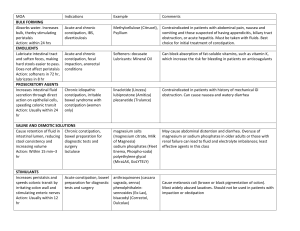
Pediatric Primary Care Management: Abdominal Pain (Part 3) Kristina Bohm, DNP, APRN, FNP Community Faculty Metropolitan State University: School of Nursing 6-month-old Male Intussusception • Epidemiology • Most commonly occurs between 5 and 10 months of age • Most common cause of intestinal obstruction in children 3 months to 6 years of age • 80% of cases occur before 2 years of age • Generally idiopathic in younger infants • Predisposing Factors • • • • • • • • • • Polyps Meckel diverticulum Henoch-schonlein purpura Constipation Lymphomas Lipomas Parasites Rotavirus Adenovirus Foreign bodies • Pathophysiology Intussusception History Physical Exam • Paroxysmal, episodic colicky abdominal pain • Observe infant’s appearance and behavior • Currant jelly stool • Sausage-like mass may be felt in RUQ of abdomen with emptiness in RLQ (Dance sign) • Vomiting every 5 to 30 minutes (nonbilious initially) • Screaming with drawing up of legs with periods of calm, sleeping or lethargy between episodes • Abdomen often distended and tender to palpation • Grossly bloody or guaiac-positive stools Intussusception Differential Diagnoses Diagnostic Tests Incarcerated hernia Testicular torsion Acute gastroenteritis Appendicitis Colic Intestinal obstruction • Ultrasound Intussusception: Management • Immediate referral to pediatric radiologist and pediatric surgeon 12-Year-Old Girl Appendicitis Epidemiology Pathophysiology Perforation most common in children under 5 years of age Average age in children is 6 to 10 years old 4 cases per 1000 children 2:1 male to female ratio Rare in infancy • Inflammation of the appendix that leads to distention and ischemia that can result in necrosis, perforation, and peritonitis or abscess formation Appendicitis History • Pain • Nausea • Anorexia • Stool – low volume with mucus • Fever • Scoring System: 4 or less is highly sensitive in excluding diagnosis of appendicitis: • • • • • • • • Nausea/emesis (1 point) Anorexia (1 point) Migration of pain to RLQ (1 point) Low-grade fever (1 point) RLQ tenderness on light palpation (2 points) Cough/percussion/heel tapping tenderness at RLQ (2 points) Leukocytosis (>10,000/mm3) (1 point) Left shift (>75% neutrophilia) (1 point) Physical Exam Involuntary guarding, RLQ rebound tenderness, max pain over McBurney point Heel-drop jarring test Positive Psoas sign or obturator sign (or both) Rovsing sign or rebound tenderness Tenderness and possibly a mass on right side on rectal exam Appendicitis Differential Diagnoses Diagnostic Tests • • • • • • • • • • • • • • • • • • Gastroenteritis Constipation UTI Pregnancy PID Pneumonia Duodenal ulcer Intestinal obstruction Peritonitis Intussusception CBC with differential Amylase, lipase, liver enzymes UA Stool sample Abdominal Xray Ultrasound CT scan with contrast B-hCG Surgical consult for appendectomy Appendicitis: Managemen t Open Laparoscopic Pain Management Follow-up 2-4 weeks post-op 12-Year-Old Girl Constipation Epidemiology Pathophysiology • 17-40% of children constipation starts in the 1st year of life • Many etiologies for constipation • Functional constipation has no underlying medical disease responsible Constipation: History & Physical Exam Physical Exam • Growth charts • GI • Skin • Neuro http://bowelcontrol.nih.gov/bristol.aspx (Tabbers, 2014) Constipation: Differential Diagnoses • (Tabbers, 2014) Constipation • To Diagnose: (Rome Foundation, 2015) Constipation: Management Infants < 6-months-old (Tabbers, 2014) Constipation: Management Infants >6-months-old (Tabbers, 2014) Constipation: Management (Tabbers, 2014) 6-Month-Old Female Hernia: Pathophysiology Umbilical Hernia Inguinal Hernia • Weakness or imperfect closure of the umbilical ring • Incomplete closure of processus vaginalis http://drmatthewweiner.com/surgery-for-umbilical-hernias/ • Males 8-10: females 1 http://www.mayoclinic.org/diseases-conditions/inguinal-hernia/multimedia/inguinal-hernia/img-20007189 Hernia: History & Physical Exam Umbilical Inguinal • Swelling peri-umbilical area • Swelling in inguinal, scrotal, or both • Direct: push outward through the weakest point in the abdominal wall • Indirect: push downward at an angle into the inguinal canal • Fussy & distended = incarcerated Hernia: Management Umbilical Inguinal Hernia • Refer to surgery if • US if need for dx • Persists > 5-years-old • Nonreducible • Dramatically enlarges • Incarceration is rare • Attempt to reduce it • Refer to surgeon within 1-2 weeks • Do NOT resolve spontaneously References Maaks, D.L. G., Starr, N., & Gaylord, N. (2020). Burns' Pediatric Primary Care (7th ed.). Elsevier Health Sciences (US). Rome Foundation. (2015). Rome III diagnostic criteria for functional GI disorders. Retrieved from http://romecriteria.org/criteria/ Tabbers, et al. (2014). Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHN and NASPGHAN. JPGN, 58(2): 258 -274