and clinicians throughout treatment. Some examples of variables within the SCAMP domains are provided in Table 16.1. Overview of ComB Treatment At the core of ComB treatment (Mansueto et al., 1997) is the clinician’s task of working collaboratively with the patient, first to identify and then to change relationships between the antecedent and consequential variables presumed to instigate and maintain the BFRB. Treatment begins with a functional analysis employing an in-depth structured assessment to identify an individual’s unique pattern of SCAMP antecedents and consequences that foster performance of the BFRB. Change is accomplished through an individualized treatment plan in which established behavior patterns are interrupted and nonharmful alternative behaviors are substituted to 323 324 Charles S. Mansueto Table 16.1. Five domains of the ComB model Sensory domain Antecedents Consequences Cognitive domain Antecedents Consequences Affective domain Antecedents Consequences Motor domain Antecedents Consequences Place domain Antecedents Consequences Urges to pull hair or pick skin; the feel or sight of coarse hairs or blemished skin; itching or irritation at the site; etc. Satisfaction at accomplishing goals like removing unwanted hairs or smoothing out rough skin; achieving desired sensations through pulling or picking, or through employment of secured hair skin products (e.g., manipulating, nibbling hairs or skin), etc. Facilitating thoughts or beliefs like “I’ve got to pop this pimple”; “These crooked eyelashes have to go”; “I’ll just pull a few”; “This scab looks disgusting”; etc. Thoughts like “That was a good pop”; “I’ve got that annoying stub”; “That feels nice and smooth now”; “Got a nice plump root”; etc. Unwanted feeling like being bored, stressed, anxious, depressed, tired, lethargic, overstimulated, etc. Satisfying feeling states achieved by hair pulling or skin picking like pleasurable feelings, alleviation of boredom, stress and anxiety reduction, feeling energized, etc. Habits involving facilitative postural cues and unconscious motor habits like twirling or stroking the hair, running fingertips across skin, resting fingers against the face, rubbing the eyes, etc. Note: In the case of the consequences in the motor modality, the presumption is that the expression of the habit serves as a reinforcing consequence. External, environmental cues that trigger BFRB behaviors such as the presence of physical implements like mirrors or tweezers; settings like the bathroom, car, or bedroom; opportunities like being alone; etc. Note: reinforcers in the place modality are not ordinarily functional in maintaining with a few exceptions, such as when performance of the BFRB elicits desirable reactions from others. meet the idiosyncratic functions served by hair pulling or skin picking. Alternative behaviors are carefully chosen within the domains that are identified, as relevant to each individual’s needs. Treatment is modified, as necessary, in response to feedback regarding the utility of specific treatment recommendations. With practice, it is expected that predispositions to pull hairs or to pick skin (and their accompanying urges) will weaken as healthy alternative habits are established. This process utilizes the SCAMP formulation as a guide for the assessment of BFRB-relevant features, for the functional analysis of those features and for decision-making in treatment implementation. The ComB Treatment Process As the ComB conceptual model is based on familiar behavioral principles, ComB treatment encompasses a wide range of techniques drawn from standard behavioral, cognitive, and CBT practice. These are familiar to CBT practitioners as they are Trichotillomania and Excoriation Disorder widely used to treat a broad range of disorders. Therapists are encouraged to draw on their training, knowledge, and skills as client needs become apparent. For example, a therapist skilled in motivational interviewing (Rollnick & Miller, 1995) may incorporate those techniques to increase an individual patient’s motivation and willingness to employ interventions taught in ComB treatment. If a BFRB patient is burdened with stress or anxiety and has poor coping mechanisms, a therapist with expertise in the use of mindfulness-based stress reduction (e.g., Kabat-Zinn & Chapman-Waldrop, 1988), acceptance and commitment therapy (Hayes, 1999; Woods et al., 2006) or dialectical behavior therapy skills (Keuthen et al., 2010; Linehan, 1993) might provide any of these as therapeutic interventions. Because such interventions require a significant amount of specialized training and experience, other established and widely used cognitive behavioral techniques such as more traditional stress management techniques (e.g., diaphragmatic breathing, progressive muscle relaxation, cognitive coping techniques, problem solving) will suffice in most cases. Because ComB treatment is uniquely tailored to the individual needs of each patient, the treatment process is expected to be both creative and organic rather than rigidly applied. The flexible and patient-oriented nature of the treatment process results in therapy that may appear quite different from one patient to another, due to factors such as the therapist’s skill set, judgment, and decisionmaking as well as the patient’s preferences. There are two important preliminary considerations for the therapist to address prior to beginning formal ComB treatment: First, the therapist should determine that the BFRB is the appropriate target for treatment and that there are no more prominent conditions overshadowing it. This is significant, because BFRBs frequently co-occur with other disorders such as depression, anxiety, and OCD. The question of whether to address other disorders first or concurrently with BFRB treatment should be determined at the outset. Some comorbid conditions, such as milder forms of depression or anxiety, may be secondary to hair pulling or skin picking. They may either abate with successful treatment of the BFRB or may not significantly undermine treatment if left unaddressed. When significant comorbidity renders an individual incapable of benefiting from ComB treatment, other conditions may be more appropriately targeted prior to efforts to treat the BFRB. Second, more so than those with many other disorders, people who suffer from BFRB are highly sensitive to the self-induced aspects of the problem. It is typical therefore, for secondary features such as shame, poor self-esteem, and impaired social functioning to be significant issues among these patients. The therapist needs to be sensitive to this from the first encounter. Care should be taken throughout the course of treatment to help the patient move toward healthy self-acceptance and normalized social functioning. Subtle, nonverbal cues – a brief look of disgust fleeting across the therapist’s face, for example – can damage efforts of rapport-building and thus may severely compromise prospects for successful treatment. A casual, accepting, and nonjudgmental tone adopted by the therapist during detailed and frank exchanges about the BFRB can facilitate resolution of these issues. 325 326 Charles S. Mansueto As mentioned above, ComB treatment is administered in a flexible, creative, and individually tailored manner. Treatment does proceed methodically through a series of four phases: (1) psychoeducation and assessment, (2) functional analysis (identification and organization of maintaining factors within relevant domains), (3) implementation of specific interventions, and (4) evaluation, termination, and relapse prevention. However, these phases are not rigidly prescribed. Elements associated with any one of the phases can be provided in any of the other phases as determined by the therapist’s judgment and the patient’s needs. A case description of a patient who both pulls out her hair and picks at her skin will be provided to illustrate all phases of treatment. HPD and SPD Combined: A Case Description Kaitlyn, 22 and single, is one year out of college and is living alone in Florida where she works at her first “real” job. Since she was a teenager she had a problem with hair pulling. At first it was her eyebrows, which she would pull sporadically when she had the necessary privacy; she said she does not remember why. When her mother noticed that she had patches of missing eyebrows, she made quite a fuss and never let up. Kaitlyn made a sincere effort to stop pulling and allow her eyebrows to grow back. At some point, in desperation, she began to pull out hairs from her legs instead of her brows, as it was easier to keep that pulling a secret. It worked pretty well. Her eyebrows mostly grew back, and missing leg hairs were easier to hide. Other problems began to develop, though. Sometimes it was hard to grab hold of the hairs on her legs with just her finger, so she began using tweezers to pull the short hairs and to dig out deeply buried hairs. Her legs bled when she dug too deeply and scabs would form on the damaged skin. It was impossible for Kaitlyn to resist picking off scabs as she had to shave her legs and their roughness bothered her anyway. During high school this was more of an inconvenience, though at times there was enough visible damage to prevent her from wearing clothes that bared her legs. Sometimes she resorted to using makeup to camouflage the damage she had done. Still, the problems were relatively minimal and she was reasonably happy and well adjusted through the remaining years of high school. Things were even better most of the time after she went away to college. She found that dorm life, as well as a busy academic and social life, helped her keep her problem manageable. It was still occurring but much less frequently and with less severity. Now, living alone, with more privacy and more free time, things were getting out of hand. Fortunately, she could wear slacks at work, but in the Florida climate she longed to wear shorts and skirts, and swimsuits at the beach. Another big problem was that she had met a guy whom she liked very much. Their relationship had all the indications of becoming more serious, but she had so far avoided his invitations to accompany him to pool parties and some other outdoor activities. Moreover, she wanted more intimacy with him but had disallowed that for fear of his reaction when he saw her bare legs. The more upset she became about her Trichotillomania and Excoriation Disorder circumstances, the worse her BFRBs became. Her new life was being spoiled by problems over which she had no control. A new problem added to her woes. Living in her own apartment, she had been enjoying her growing independence and freedom from the constraints that she had felt when she lived at home. Unfortunately, she remained dependent on her mother for financial assistance as she struggled to pay back college loans and to cover other living expenses. Her relationship with her mother was always difficult, but now she was an adult and wished she were treated like one. Hundreds of miles away from home, her mother, always an anxious and controlling parent, was phoning her almost every afternoon just as Kaitlyn arrived back from work. She had a way of asking intrusive questions and providing unwanted advice during those calls. Though she tried to maintain her composure, Kaitlyn inevitably felt trapped, unable to get a word in edgewise, and grew more frustrated and angry as the conversations became prolonged and more one-sided. Kaitlyn’s usual pattern was to fall down on her couch holding her cell phone and pull out leg hairs. She realized she couldn’t blame everything on her mother because a lot of damage was done in situations where her mother had nothing to do with it. On top of that, a new development was pushing her over-the-edge. Seemingly out of nowhere, she began pulling hair from her scalp. She had no idea where that came from and could not recall even thinking about doing it. It wasn’t clear to her when it started. All she knew was that, for at least two months, she had a growing, egg-shaped bald spot above her left ear, which was increasingly difficult to keep hidden from others. One night after a particularly frustrating episode in which a lot of hairs were pulled, Kaitlyn went on line, discovered the TLC Foundation for BFRBs’ website, and found a trained therapist near her. What follows is a description of her therapy. Phase 1: Assessment and Psychoeducation Kaitlyn made the appointment with Dr. Benton, but she was very nervous about the first visit. No one knew all the details about her pulling and picking practices. For example, sometimes her skin picking didn’t stop at her upper legs but continued to the pubic area. She had damaged her skin there also. She had other embarrassing secrets as well. She would scratch off little scabs and pieces of dry skin with her fingernails, put them in her mouth, nibble, and swallow them. She could never tell anybody that. Dr. Benton, however, put her at ease during the first session. Kaitlyn listened dumbfounded as he spent some time describing how common these problems were, how difficult it could be to live with them, and how their impact on his patients’ lives could be profound. She felt relieved when he mentioned that pulling pubic hair was occurring in at least half of the people who pulled out hair. Later, he told her that more than half of the people who pull hair or pick skin did something oral with the products of the pulling and picking. He seemed to understand that there were many ways that pulling hair or picking skin could result in some desirable outcomes for the person who did it. Dr. Benton said for some, it just felt really good; for others, it 327 328 Charles S. Mansueto helped them handle emotions that they just didn’t want to feel. It gave them something to explore with the fingers, eyes, or mouth as a distraction when they were bored. He knew about and seemed to understand the “weird” things that people did with hairs, scabs, and skin – even people who didn’t have a BFRB problem. He seemed to understand that, while part of a person with BFRBs really wants to stop because