Emergency Medicine Case Studies: Trauma, Pregnancy, Neurology
advertisement
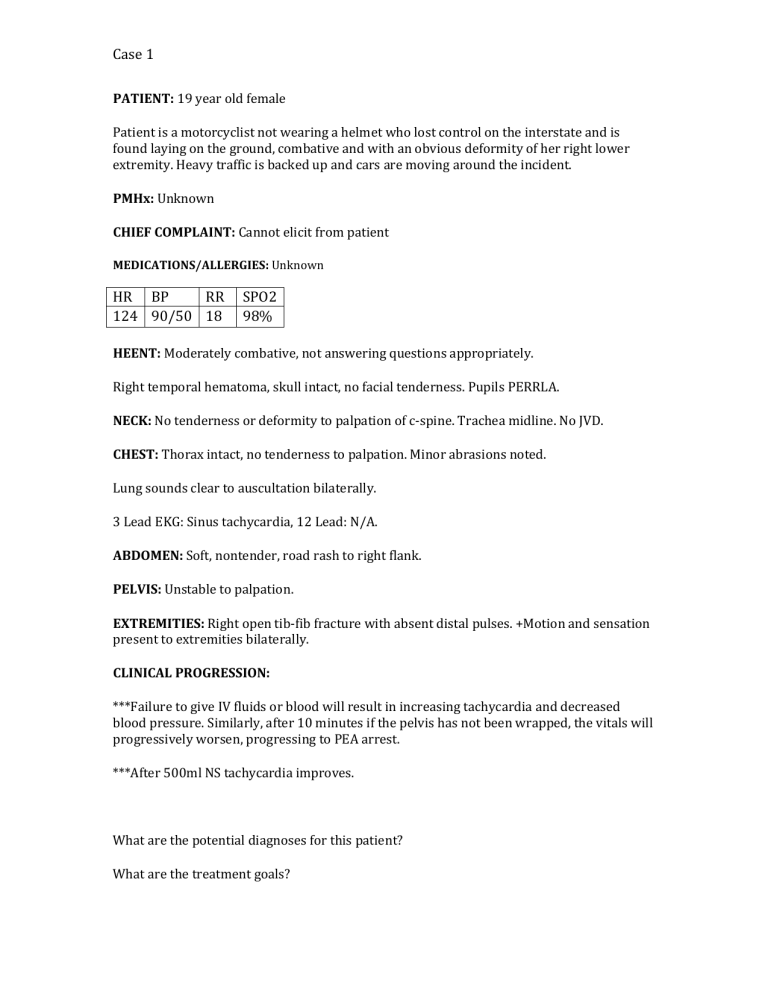
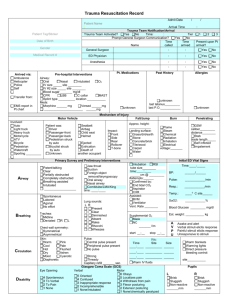
Case 1 PATIENT: 19 year old female Patient is a motorcyclist not wearing a helmet who lost control on the interstate and is found laying on the ground, combative and with an obvious deformity of her right lower extremity. Heavy traffic is backed up and cars are moving around the incident. PMHx: Unknown CHIEF COMPLAINT: Cannot elicit from patient MEDICATIONS/ALLERGIES: Unknown HR BP RR 124 90/50 18 SPO2 98% HEENT: Moderately combative, not answering questions appropriately. Right temporal hematoma, skull intact, no facial tenderness. Pupils PERRLA. NECK: No tenderness or deformity to palpation of c-spine. Trachea midline. No JVD. CHEST: Thorax intact, no tenderness to palpation. Minor abrasions noted. Lung sounds clear to auscultation bilaterally. 3 Lead EKG: Sinus tachycardia, 12 Lead: N/A. ABDOMEN: Soft, nontender, road rash to right flank. PELVIS: Unstable to palpation. EXTREMITIES: Right open tib-fib fracture with absent distal pulses. +Motion and sensation present to extremities bilaterally. CLINICAL PROGRESSION: ***Failure to give IV fluids or blood will result in increasing tachycardia and decreased blood pressure. Similarly, after 10 minutes if the pelvis has not been wrapped, the vitals will progressively worsen, progressing to PEA arrest. ***After 500ml NS tachycardia improves. What are the potential diagnoses for this patient? What are the treatment goals? Case 1 PATIENT: 31 year old female Patient was the restrained passenger of a vehicle that was struck by a truck during a snow storm. There is moderate intrusion into the passenger compartment and shattered windows. The patient is found sitting in the passengers seat holding her abdomen complaining of pain. The passenger side door must be removed by the fire department to gain access to the patient. HEENT: Patient is awake and alert with a GCS of 15. She denies LOC but states striking her head on the airbag. Pupils are PERRLA. No facial injuries noted. NECK: Patient has no deformity of neck and denies tenderness to palpation of c spine. CHEST: Red abrasion from seatbelt across the chest. Patient reports mild tenderness to palpation. Equal bilateral chest rise. Patient does not display any signs of increased WOB. Denies SOB. ABDOMEN: Patient is visibly gravid and reports she is P1 G2 x28 weeks with 1 prior miscarriage at 18 weeks 2 years ago. Patient reports diffuse abdominal pain that is 10/10 and describes it as tearing. BACK: Flank ecchymosis present. SKIN: Pink, warm, dry. Brisk cap refill. PELVIS: Intact and stable GI/GU: Blood noted on seat when patient is moved EXTREMITIES: PMS intact x4 extremities, patient denies injuries. CLINICAL PROGRESSION: Patient becomes hypotensive during transport suggesting fetal demise and severe internal bleeding. VITALS: HR: 138 BP: 82/56 RR: 10 SPO2: 92% RA What is concerning about this patient? Why does this patient not initially show signs of shock? What is your treatment plan? Case 1 PATIENT: 78 year old male Patient sustained a fall down 18 steps onto a concrete basement floor. He is unsure if he lost consciousness but has a large hematoma to the occiput. He does not remember the fall but felt dizzy prior to the event. HEENT: Patient is awake and confusedwith a GCS of 14. Unknown LOC, + amnesia of event. Pupils are unequal, left pupil is 5mm right pupil is 3mm. They are sluggish to light. Patient reports headache that feels like his head is in a vice grip. NECK: Patient has no deformity of neck but reports tenderness to c spine palpation. No trachea deviation or JVD present. CHEST: Equal chest rise and fall. No symptoms of WOB present. ABDOMEN: Soft, non tender. BACK: Redness noted to flanks where patient was laying on the floor. SKIN: Pink, warm, dry. PELVIS: Intact and stable GI/GU: N/A EXTREMITIES: PMS present CLINICAL PROGRESSION: Patient becomes altered and unable to answer questions while stair chairing to stretcher. During transport he becomes unresponsive GCS of 3. VITALS: HR: 48 BP: 204/118 RR: Irregular, deep and rapid alternating SPO2: 89% RA What is your diagnosis of this patient? How would you manage this patient? What clinical findings support your diagnosis?