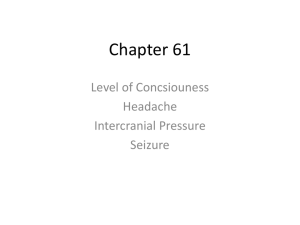
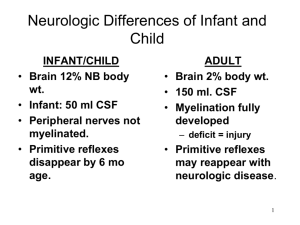
NCMB 418 NEUROLOGICAL EMERGENCIES Diagnostic Tests Skull and spinal radiography - Always check with the client about the possibility of pregnancy before any radiographic procedures are done CT Scan - An informed consent is needed for any invasive procedure, including those that use contrast medium (dye) - Assess the need to withhold metformin (worst adverse effect of metformin: LACTIC ACIDOSIS) if iodinated contrast dye is used for a diagnostic procedure Magnetic Resonance Imaging (MRI) - A noninvasive procedure that identifies: Tissues Tumors Vascular abnormalities It is similar to CT scanning but provides more detailed pictures - An informed consent is needed for any invasive procedure, including those that use contrast medium (dye) - An MRI is contraindicated in a pregnant Increase in amniotic fluid temperature that occurs during the procedure maybe harmful to the fetus Lumbar Puncture - Check for infection - Insertion of a spinal needle through L3-L4 (it is the safest landmark) interspace into the lumbar subarachnoid space to; Obtain CSF Measure CSF fluid or pressure Instill air, dye, or medications - The test is contraindicated in clients with increased intracranial pressure (ICP) Will cause a rapid decrease in pressure (leading to BRAIN HERNIATION) in the SCF around the spinal cord Electroencephalography (EEG) Neurological Assessment Assessment of Risk Factors Trauma Hemorrhage Tumors Infection Toxicity Metabolic disorders Hypoxic conditions Hypertension Cigarette smoking Stress Aging process Chemicals, either ingestion or environmental exposure The most sensitive indicator of neurological status: LOC Anatomy and Physiology Normal ICP: 5-15mmHg >20mmHg need treatment! Cerebral Perfusion Pressure 𝐶𝑃𝑃 = 𝑀𝐴𝑃 – 𝐼𝐶𝑃 Cerebral Perfusion Pressure - Cerebral metabolic need= cerebral blood flow Mean Arterial Pressure Intracranial Pressure BRAIN: badly needs, but cannot store them, therefore the brain depends ADEQUATE BLOOD SUPPLY on to obtain EGO Electrolytes Glucose Oxygen Increased ICP: CUSHING’S TRIAD Cerebral angiography - To see if there are part of cerebral vessels that are blocked NCMB 418 INCREASED ICP Causes Trauma Hemorrhage Growths and tumors Hydrocephalus Edema Inflammation Results Impedes - Circulation to the brain - Absorption of CSF Affect the functioning of nerve cells Brainstem compression Death Assessment Abnormal respirations Rise in blood pressure with widening pulse pressure - PP = SBP - DBP - 40mmHg Slowing of pulse Elevated temperature Vomiting Pupil changes Late signs of Increased ICP include; (CUSHING’S TRIAD: signs of increased ICP and impending herniation) - Increased systolic BP - Widened pulse pressure - Slowed heart rate Other late signs include changes in motor function; - Weakness too hemiplegia - A positive Babinski’s reflex - Decorticate or decerebrate posturing, and seizures Intervention Monitor respiratory status and prevent hypoxia Avoid the administration of morphine sulfate - To prevent the occurrence of hypoxia Maintain mechanical ventilation as prescribed - Maintaining the PaCO2 at 30-35mmHg Vasoconstriction of the cerebral blood vessels Decreased blood flow decreased ICP Maintain body temperature ↑ Body temperature ↓ ↑ Metabolic activities in the brain ↓ ↑ ICP Prevent shivering - Can increase ICP Monitor - Eletrolye levels - Acid-base balance - I and O Limit fluid intake to 1200mL/day Instruct client to avoid straining activities - Coughing - Sneezing Instruct the client to avoid Valsalva’s maneuver Note: For the client with increased ICP; - Elevate the HOB 30-40 degrees - Avoid the Trendelenburg’s position ↑ Preload ↑ BF going to the brain - Prevent flexion of the neck and hips Medications Antiseizure - Seizures increase metabolic requirements and cerebral blood fluid and volume, thus increasing intracranial pressure (ICP) - Medications may be given prophylactically to prevent seizures Antipyretics and Muscle Relaxants - Temperature reduction decreases metabolism, cerebral blood flow, and thus ICP - Antipyretics prevent temperature elevations - Muscle relaxants prevent shivering BP Meds - May be require to maintain cerebral perfusion at a normal level - Notify the PHC provider if the BP <100mmHg systolic 150mmHg systolic IV Fluids - Via an infusion pump to control the amount administered - Infusions are monitored closely because of the risk of promoting: Additional cerebral edema Fluid overload Corticosteroids - Stabilize the cell membrane