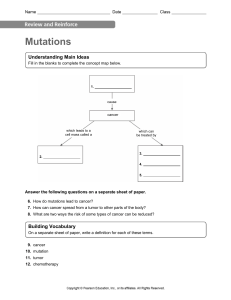
NEOPLASIA CANCER ….. • Affects all age groups • 2nd leading cause of death among children • Estimated 1.66 million newly diagnosed Americans • 580, 350 American deaths • Improved survival rates NEOPLASIA & NEOPLASM • The process of altered cell differentiation and growth • Characterized by uncoordinated growth • Lack normal regulatory controls over cell growth and division Neoplasm • The new growth resulting from the process of process of neoplasia CHARACTERISTICS OF NEOPLASMS Excessive and uncontrolled proliferation • In benign neoplasms: • Well differentiated cells • Cells resemble the normal structure and function of its counterpart • Ability to control cell proliferation is lost • In malignant neoplasms: • No control of cell differentiation or proliferation BENIGN & MALIGNANT NEOPLASMS: CHARACTERISTICS Benign Slow and progressive Malignant Variable and depends of level of differentiation Growth may stop or regress Mostly characterized by rapid growth May compress blood vessels and outgrow blood supply Growth by expansion Invade and infiltrate local tissue Remain localized to site of origin Not surrounded by fibrous capsule- no clearly defined margins Cannot infiltrate, invade, or metastasize Surrounded by fibrous capsule No metastatic capabilities Able to metastasize through invasion of blood and lymph systems TUMOR COMPONENTS • All tumors are composed of 2 types of tissue: – Parenchymal tissue: specific functional cells of an organ or tissue • Made of neoplastic cells • Determine tumor’s behavior • Determine component for which tumor is named – Connective Tissue: forms supporting tissue framework • Includes connective tissue, extracellular mix, and blood vessels • Essential to tumor growth NEOPLASMS - NOMENCLATURE Benign tumors usually are named by adding the suffix – “oma” to the parenchyma tissue type from which the growth originated. E.g. Fibrous tissue - Fibroma Malignant tumors are designated with more than one suffix; “-carcinoma”, “-sarcoma” E.g. Fibroid tissue - Fibrosarcoma Gland like structure - Adenocarcinoma TISSUE TYPES & NAMING MALIGNANT NEOPLASM – CATEGORIES • Solid Tumors – Cancer in situ: localized, pre-invasive state of a tumor – Metastasis: tumor cells spread to distant sites • Hematologic cancers – Cancers of the blood and lymph – Begin as disseminated diseases by nature CELL DIFFERENTIATION Normal • Atrophy: cells become smaller and decrease functionality • Hypertrophy: Increase in size of cell and its functional components • Hyperplasia: increase in number of cells caused by a stimulus which ceases after the stimulus is removed Abnormal • Anaplasia: cells are poorly differentiated or undifferentiated • Pleomorphism: cells and nuclei of tumors display variations in size and shape PLEOMORPHISM • Pleomorphism is a characteristic of malignant neoplastic cells • Cromatin is coarse and clumped • Nuclei are larger than normal • Nuclei have large amount of DNA • Large number of mitoses • Atypical mitotic figures TUMOR GRADING • Based on degree of differentiation and Number of proliferating cells • The better differentiated the cells are, the lower the grade • Scale ranges from Grade I to Grade IV GENETICS AND NEOPLASMS • Normal cells have corrective processes when replicating • Genetic instability: alterations in growth regulatory genes and genes involved in cell cycle progression and arrest • Result in chromosomal abnormalities • Hallmark of cancer cells! • Aneuploid: cells have an abnormal number of chromosomes NEOPLASTIC CELL GROWTH CELL CYCLE – HOW TUMOR GROWS • Rate of growth of tissues depends on: – Number of cells actively dividing – Duration of cell cycle – Number of cells lot relative to number of cells produced • In cancerous tissue, more cells are involved in the cell cycle • Cell cycle times are same for normal and cancerous tissue, but cancerous cells do not die and continue to proliferate. • In cancerous tissue, cells continue to replicate until their growth is limited by a lack of blood supply and/or nutrients CANCER – MODES OF SPREAD • Cancer – Latin Word meaning “Crablike” • Types