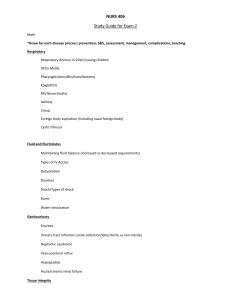
Review Article The Multidisciplinary Evaluation and Management of Cleft Lip and Palate Nathaniel H. Robin, MD, Heather Baty, MS, Judith Franklin, RN, Fran C. Guyton, MS, Judith Mann, MS, Audie L. Woolley, MD, Peter D. Waite, MPH, DMD, MD, and John Grant, Abstract: Cleft lip with or without a cleft palate (CLP) and cleft palate alone (CPA) are common birth defects, with a combined birth prevalence of about 1 to 2/1,000.1 Affected children have a number of medical issues and potential complications, and therefore require a wide variety of healthcare specialists beyond plastic surgeons and dental specialists. For this reason, the best environment in which to deliver this care is a multidisciplinary cleft clinic (MCC) that features a team of healthcare providers, including audiology, pediatric otolaryngology, speech pathology, occupational/feeding therapy, and genetics. In this setting, the many medical issues that these children face are comprehensively addressed in the most convenient manner, as all the specialists can be seen in a single busy day. Furthermore, the referring primary care provider (PCP) will receive a concise letter that documents the team evaluation, including future management plans and recommendations for therapy. Unfortunately, few papers are available in the literature that review the workings of these clinics. In this paper we will provide such an overview, discussing the management issues for children with CLP/CPA, and how these are addressed by members of the MCC. Key Words: multidisciplinary cleft team, plastic surgery, speech pathology, maxillofacial surgery, craniofacial genetics C left lip with or without a cleft palate (CLP) and cleft palate alone (CPA) are among the most common birth defects, with a combined birth prevalence of about 1 to 2/1,0001 (Table 1). Children with CLP/CPA face a wide variety of medical issues and medical complications. These extend beyond the surgical correction of the congenital defect, and therefore require evaluation and interventions by a wide variety of specialists. These issues are not static, as different issues manifest or become more important at different ages. Departments of Genetics, Pediatrics, Rehabilitation Services, Oral and Maxillofacial Surgery and Surgery, University of Alabama at Birmingham, Birmingham AL. Reprint requests to Nathaniel H. Robin, MD, Department of Genetics, University of Alabama at Birmingham, Kaul 210D, 1530 3rd Avenue South, Birmingham, AL 35294. Email: nrobin@uab.edu Accepted October 24, 2005. Copyright © 2006 by The Southern Medical Association 0038-4348/0⫺2000/9900-1111 Southern Medical Journal • Volume 99, Number 10, October 2006 MD For example, in the newborn period, making sure the infant can feed adequately is the primary concern,2 but later, orthodontic and cosmetic issues become more prominent. Other potential complications include hearing loss, speech, dental, and orthodontic complications. These require consistent monitoring through adolescence and into adulthood. To address the variety of primary and secondary problems associated with CLP/CPA, these individuals will see many different specialists (Table 2). This is best accomplished in the setting of a multidisciplinary cleft clinic (MCC).3 As many as a dozen different specialists can be seen in a single visit, making it convenient not only for parents but the child’s primary care provider (PCP) as well, as the PCP will receive a single concise letter summarizing the many specialists’ evaluations. This letter typically comes from the clinic director. While this person is often the lead craniofacial surgeon or clinic pediatrician, it can be any of the professionals listed in Key Points • Cleft lip and palate (CLP) is a common birth defect, but one that requires a multidisciplinary approach to optimize the chance of successful outcome. • The multidisciplinary cleft team includes members from many different medical specialties and branches. Understanding the roles of these professionals is important for the primary care provider to facilitate the best outcome for these patients. • There are a variety of causes of CLP, including genetic and nongenetic causes. Identifying the cause for a given patient is important to patient, their family as well as the healthcare team. • Planning the surgical repairs must take into account many different considerations and must balance functional and aesthetic outcomes in the developing child. These include speech production, dental health, and facial growth. • A child with CLP faces many potential associated complications, including feeding problems, hearing loss, and speech problems. These are monitored and treated by various professionals in the CLP team. 1111 Robin et al • The Multidisciplinary Evaluation and Management of Cleft Lip and Palate Table 1. Facts about cleft lip ⴙ/- palate (CLP) and cleft palate alone (CPA) Overall incidence of CLP and CPA is 1-2/1000 children CPA is about 1/1500, but it is more common if submucous CPA is included. Bifid uvula occurs in 1 of 80 patients and often occurs in isolation, with no clefting of the palatal muscles. Incidence of CLP varies by race. It is highest among American Indians, at 3.6 cases per 1000 live births, and lowest among African Americans, with 0.3 cases per 1000 live births. The incidence of CPA does not vary by race. Of all CLP and CPA: 20% of all clefts are isolated cleft lip (18% unilateral, 2% bilateral) 50% are CLP (38% unilateral, 12% bilateral) 30% are CPA CLP is twice as common in males; CPA is twice as common in females. Table 2. With the clinic coordinator, the director is responsible for overseeing the overall evaluation and management of the