of the damage done to their bodies and the impact on their lives, another part of them doesn’t want to give up the shorter-term, positive returns of engaging in those behaviors. That was the therapist’s job, he said, to mobilize the part of her that wanted to cease damaging her body, and to find healthy ways to meet the needs currently being met by BFRBs. Kaitlyn had feared the worst of this initial session and now was feeling safe, understood, and in good hands. Dr. Benton gave her some informative pamphlets from the TLC Foundation about BFRBs to read at home that included information about online support groups. Dr. Benton made it clear that BFRBs are not an indication of any deep-seated problems and that her therapy would directly address the hair pulling and skin picking. He would use a therapy approach called comprehensive behavioral treatment, or ComB, that she would learn more about during the following sessions. However, he did give her a brief overview of SCAMP domains. She immediately understood that there was more complexity to her hair pulling and skin picking than she had recognized. Dr. Benton’s obvious familiarity with BFRBs helped Kaitlyn trust the process that would follow. Assessment Having gained sufficient information, Dr. Benton confirmed that Kaitlyn met criteria for two disorders: HPD and SPD. He believed that her sadness, anxiety, and anger issues were largely secondary to BFRB problems. Dr. Benton had Kaitlyn fill out two brief measures: the Massachusetts General Hospital (MGH) Hair Pulling Scale (Keuthen et al., 1995), and the Skin Picking Severity Scale (SPSS) (Keuthen et al., 2001a). (See Appendices 16.1 and 16.2 for these measures.) These would be administered weekly throughout her treatment. At this early stage of treatment, Kaitlin was introduced to self-monitoring and recording of information about her BFRBs. She was given self-monitoring forms to be used weekly, which would help her keep track of incidences of hair pulling and skin picking and other information that would be used in the course of treatment (a sample Weekly Self-Monitoring Form is provided in Table 16.2). There is no ideal or definitive method of monitoring BFRBs. The sample form provided may be modified in any number of ways to better suit individual patients. For instance, hair pulling severity might be monitored as the number of hairs pulled daily. Note that because there is no perfect metric for all forms of BFRBs, a subjective rating by the patient (severity Score, 1–10) was employed to help increase awareness and to uncover other useful information. These self-monitoring forms were to be completed between sessions. Kaitlyn was helped to understand that this would allow her and Dr. Benton to identify specific cues that preceded hair pulling and skin picking episodes, and to document Trichotillomania and Excoriation Disorder 329 Table 16.2. Weekly self-monitoring form Date Place Activity Internal cues thoughts, sensations, emotions External cues time of day, implements, etc. Interventions used (if any) # of Hairs pulled or severity score (1–10) the desirable effects derived from her BFRBs. With help from Dr. Benton they organized information she brought back into SCAMP domains. With a little practice, Kaitlyn incorporated SCAMP concepts into her conversations with Dr. Benton as well as into the ways she came to think about hair pulling and skin picking. What follows is a summary of the information she provided, organized into SCAMP domains, that Dr. Benton used to complete the functional analyses of her HPD and SPD. Phase 2: Functional Analysis: Identification and Organization of Maintaining Factors within Relevant Domains Most of Kaitlyn’s BFRB problems could be organized into three main clusters: focused pulling and picking while bathing, focused pulling and picking while on the phone with her mother, and largely automatic pulling and picking in a wide variety of situations – chiefly sedentary ones or while deeply absorbed in an activity. Each cluster would be subjected to separate analyses. Bathing: Uses tweezers to pull out unwanted hairs on her legs and to dig deeply through her skin to remove ingrown hairs from her legs, but also from the pubic area. Sensory Antecedents: Visual and tactile detection of “stubs” – short, dark, new hair growth on her legs, and detection of ingrown hairs. Sensory Consequences: Desirable feeling of smoothness when fingertips explore skin after hair removal, sight of skin devoid of stubs. Cognitive Antecedents: “Hate these stubs”; “Got to get the ingrown hairs out or they’ll get sore and infected.” Cognitive Consequences: “Got that one!”; “Mission accomplished!” Affective Antecedents: Neutral feelings turn quickly to intense distress after detection of the sharp hairs and the ingrown hairs. Affective Consequences: Immediate reduction of distress on removal of hairs. Motor Antecedents: None – all BFRB behaviors are done with complete awareness. Motor Consequences: None. 330 Charles S. Mansueto Place Antecedents: Bright bathroom lights, tweezers within reach (a wellpracticed behavioral pattern when bathing). Place Consequences: None. On Phone with Mother: Pulls leg hairs with tweezers and digs for ingrown hairs while talking on the phone. Sensory Antecedents: None initially to trigger the BFRB behaviors, but once picking and pulling has begun, she targets the new, prickly hairs and the ingrown hairs that she detects by sight and touch. Sensory Consequences: Minimal; in these situations, she gets little actual satisfaction from the removal of those hairs, and doesn’t bother to “finish the job” or to enjoy the smoothness of her skin on her fingertips. Cognitive Antecedents: No hair or skin-related thoughts – just angry thoughts in response to her mother’s comments. Cognitive Consequences: Not as notable as when bathing, but still an element of “Got that one!” occurring sporadically. Affective Antecedents: Anger, frustration, and feelings of being trapped. Affective Consequences: Distraction from negative feelings, reduced level of distress. Motor Antecedents: Minimal; phone in left hand, tweezers in right is typical position on the couch, which facilitates performance of the BFRB; however, all BFRB behaviors are done with complete awareness. Motor Consequences: None. Place Antecedents: A second pair of tweezers kept between the couch cushions (leading to a well-practiced behavioral pattern in this situation). Place Consequences: None. Automatic Picking and Pulling in Various Situations: With self-monitoring and Kaitlyn’s growing self-awareness, it became clear that in many situations it seemed that her left hand had “a mind of its own.” The situations in which this type of pulling occurred were expanding – even to her desk at work. All pulling from the scalp was done with her fingers, never with tweezers. In those situations, her fingers would go to her scalp as she concentrated on something else. She had a “favorite spot,” over her left ear, from which she removed hair and produced a bald spot, roughly the size and shape of an egg. At those times her fingertips would explore the edges of the spot and pull out individual hairs, but more often a few at a time. Otherwise, her fingertips explored the denuded area, pulling out any new growth she could grasp. When she caught her fingers at her scalp, usually she would pull her hand away, but before long, the pattern repeated itself. Sometimes she would just give up and let it happen. Kaitlyn eventually told Dr. Benton about one aspect of her BFRB that she had been holding back from him: she enjoyed picking scabs off her legs, usually while lounging around her apartment. She acknowledged that she would bite and swallow bits of scabs, particularly enjoying the “crunchy ones.” This behavior pattern also had an element of unconsciousness to it Trichotillomania and Excoriation Disorder some of the time, so Dr. Benton combined it with hair pulling from the scalp for the functional analysis. Sensory Antecedents: None that she was fully aware of prior to pulling hair or picking scabs; after pulling from the scalp she sometimes rolled hairs between her fingertips; when scratching scabs from her legs, she had more awareness of the biting and swallowing than of the picking. Sensory Consequences: Sometimes gets satisfaction out of clearing her bald spot of new growth; her fingertips detect smoothness in that denuded area, eliminating scabs on her legs again produces a detectable smoothness – that smoothness and the nibbling on scabs are experienced as pleasurable. Cognitive Antecedents: Few hair- or skin-related thoughts in either case. Cognitive Consequences: None notable, but occasional positive thoughts like “Got that stub”; ”Nice and smooth”; “Good crunchy one.” Affective Antecedents: Sometimes boredom, sometimes mild restlessness in both cases. Affective Consequences: Mildly stimulating when bored, mildly soothing when restless. Motor Antecedents: Without awareness, hands move to the pulling or picking site. Motor Consequences: Habit is expressed by activity at the pulling or picking site. Place Antecedents: No fixed place requirement; however, privacy, a sitting position, at least one hand free, and access to the pulling or picking site are precursors. Place Consequences: None. Phase 3: Implementation of Specific Interventions Now Kaitlyn and her therapist were both aware of the many antecedents and the consequences associated with hair pulling and skin picking organized within the SCAMP domains. It was time to implement some of the techniques that interfered with “business as usual.” The place domain variables, once identified, pinpointed the environments in which other contributing SCAMP variables would have to be addressed. Information from Dr. Benton’s semi-structured interview and Kaitlyn’s self-monitoring forms helped determine that therapeutic interventions would target elements associated with three discretely different circumstances: the two high-risk situations (the bath and the phone calls with her mother) as well as the various random places in which the less mindful, more automatic pulling and picking typically happened. Dr. Benton told Kaitlyn during the next session that they would put treatment elements in place that were designed to meet some of the needs currently met by her BFRBs. These elements would also interfere with BFRB performance, allowing healthier behavior patterns to be established in their place. He provided Kaitlyn with an “intervention ideas list” (see Table 16.3) and asked her to review it during the week. He explained that these were specific interventions organized according to SCAMP domains. 331 332 Charles S. Mansueto Table 16.3. Intervention ideas list Sensory (decrease cues through healthy grooming; stimulate the senses in other ways) Interventions that can soothe or stimulate the whole body: Warm bath, cool shower, exercise, dance Cognitive (dispute unhelpful beliefs and attitudes; replace with more helpful ones) How to think about yourself, the growth and healing of hair and skin, and the nature of BFRBs in ways that will help the recovery process: Cognitive restructuring: Restate BFRB-facilitating thoughts using accurate undistorted, nonjudgmental language. Learn more about BFRBs and treatment. Go to responsible websites and other sources for more information about your condition and ways to recover from it. Adaptive self-talk: Talk to yourself in positive ways that are encouraging – as you would with your best friend. Problem-solving: Explore alternative solutions to problems, such as assertiveness. Mindfulness: Learn mindfulness techniques to recognize the sensations, emotions, and thoughts that trigger picking or pulling and then sit with the experiences without acting on them. Affective: Find better ways to respond to and balance uncomfortable emotions/other internal states Calm the affective system Activate, energize the affective system Schedule pleasurable activities (e.g., socialize, sports, gardening, hiking, crafts) Cool shower Effective communication/assertiveness Gentle, moderate, or vigorous exercise Volunteer work Make a realistic to-do list (daily, longer term) Deep breathing Relaxation exercise (scheduled or as needed) Meditation, yoga Positive visualization Mindfulness exercises Acceptance Warm bath Interventions That Can Both Calm or Simulate the Talk things through with friends or a confidant Medications Journal writing Use affirmations Affective System, Depending on the Need Create daily gratitude lists Do housework Listen to music Motor: Increase awareness, interfere with access, engage in alternative activities Keep fingers from target area Wear finger bandages Cover fingertips with medical tape Wear driving gloves Keep hands moist with lotion Cut fingernails short Wear light cotton gloves Wear elbow brace Make an effort to not cross the boundary to BFRB site (e.g., hands stop at necklace) Keep hands busy in other ways Use “fiddle toys” Groom nails: manicure/pedicure Engage in knitting or other craft Engage in physical exercise Clench fists Make it harder to pick or pull Tape/bandage on picking site Wear clothes that cover the picking site Wear glasses Put ophthalmological ointment on eyelids Wear false eyelashes or makeup Wear a hat/bandana/headband Put hair in pony tail, braids, or other hair style that decreases access to hair Get short haircut Wear a wig or hairpiece Wet hair and/or leave conditioner in hair Get professional help (e.g., haircut, laser treatment, electrolysis, prescription medicine) Trichotillomania and Excoriation Disorder 333 Table 16.3. (cont.) Place/environment: Decrease triggers (physical location, activity, time of day, privacy) Decrease environmental cues Adjust schedule or activities Try to avoid using computer or TV during high-risk times, or use motor interventions to block access Contact someone for support Avoid being alone in high-risk situations Keep hands “busy” during high-risk times Plan “wind down” activities at night Put “caution” sign on bathroom door or mirror Keep “fiddle” toys in trigger locations Put a timer in the bathroom Remove/cover mirrors Eliminate tweezers/magnifying