Neuroanatomy Study Guide: Motor, Sensory, and Circulatory Systems
advertisement

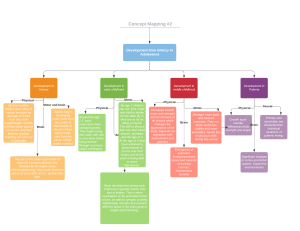
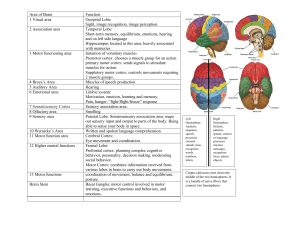
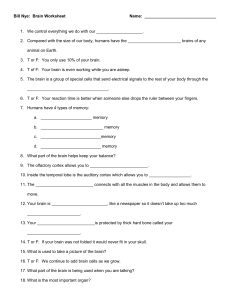
Question extrafusal fibers LMN damage CNI Olfactory stationary blockage diaschisis AVM ipsilateral cerebellar peduncles ataxia, a? tremor, and ? spastic paralysis, hypertonia, hyperreflexia caudate nucleus, putamen, substantia nigra internal carotid artery vertebral artery system circle of willis broca’s aphasia may result in unilateral vocal fold paralysis bilaterally innervated upper face and unilateral lower face posterior cerebral artery sense organ, nerve tracts, cerebral cortex long term memory depolarization What is/are… alpha motor neurons ipsilateral CN damage sensory nerve not on brainstem easily damaged no relay through thalamus thrombotic CVA death of cells at a distance from site of lesion arterial venous malformation causes death in younger patients cause an aneurysm same side LMN cerebellum transfer motor information disorders that result from cerebellar damage symptoms of bilateral UMN damage basal ganglia – gas/brakes for motor mvmt major blood supplier to the brain other system that supplies the brain circle of arteries site of lesion: broca’s area, left frontal lobe X vagus nerve, recurrent branch XII facial nerve upper face has backup lower face is contralateral feeds lateral occipital lobe blockage vision symptoms elements of the sensory system has unlimited capacity neuron cell moves closer to threshold less negative intracellular status neural impulse – depolarization, polarization – put terms in order, but no diagram major things that happen during fetus, embryo, and zygote phases embryonic stem cells, general concept Glossary proprioception homunculus dysarthria apraxia position and movement of our body parts muscle weakness in your mouth trouble getting the muscles of the mouth to move the right way to say words hypotonia decreased muscle tone Module 3: Neural Functioning depolarization polarization hyperpolarization neuron cell grows less negative/more positive (getting closer to threshold) at a particular spot on the neuron's membrane neuron cell grows more negative/less positive at a particular spot on the neuron’s membrane when the membrane potential becomes more negative at a particular spot on the neuron's membrane Module 4: Circulatory System and Mechanism of Injury Carotid Artery System carotid artery system internal carotid artery external carotid artery anterior cerebral artery (ACA) middle cerebral artery distribution supplies 80% of blood to brain anterior common carotid divides into external and internal carotid brings oxygen-rich blood to the brain from the heart splits into anterior, middle, and posterior cerebral arteries brings blood to the facial musculature, forehead, around the oral, nasal, and orbital cavities (the external structures) part of carotid system supplies blood to: - the medial surfaces of the hemispheres of the brain above the corpus callosum (including the motor strip) - posterior frontal lobe, corpus callosum, basal ganglia damage impaired motor function part of carotid system runs along the lateral sulcus supplies blood to: - the lateral, frontal, and temporal lobes - posterior cerebral artery distribution Blood Brain Barrier structure functions Major Imaging Systems Computerized Tomography perisylvian region of the brain (angular gyrus, Broca’s, Wernicke’s, arculate fasciculus) damage aphasia, language impairments part of basilar system supplies blood to: - medial surface of the occipital lobe - lower parts of the temporal lobe - thalamus damage visual deficits, auditory perception deficits and issues with thalamus not necessarily a single structure or physical barrier a combo of a physical barrier + CSF + cerebral capillaries maintains homeostasis prevents toxins from entering the brain lets lipid-soluble through (ethanol, carbs, caffeine) water-soluble is difficult (Na and K) CT-scan series of x-rays taken around a center point and reconstructed to create a 3D image fast and well-tolerated by patients can detect hemorrhages not good at differentiating gray and white matter MRI fMRI EEC PET Module 5: The Motor and Sensory Functions CNS Components of Motor System What are the CNS components motor cortices of the motor system? basal ganglia cerebellum Motor Cortices primary motor cortex located in the precentral gyrus of the frontal lobe the basal ganglia and the cerebellum relay information to the motor