Urinary System Study Guide: Anatomy, Function, and Problems
advertisement

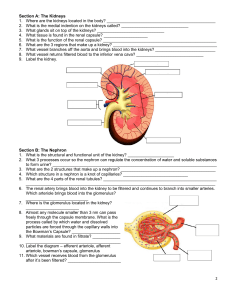
Urinary System (US) Introduction 1. What are the 5 functions of the US? 2. What 4 parts of the US ? 3. What is the function of the kidneys? The ureters? The bladder? The urethra? Kidneys 4. 5. 6. 7. 8. Where are the kidneys located? What does retroperitoneal mean? What do you call the big indent on the medial side of the kidney? What is its entrance called? What enters the kidney here? Arrange the following in order Major calyx (MJC) Minor calyx (MNC) Renal papilla (RPP) Renal pyramid (RPY) Renal pelvis (RPL) 9. What are the 2 regions of the kidney? Which houses the renal pyramids? The renal columns? 10. What are the 3 things the kidneys do to maintain homeostasis? 11. How do they accomplish their tasks? 12. What are 3 other functions the kidneys perform, not relating to the formation of urine? 13. What arteries supply blood to the kidneys? 14. Where does it enter the kidney? 15. Arrange the following in order of entering the kidney Arcuate arteries (AA) Afferent arterioles (AFA) Collecting duct (CD) Interlobar arteries (IA) Inferior vena cava (IVC) Interlobular arteries (ILA) Nephron (N) Papilla (P) Renal artery (RA) Renal vein (RV) 16. How many nephrons are in a kidney? 17. What are the 2 main parts of a nephron? 18. Arrange the following nephron structures in order as urine is formed. Ascending loop of Henle (ALH) Collecting duct (CD) Descending loop of Henle (DLH) Distal convoluted tubule (DCT) Glomerulus (G) Glomerular/Bowmans capsule (GC) Mino0r calyx (MC) Proximal convoluted tubule (PCT) Renal papilla (RP) 19. Some blood does not enter the Bowman’s capsule from the glomerulus. Through what blood vessel does that blood go? 20. What is it about that blood vessel that causes the high pressure back in the glomerulus? 21. What blood vessel does the blood flow into from the blood vessel in #19? 22. The juxtaglomerular apparatus (JGA) is comprised of cells from what 3 sources? 23. What is the function of the JGA? Urine formation 24. Arrange the following processes in order of use in urine formation Glomerular filtration (GF) Tubular reabsorption (TR) Tubular secretion (TS) 25. How is glomerular filtration different from the filtration that occurs at other capillary sites? 26. What is the purpose of tubular reabsorption? Secretion?. 27. What is the final product of the 3 processes? 28. Why are glomerular capillaries more permeable than other capillaries? 29. What force causes the movement of filtrate out of the glomerular capillaries? 30. In what direction (increase or decrease) would high blood pressure affect the amount of urine formed? Why? 31. How much does the glomerulus filter in 24 hours? 32. How does your US respond to maintain blood pressure homeostasis when blood pressure drops? 33. Why would the JGA cells secrete rennin 34. What does rennin react with in the blood? 35. Arrange the following order of activation Aldosterone (AL) Angiotensinogen (A) Angiotensin I (AI) Angiotensin II (A2) Renin (R) 36. What 2 actions does angiotensin II perform to help maintain blood pressure? 37. What role can the heart play in regulating blood pressure? 38. What is the function of tubular reabsorption? 39. Tubular reabsorption involves substances from _____ moving into _____. 40. Some water is reabsorbed by the passive process of osmosis. The active transport of sodium ions results in more water being reabsorbed. Arrange the following steps in the reabsorption of water a. Negative ions are attracted to the positive ions b. Osmotic pressure increase in the plasma c. Positive sodium ions are actively transported out of the filtrate back into the blood d. Water moves from a lesser solute region to a higher one 41. What % of blood does not get filtered by the glomerulus? 42. How does the body use tubular secretion to maintain body pH? 43. In what part of the nephron does most tubulat secretion take place? 44. What 2 hormones are used to maintain fluid balance by the kidney? 45. How does aldosterone affect water movement in the nephron? 46. Arrange the following activities relating to ADH a. ADH travels to the kidneys b. Amount of urine decreases c. Amount of water in blood decreases d. Hypothalamus signals pituitary e. Osmotic pressure of body fluids increases f. Pituitary releases ADH g. ADH causes water more reabsorption by the nephron 47. Compare and contrast urea and uric acid. 48. What are the 5 substances that might be found in normal urine? 49. What is a normal amount of output? 50. What are 2 things that might affect urine output? 51. What is the function of the ureters? 52. What moves the urine through the ureters? 53. What are the 2 functions of the bladder? 54. What are the 3 holes of the trigone, openings for? 55. What is another term for micturition? What occurs during micturition? 56. What triggers micturition? 57. What is the range of urine volume the bladder would be holding to cause the micturition reflex? 58. What is the function of the urethra? Problems in the US 59. How does shock kill kidney cells? 60. Why is protein in the urine such a problem? 61. How might rennin be a problem? 62. What is glucosuria? When might it occur? 63. What causes gout? What is gout? 64. In what part of the kidney do kidney stones form? What are the 4 common causes of kidney stones? 65. What is cystitis? Why is it more common in women? 66. What is an automatic bladder?