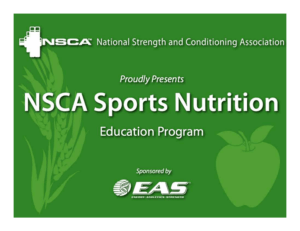
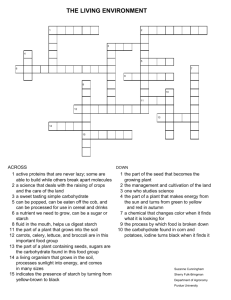
Chapter 3 Armstrong N, McManus AM (eds): The Elite Young Athlete. Med Sport Sci. Basel, Karger, 2011, vol 56, pp 47–58 Nutrition and Elite Young Athletes Asker Jeukendrupa ⭈ Linda Cronina,b a School of Sport and Exercise Sciences, University of Birmingham, Birmingham, bDepartment of Life Sciences, Roehampton University, London, UK Nutrition can play an essential role in the health of elite young athletes as well as exercise performance. Children and adolescents need adequate energy intake to ensure proper growth, development, and maturation. In addition, the requirements may further increase with increasing exercise training. There are, however, several metabolic differences that result in slightly different advice for young versus adult athletes. For example, younger athletes generally rely more on fat as a fuel, have smaller glycogen stores and have a limited glycolytic capacity. This would imply reduced carbohydrate requirements but a greater capacity to oxidize fat. There are also differences in thermoregulation, although the exact impact on fluid requirements is not clear. The limited evidence suggests that acute energy and fluid imbalances can be detrimental to performance and there may be benefits of ingesting carbohydrate and fluid during exercise, especially during more prolonged exercise. Exogenous carbohydrate oxidation rates have been reported to contribute more to energy expenditure in children. This may, however, simply be a reflection of the fact that the oxidation of this carbohydrate is not limited by body size, but by absorption. Absorption rates are likely to be similar in children and adults and therefore exogenous carbohydrate oxidation rates should be comparable. The relative contribution will therefore be higher because of the lower absolute intensities in children. There are a large number of questions still unanswered and sports nutrition advice to the elite young athlete is largely extrapolated from the adult population. Therefore, more research is needed in the years to come to give better advice to these young athletes. Copyright © 2011 S. Karger AG, Basel For many children and adolescents who are strongly committed to sport, nutrition is not on the radar. However, nutrition is a major component of their training. Nutrition interacts not only with growth and development, but also with recovery, performance, avoiding injury and problems that may arise as a result of deficiencies. Nutrition is important for both health and performance. This chapter addresses some of the main nutritional issues of young athletes and discusses nutrition for children from the age of 6 to 20 years. Where no evidence is available, information on young adults will be used. Energy Requirements The growth of pre-pubertal children (between 2 and 10 years) is linear and occurs at a relatively constant rate of 6 cm per year. The median heights and weights for boys and girls are similar, averaging 87 cm and 12 kg at the age of 2 years to 137 cm and 32 kg by the age of 10 years. Even in childhood, boys tend to have slightly greater lean tissue mass and a lower proportion of body fat than girls. Children and adolescents need adequate energy intake to ensure proper growth, development, and maturation. Dietary reference values (DRVs) have been established for various ages. The athletic or Downloaded by: Univ. of Michigan, Taubman Med.Lib. 141.213.236.110 - 7/22/2013 7:20:37 AM Abstract 48 expenditure and exercise economy disappear [3]. Thermoregulation in children has been discussed in more detail by Falk and Dotan [4]. It is important to educate children to eat a healthy and balanced diet and to encourage good eating habits. This can reinforce lifelong eating habits that contribute to the overall well-being of children and may enhance performance. On the other hand, any bad habits are difficult to get rid of later in a sporting career and should therefore be avoided. There is an important role for both coach and parents to encourage appropriate eating behaviours, but also to avoid bad habits such as too much attention to body weight (see section on weight management). Exercise Metabolism in Children The quality of the muscle – rather than the quantity – is a major determinant of substrate utilisation. Studies in adults clearly show a correlation between mitochondrial density of the muscle and fat metabolism (i.e. the more mitochondria, the higher fat oxidation rates during exercise). There also seems to be a correlation between muscle fibre type and substrate metabolism with higher percentage type I fibres favouring fat metabolism. For obvious reasons, very few studies have investigated muscle composition in children. However, a study by Bell et al. [5] found a similar mitochondrial to myofibrillar volume ratio in children and adults, indicating that with growth and maturation, increases in muscle mass are paralleled by an increase in mitochondria within these fibres. The maximal oxygen uptakes (V̇O2 max) of these children were similar to the V̇O2 max of an average adult (45 ml • kg–1 • min–1) and it was argued that the oxidative capacity of children could be further developed later in life when an endurance training programme was followed (or reduced when a sedentary lifestyle was adopted). In one study muscle fibre type composition was determined in a large number of 16-year-olds and reassessed 10 Jeukendrup · Cronin Downloaded by: Univ. of Michigan, Taubman Med.Lib. 141.213.236.110 - 7/22/2013 7:20:37 AM very active child or adolescent generally will have needs in excess of this level due to the greater energy expenditure from their higher levels of physical activity. It is difficult to establish a DRV for energy for this group because of very large inter-individual variability. In adolescents in particular the onset of the growth spurt, which is a major impetus