cortex through the thalamus motor plans and signals that initiate movement are supplied to the premotor and supplemental motor mostly contralateral some bilateral innervation “motor homunculus” lower 1/3 is dedicated to speech and voice premotor and supplementary motor cortex cortical motor areas that influence movement are all connected to the primary motor cortex via reciprocal connections also receive connections also receive connections from same motor areas in contralateral hemisphere; these areas appear to be the place for initial planning for complex sequences of movement receive info from Broca’s area and association cortex of parietal lobe pass info to primary motor cortex and brainstem and spinal cord bilateral activation initial planning for complex sequences of movement Basal Ganglia basal ganglia in diencephalon a cluster of nuclei located deep within cerebral cortex; 5 components: 3 main nuclei – caudate nucleus, putamen, and globus pallidus; 2 associated nuclei – subthalamic nuclei, substantia nigra they modify motor movements that originate in the motor cortex; refinement of voluntary motor movement before info is transmitted to the brainstem and spinal cord known roles: - regulation of muscle tone - regulation of ongoing movements - inhibiting extraneous motor activity movements (this will be important when we consider some symptoms of diseases such as Parkinsons) - motor learning(these are movements that eventually become automatic, like a golf swing or tying your shoes and are first learned by the motor cortex and then, once they are automatic, are regulated by the basal ganglia) - adjustments to automatic movements such as arm swinging and certain facial expressions effects of damage (lesions) to basal ganglia different types of dyskinesias Basal Ganglia Diseases loss of inhibitory control over motor behaviors - the neurophysiological consequence: since the basal ganglia works as an inhibitory influence over the other motor areas, damage results in DISihibition (it loses inhibitory control over some motor patterns) symptoms: - dyskinesia – involuntary movements - bradykinesia – slow movements - hypokinesia – limited range of mvmt - postural abnormalities - altered muscle tone athetosis – slow involuntary writhing mvmt - occur in sequence - usually accompanied by increased muscle tone - when speech muscles are involved, this can result in a particular kind of dysarthria ballism – violent, forceful flinging mvmt - usually only on one side (unilaterally) - result of damage to subthalamic nucleus chorea – involuntary, rhythmic mvmt - mostly in distal extremities such as facial or oral muscles - can significantly affect swallowing, speech, and voice due to loss of voluntary control over the oral and pharyngeal muscles tremor - most common form - resting – occurs while body is at rest/not working against gravity - action – occurs when body maintains a position against gravity (standing, arm out) - intention/terminal – increase in tremor activity as the body part nears an object *all of these exhibit mvmt disorders (because they affect the basal ganglia) Parkinson’s - destruction of dopamine producing cells (in substantia nigra) - disrupts balance of neurotransmitters ACH resulting in mvmt disorder - some forms are hereditary Huntington’s (Chorea) - degeneration in caudate nucleus - hereditary transmission Wilson’s - degeneration in basal ganglia - accumulation of copper - swallowing and dysarthria - hereditary transmission Cerebellum functions of the cerebellum cerebellar connections to brainstem muscle synergy - coordination - smoothness - cerebellum is responsible for the ongoing monitoring of the movement so that there's accurate coordination of muscle groups - looking at the cerebellum's connections with other parts of the nervous system allows us to identify its specific functions muscle tone - helps to regulate muscle tone so that we're prepared for the upcoming movements range of movement - ROM - helps to regulate and influences range and strength of movement - along with the basal ganglia strength of movement equilibrium - has a role in maintenance of equilibrium - because of its connections with the vestibular system receives extensive sensory input - but is not involved in sensory discrimination or interpretation influences motor function - but when lesioned does not result in paralysis involved in motor learning - by modifying motor activity based on results of movement knows both what the body wants to do and what it is doing (knows intention