child and ensuring continuous communication with the parents and the PCP. Just as there is no single accepted leadership structure for a MCC, the responsibilities of a team member may be somewhat different in a different center. For example, in one clinic, alveolar bone grafting is done by a plastic surgeon, in another it is done by a maxillofacial surgeon. With this vast array of specialized healthcare providers, the MCC may seem mystifying, even intimidating, to most PCPs. There are many specialists in unfamiliar fields, each evaluating and prescribing focused therapies. However, as the PCP oversees the overall care of the child, they must have some familiarity with the MCC. It is the purpose of this article to review the management issues for children with CLP/CPA and how these are addressed by members of the MCC team. The Newborn Period–Feeding One of the first and most critical aspects of early management of the newborn with a CLP is adequate feeding and nutrition. In one study, parents of infants with CLP reported that their greatest concerns and problems were around feeding issues, more so than the etiology of the cleft or surgical repair.2 For this reason, the first CLP team member to evaluate the child is often the occupational therapist. All CLP infants are at risk for feeding difficulties due to the interruption of the baby’s seal on the nipple (with a cleft lip), and the loss in the strength of the suck (with a cleft palate). The occupational therapist will make an initial assessment and appropriate recommendations about the best utensil (ie, bottle and nipple) for the baby, and educate the family (and the staff, if the baby is in the hospital) in the best feeding techniques, as well as the warning signs for problems that may arise. CLP infants typically take a very long time to feed and still take only small amounts of formula from the bottle. 1112 Table 2. Healthcare personnel in a typical cleft clinic Clinic Directora Clinic Coordinator (assistant to the clinic director) Audiologists Craniofacial Surgeon Geneticist Neurosurgeons Nurses Occupational Therapists Oral and Maxillofacial Surgeons Orthodontists Otorhinolaryngologists (ENT) Pediatrician Pediatric Anesthesiologists Pediatric Dentists and Prosthodontists Pediatric Radiologists Physical Therapists Plastic Surgeons Speech Language Pathologists Surgeon’s Assistant a The clinic director can be any member of the team. There is no single model, but the most common is for the director to be the clinic’s pediatrician or one of the craniofacial surgeons. These infants will often fatigue before taking the needed volume, and not gain weight. This is undesirable for many reasons, including causing a delay in the first surgical repair. To address this problem, a bottle that allows assisted sucking with an orthodontic nipple is recommended. These are wide and soft and will assist in sealing the cleft and decreasing the air intake. Concentrating the formula (or supplementing breast milk) may be done as well. This is usually done in conjunction with a pediatric nutritionist. Parents will often ask about breastfeeding an infant with CLP. This may be possible if the palate is uninvolved, as the breast tissue works as a mold to seal the cleft lip and promote suction. However, if the palate is involved, it is not likely that adequate suction can be achieved. The occupational therapist will work with the child and family on an ongoing basis. Problems may arise at any time, but especially following surgical repairs, and when foods are advanced to textures, spoon-feeding and cup drinking, and later onto semisolid and solid foods. While most children will adapt to these advances in diet without difficulty, some will require more direction from the feeding therapist working with a nutritionist to make this a smooth transition. The Initial Visit to the Multidisciplinary Cleft Clinic The initial visit to the MCC typically includes a team evaluation of the infant during which a diagnosis will be © 2006 Southern Medical Association Review Article Fig. 1 A child with velocardiofacial syndrome (del22q11.2). Note the narrow palpebral fissures, broad nasal root with a bulbous tip, malar flattening, small mouth with sharp corners, and small ears. made (eg, isolated versus syndrome CLP), and a general treatment plan will be determined. This initial treatment plan will include introduction of the family members to the team concept of care. In this treatment paradigm, all potentially involved caregivers are available through the MCC and will be introduced as appropriate. For example, families with a 5-day old infant will meet with the audiologist, geneticist, occupational therapist, nurse and plastic surgeon, but not an orthodontist. Therefore, the primary goal of the initial visit is to provide information, clarify the diagnosis and to begin preparing the infant for the first operation. Genetics Evaluation Every child with a CLP should be evaluated by a medical geneticist at some point to determine if the CLP is an isolated finding or if it is part of a genetic syndrome. Some children, especially those with multiple anomalies, will have had a genetics evaluation during the newborn period. However, many will not have been seen by a geneticist, especially those who have no other major anomalies. A genetics evaluation typically includes a detailed history, including taking a 3 to 4 generation pedigree, and a detailed physical “dysmorphologic” examination that focuses Southern Medical Journal • Volume 99, Number 10, October 2006 on form, size, proportion, positioning, spacing, and symmetry.4 While there are many potential benefits, the fundamental purpose is to identify a genetic syndrome. Approximately 