lOMoARcPSD|11871570
WK5- Haemostasis
Haematology and Transfusion Science (Ulster University)
Studocu is not sponsored or endorsed by any college or university
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
WK 5 Haemostasis
INTRODUCTION
This aim of this week is to introduce the various components of haemostasis and explain how they interact to
maintain two contradictory needs :
the need to minimize blood loss following injury and
the need to keep the blood fluid and circulating around the body.
There is a delicate balance between these two requirements and
this lecture will explore each component in isolation but also demonstrate the sequencing and coordination
between the various components found in a normal haemostatic system.
Understanding the information in this lecture is essential for appreciating the content of Lecture 6, when we
discuss disorders of haemostasis.
CONTENTS
•
HAEMOSTASIS
•
PLATELETS
•
THE COAGULATION CASCADE
•
FIBRINOLYSIS
•
LABORATORY TESTS OF HAEMOSTASIS
•
CONCLUSION
•
RECOMMENDED READING
LEARNING OUTCOMES
At the end of this week's lecture you should be able to:
•
Name the five major components of haemostasis
•
Understand the role of platelets in haemostasis
•
Summarise the coagulation cascade and the interaction of its factors
•
Recognize the importance of fibrinolysis
•
Understand how the various components of haemostasis interact in the haemostatic response
•
Explain how various laboratory tests are used to investigate coagulation.
HAEMOSTASIS
•
Haemo = ‘blood’
Stasis = ‘stop’ (Greek)
•
Haemostasis is one of the most important survival mechanisms in higher animals and is the ability to
minimize blood loss following injury by coagulation of blood.
•
However, such a response needs to be tightly controlled to ensure that coagulation does not occur all the
time, thereby affecting the normal function of blood.
•
Therefore, the haemostatic system represents a delicate balance between pro-coagulant and anti-coagulant
mechanisms, involving complex feed-back and feed-forward pathways that integrate together the major
components.
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
Haemostasis involves 5 main components
•
blood vessels
•
platelets
•
coagulation factors
•
coagulation inhibitors
•
fibrinolysis.
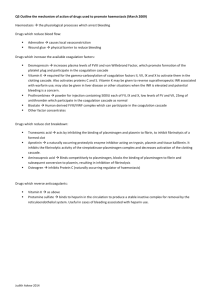
Coagulation Cascade
The interaction between blood vessel activity (vasoconstriction), platelet activity and coagulation cascade (containing
both coagulation factors and inhibitors) in response to vessel injury. The stable haemostatic plug is then broken down
by fibrinolysis (not shown above).
VIDEOLINKS: OVERVIEW OF HAEMOSTASIS
Two short animated clips, introducing the overall concept of haemostasis. It may help to watch these before
progressing to read the notes below.
At the end of the lecture two other, more detailed videoclips are provided covering the same processes.
Clip 1. http://www.youtube.com/watch?v=xNZEERMSeyM
Clip 2. (A little more fun!) http://www.youtube.com/watch?v=9QVTHDM90io&feature=related
VASOCONSTRICTION.
The basic structure of blood vessels comprises 3 distinct layers:
Tunica intima: This is the innermost layer which lies in direct contact with the flow of blood. It is composed
mainly of endothelial cells. The hollow internal cavity in which the blood flows is called the lumen.
Tunica media: This is the central layer which is made up of smooth muscle and elastic tissue. This is the most
variable layer as its composition varies with blood vessel type. In the aorta it is composed of mainly elastic
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
fibres to facilitate pressure changes, whereas in muscular arteries it consists of mainly smooth muscle cells
aiding rhythmic contraction.
Tunica externa/adventitia: This is the outermost layer which is composed of connective tissue.
Following injury, there is immediate vasoconstriction of the injured vessel which acts to slow down flow of
blood to the area and to increase activation of platelets and coagulation factors.
The endothelial cells play a crucial role in this mechanism as they release a number of substances that
subsequently play a role in the coagulation process.
Under normal circumstances, they produce prostacyclin and nitric oxide, which cause vasodilation and
inhibit platelet activity, thereby preventing coagulation.
After injury, however, they release endothelin (ET-1), which acts as a powerful vasoconstrictor and activator
of platelets, thereby promoting coagulation.
In addition, they release, and have receptors for, a number of molecules
The endothelial cells of the tunica intima release several substances into the lumen of the blood vessel which
subsequently play a role in the coagulation process.