and results) superior cerebellar peduncle - has the bulk of efferent fibers - output: red nucleus thalamus brainstem (reticular formation) & spinal cord middle cerebellar peduncle - afferent - receives input from brainstem & cortex the structure of the cerebellum and each part’s function Cerebellar Dysfunction ataxia tremors dysdiadochokinesia dysmetria rebound inferior cerebellar peduncle - afferent - input: spinal cord, brainstem, & vestibular system afferent connections (receives from): - motor cortex - spinal cord - brainstem efferent connection (sends to): - thalamus - brainstem (red nucleus) posterior lobe (cerebrocerebellum) - connections to cortex via brainstem & thalamus - for coordination and smoothing (synergy) - lesions result in tension tremors anterior lobe (spinocerebellum) - connections to brainstem & spinal cord - for modifications in muscle tone - lesions result in hypotonia flocculonodular lobe - connections to vestibular system - reflexive equilibrium and balance - lesions impact balance and gait dyscoordinated muscle activity (irregular movements) causes: - hereditary (recessive & dominant forms) - acquired (tumor, stroke, head-injury) symptoms: - ataxic dysarthria – slurred speech - difficulty walking (wide, drunken gait; feet placed farther apart for balance) - disruption of fine motor control (writing, eating, swallowing) - clumsiness - hypotonia action (intention) tremors – during mvmt terminal tremors – worsens as limb approaches target postural tremors – when body/limb is held against gravity awkward performance of rapid alternative movements disruption of rhythmic movements impairment in judging distance to target hypermetria – overshooting the target hypometria – undershooting the target inability of agonist and antagonist muscles to adapt to rapid changes in load disequilibrium E.G. patient pushes against doctors hand, hand is quickly removed, patient’s hand moves beyond point where it would normally stop in an exaggerated fashion unsteady, lurching gait appears drunk exaggerated movements of legs (trying to overcompensate) tendency to fall UMN vs LMN UMN tracts UMN and motor function LMN tracts LMN and motor function UMN damage LMN damage all the corticospinal and corticobulbar tracts contained within the CNS after the message/motor plan is sent out by the pmc and it interacts with the bg and cerebellum, then it travels through the cortical area, through the area of the corona radiata, into the internal capsule as part of the UMN system, then it interfaces with the appropriate motor nuclei on the brainstem and the spinal cord (but we're going to focus on the brainstem) at which point the synapse with the motor nuclei of the various cranial nerves we're talking about LMN... motor neurons in the cranial and spinal nerves second order neurons final common pathway sends the information to the skeletal muscles spastic paralysis (requires bilateral lesion to occur) spastic dysarthria (bilateral lesion) apraxia (unilateral damage) hypertonia hyperreflexia clonus: a sustained jerk Babinski sign - a positive B-sign: when you stroke the bottom of an adult’s foot and their toes go up and out (that’s abnormal) little/no atrophy flaccid paralysis (or weakness) hypotonia hyporeflexia atrophy (of muscles) fasciculations: a wormy movement under the flesh normal reflexes motor unit LMN + group of muscle fiber = motor unit redundancy of innervations - temporal and spatial summation - we are capable of gradation of force (varying amounts of force), this is done through redundancy of innervation - we have 2 ways of handling that: temporal and spatial - temp - inc rate of firing for the motor units increases the force, in some cases we inc force by inc the number of motor units - spatial - ? innervation ratios - limbs, gross motor, 500:1 - larynx, fine motor, 25:1 - number of muscle fibers per axon - helpful to think about student to teacher ratio, 1 teacher to 25 kids = more control Pyramidal and Extrapyramidal Systems gamma loop muscle conditions pyramidal pathways gamma loop = feedback between the alpha motor neurons, extrafusal fibers, and gamma motor neurons/intrafusal fibers (proprioceptive elements, and those innervate and work together to help adjust muscle length and the velocity of muscle movement to help maintain tone and stretch reflex) muscle tone and stretch reflex sensory input to spinal cord and brainstem static postures extrapyramidal system paresis – alpha motor neuron damage paralysis – no input from LMN atrophy – loss of muscle bulk