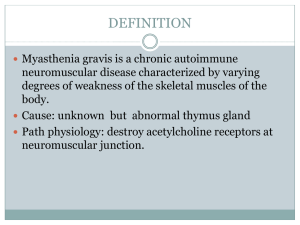
MS Patho Autoimmune, chronic, degenerative, & progressive Demyelination (loss of the myelin sheath ) of CNS nerve fiberseventually nerve function is lost permanently. Plaques (scar tissue) seen on MRI-nerve impulse can’t be conducted across scar tissue. Women affected more than men S/S The onset of MS is often slow and gradual. Vague symptoms occur over months or years. For some patients, MS is marked by rapid, progressive deterioration. Others have remissions and exacerbations. Blurred or double vision, red-green color distortion, or even blindness in one eye may be the first symptom experienced by a person with MS. Weakness, muscle spasticity, nystagmus, ataxia, dysarthria, dysphagia, bowel and bladder issues, fatigue, impaired sensation, 50% have cognitive deficits, labile emotions. Short term memory, word finding, worsening visual changes may occur in later stages Death usually occurs due to infection like pneumonia o Cardiomyopathies o Aortic Disorders Valve disorders MG Autoimmune, chronic. Remissions and Exacerbations, progressive Antibodies attack acetylcholine (ACh) receptor sites= not enough sites to have nerve transmission Weakness worsens during the day or at times of stress; improves with rest. Thymus gland may be involved- thymectomy Diplopia-(double vision), eye lid drooping (ptosis), difficulty chewing and swallowing, respiratory paralysis & failure. Face & mouth most affectedSnarling appearance - Myasthenia Crisis- is an acute exacerbation of muscle weakness triggered by infection, stress, surgery, emotional distress, or inadequate medication (pyrostigmine). S/S: Hypoxia, tachycardia, HTN, tachypnea, dyspnea, ↓ UO, absence of cough/gagairway crisis, ptosis (droopy eyelid), diplopia (double vision), May need intubation and mechanical ventilation Tensilon test used to diagnose myasthenia crisis versus cholinergic crisis (caused by too much medication). A positive Tensilon test the symptoms get better when Tensilon given. Atropine needed at bedside during test for possible severe bradycardia and resp failure Cholinergic Crisis- Nursing Care Nursing Considerations Accommodate room and nursing care for vision changes during an exacerbation. For constipation give diet ↑ fiber & fluids - Provide safety -Fall risk, balance issues -Monitor for dysphagia/eating issues -Monitor resp status b/c ↓ diaphragm strength Patient Teaching - Teach to avoid over-fatigue and triggers (infection, trauma, after childbirth, stress) -Teach to take medications prior to more active or stressful times -Pregnancy- s/s may improve while pregnant -Plan rest periods throughout the day Nursing Considerations -Prevent aspiration - Assess and monitor: * Respiratory failure * Nutrition due to impaired swallowing - Communication - Visual Changes - Avoid/ Assess fatigue & make sure patient gets rest - Plan activities at times of max muscle strength Patient Teaching: - Follow medical regimen closely - Cluster care - Teach about complications of the disease & therapy (crisis conditions) & what to do about them. S/S: caused by too much medication, causes SLUD: salivation, lacrimation, urination, defecation/diaphoresis (all increased). PD Chronic, Progressive Dopamine deficiencydegeneration of dopamine producing neurons in substantia nigra disrupts balance of ACh & dopamine in basal ganglia Mild tremor at rest, slight limp, ↓ arm swing shuffling, propulsive gait w/ arms flexed & loss of postural reflexes, slight change in speech patterns 1. Tremor- 1st sign (affect handwriting); worse at rest & is aggravated by emotional stress or ↑ concentration; hand tremor- pill rolling- circular movements of the fingers in a circular motion, akinesia (loss of voluntary muscle movement. Loss of voluntary muscle movement 2. Rigidity- ↑ resistance to passive motion when the limbs are moved through their range of motion. Cog wheel→ jerky rigidity 3. Bradykinesia- slowness of all voluntary movements & speech; stooped posture (kyphosis), masked faces (difficulty controlling facial movements, can’t catch up, dead pan expression), drooling of saliva→ depression, & shuffling gait; difficulty in initiating movement, uncontrolled backward motion - Secondary S/S: Muscle Weakness (difficulty speaking, slowness of speech, dysphagia- airway & lungs are at risk), GB An acute form of polyneuritis (inflammation of many nerves) that results in a temporary, flaccid paralysis lasting for weeks to months; is reversible; may