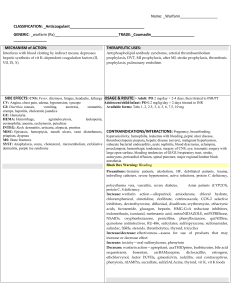
Chp. 9 Drugs for Coagulation Disorders Anticoagulants • Used in thrombotic disorders Antiplatelets Thrombolytics • Used to prevent arterial thrombosis • Dissolve thrombi and limit tissue damage in thromboembolic disorders Title Ipsum dolor sit • Lorem ipsum dolor sit amet, consectetuer adipiscing elit. • Nunc viverra imperdiet enim. Fusce est. Vivamus a tellus. • Pellentesque habitant morbi tristique senectus et netus et malesuada fames ac turpis egestas. Proin pharetra nonummy pede. Mauris et orci. Rudins: Bival, Desi Vitamin K antagonist Edoxaban Adenosine Diphosphate Receptor Antagonists Phosphodiesterase-3 Enzyme InhibitorCilostazol Alteplase Indirect Thrombin Inhibitor Anticoagulant • Action: • Heparin combines with antithrombin III: inactivate clotting factors IX, X, XI, and XII; • inhibit conversion: prothrombin to thrombin; and prevent thrombus formation • Inactivates thrombin; inhibits factor XIII; V, VIII & platelet aggregation • Use: Prophylactic: prevent clot formation; therapeutically: thromboembolic disorders-prevent further clot formation Adverse Effects Contra • GI ulcerations: PUD, UC • Intracranial bleeding, aneurysm, blood disorders • Severe renal/liver disorders • Severe HTN, PV • Recent eye, spinal cord, brain surgery • Caution use: HTN, renal, hepatic, alcoholism, GI disorders, drainage tubes, threatened AB, occupationshigh trauma risk Interactions • Other antithrombotic drugs will increase effect: Box 9.2 • Decrease anticoagulant drug effect • Digoxin, NTG IV, tetracycline, antihistamines HERBALS: G’s: garlic, ginger, ginkgo, ginseng Chamomile, High-dose Vit. E Laboratory to Monitor • Maintain 1.5-2.5 times control or baseline • Normal baseline value: 25-35 seconds • Therapeutic 45-70 seconds • >100 seconds • STOP • Assess • Notify • HOLD x1 h or as per protocol • Repeat PTT/INR/PT Nursing • Baseline vs, CBC: PLTs, Hematocrit levels • Use infusion pump for continuous infusion • Monitor rate of infusion • Monitor aPTT every 4-6 hours • SQ route: 20-22 gauge needle to withdraw med from vial, change needle to smaller gauge 25-26 gauge, ½ to 5/8 inches long • Give deep SQ in abdomen, distance of 2 inches from umbilicus. • DO NOT ASPIRATE, MASSAGE, RUB Administering Injectable Anticoagulant Therapy: Nursing Administration • Avoid giving any IMs or IV injections • Hold pressure over an IM or IV site for at least 5 minutes • Route: SQ; site: abdomen • Rotate site • 2 inches from belt line (umbilicus)& above iliac crest • Do NOT aspirate, massage or rub site after administration • Have antidote on hand: ________________ 11 Nursing: Heparin • Rotate injection site • Teach patient signs of bleeding: • bruising, bleeding gums, abdominal pain, nose bleeds, coffee-ground vomitus, black tarry stools, hematuria (discolored, tea or cola color urine) • AVOID use of OTC NSAIDS, ASA, or meds with salicylates • USE ELECTRIC SHAVER, SOFT BRISTLE TOOTHBRUSH 12 Nursing Hemorrhage/bleeding • Monitor vs • Instruct to observe for bleeding, increased HR, decreased BP, bruising, petechiae, hematomas, black tarry stools • OD: STOP, notify, administer antidote • Monitor aPTT: Keep value at 1.5-2.5 times the baseline • HIT • Monitor PLT count • STOP Heparin if PLT less than 100,000/mm3 • Can use non-heparin anticoagulants as subs: DTI: argatroban Other: Parenteral Anticoagulants • Low molecular weight heparin: ENOXAPARIN [C] • Route: SQ • Indications: • • • • prevent deep vein thrombosis (DVT) in postop clients Treat DVT & PE Prevent complications in angina, non-Q wave MI & ST elevation MI NEVER GIVE HEPARIN & LOVENOX CONCURRENTLY TO THE SAME PATIENT 14 Administering EnoxaparinTherapy Enoxaparin : Deep SQ with patient lying down Do not expel air bubble before injection Hold down for 10 sec after administration Insert tuberculin syringe & needle into a skinfold b/w thumb and forefinger @ 90-degrees Hold • Hold skinfold until injection is completed15 