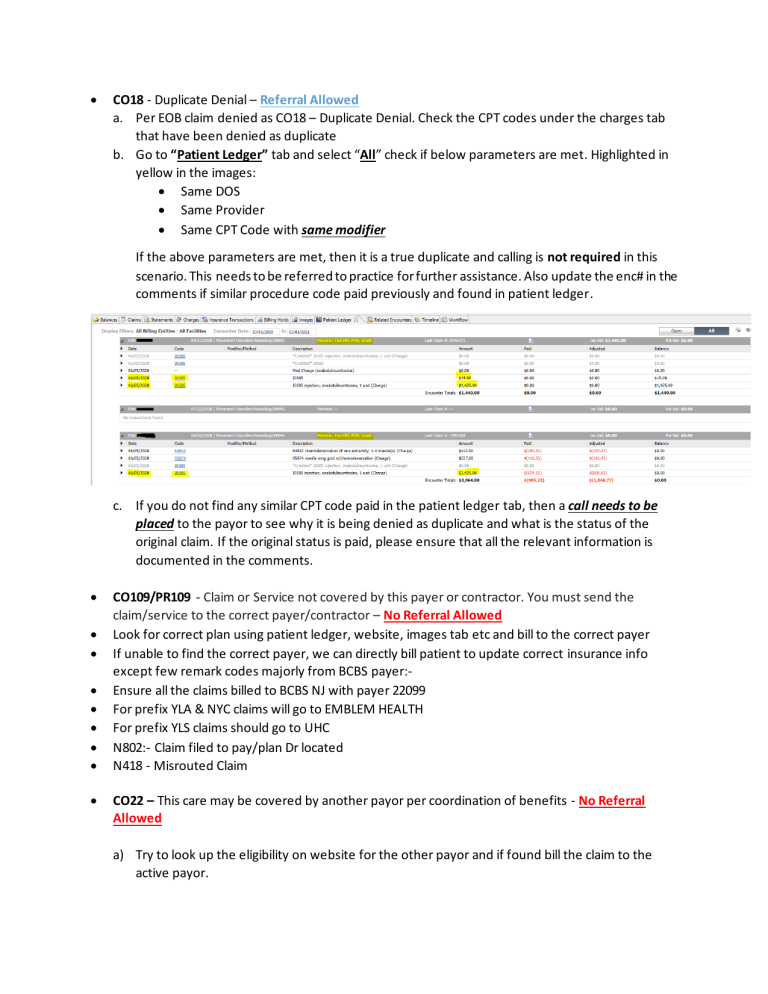
• CO18 - Duplicate Denial – Referral Allowed a. Per EOB claim denied as CO18 – Duplicate Denial. Check the CPT codes under the charges tab that have been denied as duplicate b. Go to “Patient Ledger” tab and select “All” check if below parameters are met. Highlighted in yellow in the images: • Same DOS • Same Provider • Same CPT Code with same modifier If the above parameters are met, then it is a true duplicate and calling is not required in this scenario. This needs to be referred to practice for further assistance. Also update the enc# in the comments if similar procedure code paid previously and found in patient ledger. c. If you do not find any similar CPT code paid in the patient ledger tab, then a call needs to be placed to the payor to see why it is being denied as duplicate and what is the status of the original claim. If the original status is paid, please ensure that all the relevant information is documented in the comments. • • • • • • • • • CO109/PR109 - Claim or Service not covered by this payer or contractor. You must send the claim/service to the correct payer/contractor – No Referral Allowed Look for correct plan using patient ledger, website, images tab etc and bill to the correct payer If unable to find the correct payer, we can directly bill patient to update correct insurance info except few remark codes majorly from BCBS payer:Ensure all the claims billed to BCBS NJ with payer 22099 For prefix YLA & NYC claims will go to EMBLEM HEALTH For prefix YLS claims should go to UHC N802:- Claim filed to pay/plan Dr located N418 - Misrouted Claim CO22 – This care may be covered by another payor per coordination of benefits - No Referral Allowed a) Try to look up the eligibility on website for the other payor and if found bill the claim to the active payor. b) If we did not find any other payor information, check other encounters/images tab/power chart to see if there is any other active insurance. If located, then check the eligibility and bill it to the other/active payor c) If we still cannot locate any active insurance, then we can go ahead and bill the same to the patient. • CO97-PI97 – Pmt included in allow for other svc/proc - No Referral Allowed a) Check charges tab to see how many CPT’s were billed in the claim b) If one CPT code is denied as inclusive and rest all CPT’s have been paid, then we can adjust the denied using 2700 adjustment code a) If only one CPT code was billed and was denied as bundling, then call payor and ask the primary cpt code with which it was bundled. Check if the procedure code was earlier billed in patient ledger, if yes then mention the same in comments and adjust the denied cpt code using adjustment code 2700. Post adjustment once the insurance pending goes to 0, complete the benefit order. Adjustments are to be taken from the Charges tab. c) If rep is not able to locate the primary cpt code, then ask the rep to reprocess the claim d) If amount is >3k do not adjust the balance, refer it to practice first for further review • CO96 – Non-Covered Services – Referral Allowed a) Call payor to see why the claim has been denied as non-covered. Do not send directly to payor as per the EOB without calling. Once the reason is obtained from the payor (e.g. coding issues etc) as to why the claim was denied for non-covered services, then forward to practice review with detailed comments. • PR96 – Non-Covered Services – No Referral Allowed a) Call payor to see why the claim was denied as non-covered, e.g. if the cpt is not covered as per plan etc. Post which if its patient responsibility then bill the claim to patient. • CO197 - Precert/auth/notification absent - Referral Allowed b) Call payor to ascertain if the authorization is required for the service or if the provider is not credentialed c) If the services require an auth then confirm if there is a valid auth on file or not or if we can do a retro auth. If yes, ask the rep to send the claim back for reprocessing. If no, then send the claim to practice requesting an authorization d) If the provider is not credentialed or out of network check with payor if there is an auth on file or not. If yes, ask the rep to send the claim back for reprocessing. If no, check credentialing grid and if provider status shows “provider non par/pending par/blank” then adjust the claim with non-par alias code 2900 e) In credentialing grid if the provider shows as “Address not listed or termed” then this needs to be added in the non-par tracker for Elishia to review the credentialing status f) Post adjustment once the insurance pending goes to 0, complete the benefit order AUTH for Horizon Payer with 3HZN member id:- Please see below the updated workflow for denials received for no authorization for Horizon plans only (Insurance ID containing 3HZN): 1) Check the claim form to ensure that no authorization code was billed. If a auth was billed then contact payor to have the claim reprocessed. 