PLATELETS
Platelets are involved in the cellular mechanism of primary haemostasis that leads to the formation of blood
clots.
Platelets are formed in the bone marrow from by the fragmentation of megakaryocyte cytoplasm.
The megakaryocyte matures by endomitotic synchronous nuclear replication, which enlarges the cytoplasmic
volume as the number of nuclear lobes increases in multiples of two.
Eventually the cytoplasm becomes granular and the platelets are released. Each megakaryocyte produces
approximately 4000 platelets
VIDEO LINK: NORMAL PLATELET PRODUCTION FROM MEGAKARYOCYTE
https://www.youtube.com/watch?v=PfFcr7ytN58
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
PLATELET CHARACTERISTICS
Platelets are disc shaped and measure approximately 2-4 µm in diameter.
Platelet production is stimulated by thrombopoietin (TPO), which is produced at a constant rate in the liver.
Megakaryocytes and platelets express the receptor c-Mpl for TPO and the relative saturation of this receptor
is the means by which platelet production is controlled.
If platelet levels are low, the free levels of TPO in the blood will rise, bind to c-Mpl on megakaryocytes and
stimulate their maturation.
A platelet has a lifespan of 9-10 days and normal numbers are in the range
150 - 400 x 109 /L.
Under normal circumstances, they circulate in a quiescent state, but will undergo a rapid activation following
damage to a vessel wall.
The ability to rapidly activate is due to their complex structure, which helps mediate the coagulation process.
PLATELET STRUCTURE
The ultrastructure of a platelet. The glycocalyx coat is made up of a wide variety of membrane-bound glycoproteins
and receptors which mediate the actions of the platelet.
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
PLATELET STORAGE GRANULES
Dense granule. These contain high levels of ATP, ADP, serotonin and calcium ions.
a-granule. These contain a rich mix of proteins which aid the response to tissue injury, promoting efficient
haemostasis, repair, inflammation and immune response. These
include:
o
Angiogenic factors (e.g. VEGF)
o
Coagulation Factors (e.g. Factor V)
o
Fibrinolytic Factors (e.g. Plasminogen, antiplasmin)
o
Growth Factors (e.g. PDGF, EGF)
o
Aggregation factors (Fibrinogen, von Willebrand Factor)
o
Chemokines (for WBC recruitment)
Lysosomes. These contain hydrolytic enzymes
PLATELET FUNCTION
The main function of platelets is the formation of a haemostatic
plug in response to vascular injury. However, they also play a
critical role in several other processes
PLATELET ADHESION
The initial event that occurs after the vessel wall becomes
damaged is the adhesion of platelets to the subendothelium
This occurs through the interaction of GP1b complex with von Willebrand Factor (vWF).
vWF is a large glycoprotein synthesised primarily by endothelial cells and is able to bind GP1b complex as a
consequence of binding collagen and/or elevated shear forces.
Once this initial binding occurs, a process of platelet ‘rolling’ occurs as the blood flow forces the platelet to
roll over whilst still anchored by the initial binding point.
Platelet adhesion. The initial interaction occurs between the GPIb complex (consisting of 4 proteins; GPIba,
GPIbb, GPIX, GPV) and von Willebrand Factor (vWF). Thereafter, GPIIb/GPIIIa binds vWF as well, whilst GPIa
and GPIIb (not shown) bind collagen.
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
Rolling brings other parts of the platelet into contact with the endothelium and further interactions occur,
stabilising the binding of the platelet and protecting it against the shear forces of the blood flow.
The GPIIb/GPIIIa complex (also known as aIIb/b3 integrin) interacts with vWF as well, whilst the GPIa /GPIIb
complex (also known as a2/b1 integrin) makes associations with collagen.
These main interactions are supported by several other integrins and adhesion complexes
The result that the platelets become captured and stably adhered to the subendothelium at the site of the
injury.
Platelets will also exhibit a change in morphology from a disc-shape to a rounded appearance to a ‘spiky’ cell
with finger-like projections known as filopodia
This is brought about by a rearrangement of the actin cytoskeleton and increases the number of locations
where further binding can occur, thereby promoting further adhesion and aggregation.
Adhesion also leads to the activation of intracellular signalling, which stimulates the platelet granules to
release their contents
PLATELET AGGREGATION
Following adhesion, the platelets change in shape promotes cross-linking between platelets leading to
aggregation.
