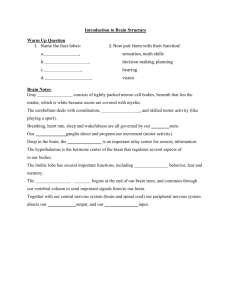
At the completion of this lesson, the student will be able to: 1. Review the functions of the central and peripheral nervous system. 2. Explain the purpose of the reflex arc. 3. Relate the name and function of the 12 cranial nerves. Learning Objectives 4. Discuss the developmental considerations of the infant and aging adult. 5. Describe subjective data used during the neurological exam. 6. Describe tests used on the 12 cranial nerves, deep tendon reflexes (DTR's) ,cerebellar and sensory function. 7. Recognize the 10 warning signs of Alzheimer Disease. 8. Recognize abnormalities in muscle tone and movement. 9. Differentiate between ischemic and hemorrhagic stroke. • Receive external and internal sensory stimulation from the environment such as: hearing, vision, taste, smell, pain, and touch Structure & Function: Nervous System • Allows for the integration of information to be processed by thinking, reasoning, and remembering (e.g., our personality, consciousness, learning and memorizing ability) • Assists with body movements of the skeletal muscles by nerve impulses that stimulate contraction • Works with the endocrine system to regulate and maintain homeostasis Central Nervous System • Includes the spinal cord/brain and carries motor (efferent) messages out towards the muscles/glands of the body • Cerebral Cortex “Cerebrum”: gray matter that surrounds outer layer of nerve cell bodies. Governs thought, memory, reasoning, sensation, and voluntary movements. • Each Hemisphere is divided into right/left and is further divided into four lobes (frontal, parietal, occipital, temporal) Wernicke’s center (temporal): speech interpretation and language comprehension has no meaning Broca’s center (frontal): motor control of speech unable to talk, but understands language Anatomy Info. (2021). Occipital Lobe: Anatomy, Location, and Function. Retrieved fromhttps://anatomyinfo.com/occipital-lobe-function/ Parietal lobe Occipital lobe Frontal lobe Temporal lobe Sensory area (touch, pain, pressure, and temp.) Focus of the eye motor control of voluntary muscles Control of speech production, Social behavior Hearing, taste, smell fx Integration site for visual perception Visual recognition Personality, concentration, organization, and problem solving “cognitive skills”, reasoning, planning, judgement Process language That is heard (speech perception) Helps form memories Control center for emotions Recall of tasks Language skills • Brain stem-[between the thalamus and spinal cord] *lowest area that connects the brain and spinal cord* Regulates unconscious body functions (HR, Breathing, BP, and swallowing by the medulla) Contains cranial nerves III-XII [midbrain, pons, medulla] Central Nervous System • **Cerebellum- [under the cerebrum and behind brainstem] Contains major motor/sensory pathways, helps maintain equilibrium, helps with skeletal muscle coordination, body posture, and balance. • Thalamus-relay station for sensory impulses to the cerebral cortex and information for movement is processed here ; olfactory stimuli only sense that bypasses this region • Hypothalamus- [below the thalamus] Regulates homeostasis and regulates functions (e.g., hunger, anger, response to pain, body temp., pituitary gland to generate responses in the body, and water balance) • Carries sensory (afferent) messages to the CNS via nerve bundle fibers outside the CNS • reflex arc-simplest nerve pathways that bypass brain and controlled by spinal cord via synapse Peripheral Nervous System enters and exits at same level of spinal cord d/t autonomic nervous response without conscious thought of the stimulus allowing quick reaction to painful or damaging situations Ex: Knee jerk (patellar tendon reflex) Stimulus is the hammer and response is the muscle contracting To allow the knee to jerk and move foot upward Cell bodies on posterior horn of spinal cord= relay information Cell bodies in anterior horn= for voluntary or reflex motor activity Types of Reflexes :automatic movement (quick response) that protects the body and help w/balance and muscle tone Peripheral