for increased energy requirements, is unpredictable. Prolonged inadequate energy intake may result in short stature, delayed puberty, menstrual irregularities or absence, poor bone health and increased risk of injuries [1]. Certain categories of young athletes are more at risk for developing eating disorders like distance runners, jumpers and gymnasts. It is important to realise that it is impossible to derive estimations of energy expenditure for children based on adult data. It has repeatedly been demonstrated that children are less metabolically efficient during motor activities, resulting in higher energy requirements per kilogram body mass during activities. For example, one study reported that children require 30% more energy during running [2]. There may be several explanations for the higher energy expenditures. First, children have a higher resting metabolic rate, but they also have a disadvantageous stride frequency and stride length (imposed by shorter limbs). Traditionally, it has been stated that children’s lower mechanical efficiency would negatively affect the regulation of their body temperature, however this supposition was based upon studies that did not exercise children and adults at the same relative exercise intensity and so children were actually working at a higher exercise intensity than adults, consequently resulting in higher heat production. Similarly, the initial studies did not account for children’s shorter leg length (i.e. their higher stride frequency), nor account for how this would affect the metabolic cost of any exercise undertaken. However, if when comparing thermoregulation effects in children and adults relative exercise intensity is calculated by adjusting treadmill speed to stride frequency, the differences between adults’ and children’s energy Nutrition children seems to exist until mid- to late puberty, after which a more ‘adult-like metabolic profile’ seems to be evident [14]. It has been suggested that as fat metabolism appears to be more dominant in exercising children than in adults, children may possibly have a reduced requirement for dietary carbohydrates, particularly prepubescent children [12, 15]. Protein In order to support growth and development, children and adolescents have protein requirements that are relatively high compared to adults. The Recommended Daily Allowances (RDAs) for protein in the United States and Canada are displayed in table 1. However, the protein requirements for young elite athletes are likely to be higher. Boisseau et al. [16] studied protein requirements of 14-year-old soccer players, who played 10–12 h per week, using nitrogen balance measurements. The estimated daily protein needed to maintain nitrogen balance was 1.04 g • kg–1 • day–1. It was suggested that the RDA for protein for these young athletes was 1.40 g • kg–1 • day–1 (or 75 g • day–1 in this group), which would be well above the RDA for non-athletic children (52 g • day–1) [17]. However, as is the case with adult athletes [18] this requirement is quite easily met. The study in soccer players was performed in France and the suggested RDA of 1.40 g • kg–1 • day–1 is still well below the average protein intake by that age group in France (2.07 g • kg–1 • day–1). In the United States [19] and in Australia protein intake by children and adolescents are generally 2–3 times the RDA (USA) or recommendations in the United Kingdom (table 1) or Australia (not listed). Even in sports where elite young athletes were reported to restrict energy intakes, protein intakes were still between 1.5– 2.0 g • kg–1 • day–1 [1]. Although on the whole protein requirements seem to be no particular concern in young athletes, it is important to be aware that there may be individuals who, perhaps through a 49 Downloaded by: Univ. of Michigan, Taubman Med.Lib. 141.213.236.110 - 7/22/2013 7:20:37 AM years later when they were biopsied again to determine the muscle fibre type composition [6, 7]. It was concluded that fibre type did not change significantly (~52% type I fibres, 33% type IIA and 15% type IIX). Based on the limited information available it seems fair to conclude that there are no major shifts in muscle fibre type or composition with age, however, mitochondrial density can be increased with specific training. Even though the phenotypic characteristics of the muscle may be similar in children and adults, there do appear to be differences in substrate utilisation. These differences have been discussed in more detail elsewhere [8] but include a lower glycolytic capacity, a higher oxidative capacity and higher rates of fat oxidation. For more detailed reviews the reader is referred to Riddell [8] and Boisseau and Delamarche [9]. In brief, studies using indirect calorimetry suggest that the proportion of fatty acids to carbohydrates used for energy during exercise is different in children than in adults, possibly due to children’s smaller endogenous carbohydrate stores. In fact, the contribution of fatty acid oxidation towards energy production has been reported to be larger for both girls and boys than it is for adults [8, 10–12], suggesting that children are well equipped for sustained aerobic activity, but that their capacity for anaerobic performance may be limited by their maturation status [9, 13]. This difference, however, seems to diminish throughout adolescence, especially in boys [8, 14], suggesting that the hormones associated with puberty (i.e. growth hormone, insulin-like growth factor, sex steroids and catecholamines) play an influential role in controlling the regulation of energy metabolism in children [9]. In fact, pubertal development has long been associated with a period of insulin resistance and reduced insulin-stimulated glucose disposal at rest in pubescent children, when compared to pre-pubertal children and is probably caused by the conservation of carbohydrate stores for the energy requirements of growth. This difference in substrate utilisation in Table 1. Recommended protein intake for boys and girls versus typical intake in USA and Australia Gender and age Males Females Recommendations Examples of reported intake, g/day RDA USA and Canada g/kg/day RDA, g/day 1–3 years 1.05 13 4–8 years 0.95 19 20 (4–6 years) 66 64 9-13 years 0.95 34 28-41 (7–10 years, 11–14 years) 81 75 14–18 years 0. 