GPIIb/IIIa normally exists in a low-affinity form, but in activated platelets, it switches to a form with high
affinity for ligands such as fibrinogen, vWF and fibronectin, thereby promoting adhesion and aggregation
between platelets.
This process is also mediated by the release of the contents of the granules into the environment,
particularly ADP which plays a positive feedback role in promoting activation.
THROMBOXANE A2
The production of thromboxane A2 (TxA2) is also critical.
It is synthesised in the platelet and acts by inhibiting the action of the enzyme adenylate cyclase (cAMP),
which results in increased Ca2+ levels, which promotes aggregation.
Under normal circumstances, cAMP levels are controlled by the production of prostacyclin from endothelial
cells which promotes the action of cAMP and lowers Ca 2+ levels, ensuring platelet activation and aggregation
does not occur when there is no injury.
The opposing roles of prostacylcin and thromboxane in mediating cAMP activity and levels of Ca 2+ ions.
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
VIDEOLINK : PLATELET ADHESION & ACTIVATION
http://www.youtube.com/watch?v=0pnpoEy0eYE
PLATELET STABILIZATION
The end result is the production of a platelet aggregate which acts to plug the site of injury.
However, this plug is unstable and requires promotion of the coagulation pathway to ensure that a stabilized clot
occurs, by generating fibrin molecules, which integrate with the primary platelet plug.
Platelets contribute to this by :
o
Releasing components of the coagulation cascade from the granules
o
Remodelling actin cytoskeleton to retract platelets together
o
Providing a negatively charged phospholipid surface upon which the tenase and prothrombinase complexes
of the coagulation pathway can assemble
THE COAGULATION CASCADE
The blood coagulation system is composed of a series of specific plasma proteins (coagulation factors)
that are activated in a particular sequence.
Each step is characterized by the conversion of an inactive proenzyme into an enzyme which results in
the active site of the enzyme being revealed.
The coagulation factors are referred to by their order of discovery and are named using Roman numerals
from I to XIII.
However, only 12 exist, as Factor VI was mistakenly identified as a separate factor, only to be later
identified as active form of Factor V
COAGULATION FACTORS OF THE
COAGULATION CASCADE
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
Several of the coagulation factors listed on
previous slide exist as zymogens (inactive
proenzymes) which are activated when
cleaved by a specific enzyme.
They are mostly serine proteases, which
become activated when a short peptide is
removed from the proenzyme form,
exposing a serine site which can then act in
an enzymatic fashion itself
Serine protease activity, exemplified by the
action of Factor IXa upon Factor X, activating the serine site by cleavage of part of the protein. The activated
forms are denoted by a small ‘a’ (FXa)
CHANGES IN COAGULATION CASCADE UNDERSTANDING
Traditionally, the coagulation cascade was divided into an extrinsic pathway and an intrinsic pathway, which
both converged into the common pathway.
These terms are still widely used and the traditional breakdown of the pathway is still referred to.
However, research over the past decade has shown it that it is the exposure of blood to Tissue Factor (Factor
III) that is the key initiating event in coagulation.
Hence, the extrinsic pathway is now more correctly known as the Tissue Factor pathway.
Likewise, the intrinsic pathway is more accurately called the Contact Activation pathway and is now known
to only play a minor role in contributing to coagulation.
However, knowledge of the contact activation pathway is important in understanding laboratory testing of
coagulation as we will see.
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
TISSUE FACTOR INITIATES THE COAGULATION CASCADE
Tissue Factor (TF) is a glycoprotein expressed on the surface of cells and does not normally come into direct
contact with circulating blood.
Following an injury, however, the TF-expressing cells are exposed to the blood and the cascade proceeds as
follows
(Refer to Figure of cascade in understanding this sequence of events)
TF binds to coagulation factor VII leading to the production of the active protease factor VIIa
The Factor VIIa/TF complex then activates both Factor X and Factor IX
Factor Xa initiates the conversion of prothrombin (Factor II) to thrombin, although without its co-factor
Factor Va, only small amounts of thrombin are produced.
However, even these small amounts of thrombin can then feedback and activate Factor V, Factor VIII and
Factor XI by proteolysis.