20% of CLP and a slightly higher number of CPA occur as part of a genetic syndrome. While some are obvious, many are subtle. For example, a child with velocardiofacial syndrome (VCFS) will manifest only minor facial findings in addition to a cleft palate, and are often not recognized by general pediatricians (Fig. 1).5 Why is making this diagnosis important? A good example is a child with CP as part of VCFS. These children have a high likelihood of having other medical problems that may not be identified, such as congenital heart defect, immune deficiency and hypocalcemia. In addition, later in childhood, they would be at risk for learning disorders, behavioral problems, and psychiatric disease. Speech problems can be seen as well and include dyspraxia, forced speech, and hypernasal speech due to velopharyngeal insufficiency (VPI). While VPI can be a long-term complication for some CP patients, it is seen at a much higher rate among VCFS patients.5 Furthermore, children with VCFS can have aberrant location of the carotid arteries, which may complicate CP surgery. Knowing this diagnosis allows surgeons to look for and anticipate these complications. A genetic evaluation will help define the prognosis, aid in management decisions, define accurate recurrence risk for the parents, and permit access to appropriate support groups. Lastly, it can address the question of why the disease occurred (Table 3). At the end of the genetics evaluation, recurrence risk issues (the likelihood of having another child with a cleft) can be addressed. When the CLP is part of a genetic syndrome, counseling will focus on what is known about that syndrome, including the recurrence risk, which can range from under 1% to as high as 50% if one parent is affected with the same autosomal dominant condition. However, the majority of CLP occur as isolated findings. It is never possible to absolutely rule out the presence of a genetic syndrome in a young infant, as many conditions present only in older children as the craniofacial appearance matures, or as other findings emerge. However, in an otherwise well infant, parents can be reassured that the CLP is isolated. Recurrence risk estimates for isolated CLP range from 1 to 7%, depending on the type and severity of the cleft. The more extensive the cleft, the higher the recurrence risk (eg, unilateral CL has a lower recurrence risk than bilateral CLP).6 Furthermore, it is emphasized that Table 3. Benefits of a genetics evaluation 1. 2. 3. 4. 5. Define prognosis Anticipation of future problems Define accurate recurrence risk Answer the question of why this occurred Access appropriate support groups 1113 Robin et al • The Multidisciplinary Evaluation and Management of Cleft Lip and Palate for parents of a baby with a CLP, their recurrence risk is for a baby with a cleft of the lip, or a cleft of the lip and palate, but not of the palate alone. This is because CLP has a different embryologic and genetic basis than CPA, so it is rare that CLP and CPA would occur in the same family. However, genetic advances are occurring rapidly, so in the near future genetic testing may have a greater and very different role (see Box 1). Box 1. Advances in Understanding the Genetic Basis of Cleft Lip and Palate Today, genetic assessment is limited to differentiating between syndromic and isolated, and then quoting empirically-deduced recurrence risks for parents of the affected child. However, we are in the midst of an explosion in our understanding of the genetic basis of CLP. For example, mutations in MSX1, TBX22, and IRF6 have all been identified in nonsyndromic CLP patients.1 It is the hope and expectation that genetic testing will provide an additional level of differentiation beyond what is possible by clinical examination only. We are limited in our ability to differentiate these subtypes by clinical evaluation—the cleft that occurs due to a mutation in TBX22 may look no different from that associated with an MSX1 or IRF6 mutation, or one that is caused principally by environmental factors, such as maternal smoking. However, each type carries a different recurrence risk for the family. Today, clinical geneticists counsel unaffected parents of a child with a CP that they have approximately a 1% risk for having a child with a CP with each future pregnancy, but that recurrence risk is derived from large population studies6 that include CP patients of many etiologic subtypes. For some families, the CP is due to a mutation in IRF6, TBX22 or MSX1, and these families have a higher recurrence risk than other families, whose child’s CP was caused by environmental factors, or even by chance. We are unable to differentiate these subtypes based on clinical evaluation, so we are left to counsel these families in a most general and inaccurate manner. Another potential application of genetic testing may be offering prognostic information. It may be that the different genetic forms of CLP respond to surgery and therapies differently, with higher or lower complication rates, such as residual velopharyngeal insufficiency or maxillary underdevelopment. If this proves true, knowing the genetic subtype of a CLP patient will allow the MCC staff to modify their therapy to better address the patient’s specific risks. 