of Pathways: – Direct invasion and extension – Seeding of cancer cells in body cavities – Metastatic spread • Lymphatic or vascular system CANCER & SURGERY DIRECT INVASION • Malignant tumors – Difficult to completely remove cancer surgically – lack sharp line of demarcation • Benign tumors – Easier to remove completely – Usually encapsulated SEEDING OF CANCER CELLS • Seeding – Occurs when tumor erodes and sheds cells into body cavities – Potential complication during cancer surgery – Causes free cancer cells to enter a cavity unintentionally METASTASIS - OVERVIEW • Defined – Development of secondary tumor in other parts of the body that is distant from the primary tumor • Metastatic Pathways – Lymphatic Spread • Carcinomas – Hematogenous Spread • Sarcomas METASTASIS PROCESS • Break loose from primary tumor • Invade surrounding extracellular matrix • Gain access to a blood vessel • Survives it’s passage to bloodstream • Emerge from blood at favorable location • Invade surrounding tissue to reach distant tissue • Establish blood vessel supply and grow METASTASIS TUMORS – PRIMARY & SECONDARY • Primary Tumors – Can help predict site of metastasis for specific cancers • Secondary or Metastatic Tumors – Usually the same type of cancer – Cellular characteristics of secondary tumor can determine primary site of cancer LYMPHATIC SPREAD • Presence of tumor cells in the lymph nodes • Sentinel Node – Initial lymph node the primary tumor drains to • Example: Breast Cancer – Initial spread is primarily lymphatic HEMATOGENOUS SPREAD • Cancer cells invade blood vessels • Once in the bloodstream cells – Can spread to any part of in the body • Site of Metastasis usually related to – vascular drainage of primary tumor • Most Common Sites – Liver – Lungs METASTASIS TO DISTANT SITES • Prostate Cancer – Spreads to bone • Bronchogenic Cancer – Spreads to adrenals and brain • Neuroblastomas – Spreads to liver and bones METASTATIC PROCESS • Cancer cells must: – Break loose from primary tumor – Degrade extracellular matrix and invade surrounding tissue – Gain access to blood vessel or lymph node – Survive passage and travel to distant site in the body – Emerge at a favorable location to invade distant tissues – Begin to grow in tissue to form a tumor – Establish a blood supply METASTASIS FACTORS • Only a small portion of cancer cells are capable • These cells facilitate the spread of cancer by: – Secreting enzymes to degrade extracellular matrix – Prevent destruction from antitumor cells • tumor emboli – Promoting tumor development • Establish blood supply • Secrete growth factors and other factors that promote – Angiogenesis – Cell proliferation CANCER & GENES PROTO-ONCOGENES • Normal genes that help the cell grow and divide • When functioning properly Good genes. • If mutated ---- bad gene (oncogenes) • Example: – Think of the cell as a car; a gas pedal controls how fast the car goes – A proto-oncogene is the gas pedal of a car; controls rate of cell division/growth CANCER & GENES (CONT’D) ONCOGENES • • • • Associated with gene over-activity Cancer causing; uncontrolled cell division Occurs when proto-oncogenes are mutated Example: – A gas pedal that is stuck down; causes the car to go too fast – An oncogene is a gas pedal that is stuck down; causes uncontrolled cell division CANCER & GENES (CONT’D) Tumor Suppressor Genes (TSG) • Normally TSG are activated – Keeps the cell from dividing too quickly – Example: TSG are the brakes in a car • Inactivated TSG – leads to uncontrolled cell division – Cancers associated with Gene Underactivity – environment for cancer growth GENETIC EVENTS • Mutations – Genetic damage that changes cell’s physiology – Transforms normal cell into a cancer cell – DNA and chromosomal structural changes • Epigenetic Changes – Molecular and cellular mechanisms – change patterns of gene expression without changing DNA – “Silence” or “turned off” genes Website explaining epigenetic changes https://www.whatisepigenetics.com/what-is-epigenetics/ ONCOGENIC GENETIC CHANGES • Cancer causing when activated; increased cell proliferation • Type of Mutations • Point