fasciculation – spontaneous motor discharge, sometimes with tongue fibrillation – slow repetitive muscle potentials, not seen with eye, seen through EMGs AKA direct pathway - called this because its made up of cells very much shaped like pyramids with long branched dendrites, making up a lot of the neocerebellar cortex - corticobulbar tract corticospinal tract damage to pyramidal extrapyramidal pathways axons can be 2-3 feet long extending directly into PNS (Golgi Type I), require fewer synapses because they are so long, they have a faster response time voluntary pathways corticobulbar (corticonuclear) – cortex to brainstem corticospinal – cortex to spinal cord originates in multiple cortical areas: - primary motor cortex - primary somatosensory cortex - premotor area - supplementary motor area - parietal association cortex descending pathways - pyramidal fibers descend the corona radiata - converge to pass through the internal capsule this should be exciting to us inverted homunculus 70% of the motor fibers for the entire system synapse with cranial nerve nuclei in brainstem innervates LMN which go on to control muscles of head and neck many originate in lower third of PMC majority of innervation is bilateral (exception = lower face) decussation: anterior surface of medulla (table 6.2 in text) AKA cortico-rubrospinal tract 30% of the motor fibers synapse/interface with interneurons or cell bodies of spinal nerves contralateral and unilateral to cortical origin 90% decussate at caudal medulla - damage above this level results in contralateral symptoms (contralateral to lesion side) - damage below decussation results in ipsilateral symptoms innervates LMN which go on to control upper and lower trunk and limbs after decussation, axons form spinal white matter of the lateral corticospinal tract 10% of corticospinal fibers remained ipsilateral and form anterior corticospinal tract, this tract innervates the trunk unilateral, corticospinal = spastic hemiplegia - characterized by flex extremities (arms, fingers, legs) with the head bent towards affected side bilateral, corticobulbar = pseudobulbar palsy - implications for speech, swallowing, and chewing unilateral, corticobulbar, left hemisphere = apraxia involuntary pathways autonomic nervous system – also includes the cerebellum, red nucleus, basal ganglia, those reticular formations reflex loops involved in coordination, modulation (amplitude & frequency of activation), and regulation (rate of movement, filtering) of movement AKA indirect pathway more subconscious level speed, range, and direction of movement pathways: - basal ganglia loops - reticulospinal tract - tectospinal tract - rubrospinal tract - vestibulospinal tract reticulospinal tract influences muscle tone medial reticulospinal tract: extensor muscles - damage will influence muscle tone, extender and flexor muscles lateral reticulospinal tract: flexor muscles tectospinal tract coordinates head and eye movements vestibulospinal tract balance, equilibrium, reflex adjustments of head rubrospinal tract influences muscle tone facilitates activity in extensor muscles inhibits activity of flexor muscles Components of the Sensory Systems What are the 3 components of the sensory systems? sense organ nerves, nuclei, ganglia, and tracts sense organ nerves, nuclei, ganglia, and tracts cerebral cortex ears, eyes, touch receptors, olfactory bulbs, taste buds transducers – change one form of energy for another; end with neural energy; every sense organ has one respond to specific types of energy transmits the info towards the cerebral cortex first order sensory neurons (1st waystation) - go directly from sense organ in PNS - EX optic nerve - innervate the sense organ, in PNS, ipsilateral second order sensory neurons - projection neurons, located in brainstem or spinal cord, point of decussation, to thalamus - bring info to thalamus third order sensory neurons - project to cerebral cortex from thalamus, ipsilateral, to primary sensory cortex cerebral cortex visual field deficits Auditory System organ neural pathways cerebral cortex auditory deficits each sense has an area of the cc dedicated to its perception and integration primary cortex: somatosensory, auditory, visual, olfactory association cortex: frontal, parietal, temporal, parieto-occipital monocular blindness - damage anterior to optic chiasm tunnel vision - problem is at the optic chiasm - temporal or lateral fields are lost homonymous hemianopsia - loss of half of the visual field (either right or left) cortical