Nervous System: Reflexes 1) Deep tendon reflexes: involuntary contractions of a muscle after brief stretching caused by tendon percussion (e.g., patellar reflex) 2) Superficial (cutaneous) reflexes: withdrawal reflexes caused by noxious/tactile stimulation of the skin, cornea, and mucous membranes (e.g., plantar flexion) 3) Visceral (Organic) reflexes: (e.g., pupillary response to light and accommodation) *Primitive reflexes: abnormal in adults but normal in infants (whose central nervous system is immature) (e.g., sucking, rooting, moro, stepping/walking, Babinski, etc.) Peripheral Nervous System: Reflexes 2) Autonomic Nervous System: Controls glands and involuntary body functions (i.e. internal organs, blood vessels, smooth and cardiac muscle activity & glandular epithelial tissue) comprised of the following subdivisions: Peripheral Nervous System: Spinal Nerves Sympathetic “STRESS”: functions mainly during stress, triggers the fight-or-flight response (HR & RR increase [adrenal glands secrete adrenaline]; cold, sweaty palms; and pupil dilation, and slows digestion) Parasympathetic “PEACE”: Returns body to normal after a stressful situation and maintains normal body functions (i.e. Decreases HR/RR [adrenal glands stop secreting adrenaline], pupils constrict, digestion back to normal) **When one system stimulates a smooth muscle to contract or a gland to secrete→ then the other system inhibits (prevents) the action to keep the body in homeostasis** Four Directions of Wellness. (2016). How Do Healing Modalities Work? Your Autonomic Nervous System Explained. Retrieved from https://fourdirectionswellness.com/2016/10/18/healing-modalities-work-autonomic-nervous-systemexplained/ • Motor activity in newborn under the control of the spinal cord & Medulla Developmental Considerations : Infant • Neurons not yet myelinated and slowly begin to develop to aid in impulse conduction. The process follows the cephalocaudal and proximodistal order, therefore achieving milestones as the infant grows. • Movements are directed primarily by primitive reflexes; as cerebral cortex develops during the 1st year; it begins to inhibit these reflexes (e.g. Moro reflex- startle infant w/loud noise and note positioning seen up until 4 mths age) ** If the newborn displays high-pitched, shrill cry “cat screech” sound d/t CNS damage and should be referred for further testing as this is significant of behavioral change** Developmental Considerations : Aging • Brain cells and neurons begin to atrophy/decrease after the age of 50 • Hypothalamus less effective in thermoregulation • Nerve transmission begins to decrease in response to external stimulation (touch and pain sensation, taste, and smell diminish) • Nerve cells, cerebral blood flow, and metabolism begin to decrease Developmental Considerations : Aging • Slower reflexes, delayed responses, and changes in balance (decreased muscle strength/agility = increased risk of falls • Muscle Tremors may occur in hands, head, jaw→ repetitive facial grimacing=dyskinesia • Sleep pattern changes (i.e., insomnia, more naps in the day, and wake up earlier in the day) • Memory begins to decline (dementia, Alzheimer's, etc.) **Review Table 24.1 (p.670)** Kabb Law Team. (2019, June 27). 10 Warning signs and symptoms of Alzheimer’s. https://www.kabblaw.com/blog/10-warning-signs-and-symptoms-of-alzheimers/ • Any unusual frequent or severe headaches (HA)? Use your PQRST attribute of a symptom to elicit more information. **If states worst HA of my life→ Emergency referral Stat Subjective Data: • Ever had a head injury? Concussion-direct blow that causes rotation of the brain inside the skull and shear injury • Ever felt light-headed or faint? Syncope-temporary loss of consciousness “faint” d/t lack of cerebral blood flow (e.g orthostatic hypotension) Vertigo-rotational spinning d/t neurological disease of vestibular apparatus of the ear (e.g. Meniere’s) Subjective Data: • Ever had convulsions (seizures)? Altered LOC, involuntary muscle movements, and sensory disturbances. **Ask if they have any warning signs prior to a seizure “aura” (subjective