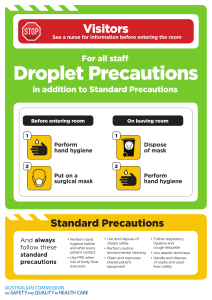
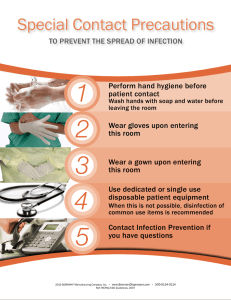
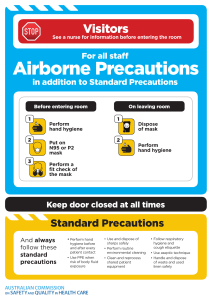
Infection Control and Prevention/Asepsis (Chapter 24) Chain of Infection o Transmission occurs when the agent leaves its reservoir or host through a portal of exit, is conveyed by some mode of transmission, and enters through an appropriate portal of entry to infect a susceptible host. Infectious Agent – microorganisms (bacteria, virus, fungi, protozoa) Presence of pathogen does not mean infection will occur Not all organisms produce disease Reservoir – natural habitat of the organism Animals, soil, water, food, objects Carriers – organism present without symptoms Portal of exit – point of escape for the organism Integumentary, respiratory, GI, Genitourinary Mode of transmission direct contact – close contact indirect contact – vector or fomite Droplet – larger particles, coughing, sneezing, talking airborne route – smaller particles, travel in air Portal of entry – point at which organism enters a new host Integumentary, respiratory, GI, Genitourinary Susceptible host – organism overcomes their defense mechanisms How to break chain of infection o Major mode of transmission is the unwashed hands of the health care worker o Hand Hygiene – including keeping nails short and not wearing acrylics o Identification of signs of infection (redness, swelling, tenderness, heat, pain) o Cleansing and technique in the care of the patient o Infection control measures (isolation, visitors, equipment) o Promote sleep, nutrition and stress reduction Risk factors for infection o Impaired skin integrity o o o o o Abnormal pH levels of GI and GU systems Decreased function of WBC Lack of immunization (natural or acquired) Bad nutrition, illness, stress Age - decreased cough reflex, abnormal swallowing reflexes, incomplete emptying of bladder, thinner epidermis o Implanted devices (foreign bodies) Hand hygiene o Before: Contact with client Moving from a contaminated body site to a clean site Invasive procedures Caring for immunosuppressed patient o After Contact with client Contact with client’s skin Contact with body fluids Contact with contaminated inanimate objects from client Removing gloves o Alcohol Rub Before and after client contact Contact with body fluid, wounds, dressing - if NOT visibly soiled o Soap Hands are visibly soiled Contact with patient with C. Difficile After using restroom Before eating Isolation Precautions o PPE (Personal Protective Equipment) Gloves – when there is possibility of soiling hands Do not eliminate need for hand hygiene Never leave patient room wearing used gloves Gowns – prevent soling of clothes with blood/body fluids Mask – prevent inhalation of aerosols and particles Goggles/face shield – when there is a risk of contaminating eyes o Precautions Standard – gloves, eyewear if possibility of plashing Contact – private room, gown, gloves, dedicated equipment Airborne – private room, respirator mask, negative air pressure room, door remains closed Droplet – private room, gown, gloves, mask, door can be open Transmission-Based Precautions (Tier Two) for Use with Specific Types of Patients CATEGORY Airborne precautions (droplet smaller than 5 microns) INFECTION/CONDITION Measles, chickenpox (varicella), varicella zoster, pulmonary or laryngeal tuberculosis BARRIER PROTECTION Private room, negative-pressure airflow (HEPA) filtration; mask or respiratory protection device, N95 respirator (depending on condition) Droplet precautions Diphtheria (pharyngeal), rubella, Private room or cohort patients; mask or (droplets larger than 5 streptococcal pharyngitis, pneumonia respirator required (depending on microns; being within or scarlet fever in infants and young condition) (refer to agency policy) 3 feet of the patient) children, pertussis, mumps, Mycoplasma pneumonia, meningococcal pneumonia or sepsis, pneumonic plague Contact precautions (direct patient or environmental contact) Protective environment Colonization or infection with Private room or cohort patients (see multidrug-resistant organisms such as agency policy), gloves, gowns VRE and MRSA, C. difficile, shigella, and other enteric pathogens; major wound infections; herpes