Once these factors are activated, this triggers a major amplification of the cascade
The thrombin-activated factors accelerate the further activation of Factor X and prothrombin respectively by
forming the tenase (VIIIa/IXa) and prothrombinase (Xa/Va) complexes.
Both the tenase and prothrombinase complexes assemble on the activated platelets, meaning the responses
localised to the area of injury.
The net effect is an explosive production of thrombin in the area of the injury which can then convert
fibrinogen to fibrin for use in stabilising the primary platelet plug.
CONTROL OF COAGULATION
It is clear that if allowed to continue unchecked, the coagulation cascade would result in the formation of
large blood clots.
Therefore, it must be controlled and this is carried out by a number of inhibitory molecules.
The table on the next slide lists several other proteins that play integral roles in the control of coagulation
These include serine protease inhibitors (serpins) that inhibit the coagulation cascade.
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
INHIBITION OF THE COAGULATION CASCADE
1. Tissue Factor Pathway Inhibitor (TFPI) quickly inhibits the initiation step, by forming a quaternary complex
with TF-FVIIa-FXa. TFPI is predominantly associated with endothelial cells.
2. The amplification of the cascade is inhibited by the action of antithrombin (AT) which interacts with
thrombin, FIX, FX and FXI to inactivate them. AT is synthesised by the liver and is present at high
concentration sin the blood
3. Thrombin also activates an anti-coagulant pathway by binding to an endothelial cell receptor called
thrombomodulin (TM), which prevents thrombin activating its procoagulant substrates.
4. Binding of thrombin to TM results in increased activation of Protein C, a process promoted by another
receptor called endothelial cell protein C receptor (EPCR).
5. Activated Protein C, along with its co factor Protein S, acts as a negative feedback loop, inactivating FVa and
FVIIIa
Binding of thrombin to thrombomodulin results
in activation of Protein C and inhibition of FVIIIa
and FVa. It also impacts upon fibrinolysis
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
FIBRINOLYSIS
The complex mechanism of
coagulation is counterbalanced by
a mechanism for the destruction of
clots.
Fibrinolysis is the process whereby
fibrin is degraded by the proteolytic
enzyme plasmin.
Plasmin is found in the plasma in its
inactive form plasminogen and can
be converted to plasmin by a
number of different factors
PLASMINOGEN
Plasminogen (PLG) is a zymogenic serine protease synthesized in the liver. It can be activated by several proteins.
The most important of these is tissue plasminogen activator (tPA), which is synthesized and released by the
vascular endothelium and has a short half-life of around 2 mins in plasma.
Upon binding fibrin, its affinity for PLG is markedly increased and converts it to plasmin.
A similar protein called urinary plasminogen activator (uPA) acts in a similar manner.
Exogenous plasminogen activators also exist, derived from non-human sources.
Streptokinase is derived from bacteria and has been used as an anti-thrombotic therapy for years.
However, nowadays, tPA has also been produced by recombinant DNA technology.
These r-tPAs (alteplase, reteplase) have been FDA-approved for treatment of thrombotic conditions such as
myocardial infarction and stroke.
PLASMIN DEGRADES FIBRIN(OGEN)
Once plasmin is produced, it then digests fibrin (or fibrinogen) into fibrin degradation products (FDPs)
FDPs such as Fragments D &E are not normally present in the serum.
Therefore, if there is a suspicion of
thrombosis in a patient (e.g. deep
venous thrombosis (DVT) or
pulmonary embolism (PE)), serum
testing for levels of Fragments D or E
may help in diagnosis.
Plasmin also degrades factors V and
VII.
Digestion of fibrin by plasmin results
in the production of fragments
named X and Y oligomers, which are
further digested to produce D-dimers
and E fragments. D-dimers are of
particular value in diagnostic testing.
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
INHIBITORS OF FIBRINOLYSIS
The fibrinolytic pathway contains a number of inhibitors to tightly control this system.
1. Plasminogen activator inhibitors
tPA and uPA are rapidly inactivated by plasminogen activator inhibitor Type I (PAI-1), which is secreted by endothelial
cells and also found in platelet a-granules.
PAI Type 2 (PAI-2) is mainly produced by the placenta and is important for inhibiting fibrinolysis during pregnancy by
its action upon tPA. However PAI can be itself inhibited by the action of activated Protein C
2. a2-antiplasmin
This serpin inactivates plasmin. It is synthesised by the liver and has a half-life of about 60 hours in the liver.