sensation that could be auditory, visual, or motor). Are there any associated signs (loss of consciousness, color change on skin, automatism (eyerolling, lip smacking), or incontinence. Assess postictal phase “after” a seizure. • Any shakes “tremors” in hands/face? • Any weakness or problem moving any part of the body? Hemi-one side of body; paresis-partial or incomplete paralysis; paralysis-total loss of motor function d/t lesion • Any problems w/coordination? Any numbness or tingling (paresthesia)? • Any problems swallowing (dysphagia)? Subjective Data: • Any problems speaking? Dysarthria (difficulty forming words); dysphasia (difficulty w/language comprehension/expression) • Any exposure to environmental or occupational hazards? Do you currently take medications and if so, what kinds? Do you consume alcohol and if so, how much? Do you consume illicit drug and if so, what type? • Test Cranial Nerves (review previous slide & p. 637-640) Inspect/Palpate Motor System Objective Data: • Muscles size (always compare sides and note it may be difficult to assess muscle mass in obese person) • Muscle strength: Test muscle groups of the extremities, neck, trunk • **Muscle Tone: Need to move extremities through passive range of motion (PROM) flexion, extension, abduction, adduction, plantar flexion, dorsiflexion. The individual should be relaxed “loose”, support the arm at the elbow and leg at the knee. You should note a mild, even resistance to movement. Cerebellar Function (coordinated/skilled movements) Objective Data: • Rapid Alternating Movements (RAM): pat knees w/both hands in supination and pronation positions then increase the pace. **If unable to do RAM you will note slow, clumsy, uncoordinated, and sloppy response “dysdiadochokinesia”** • Finger-Nose-Finger Test (p.642) • Heel-shin Test (p.642) Balance Tests (should be at the end of exam) • Gait: Should be smooth, rhythmic, and effortless w/opposing arm swinging in coordination • Tandem Walk (p. 643) Objective Data: • Tiptoe-heels • Shallow knee bend/hop • Romberg Test: Individual stands w/feet together w/ arms at the side and eyes closed for 20 sec. should note balanced posture w/slight swaying **Make sure to be close to prevent fall injury** **Positive sign=loss of balance when eyes are closed d/t cerebellar ataxia (uncoordinated/unsteady gait) (MS, alcohol intoxication) Asses the Sensory System Objective Data: • Ask the individual to identify various sensory stimuli to test the intactness of the peripheral nerve fibers, sensory tracts, and high cortical discrimination. • Complete testing of the sensory system is warranted ONLY in those w/neurologic symptoms (e.g. localized pain, numbness, and tingling) or w/abnormalities (e.g. motor deficits). • Use unbiased directions “tell me what you feel”-the person’s eyes should be closed during each of the tests and explain what will happen Anterolateral-Spinothalmic Tract 1. Pain: Ask the person to say “sharp” or “dull” when you touch the skin w/ the dull end (general response test) of the tongue blade or pointed end (sharp edge test pain) from the break of the tongue blade. Allow 2 seconds between discrimination of findings. Objective Data: Hypoalgesia (decreased pain sensation) Hyperalgesia (increased pain sensation) Analgesia (absent pain sensation) 2.Light Touch: Apply cotton wisp to skin at random sites of the arms, forearms, hands, chest, thighs, and legs and ask the person to say “Now” when sensation is felt. Hypoesthesia (decreased touch sensation) Hyperesthesia (increased touch sensation) Anesthesia (absent touch sensation) Posterior (Dorsal) Column Tract Objective Data: • 1. **Vibration: Test via a tuning fork over bony prominences by striking the tuning fork on the heel of your hand. Ask the person to indicate when the vibration starts and stops. If a vibration or buzzing sensation is felt on these distal areas of the fingers and great toes, then assume proximal spots are normal and proceed no further. **If no vibrations are felt move proximally up the bony prominences and compare left to right side. Peripheral Neuropathy worse @ the feet and gradually improves as you move up the lower extremity (e.g. DM) • 2. Tactile Discrimination “position sense”: Ask pt. to close eyes and on upper extremity grab index finger and for lower extremity grab big toe and move it up/down and have individual state position. 