1114 Short- and Long-term Planning Plastic Surgery During the initial visit to the cleft clinic, the plastic surgeon will discuss relevant surgical procedures. This discussion will include the approximate ages for the surgical procedures as well as an explanation of the relevant details of the procedure including risks and estimated length of hospital stay as well as the expected in-hospital and posthospital recovery. Representative before and after photographs of similarly affected children on whom the surgeon has operated are reviewed with the child’s family (see Box 2). Box 2. Pierre Robin Sequence Pierre Robin sequence (PRS) deserves special attention from a genetics perspective, as it represents an entity distinct from typical clefting. PRS refers to the constellation of U-shaped cleft palate, micrognathia, and glossoptosis. It is not a “syndrome,” as it has been mistakenly referred to often in past literature (for a review of the differences between syndrome and sequence, see ref 3, but a sequence is series of anomalies derived from a single anomaly. In this case, micrognathia causes the tongue to be displaced superiorly during development, interfering with palatal closure at approximately 9 weeks gestation. So the CP is not caused by genetic factors involved in palatal closure, but is due to the small jaw. However, a sequence can be part of a syndrome, as is approximately one-half of PRS cases. The most common syndromes associated with PRS are Stickler syndrome (SS), and VCFS. Therefore, every baby with PRS should have a karyotype and FISH testing for del22q11, and an eye examination looking for the typical findings of SS. As not all forms of SS have eye involvement, babies with normal eye examinations should be followed for other manifestations of SS, such as spondyloepiphyseal dysplasia, hearing loss, and early onset arthritis. To understand CLP/CPA surgery, one must have some understanding of its embryology (see ref 7 for a detailed review). The upper lip develops from three anatomic subunits which fuse together at approximately six weeks of gestation. In the noncleft lip, these three subunits are the two lateral lip elements and the central unit bordered by the two philtral columns. The philtral columns mark the normal line of fusion between these segments (Fig. 2). The failure of fusion (cleft) occurs along the line of the philtral column and may extend to the nose. A unilateral CL (uCL) will involve one philtral column (Fig. 3a). A bilateral CL (bCL) will involve both © 2006 Southern Medical Association Review Article rearrange the tissues and reconstruct the normal anatomy, with particular attention to symmetry. Planning Surgery Fig. 2 Shaded area represents the philtral anatomic subunit and is bordered laterally by the two philtral columns. philtral columns, leaving a central prolabial segment connected to the columella of the nose (Fig. 3b). The orbicularis oris muscle (which develops from branchial arch derivatives, directed by cephalic neural crest cells) courses lateral to medial along each lateral lip segment. With uCL, the muscle does not cross the cleft, and instead runs along the margin of the cleft with aberrant attachments at the columella and alar base of the nose on the side of the cleft. This muscle malalignment has been implicated in the etiology of the cleft nasal deformity. In the case of a bCL, the muscle is therefore absent from the central (prolabial) segment. This knowledge is important in explaining to parents that all the critical parts of the lip are present, so that the goal of surgery is simply to Primary surgical procedures refer to those operations that address the congenital anatomic defect in the lip, nose, palate and/or alveolar ridge (cheiloplasty, rhinoplasty, palatoplasty and gingivoplasty, respectively). The goal is to reconstruct the body part in proper anatomic and esthetic fashion (Fig. 4). Secondary procedures may be directed at complications of primary operations, residual functional or esthetic deficiencies and failures of growth which may be secondary to surgical scarring or to an underlying genetic predisposition to hypoplasia. While most children will need several operations, the exact number depends on several variables. Some can be predicted by the extent of the defect (eg, a bCLP will require more procedures than a uCL), while others are more difficult to predict, such as the likelihood of residual speech problems or orthodontic complications. Timing of Operations The initial CL repair (“cheiloplasty”) typically occurs when the infant is age 10 to 12 weeks. However, timing may be altered for infants with associated medical conditions, such as a cardiac malformation, or poor nutrition. The “Rule of Tens” provides a simple guideline for timing the first operation: weight ten pounds, age ten weeks, and hemoglobin 10 g. Meeting these parameters signifies that the child is in a positive nitrogen balance, receiving adequate nutrition. Questions about feeding are especially important for infants with CLP, as feeding difficulties are very common in early childhood. As discussed above, the occupational therapist is responsible for the ongoing monitoring of the baby’s Fig. 3 Unilateral and bilateral cleft lip examples to illustrate effect of cleft on normal philtral subunit. (a) Unilateral cleft lip palate with normal half of philtral subunit marked and shaded to the midline. Incision will mirror normal philtral column. (b) Bilateral cleft lip palate with planned philtral subunit shaded. Incisions will border this shaded area and recreate two philtral subunits. Southern Medical Journal • Volume 99, Number 10, October 2006 1115 Robin et al • The Multidisciplinary Evaluation and Management of Cleft Lip and Palate Fig. 4 Aesthetic consideration to philtral subunit illustrated in pre- and postsurgery images of the same patient. feeding and nutritional status. This becomes especially important as the time of surgery approaches, and during the recovery period. During the postoperative period, progress in feeding may be slowed or even reversed, so close monitoring is needed at this time. Some MCC teams advocate