and reduce leakiness of the BBB - Decrease cerebral edema NCMB 418 - Histamine blocker Counteract the excess gastric secretion that occurs with corticosteroid - Withdraw slowly from corticosteroid therapy to Reduce the risk of adrenal crisis Hyperosmotic Agent - Increases IV pressure by drawing fluid from the interstitial spaces and from the brain cells - Monitor renal function - Diuresis are expected Surgical Intervention: VENTRICULOPERITONEAL SHUNT Diverts CSF from the ventricles to the peritoneum Post procedure Interventions - Position client supine and turn from the bask to the non-operative side - Monitor for signs of increasing ICP resulting from shunt failure - Monitor for signs of infection TRAUMATIC BRAIN INJURY (TBI) Head injury is trauma to the skull, resulting in mild to extensive damage to the brain. Immediate complications: Cerebral bleeding Hematoma Uncontrolled increased ICP Infections Seizures Changes in personality or behavior, cranial nerve deficits, and any other residual deficits depend on the area of the brain damage and the extent of the damage Type of Head Injuries Open - Scalp lacerations - Fractures in the skull - Interruption of the dura mater Closed - Concussions Jarring of the brain Contusions Bruising type of injury to the brain tissue - Fractures Hematoma – collection of blood in the tissue that can occur as a result of a subarachnoid hemorrhage or an intracerebral hemorrhage Assessment - Assessment findings depend on the injury - Clinical manifestations usually result from increased ICP - Changing neurological signs in the client - Changes in LOC - Airway and breathing pattern changes - VS change, reflecting increased ICP - Headache, Nausea and vomiting - Visual disturbances, pupillary changes, papilledema - Nuchal rigidity Not tested until spinal cord injury is ruled out - CSF drainage from the ears or nose - Weakness and paralysis - Posturing - Decreased sensation or absence of feeling - Reflex activity changes - Seizure activity CSF can be distinguished from other fluids Presence of concentric rings - Bloody fluid surrounded by yellowish stain Halo sign CAF also tests positive for glucose when tested using a strip test Interventions Monitor - Respiratory status and maintain a patent airway Increased carbon dioxide (CO2) levels increase cerebral edema - Neuro status and VS, including temperature - Increased ICP Maintain head elevation - To reduce venous pressure Prevent neck flexion Initiate seizure precautions NCMB 418 Monitor for pain and restlessness Morphine sulfate or opioid medication - To decrease agitation and control restlessness cause by pain for the headinjures client on a ventilator - Administer with caution It is a respiratory depressant may increase ICP Monitor for drainage from the nose or ears - Fluid may be CSF Do not attempt to clean the nose, suction, or allow the client to blow her or his nose if drainage occurs Do not clean the ear if drainage is noted - Apply a loose, dry sterile dressing Check drainage for the presence of CSF Notify the PHCP is drainage from the ears or nose is noted and if the drainage tests positive for CSF Instruct the client to avoid coughing - Increase ICP Monitor for signs of infection Prevent complications of immobility Inform the client and family about the possible behavior changes SPINAL CORD INJURY (SCI) Description Trauma to the spinal cord Causes Partial Complete disruption of the nerve tracts and neurons Involves - Contusions - Laceration - Compression of the cord Motor vehicle crashes Falls Sporting and industrial accidents Gunshot or wound stab wounds Result Spinal cord edema Compromised capillary circulation and venous return SC necrosis Sequela Loss of - Motor function - Sensation reflex activity (especially in areas below the spinal cord) - Bowel and bladder control (S1 and S2) Complications Respiratory failure Autonomic dysreflexia Spinal shock Further cord damage Death Most frequently involved vertebrae C5, C6, and C7 T12 L1 Most fatal: C4 Transection of the Cord Complete transection of the cord SC is severed completely With total loss of sensation, movement, and reflex activity below the level of injury Partial transection of the cord SC is damaged or severed partially Symptoms depend on the extent and location of the damage If the cord has not suffered irreparable damage - Early treatment is needed To prevent partial damage from developing into total and permanent damage Cervical injuries Injury at - C2 to C3 is usually fatal - C4 is the major innervation to the