2) If no auth was billed on the claim then associate can check if the procedure code needs an authorization or not. This can be checked on the Horizon online tool by following the below link: https://webapps.horizonblue.com/priorauthtool 1) If the service shows as authorization required and the POS is not equal to 21 then will go ahead and refer to practice to provide an authorization for the DOS 2) If the service shows as authorization required with POS 21 then associate will have to call the payor and check for hospital authorization on file to reprocess the claim. If the rep denied for any auth being on file then refer to practice for authorization. 3) If the service shows as authorization is not required then need to contact the payor for the root cause of the denial (e.g. if the provider was non participating etc.) and work accordingly • CO26/CO27 & PR26/PR27 – Coverage Terminated - No Referral Allowed a. Check other encounters/images tab/power chart to see if there is any other active ins. If located, then check the eligibility on website and bill it to the other/active payor b. If we still cannot locate any active insurance, then we can go ahead and bill the same to the patient. No need to call payor c. Notate all the necessary info in comments like effective and termination date d. If effective and termination date could not obtained through website, please call payer and get the information • Diagnosis was invalid for the date of service reported - Referral Allowed a) Check claim form to see how many dx were billed in the claim. If there is only one dx code billed, then refer it to practice for review as per practice liaison. b) If there is more than one dx code billed on the claim, then call payor to identify which dx code is invalid. Need to mention the same in comments when sending back to practice for review c) If multiple dx code were billed but remark code says “principle dx is invalid/incomplete then we can mention the dx code in comments and refer it to practice without calling ins • CO4 – The procedure code is inconsistent with the modifier used - Referral Allowed a. Call needs to be placed to the payor to identify the correct reason for the denial. Do not send directly to practice for review b. If CPT code billed without modifier and modifier should have been appended as per analysis, we can directly refer it to practice to add modifier • CO50 – These are non-covered services because this is not deemed a ‘medical necessity’ by the payer – Referral Allowed a. Call needs to be placed to the payor to get the LCD/NCD billing guidelines because of which the claim was denied for medical necessity. Do not sent to practice without calling the payor • CO119 – Benefit maximum for this time period or occurrence has been reached - Referral Allowed a. Need to call payor to know the reason for the benefit max, e.g. if the procedure code can only be billed once in lifetime, or it can only be billed once in 90 days etc. b. Analysis:- based on analysis if CPT can be paid once in year and same CPT was found as paid in patient ledger under same provider and TAX ID, we can update that enc# and when it was paid details in comments and refer it to practice for further review c. Once the reason is obtained send the claim to practice review • CO 181 & other related denials – Procedure code was invalid for the date of service - Referral Allowed a. Need to call payor to know the exact reason of why the procedure code is not valid. b. Once the reason is obtained send the claim to practice review • Claim Paid Greater than 30 days – Referral Not Allowed a. If EOB not available in RM & CPDI, Associate must obtain all the below information along with the copy of paid EOB, before tagging the encounter for Found Money for posting: b. For Paper Check i. Check Number ii. Check Date iii. Payment Amount iv. Bulk Check Amount v. Cashed Date vi. Address it was mailed to c. For EFT Payments i. EFT Number