presurgical orthopaedics during the months before surgery. This may be as simple as taping the two lip segments together across the cleft, thereby artificially approximating the oral sphincter and allowing the lip muscle to shape the bones of the maxillary segments. More complex protocols involve weekly visits and various acrylic splints to guide the two segments of the gums together.8 Other devices, such as the Latham appliance, involve a mechanical system attached to the palatal shelves with pins. The Latham appliance has a screw which is adjusted by the parents at home, gradually pulling the two halves of the maxilla together. Surgical Technique ineffective suck during nursing. A unilateral CP will extend anteriorly into the hard palate and may involve the alveolus as well. One nasal passage is visible in the cleft with the vomer attached to the larger maxillary segment. A bilateral CP will be a midline cleft and may involve only the soft palate [Figure 5]. In this case two halves of the uvula will be seen on either side of the cleft. As the cleft extends anteriorly, it may involve the hard palate as far forward as the incisive foramen. In this case, the vomer will be visualized as a narrow midline structure in the depth of the cleft. If the cleft involves the alveolar ridge, the cleft will then deviate to one or both sides of the premaxilla. In all of these variations, the repair is similar, in that the palate is repaired in layers, first closing the nasal lining, then repositioning the levator veli palatini muscle (intravelar veloplasty) and lastly closing the oral mucosa to anatomically reconstruct the palate. With a submucous CP the palate appears intact to visual inspection, and feeding may be normal. Consequently the diagnosis may be made much later when the child demonstrates hypernasal speech. In ret- There are several accepted and widely used surgical techniques for cheiloplasty, and while a detailed discussion of each is not possible or appropriate for this review, we will provide a brief overview. Most techniques are variations of the rotation-advancement procedure first described by Millard.9 Many surgeons will also perform a simultaneous primary rhinoplasty to address the associated cleft nasal deformity at the same time as the cheiloplasty. This was once condemned, as it was believed that extensive operations on the infant nose might result in growth disturbance. However, we now know that primary rhinoplasty does not have an adverse effect on the nose.10 For infants with CLP, myringotomy tube placement is usually performed at the same time as the cheiloplasty CP. As described below, children with CLP or CPA will have eustachian tube dysfunction and most will have middle ear disease. Cleft Palate Repair. Cleft palate (CP) may manifest as unilateral, bilateral or submucous. An overt CP is typically apparent on physical examination, but if missed at that time, will present early after birth when the infant demonstrates an Fig. 5 Intraoperative photograph of a cleft palate. 1116 © 2006 Southern Medical Association Review Article rospect, a close examination may reveal the diagnostic triad of a submucous CP— bifid uvula, a palpable notch in the posterior border of the hard palate, and a central blue line or zona pellucida indicating that the levator veli palatini muscles run parallel to the midline and do not form an effective sling mechanism through the soft palate. These children may manifest frequent nasal regurgitation in infancy, be plagued by multiple episodes of otitis media and later develop hypernasal speech. The CP repair is usually performed at 6 to 12 months of age. Earlier repair results in better speech outcomes, while a later repair may have more favorable maxillary growth and therefore better dental occlusion.11 The choice of 6 to 12 months represents a balance between these 2 outcomes. Most CP repair is done in a single operation, and, as with CL surgery, there are several accepted techniques. All include a layered closure of the nasal lining and the oral lining, but some techniques include the additional step of repairing the muscles within the palate (levator veli palatine), thereby recreating the palatal muscular sling. In some cases, CP surgery will be deferred until there is sufficient growth of the maxillary segments to allow repair under minimal tension. This is done to minimize healing complications such as incision breakdown with fistula formation. Fistula formation between the oral and nasal cavities is a major complication of CP surgery, as it may adversely affect speech with nasal air escape, and permit nasal regurgitation of food. Fistulas require surgical repair, but due to the scarred tissue, the success rate is as low as 50%, even in experienced hands.12 Secondary Procedures. Secondary surgical procedures are directed at enhancing the outcomes or addressing the complications of primary operations. They may therefore address residual functional or esthetic deficiencies and failures of growth. These unplanned outcomes may be secondary to surgical scarring, or due to an underlying genetic predisposition to poor growth, as is seen with many syndrome-related forms of CLP. The most common residual deficits seen at our center include hypernasal speech due to velopharyngeal insufficiency and minor residual deformity of the nose and lip. Failure of the maxilla to grow in concert with the mandible and the resultant dental malocclusion are covered elsewhere in this text (see Oral and Maxillofacial Surgery section). Secondary Rhinoplasty. A secondary rhinoplasty is a functional as well as esthetic procedure, as it will improve nasal appearance as well as nasal patency. The widespread use in primary