mutation –Insertion, deletion, or substitution of single nucleotide –Example: Ras oncogene • Chromosomal translocation –Example: c-myc gene • Gene Amplification –Multiple copies of gene leads to overexpression –Example: HER-2/neu TUMOR SUPPRESSOR GENES – Cancer causing when gene is inactivated – Leads to uncontrolled cell growth – Mutations • Usually Recessive • Homologous deletion, inactivation, or silencing of genes – Types of TSG examples: • p53 gene – it encodes the tumor suppressor protein p53 • RB (retinoblastoma) gene TUMOR SUPPRESSOR GENES (CONT’D) • P53 Gene “Guardian of the genome” • Assist and induces DNA Repairs • Initiates apoptosis if necessary • Mutations of p53 –Prevents DNA repair and apoptosis –Can occur in any type of cancer • RB Gene • Retinoblastoma; malignant tumor of eye –2 mutations of RB gene lead to tumor TRAILS TO CANCER Genetic and Molecular: • DNA repair mechanisms • Defects in growth factor signaling pathways • Evasion of apoptosis • Development of sustained angiogenesis, invasion, and metastasis • Damage may be a result from multiple risk factors or repeated exposure to single risk factor STAGES OF CANCER • Initiation – Exposure of cells to doses of carcinogenic agents • Induces malignant transformation • Promotion – Induction of unregulated accelerated growth in already initiated cells • Progression – Process where tumor cells acquire malignant phenotypic changes STAGES OF CANCER CANCER CAUSING FACTORS • Causes - multifactorial – Interactions among host and environmental factors • Environmental factors – Chemicals, viruses, microbial, radiation, • Host factors – – – – Heredity Hormones Obesity Immunologic Mechanism HOST FACTORS • Heredity - BRCA 1 & 2 • Genetically linked with Breast Cancer • Associated with increased risk for ovarian, pancreatic, prostate, & colon cancers • Hormonal factors - Endogenous hormones • Associated with cell division in certain cancer types and increases risk • Obesity -Increased risk for breast, endometrial, and prostate cancer • • • • Insulin resistance Increased production of pancreatic insulin Increased levels of sex hormones Chronic inflammation condition HOST FACTORS (CONT’D) • Immunological mechanisms Immune surveillance hypothesis Development of cancer associated with impaired immune system Ex: Kaposi sarcoma and AIDS Immune system components Can specifically recognize cancer cells - Tumor antigens Potential to eradicate cancer cells - preventing cancer cell growth OBESITY & CANCER 3 Possible factors are: Metabolic mechanism • Obesity linked to insulin resistance -Increase insulin-> production of IGF-1 (Insulin growth factor) -Anabolic molecules stimulate cell proliferation and inhibit apoptosis Immunologic mechanism • Chronic inflammation (increased inflammatory cytokines) Increase of sex hormones • Stimulates cell proliferation, inhibits apoptosis, increase chance of malignant cell transformation (e.g. Breast cancer) CANCER GROWTH & PROGRESSION - SUPPRESSION 3 concepts Immune surveillance hypothesis • Cancer development linked to immune system. Individuals with decreased immunity have greater chance of cancer incidence (e.g. HIV-Kaposi sarcoma, Elderly). Immunotherapy • Cancer treatment that increases patient’s immunity, increases tumor destruction Tumor antigens • Antigens on tumor cells that is recognized by immune cells and antibodies TUMOR ANTIGEN DETECTORS All components of the immune system can kill cancer cells T Lymphocytes • Direct killing and activate other components of immune system B Lymphocytes • Antibodies • Kill cancer by antibody dependent cellular toxicity • Complement mediated mechanisms Natural Killer (NK) Cells Macrophages CARCINOGENESIS – DIRECT ACTING AGENTS Binds with free radicals causes cell mutation or disrupt protein synthesis that alters cell replication/regulatory controls Direct acting agents • • • • • No activation required – can just become carcinogenic Direct acting alkylating agents: e.g. anticancer drugs Nitrosamines formed in food that are smoked, fried, grilled, charcoaled. Polycyclic aroma carbons tobacco smoke, animal fat in broiled smoked