ii. Deposit Date iii. Deposit Amount iv. Cleared/Cashed Date • IF EOB available in RM & CPDI:- Update paid details, check/EFT#, paid date, bulk amount etc. no need to call insurance if EOB is available in system. • B16 – New Patient qualifications were not met - Referral Allowed a. Check patient ledger to see if we have already billed a new patient code earlier for this patient. b. If we have already billed a new patient code, then we can credit the charge and bill an established patient code as per the below grid. (PECC approved) E&M Code, New Patient 99201 99202 99203 99204 99205 E&M Code, Est. Patient 99211 99212 99213 99214 99215 c. If the new patient code was billed correctly and you do not see any previous new pt codes being billed to the payor then need to call payor to check why the claim was denied. Once the relevant information is obtained, forward to practice for review with detailed comments. • CO16 – M51 – Missing/Incomplete/Invalid Procedure codes - Referral Not Allowed a. For All payors we can crosswalk the appropriate procedure codes from the below list and bill correct procedure codes Outpatient / Office Consult Codes E&M Code, New Patient E&M Code, Est. Patient ER consults 99241; Office Consultation 99201 99211 99281 99242; Office Consultation 99202 99212 99282 99243; Office Consultation 99203 99213 99283 99244; Office Consultation 99204 99214 99284 99245; Office Consultation 99205 99215 99285 Inpatient Consultation E&M Code Desired, Hospital E&M Code Desired, Nursing Facility 99251; Inpatient Consultation Unbillable return to provider Unbillable return to provider 99252; Inpatient Consultation Unbillable return to provider Unbillable return to provider 99253; Inpatient Consultation 99221 99304 99254; Inpatient Consultation 99222 99305 99255; Inpatient Consultation 99223 99306 • CO5 – The procedure code/type of bill is inconsistent with the place of service – Referral Allowed a. Associate need to ascertain the reason by reviewing payor guidelines or by calling payor as to why the code or POS billed is inconsistent. b. Once the information is obtained send a referral to practice with detailed comments • CO58 – Treatment was deemed by the payer to have been rendered in an inappropriate or invalid place of service - Referral Allowed a. Associate need to ascertain the reason by reviewing payor guidelines or by calling payor as to why the code or POS billed is inconsistent. b. Once the information is obtained send a referral to practice with detailed comments • CO59 – Processed based on multiple or concurrent procedure rules. - Referral Allowed a. Review the insurance transactions to ensure the payment has been posted to the line items and the remaining balance is denied as CO59 b. We can adjust the amount under CO59 as contractual adjustment. Any patient responsibility needs to be billed to patient as per EOB • B23 – Procedure billed is not authorized per your Clinical Laboratory Improvement Amendment (CLIA) Proficiency Test - Referral Not Allowed a. If claim is denied for CLIA, then please review the procedure code in the folder to see if the CLIA is updated there or not. If found, then add and bill claim to payor b. If the CLIA is not on the list, please use the below Status and Action code so that the supervisor can identify the claims at day end and send it to KC team for review. Status_Code Action_Code New_Effectiveness_Metrics Claim_Denied_Clia#_Is_Invalid_Not_Available Referred_to_Supervisor Pending_Clarrification_From_Supervisor • • • • • Hospice Denials:- Referral Allowed First we need to check whether claim was billed GW & GV modifier, if yes then call insurance and ask rep to reprocess the claim If not then refer it to practice for further assistance If claim was not billed to medicare then we need to find out the medicare details through images tab, patient ledger, power chart if found then update the medicare details and bill the claim to medicare If not, then bill patient to update medicare insurance information CO-24:- Capitation denial:- Referral Not Allowed • • • • • If claim has been denied for capitation, we can adjust the balance irrespective of dollar value. Below are the guidelines to post the adjustment Capitation Amount:- Check the allowed amount in EOB which should be adjusted using adjustment code as per plan (updated in adjustment master) Contractual Amount:- Contractual amount will be adjusted separately using adjustment code 2000 If EOB is not available