cleft rhinoplasty has reduced the need for secondary nasal surgeries, but it is still needed for more severe unilateral defects and most bilateral defects. In general, the rhinoplasty is deferred until after the dentoskeletal platform has been addressed with alveolar cleft bone grafting and orthodontia. Velopharyngeal Insufficiency and Speech Assessment. A primary goal of CP surgery is normal speech. However, regardless of surgical technique, the surgeon’s experience, or Southern Medical Journal • Volume 99, Number 10, October 2006 any other measurable variable, about 10 to 20% will manifest velopharyngeal insufficiency (VPI).13 The number is even greater for those children with an underlying genetic syndrome, such as velocardiofacial syndrome.13 VPI occurs when there is an inability of the soft palate to achieve tight closure with the lateral and posterior pharyngeal walls, resulting in air that should be directed through the mouth leaking through the nose. VPI manifests itself in speech through audible nasal air escape (ANAE) and hypernasal resonance. VPI can be caused by structural abnormalities, neurogenic etiologies, or mislearning, all of which can be seen in CLP patients. A speech/language pathologist (SLP) will determine the presence or absence of velopharyngeal closure through careful speech assessment that includes a nasopharyngoscopic examination and in some cases, multiview videofluoroscopy. These will document the structure and function of the velopharyngeal mechanism. While in some cases ANAE may be evident in casual conversation, it may be so mild as to require assessment of articulation or careful clinical examination. Even mild hypernasality may distort speech sound production by reducing the child’s ability to build intraoral air pressure, affecting the consonants s, z, sh, f, p, and b. Simple methods can be used to diagnose VPI, such as holding a mirror below the nose which will be fogged by the nasal air escape, or a hearing aid stethoscope or nasal listening tube to detect nasal air flow on pressure sounds.14 Hypernasal resonance of speech is another manifestation of VPI. In the English language there are only three consonants that should be nasalized: /m/, /n/, and /ng/. Very mild hypernasality can be functional (as in the case of some dialects), but most often is pathologic, secondary to VPI. Again, simple diagnostic methods can be used to evaluate hypernasality, such as comparing the quality of resonance with the nose pinched closed and open. The degree of hypernasality can be determined using tools such as the Nasometer (Kay Elemetrics Corp., Lincoln Park, NY), which provides a visual analysis of the oral-nasal resonance ratio.15,16 Articulation (speech sound) development, while closely interrelated with resonance, must be evaluated separately. A child with a repaired CP may have articulation errors caused by VPI or by structural abnormalities such as dental malocclusions or fistulas. They may also have developmental speech delays as could be seen in a child without a cleft. Children with VPI may also develop compensatory articulation errors – errors that are caused by the child’s efforts to produce understandable speech with an inadequate speech mechanism. There are over ten different compensatory articulation strategies, such as the “glottal stop” and “pharyngeal fricative” (Box 3). With these and other compensatory errors, management of the underlying cause of the VPI, either with surgery or a dental prosthesis, is needed before speech therapy can be effective. 1117 Robin et al • The Multidisciplinary Evaluation and Management of Cleft Lip and Palate Box 3. Common Compensatory Speech Errors: The “glottal stop” and “pharyngeal fricative” A glottal stop is made by adducting the vocal cords and allowing air pressure to build below the level of the glottis followed by an explosive release of the air. Glottal stops can be heard in the interjection “uh oh” but are rarely used in English. They are present in some nonstandard English dialects such as Cockney, and are normal in other languages such as Hebrew and Japanese. A child with VPI uses the glottal stop to replace stop consonants (p, b, t, d, k, g). While this produces an aberrant sound, the glottal stop may improve speech intelligibility in a child who can only produce vowels. A pharyngeal fricative is produced by moving the posterior portion of the tongue near to the posterior pharyngeal wall then pushing air between this constriction. Pharyngeal fricatives are used in place of speech sounds which require oral air flow over some point of constriction in the mouth such as [s, z, f, sh]. As with the glottal stop, the sound produced is very aberrant but can improve a child’s ability to make him understood. Dental and Oral and Maxillofacial Issues A major goal of CLP surgery is normal midface skeletal growth, and for this to occur it is necessary to have proper reconstruction of the facial and masticatory muscles. Their normal activity stimulates primary and secondary growth centers of the facial skeleton. Abnormal oral function leads to abnormal stimulation, which will manifest as malocclusion, cross bites, impacted teeth, midface deficiency, nasal obstruction, and apnea.16 Even with the best repair, about 25% of CLP patients will have some residual jaw deformities that will require additional surgery.17 Until recently, the standard surgery would move the mandible back to fit the underdeveloped maxilla. However, current surgical techniques use complete maxillary osteotomy (LeFort 1) to advance the deficient maxilla.18 This can be done with minimal morbidity, length of stay, and yields overall better cosmetic/functional results. Such extensive surgery is