mirror Put sticky note reminders on mirrors Cover mirrors Dim lights while using toilet Stay out of certain rooms when possible or leave the door open when possible The items on the list were intended to stimulate Kaitlyn’s creativity. She might select some of the interventions directly from the list or generate some of her own. They would be introduced methodically but flexibly, deciding which targets to choose, which interventions to implement, and when to add or delete interventions. These choices would be determined by success achieved in gaining control over problem behaviors, and by Kaitlyn’s preferences in consultation with Dr. Benton. Interventions in the Bath: Kaitlyn and Dr. Benton decided to target the bath in the first effort to gain the upper hand over her BFRBs. What follows are specific interventions that were chosen by Kaitlyn. Also indicated are a few that were rejected for various reasons. For example, shifting from baths to showers was rejected because Kaitlyn thoroughly enjoyed her baths and would miss having them. Also, she worried that showers offered similar opportunities for BFRB behaviors to occur. Note that the interventions were not necessarily implemented in accordance with the order of the SCAMP domains. Often interventions in the place domain are implemented early in the process because of the relative ease of making environmental changes. Also, intervention tactics and their effects are not likely to be limited to any one SCAMP domain. Finally, all of the interventions indicated below were not implemented at the same time. Different combinations of them were chosen, implemented, and evaluated based on the judgment of Kaitlyn and Dr. Benton. Sensory Interventions: Limit visual cues, use candles instead of overhead lights, use bubble bath in the water. Limit tactile cues, wear light cotton gloves in bath when possible. Cognitive Interventions: A problem-solving approach was used. A decision was made to engage her dermatologist for laser removal of ingrown hairs. Regarding removal of “stubs,” Kaitlyn was encouraged to reframe them as “baby hairs” and get used to allowing them to grow out (later they would be removed with a depilation device recommended by her dermatologist). 334 Charles S. Mansueto Affective Interventions: Problem-solving in the cognitive and sensory domains greatly reduced Kaitlyn’s stress during bathing, thereby reducing the need to provide specific affective interventions for the bath. Motor Interventions: None deemed necessary, as all BFRB behaviors were focused. Place Interventions: Removed tweezers from the bathroom (see other tactics above, under Sensory Interventions). Interventions on the Phone with Mother: These recurrent BFRB episodes required a very different SCAMP-based plan than the bath. Sensory Interventions: None. Cognitive Interventions: Learned the importance of straightforward and assertive communication and, with some reading and practice, used her assertiveness skills with her mother; her mother agreed to prevent their phone conversations from falling into the patterns that Kaitlyn found so distressing; agreement was reached to limit phone calls to three times per week and to fifteen minutes’ duration. Affective Interventions: Practiced diaphragmatic breathing to reduce stress during conversations with her mother (also prepared for calls with five minutes of diaphragmatic breathing); Kaitlyn also practiced diaphragmatic breathing to alleviate work-related stress and other life stressors. Motor Interventions: Free hand was kept busy with manipulation of objects that provided pleasing sensations (after sampling a number of possibilities, she found that she preferred sensory substitutes with smooth, cool surfaces like polished stones, metal balls, etc.). She intentionally wore pants that were tight around the ankles and had drawstrings, which she would intentionally knot when she felt particularly vulnerable to picking. Place Interventions: Removed tweezers from the couch cushions and placed basket containing polished stones, bracelets, and other sensory substitutes within reach of the couch. Interventions for Mainly Automatic Pulling and Picking: The third SCAMPbased plan would address BFRB activity that was occurring in many different situations where hair was pulled from the scalp and scabs were picked from the legs, nibbled, and ingested. Sensory Interventions: Preferred sensory substitutes were kept available in places where automatic performance of BFRB behaviors were very likely (i.e., desk at work, armchair where she watched TV, etc.). Wearing bracelets consisting of large, smooth stones, keeping small hard candies available to provide an alternative to ingestion of BFRB products; hard candies were eventually replaced with taco chips that could be nibbled and swallowed in small pieces. Kaitlyn applied medicated ointment to her legs, which softened the scabs and made them taste unpleasant. Cognitive Interventions: Planning ahead to ensure that sensory interventions were available at necessary times and places; Kaitlyn reminded herself the Trichotillomania and Excoriation Disorder 335 baby hairs growing in her bald spot would help her regain healthy and attractive hair. Affective Interventions: Diaphragmatic breathing for emotional-regulation in “tense” situations where she might be vulnerable to BFRB activity; anticipated situations where she might be bored and kept stimulating activities available (e.g., apps on smartphone, crossword puzzles, news sites, email, etc.). Motor Interventions: Ensured free hands were occupied with sensory substitutes; bandages were worn on fingers employed in automatic pulling and picking (when it was not awkward to do so) to promote awareness. She engaged in activities that occupied her hands (e.g., grooming nails, needlepoint). She kept her fingernails short. Place Interventions: Sensory substitutes and stimulating activities were kept readily available; the occasional use of head coverings was discontinued because they made her scalp itch and that “invited pulling.” Phase 4: Evaluation, Termination, and Relapse Prevention Evaluation: Progress in therapy was monitored by weekly scores on the MGH Hair Pulling Scale (MGH/HPS) and the MGH Skin Picking Scale (MGH/SPS). These scales can be found in Appendices 16.1 and 16.2. Weekly scores through the course of 15 therapy sessions are shown in Figure 16.1. As Figure 16.1 shows, from the first therapy session through to the fifteenth therapy session, Kaitlyn’s scores on the MGH/HPS declined from 18 to 6. On the MGH/SPS her scores declined from 24 to 10. Self-recorded data, with approximate Progress in ComB Treatment 30 Score 23 15 8 0 1 2 3 4 5 6 7 8 9 10 11 12 13 Session MGH Hair Pulling Scale MGH Skin Picking Scale Figure 16.1. Kaitlyn’s progress in ComB treatment for two BFRBs. 14 15 336 Charles S. Mansueto numbers of hairs pulled, proved unreliable as a measure of BFRB severity. However, record keeping was used for other therapeutic purposes, such as raising awareness about critical variables associated with BFRBs. By all indications, Kaitlyn achieved a substantial reduction in her BFRB symptoms. Termination: Kaitlyn and Dr. Benton agreed to terminate treatment at session fifteen. Kaitlyn did not achieve total symptom cessation (which, while less than ideal, is not unusual), but she was pleased with her improvement. New hair growth was filling in her bald spot, she had begun laser treatments, and her skin was looking much better. She was hopeful that the techniques she learned in therapy would continue to serve her well. She was very optimistic about her prospects for a life unencumbered by BFRBs. Relapse Prevention: Dr. Benton had one final issue to discuss with Kaitlyn before she left his care. He cautioned her about the dangers of complacency in managing BFRBs. Research and clinical experience tell us that “slips” (sudden symptom recurrence) are almost inevitable when recovering from BFRBs. It is illadvised to think in terms of “cure” and prudent to think in terms of “management.” In precaution against a full-blown relapse, Kaitlin was provided with a relapse prevention plan to implement should a slip occur. This included the following steps: 1. 2. 3. 4. Phase out interventions gradually, and reinstate them as needed. Remain vigilant about returning urges. Maintain involvement with an online BFRB support group. Anticipate challenging life circumstances, and remain prepared BFRB resurgence. 5. Return to a multifaceted self-help plan in the event of a major slip. 6. Schedule an additional “booster” therapy session on an as-needed basis. for Comments and Conclusions Evidence in Support of ComB Treatment ComB treatment is a conceptual model based on established behavioral principles and sound theoretical formulations derived from decades of laboratory and clinical research. Many specific interventions, tailored for ComB treatment, are familiar transdiagnostic CBT techniques. These treatment components comprise a wide range of behavioral and cognitive techniques frequently described in the scientific literature and used extensively by thousands of CBT practitioners to treat a broad range of disorders. While ComB has yet to be tested in a randomized controlled paradigm, research efforts are underway to bolster empirical support. A treatment manual for ComB was developed (Mouton-Odum et al., 2013) and was utilized in a recent pilot test of ComB efficacy (Falkenstein et al., 2016). Uncontrolled preliminary data showed that ComB treatment reduced HPD symptom severity and impairment with substantial effects, and with a modest decline in improvement at three-month Trichotillomania and Excoriation Disorder follow-up. A current study is underway to study ComB treatment in a randomized trial with a minimal attention-placebo control. A future study is planned in which the efficacy of ComB is compared head-to-head with HRT. In the clinical realm, hundreds of therapists have been trained in the ComB treatment approach through the Professional Training Institute of the TLC Foundation for BFRBs. Many clinicians have adopted the ComB approach, having acquired informal training through various mechanisms, such as exposure to written accounts in the professional literature (Mansueto et al., 1999; Stemberger et al., 2000, 2003) and by viewing a ComB training series, TLC’s Virtual Professional Training Institute, produced and distributed by the TLC Foundation. While this chapter has focused on treatment for adults with BFRBs, with minor modifications the ComB treatment approach has been adapted for use with children and adolescents by many clinicians for individual therapy applications and for self-help (Golomb & Vavrichek, 2000). ComB Treatment in Perspective While the need exists for further outcome research to determine whether ComB treatment is most effective and efficient for the individual who suffers from BFRB, decades of clinical observations and testimonials by numerous expert clinicians support the following conclusions: ComB provides a likely effective alternative to existing CBT approaches. ComB addresses the diverse and idiosyncratic elements that foster BFRBs in user-friendly form. ComB guides assessment of information relevant to an individual’s BFRB and organizes it into categories recognized as valid and useful. ComB helps generate a wide variety of possible therapeutic interventions. ComB guides the therapist and patient through a collaborative process of clinical decision making, ensuring that therapy fits well with the unique characteristics of each patient. At this time, no other single treatment for BFRBs has been recognized as providing these advantages within an integrated conceptual framework and comprehensive treatment approach. REFERENCES American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders (3rd ed., revised) (DSM-III-R). American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.) (DSM-5). American Psychiatric Association. Arnold, L. M., McElroy, S. L., Mutasim, D. F., Dwight, M. M., Lamerson, C. L., & Morris, E. M. (1998). Characteristics of 34 adults with psychogenic excoriation. Journal of Clinical Psychiatry, 59(10), 509–514. 