85 52 45 (14–16 years) 97 120 19–30 years 0.80 56 56 1–3 years 1.05 13 4–8 years 0.95 19 20 (4–6 years) 66 64 9–13 years 0.95 34 28–41 (7–10 years, 11–14 years) 68 75 14–18 years 0.85 46 45 (14–16 years) 68 80 19–30 years 0.80 46 45 72 GDA, UK g/day P intake in USA P intake in AUS 55 109 55 combination of energy restriction and a vegetarian diet, have a very low protein intake. Carbohydrates It has been shown that carbohydrate ingestion in adults both before and during exercise can delay fatigue and improve endurance performance. Unlike protein which has a quite general recommendation, recommendations for carbohydrate intake highly depend on the intensity, type and 50 duration of exercise that is performed by young athletes. Carbohydrate loading is a technique that is often used by adult athletes to maximize muscle glycogen stores and enhance endurance exercise performance. Glycogen loading is not advised for children [22] but since most events will be shorter and glycolytic capacity is limited, it must be questioned whether such a strategy would be beneficial at all. A relatively high carbohydrate diet is advised but there is probably no need to follow a dedicated glycogen loading regimen. Jeukendrup · Cronin Downloaded by: Univ. of Michigan, Taubman Med.Lib. 141.213.236.110 - 7/22/2013 7:20:37 AM These data show that recommendations are exceeded and, at least at the group level, protein intake is more than adequate. RDA data derived from Dietary Reference Intakes (DRIs): Recommended Intakes for Individuals, Macronutrients. Food and Nutrition Board, Institute of Medicine, National Academies, 2005 [17] and Working Group Report. Guideline Daily Amounts (GDA) derived from report of the IGD/PIC Industry Nutrition Strategy Group Technical Working Group on Guideline Daily Amounts (GDAs). Watford, UK. IGD, 2005 [20]. Intake data from references [19] USA and [21] Australia. Nutrition aged 13–19 years periodically drank a carbohydrate drink (2% glucose and 4% sucrose), whilst completing a cycle test at 60% V̇O2 max, their subjective rating of exercise intensity was significantly decreased by 1–2 points (RPE scale). Beneficial effects of carbohydrate ingestion on subjective ratings of perceived exertion have been reported in healthy adults too, although interestingly in the boys the effect occurred after just 60 min of moderate intensity cycling, rather than after 90–120 min, commonly reported in adult studies. This effect occurring earlier in children could be due to be the result of smaller carbohydrate stores in children and therefore their earlier reliance on exogenous carbohydrate. It must be noted, however, that this finding was not reproduced in a more recent study, where ingestion of a 6% carbohydrate-electrolyte solution was found to have no effect on RPE in boys during a 60 min cycling test at ~70% peak V̇O2 [12]. It has been suggested that the ingestion of carbohydrates may alter the substrates used by exercising children. Indeed, Riddell et al. [33] reported that the ingestion of a 13C-labeled glucose solution induced a sparing of endogenous glucose utilization in boys (from 68 to 59% of total energy utilization) and decreased fat utilization (from 32 to 18% of total energy expended). Furthermore, subsequent studies have also reported that children appear to oxidize relatively more exogenous carbohydrate during exercise than do adults [11, 12], despite their lower whole body rate of carbohydrate oxidation and much higher rate of fat oxidation. In fact, one study looking at the effect of pubertal status and age on exogenous carbohydrate oxidation reported that exogenous carbohydrate oxidation contributed to ~30% of the total energy expenditure in the pre-pubertal and early pubertal boys, compared to only ~24% in the mid-to-late pubertal boys. It was suggested that the reliance on exogenous carbohydrate oxidation during exercise is sensitive to pubertal status, rather than just chronological age [12]. 51 Downloaded by: Univ. of Michigan, Taubman Med.Lib. 141.213.236.110 - 7/22/2013 7:20:37 AM During exercise in adults carbohydrates can help by maintaining high rates of total carbohydrate oxidation, sparing endogenous muscle glycogen stores and maintaining blood glucose concentrations, particularly in the later stages of exercise [for reviews, see 23, 24]. In addition to these metabolic effects there is also evidence to suggest that carbohydrates may affect central drive (or motivation) too, possibly via oral carbohydrate receptors [25–27]. In contrast, neither glucose consumption before [28] or during [11] exercise has been reported to improve performance time in male adolescents. In fact, in a study by Riddell et al. [11], twelve 10to 14-year-old boys intermittently drank either water or a 6% glucose drink whilst undertaking 90 min of cycling at 55% peak V̇O2, followed by an all-out performance ride to volitional exhaustion at 90% peak power. Although there was a trend for the glucose solution to improve performance time (occurring in seven of the 12 boys), this finding was not consistent and no significant differences were found in performance between the two drinks (water session: 142 ± 37 s vs. glucose: 177 ± 33 s). Interestingly though, the same study showed that drinking a 3% glucose plus 3% fructose solution did result in cycling time significantly improving by ~40% (202 ± 40 s). Although this finding of an improved performance with a glucose plus fructose drink has also been reported in adult studies [29], the mechanisms may be very