SUMMARY
Following injury to a blood vessel, a number of events occur. Although these are listed below, be aware that these
mechanisms occur rapidly and overlap, rather than occurring sequentially.
Vasoconstriction
•
Immediate contraction of injured vessel
•
Reflex in surrounding small arteries
•
Reduced blood flow
Platelet Activation
•
Contact activation of platelets
•
Platelet aggregation
•
Primary haemostatic plug
Tissue factor activation of Factor VII
•
Coagulation cascade
•
Produces fibrin to stabilise haemostatic plug
•
Tightly regulated process, under feedback control
•
Plasmin produced to degrade fibrin clot
•
Plug digested as wound heals
•
Tightly regulated process, under feedback control
Fibrinolysis
•
VIDEOLINKS : OVERVIEW OF HAEMOSTASIS
•
Two more comprehensive videoclips to help you understand these processes.
•
Part 1 http://www.youtube.com/watch?v=RP1eLdkdJKg&feature=mfu_in_order&list=UL
•
Part 2 http://www.youtube.com/watch?v=oj9E33BZMsI&feature=mfu_in_order&list=UL
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
LABORATORY TESTS OF HAEMOSTASIS
A number of screening tests provide us with the means to assess platelet function, coagulation efficiency and
fibrinolytic activity.
Some commonly used tests in the clinic are listed on next slide and are discussed below.
In next week’s lecture we will refer to these and others in the investigation of haemostatic disorders.
Note that although these tests can be performed manually, improving technology and availability of
commercial kits means that these tests are being increasingly automated.
However, the interpretation of results still requires understanding of the principles involved.
PRACTICAL HAEMOSTASIS
http://www.practical-haemostasis.com/
Although current understanding of the coagulation cascade means the contact activation pathway is not
considered as important in initiating coagulation, the traditional concept of the coagulation cascade as
shown on next slide is useful in demonstrating how different tests can assess deficiencies in different parts of
the coagulation process.
However, please remember that the cell-based model of coagulation presented earlier in the lecture
provides a truer reflection of what is occurring during coagulation.
The traditional
concept of the
coagulation
cascade, showing
the contact
activation
pathway
(intrinsic) in red,
the tissue factor
pathway (extrinsic
) in blue and the
common pathway
in green.
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
PROTHROMBIN TIME (PT)
This measures the factors involved in the extrinsic and common pathways (FVII, FX, FV, prothrombin and
fibrinogen).
It is based on the principle that plasma (obtained from blood to which a calcium-binding anticoagulant
(citrate) has been added), will clot in a few seconds when re-calcified in the presence of tissue factor.
The elapsed time between the addition of calcium-tissue factor mixture and the presence of a detectable clot
is the prothrombin time.
In practice, this usually involves adding thromboplastin, which contains Tissue Factor and calcium, to the
plasma sample.
Normal time for clotting is 10-16 seconds, meaning the effect of the intrinsic pathway (via activation of FIX) is
negligible.
Principle: Plasma, obtained from
blood to which a calcium-binding
anticoagulant (citrate) has been
added, will clot in a few seconds
when re-calcified in the presence of
tissue factor. The elapsed time
between the addition of calciumtissue factor mixture and the
presence of a detectable clot is the
prothrombin time.
PROTHROMBIN TIME IN PRACTICE
Different types of thromboplastin are available from different manufacturers and different labs use different
sources.
Whilst they will all work in a similar fashion, this may give rise to variation in analytical performance.
For this reason, PT results can be presented as an international normalized ratio (INR), which attempts to
achieve an acceptable degree of inter-laboratory standardisation.
This means calibrating the thromboplastin used against an International Reference Preparation to generate
an International Sensitivity Index (ISI) value.
Although manufacturers provide ISI values on their commercial thromboplastin, it is good practice for
hospital laboratories to calibrate the thromboplastin using their own equipment to generate a local ISI value
to account for lab-specific variables.
This will include the use of a local geometric mean normal prothrombin time (GMNPT) value, which is
generated by averaging the PTs of several plasma samples using a given batch of thromboplastin and local
instrumentation.
Once all these figures are generated, the INR can be calculated thus:
INR = {Patient PT (s) / GMNPT (s)} ISI
The normal range for the INR is 0.8–1.2.