337 338 Charles S. Mansueto Azrin, N. H., & Nunn, R. G. (1973). Habit-reversal: A method of eliminating nervous habits and tics. Behaviour Research and Therapy, 11(4), 619–628. doi:10.1016/0005-7967(73) 90119-8. (1977). Habit control: Stuttering, nail biting, and other nervous habits. Simon and Schuster. Azrin, N. H., Nunn, R. G., & Frantz, S. E. (1980). Treatment of hairpulling (trichotillomania): A comparative study of habit reversal and negative practice training. Journal of Behavior Therapy and Experimental Psychiatry, 11(1), 13–20. doi:10.1016/0005-7916(80)90045-2 Bloch, M. H., Landeros-Weisenberger, A., Dombrowski, P., Kelmendi, B., Wegner, R., Nudel, J., Pittenger, C., Leckman, J. F., & Coric, V. (2007). Systematic review: Pharmacological and behavioral treatment for trichotillomania. Biological Psychiatry, 62(8), 839–846. doi:10.1016/j.biopsych.2007.05.019. Chamberlain, G. A., Fineberg, N. A., & Odlaug, B. L. (2012). Pharmacotherapy. In J. E. Grant, D. J. Stein, D. Woods, & N. J. Keuthen (Eds.), Trichotillomania, skin picking, and other body-focused repetitive behaviors. American Psychiatric Publishing. Christenson, G. A., & Mackenzie, T. B. (1994). Trichotillomania. In M. Henson & R. T. Ammerman (Eds.), Handbook of prescriptive treatments for adults. Plenum. Christenson, G. A., Mackenzie, T. B., & Mitchell, J. E. (1991). Characteristics of 60 adult chronic hair pullers. American Journal of Psychiatry, 148(3), 365–370. doi:10.1176/ajp.148.3.365 Christenson, G. A., & Mansueto, C. S. (1999). Trichotillomania: Descriptive characteristics and phenomenology. In D. J. Stein, G. A. Christenson, & E. Hollander (Eds.), Trichotillomania. American Psychiatric Press. Christenson, G. A., Ristvedt, S. L., & Mackenzie, T. B. (1993). Identification of trichotillomania cue profiles. Behaviour Research and Therapy, 31(3), 315–320. doi:10.1016/00057967(93)90030-x Falkenstein, M. J., Mouton-Odum, S., Mansueto, C. S., Golomb, R. G., & Haaga, D. A. F. (2016). Comprehensive behavioral treatment of trichotillomania: A treatment development study. Behavior Modification, 40(3), 414–438. doi:10.1177/0145445515616369 Flessner, C. A. (2012). Diagnosis and comorbidity. In J. E. Grant, D. J. Stein, D. Woods, & N. J. Keuthen (Eds.), Trichotillomania, skin picking, and other body-focused repetitive behaviors. American Psychiatric Publishing. Flessner, C. A., Busch, A. M., Heideman, P. W., & Woods, D. W. (2008). Acceptanceenhanced behavior therapy (AEBT) for trichotillomania and chronic skin picking. Behavior Modification, 32(5), 579–594. doi:10.1177/0145445507313800 Flessner, C. A., & Woods, D. W. (2006). Phenomenological characteristics, social problems, and the economic impact associated with chronic skin picking. Behavior Modification, 30 (6), 944–963. doi:10.1177/0145445506294083 Gianoli, M. O., & Tolin, D. F. (2012). Cognitive-behavioral therapy for pediatric trichotillomania. In J. E. Grant, D. J. Stein, D. Woods, & N. J. Keuthen (Eds.), Trichotillomania, skin picking, and other body-focused repetitive behaviors. American Psychiatric Publishing. Gluhoski, V. L. (1995). A cognitive approach for treating trichotillomania. Journal of Psychotherapy Practice and Research 4, 277–285. Golomb, R., Franklin, M., Grant, J. E., Keuthen, N. J., Mansueto, C. S., Mouton-Odum, S., Novak, C., & Woods, D. (2011). Expert consensus treatment guidelines for trichotillomania, skin picking, and other body-focused repetitive behaviors. Scientific Advisory Board of the Trichotillomania Learning Center. Golomb, R. G., & Vavrichek, S. M. (2000). The hair pulling “habit” and you: How to solve the trichotillomania puzzle. Writers’ Cooperative of Greater Washington. Grant, J. E., Chamberlain, S. R., & Odlaug, B. L. (2012). Alternative treatments. In J. E. Grant, D. J. Stein, D. Woods, & N. J. Keuthen (Eds.), Trichotillomania, skin picking, and other body-focused repetitive behaviors. American Psychiatric Publishing. Trichotillomania and Excoriation Disorder Grant, J. E., Levine, L., Kim, D., & Potenza, M. N. (2005). Impulse control disorders in adult psychiatric inpatients. American Journal of Psychiatry, 162(11), 2184–2188. doi:10.1176/ appi.ajp.162.11.2184 Grant, J. E., & Odlaug, B. L. (2009). The obsessive-compulsive spectrum and disorders of the skin: A review. Expert Review of Dermatology, 4, 523–532. Hayes, S. C., Strosahl, K., & Wilson. K. G. (1999). Acceptance and commitment therapy: An experiential approach to behavior change. Guilford Press. Kabat-Zinn, J., & Chapman-Waldrop, A. (1988). Compliance with an outpatient stress reduction program: Rates and predictors of completion. Journal of Behavioral Medicine, 11, 333–352. Keijsers, G. P. J., Van Minnen, A., Hoogduin, C. A., Klaassen, B. N. W., Hendriks, M. J., & Tanis-Jacobs, J. (2006). Behavioural treatment of trichotillomania: Two-year follow-up results. Behaviour Research and Therapy, 44(3), 359–370. doi:10.1016/j.brat.2005.03.004 Keuthen, N. J., Aronowitz, B., Badenoch, J., & Wilhelm, S. 1999. Behavioural treatment for trichotillomania. In D. J. Stein, G. A. Christenson, & E. Hollander (Eds.), Trichotillomania. American Psychiatric Press. Keuthen, N. J., Fraim, C., Deckersbach, T., Dougherty, D. D., Baer L., & Jenike, M. A. (2001a). Longitudinal follow-up of naturalistic treatment outcome in patients with trichotillomania. The Journal of Clinical Psychiatry, 62(2), 101–107. doi:10.4088/jcp.v62n0205 Keuthen, N. J., O’Sullivan, R. L., Ricciardi, J. N., Shera, D., Savage, C. R., Borgmann, A. S., Jenike, M. A., & Baer, L. (1995). The Massachusetts General Hospital (MGH) Hairpulling Scale: 1. Development and factor analyses. Psychotherapy and Psychosomatics, 64(3–4), 141–145. Keuthen, N. J., Rothbaum, B. O., Welch, S. S., Taylor, C., Falkenstein, Martha, Heekin, M., Jordan, C. A., Timpano, K., Meunier, S., Fama, J., & Jenike, M. A. (2010). Pilot trial of dialectical behavior therapy-enhanced habit reversal for trichotillomania. Depression and Anxiety, 27(10), 953–959. doi:10.1002/da.20732 Keuthen, N. J., Wilhelm, S., Deckersbach, T., Engelhard, I. M., Forker, A. E., Baer L., & Jenike, M. A. (2001b). The Skin Picking Scale: Scale construction and psychometric analyses. Journal of Psychosomatic Research, 50(6), 337–341. Lazarus, A. A. (1981). The practice of multimodal therapy. McGraw-Hill. Lerner, J., Franklin, M. E., Meadows, E. A., Hembree, E., & Foa, E. B. (1998). Effectiveness of a cognitive behavioral treatment program for trichotillomania: An uncontrolled evaluation. Behavior Therapy, 29(1), 157–171. doi:10.1016/s0005-7894(98)80036-1 Linehan, M. M. (1993). Cognitive behavioral treatment of borderline personality disorder. Guilford Press. Mansueto, C. S. (1990). Typography and phenomenology of trichotillomania. Paper presented at meeting of the Association for the Advancement of Behavior Therapy, San Francisco, CA, November. (1991). Trichotillomania in focus. OCD Newsletter of the Obsessive Compulsive Foundation, 5(3), 10–11. Mansueto, C. S., Goldfinger-Golomb, R., McCombs-Thomas, A., & Townsley-Stemberger, R. M. (1999). A comprehensive model for behavioral treatment of trichotillomania. Cognitive and Behavioral Practice, 6(1), 23–43. doi:10.1016/s1077-7229(99)80038-8 Mansueto, C. S., & Rogers, K. E. (2012). Trichotillomania: Epidemiology and clinical characteristics. In J. E. Grant, D. J. Stein, D. Woods, & N. J. Keuthen (Eds.), Trichotillomania, skin picking, and other body-focused repetitive behaviors. American Psychiatric Publishing. Mansueto, C. S., Townsley-Stemberger, R. M., McCombs-Thomas, A., & GoldfingerGolomb, R. (1997). Trichotillomania: A comprehensive behavioral model. Clinical Psychology Review, 17(5), 567–577. doi:10.1016/s0272-7358(97)00028-7 339 340 Charles S. Mansueto Mansueto, C. S., Vavricheck, S. M., & Golomb, R. G. (n.d.). Overcoming hair pulling and skin picking for good: A self-help guide to comprehensive behavioral (ComB) treatment [Unpublished manuscript]. McGuire, J. F., Ung, D., Selles, R. R., Rahman, O., Lewin, A. B., Murphy, T. K., & Storch, E. A. (2014). Treating trichotillomania: A meta-analysis of treatment effects and moderators for behavior therapy and serotonin reuptake inhibitors. Journal of Psychiatric Research 58, 76–83. doi:10.1016/j.jpsychires.2014.07.015 Miltenberger, R. G., & Fuqua, R. W. (1985). A comparison of contingent vs non-contingent competing response practice in the treatment of nervous habits. Journal of Behavior Therapy and Experimental Psychiatry, 16(3 ),195–200. doi:10.1016/0005-7916(85)90063-1 Mouton, S. G., & Stanley, M. A. (1996). Habit reversal training for trichotillomania: A group approach. Cognitive and Behavioral Practice, 3(1), 159–182. doi:10.1016/s1077-7229(96) 80036-8 Mouton-Odum, S., Mansueto, C. S., & Golomb, R. G. (2013). Manual for comprehensive behavioral treatment of trichotillomania [Unpublished manual]. Odlaug, B. L., & Grant, J. E. (2012). Pathological skin picking. In J. E. Grant, D. J. Stein, D. Woods, & N. J. Keuthen (Eds.), Trichotillomania, skin picking, and other body-focused repetitive behaviors. American Psychiatric Publishing. O’Sullivan, R. L., Mansueto, C. S., Lerner, E. A., & Miguel, E. C. (2000). Characterization of trichotillomania: A phenomenological model with clinical relevance to obsessivecompulsive spectrum disorders. Psychiatric Clinics of North America, 23(3), 587–604. Rollnick, S., & Miller, W. (1995). What is motivational interviewing? Behavioural and Cognitive Psychotherapy, 23, 325–334. doi:10.1017/S135246580001643X Rosenbaum, M. S., & Ayllon, T. (1981). The habit-reversal technique in treating trichotillomania. Behavior Therapy, 12(4), 473–481. doi:10.1016/s0005-7894(81)80085-8 Rothbaum, B. O. (1992). The behavioral treatment of trichotillomania. Behavioral Psychotherapy, 20, 85–90. Schumer, M. C., Bartley, C. A., & Bloch, M. H. (2016). Systematic review of pharmacological and behavioral treatments for skin picking disorder. Journal of Clinical Psychopharmacology, 36(2), 147–152. doi:10.1097/JCP.0000000000000462 Stemberger, R. M., Stein, D. J., & Mansueto, C. S. (2003). Behavioral and pharmacological treatment of trichotillomania. Brief Treatment and Crisis Intervention, 3, 339–352. Stemberger, R. M. T., Thomas, A. M., Mansueto, C. S., & Carter, J. G. (2000). Personal toll of trichotillomania: Behavioral and interpersonal sequelae. Journal of Anxiety Disorders, 14(1), 97–104. doi:10.1016/S0887-6185(99)00028-6 Tarnowski, K. J., Rosén, L. A., McGrath, M. L., & Drabman, R. S. (1987). A modified habit reversal procedure in a recalcitrant case of trichotillomania. Journal of Behavior Therapy and Experimental Psychiatry, 18(2), 157–163. doi:10.1016/0005-7916(87)90030-9 van Minnen, A., Hoogduin, K. A. L., Keijsers, G. P. J., Hellenbrand, I., & Hendriks, G.-J. (2003). Treatment of trichotillomania with behavioral therapy or fluoxetine. Archives of General Psychiatry, 60(5), 517–522. doi:10.1001/archpsyc.60.5.517 Walsh, K. H., & McDougle, C. J. (2001). Trichotillomania: Presentation, etiology, diagnosis, and therapy. American Journal of Clinical Dermatology 2, 327–333. Woods, D. W., Wetterneck, C. T., & Flessner, C. A. (2006). A controlled evaluation of acceptance and commitment therapy plus habit reversal for trichotillomania. Behaviour Research and Therapy, 44(5), 639–656. doi:10.1016/j.brat.2005.05.006 17 Cognitive Behavioral Therapy for Hoarding Disorder Caitlin A. Stamatis, McKenzie K. Roddy, and Kiara R. Timpano Overview of Hoarding Disorder The three hallmark characteristics of hoarding disorder (HD) include difficulties discarding, excessive acquiring, and clutter (Frost & Hartl, 1996; Pertusa et al., 2010). HD symptoms are dimensionally distributed (Timpano et al., 2013), ranging from normative saving and collecting behaviors to extreme hoarding tendencies, with approximately 1.5–3% of the population meeting criteria for HD (Nordsletten et al., 2013; Timpano et al., 2011). In extreme cases, excess clutter hinders basic activities of daily living and contributes to dangerous living conditions (Frost et al., 2000), while acquiring tendencies can cause substantial monetary difficulties (Frost et al., 2009; Mueller et al., 2007). Beyond the core features, HD is also associated with high levels of comorbidity across both psychiatric (e.g., depression) and healthrelated (e.g., chronic pain) syndromes. Given these considerations, along with the fact that hoarding-related impairments extend past the individual to include economic and societal burdens, HD has been identified as a significant public health crisis (Tolin et al., 2008). Consequently, developing and refining therapeutic interventions for individuals with hoarding disorder constitutes a critical step in reducing hoarding-related burden. Case Vignette Ron is a 71-year-old, single, Caucasian male who self-referred to at an outpatient clinic for individual therapy to address symptoms of hoarding, which he stated had worsened since losing his wife 10 years prior. He presented primarily with distress around the amount of clutter in his two-bedroom house, as well as in his two storage units. Ron also endorsed low mood, which he attributed to a combination of his hoarding difficulties and perceived uncertainty about the future. Ron had recently retired from working as an accountant, lost his house to foreclosure, and moved into a smaller home owned by his son. Ron hoped to spend his retirement traveling and spending time with his grandchildren. However, he felt “trapped” and “dirty” due to the clutter, which also prevented him from having visitors in his home. 341 342 Stamatis, Roddy, and Timpano Etiology of Hoarding Understanding the etiological model for HD, including vulnerability and maintaining factors, is essential for accurately conceptualizing cases and executing treatment plans. According to cognitive behavioral models of hoarding, risk for HD stems from a combination of genetic and familial factors, information-processing deficits, cognitive beliefs, emotional responses, and reinforcement learning. Research on risk factors points to a strong heritable component, with approximately 50% of the variance explained by genetic factors (Hirschtritt & Mathews, 2014; Iervolino et al., 2009). Various candidate genes, particularly those regulating serotonergic function, have been posited as relevant to hoarding (Hirschtritt & Mathews, 2014), though conclusive findings are lacking. Family values and parenting behaviors have also been found to influence hoarding risk (Landau et al., 2011), with studies indicating that family beliefs about saving and wastefulness are commonly reported in adults with HD (Gilliam & Tolin, 2010). Additionally, early life stress and trauma have been linked with risk of hoarding behaviors (Cromer et al., 2007; Tolin et al., 2010). Individual differences in personality traits (e.g., perfectionism, dependency, and paranoia), along with transdiagnostic cognitive and emotional risk factors (e.g., distress tolerance, anxiety sensitivity), represent additional facets that may contribute to HD (Timpano et al., 2011). Patients with HD often exhibit patterns of cognitive impairment, which are theorized to reflect a more general information processing risk that may be present prior to the onset of clinically significant hoarding symptoms (Woody et al., 2014). Deficits in executive function, attention, and memory constitute the primary information-processing abnormalities observed in and reported by patients with HD (Morein-Zamir et al., 2014). Patients with HD often display symptoms of attention-deficit/hyperactivity disorder (ADHD), including tangentiality and difficulty sustaining attention, which may interfere with sorting and discarding processes (Tolin & Villavicencio, 2011; Weintraub et al., 2018). Difficulties with categorizing objects and, in particular, difficulties with making decisions have also been associated with the core features of HD. Finally, while overall memory deficits are not observed in HD, patients with hoarding report poorer confidence in their memory, along with greater reliance on visual memory cues (Hartl et al., 2004). Jointly, these findings point toward the notion that HD is associated with a