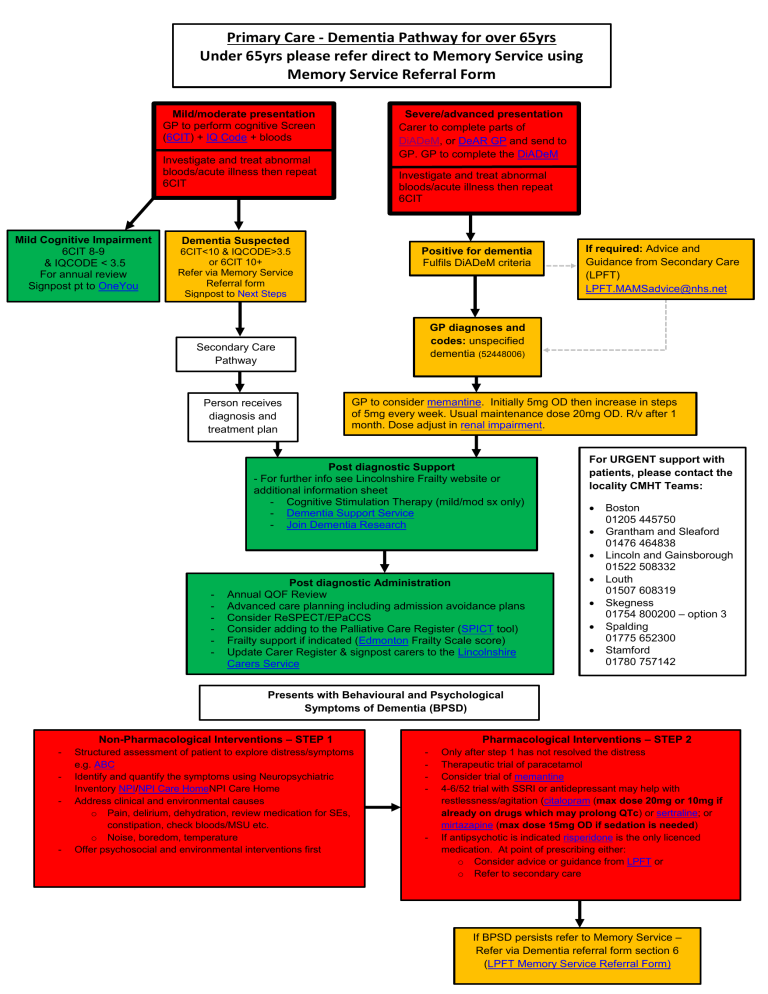
Primary Care - Dementia Pathway for over 65yrs Under 65yrs please refer direct to Memory Service using Memory Service Referral Form Mild/moderate presentation GP to perform cognitive Screen (6CIT) + IQ Code + bloods Severe/advanced presentation Carer to complete parts of DiADeM, or DeAR GP and send to GP. GP to complete the DiADeM Investigate and treat abnormal bloods/acute illness then repeat 6CIT Mild Cognitive Impairment 6CIT 8-9 & IQCODE < 3.5 For annual review Signpost pt to OneYou Investigate and treat abnormal bloods/acute illness then repeat 6CIT Dementia Suspected Positive for dementia Fulfils DiADeM criteria 6CIT<10 & IQCODE>3.5 or 6CIT 10+ Refer via Memory Service Referral form Signpost to Next Steps GP diagnoses and codes: unspecified dementia (52448006) Secondary Care Pathway Person receives diagnosis and treatment plan If required: Advice and Guidance from Secondary Care (LPFT) LPFT.MAMSadvice@nhs.net GP to consider memantine. Initially 5mg OD then increase in steps of 5mg every week. Usual maintenance dose 20mg OD. R/v after 1 month. Dose adjust in renal impairment. Post diagnostic Support - For further info see Lincolnshire Frailty website or additional information sheet - Cognitive Stimulation Therapy (mild/mod sx only) - Dementia Support Service - Join Dementia Research For URGENT support with patients, please contact the locality CMHT Teams: - Post diagnostic Administration Annual QOF Review Advanced care planning including admission avoidance plans Consider ReSPECT/EPaCCS Consider adding to the Palliative Care Register (SPICT tool) Frailty support if indicated (Edmonton Frailty Scale score) Update Carer Register & signpost carers to the Lincolnshire Carers Service Boston 01205 445750 Grantham and Sleaford 01476 464838 Lincoln and Gainsborough 01522 508332 Louth 01507 608319 Skegness 01754 800200 – option 3 Spalding 01775 652300 Stamford 01780 757142 Presents with Behavioural and Psychological Symptoms of Dementia (BPSD) Non-Pharmacological Interventions – STEP 1 - - Structured assessment of patient to explore distress/symptoms e.g. ABC Identify and quantify the symptoms using Neuropsychiatric Inventory NPI/NPI Care HomeNPI Care Home Address clinical and environmental causes o Pain, delirium, dehydration, review medication for SEs, constipation, check bloods/MSU etc. o Noise, boredom, temperature Offer psychosocial and environmental interventions first Pharmacological Interventions – STEP 2 - - Only after step 1 has not resolved the distress Therapeutic trial of paracetamol Consider trial of memantine 4-6/52 trial with SSRI or antidepressant may help with restlessness/agitation (citalopram (max dose 20mg or 10mg if already on drugs which may prolong QTc) or sertraline; or mirtazapine (max dose 15mg OD if sedation is needed) If antipsychotic is indicated risperidone is the only licenced medication. At point of prescribing either: o Consider advice or guidance from LPFT or o Refer to secondary care If BPSD persists refer to Memory Service – Refer via Dementia referral form section 6 (LPFT Memory Service Referral Form)