different, as the amounts of carbohydrate ingested in these studies were much larger and the exercise duration longer. In addition to enhancing exercise performance in endurance exercise, carbohydrate ingestion has also been shown to increase performance in intermittent, high-intensity exercise [30] and increase explosive strength and speed, as well as shooting skill performance [31] in a basketball skill test. Furthermore, the subjective rating of perceived exertion (RPE) may also be influenced by carbohydrate ingestion. In another study by Riddell et al. [32], it was reported that when healthy boys 52 maturation dependent decline in muscle glucose uptake has also been reported [39]. Alternatively the increased reliance on exogenous carbohydrate oxidation could be because the ability of exercising muscle to catabolise endogenous glycogen as an energy substrate is less in boys than in men [40]. Interestingly though, this same pubertal effect has not been found in girls [34]. Carbohydrate intake during exercise has been linked with improved performance, but also with increases in gastrointestinal symptoms. When 18 adolescents undertook intermittent high-intensity exercise for 48 min (treadmill sprinting, lateral hops and shuttle run), ingestion of an 8% CHO drink caused a higher rating of gastrointestinal discomfort (stomach upset and side ache) than ingestion of a 6% drink [41]. The use of carbohydrate drinks during such short duration and highintensity activities should be questioned anyway as it is unlikely to give any metabolic advantage. To date, there have been no studies investigating either the performance effects of carbohydrate or the rate of carbohydrate oxidation in highly trained elite young athletes. Due to this dearth of information, we have relied upon studies undertaken on healthy active boys and girls to inform this section; however, as it is known that both insulin sensitivity and substrate utilization during exercise are affected by training, it is possible that the outcomes of such studies on elite young athletes could differ from those obtained on active children. Also, the exercise capacity and the absolute intensities these athletes would exercise at are higher than their untrained counterparts and it is therefore more likely that their metabolism will behave more like that of older children. Fat Very few studies have investigated fat intake or fat requirements in active children. Although certain fats are important for growth and development, the Jeukendrup · Cronin Downloaded by: Univ. of Michigan, Taubman Med.Lib. 141.213.236.110 - 7/22/2013 7:20:37 AM Timmons et al. [34] have suggested that this higher rate of carbohydrate oxidation may be due to an increased recruitment and rate of translocation of insulin-sensitive GLUT4 glucose protein transporters to the muscle membrane cell, resulting in a higher glucose uptake in exercising children. However, there may be another explanation that is much simpler. In adult studies, it has clearly been demonstrated that exogenous carbohydrate oxidation is limited by absorption rather than a muscle phenomenon [23, 24, 35]. The delivery of carbohydrate to the muscle is the rate-limiting step, not the oxidation in the muscle itself [for reviews, see 23, 24, 35]. It is not unlikely that in children the same limitation applies. It has been found that in children under the age of 5 years, the efficiency of carbohydrate absorption is lower than in adults, but this gradually increases with age until the fifth year. The rate of absorption also varies depending upon the ratio of glucose to fructose in the drink [36]. Although there is limited information regarding the rate of intestinal absorption of carbohydrates in exercising conditions in children, some studies comparing oral 13C-bicarbonate dynamics between children and adults have suggested no differences between children and adults in the absorption of the tracer either at rest [37] or during exercise [38]. If there are indeed no differences in carbohydrate absorption between children and adults, this would provide an explanation for many of the findings in previous studies. Similar absorption rates in children and adults would result in similar exogenous carbohydrate oxidation (in g • min–1). Because adults exercise at a higher exercise intensity and energy expenditure is greater, the same exogenous carbohydrate oxidation results in a smaller contribution to energy expenditure. In contrast exogenous carbohydrate oxidation in children will contribute more to energy expenditure. With the current limited evidence, it is impossible to definitively determine what the mechanism is. A muscle phenomenon cannot be excluded, however, because in growing rats a Thermoregulation and Fluid Requirements One of the main ways that humans lose heat is through the evaporation of sweat and the associated convection of body heat away from the surface of the skin. As children have a higher ratio of body surface area to body mass [43] (at the age of 8 years it is approximately 50% higher than that of an adult) it has been suggested that exercising children should be able to dissipate heat quicker than adults, giving their thermal homeostasis an advantage over that of exercising adults, at least up to the point at which ambient temperature exceeds skin temperature, after which this advantage is supposedly reversed. In practice, however, this has not been found to be the case and instead adults and active children seem to experience similar core temperatures, even when exercising at high temperatures [44]. Whether the same finding would occur in elite young athletes, as compared to these active but not competitive children, is yet to be determined. Heat loss through the evaporation of sweat can result in large fluid and electrolyte losses. In adults, the dehydration caused by this fluid loss has been shown to be detrimental to motor Nutrition control