meat. Asbestos, insecticides, chromium, nickel, certain metals. CARCINOGENS - INDIRECT-ACTING AGENTS Indirect acting agents (procarcinogens/initiators) • Become active after metabolic conversion • High fat diet-increase bile acids->secondary bile acids in presence of anaerobic bacteria of colon->carcinogens or promoters • Alcohol-metabolite acetaldehyde alters DNA synthesis can cause mutation in cells CARCINOGENESIS – IONIZING & UV RADIATIONS Ionizing radiation • Related to dose of radiation, sex, age of exposure: Leads to • • • • chromosomal breakage Translocations Point mutations Example: in utero exposure -> ionizing radiations, industrial workers etc. leukemia and childhood cancer related to exposure to ionizing radiations. • UV radiations - Low energy rays emitted by the sun - not deeply penetrate skin • Effects are additive, more exposure, more chances • Delay in cancer detection CARCINOGENESIS - ROLE OF VIRUS • Human papilloma virus (HPV) • Some types cause benign warts • Some types such as 16, 18, 33,35 etc. cause squamous cell carcinoma of cervix, pharynx, and anogenital area • Vaccine available against 9 types HPV viruses – 7 of them HR types • Epstein-Barr virus (EBV) • Burkitt lymphoma-tumor of B lymphocytes caused by EBV – issue in immunocompromised individuals • HepB Virus – Liver cancer • Human herpes virus 8 (HHV-8) - cause Kaposi sarcoma in AIDS CARCINOGENESIS - BACTERIA • Helicobacter pylori (H. Pylori) – Associated with gastric adenocarcinoma and gastric lymphomas • Due to chronic inflammation and atrophy of stomach lining LOCAL EFFECTS OF CANCER COMPRESSION & EFFUSION - Impairs normal function of local sites Compression Growth causes compression of surrounding body structures • Abdominal cancer abdominal cavity compress = bowel obstruction • Blood Vessel Ischemia and necrosis, bleeding Effusion (fluid) build up Impaired lymphatic circulation/serous exudate • Pleural effusion chest pain, shortness of breath, cough • Ascites abdominal discomfort, swelling (e.g. ovarian cancer) SYSTEMIC EFFECTS OF CANCER Anemia • • • • Due to blood loss Treatment effects iron deficiency-iron metabolism dysregulation, Impaired red blood cell production bone marrow failure Hemolysis Cancer anorexia • Cachexia syndrome- wasting away due to cytokines • TNF- alpha secreted by macrophages in response to tumors influences 5-HT (serotonin) levels and function – anorexia Cancer related fatigue • Fatigue not relieved by sleep or rest Sleep disturbances • Serotonin levels/ regulation is needed for sleep cycle SYSTEMIC EFFECTS – PARANEOPLASTIC SYNDROME PROBLEMS IN THE BODY NOT DIRECTLY RELATED TO TUMOR OR METASTASIS Endocrine complications: • Most cells of body have biochemical pathways to release or make peptide hormones - but do not express it - tumors express this function • SIADH, Cushing Syndrome, Hypercalcemia Hematological complications • Tumor produce procoagulation factors venous thrombosis, thrombotic endocarditis Neurological Complications • Myasthenia gravis - Eaton Lambert syndrome secondary to small cell lung cancer Dermatologic Complications • Acanthosis nigricans - associated with gastric carcinoma SCREENING METHODS – BENEFITS & LIMITATIONS Benefits • Prevention method, early recognition leads to better outcomes ( Mammography/ Breast self exam) Limitations • No reliable screening for early detection when cancer is still small, before metastasis DIAGNOSING CANCER – TUMOR MARKERS • Tumor markers-used for screening/prognosis once malignancy is established; monitor treatment. • Indicates if more aggressive treatment is needed • Examples of tumor markers hCG- hormone produced in placenta dx gestational trophoblastic tumors PSA- produced by prostate - prostate cancer CA-125 - ovarian cancer Alpha-fetoprotein-found in fetal yolk sac and GI structures fetus liver cancer, germ cell cancer of testes CEA (carcinoembryonic antigen) - found in embryonic tissues – colorectal, pancreas, lung, stomach CD blood cell antigens on leukocytes - leukemia and lymphomas • Limitations of tumor markers: Levels not elevated in early stages; all markers are often high in benign