PT testing is most often used in monitoring warfarin therapy, Vitamin K deficiency and other bleeding
disorders. These will be discussed in detail in Lecture 6.
ACTIVATED PARTIAL THROMBOPLASTIN TIME (aPTT)
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
aPTT measures factors involved in the intrinsic and common pathways.
Patient plasma is incubated for a set time (2-5 mins) with a contact activator to activate FXII.
Usually the activator is silica or kaolin.
Although this is not a significant reaction in vivo, this is used in the design of the aPTT because it initiates the
cascade independent of thrombin and FVII and will activate FXI.
The thromboplastin used is ‘partial’ because it does not include Tissue Factor, meaning no activation of the
tissue factor (extrinsic) pathway.
After incubation, calcium is added and the time taken for a clot to form recorded.
The normal time for clotting is 30-40 seconds.
Like with PT testing, however, hospitals will often calculate an aPTT ratio value, in which the patient value is
normalised against a aPTT value generated from a panel of control plasma samples at a local level.
aPTT testing is often used in monitoring of heparin treatment. This will be discussed further in Lecture 6.
Principle:
•
9 parts of whole blood are drawn into 1 part of citrate anticoagulant and plasma is harvested.
•
Citrated plasma is incubated with aPTT reagent (phospholipid + contact activator reagent) at 37 oC.
•
aPTT reagent contains phospholipids which substitute for 3 and micronized silica which acts as a surface for
contact activation.
•
Calcium chloride is added and the clotting time is measured.
•
aPTT tests for all the factor in the intrinsic system (Factors I, II, V, VIII, IX, X, XI, and XII). It does not measure
the activity of factor VII.
THROMBIN TIME (TT)
This is a simple test, whereby thrombin is added to patient plasma to directly convert fibrinogen to fibrin.
Normal clotting time is 14-16 seconds.
FIBRINOGEN TEST
The Clauss fibrinogen assay involves diluting plasma to be tested (to minimise effect of interfering
substances), mixing it with a strong concentration of thrombin and measuring how long it takes to clot.
This time is read of a standard curve to get the fibrinogen concentration in the plasma.
Alternatively, ELISAs can be used to measure total amount of fibrinogen antigen present, irrespective of
function.
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
It is also possible for automated analysers to be used to assess fibrinogen levels based on photo-optical
detection of clot during the PT test.
The reference range for fibrinogen is generally between 1.5-4.0g/L
ONE STAGE FACTOR ASSAYS
Based on the results from other screening tests, as well as family history, an assay can be performed to
assess deficiency of individual factors.
A one-stage test involves making serial dilutions of plasma to be tested.
One volume of each dilution is mixed with an equal volume of plasma which is known to be deficient in a
particular factor (e.g. FVIII)
The aPTT test is then performed.
Principle of a one-stage Factor assay.
Plasma to be tested is diluted and mixed 1:1 with
plasma which is known to be deficient in a particular
factor (in this example FVIII). The aPTT test is
performed and clotting times plotted on a graph
In the example on the previous slide, the only source
of FVIII can come from the patient plasma.
The clotting times of each dilution is plotted and
compared with a control plot.
Two parallel lines should be the result.
If the patient line is to the right of the control, it
indicates longer clotting time and a deficiency in the level of the factor being measured (see graph on next
slide)
These tests can be carried out manually or on automated analysers, but in both cases, scrutiny of the plots is
crucial, especially since inhibitors, dilution range and very low levels of factor can affect assay validity and
may result in graphs where the lines are not parallel.
Results from a one-stage Factor assay demonstrate that the
test plasma (red line) has longer clotting times than control
plasma (blue line) shifting it to the right. Therefore, this test
plasma has a deficiency in the factor being tested for (in this
example FVIII).
PLATELET TESTING
Platelet testing will normally involve a straightforward count and examination of morphology.
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
This can be done manually, but is more commonly carried out by automated analysers.
Blood films will also allow microscopic examination of the platelets in a blood sample. In addition, the
following tests can be performed
Bleeding Time
A simple test, in which a small incision is made on the forearm and time taken to stop bleeding recorded. It is
not easy to standardise this test, so increasingly automated analysis is preferred. Various instruments are
now available which screen for defects in the primary haemostatic response (ie platelet function).
PLATELET AGGREGATION
Automated aggregometers are now available which use photo-optical measurement to assess extent of
platelet aggregation after a stimulating factor is added (e.g. ADP).