and physical performance [45], so adults are advised to balance any fluids lost from sweating, with fluid intake. However, there are large differences in sweat rates between children and adults. In fact, when investigated in boys aged 9 years in hot and humid conditions (45°C and 97% relative humidity), it was reported that their sweat rate was only half that of men. This muted response, which also is similar to that seen in both young girls and adult females, is probably due to the underdevelopment of the peripheral sweating mechanism in younger boys. In fact once the circulating levels of the male sex hormones start to increase during puberty, the sweat rate is seen to increase rapidly. It seems tempting to conclude that if the young athlete’s ability to sweat is reduced, particularly before puberty, then their risk of developing sweat induced dehydration will also be reduced. However, as sweating is the main way of dissipating heat during exercise, it is possible that children’s core body temperature could increase at a more rapid rate than an adult’s. Ultimately, however, it seems that the reduced sweat rate does not impair children’s heat loss during exercise [44]. Instead, it seems that children utilize different, but just as effective, thermoregulatory mechanisms [44, 46–47] (see Falk and Dotan [4] for a more in-depth discussion). Therefore, as dehydration levels and more importantly the risk of developing a heat-related illness seem to be similar between adults and younger athletes, then the recommendation regarding fluid replacement is likely to be similar too. Young athletes underestimate the amount of fluid they need to consume during prolonged exercise in order to stay hydrated, especially in hot and humid conditions and in particular when the fluid available to them is water. As thirst is often reported to be a poor indicator of fluid needs, it is important to encourage drinking before, during and after exercise to prevent dehydration. Previous research has shown that involuntary hypohydration can reach up to 1–2% in both unacclimatised, 53 Downloaded by: Univ. of Michigan, Taubman Med.Lib. 141.213.236.110 - 7/22/2013 7:20:37 AM link with performance is far less clear. Although it is often recommended that 25–30% of energy should come from dietary fat, such recommendations for total fat intake are highly dependent on the energy expenditure. As in adults first priorities are adequate protein and carbohydrate intake and fat can make up for the remaining energy. Restricting fat intake in non-obese children has been suggested to impair growth and development, although it is not clear whether this is a direct effect of low fat intake or low energy [42]. If weight loss is required in children who are involved in relatively hard physical training, it seems sensible to reduce the fat intake rather than protein or carbohydrate (see also the section on weight management below). 54 in the heat state that a child who weighs 40 kg should drink 150 ml of cold water or flavoured salted beverage every 20 min and an adolescent who weighs 60 kg should drink 250 ml, even if the child does not feel thirsty. Such guidelines, however, are very general and do not take into account environmental conditions, exercise intensity, acclimatisation and individual differences. With a lack of studies showing the effects of dehydration in children and the impact on performance, it is very difficult to give balanced and objective guidelines. At an elite level, it seems sensible to develop an individual strategy that aims to reduce fluid losses in excess of 3% body mass. This can be done by measuring body weights before and after training and correcting them for fluid intake to obtain some measure of sweat rates. This would eventually allow the prediction of sweat rates in similar conditions. Nutrition Supplements Supplement use amongst junior athletes is common. In a study of 32 track and field junior athletes selected for Team Great Britain at the World Junior Championships, it was found that 62% of the sample used supplements [55]. Females (75%) were found to use more supplements than males (55%), although this difference was not statistically significant. This trend may be attributed to a greater awareness among females, greater genuine need for supplementation (e.g. menstrual loss) or advertising campaigns having a greater influence on females [55]. The most commonly used supplements were multivitamins, followed by vitamin C and iron [55]. In a review, McDowall [56] concluded that the prevalence of supplement use was between 22 and 71% in young athletes (age ranges from 13 to 19 years). The most frequently cited reasons for using a supplement were: health benefits, illness prevention, enhancing performance, taste, rectifying a perceived poor diet and increasing energy [57]. Jeukendrup · Cronin Downloaded by: Univ. of Michigan, Taubman Med.Lib. 141.213.236.110 - 7/22/2013 7:20:37 AM untrained [48] as well as acclimatised, trained [49] boys. Whilst education for parents, coaches, teachers and indeed young athletes themselves can improve fluid intake in elite young athletes, research has also shown that there are other ways to enhance thirst and therefore stimulate drinking. One of these is through the addition of small amounts of sodium chloride to water, as this sensitises the thirst mechanism through the maintenance of plasma osmolality and reduces the diuretic effect of water [13, 49, 50], whilst also replacing lost electrolytes. Another way is through the addition of carbohydrate to the drink, as this increases the palatability of the solution [51]. Finally, the addition of flavour is another important way to promote increased re-hydration. In fact, RiveraBrown and colleagues [49] reported that in heat acclimatised, trained boys the addition of flavour to a carbohydrate-electrolyte drink helped to reduce voluntary dehydration by 32%, which was enough