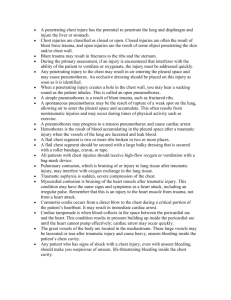
Common therapeutic measures - Deep breathing & coughing Pursed-lip breathing Tripod breathing Accessory muscle use Chest physiotherapy Suctioning Oxygen therapy Mechanical ventilation Airway obstruction - May be complete (medical emergency) or partial Causes: - Aspiration Laryngeal edema Laryngeal or tracheal stenosis - narrowing of the upper airway between the larynx and the trachea CNS depression – poor ventilation = collapse Allergic reaction/ anaphylaxis Pneumonia – too many secretions Broncho/tracheal spasm Symptoms: - Stridor Use of accessory muscles Suprasternal and intercostal retractions Wheezing Tachycardia Cyanosis Tracheostomy Tracheotomy - Surgical incision into the trachea for the purpose of establishing an airway - Tracheostomy is inserted into the tracheal cartilage Indications - To bypass an upper airway obstruction To facilitate removal of secretions To permit long-term mechanical ventilation To permit oral intake and speech in the patient requiring long- term mechanical ventilation - Cancer Trauma (attempted hanging) Long term ventilation – permitting oral intake and speech Pneumonia Quadriplegics Head and neck surgery Complications - NO filtering NO warmth & moisture = more lung infections NO control of when sputum/mucus comes out NO vocalization WHEN CUFF IS INFLATED Cuffed tracheostomy – for patients who require positive pressure ventilation and airway protection Uncuffed tracheostomy – used when patient no longer needs positive pressure ventilation and has no significant aspiration risk Nutrition - Thickened fluids, enteral feeds, Parenteral nutrition Suctioning effects Hypoxia Tissue trauma Infection Vagal stimulation – can cause pulse to drop = syncope Bronchospasm When can the trach be removed (Decannulation) - When the patient is stable and able to breathe on their own When the patient is able to expectorate secretions When the patient’s gag reflex has returned Asthma - Chronic Inflammatory disorder of the airways; reactive airway disease Triggers of asthma attacks: allergens, exercise, respiratory infections, nose and sinus problems, drugs and food additives Signs and Symptoms: o Dyspnea o Productive cough, accessory muscle use, audible wheezes o Tachycardia, tachypnea o Air trapping as a result of bronchospasm o Edema and mucous in bronchioles Nursing Assessments o Hx of exposure to triggers/ allergens o Hx of Asthma o RR and O2 Sat o Accessory muscle use, audible and auscultated wheezing, auscultated deep breathing o Peak flow – maximum speed of expiration; measures airflow through the bronchi and therefore the degree of obstruction to the airways o Assess for severity o Peak Expiratory Flow Rate (PEFR) Interventions: o Administer SAGA; 1 puff every 30 to 60 seconds -> up to 20 puffs o Reassess Q20 Q30 Q60 minutes o Take ABG if severe and not improving Medications o Ipratropium Bromide (Atrovent) – prevents bronchoconstriction o Oral corticosteroids (Prednisone) – Anti-inflammatory o Epinephrine (Ventolin) – Bronchodilator; Increases Heart rate o o Anti-inflammatory drugs: corticosteroids, antileukotrienes, Anti IgE Bronchodilators: B-agonists (Short and long acting) o o Ventolin; short-acting B Agonist – rescue drug Anticholinergic drugs Methylxanthines Chronic Obstructive Pulmonary Disease (COPD) - Characterized by progressive, partially reversible airflow obstruction, systemic manifestations, and increasing frequency and severity of exacerbations Signs and Symptoms o Dyspnea, difficulty breathing, SOB, limitations in activity o Chronic bronchitis and emphysema o Lungs are struggling to expand and contract Causes o Cigarette smoking o Chemicals and dust o Infection o Heredity o Aging Complications o Cor pulmonale o Acute exacerbations of COPD o Acute respiratory failure Management of COPD o Goals: symptom relief and slowing down of disease progression, improve activity tolerance o Smoking cessation o Influenza vaccine o Drug therapy: Bronchodilators, steroid inhalers (Anti-inflammatory) o Pulmonary rehabilitation o Oxygen Therapy Pulmonary Embolism Occlusions can be caused by: o Blood clot o Air embolism (from iv therapy) o Fat embolism o Bacterial Clumps o Amniotic fluid Risk factors o Surgery of pelvis or lower extremities (Dislodging of clots from DVT) o Immobility o Obesity o Estrogen therapy – estrogen increases plasma concentration of clotting factors = more clotting o Clotting abnormalities Signs and Symptoms o Sudden onset difficulty breathing o Chest pain (pleuritic) on INSPIRATION o Palpitations o Tachypnea and tachycardia o Low BP, O2 Sats o Collapse and sudden death Diagnostics o D-dimer – tells us about the presence of a blood clot by detecting fribrinogen o ABG- decreased PaO2 (Partial pressure of oxygen in the blood) due to blocked pulmonary vessels o ECG, CXR, CT o Pulmonary Angiogram Management o Oxygen therapy o Thrombolysis o Anticoagulation o Embolectomy Patient teaching o Maintain and follow medication routine o Maintain health through nutrition and exercise o o o Smoking cessation No birth control – why though? In some women, the estrogen in combination hormonal birth control methods increases the risk of a blood clot in a leg (deep vein thrombosis, or DVT) or a blood clot in a lung (pulmonary embolism, or PE). Immobility/stasis – risk for clot formation Chest Trauma Rib Fractures - Most common with 5th to 