blindness - damage to visual cortex - if bilateral, then total blindness visual agnosia - association area is damaged - we can’t recognize object by sight but we can detect that it’s there ear as transducer external ear – collects sound middle ear – impedance matching, air-fluid interface inner ear – cochlea converts fluid vibrations to neural energy VIII Acoustic Nerve primary auditory cortex temporal association cortex conductive hearing loss sensory hearing loss auditory agnosia path of efferent motor info: info from the primary motor cortex down through the cerebral peduncles to brainstem they decussate (cross midline) and enter through the middle cerebellar peduncle to the cerebellum then is processes and further refined as it leaves the superior peduncle and goes back to the tegmentum of the midbrain where the fibers cross back to the original point of origin through the thalamus and then back up to the motor cortex Module 6: Central language Mechanisms and Higher Cortical Functions Unimodal and Multi-Modal Association Cortices unimodal association cortex multimodal association cortex deal with only one kind of sensory information deal with two or more kinds of sensory information (receive projections from several different sensory regions) somatosensory association cortex auditory association cortex visual association cortex parietal association cortex prefrontal area visual association cortex these areas are the largest in humans represent the highest level of cortical development responsible for: - language – receptive comprehension, expression, production - cognition – awareness, perception, reasoning, and judgment - memory – short-term, long-term unimodal sensory: touch and proprioception unimodal sensory: hearing unimodal sensory: visual multimodal location: posterior portion of superior parietal lobule multimodal location: everything outside PMC and premotor area unimodal association Major Components of Central Language Mechanism Perisylvian Region contains areas responsible for language functions: - angular gyrus - association cortices - Broca’s area - Wernicke’s area - arcuate fasciculus (connects Broca’s and Wernicke’s) Wernicke’s area association cortex in left hemisphere (for majority of people) reception of speech many links to limbic system, somatosensory area, visual and auditory areas linguistic concepts of meaning and syntax involved with auditory perception: sound information goes from 8th cranial nerve to inferior colliculus in brainstem to medial geniculate in thalamus up to primary auditory cortex and then to Wernicke's involved with storage and retrieval of mental representation of word meanings, grammar and linguistic rules Broca’s area motor programmer for speech and articulation movements that are to be executed by primary motor cortex Primary motor cortex extends through internal capsule of the brainstem to the spinal cord Angular gyrus integration of visual, auditory, and tactile information for reading and writing Arcuate fasciculus projection fiber that connects Wernicke's to Broca's Supramarginal gyrus hearing and writing Wernicke-Geschwind Model What is it? an early model for understanding how speech is produced in humans What does it seek to explain? a historical model developed to understand the pathway in the brain responsible for auditory and visual cognition and speech responding comprehension and responding to spoken language https://brainstuff.org/blog/what-is-the-wernicke-geschwind-model What does it posit? area of focus type of theory spoken word pathway cognition pathway written word pathway limitations of the model Aphasia Types aphasia Broca’s aphasia certain areas communicate with others in order to extract information about the meanings of words, before that information is passed to the speech production and motor areas of the brain the Perisylvian Region connectivist spoken word area 41 Wernicke’s area (contains sound images of words) hear and comprehend word auditory info goes from ear to primary auditory cortex in the temporal lobe (?), then that coded info is sent to Wernicke’s, then (for motor response) through arcuate fasciculus to Broca’s, to motor cortex Wernicke’s area Broca’s area (stores motor programs for speaking words) facial area of motor cortex cranial nerves speak written word area 17 area 18, 19 angular gyrus Wernicke’s area read visual info goes from eyes to primary visual cortex in the occipital lobe, then to angular gyrus, then to Wernicke’s area, then (to make a motor response) through arcuate