simplex; scabies; varicella zoster (disseminated); respiratory syncytial virus in infants, young children or immunocompromised adults Allogeneic hematopoietic stem cell transplants Private room; positive airflow HEPA filtration for incoming air; mask to be worn by patient when out of room during times of construction in area Medical Asepsis – clean technique, reduces the transfer of pathogens o Hand hygiene/ PPE / Clean gloves o Single use items or patient specific o Used with wounds that are not surgical Surgical Asepsis – sterile technique, no microbes, or spores a. Used in procedures that introduce a foreign body into a patient i. Catheter, central line, dressing change 1. Only sterile items can touch another sterile item 2. Open packages away from you 3. Outside packaging is not sterile 4. Avoid spilling or moisture, a wet field is NOT sterile 5. Hold sterile objects above the weight 6. Keep sterile field in sight 7. Do not reach over the sterile field 8. Outer one inch of sterile field is considered contaminated 9. When in doubt consider contaminated Principles of Sterile glove downing Patient Teaching o Wash hands before preparing food and before eating o Prepare foods at temperatures high enough to ensure that they are safe to eat o Wash hands, cutting boards, and utensils with hot, soapy water before and after handling raw poultry and meat o Keep foods refrigerated, especially those containing mayonnaise o Wash raw fruits and vegetables before serving them o Use pasteurized milk and fruit juices o Wash hands after using the bathroom o Use individual personal care items, such as washcloths, towels, and toothbrushes, rather than sharing Hygiene (Chapter 31) Factors that affect hygiene o Culture o Socioeconomic class o Spiritual practices o Developmental level o Health state o Personal preferences Nursing measures to implement hygiene o respect the patient’s personal preferences o encourage as much self-care as the patient can perform o implement interventions to meet the patient’s need for privacy o Promote physiologic and psychological wellness. Principles of Hygiene o Oral care Provide the needed supplies Be mindful of patients that are NPO or poor intake Swallowing difficulties can use suction swab o Denture care be careful where they are left. Towel in sink can prevent breaks if dropped. Label container and be sure patient is removing at night. When left in long periods routinely, can impact the fitting. Store in cool water of denture cleansing product. Cool water to wash dentures to avoid warping material o Shaving – ask first If risk of bleeding do NOT use razor, use electric razor o Perineal care – Provide privacy & explain procedure before starting Last area to be completed in bed bath Front to back or least contaminated area to most. Use clean portion of wash cloth with each swipe or use disposable cloth. Male uncircumcised- retract foreskin when washing and pull back when finished to prevent constriction o Bed Bath patients are not on bed rest but require total or partial assistance with bathing in bed due to physical limitations, such as fatigue or limited range of motion. Complete – nurse performs the entire bath Partial – patient can help assist you Safety interventions during bed bath/care o Bed locked o Raised up to nurse’s waist o Side rails up as appropriate Activity/ Mobility (Chapter 33) Planning Exercise programs based on patient condition o Patient without mobility problems, Identify personal benefits of regular exercise List support systems that will reinforce exercise efforts Follow a program of regular physical exercise that improves cardiovascular function, endurance, flexibility, and strength o Patients at high risk for specific mobility problems Demonstrate correct body alignment whenever observed (alignment) Demonstrate full range of joint motion (joint mobility) Demonstrate adequate muscle mass, tone, and strength to perform functional ADLs (muscle mass, tone, strength) o Patients who are immobile Be free from alterations in skin integrity Show signs of adequate venous return Be free of contractures Performing Range of Motion exercises o Passive - patient is unable to move independently, and the nurse moves each joint through its range of motion o Active - patient independently moves joints through their full range of motion (isotonic exercise) Body Mechanics – coordinated use of body parts to produce and maintain equilibrium Types of exercises o Isotonic exercise: active movement such as doing ADLs, independent ROM, walking o Isometric exercise: muscle contraction without shortening as holding a yoga pose o Isokinetic exercise: muscle contraction with resistance such as lifting weights o Aerobic- muscle movement that increases heart rate & blood flow, Cardiovascular conditioning o Stretching- movement that stretches gently through ROM. Increases ROM, improves circulation, posture o Strength and endurance- muscle building such as weight training Positioning patients safely in bed o Fowler’s: Head of bed (HOB) 45-60 degrees. Promotes cardiac & respiratory function. Buttocks, heals, sacrum, scapula bear weight & risk skin breakdown o High Fowler’s: HOB 90 degrees o Semi Fowler’s: HOB 30 degrees o Supine: lying on back o Lateral: side lying o Sims’: lying on side lower arm behind patient and upper arm is flexed at shoulder and elbow o Prone: lying on abdomen with head turned to side Risk for immobility o Contractures o Skin breakdown o Assessments Braden scale – lower number higher risk for pressure ulcer Assistive Devices for immobile patients Safety (Chapter 27) Behaviors that may indicate need for restraint o Last resort, only used protect the safety of the patient, staff, or others. o Medical – assess every 1hr Check for circulation, mobility, sensation Check 2 fingers o Behavioral – check every 15 mins Check circulation, mobility, sensation Check 2 fingers Restraint alternatives o Assess for causes of the agitation (respiratory, vitals, pain, glucose, labs, medications) o Frequent toileting o Offer beverages o Reduce noise, lighting, stimulation o Calm, simple, and clear directions o Distraction and redirection o Diversional activities- games, books, conversation o Tubing out of reach o Alarm systems o Allow for mobility/walking if restless o Low height beds (long term care), floor mats o Hearing aids, glasses in use o Pillows for positioning o Use of music, therapeutic touch o Temperature of surroundings How to manage Fall Risk Patients o Risk factors for falls >65yo history of falls lower body weakness poor vision gait or balance issues postural dizziness problems w feet or shoes use of psychoactive medications hazards in the home o Preventing falls Complete a risk assessment. Indicate risk for falling on patient’s door and chart. Keep bed in low position. Keep wheels on bed and wheelchair locked. Leave call bell within patient’s reach. Instruct patient regarding use of call bell. Answer call bells promptly. Leave a night light on. Eliminate all physical hazards in the room (clutter, wet areas on the floor). Provide nonskid footwear. Leave water, tissues, bedpan/urinal within patient’s reach. Move bedside commode out of sight to discourage attempts at independent transfer (as appropriate). Document and report any changes in patient’s cognitive status to the health care team at the change of shift. Use alternative strategies, when necessary, instead of restraints. As a last resort, use the least restrictive restraint according to facility policy. If restraint is applied, assess patient at the required intervals. o Post fall assessment/nursing care stay w patient assess for injuries DO NOT immediately move patient unless they have been assessed for injury call for help and notify the provider based on fall they may need CT scan or another diagnostic workup prevention: team huddles + fall alert systems Fall Risk tools - high score is bad: means they are more likely for a fall o Morse – rapid simple 6 variables o Hendrich Tools - evaluates eight independent risk factors. Seizure Precautions o Bed in lowest position with padded side rails o Mat on floor if possible o Ensure oxygen is set up and suction set up in place o Loose clothing Moving Patients o Assessments – mobility and strength Determine assistance/equipment required o Planning communicate clearly think about its determine assistance raise side rail on opposite side of bed arrange equipment evaluate body alignment understand equipment educate patient, as always