to maintain euhydration over a 3-hour period of intermittent cycling exercise (at 60% V̇O2 max) in 30°C heat (53–62% relative humidity). Further, Meyer et al. [52] compared water and different flavoured drinks in exercising Canadian children and found that children preferred grapeand orange-flavoured drinks to apple-flavoured drinks and water. It is likely, however, that these findings are heavily influenced by cultural factors and that different preferences would occur in different areas and countries. Current recommendations for fluid replacement in children are scant. The 2007 American College of Sports Medicine (ACSM) position statement on ‘Exercise and Fluid Replacement’ barely refers to children’s needs, only referring to the fact that pre-pubescent children have a lower sweat rate than adults [53], whilst the 2009 ACSM position statement on ‘Nutrition and Athletic Performance’ does not comment upon children’s or adolescents’ needs at all. In contrast, the policy statement re-issued in 2000 by the American Academy of Pediatrics [54], regarding the fluid replacement guidelines for children during exercise Nutrition Regardless of whether supplements have the effects they are claimed to have, it is clear that young elite athletes have a perceived need for nutritional supplementation. However, there must be reservations to even the most commonly used supplements regarding long term use, combinations and appropriate dosages in an elite young athlete. These reservations concern: (1) an increased health risk to an otherwise healthy population, and (2) the possibility of positive doping tests caused by supplements containing banned substances [61]. To minimise potential health risks arising from potentially inappropriate supplement use, an increased involvement of health professionals, with appropriate training, is desirable. Although we do not want to engage in detailed discussions of a long list of supplements, one supplement has received substantial attention recently. Caffeine is one of the most widely used drugs and energy drinks containing caffeine are now marketed specifically to young adults and children. It is therefore important to understand the effects of caffeine in this population. Energy drinks containing high concentrations of sugars and caffeine represent the fastest growing segment of the beverage industry. Very few studies have examined the physiological and psychological effects of caffeine and therefore it is difficult to give sound advice on caffeine use for young athletes. However, there is evidence that children and adolescents, although receiving similar benefits, may be particularly vulnerable to the negative effects of caffeine. Therefore, caffeine should be used with caution. In general, supplements for younger athletes are not recommended [22]. Weight Management and Dangers Perhaps one of the greatest threats to child health is inappropriate weight control in young athletes. If a reduction in body mass is desired, this should be done gradually and not more than 1.5% of 55 Downloaded by: Univ. of Michigan, Taubman Med.Lib. 141.213.236.110 - 7/22/2013 7:20:37 AM In a recent study amongst elite young UK athletes (mean age 17.7 years), supplement use was investigated [58]. Of the 1,674 questionnaires distributed, 412 were returned and 403 were within the age range required. Single supplement use was reported by 48.1%. The most popular supplements were sports drinks consumed by 41.7% of all athletes and 86.6% of the supplement users. Other popular supplements included vitamin C (22.8%), multivitamins (22.8%), whey protein (21.3%) and creatinine (13.4%). Echinacea (7.7%), caffeine (5.7%), iron (4.7%), ginseng (1.7%) and melatonin (1.0%) were amongst the most often reported supplements. Among the desired outcomes resulting from supplement use, maintaining strength was the most frequently cited reason among all athletes in the sample (34.7%) and supplement users (72.2%), followed by avoiding sickness (56.1% of users) and endurance enhancement (55.2% of users). One-third of the supplement user athletes listed the ability to train longer (30.4%) and helping to recover (32.5%) among the reasons, whereas 23.2% take supplements to remedy imbalanced diet. A difference noted between this study and a similar survey in elite adult athletes [59, 60] was that the reasons for supplement use were mostly performance based. The younger elite athletes seemed to appear less ‘health conscious’ and more ‘performance focused’ than their adult counterparts. The source of the advice varied and was different for different supplements. Interestingly, many young athletes appeared to decide on their nutritional supplementation themselves without advice. There was, however, considerable overlap between self-managed supplementation and medical advice. The coaches’ role in advising athletes on supplements, especially in taking energy drinks and protein was also evidenced. Among health professionals, athletes indicated that advice was sought from nutritionists and/or physiotherapists. The only exception was iron supplementation, which was taken following the general practitioners’ advice. body mass per week [62]. A more rapid weight loss may result in muscle protein breakdown, and this may interfere with growth and development. To lose half a kg of fat in 1 week, one must expend 14,700 kJ (3,500 kcal) more than one consumes. It is often suggested that the preferred way to do this is to consume 7,350 kJ (1,750 kcal) fewer per week and expend 7,350 kJ (1,750 kcal) more per week by exercising. When possible, the athlete should be counselled by a registered dietician who has experience of working with athletes and their families. A lean and light physique is often desired in certain sports, especially endurance sports such as distance running and aesthetic sports such as gymnastics. Although in some cases there are clear links to better performance it