in RM or CPDI, we will not post the adjustment will request the EOB first. If in case EOB is available on website, we will forward it to posting team to post the denial in CPM CAN’T ID:-New Born Baby:- Referral Not Allowed • • • If claim denied as patient can not be identified and patient is new born We need to verify the subscriber details in claim form whether it was billed with appropriate information or not If not we can make changes in claim form or in encounter level to bill the claim with correct subscriber or patient information Telehealth POS (02) update: Referral Not Allowed ( Call is not required if claim billed with Modifier) Telehealth CPT codes 99441 – 99445, These codes will not require 95/GT modifier to be billed with them. We can remove the modifiers from these CPT codes and rebill corrected claims back to payor upon receipt of related denials. For other CPT’s:- we can change telemedicine modifier based on payer guidelines instead of sending them to practice. For example: If UHC Medicare payer required 95 modifier but claim was billed with GT and denied, we can go ahead and change the modifier to 95 instead of sending the referral back to practice / R1 coding. Call is still needed to validate the exact denial which is causing the issue payer/CPT/POS/Modifier combination that are causing the denials. Small Dollar Balance Adjustment:- We have approval to adjust $4.99 or below as small dollar adjustment. Please use RCA38 with ARM18 and adjustment alias code 2505. • Other Bundling Denials - Referral Not Allowed • 99000 This proc is not paid separately, if CPT 99000 denied for this reason (inclusive) we can directly adjust with adjustment alias code 2908. • If claims denied for CPT 93306 with modifier 26 as - “CO4 – Procedure code inconsistent or missing modifier”. We can have these sent directly to the practice for review without calling the payor first. • PR204:- we can not directly bill patient . Also refer the below pointers for some specific payers:- We are no longer billing the claims directly to patient. 1) Need to do a follow up with insurance if the denial is because of plan benefits. 2) If the denial is due to Plan benefit then we can bill the claims to patient. 3) If the denial is due to provider’s credentials, then we need to refer them to Practice. 4) Its mandatory to mention the call reference number in comments. 5) Comments needs to be more specific and descriptive to understand the scenario. • • • • • All Payor Consult Codes – Crosswalk corrected claim BCBS NYC Prefix – Emblem Health (GHI) BCBS YLS Prefix – UHC PR 204 & CO 204 – Not to be billed to patient – call insurance and validate the denial Release unnecessary work queue (Referrals, Found Money, Posting Queues etc.) CO-8 :- Proc cd inconsistent w/provider type - No Referral Allowed • • • • if the provider/payer/tax id combination is listed in the CG as “pending” o use “Non Par Credentialing” work item If the provider/payer/tax id combination is not listed in the CG o use “Non Par Credentialing” work item If the provider/payer/tax id combination is listed in the CG as “Participating” o Please call the payer and confirm the credentialing information and reprocess o If the provider Is not credentialed – use “Non Par Credentialing” work item CO242 – Services not provided by network/primary care providers – No Referral Allowed a) Check the provider credentialing grid to see if the provider was participating on the DOS. If the provider is not credentialed or out of network per credentialing grid on DOS then adjust the claim with non-par alias code 2900 b) Also if claim denied for credential issue and TFL has exhausted then encounter balance can written off with non-par alias code 2900. Found Money Update: As per instruction given by Hendo on leadership call, we must move all VCC payment in found money. As per Payment team we have find out some payment series like 002, 003, 005. If we have any different check #, then either team will follow the previous notes or will call to the insurance to confirm that payment is VCC or not. All VCC payment will move to found money Queue Will use the below status and action code: Status Code Action Code Claim Paid - Virtual Card Payment EFT not Enrolled 1. High Dollar Adjustment (>3K) Approval cases will be referred to “Sharon’Kosman” as T-2 Referral 2. All the Coding related (CPT, DX, MOD etc) & Duplicate Denial referrals regardless of practice will be referred to “Angela’Smith”