general deficit in selfregulatory abilities (Timpano & Schmidt, 2013), a hypothesis supported by emerging neuroimaging research on HD (Slyne & Tolin, 2014). The handful of extant neuroimaging studies on HD indicate that saving tendencies are linked with abnormalities in cognitive and affective brain circuits, including the orbitofrontal cortex, dorsal anterior cingulate cortex, and temporal regions (Mataix-Cols et al., 2004; Saxena et al., 2004; Tolin et al., 2009, 2012). Along with the aforementioned cognitive and biological risk factors, core beliefs contributing to hoarding symptoms include cognitions about the self, possessions, responsibility, memory, and control (Frost & Hartl, 1996). Individuals at risk for HD may report greater valuation of possessions in terms of instrumental value, CBT for Hoarding Disorder intrinsic beauty, sentimental value, and comfort (Frost et al., 1995; Grisham et al., 2009). In the same way as individuals with depressive and anxiety spectrum disorders, patients with hoarding often report negative beliefs about the self, including a sense of vulnerability and helplessness, along with negative thoughts about likability and social relationships. More unique to hoarding pathology are thoughts relating to saving objects, including beliefs about memory (e.g., “This object tells a story”), responsibility (e.g., “I am responsible for this possession”), and control (e.g., “I must ensure that things are sorted the right way”; Frost et al., 1998; Steketee et al., 2003). Similarly, core beliefs about control, safety, and opportunity have been linked with excessive acquiring (Kyrios et al., 2004). Negative beliefs in hoarding are strengthened through a combination of positive and negative reinforcement loops, which contribute to the core symptoms of excessive acquiring, difficulty discarding, and clutter. For example, discarding will invariably elicit strong negative emotions for individuals with hoarding (e.g., distress, anger, grief ), and patients will subsequently be less likely to actually discard in order to avoid these emotions. In contrast, the positive emotions experienced when acquiring new objects can reinforce collecting behaviors. Assessment Assessment for HD covers five major symptom categories: difficulties discarding and acquiring, clutter, problems of living, saving cognitions, and comorbid conditions (Frost & Hristova, 2011). In addition to helping define the severity of hoarding for a particular patient, the assessment process represents a key step in conceptualizing the case. Throughout the assessment and case conceptualization process, it is helpful to keep the general etiological model of hoarding in mind (see Figure 17.1) and to begin mapping the patient’s own experiences and relevant components onto the model. The different assessment categories described below, along with relevant measures for each category, are intended to help clinicians map out an individual patient’s idiographic model of hoarding (see Figure 17.2 for a blank copy of the model). The assessment process with patients with HD is complicated by several factors that deserve separate consideration. First and foremost is the issues present by variable levels of insight and motivation. For example, patients may minimize reports of clutter for a number of distinct reasons: one patient could underreport impairment due to clutter because she views her possessions as positive and egosyntonic, whereas a second may minimize reports of clutter due to shame or embarrassment. By using mutual language to describe hoarding behaviors and possessions, the clinician may increase transparency of reporting. It is particularly important to avoid the use of judgmental language (e.g., “junk”) and to help reduce the impact of stigma the patient may be experiencing, including self-stigma. For example, if a client refers to the clutter in their home as their “collection of treasures,” the therapist might use the phrase “collection” during the assessment phase to reinforce the no-judgmental stance. During the treatment phase, the 343 344 Stamatis, Roddy, and Timpano Environment Indecision Depression and Anxiety Stressful Life Events Core Vulnerabilities and Comorbidity Genetic Factors Selfreferential beliefs Neurobiology Coping InformationProcessing Deficits Object Intrinsic valuation Emo-tion-al-ly Cognitive Styles and Beliefs Individual Differences Object Attachment Poor planning Memory Object Instrumental valuation Problemsolving deficits Organization difficulties Attention deficits Interpersonal Attachment Emotional Responses and Processes Positive Reinforcement Negative Reinforcement · Positive Emotions · Negative Emotions · Approach behaviors · Avoidance Behaviors Acquiring Difficulties Discarding Clutter Figure 17.1. Etiological model of hoarding disorder. therapist would then help the client understand that their “collection” is the result of HD. Another example might be the term used to describe HD. If a patient is more comfortable with being called a “pack rat” or a “collector,” then these terms should be used by the therapist. A second issue to consider is that the average treatment-seeking patient with HD is likely to be an older adult. Consequently, clinicians should be prepared for the assessment process to take more time and potentially require special accommodations. The American Psychological Association’s “Guidelines for Psychological Practices with Older Adults” represents a helpful framework for managing additional issues that may arise during assessment with this population (American Psychological Association, 2014). A third consideration is that family members may be directly or indirectly impacted by the HD symptoms. It is not uncommon for family members to be a driving force behind treatment-seeking behavior, which may reflect the patient’s ambivalence about changing. Sometimes family members can be helpful in providing a more objective assessment of the hoarding symptoms and associated CBT for Hoarding Disorder 345 Memory Core Vulnerabilities and Comorbidity InformationProcessing Deficits Cognitive Styles and Beliefs Approach Behaviors · · · · Emotional Responses and Processes Positive Reinforcement · Positive Emotions • Negative Emotions · · · · Acquiring SIR A = CAS = Negative Reinforcement Difficulties Discarding SIR D = HRS = Avoidance Behaviors · · · · Clutter SIR C = CIR = Figure 17.2. Blank copy of hoarding case conceptualization model. difficulties. At the same time, the family may also be experiencing extremely high levels of discord (e.g., arguments, criticism, and rejection) relating to the patient’s hoarding behaviors (Tolin et al., 2008). Final consideration for completing an assessment with hoarding patients is that the level of clutter may present true safety risks for the patient and anyone living in the hoarded home. Inasmuch as the impacted individuals include children or elderly individuals, relevant reporting laws may have to be taken into account. Symptom Severity Symptom severity of HD should be assessed at intake and throughout treatment to monitor progress. The Saving Inventory-Revised (SI-R; Frost et al., 2004) is a 23item self-report measure that divides into three subscales: difficulty discarding, acquiring, and clutter. The SI-R is both reliable and valid within a hoarding population and demonstrates discriminative validity between hoarding and other mood symptoms. A cutoff total score of 41 is associated with probable diagnosis, with 62 representing the average score for patients with HD and 24 representing the 346 Stamatis, Roddy, and Timpano average score for individuals without HD (Frost et al., 2004; Muroff et al., 2014; Tolin et al., 2011). The Hoarding Rating Scale (HRS; Tolin et al., 2013) is an additional severity instrument that is ideal for ongoing monitoring. The HRS can be used either as a clinician-administered interview or as a self-report measure. This scale is commonly used in community settings due to its high validity and brief format, with five items rated on a Likert-type scale from no problem (0) to extreme difficulties (8). The five items assess the main features of HD, including difficulty discarding, acquisition, clutter, functional impairment, and distress. Of note, a client must score at or above a 4 on the items measuring clutter, difficulty discarding, and either distress or functional impairment in order to meet criteria for HD. A total score of 14 or greater is indicative of clinical levels of HD (Tolin et al., 2010). Clutter As previously discussed, clients often struggle to accurately estimate the amount of clutter in their homes. A helpful tool for more accurately assessing clutter severity is the Clutter Image Rating Scale (CIR; Frost et al., 2008). The CIR provides nine photographs of a bedroom, kitchen, and living room, each with increasing amounts of clutter (rated 1 to 9, with 4 considered the clinical cutoff ). Clients are instructed to view the pictures and rate from 1 to 9 the amount of clutter for each room in their house is that is considered their domain. Using the general living room photo from the CIR, clinicians should also assess storage areas such as garages, basements, storage units, attics, and any additional rooms in the home. It is helpful to emphasize that clients should rate the volume of clutter rather than the content, which may look very different from the items pictured. In general, ratings should be based only on areas that are fully under the client’s control, as spouses or family members will often limit or control the amount of clutter in shared spaces. The CIR is especially informative when used in conjunction with photos of the client’s home or an actual visit to the home, which allows clinicians to consider both client perceptions and their own clinical ratings of available data. To facilitate this process, clinicians may ask patients to print photos of their living spaces prior to the assessment session, or to bring in photos on their phone. Acquiring Although the SIR provides a nice snapshot of the severity of any acquiring behavior, it may be necessary to include a more detailed assessment of the types of acquiring that a patient may be doing (Frost et al., 2009). While the most common method of acquisition is purchasing items (active acquiring), other objects may be acquired by collecting free items (e.g., giveaways or items discarded by others). The Compulsive Acquisition Scale (CAS; Frost et al., 2002) includes two subscales that capture buying behaviors and the excessive acquisition of free objects. A cutoff of 48 has been found to distinguish those with clinically significant collecting behaviors from normative acquiring tendencies (Frost et al., 2009). A final consideration is that some individuals with HD may also endorse stealing objects (e.g., taking CBT for Hoarding Disorder magazines from waiting rooms or a roll of toilet paper from work) as a means of acquiring (Timpano et al., 2011). Although this form of acquiring appears to be rare, clinicians should be aware of the possibility (Frost et al., 2013). Problems of Living Clinical levels of clutter can interfere with necessary tasks (e.g., bills get lost and go unpaid) and restrict functionality of the home (e.g., cluttered furniture prevents cooking in the kitchen or bathing in the shower). In more extreme cases, clutter can obstruct pathways or entire rooms, creating fire and safety hazards; consequently, problems of living represent a crucial area of consideration during assessment of HD symptoms. Along with patient and family member reports of problems of living, professionals in the community who interact with patients with HD (e.g., social workers and firefighters) may provide valuable insight into the severity of HD-related interference in daily life. The HOMES Multidisciplinary Risk Assessment (HOMES; Bratiotis, 2011) was designed as in inclusive measure of assessing HD-associated problems of living. The checklist is a straightforward means of assessing health, mental health, obstacles, endangerment, and structure and safety. For a more in-depth view, the Activities of Daily Living for Hoarding (ADL-H; reported in Grisham et al., 2006) is a self-report scale that assesses the extent to which HD symptoms interfere with everyday activities such as bathing, preparing meals, and accomplishing daily tasks. The ADL-H contains 16 items assessing activities of living, as well as seven items assessing quality of living conditions and six items assessing health and safety. Saving Cognitions A measure of saving cognitions is particularly useful for identifying problematic thinking patterns that can be addressed during cognitive behavioral therapy (CBT) for HD. The Savings Cognitions Inventory (SCI; Steketee et al., 2003) is a 23-item scale that consists of four subscales regarding beliefs about saving. Specifically, the subscales measure desire for control over items, responsibility for possessions, emotional attachment, and concerns about memory. Clinicians should additionally assess for interpersonal or attachment difficulties, along with patient coping styles and emotionality, all of which can shape an individual’s manifestation of HD. Comorbid Conditions In addition to hoarding-specific symptomology, it is important to complete a thorough intake assessment and identify any comorbid conditions. Depressive symptoms, social anxiety, generalized anxiety, and ADHD are all commonly comorbid with HD and can interfere with treatment if not properly addressed (Frost et al., 2011; Hall et al., 2013). Additionally, although HD is classified by DSM-5 as an obsessive-compulsive spectrum disorder and a diagnosis separate from OCD, individuals with comorbid OCD with contamination concerns may struggle with components of HD treatment such as allowing assessors or therapists into their home. Understanding how additional diagnoses contribute to individual vulnerabilities is critical to case conceptualization, discussed below. 