is important to be aware that there are also risks of energy deficiency, micronutrient deficiencies, menstrual irregularity, poor bone health and eating disorders. These issues are reviewed in more detail in an excellent review by Manore et al. [63]. Conclusions Children and adolescents need adequate energy intake to ensure proper growth, development, and maturation, but also to ensure optimal exercise performance. There are several metabolic differences between young and adult athletes. Younger athletes generally rely more on fat as a fuel, have smaller glycogen stores and have a limited glycolytic capacity. Glycogen loading is not advised and there is limited evidence that carbohydrate intake during prolonged exercise can be beneficial. There are differences in thermoregulation, but the impact on fluid requirements is not clear. The limited evidence suggests that acute energy and fluid imbalances can be detrimental to performance and there may be benefits of ingesting carbohydrate and fluid during exercise, especially during more prolonged exercise. Rapid weight loss and too much focus on weight in children can pose a health risk. Supplements are not recommended for children. References 56 6 Glenmark B, Hedberg G, Kaijser L, Jansson E: Muscle strength from adolescence to adulthood–relationship to muscle fibre types. Eur J Appl Physiol Occup Physiol 1994;68:9–19. 7 Glenmark B: Skeletal muscle fibre types, physical performance, physical activity and attitude to physical activity in women and men: a follow-up from age 16 to 27. Acta Physiol Scand Suppl 1994;623:1–47. 8 Riddell MC: The endocrine response and substrate utilization during exercise in children and adolescents. J Appl Physiol 2008;105:725–733. 9 Boisseau N, Delamarche P: Metabolic and hormonal responses to exercise in children and adolescents. Sports Med 2000;30:405–422. 10 Martinez LR, Haymes EM: Substrate utilization during treadmill running in prepubertal girls and women. Med Sci Sports Exerc 1992;24:975–983. 11 Riddell MC, Bar-Or O, Wilk B, Parolin ML, Heigenhauser GJ: Substrate utilization during exercise with glucose and glucose plus fructose ingestion in boys ages 10–14 yr. J Appl Physiol 2001;90:903–911. 12 Timmons BW, Bar-Or O, Riddell MC: Oxidation rate of exogenous carbohydrate during exercise is higher in boys than in men. J Appl Physiol 2003;94:278–284. 13 Bar-Or O: Nutritional Considerations for the child athlete. Can J Appl Physiol 2001;26(suppl):S186–S191. 14 Stephens BR, Cole AS, Mahon AD: The influence of biological maturation on fat and carbohydrate metabolism during exercise in males. Int J Sport Nutr Exerc Metab 2006;16:166–179. Jeukendrup · Cronin Downloaded by: Univ. of Michigan, Taubman Med.Lib. 141.213.236.110 - 7/22/2013 7:20:37 AM 1 Bass S, Inge K: Nutrition for special populations: children and young athletes; in Burke LM, Deakin V (eds): Clinical Sports Nutrition. Sydney, McGraw-Hill, 2006, pp 589–632. 2 Krahenbuhl GS, Williams TJ: Running economy: changes with age during childhood and adolescence. Med Sci Sports Exerc 1992;24:462–466. 3 Maliszewski AF, Freedson PS: Is running economy different between children and adults? Pediatr Exerc Sci 1996;8:351– 360. 4 Falk B, Dotan R: Temperature regulation and elite young athletes; in Armstrong N, McManus AM (eds): The Elite Young Athlete. Med Sport Sci. Basel, Karger, 2011, vol 56, pp 126–149. 5 Bell RD, Macdougall JD, Billeter R, Howald H: Muscle-fiber types and morphometric analysis of skeletal-muscle in 6-year-old children. Med Sci Sports Exerc 1980;12:28–31. Nutrition 27 Jeukendrup AE, Chambers ES: Oral carbohydrate sensing and exercise performance. Curr Opinion Clin Nutr Metab Care 2010;13:447–451. 28 Hendelman DL, Ornstein K, Debold EP, Volpe SL, Freedson PS: Preexercise feeding in untrained adolescent boys does not affect responses to endurance exercise or performance. Int J Sport Nutr 1997;7:207–218. 29 Currell K, Jeukendrup A: Superior performance with ingestion of multiple transportable carbohydrates. Med Sci Sports Exerc 2008;40:275–281. 30 Horswill C, Curby D, Bartola W, Stofan J, Murria R: Effect of carbohydrate intake during wrestling practice on upper-body work in adolescents. Pediatr Exerc Sci 2006;18:470–482. 31 Dougherty KA, Baker LB, Chow M, Kenney WL: Two percent dehydration impairs and six percent carbohydrate drink improves boys basketball skills. Med Sci Sports Exerc 2006;38:1650– 1658. 32 Riddell MC, Bar-Or O, Gerstein HC, Heigenhauser GJ: Perceived exertion with glucose ingestion in adolescent males with IDDM. Med Sci Sports Exerc 2000;32:167–173. 33 Riddell MC, Bar-Or O, Schwarcz HP, Heigenhauser GJ: Substrate utilization in boys during exercise with [13C]glucose ingestion. Eur J Appl Physiol 2000;83:441–448. 34 Timmons BW, Bar-Or O, Riddell MC: Energy substrate utilization during prolonged exercise with and without carbohydrate intake in preadolescent and adolescent girls. J Appl Physiol 2007;103:995–1000. 35 Jeukendrup AE: Carbohydrate and exercise performance: the role of multiple transportable carbohydrates. Curr Opinion Clin Nutr Metab Care 2010;in press. 36 Nobigrot T, Chasalow FI, Lifshitz F: Carbohydrate absorption from one serving of fruit juice in young children: age and carbohydrate composition effects. J Am Coll Nutr 1997;16:152–158. 37 Armon Y, Cooper DM, Springer C, Barstow TJ, Rahimizadeh H, Landaw E, Epstein S: Oral [13C]bicarbonate measurement of CO2 stores and dynamics in children and adults. J Appl Physiol 1990;69:1754–1760. 38 Zanconato S, Cooper DM, Barstow TJ, Landaw E: 13CO2 washout dynamics during intermittent exercise in children and adults. J Appl Physiol 1992;73:2476– 2482. 39 Dolan PL, Boyd SG, Dohm GL: Differential effect of maturation on insulin- vs. contraction-stimulated glucose transport in Zucker rats. Am J Physiol 1995;268:E1154–E1160. 40 Zanker C: Sport nutrition in childhood: meeting the metabolic demands of growth and exercise. Ann Nestlé 2006;64:63–76. 