Platelet rich plasma (PRP) is prepared by gentle centrifugation to remove RBCs and WBCs, after which an
agonist is added to the PRP in a cuvette.
As the platelets aggregate, more light is allowed to pass through the cuvette and this can be recorded
graphically
Normal platelet aggregation plot, showing response
of PRP to the addition of ADP. The stages of
activation as discussed earlier in lecture are marked.
PLATELET FUNCTION ANALYSER (PFA-100)
The PFA-100 is a widely used commercially available test for platelet function.
In it, blood to be tested is sucked up through a fine capillary needle and directed onto a collagen membrane
which is coated in ADP or epinephrine.
The collagen mimics exposure to endothelial matrix, whilst the coating mimics localized activation.
The time taken for the platelets to adhere, aggregate and occlude the pores in the membrane is recorded.
VIDEO CLIP : http://www.platelet-research.org/3/pfa.htm
FIBRINOLYSIS TESTING
D-dimer Testing
As we have seen, degradation of fibrin results in production of fibrin degradation products (FDPs), including
D-dimer molecules.
D-dimer testing in the laboratory is based on immunological principle (e.g. ELISA) in which an antibody to a
D-dimer epitope can detect the amount present.
Since D-dimer is not normally present in plasma, any detection would suggest the presence of a clot, which
may be caused by a thrombotic disorder.
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
However, there is often false positive (and false negative) results with D-dimer testing, so it is commonly used
in conjunction with scanning techniques such as ultrasound to accurately diagnose a condition.
CASE STUDY: TEST YOURSELF
(From: Haematology. Moore, Knight, Blann (Eds), Oxford University Press, 2010)
A 5-year-old boy presents with a large intramuscular haematoma, having no previous history of bleeding from minor
cuts and abrasions. His screening test values are as follows:
Which of these is abnormal, what is the probable diagnosis and what further investigations would you perform to
test the diagnosis?
TEST
RESULT
NORMAL RANGE
PT (s)
11.9
10.0 - 14.0
aPTT (s)
102.3
32.0 - 42.0
TT (s)
9.3
9.0 - 11.0
Fibrinogen (g/L)
3.8
1.5 - 4.0
Platelet count (x 109/L)
250
150 - 400
Answer to Case Study
The isolated elevated aPTT result indicates an intrinsic pathway defect.
The lack of bleeding from minor trauma with a normal platelet count makes a primary haemostatic disorder unlikely.
The severity of the haematoma together with the results above and the patient’s gender suggest a haemophilia
Further investigation would begin with assays for FVIII and FIX, the most common forms.
For further explanation of this diagnosis, we will examine haemophilia in Lecture 6
CONCLUSION
In this lecture we have discussed the process of haemostasis and observed how it is a tightly regulated process which
controls both normal blood flow and coagulation in response to vessel injury.
We have also looked at various laboratory tests which are used to test for coagulation efficiency.
The understanding of haemostasis and these tests will be important as we move to next week’s lecture, in which we
discuss disorders of haemostasis and how they are investigated in the diagnostic laboratory.
RECOMMENDED READING
Hoffman M.
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)
lOMoARcPSD|11871570
A cell-based model of coagulation and the role of factor VIIa.
Blood Rev. 2003 Sep;17 Suppl 1:S1-5.
Brass L.
Understanding and evaluating platelet function.
Hematology Am Soc Hematol Educ Program. 2010;2010:387-96
Mosesson MW.
Fibrinogen and fibrin structure and functions.
J Thromb Haemost. 2005 Aug;3(8):1894-904
Favaloro EJ, Lippi G.
Coagulation update: what's new in hemostasis testing?
Thromb Res. 2011 Jan;127 Suppl 2:S13-6. Review.
Guy’s and St Thomas’ Centre for Haemostasis and Thrombosis
http://www.guysandstthomas.nhs.uk/our-services/haemostasis-thrombosis/overview.aspx
Lab Tests Online
http://www.labtestsonline.org/understanding/analytes/coagulation_factors/test.html
Pathology Outlines : Coagulation Chapter
http://www.pathologyoutlines.com/coagulation.html
Practical Haemostasis
http://www.practical-haemostasis.com/
Downloaded by Pete Ridden (peter.j.ridden@gmail.com)