347 348 Stamatis, Roddy, and Timpano Case Vignette: Assessment During Ron’s intake session, the therapist conducted the Structured Clinical Interview for DSM-5 (SCID-5) (First & Williams, 2016), with the goal of gaining insight into Ron’s hoarding and depressive symptoms, as well as ruling out OCD given his comments about the “dirty” feeling surrounding clutter. Based on the SCID-5, Ron met criteria for hoarding disorder, as well as major depressive disorder, mild, single episode. His concerns about dirt relating to the clutter were attributable to the dust and mold growing in his storage units, and he denied ritualistic behaviors relating to these concerns, indicating that they were unlikely to represent a symptom of OCD but rather represented realistic appraisals of hoarding-related consequences. Ron did not endorse any excessive acquiring behaviors. Various hoarding-specific measures were utilized to obtain a more comprehensive picture of Ron’s condition. From the HRS, Ron’s symptoms appeared to be on the more severe end (total score = 34/40), which was supported by his ratings of 6 and higher on the CIR of photos of his bedroom, which he considered his personal domain in the home. Ron’s primary reasons for saving, gleaned from the SCI, were generally related to memory and responsibility. This information was used to conceptualize Ron’s case (Figure 17.3), which was subsequently used for treatment planning. Ron had very few acquiring behaviors, thus treatment was focused on his difficulty discarding. Additionally, we did not assess for problems with living (e.g., HOMES) because Ron functioned successfully in the professional sphere for many years, and was currently living with his son. Overview of Available Treatments for Hoarding Disorder Given the complexity of both the clinical characteristics and associated features of HD, it is perhaps not surprising that hoarding has historically been acknowledged as a difficult treatment target (Abramowitz et al., 2003; Bloch et al., 2014; Pertusa et al., 2010). In addition to heterogeneous presentations and complex comorbidity patterns, clients with HD often exhibit low insight and motivation. Furthermore, very few clinicians are trained to accurately assess and diagnose HD or provide effective treatments. In spite of these challenges, a handful of empirically supported treatments have been developed and tested to treat hoarding disorder. In particular, since the addition of hoarding disorder as an independent diagnostic entity to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013), the literature on treating hoarding independent of OCD has grown substantially (Timpano et al., 2016; Tolin et al., 2015). The best-supported form of HD treatment is CBT for hoarding, which is discussed in detail in a later section. Immediately below, we briefly summarize alternative treatment modalities applied to HD and the current evidence for their efficacy. CBT for Hoarding Disorder 349 Recent widower Decisionmaking difficulties Depression Core Vulnerabilities and Comorbidity Pressure from chilldren Lost home to foreclosure Memory Responsibility Cognitive Styles and Beliefs Recent retirement Need to control objects InformationProcessing Deficits Fear of regret Poor planning Instrumental value Avoidance Behaviors Emotional Responses and Processes Approach Behaviors anything tied with fond memories · Souvenirs from travels · Unproductive churning · Saving Positive Negative Reinforcement Reinforcement · Positive Emotions · Negative Emotions Pleasure; joy; Sadness; anxiety nostalgia Acquiring Difficulties Discarding Clutter SIR A = 9 CAS = 24 SIR D = 26 HRS = 34/40 SIR C = 24 CIR = 6 · Decisions about objects · No planning for future · Multiple (unnecessary) storage units · Lack of follow-through · Avoidance of certain stores Figure 17.3. Ron’s case conceptualization. Pharmacological Treatments A limited number of pharmacological interventions have been tested as a treatment for hoarding with and without comorbid OCD (Timpano et al., 2016). Results from a recent meta-analysis indicate that selective serotonin reuptake inhibitors (SSRIs) (specifically, paroxetine and sertraline), along with the serotonin and norepinephrine reuptake inhibitor (SSNRI) venlafaxine, are the most well-supported pharmacologic treatments for HD (Brakoulias et al., 2015). More limited evidence exists regarding the efficacy of medications indicated for the treatment of ADHD, such as methylphenidate and atomoxetine (Grassi et al., 2016; Rodriguez et al., 2013), to target deficits in attention and executive function frequently observed in HD. A larger issue relevant for using pharmacotherapy to treat HD, which is documented in several case studies, is a general reluctance of patients with HD to pursue medications. Family Treatments Given the influence of the patient’s clutter, saving, and acquiring on the household, hoarding tendencies can have a secondary, albeit significant, negative impact on Attentional focus 350 Stamatis, Roddy, and Timpano family members, who in turn may be involved in managing or accommodating patient behaviors. Family-focused interventions for hoarding may constitute a particularly helpful alternative treatment when patients with HD exhibit poor motivation or insight (Tompkins & Hartl, 2013). Components of family therapy for HD include psychoeducation about HD, harm reduction techniques, and motivational interviewing skills. In addition, relatives are taught about the role of family accommodation in maintaining HD symptoms, as well as ways of reducing accommodation (Chasson et al., 2014). Community-Focused Interventions HD may confer a number of problems impacting the community, including potential evictions, fire and health hazards, and suspected cases of neglect. Accordingly, mental health professionals must often collaborate with other service providers and professionals enforcing health and safety codes to best serve a client with HD. Various models have been developed to characterize coordinated service intervention for HD (Bratiotis & Woody, 2014). Community-based models range from informal partnerships to formalized hoarding task forces, which function in the areas of case consultation and treatment, while also pursuing policy change and advocacy work (Bratiotis, 2013). Poised to tackle a unique challenge among psychological treatments, community interventions for HD must balance the needs of the patient (e.g., manage housing issues, retaining control over decision-making regarding possessions) and of the broader community (e.g., reducing safety risks and sanitation issues, promoting compliance with local laws). For the clinician, this may involve implementing shorter-term harm-reduction strategies, which aim to reduce clutter to a level that is no longer an active safety concern, prior to beginning longer-term work on core hoarding symptoms such as difficulty discarding (Tompkins, 2015). Cognitive-Behavioral Therapy for Hoarding Evidence Basis for CBT for HD As previously indicated, CBT for hoarding disorder boasts the greatest empirical support. CBT for hoarding was created to provide therapists with a manualized, skills-based approach to treating individual clients with HD (Steketee et al., 2000). The specialized protocol for hoarding has since been adapted and tested in group format, with a growing number of clinical trials supporting the efficacy of group CBT for HD (Gilliam et al., 2011; Muroff et al., 2009, 2012; Steketee et al., 2010). Additionally, CBT for HD has been adapted for special populations, including group CBT for older adult clients (Ayers et al., 2011). There have also been versions of the treatment created in self-help and web-based formats (Frost et al., 2012; Muroff et al., 2010; Tolin et al., 2013), which provide a promising means of targeting HD symptoms in areas with limited access to specialized service providers. CBT for Hoarding Disorder To date, the data from empirical studies on CBT for HD are promising, with certain aspects of HD showing greater response to treatment. In two important translational studies, CBT for hoarding was tested in more naturalistic, real-world settings (Mathews et al., 2016; Moulding et al., 2016), and both of these naturalistic studies yielded significant HD symptom reductions. A recent meta-analysis revealed that CBT produced the greatest reductions in difficulty discarding (Tolin et al., 2015), which is promising given that this is the core feature of HD. However, the same meta-analysis indicated that clutter and excess acquiring displayed more muted responses to intervention. Of note, longer treatment and frequency of home visits predicted better clinical outcomes. Taken as a whole, the current treatment outcome literature on HD indicates that while overall evidence of CBT for HD is positive, rates of clinically significant change tend to be modest, such that many patients continue to exhibit clinically significant HD symptoms on termination (Tolin et al., 2015). Overview of Treatment Components Individual CBT for hoarding disorder involves an average of six hour-long sessions, depending on the client’s specific needs and range of symptoms (Muroff et al., 2014; Steketee et al., 2010). Delivered in group format, CBT for hoarding can involve between 12 and 20 sessions (Gilliam et al., 2011; Muroff et al., 2009, 2012), with protocols for use in geriatric populations having an average length of 24 sessions (Ayers et al., 2011, 2014. Manualized self-help and peer support groups are typically 15 weeks in length. For telehealth-based CBT for hoarding, which allows therapists to provide treatment via technologies such as phone or video calls rather than in person, the number of sessions is variable (Muroff et al., 2010). Cognitive behavioral treatment begins with detailed assessment of HD symptoms, as well as relevant comorbidities and any safety concerns to aid in case conceptualization and treatment planning (Muroff & Underwood, 2016). As discussed above, the assessment phase should also be used to begin mapping a particular patient’s specific experiences onto the general CBT conceptualization of hoarding, to allow for more specific treatment planning (see Figure 17.3 for a patient example). During the initial treatment modules, the clinician provides psychoeducation on HD etiology and treatment with CBT, with patients setting realistic treatment goals. Next, patients learn skills for problem-solving, organizing, and making decisions. The bulk of treatment focuses on the use of behavioral techniques and cognitive interventions to reduce saving and acquiring behaviors and beliefs and to increase sorting and organizational practices and discarding behaviors. The balance between behavioral and cognitive techniques, as well as the order in which they are introduced and used throughout treatment, may differ across clients, depending on motivational factors, the rigidity of saving beliefs, and other considerations (e.g., safety concerns may prioritize behavioral interventions). Sessions can take place exclusively within the therapist’s office, by having clients bring belongings into session; however, home visits are typically helpful and sometimes necessary. In 351 352 Stamatis, Roddy, and Timpano the event that sessions take place only in the office, it is recommended that clients do not sort any of the objects prior to coming into session, in an effort to reproduce a sorting experience as naturalistic as possible. For clients with greater difficulties with acquiring, therapists may also want to incorporate nonacquiring “shopping” exposures. These nonacquiring exposures involve trips to specific stores (e.g., bigbox stores) or events (e.g., yard sales), and involve exposure to objects without actually collecting any items. Throughout treatment, therapists help clients to foster alternative pleasurable activities (e.g., social activities) and utilize motivational interviewing techniques to enhance treatment adherence. Treatment wraps up with several relapse prevention sessions. Below, we describe the core treatment modules implemented across all CBT for hoarding treatments (Timpano et al., 2016; Tolin et al., 2015). Key Interventions Psychoeducation Following assessment and case conceptualization, treatment starts with psychoeducation about HD, as well as comorbid symptoms as relevant to the individual client. The therapist provides the client with an overview of the CBT model of HD, integrating the client’s specific symptoms of difficulty discarding, clutter, and excessive acquiring, as well as distress and impairment, into the description. Risk and vulnerability factors for HD are shared and discussed, which may yield additional information relevant to treatment while helping the client to better understand the relationships between the thoughts, emotions, and behaviors that have contributed to their hoarding symptoms. Throughout this module, it is important to address questions and elicit client feedback on extent to which the CBT model resonates with the client’s experience of hoarding symptoms, as well as ways in which these symptoms engender distress and impairment. By accruing concrete information about client symptoms, the therapist may present the intervention plan in a manner that directly addresses the client’s specific concerns. For example, when discussing the course of HD, clients will often report that they noticed a propensity to save or collect early in life, even though they may not have come in for treatment until much later, when the clutter has become unmanageable or when social or housing concerns have arisen. The therapist may use this information in describing the CBT triangle, pointing out that therapy will address the underlying cognitive factors (e.g., early beliefs about saving), while also targeting the problem behaviors (e.g., difficulty discarding) in order to reduce negative emotion and impairing clutter. Motivational Interviewing (MI) By integrating techniques from motivational interviewing (MI) during early sessions, the therapist targets common barriers to treatment (described in detail below) that are likely to arise during later sessions. As early as the diagnostic feedback and psychoeducation sessions, the therapist may adopt an ask-tell-ask-reflect style to elicit “change talk” from the client. Key strategies from