41 Shi X, Horn MK, Osterberg KL, Stofan JR, Zachwiega JJ, Horswill CA, Passe DH: Gastrointestinal discomfort during intermittent high-intensity exercise: effect of carbohydrate-electrolyte beverage. Int J Sport Nutr Exerc Metab 2004;14:673–683. 42 Butte NF: Fat intake of children in relation to energy requirements. Am J Clin Nutr 2000;72:1246S–1252S. 43 Rowland T: Children’s Exercise Physiology. Champaign, Human Kinetics, 2005. 44 Inbar O, Morris N, Epstein Y, Gass G: Comparison of thermoregulatory responses to exercise in dry heat among prepubertal boys, young adults and older males. Exp Physiol 2004;89:691–700. 45 Armstrong LE, Costill DL, Fink WJ: Influence of diuretic-induced dehydration on competitive running performance. Med Sci Sports Exerc 1985;17:456–461. 46 Rowland T: Thermoregulation during exercise in the heat in children: old concepts revisited. J Appl Physiol 2008;105:718–724. 47 Falk B, Dotan R: Children’s thermoregulation during exercise in the heat: a revisit. Appl Physiol Nutr Metab 2008;33:420–427. 48 Wilk B, Bar-Or O: Effect of drink flavor and NaCl on voluntary drinking and hydration in boys exercising in the heat. J Appl Physiol 1996;80:1112–1117. 49 Rivera-Brown AM, Gutierrez R, Gutierrez JC, Frontera WR, Bar-Or O: Drink composition, voluntary drinking, and fluid balance in exercising, trained, heat-acclimatized boys. J Appl Physiol 1999;86:78–84. 50 Manore MM: Effect of physical activity on thiamine, riboflavin, and vitamin B6 requirements. Am J Clin Nutr 2000;72:598S–606S. 57 Downloaded by: Univ. of Michigan, Taubman Med.Lib. 141.213.236.110 - 7/22/2013 7:20:37 AM 15 Foricher JM, Ville N, Gratas-Delamarche P: Effects of submaximal intensity cycle ergometry for one hour on substrate utilization in trained prepubertal boys versus trained adults. J Sports Med Physical Fit 2003;43:36–43. 16 Boisseau N, Vermorel M, Rance M, Duche P, Patureau-Mirand P: Protein requirements in male adolescent soccer players. Eur J Appl Physiol 2007;100:27– 33. 17 Dietary Reference Intakes (DRIs): Recommended intakes for individuals, Macronutrients; in: Medicine, ed 1. Washington, Food and Nutrition Board, Institute of Medicine, National Academies, 2005. 18 Tipton KD, Witard OC: Protein requirements and recommendations for athletes: relevance of ivory tower arguments for practical recommendations. Clin Sports Med 2007;26:17–36. 19 Fulgoni VL 3rd: Current protein intake in America: Analysis of the National Health and Nutrition Examination Survey, 2003–2004. Am J Clin Nutr 2008;87:1554S–1557S. 20 IGD: Working Group Report. Guideline Daily Amounts (GDA) derived from report of the IGD/PIC Industry Nutrition Strategy Group Technical Working Group on Guideline Daily Amounts (GDAs), Watford, 2005. 21 McLellan W, Podger A: National Nutrition Survey, selected highlights, Australia 1995. Canberra, Australian Bureau of Statistics and the Department of Health and Family Services, 1997. 22 Meyer F, O’Connor H, Shirreffs SM: Nutrition for the young athlete. J Sports Sci 2007;25(suppl 1):S73–S82. 23 Jeukendrup A: Carbohydrate feeding during exercise. Eur J Sport Sci 2008;8:77–86. 24 Jeukendrup AE: Carbohydrate intake during exercise and performance. Nutrition 2004;20:669–677. 25 Carter JM, Jeukendrup AE, Jones DA: The effect of carbohydrate mouth rinse on 1-h cycle time trial performance. Med Sci Sports Exerc 2004;36:2107– 2111. 26 Chambers ES, Bridge MW, Jones DA: Carbohydrate sensing in the human mouth: effects on exercise performance and brain activity. J Physiol 2009;587:1779–1794. 55 Nieper A: Nutritional supplement practices in UK junior national track and field athletes. Br J Sports Med 2005;39:645–649. 56 McDowall JA: Supplement use by young athletes. J Sports Sci Med 2007;6:337– 342. 57 O’Dea JA: Consumption of nutritional supplements among adolescents: usage and perceived benefits. Health Educ Res 2003;18:98–107. 58 Petroczi A, Naughton DP, Pearce G, Bailey R, Bloodworth A, McNamee M: Nutritional supplement use by elite young UK athletes: fallacies of advice regarding efficacy. J Int Soc Sports Nutr 2008;5:22. 59 Petroczi A, Naughton DP, Mazanov J, Holloway A, Bingham J: Performance enhancement with supplements: incongruence between rationale and practice. J Int Soc Sports Nutr 2007;4:19. 60 Petroczi A, Naughton DP, Mazanov J, Holloway A, Bingham J: Limited agreement exists between rationale and practice in athletes’ supplement use for maintenance of health: a retrospective study. Nutr J 2007;6:34. 61 Geyer H, Parr MK, Koehler K, Mareck U, Schanzer W, Thevis M: Nutritional supplements cross-contaminated and faked with doping substances. J Mass Spectrom 2008;43:892–902. 62 Promotion of healthy weight control practices in young athletes. Pediatrics 2005;116:1557–1564. 63 Manore MM, Kam LC, Loucks AB: The female athlete triad: components, nutrition issues, and health consequences. J Sports Sci 2007;25(suppl 1):S61–S71. Prof. A.E. Jeukendrup School of Sport and Exercise Sciences University of Birmingham Birmingham B15 2TT (UK) Tel. +44 0 121 414 4124, Fax +44 0 121 414 4121, E-Mail A.E.Jeukendrup@bham.ac.uk 58 Jeukendrup · Cronin Downloaded by: Univ. of Michigan, Taubman Med.Lib. 141.213.236.110 - 7/22/2013 7:20:37 AM 51 Shi X, Summers R, Schedl H, Flanagan S, Chang R, Gisolfi C: Effects of carbohydrate type and concentration and solution osmolality on water absorption. Med Sci Sports Exerc 1995;27:1607– 1615. 52 Meyer F, Bar-Or O, Salsberg A, Passe D: Hypohydration during exercise in children: effect on thirst, drink preferences, and rehydration. Int J Sport Nutr 1994;4:22–35. 53 Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ, Stachenfeld NS: American College of Sports Medicine position stand: exercise and fluid replacement. Med Sci Sports Exerc 2007;39:377–390. 54 Climatic heat stress and the exercising child and adolescent. American Academy of Pediatrics Committee on Sports Medicine and Fitness. Pediatrics 2000;106:158–159.