diaphragm by the phrenic nerve - Above C4 Respiratory difficulty Paralysis of all four extremities - C5 and C8 Movement in the shoulder Decrease respiratory reserve Thoracic level injuries Loss of movement of the chest, trunk, bowel, bladder, and legs may occur, depending on the level of injury Paraplegia Autonomic dysreflexia with lesions or injuries above T6 and in cervical lesions may occur Visceral distention form noxious stimuli such as distended sweating or an impacted rectum may NCMB 418 cause reactions such as sweating, bradycardia, hypertension, nasal stuffiness, and goose flesh Lumbar and sacral level injuries Loss of movement and sensation of the lower extremities may occur S2 and S3 center on micturition - Below this level, the bladder will contract but not empty (neurogenic bladder) Injury above S2 in males - SNS nerve damage - (+) erection - (-) ejaculation Injury between S2 and S4 - SNS and PNS damage - (-) erection - (-) ejaculation Remember Always suspect SCI when trauma occur until this injury is rules out Immobilize the client n a spinal backboard with the head in a neutral position - To prevent an incomplete injury from becoming complete Emergency Interventions Emergency management is critical - Improper movement can cause further damage and loss of neurological function Assess the respiratory pattern and maintain patent airway Prevent head flexion, rotation, or extension During immobilization - Maintain traction and alignment on the head by placing hands on both side of the head by the ears Maintain an extended position Logroll the client No part of the body should be twisted or turns, and the client is not allowed to assume a sitting position In the ER, a cervical fracture should be place immediately in skeletal traction via skull tongs or halo traction - To immobilize the cervical spine and reduce the fracture and dislocation SPINAL AND NEUROGENIC SHOCK Spinal Shock A complete but temporary loss of motor, sensory, reflex, and autonomic function that occurs immediately after injury as the cord’s response to the injury Usually last less than 48 hours but can continue for several weeks Neurogenic Shock Occurs most commonly in client with injuries above T6 and usually is experiences soon after the injury Massive vasodilation occurs, leading to: - Pooling of the blood in blood vessels - Tissue hypoperfusion - Impaired cellular metabolism Assessment Neurogenic shock - Hypotension - Bradycardia Spinal shock - Flaccid paralysis - Loss of reflex activity below the level of the injury - Bradycardia - Hypotension - Paralytic ileus Interventions Monitor for - Signs of shock following a spinal cord injury - Hypotension and bradycardia - Reflex activity - Bowel and urinary retention - Return of reflexes Assess bowel sounds Provide supportive measures as prescribed, based on the presence of symptoms SPINAL AND NEUROGENIC SHOCK Description Also known as autonomic hyperreflexia It generally occurs - After the period of spinal shock is resolves - Injuries above T6 and in cervical lesions Triggers - Visceral distention - Distended bladder or - Impacted rectum It is a neurological emergency Sequela - Hypertensive stroke Assessment NCMB 418 Sudden onset Severe throbbing headache Severe hypertension and bradycardia Flushing above the level of the injury Pale extremities below the level of the injury Nasal stuffiness Nausea Dilated pupils or blurred vision Sweating Piloerection (goose bumps) Restlessness and a feeling of apprehension Nursing Priority Actions Raise the HOB and ask that the health care provider (HCP) be notified Loosen tight clothing on the client Check for bladder distention or other noxious stimulus Administer an antihypertensive medication Document occurrence, treatment, and response CEREBRAL ANEURYSM Description Dilatation of the walls of a weakened cerebral artery; can lead to rupture Assessment - Headache and pain - Irritability - Visual changes - Tinnitus - Hemiparesis - Nuchal rigidity - Seizures Interventions Maintain a patent airway (suction only with an HCP’s prescription) Administer oxygen as prescribed Monitor vital signs and for hypertension or dysrhythmias Avoid taking temperatures via the rectum Initiate aneurysm precautions Aneurysm Precautions Maintain the client on bed rest in a semi-fowler’s or a side-lying position Maintain a darkened room (subdued lighting and avoid direct, bright, artificial lights) without stimulation (a private room is optimal) Provide a quiet environment (avoid activities or startling noises); a telephone