best performed after bone growth is complete, usually the age of menarche for girls and about age 18 for boys. Orthodontic treatment may be performed at different stages of the patient’s development, depending on the particular problem. As the treatment is often lengthy, unpleasant, and expensive, it presents a burden to both the family and child. They must be motivated to complete the treatment and able to remain compliant over the course of the therapy, which is often several years. As discussed above, some centers treat neonates with CLP using maxillary obturators and 1118 arch molding. These devices prevent nasal reflux, and keep the tongue from displacing the cleft segments. The splint is modified by the pediatric dentist allowing the function of the lips to bring the segments in better anatomic location, thereby assisting in closure of the alveolar defect and hard palate. In somewhat older children, once primary teeth erupt, palatal expanders can be used to move the segments and align the palatal arches. This is intended to prevent malocclusion in the deciduous dentition, an important step in reducing the occurrence of later orthodontic problems. During the period of mixed dentition (presence of both permanent and deciduous teeth) orthodontic treatment is focused on preparing for alveolar bone grafting. As many as 75% of CLP patients have osseous defects of the maxillary alveolar bone, and grafting this defect is needed to normalize facial and dental function. Typically, bone grafting is done before orthodontic treatment, as it will lessen the time in braces, and gives more time for eruption and support of the permanent teeth.19 The orthodontist and the oral and maxillofacial surgeon must work together in preparing the area for grafting. The palatal segments must be aligned, and the cleft area should be clear of chronic inflammation from the teeth or fistula. Baby teeth adjacent to the cleft should be extracted at least 1 month before to allow healthy attached gingiva. Timing is critical, as this is best done after the majority of facial growth is complete and the secondary dentition is erupting; typically at about 6 to 8 years of age, or when the central incisors are erupting. Secondary bone grafting yields superior results to primary grafting, which is done in the first 18 months of life. This is because primary bone grafting retards growth and the quality of bone is poor by the time the cuspid erupts.20 In older children and adolescents, orthognathic surgery is often required in addition to orthodontic treatment, as the secondary skeletal jaw deformities must be corrected to get the teeth in proper alignment. This is most predictable after growth is complete as an adult. Oral Hygiene Many parents of a child with a CLP assume that their child’s dentition is hopeless and therefore ignore routine dental care. Teeth will often be poorly formed, lacking enamel, and be at risk loss due to decay. However, the presence of functional teeth actually stimulates and retains alveolar bone, and is important for lip support and function. Furthermore, CLP patients are often missing teeth, and therefore the teeth that do form will be carefully protected. Routine oral hygiene and prevention of dental caries is therefore very important, and should begin as soon as the first tooth erupts. Hearing and CLP Otitis media (OM) with middle ear effusion (MEE) is present in virtually all infants under 2 years of age with an unrepaired CP.21 This is attributed to eustachian tube dys© 2006 Southern Medical Association Review Article function. Although anatomically patent, they are unable to open properly and ventilate the middle ear. Following CP repair, rates of OM are reduced, but for most patients, middle ear disease remains an important problem well into adult life.22 If untreated, chronic middle ear disease can extend to the inner ear resulting in sensorineural hearing loss.3 Whether permanent or intermittent, this hearing loss can have a significant negative impact on speech and language development, resulting in language deficits, lowered academic performance, reduced cognitive skill and behavioral problems.23 It is therefore crucial that children with CP have frequent and consistent hearing evaluations throughout childhood and beyond. While minimal guidelines exist,3 each child must be reviewed individually at each clinic visit to determine if additional testing is needed. An audiologist should obtain a baseline hearing evaluation at the initial MCC visit, and follow-up testing at each subsequent visit. If middle ear pathology is suspected, referral is made to the pediatric otolaryngologist for management. This includes early myringotomy, aspiration of fluid, and insertion of myringotomy tubes followed by repeat tube insertion as needed to maintain middle ear ventilation. For patients with an associated CL, myringotomy tubes can be placed at the same time of CL repair, around 2 to 3 months. For CPA patients with persistent MEE, myringotomy and tympanostomy tube insertion should be done within the first year of life.23 For children whose hearing is within the normal range, tube insertion can be delayed beyond 12 months, or even indefinitely. For such children, tympanometry is done every visit until they have been symptom free, with normal tympanograms and no episodes of otitis media for one year. For all children, tympanograms are a recommended part of an annual comprehensive evaluation until at least age six.3 However, children with intermittent OM/MEE are followed as long as hearing loss and/or abnormal tympanometry presents. In such children, myringotomy tubes should be re-inserted once they extrude. Long-term Issues The long-term health concerns