Alternate • Alternate b/w left and right anterolateral and left & right posterolateraol abdominal wall Do not aspirate • Do not aspirate to avoid tissue damage Do not rub or massage • Do not rub or massage site to avoid bruising Warning • Box warning: spinal/epidural hematoma 16 Fondaparinux: Selective inhibitor factor Xa 17 • Use: prophylaxis for tx of DVT or PE [postop]; treat acute DVT/PE in conjunction with warfarin • Contra: CrCl <30 mL/min or a body weight of less than 50 kg • Bleeding/Hemorrhage: most common; Thrombocytopenia: D/c if PLT falls <150,000; HYPOKALEMIA • Do not give for 6-8 hours post surgery • Used in conjunction w/warfarin or other AC • No antidote; no standardized test to measure • Route: Injection via SQ Interactions • Herbal products • Garlic, ginger, glucosamine or ginkgo: Increase risk of BLEEDING • Nsg: • Teach that medication has an increased risk for bleeding • Monitor for bleeding 18 Vitamin K Antagonist • Warfarin: PROTOTYPE • ROUTE: PO • Action: • Antagonizes vitamin K, preventing the synthesis of factors II,VII, IX, X, 20 Warfarin: AE • Hemorrhage • VS, teach to observe for bleeding, baseline International Normalized ratio [INR] • Hepatitis • Monitor AST/ALT • Toxicity/OD • Give vitamin K IV slowly • Fresh frozen plasma (FFP) if Vitamin K cannot control bleeding 21 Contraindications • Pregnancy Cat. X: fetal hemorrhage, CNS effects • LOW PLT count or uncontrolled bleeding • Certain surgeries • Vit K deficiencies, severe kidney/liver disease, alcohol use • Bleeding diseases as hemophilia, PUD, severe HTN or threatened abortion, dissecting aneurysm • Breast feeding: enters breast milk 22 Interactions • Interactions: amiodarone [INR increases 50%]: cut warfarin dose in half when amiodarone added • Drug-food interactions: Foods high in Vit. K: Green leafy veggies: decrease anticoagulant effect of warfarin • Nsg: Consistency in intake • Herbals: SJW,, don quai, ginkgo, garlic, saw palmetto: increased risk of bleeding • Oral contraceptives, phenobarbital, Vit. K: decrease anticoagulant effect • Nsg: • avoid concurrent use if possible • Monitor PT/INR: watch for reduced PT/INR levels • Adjust accordingly to INR 23 Nursing 24 • Administration is usually oral, once daily, and at the same time each day. • Obtain baseline vital signs. • Monitor PT levels (therapeutic level 18 seconds) and INR levels (therapeutic levels 2 to 3); mechanical/artificial heart valves: INR 2.53.5 • INR levels are the most accurate. • Hold dose and notify the provider if these levels exceed therapeutic ranges. • Obtain baseline and monitor CBC, platelet count, and Hct levels. • Be prepared to administer vitamin K for warfarin toxicity. • ● Plan for frequent PT monitoring Nursing • Bridging to warfarin if on Heparin continuous infusion • Started 2-3 day while pt is on Heparin IV therapy • Must have therapeutic INR in order to transition to warfarin PO, in other words for the drip of Heparin to be d/c • Normal range: 0.8-1.2 • Therapeutic range: 2-3; if mechanical heart valves: maintain INR 2.5-3.5: why: risk for thrombi • Consistent amount of green leafy veggies • Antidote/antagonist on hand: Vit K 25 Teach Teach to avoid alcohol, OTC and nonprescription meds to prevent AE and med interactions [risk of bleeding] Prevent Prevent development of thrombi by avoiding sitting for prolonged periods of time, not wearing constricting clothing and elevating and moving legs when sitting Wear Nursing Record Use Wear medic-alert bracelet indicating warfarin use Record dosage, route, time on daily basis. Report this to provider Use soft bristle toothbrush, electric razor for shaving] Report Report any signs of bleeding Follow Follow-up with provider for regular monitoring of INR Reinforce Reinforce safety w/all anticoagulants 26 DIRECT-THROMBIN INHIBITOR • Route: PO • Action: binding with and inhibiting thrombin, thus preventing a thrombus from developing • Use • Stroke prevention, systemic