MI that aid in eliciting CBT for Hoarding Disorder motivational factors for a given client include reflective listening, asking open-ended questions, and generating pros and cons to encourage behavioral change. For example, “You just really love your belongings, and at the same time, reducing clutter would allow you to have your grandchildren come over. What are some other ways life would be different if you reduced the clutter in your home?” Clients may create a decisional balance, and therapists can use change rulers to elicit additional change talk (Miller & Rollnick, 2012). The use of metaphors and examples, which can be personalized to the individual, can help to further assist clients with HD in identifying motivational factors. Jointly, these techniques are aimed at helping the patient consider their symptoms and the resulting consequences more objectively and to encourage change by having the patient selfgenerate both positive and negative facets and outcomes of their behavior and how this may or may not line up with their treatment goals. Given that motivational lapses are fairly common among clients with HD, therapists may pull from and adapt MI strategies to hoarding as needed throughout the course of therapy. Skills Training Having agreed on a treatment plan with the client and established motivations for behavioral change, the therapist and client move to the skills training modules. As previously described, individuals with HD often exhibit and report deficits in planning, organizing, and categorizing objects. Consequently, teaching clients concrete skills prior to beginning the behavioral components of treatment helps to reduce potential barriers. The ultimate goal of skills training is for clinicians to equip clients with specific skills that will be essential to successful sorting and discarding exposures during the next phase of treatment. Through the core components of skills training, the therapist will teach problem-solving steps and discuss the importance of planning prior to acting. For instance, clients learn the technique of linking important items (e.g., keys, wallet) with appliances used frequently (e.g., coffeemaker). Clients also learn to prioritize important tasks and divide projects into manageable steps, an important skill to make later discarding sessions more manageable. Given the attention difficulties that many patients experience, regardless of whether they meet criteria for ADHD or not, it is often helpful to provide skills to manage distractions. For example, clients may be assisted in setting up a calendar system to manage appointments and daily activities, using timers to guide sorting sessions, and creating staging areas to remain focused on sorting the specific items at hand. During the skills training module, the therapist also introduces the use of decision trees in dealing with objects, which involve establishing a hierarchy of decisions (e.g., save or discard?), as well as stepwise contingencies based on those decisions (e.g., If discard, what category does it belong to? Options: trash, recycling, donations) and specific instructions to handle objects within each category (e.g., If donation, place in donation bin and identify plan for removing donation bin at the end of the sorting session). Additional skills covered in this module include identifying categories that will be used in later sorting, and establishing guidelines for the 353 354 Stamatis, Roddy, and Timpano length of time items need to be saved (e.g., tax documents should be saved for seven years and can then be discarded). Behavioral Experiments and Exposures Across the various CBT protocols for HD, the majority of sessions (at least 10) are devoted to sorting and discarding exposures, as well as nonacquiring exposures for clients who endorse acquiring symptoms (Ayers et al., 2011; Muroff et al., 2014; Steketee & Frost, 2013). Although discarding and nonacquiring exposures share many features with traditional exposures for anxiety disorders, conducting exposure therapy with patients with HD also presents unique challenges. Often, discarding exposures lead to discussions of distress tolerance to the uncomfortable and challenging process of making decisions about objects. Given these challenges, structure is key to promoting productive exposure sessions, whether it is in the office, during home visits, or while the clients are practicing sorting on their own. Prior to beginning exposures, rules and guidelines discussed during the skills training modules are refreshed, including the establishment of categories for sorting and the “only handle it once” (OHIO) rule. It is critical to assist the client in creating schedules for discarding sessions at home. The therapist will provide the client with support in establishing a reminder system, which may include smartphones or an easily carried paper-and-pencil planner, and in generally maximizing the feasibility of the discarding plan. The client is encouraged to determine a final “home” for each item sorted during a session, with an emphasis on saving enough time during each exposure to ensure that all items have a proper home. Interim “staging areas” can be created for use during exposure sessions, and the sorting area should be clear and organized in order to facilitate following the OHIO rule. To provide additional structure during sorting, clients may find it helpful to hang up a copy of the sorting rules (see Table 17.1 for example), as well as a list of questions to help make decisions about objects, which are introduced during the cognitive techniques module (see below). In order to promote success in discarding, the therapist must provide the patient with significant preparation prior to beginning in-session sorting. The first component of exposures for HD involves providing the client with psychoeducation and rationale. The therapist highlights the role of avoidance in maintaining hoarding and anxiety symptoms, also teaching the client about the process of habituation. It is important to make use of graphs and figures to emphasize that habituation is not a linear process, but rather that we expect ups and downs within an overall downward trend in anxiety. When the client has exhibited an understanding of the reasoning behind exposure therapy and a willingness to engage with the intervention, the next step is to create a hierarchy. The therapist aids the client in brainstorming a variety of items and situations that increase in difficulty. It is generally useful to provide the client with sample anchors. For example, “A zero on my hierarchy might be getting rid of expired food, whereas a ten for me would be sorting through my grandfather’s belongings after he recently passed away. What would a zero look like for you? A ten?” The therapist will emphasize that exposure therapy starts with an item or CBT for Hoarding Disorder 355 Table 17.1. Example sorting: Rules for Rona Sorting papers Sorting books If dated pre-2000 ! discard If tax related, keep anything since 2014 Newspaper/magazine clippings Recipes ! save Past travel related ! discard Future travel related ! keep Notes/handwritten lists ! Ron decide Instructions/manuals ! keep Documentation of art ! keep Paid bills older than four years ! shred and discard Bank statements older than three years ! shred and discard Accounting books ! keep Nature books Picture books ! donate Natural history books ! keep Fiction books ! Ron sort If read ! donate First edition books ! keep Children’s books ! daughter decides Old (dated) textbooks ! donate Sorting objects If old (dated) and unused ! donate Any art or artifacts ! keep Related to travel ! keep in travel box Photos ! keep For other objects ! make best guess what is useful for Ron a Ron and therapist developed these sorting rules collaboratively during session. He practiced sorting with therapist and volunteer before using rules with family when they came to town. situation that is level three in difficulty, and that over time more difficult situations will be tackled. Clients will begin bringing items into session to practice discarding exposure techniques with the therapist, who then assists the client in structuring athome exposure sessions. In session, the therapist will aid the client in asking questions and referring to decision trees about objects to help make decisions about the right “home” for a given item. Clients learn to rate their Subjective Units of Distress (SUDs) every five minutes throughout an exposure session, an important self-monitoring skill to understand emotional responses to decisions about objects, and to highlight the natural reduction in distress through habituation over time. In more advanced exposure sessions, clients may begin to set time goals for making decisions about objects or set a priori goals for the proportion of objects to be discarded from a given pile. Nonacquiring exposures are typically conducted during later sessions as needed and after a separate hierarchy has been established. To promote nonacquiring, clients are encouraged to reflect on triggers of compulsive shopping or acquiring, and to establish clear acquiring rules. Depending on the client’s acquiring tendencies, the therapist will work with the client to establish plans for nonacquiring shopping exposures. Starting with a difficulty level of three on their nonacquiring hierarchy, clients will go to a specific store or event with the goal of not purchasing or picking up free items, rating their SUDs throughout. During the exposures, clients learn to rate their SUDs over time, and to ask questions about objects that will help inform their decision to acquire (see following section on cognitive 356 Stamatis, Roddy, and Timpano techniques). Moreover, the therapist will work together with the client to identify alternative sources of coping and pleasurable activities that the client can perform instead of acquiring or when urges to acquire surface. Given the role of positive emotionality in HD, it is critical to promote engagement in adaptive pleasurable activities as the client reduces their acquiring. Cognitive Techniques The first step in introducing cognitive techniques is for the therapist and client to identify cognitive errors and related core beliefs that influence current symptoms. Clients are assigned behavioral monitoring exercises between sessions, which may include a thought record specific to emotional experiences about objects (e.g., Steketee & Frost, 2013). During sessions, the therapist makes use of both general cognitive strategies and others that are specifically targeted for hoarding. General cognitive techniques include Socratic questioning and asking for evidence, using the downward arrow technique to help identify core beliefs, focusing on perfectionism as a continuum, considering advantages and disadvantages, and honing in on costs of saving items and benefits of discarding (Steketee & Frost, 2013). The hoardingspecific strategies focus more directly on questions about keeping versus discarding possessions (Ayers et al., 2011; Muroff et al., 2014; Steketee & Frost, 2013). Questions such as “How many do I already have? How many would be enough? Do I have a specific plan to use this item within a reasonable timeframe? Would I die without it?” can be crucial in assisting patients in clarifying motivating factors for discarding, as well as the next steps in a sorting exercise. In an additional cognitive strategy, the therapist role-plays the client perspective, asking the client to play the role of a third person questioning the therapist about decisions to keep or discard items. As in the motivational interviewing module, metaphors and stories serve to enhance the introduction of cognitive techniques. For example, while helping clients to grapple with the subjectivity of “needs” versus “wants,” the therapist may share a version of the following: Let’s take the example of going to the beach. Is this a “want” or a “need”? [Client(s) will say want]. Okay, it seems like a want – and maybe for me, right now, going to the beach is a want rather than a need. But let’s say I’m very depressed and overworked, and I’ve been having trouble taking pleasure in the activities I usually enjoy, such as going to the beach. In this case, would taking some time to go to the beach feel more like a want or a need for me? [Need]. The same thing applies to objects – that is, the same item could be a want for one person and a need for another person, or even a want for one person at a certain time in their life and a need for that same person at a different time in their life. A final cognitive strategy that can be extremely powerful involves behavioral experiments that test certain beliefs patients have related to objects, their ability to cope without the objects, and their assumptions about what will happen should they no longer own an object. For example, clients commonly assert the belief that they would feel immense distress if they no longer had certain possessions. As a behavioral experiment, a client may test the strength of the distress they believe they CBT for Hoarding Disorder would feel living without one specific item. To do so, the client would give this possession (e.g., a set of magazines from several years prior) to the therapist, with the agreement that if after one month the client still feels they need the object, it will be returned; otherwise, it will be discarded. The client would be instructed to rate on a 1–10 scale the extent to which they feel distressed about not having the object each week. Clients typically report minimal distress and often forget that the therapist even has the item. By testing client beliefs using the behavioral experiment framework, the therapist provides the client with concrete data to illustrate the extent to which they overestimate the future negative impact of discarding items. Relapse Prevention Toward the end of treatment, at least one session is dedicated to relapse prevention. The broad goal of relapse prevention is to increase the likelihood that clients will continue to engage in daily sorting and discarding exposures. During the relapse prevention module, the client is prompted to reflect on progress gained in therapy and to write down key skills learned. The definitions of cognitive strategies are elicited, and clients are encouraged to identify which of these strategies they have been using, and which they would like to make a stronger effort to implement moving forward. In addition, the clinician reviews concepts relating to exposure therapy, including avoidance and habituation, and the client identifies and problemsolves barriers to implementing exposures in their day-to-day life. Clients also consider warning signs and behaviors of getting “stuck” in treatment, such as missing a day of discarding. Barriers and Obstacles General Prognosis In the context of treatment for OCD and related disorders, hoarding symptoms have historically been associated with poorer responses to CBT and other interventions (Abramowitz et al., 2003; Bloch et al., 2014). Given that HD was added to the DSM-5 as an independent diagnostic entity fairly recently (Mataix-Cols et al., 2010), the literature on HD treatment remains relatively new and indicates only modest support for intervention effects (Thompson et al., 2017). Aggregating the effects of treatment trials of CBT for hoarding (Tolin et al., 2015), a meta-analysis indicated that although CBT produced reliable decreases in HD symptoms, most patients continued to endorse symptom levels in the clinically significant range after treatment. In terms of long-term effects, the maintenance of treatment gains has been reported at six-month (O’Connor et al., 2018) and 12-month (Muroff et al., 2014) follow-up assessments after group and individual CBT for hoarding, respectively. However, given the chronicity of hoarding symptoms, longer-term investigations of HD symptom course following treatment – for example, at two years posttreatment – are warranted. 