9th ribs -> subclavian artery rupture - Manifestations include: pain, tenderness, muscle spasm, bruising Management o Pain control o Promote chest expansion o Nerve Blocks (anesthesia) o DBC o Anti-inflammatory drugs Flail Chest - When two or more adjacent ribs are fractured at 2 or more sites resulting in a free-floating rib (flail) segment - Instability of chest wall Manifestations o Paradoxical Chest movement – when chest wall moves in on inspiration and moves out on expiration; reverse of normal action o Rapid shallow respirations and tachycardia o Lung contusion – lung bruising due to chest trauma o Atelectasis – complete or partial collapse of the entire lung or area of the lung Management o Intubation and sedation (induced coma) o Mechanical ventilation o Humidified O2 o Crystalloid IV fluids o Diuretics for pulmonary contusion (bruising causes an increase in fluid which may lead to pulmonary edema) o Serial CXR, abg, pulse oximetry Hemothorax - Blood in the pleural cavity - Collection of greater than 25mL of blood greatly reduces expansion of lung Manifestations o Chest pain, SOB, Tachycardia, Anxiety, restlessness o Decreased or absent breath sounds of affected side o Asymmetric chest wall movement Management o o o o Objective: stabilize patient, stop bleeding, remove blood from pleural space, and monitor for increased blood loss CXR then Thoracentesis (withdrawal of fluid from test tube) Pain control Check hemoglobin levels (most likely will drop) Pneumothorax - A collection of air in the pleural space Types o Closed – spontaneous, no external wound (intubation, rib puncture, blebs?) o Tension – caused by open or closed pneumothorax ?? huh o Open – chest trauma (gun shot/ knife wounds) Manifestations o Similar to hemothorax o Air expansion on unaffected side only o Asymmetrical chest movement o Absent breath sounds on affected side Signs and symptoms o Chest pain, SOB, tachycardia, anxiety, restlessness Management o Thoracentesis followed by chest tube o Pain control o Pigtail CT with Heimlich valve – a device that may be used with a chest tube to help remove air from spaces around the lungs; a one way valve sensitive to pressure changes; pushes open to remove air from chest and then closes to prevent air from reentering Tension Pneumothorax - When rapid accumulation of air enter but does not leave the pleural space - Causes severe intrapleural high-pressure tension - Leads to a collapsed lung - Requires immediate needle decompression Manifestations o Same as pneumothorax o Obstructive shock (decreased BP, increased pulse and resp) o Mediastinal shift o Subcutaneous emphysema (rice krispy feeling) o Tracheal deviation Management o Immediate thoracentesis (needle decompression) 2nd intercostal space mid clavicular through to pleural space o Immediate chest tube (pleuravac) o Pain control and surgery Open Pneumothorax - Results from chest wound that allows air to move in and out FREELY (life threatening) Manifestations o Same as pneumothorax o Shock-like symptoms o Mediastinal Flutter Management o Requires IMMEDIATE treatment o 1 way valve device Sterile non permeable package of tegaderm attached with tape on 3 sidesallows air out but not back in o Chest tube o Pain control and surgery Pulmonary Contusion - Damage to lung tissues resulting in hemorrhage from capillary damage and localized edema - Causes fluid build up in lungs – interferes with gas exchange Manifestations o SOB, chest pain, hypoxemia, sang-tinged secretions, crackles, wheezing Subcutaneous Emphysema - The presence of gas within the tissue beneath the skin Management – high concentrations of oxygen may help promote REABSORPTION of SC air Chest Tube - Drains inserted into the pleural space to drain air or fluid - Re-establish negative pressure, allowing the lung to fully expand Indications o Trauma o Thoracic surgery (cardiac and lung) o Pleural effusion o Pneumothorax and hemothorax Nursing Roles pre-insertion o Patient teaching o Gather supplies o Baseline VS, H-T assessment o Position patient, semi-fowlers beside table or supine with arms raised Patient sits at side of bed with arms on the table Nursing roles post-insertion o Set and connect to suction o Position and secure drainage system o Apply dressing o Observe amount, color, consistency of dressing Important things to note o Chest tubes use gravity and/ or suction to restore negative pressure and remove air, fluid, or blood from the pleural space o Never irrigate/ never milk Three bottle system 1st Compartment o Collects drainage o If full, replace whole pleuravac system o Vents air to the second compartment 2nd Compartment o H2O seal o Prevents air from re-entering a patient’s pleural space o One way valve o Rises and falls with inspiration and expiration (tidaling) Continuous bubbles – may indicate possible air leak in tubing o Tube is submerged under 2cm of water o Air leaves and then enters 3rd compartment - - Tidaling corresponds with respiration; labored breathing causes more tidaling o No tidaling = tubing may be occluded by a clot or kink, or the. lung may be fully reexpanded Bubbling slight with expiration if pneumothorax or if coughing/sneezing o Intermittent bubbling – pleural space is leaking air – means air is being expelled o Continuous bubbling – indicate air leak in tubing Start at patient 3rd compartment o Tube depth determines suction o Wet suction?