embolization [nonvalvular Afib] • Tx/prevent DVT & PE AE • Bleeding Nsg • Teach to report signs of bleeding • SEVERE: Antidote: IDARUCIZUMAB; or if needed hemodialysis • Elective surgery/invasive procedure should stop taking dabigatran before 1-2 surgery if CrCl >50 or 3-5 days CrCl <50 • GI effects: dyspepsia, abd. Pain, gastritis, anemia • Take Dabi with food • Might need PPI or H2RA for upset GI • Other • Back pain, nausea, hypotension, headache: Bivalirudin • Injection-site mass, anemia, nausea, deep thrombophlebitis: Desirudin 28 Interactions • Other anticoagulants and thrombolytics: increase risk of bleeding • Monitor coagulation studies • Herbals: feverfew, garlic, glucosamine, ginkgo bilboa, saw palmetto: Bleeding risk Nsg • Dabigatran: • Oral capsules: swallowed whole; take w/or without food. Use within 30 days • D/C other anticoagulants when starting dabigatran • Bivalirudin: IV direct bolus or infusion • Argatroban: IV continuous infusion. Stop heparin & check PTT before starting • Desirudin: Deep SQ into abdomen or thigh 29 DTI: Xaban Family • Rivaroxaban: Prototype • Others: Apixaban, edoxaban • Action: • Rivaroxaban inhibits platelet activation and formation of fibrin clotting by inhibition of factor Xa in both intrinsic and extrinsic coagulation pathways • Use: Tx & secondary prevention VTE, stroke [nonvalvular afib] patients • AE: Bleeding Contra • Increased risk hemorrhage: pregnancy • Previous allergy, active bleeding, severe kidney impairment or mod to severe liver impairment • Cautious use: taking other anticoagulants, antiplatelet or fibrinolytics: mild or mod kidney problems Interactions • Herbals: • St. John’s wort: decrease levels Rivaroxaban • Alfalfa, anise, Feverfew, garlic, ginger, glucosamine, gingko, saw palmetto, grapefruit: increase risk of bleeding 31 NURSING • Administer tabs PO once daily with/without food, same time each day; NV afib: evening meal • No monitoring of INR or other coagulation parameter needed • Stroke and systemic emboli prevention: once daily with evening meal • Baseline & Monitor H/H, liver, kidney function-BUN/SCr & CrCL • Observe & Teach to watch for bleeding • Instruct to notify all providers about use esp before spinal/or epidural procedures: increase hematoma or bleeding around spine 32 Antiplatelets 33 • Antiplatelet/cyclooxygenase inhibitor • SELECT PROTOTYPE MEDICATION: Aspirin [C]-Inhibit synthesis of prostaglandins; prevents formation of thromboxane A-2; • Antiplatelet/glycoprotein inhibitors [GP Ila/Ilb] • SELECT PROTOTYPE MEDICATION: Abciximab [C]-monoclonal • OTHER MEDICATIONS: Eptifibatide, tirofiban • Antiplatelet/arterial vasodilator: Dipyridamole; • Phosphodiesterase-3 enzyme inhibitor: cilostazol • Antiplatelet/Adenosine Disphosphate Receptor Antagonist [ADP inhibitors]: Clopidogrel [B]; other: Ticagrelor, prasugrel, cangrelor • Clopidogrel: • ADP Action: prevent platelets from clumping together by inhibiting enzymes and factors that normally lead to arterial clotting. ● inhibit platelet aggregation at the onset of the clotting process. These medications alter bleeding time. ADP Receptor: Clopidogrel • Use • Primary prevention of acute myocardial infarction • Prevention of reinfarction in clients following an acute myocardial infarction • Prevention of ischemic stroke or transient ischemic attack , ischemic event: symptomatic atherosclerosis or w/Acute coronary syndromes • AE [Clopi]: Pruritis, rash, purpura, diarrhea, TTP, hemorrhage, severe neutropenia • *Poor metabolizers for CYP2C19: prasugrel or ticagrelor Routes • ROUTES OF ADMINISTRATION • ● Aspirin: Oral ● Abciximab: IV ● Clopidogrel: Oral ● Dipyridamole: Oral ASA: AE • GI effects: n/v/dyspepsia • Hemorrhagic stroke • Prolong bleeding time, GI bleed, Thrombocytopenia • Tinnitus, hearing loss • Clopidogrel • BLEEDING • GI: diarrhea, dyspepsia, pain 37 AE • Abciximab • HYPOTENSION; Bradycardia [HR/Pulse < 60 beats per minute] • Nsg: Monitor HR and BP 38 • Dipyridamole • GI: similar to ASA • Nsg: • Take w/food • Do not crush or chew medication • Monitor hydration if GI upsets AE • Abciximab • HYPOTENSION; Bradycardia [HR/Pulse < 60 beats per minute] • Nsg: Monitor HR and BP 39 • Dipyridamole • GI: similar to ASA • Nsg: • Take w/food • Do not crush or chew medication • Monitor hydration if GI upsets Contra • ASA: bleeding disorders • Third trimester use • Thrombocytopenia • DO NOT give to children or adolescents who have a fever or recent chickenpox [Reye’s Syndrome] • Caution: elderly 40 • Abciximab • Low plts, recent stroke, uncontrolled BP, recent surgery • Clopidrogrel • Low plts, bleeding history from PUD and intracranial bleed, breastfeeding • Cautious use in PUD, severe kidney or hepatic disease Interaction • Drugs That Increase the Effects of Clopidogrel • Aspirin, nonsteroidal anti-inflammatory drugs, platelet inhibitors, thrombolytics • Increase the risk of bleeding • Atorvastatin: May affect antiplatelet activity • Herbal: Increase effects of Clopi: garlic, ginkgo, ginger, green tea, horse chestnut, SJW NSG • Aspirin 325 mg should be taken during initial acute episode of myocardial infarction. • Clopidogrel is sometimes prescribed concurrently with aspirin, which increases the risk for bleeding. • Clopidogrel should be discontinued 5 to 7 days before an elective surgery. • CLIENT EDUCATION • ● Prevention of strokes, myocardial infarctions, and reinfarction can be accomplished with low-dose aspirin (81 mg)-this is a baby aspirin dose [safe for daily use] • ● Notify the provider regarding aspirin use 42 ACTION: Alteplase is a protein that lyses unwanted fibrin blood clots by catalyzing the conversion of plasminogen to plasmin. AE/Contraindications • • • • • Bleeding-main adverse effect Major risk of rtPA therapy is symptomatic brain hemorrhage tPA overdose, aminocaproic acid serves as an antidote Contraindications Risk C • • • • • Hemorrhagic stroke Active internal bleeding Closed head or spinal trauma Brain tumors Cautious use: severe HTN, Cerebral vascular disorders, recent GI or GU bleeding, major surgery within past 10 days Interactions • Concurrent use of other medications that enhance bleeding [NSAIDS, Heparin, Warfarin, thrombolytics, antiplatelets] • Herbals: cat’s claw, dong quai, evening primrose, feverfew, garlic, ginkgo, green tea, horse chestnut, red clover • Nsg • If concurrent use: Monitor carefully for signs of bleeding 45 Nursing 46 • Use of thrombolytic agents should take place as soon as possible after onset of manifestations (within 3-4.5 hr is best: Stroke) • Clients receiving a thrombolytic agent should be monitored in a setting that provides for close supervision and continuous monitoring during and after administration of the medication. • Obtain the client’s weight to calculate the dosage. • Obtain baseline platelet counts, hemoglobin (Hgb), hematocrit (Hct), aPTT, INR, and fibrinogen levels. Monitor periodically. • Minimize IM injections: bleeding, bruising, hematoma • Cardiac monitoring: dysrhythmias: Sinus brady, PVC, VTac Nursing • Obtain baseline vital signs (heart rate, blood pressure), and monitor frequently per protocol. • Nursing care includes continuous monitoring of hemodynamic status to assess for therapeutic and adverse effects of thrombolytic (relief of chest pain, indications of bleeding) • Discontinue thrombolytic therapy if life-threatening bleeding occurs. • Treat blood loss with whole blood, packed red blood cells, and/or fresh frozen plasma. • Ensure that IV aminocaproic acid is available for administration in the event of excessive fibrinolysis 47 Nursing 48 • After thrombolytic Rx: administer heparin or ASA as prescribed to decrease risk of rethrombosis • After thrombolytic Rx: give beta blocker as prescribed why? Lower O2 myocardial 22 consumption • Give H2RA or PPI to prevent GI bleeding Other: Control Bleeding: Pg. 169-170 Chapter • Cascade • Key concepts • Blackbox warnings