357 358 Stamatis, Roddy, and Timpano Treatment Barriers While empirical evidence for HD treatment prognosis remains in its early stages, a number of barriers and obstacles have been identified in the context of delivering hoarding treatment to clients. Common factors that stand to stymie HD interventions include low motivation and insight, comorbid conditions, the involvement of family and friends, limited resources, and legal problems. Contributing to poor insight, perceptions of clutter may vary significantly across individuals, and individuals with HD often exhibit anosognosia, or a lack of awareness of the impact and severity of their symptoms (Frost et al., 2010). A key strategy in combating this obstacle, along with the rigid beliefs and defensiveness that similarly hinder treatment progress, is drawing from MI to increase awareness of the discrepancies between the client’s current concerns and their goals and values. A related consideration is whether distress tolerance skills should be infused with the general treatment approach described above, to increase motivation and encourage full engagement with the sorting exposures. There is growing research support for a specific association between greater hoarding severity and a subjective sense that one has difficulties handling distressing situations (Shaw et al., 2015; Timpano et al., 2014), which may contribute to avoidance behaviors and poor coping responses. These findings have led some newer treatment manuals to recommend directly addressing emotional processes, with a particular focus on distress tolerance, in therapy with patients with HD (Tolin et al., 2017). Another issue that arises in treatment is the influence of comorbid conditions across medical (e.g., pain, mobility issues) and psychological (e.g., social anxiety, ADHD) domains. Beyond the individual, treatment interference may relate to the misguided attempts to help by family members and friends. When loved ones become involved in treatment, it is essential that they agree to follow the guidelines developed by the therapist and client (Frost & Steketee, 1998). Conversely, limited social support and other resources, along with higher levels of distrust (Weintraub et al., 2018), can slow treatment progress. Finally, legal problems such as eviction, loss of housing benefits, and competency questions may create significant obstacles during hoarding treatment. Given the uniquely high likelihood of housing-related legal issues in HD compared with other disorders, clinicians must work closely with an interdisciplinary team (e.g., social workers, community members, and law enforcement) to provide the client with comprehensive care (Bratiotis & Woody, 2014). Case Vignette: Treatment At the start of treatment with Ron, psychoeducation about hoarding disorder and the CBT model for hoarding were discussed. Ron initially reported high motivation and capability for sorting and discarding objects. Therefore, the therapist assigned Ron the homework of sorting objects for 20 minutes per day between sessions, emphasizing the importance of following through with discarding or recycling items that were sorted into those piles as well as abiding by the OHIO rule. However, it quickly became apparent that Ron’s depression was interfering with his ability to CBT for Hoarding Disorder sort and discard independently. Ron reported difficulty getting started sorting, related to his anhedonia and low motivation. The therapist addressed these treatment-interfering behaviors in three ways. First, the therapist assisted Ron in planning specific times to sort and setting alarms as reminders. Second, the therapist introduced the idea of behavioral activation to help Ron improve his mood and reduce interfering depressive symptoms. Ron identified walking more frequently around his neighborhood as a behavioral strategy to increase his social interactions and physical activity. Third, the therapist had Ron bring a banker box into session to sort in session together as the first sorting exposure. The therapist used this in-session exposure to gather important insights about how Ron related to objects and was able to start to address these with the client. First, Ron had several saving beliefs such as difficulty with items that he considered “unique” and difficulty discarding items without knowing the item’s future home (e.g., Would someone else read and enjoy this book, or would it end up in the landfill?). Second, Ron struggled to make decisions about objects when not all objects in that category were present (e.g., he could not sort CDs unless his entire collection was present). In-session sorting was repeated several times so Ron and the therapist could consider how emotions and memories connected to the objects. Ron began to distinguish “good” reasons for saving from instances in which “HD was putting up a roadblock” that prevented him from moving forward. Throughout these sessions, the therapist approached Ron’s objects with open-minded curiosity. Finally, Ron and his therapist discussed items within a particular category that he considered meaningful; they ranked items along a gradient from very meaningful (e.g., artwork he and his wife had collected during their travels) to somewhat meaningful (e.g., a brochure from a museum he wants to visit). Toward the end of treatment, Ron had made significant progress sorting and discarding objects in his home; however, he had yet to sort items in his storage units, and his daughter was coming to town to help with this process. The therapist aided Ron in preparing for his daughter’s visit in several ways. First, Ron and his therapist created a list of sorting rules collaboratively in session that he and his daughter would use while sorting the storage units (Table 17.1). Second, in order to practice sorting, the therapist and a volunteer from the outpatient clinic spent one therapy session doing a practice sort with Ron at the storage unit with his permission. During this session, Ron practiced explaining the sorting rules to the volunteer and allowed the therapist and volunteer to sort alongside him using the sorting rules. Third, when Ron’s daughter came to town, she joined Ron for a family therapy session. Ron led the session, explaining the CBT model of hoarding to his daughter and sharing with her the progress he had made in treatment. Finally, time in session was devoted to collaboratively creating a relapse prevention plan with both Ron and his family. Conclusion Hoarding disorder, defined by difficulty discarding, excessive acquiring, and clutter, represents a difficult condition to assess and treat. Identification of individuals 359 360 Stamatis, Roddy, and Timpano suffering from HD is a critical public health issue, as HD can interfere with activities of daily living and create safety or fire hazards in extreme cases. Detailed assessment of HD symptoms is critical to successful treatment; by considering which features of HD are salient for a given client, therapists can better address individual factors such as saving beliefs that may contribute to discarding roadblocks. Often comorbid with other psychological disorders, HD can be especially challenging to treat in the presence of interfering mood and affective symptoms, as well as other issues such as information-processing impairments. However, there is evidence that HD responds well to cognitive behavioral treatment in a variety of modalities (individual, group, and community level). As demonstrated in the treatment overview and case vignette sections, the successful treatment of HD necessitates a combination of cognitive techniques, such as addressing core beliefs around saving and acquiring, as well as behavioral techniques, such as sorting exposures. Despite certain challenges, treating clients with HD is incredibly rewarding clinical work. As clients gain mastery of the techniques and see tangible evidence of their improvement by decreasing cutter and acquisition, they are often incredibly grateful for the help and guidance of therapists and community partners. Summary of Key Points Hoarding symptoms are influenced by positive and negative reinforcement systems, both of which constitute important treatment targets. Although hoarding disorder remains a challenging condition to treat, cognitive behavioral therapy may help reduce clutter, acquiring, and difficulty discarding symptoms. Cognitive behavioral therapy for hoarding disorder involves symptom assessment, psychoeducation, skills training, discarding exposures, and cognitive restructuring. When treating patients with hoarding disorder and their family members, therapists will often collaborate with social workers and individuals in the broader community. Patience and flexibility are essential when working with patients who have hoarding disorder. REFERENCES Abramowitz, J. S., Franklin, M. E., Schwartz, S. A., & Furr, J. M. (2003). Symptom presentation and outcome of cognitive-behavioral therapy for obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology, 71(6), 1049. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. American Psychological Association. (2014). Guidelines for psychological practice with older adults. The American Psychologist, 69(1), 34. Ayers, C. R., Saxena, S., Espejo, E., Twamley, E. W., Granholm, E., & Wetherell, J. L. (2014). Novel treatment for geriatric hoarding disorder: An open trial of cognitive CBT for Hoarding Disorder rehabilitation paired with behavior therapy. The American Journal of Geriatric Psychiatry, 22(3), 248–252. Ayers, C. R., Wetherell, J. L., Golshan, S., & Saxena, S. (2011). Cognitive-behavioral therapy for geriatric compulsive hoarding. Behaviour Research and Therapy, 49(10), 689–694. Bloch, M. H., Bartley, C. A., Zipperer, L., Jakubovski, E., Landeros-Weisenberger, A., Pittenger, C., & Leckman, J. F. (2014). Meta-analysis: Hoarding symptoms associated with poor treatment outcome in obsessive-compulsive disorder. Molecular Psychiatry, 19(9), 1025. Brakoulias, V., Eslick, G. D., & Starcevic, V. (2015). A meta-analysis of the response of pathological hoarding to pharmacotherapy. Psychiatry Research, 229(1–2), 272–276. Bratiotis, C. (2013). Community hoarding task forces: A comparative case study of five task forces in the United States. Health & Social Care in the Community, 21(3), 245–253. Bratiotis, C., Sorrentino Schmalisch, C., & Steketee, G. (2011). The hoarding handbook: A Guide for human service professionals. Oxford University Press. Bratiotis, C., & Woody, S. (2014). Community interventions. In R. O. Frost & G. Steketee (Eds.), The Oxford handbook of hoarding and acquiring (p. 316). Oxford University Press. Chasson, G. S., Carpenter, A., Ewing, J., Gibby, B., & Lee, N. (2014). Empowering families to help a loved one with hoarding disorder: Pilot study of family-as-motivators training. Behaviour Research and Therapy, 63, 9–16. Cromer, K. R., Schmidt, N. B., & Murphy, D. L. (2007). Do traumatic events influence the clinical expression of compulsive hoarding? Behaviour Research and Therapy, 45(11), 2581–2592. First, M. B., & Williams, J. B. (2016). SCID-5-CV: Structured clinical interview for DSM-5 disorders: Clinician version: American Psychiatric Association Publishing. Frost, R., Kim, H.-J., Morris, C., Bloss, C., Murray-Close, M., & Steketee, G. (1998). Hoarding, compulsive buying and reasons for saving. Behaviour Research and Therapy, 36(7–8), 657–664. Frost, R., Rosenfield, E., Steketee, G., & Tolin, D. (2013). An examination of excessive acquisition in hoarding disorder. Journal of Obsessive-Compulsive and Related Disorders, 2(3), 338–345. Frost, R., Ruby, D., & Shuer, L. (2012). The buried in treasures workshop: Waitlist control trial of facilitated support groups for hoarding. Behaviour Research and Therapy, 50(11), 661–667. Frost, R., & Steketee, G. (1998). Hoarding: Clinical aspects and treatment strategies. In M. Jenike, L. Baer, & W. E. Minichiello (Eds.), Obsessive compulsive disorders: Practical management (3rd ed., pp. 533–554). Mosby. Frost, R., Steketee, G., & Williams, L. (2000). Hoarding: A community health problem. Health & Social Care in the Community, 8(4), 229–234. (2002). Compulsive buying, compulsive hoarding, and obsessive-compulsive disorder. Behavior Therapy, 33(2), 201–214. Fr