tumors DIAGNOSING CANCER – CYTOLOGY & BIOPSY (CONT’D) • Cytologic studies Pap smear - cervical cancer Cells from body secretions (nipple drainage, pleural/peritoneal fluid, and gastric washings) - Detects abnormal cells that lack intracellular structure of normal cells, cancer cells exfoliate and mix with secretions where it grows • Tissue biopsy-remove tissue and study under microscope Fine needle biopsy- palpable lesions (breast, thyroid, lymph, pancreas) Endoscopy – body cavities (bronchoscopy/cystoscopy), laparoscopy Excision biopsy- remove whole tumor and pathologist can look at nature of mass or margins to determine if whole tumor was removed DIAGNOSING CANCER – OTHER METHODS (CONT’D) • Immunohistochemistry- monoclonal antibodies • Can detect tissue specific or organ specific antigens to find the site of origin • Detects molecules that are of prognostic or diagnostic importance such as estrogen receptors on breast cancer cell (useful in anti estrogen therapy) • Microarray technology- analyzes and quantifies expression of large number of genes • • • • • Determines overall patterns of behavior Used for prognosis Identify tumor type Examines changes to tumor cell after therapy Classify hereditary tumors CANCER – GRADING & STAGING • Grading- scale I, II, III, and IV Cellular examination of tumor cells to see what level of differentiation compared to normal cells I- well differenced to IV (very differentiated) • Staging- Find out where the tumor has spread: surgery, CT, MRI Size of primary tumor Local growth (inside or outside of organ) Lymph node involvement Distant Metastasis 2 METHODS TNM system (T-Tumor size T1,T2,T3,T4; N - regional lymph node involvement N0, N1, N2,N3; M-metastasis M0, M1. AJC (American Joint Committee) system - Stages 0, I, II, III, IV CANCER - TREATMENT CANCER Rx - GOALS • Three major goals of cancer treatment • Curative • Control • Palliative CANCER SURGERY USES • • • • Diagnosis Staging of cancer Tumor removal Palliation (i.e. relief of symptoms) when a cure cannot be achieved TYPES - Determined by • • • • • Extent of disease Location and structures involved Tumor growth rate and invasiveness Surgical risk to the patient Quality of life the patient will experience after the surgery RADIATION THERAPY Uses • • • • • A Primary treatment method for cancer Pre/post-operative Rx (with or w/o chemo & surgery) Palliative treatment to reduce symptoms with advanced cancers Reduce pain associated with bone metastasis Oncologic emergency Rx (spinal cord compression, bronchial obstruction, & hemorrhage) Types • External beam or teletherapy - Linear accelerator or cobalt-60 beams aimed at tumor • Bradytherapy - Sealed radioactive source is placed close to or directly in the tumor site • Systemic therapy - Radioisotopes with a short half life are given PO or injected into the tumor site. Beneficial effects – How? • Radiation Injures rapidly proliferating and poorly differentiated cells than normal tissues Harmful effects – How? • Radiation damages all rapidly proliferating cells. • This means cells of the bone marrow and mucosal lining of the GI tract are frequently damaged CHEMOTHERAPY • Chemotherapy is a major systemic cancer treatment modality • Only treatment form that enables drugs to reach tumor site and distant sites. • Uses • Primary treatment form or part of multimodal treatment plan • Most hematologic and some solid tumors CHEMOTHERAPY (CONT’D) Mechanism of beneficial effects • More toxic to rapidly proliferating cells than cells incapable of replicating or in G0 phase of cell cycle. Mechanism of harmful effects • Chemo drugs are toxic to all cells. • Also attack rapidly proliferating cells of normal tissue • Side effects - Most common: anorexia, nausea, and vomiting, as well as alopecia. Acute (few days post chemo), Intermediate (few weeks) Long term (months to years) DRUGS & CELL CYCLE • Cell cycle-specific drugs Drugs that exert their action during a specific phase of the cell cycle Methotrexate- interferes with DNA synthesis- disrupts S phase of cell cycle • Cell cycle-nonspecific drugs Drugs that exert their effects throughout