in the room is not usually allowed Reading, watching television, and listening to music are permitted, provided that they do not overstimulate the client Prevent any activities that initiate the Valsalva maneuver - Straining at stool - Coughing Provide stool softeners to prevent straining Administer care gently (such as the bath, back rub, range of motion) Limit invasive procedures Maintain normothermia Prevent hypertension Provide sedation Provide pain control Administer prophylactic antiseizure medication Provide deep vein thrombosis (DVT) prophylais as prescribed SEIZURES Seizures Abnormal, sudden, excessive discharge of electrical activity within the brain Epilepsy Chronic seizure activity Indicates brain or CNS irritation Causes Genetic factor Trauma Tumora Hypoglycemia Toxicity Infections Status epilepticus - Rapid succession of epileptic spasms without intervals of consciousness - A potential complication: BRAIN DAMAGE NCMB 418 Assessment Seizure history Type of seizure Occurrences before, before, and after the seizure Prodromal signs, such as mood changes, irritability, and insomnia AURA: sensation that warns the client of the impeding seizure Loss of motor activity or bowel and bladder function or loss of consciousness during the seizure Occurrences during the postictal state such as headache, loss of consciousness, sleepiness, and impaired speech or thinking Types of Seizures Tonic-Clonic - May being with an aura - Involves the stiffening or rigidity of the muscles of the arms and legs - Usually lasts 10 to 20 seconds, followed by loss of consciousness Clonic phase Hyperventilation and jerking of the extremities Lasts about 30 seconds Full recovery may take several hours Absence - A brief seizure that lasts seconds - May or may not lose consciousness - No loss or change in muscle tone occurs - May occur several times during a day - Victim appears to be daydreaming - More common in children Myoclonic Myoclonic - A brief generalized jerking or stiffening of extremities - Victim may fall from the seizure Partial Seizure Simple Partial - The simple partial seizure procedures sensory symptoms accompanied by motor symptoms that are localized or confined to a specific area. The client remains conscious and may report an aura Complex Partial - A psychomotor seizure - The area of the brain most usually involves is the temporal lobe - The seizure is characterized by periods of altered behavior of which the client is not aware - The client loses consciousness for a few seconds Interventions If the client is having a seizure, maintain a patent airway Do not force the jaws open or place anything in the client’s mouth Note the time and duration of the seizure Assess behavior at the onset of the seizure: If the client has experiences an aura, if a change in facial expression occurred, or if a sound or cry occurred from the client If the client is standing or sitting, place the client on the floor and protect the head and body Support airway, breathing, and circulation Administer oxygen Prepare to suction secretions Turn the client to the side to allow secretions to drain while maintaining the airway Prevent injury during the seizure Remain with the client Do not restrain the client Loosen restrictive clothing Note the type, character, and progression of the movements during the seizure Monitor for incontinence Administer intravenous medications as prescribed to stop the seizure Document the characteristics of the seizure Provide privacy Monitor behavior following the seizure, such as the state of consciousness, motor ability, and speech ability Instruct the client about the importance of lifelong medication and the need for follow-up determination of medication blood levels STROKE (BRAIN ATTACK) Description A sudden focal neurological deficit and is caused by cerebrovascular disease Cerebral anoxia lasting longer than 10 minutes - Causes cerebral infarction with irreversible change Cerebral edema and congestion cause further dysfunction Diagnosis - CT scan - Electroencephalography - Cerebral arteriography NCMB 418 - MRI Transient ischemic attack (TIA) - A warning sign of an impending stroke The permanent disability cannot determined until cerebral edema subsides The order in which function may return - Facial - Swallowing - Lower limbs - Speech - Arms Carotid endarterectomy - Surgical intervention used in stroke management - Targeted at stroke prevention, especially in clients with symptomatic carotid stenosis Causes Ischemic stroke - Thrombosis - Embolism Hemorrhagic