for CLP patients, as well as for children with birth defects in general, have been insufficiently studied.24 It is reasonable to assume that individuals with CLP should have relatively normal long-term health, as CLP is a repairable birth defect, and the associated medical issues are for the most part readily treatable.25 However, several studies have suggested that individuals with CLP have a higher than expected incidence of psychiatric and behavioral diseases,26 –27 an increased risk for cancer,28 –29 and an increased mortality in general from all major causes of death.25 There is no readily apparent explanation for these concerning findings, as these are not related to the occurrence of associated anomalies or coexisting syndromes. While these Southern Medical Journal • Volume 99, Number 10, October 2006 findings must be viewed as preliminary, they emphasize the need for more comprehensive and extended follow-up of CLP patients to monitor for these and other long-term healthcare complications. Acknowledgments NHR is supported by NIDCD 1 P50 DE16215. References 1. Cox TC. Taking it to the max: The genetic and developmental mechanisms coordinating midfacial morphogenesis and dysmorphology. Clin Genet 2004;65:163–176. 2. Young JL, O’Riordan MA, Goldstein JA, Robin NH. What information do parents of newborns with cleft lip, palate or both want to know. Cleft Palate Craniofac J 2001;38:55–58. 3. American Cleft Palate-Craniofacial Association. Revised April 2000. Parameters for Evaluation and Treatment of Patients with Cleft Lip/ Palate or Other Craniofacial Anomalies, April 2000 (available at http:// www.cleftline.org/). 4. Falk MJ, Robin NH. The primary care physician’s approach to congenital anomalies. Prim Care 2004;31:605–619. 5. Shprintzen RJ. Velocardiofacial syndrome. Otolaryngol Clin North Am. 2000;33:1217–1240. 6. Wyszynski DF, Zeiger J, Tilli MT, et al. Survey of genetic counselors and clinical geneticists regarding recurrence risks for families with nonsyndromic cleft lip with or without cleft palate. Am J Med Genet 1998; 79:184–190. 7. Larsen WJ. Human Embryology, 2nd ed. Philadelphia: Churchill Livingstone 1997. 8. Grayson BH, Santiago PE, Brecht LE, et al. Presurgical nasoalveolar molding in infants with cleft lip and palate. Cleft Palate Craniofac J. 1999 Nov;36:486–498. 9. Cleft Craft: The evolution of Its Surgery, Vol. III: Alveolar and Palatal Deformaties. Boston, H Little, Brown & Co., 1976. 10. Salyer KE, Genecov ER, Genecov DG. Unilateral cleft lip-nose repair: a 33-year experience. J Craniofac Surg. 2003;14:549–558. 11. Rohrich RJ, Love EJ, Byrd, et al Optimal timing of cleft palate closure. Plast Reconstr Surg. 2000;106:413–421; quiz 422; discussion 423– 425. 12. Thaller SR. Staged repair of secondary cleft palate deformities. J Craniofac Surg. 1995 6:375–380; discussion 381. 13. Witt PD, Myckatyn T, Marsh JL, et al. Need for velopharyngeal management following palatoplasty: an outcome analysis of syndromic and nonsyndromic patients with Robin sequence. Plast Reconstr Surg. 1997 99:1522–1529; discussion 1530 –1534. 14. Blakely R. Palate Dysfunction and Speech Disorders: Evaluation and Treatment Planning Programs for Children and Adults. Austin, PROED, Inc, 2000. 15. Shipley KG, McAfee JG. Assessment in Speech-Language Pathology: A Resource Manual, 3rd ed. Clifton Park, Delmar Publishing, 2002.. 16. Anastassov GE, Joos U. Comprehensive management of cleft lip and palate deformities. J Oral Maxillofac Surg 2001;59:1062–1075; discussion 1075–1077. 17. Ross RB. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Cleft Palate J 1987;24:5–77. 18. Georgiade NG, Latham RA. Maxillary arch alignment in the bilateral cleft lip and palate infant, using pinned coaxial screw appliance. Plast Reconstr Surg. 1975 56:52–60. 1119 Robin et al • The Multidisciplinary Evaluation and Management of Cleft Lip and Palate 19. Precious DS. Alveolar bone grafting. Oral and Maxillofacial Clinics of North America 2000;12:501–513. 20. Waite PD, Waite DE. Bone grafting for the alveolar cleft defect. Semin Orthod 1996;2:192–196. 21. Paradise JL, Bluestone CD, Felder H. The universality of otitis media in 50 infants with cleft palate. Pediatrics 1969;44:35–42. 22. Paradise JL, Bluestone CD. Early treatment of the universal otitis media of infants with cleft palate. Pediatrics 1974;53:48–54. 23. Downs M. Contribution of Mild Hearing Loss to Auditory Language Learning Problems, in Roser R, Downs M (eds): Auditory Disorders in School Children. New York, Thieme Medical Publishers, 1995, pp 198. 24. Hunt GM, Oakeshott P. Outcome in people with open spina bifida at age 35: prospective community based cohort study. BMJ 2003;326:1365– 1366. 25. Christensen K, Juel K, Herskind AM, et al. Long term follow up study of survival associated with the left lip and the palate at birth. Br Med J 2004; 238:1405. 26. Ramstad T, Ottem E, Shaw WC. Psychosocial adjustment in Norwegian adults who had undergone standardised treatment of complete cleft lip and palate. II. Self-reported problems and concerns with appearance. Scand J Plast Reconstr Surg Hand Surg 1995;29:329–336. 27. Christensen K, Mortensen PB. Facial clefting and psychiatric diseases: a follow-up of the Danish 1936-1987 Facial Cleft cohort. Cleft Palate Craniofac J 2002;39:392–396. 28. Zhu JL, Basso O, Hasle, et al. Do parents of children with congenital malformations have a higher cancer risk? A nationwide study in Denmark. Br J Cancer 2002;87:524–528. 29. Zack M, Adami HO, Ericson A. Maternal and perinatal risk factors for childhood leukemia. Cancer Res 1991;51:3696–3701. Having a family is like having a bowling alley installed in your brain. —Martin Mull 1120 © 2006 Southern Medical Association