all phases of cell cycle Alkylating agents- disrupting DNA when cells are dividing and in resting state MULTIMODAL TREATMENT • Treatment plans more than one type of therapy better prognosis. • Making use of varying : • • • • • Mechanisms of action, Metabolic pathways Times of onset of action and recovery, s Side effects Combinations of drugs and treatments are often more effective • Increasing the life expectancy some types of cancer. HORMONE THERAPY • Hormone therapy Administration of drugs used to deprive cancer cells of hormonal signals that otherwise would stimulate them to divide Used for cancers that are responsive to or dependent on hormones for growth. • Breast, prostate, and endometrial cancer. • Antihormone therapy Antihormone drugs are exogenous hormones that alter hormone receptor function • Bind to hormone receptors making them inaccessible to hormone stimulation. E.g. Prostate cancer – antiandrogen therapy; breast cancer – antiestrogen therapy BIOTHERAPY • Biotherapy - uses immunotherapy and biologic response modifiers to change a person’s immune response and modify tumor cell biology • Monoclonal antibodies Developed antibodies directed against tumor specific antigens as well as signaling molecules. • Adjuvants Cancer treatment used after surgical intervention. E.g. Bacillus calmette-guerin (BCG) • Attenuated strain of the bacterium that causes Bovine Tuberculosis. • Treat noninvasive bladder cancer after surgical ablation • BCG acts locally to stimulate an immune response- reduces relapse rate. BIOTHERAPY (CONT’D) • Cytokines Mediators of acute and chronic phase reactions Systemic inflammatory response to insults of the body such as viral illnesses and neoplastic processes. In cancer treatment, • IL-2 may also promote CD8+ and natural killer cell activity (NK). • It also promotes differentiation of CD4+ cells into T helper subclasses. • IL-2 a cytokine has been used in high doses to successfully to stimulate an immune response, and achieve an objective response in the treatment of patients with melanoma and Renal cell cancer (RCC) GOAL OF TARGETED THERAPY: • Selectively attack malignant cells while leaving normal cells unharmed. • The first targeted therapies were monoclonal antibodies. • Research working on drugs that can disrupt molecular signaling pathways such as those that use the protein tyrosine kinases. To learn more about monoclonal antibodies: https://www.cancer.org/treatment/treatments-and-side-effects/treatmenttypes/immunotherapy/monoclonal-antibodies.html CHILDHOOD CANCERS • Cancer is the leading cause of disease related deaths among children between age 1-14 in the US • Common types of cancers during childhood stages 0 - 2 years of life (embryonal tumors) • Neuroblastoma • Retinoblastoma • Wilms tumor 2 – 5 years • Acute lymphocytic leukemia has a peak incidence in children 2 to 5yrs of age. Puberty & Adolescence Bone malignancies Lymphoma Thyroid cancer Malignant melanoma Gonadal germ cell tumors Testicular and ovarian carcinoma CHILDHOOD CANCERS – CAUSES, S/S CAUSES - No one cause of childhood cancer • A number of genetic conditions are associated with childhood cancer (although relatively rare) Ex. Down syndrome Genetic susceptibility + environmental exposures SIGNS AND SYMPTOMS - No early warning signs or screening tests • • • • • Prolonged fever Unexplained weight loss Persistent lymphadenopathy Growing mass (Especially with weight loss) Abnormalities of central nervous system function CHILDHOOD CANCERS – DIAGNOSIS & Rx Diagnosis Early detection is imperative because many childhood cancers are curable • Minimizes amount and duration of treatment for cure Treatments of childhood cancers Complex and continuously evolving Multidisciplinary and multimodal therapy Chemotherapy most common, followed by surgery, then radiotherapy, and then biologic agent therapy LONG TERM EFFECTS OF Rx REFERENCES 1. Porth, C.M. (2015). Essentials of Pathophysiology: Concepts of Altered States (4th Edn), Philadelphia, PA, Wolters Kluwer. 2. Kumar,V., Abbas, A.K. (2013). Robbin’s Basic Pathology (9th Edn), Philadelphia, PA, Elsevier Saunders.