fasciculus to Broca’s area, then to motor cortex (which can send an outward motor command) no model explains everything largely outdated due to inconsistencies in human case studies where an injury doesn’t cause the expected deficiency based on the model (on the other hand) sometimes injuries outside of the regions identified in the model can cause various forms of aphasia (the difficulty in speech production) a language disorder that happens when you have brain damage (usually the left hemisphere) may make it hard to understand, speak, read, or write “non-fluent aphasia” may only be able to say three or four words at a time limited vocabulary trouble finding the words they want to use tend to understand speech https://www.aphasia.org/stories/different-types-aphasia/ Wernicke’s aphasia “fluent aphasia” speaking isn’t difficult the problem is that the person isn’t forming coherent words, or those words aren’t coming together into coherent sentences affects reading and writing https://www.aphasia.org/stories/different-types-aphasia/ anomic aphasia can’t find the words they want to use, and this is particularly true for nouns and verbs use synonyms or vague fillers to get around this understand speech and can usually read, but you see the same difficulties with their writing https://www.aphasia.org/stories/different-types-aphasia/ global aphasia the most severe form cannot speak many words sometimes don’t understand speech cannot read or write people may have it for a short period of time following a brain injury or stroke and then move into a different type of aphasia as their brain health improves https://www.aphasia.org/stories/different-types-aphasia/ primary progressive aphasia paraphasia dysphagia Memory Processes and Forms What is cognition? perception attention memory reasoning problem solving What is memory? three processes related to memory sensory memory short-term (working) memory actually a form of dementia where people lose the ability to speak, write, and read over time a gradual loss of language a type of language output error commonly associated with aphasia characterized by the production of unintended syllables, words, or phrases during the effort to speak usually with fluent forms of aphasia swallowing problems the mental functions of an individual which allow them to think, process information, learn, and remember includes: perception, attention, memory, reasoning, problem solving process of attaining awareness and understanding of sensory information ability to selectively concentrate on one aspect of the environment while ignoring others ability to store, retain, and retrieve information a cognitive process of looking for reasons for beliefs, conclusions, actions, or feelings finding a solution to a problem the ability to retain and utilize acquired information or knowledge encoding – formation of a memory trace (temporary recording of knowledge or experience) storage – temporal maintenance of a memory trace recall – reactivating a stored memory for current use 1st level holds stimuli in a raw (sensory) form so that you can register and attend to it 2nd level limited capacity storage of information allows us to hold and manipulate information in real time, as well as call up long-term memory to interact with current memory traces affected by temporal factors if memory trace is not rehearsed, the memory will fade in a matter of minutes long-term memory 3rd level permanent and possible limitless memory store, containing all our knowledge of the world and memories of the past declarative-conscious a type of long-term memory memory episodic – memory of events semantic – memory of knowledge, facts non-declarative a type of long-term memory unconscious memory from classical conditioning context or procedural learning AKA procedural or implicit memory Cortical Areas Involved with Memory frontal association area working memory prefrontal area lesions result in short-term (working memory difficulties) hippocampus for conversion of memory trace to long-term memory (declarative memory) lesions result in amnesia & inability to form new long-term memories episodic & semantic memory amygdala emotional memory (non-declarative memory) memory related to smell and taste episodic & semantic memory parietal lobe non-verbal memory temporal lobe semantic memory basal ganglia non-declarative memory (motor learning) cerebellum non-declarative memory (motor learning) occipital lobe visual memory Major Classifications of Dementia dementia degenerative process of the