stroke - Rupture of a vessel Manifestations of different types of stroke are similar It is critical to determine the type of stroke occurring Type cannot be determined solely based on manifestations The correct and appropriate treatment for the stroke type must be initiated Risk Factors Atherosclerosis Hypertension Anticoagulation therapy Diabetes mellitus Stress Obesity Oral contraceptives A critical factor in the early intervention and treatment of stroke Accurate identification of stroke manifestations Establishing the onset of the manifestations Stroke screening scales may be used to identify stroke manifestations quickly. Identification of the type of stroke Critical in determining the appropriate treatment Done using a CT scan Clinical manifestations of stroke based on type: Assessment Depend on the area of the brain affected Lesions in the cerebral hemisphere result in manifestations on the contralateral side, which is the side of the body opposite the stroke Airway patency is always a priority Pulse (may be slow and bounding) Respirations (Chyne-Strokes) Blood pressure (hypertension) Headache, nausea, and vomiting Facial drooping Nuchal rigidity Visual changes Ataxia Dysarthria Dysphagia Speech changes Decreased sensation to pressure, heat, and cold Bowel and bladder dysfunctions Paralysis Aphasia Expressive - Damage occurs n Broca’s area of the frontal brain - The client understands what is said but is unable to communicate verbally Receptive - Injury involves Wernicke’s area in the temporoparietal area - The client is unable to understand the spoken and often the written word Global or mixed - Language dysfunction occurs in expression and receptions - 4 interventions for aphasia Provide repetitive directions Break tasks down to 1 step at a time Repeat names of objects frequently used NCMB 418 Allow time for the client communicate Use a Picture board Communication board Computer technology to Intervention: Acute Phase Maintain a patent airway and administer oxygen as prescribed Monitor VS Usually a BP of 150/100mmHg - Maintained to ensure cerebral perfusion Suction secretions - To prevent aspiration as prescribed - Never suction nasally or for longer than 10 seconds To prevent increased ICP Monitor for increased ICP - Most at risk during the first 72 hours following the stroke Position the client on the side to prevent aspiration, with HOB elevated 15-30 degrees as prescribed Monitor LOC, pupillary response, motor and sensory response, cranial nerve function, and reflexes Maintain a quiet environment Insert a urinary catheter as prescribed Administer IV as prescribed Maintain fluid and electrolyte balance Prepare to administer - Anticoagulants - Antiplatelet - Diuretics - Antihypertensive - Antiseizure medications as prescribed Intervention: Post-acute Phase Continue with interventions from the acute phase Position - 2 hours on the unaffected side - 20 minutes on the affected side - The prone position may also be prescribed Provide skin, mouth, and eye care Perform passive ROM exercises - To prevent contractures Place antiembolism stockings on the client - Remove daily to check skin Monitor the gag reflex and ability to swallow Provide sips of fluids and slowly advance diet to foods that are easy to chew and swallow Provide diet that is - Soft and semisoft foods - Flavored - Cool and warm - Thickened fluids Stroke client can tolerate these types of food better Eating position - In a chair or sitting up in bed - With the head and neck positioned slightly forward and flexed Place food in the back of the mouth on the unaffected side - To prevent trapping of food in the affected cheek. Intervention: Chronic Phase Neglect syndrome – the client is unaware of the existence of his or her paralyzed side (unilateral neglect), which places the client at - Risk for injury Teach the client to touch and use both sides of the body Hemianopsia - The client has blindness in half of the visual field. - Hemonymous hemianopsia – is blindness in the same visual field of both eyes - Encourage the client to turn the head to scan the complete range of vision; otherwise, he or she does not see half of the visual field Assess the need for assistive devices - Cane - Splint - Walker - Braces Teach transfer technique from bed to chair and from chair to bed Provide gait training Initiate physical and occupational therapy for assessment and the need for adaptive equipment or other supports for self-care and mobility Refer client to a speech and language pathologist as prescribed