progress rapidly and become an emergency Usually develops 1-3 wks after upper respiratory or GI infection. Ascending paralysis starts in lower extremities and is symmetrical; paresthesia (numbness & tingling); hypotonia (reduced muscle tone); areflexia (lack of reflexes) facial weakness, extraocular eye movement difficulties, dysphagia, & paresthesia of face Normal CSF protein- 5-45 mg/dL- will be high with GB - hallmark sign- ascending paralysis (to chest), including diaphragm = resp. arrest Avoid Complications * Injury→ FALLS, FALLS, FALLS!! Malnutrition (trouble swallowing) & drooling Impaired Verbal Communication Social Isolation (drooling) -Airway obstruction r/t dysphagia Depression (don’t be afraid to ask) - Assess and Monitor: swallowing difficulties -Encourage independence, encourage assistive devices as needed, -Provide a safe environment Promote sleep and rest -Encourage ROM Assist with ADL/maximize communication -Keep patient physically active, Patient Teaching: - Remove area rugs & excess furniture to avoid stumbling, handrails and ramps at home - Clothing: use slip-on shoes & Velcro hook-&-loop fasteners or zippers instead of buttons & hooks - Maintain activity has much as possible - Taking medications everyday Sinemet- levodopa/carbidopa combination drug; Levodopa crosses the blood-brain barrier and is converted to dopamine while carbidopa that inhibits enzyme break down of dopamine. Side effects of levodopa include nausea, vomiting, and occasional heart rhythm disturbance Be aware of caregiver fatigue-physical and mental health may decline as the disease progresses and stress increases. -Monitor for respiratory failure (most serious complication) r/t paralysis of thoracic nerves- may need intubation. -Treat with immunoglobulin, plasmapheresis -Without tx: total paralysis → ventilator support -Good chance of FULL recovery w/ good care -Patient is fully awake & alert→ no cognitive impairment -Assess for ascending paralysis and ↓cranial nerve function SLE Autoimmune multisystem inflammatory disease (chronic and progressive) that is unpredictable associated with abnormalities of immune system. It affects the skin, joints, serous membranes (pleura, pericardium); renal, hematologic, & neurologic systems. More common in women (childbearing years or post-partum), affects African Americans, Asians, Hispanics, & Native Americans more than Caucasians Unpredictable, alternating periods of exacerbations & remissions. Mostly affects the lining of the lungs, heart, nervous tissue, kidneys, MS & skin Skin- discoid lesions; Butterfly rash on face/cheeks; alopecia, polyarthralgia with morning stiffness; arthritis- Swan neck fingers, weakness, Tachypnea, pleurisy, dysrhythmias, Lupus nephritis (Ranging from mild proteinuria to glomerulonephritis). Primary goal in treatment is slowing the progression of nephropathy & preserve renal function, generalized/focal seizures, peripheral neuropathy; cognitive dysfunction, disorientation, memory deficits, Psychiatric symptoms (depression, mood disorders, anxiety, & psychosis); headaches (exacerbation of disease) Formation of antibodies against blood cells (erythrocytes, leukocytes, thrombocytes, & coagulation factors), Anemia, mild leukopenia, thrombocytopenia, excessive bleeding or blood clot development, Increased susceptibility to infections. Fever should be considered serious. Infections such as pneumonia are a common cause of death. Fatigue & weight loss Nursing Care: - Monitor skin integrity & provide frequent oral care - During exacerbation, patient will become abruptly, dramatically ill. Record severity of symptoms and response to therapy - Observe for fever pattern, Joint inflammation, Limitation of motion, Location and degree of discomfort, Fatigability -Infection (b/c steroids & poor immune) - Strict asepsis, Monitor WBC, protect against infection, adequate nutrition - Monitor for potential GI & renal effects due to NSAIDs (Observe for signs of bleeding from meds- pallor, skin bruising, petechiae, or tarry stools) - Monitor BUN & creatinine levels frequently for signs of renal impairment Patient Teaching: - Reiterate that adherence to treatment does not necessarily halt progression or exacerbations, disease is unpredictable - Minimize exposure to precipitating factors – fatigue, stress, people with infection, sun exposure. Wear SPF loose clothing w/ long sleeves, wide brimmed hats, avoid going outside 10a-3p Report fever, increased fatigue, and/or rash to HCP