CNS, affecting older adults diffuse impairment of memory, intellect, and cognition may include behavioral and personality changes as well as physical impairments in the later stages additional characteristics: acquired, gradual onset, persistent, interferes with daily living (ADLs), disorientation, lapses in judgment, difficulty with mentally challenging tasks, misplaced items, apathy and loss of initiative, mood changes cortical (neurodegenerative) Alzheimer’s disease Pick’s disease subcortical PD Huntington’s disease HIV mixed multi-infarct vascular disease associated disorders Wilson’s disease HIV encephalopathy post-traumatic Alzheimer’s disease Pick’s disease (FTD) vascular dementia subcortical dementias Huntington’s disease alcohol-related 50-70% of all dementias 2-3x more likely in females unknown cause neurofibrillary tangles, neuritic plaques, and granulovacuolar degeneration tendencies that we think cause the disease tangles tend to appear in temporal and frontal lobes and hippocampus plaque = anywhere in cortex rano = small fluid filled cavities that contain debris, in the nerve cell, often in hippocampus ALSO... neuronal atrophy - loss of synapses because of plaque and tangles neurochemical deficiency - not enough ACH medical treatment – aimed at symptoms and slowing progression stages – early, mid, and late; memory and orientation are first symptoms speech and language – early: mild word retrieval, occasional paraphasias and subtle comprehension problems; middle: more obvious problems with word retrieval, sentence fragments, topic maintenance; late: severely compromised, non-functional reading/writing, bizarre communication devoid of meaning, unaware of errors, echolalic (repeats what is said to them) rare, 2% of dementia patients frontal lobe pathology ages 40-60 shrinkage of brain, proliferation of glial cells often misdiagnosed as AD and depression some of the key differences… personality and emotions are initial symptoms apathy and indifference social problems obsessional behaviors language and communication breakdown early in disease, memory and orientation remain intact until later progression vascular in nature cortical and subcortical processes CVD/HTN – preventable deficits in memory, cognition and ADL at risk for stroke factors change in basal ganglia, thalamus and brain stem begins with motor symptoms Huntington’s Disease Parkinson’s Disease HIV/AIDs inherited, degenerative Parkinson’s disease HIV/AIDS chorea – movement disorder cognitive decline personality changes, agitation, depression, paranoia, and delusions 1 in 20,000 loss of caudate nucleus, basal ganglia and frontal and temporal lobe ages 40-60, death in 15-20 years medical treatment – antidepressants, antipsychotics speech and language – hyperkinetic dysarthria, dysphasia and memory Michael J Fox age 50-65 years, death 15-20 years post dx (?) deterioration of dopamine production in basal ganglia pill rolling (rubbing fingers together as if there’s a pill between them), tremor, rigidity, impaired gait and balance 15-20% of patients have dementia speech and language – voice, vocabulary, syntax, drooling and swallowing most less than 35 years old 70% encephalopathy leading to dementia in late stages med – slow progression and infections variable development, can be gradual or sudden death because of pneumonia or other infection speech and language – dysarthria Quiz Memory of knowledge/facts semantic; episodic is known as _____ memory; Memory of events is _____ memory. Recall of a movie plot is an declarative, episodic memory example of which type of memory? Which neurological disorder Huntington’s disease is characterized by personality disorder, cognitive decline, and movement disorder? Damage to the cerebellum is procedural (non-declarative) most likely to result in which type of memory impairment? ASCVD and HTN are common vascular dementia causes of which type of dementia? Which category of cortical multi-modal association cortex area is responsible for the highest level of cognitive functioning? Match the term with the possible disorder. perception agnosia memory dementia attention attention deficit disorder problem-solving frontal lobe injury language aphasia Match the type of dementia with the underlying neurological condition. Picks Disease frontal lobe pathology, proliferation of glial cells Alzheimers Disease neurofibrillary plaques and tangles sub-cortical dementias changes to basal ganglia, thalamus Human Immunodeficiency opportunistic infection of the brain Virus Encephalopathy