3. **Stereognosis: Place a familiar object (keys, paper clip, coin, etc) and ask person to identify the object. Objective Data: 4. Graphesthesia: Ask the person to identify the “number or letter” traced on the palm of the hand w/eyes closed using a blunt object. 5. Point Location: Ask the person to point to the location w/ his or her finger where you touched on their skin after prompt withdrawal. **Be familiar with grading scale** A. Biceps reflex: place your thumb on the biceps tendon and strike a blow on your thumb. You should note contraction of the bicep and flexion of the forearm. B. Triceps reflex: strike the blow above the elbow and you should note extension of the forearm. Objective Data: C. Brachioradialis reflex: Hold individual’s thumbs to suspend the forearms in relaxation. Strike 2-3 cm above the radial styloid process on the forearm and should note flexion and supination of the forearm. D. Quadriceps “Knee Jerk”: Allow lower legs to dangle freely and strike the tendon below the patella and should note extension of the lower leg. E. Achilles “Ankle Jerk” reflex: Position person w/knee flexed, and hip externally rotated as you strike tendon and note plantar flexion as it presses against your hand. Neurological Recheck: • Head trauma or neurological deficit may be d/t systemic disease and must be monitored closely Objective Data: **Assess for signs of increased intracranial pressure by examining LOC, Motor function, Pupillary response, and Vital Signs ** (Hypertension, bradycardia, pupil dilation, Headache, blurry vision, confusion, irritability, vomiting) • LOC: Orientation to person, place, time • Motor fx: Assess upper extremities by arm strength from hand grips, lifting arms for noting any drift. Assess lower extremities by straight leg raises or pressing foot against your hand noting resistance. • Pupillary response: Note size, shape, symmetry of both pupils • Vital Signs: Temp., HR, BP, Resp. • Stroke: Interruption of blood supply to the brain • Risk Factors: S&S: • “Ischemic” numbness/tingling, swallowing/drooling, loss of balance/coordination, drowsiness/loss of consciousness • “Hemorrhagic” Severe H/a, N/V, sudden loss of consciousness, focal seizures **Hyperreflexia and possible clonus occur on the involved side** Centers for Disease Control and Prevention. (2019, August 19). Stroke Death Rates. https://www.cdc.gov/dhdsp/maps/national_maps/stroke_all.htm Memorial Health System. (2020). Spot a stroke-B.E.F.A.S.T. Retrieved from https://www.memorialmedical.com/service s/stroke-services/spot-a-stroke-fast • **Review Table 24.6 (p. 675) + p. 672/673 Samarpan Physiotherapy Clinic. (2019, March 2). List of abnormal gait. https://samarpanphysioclinic.com/2019/03/02/list-of-abnormal-gait-physiotherapy-treatment/ • Anatomy Info. (2021). Occipital Lobe: Anatomy, Location, and Function. Retrieved fromhttps://anatomyinfo.com/occipital-lobe-function/ References • Centers for Disease Control and Prevention. (2019, August 19). Stroke Death Rates. https://www.cdc.gov/dhdsp/maps/national_maps/stroke_all.htm • Dyer, J.G. (2014). Anatomy & physiology made incredibly visual (2nd ed.), Philadelphia, PA: Wolters Kluwer Health • Four Directions of Wellness. (2016). How Do Healing Modalities Work? Your Autonomic Nervous System Explained. Retrieved from https://fourdirectionswellness.com/2016/10/18/healingmodalities-work-autonomic-nervous-system-explained/ • Jarvis, C., & Eckhardt, A. (2020). Physical Examination & Health Assessment (8th ed.). St. Louis, MO: Elsevier • Kabb Law Team. (2019, June 27). 10 Warning signs and symptoms of Alzheimer’s. https://www.kabblaw.com/blog/10-warning-signs-and-symptoms-of-alzheimers/ • Loreto Sixth form College. A level Biology. Retrieved from http://loretocollegebiology.weebly.com/synapses.html • Marieb, E.N., & Hoehn, K. (2016). Human anatomy and physiology (11th ed.), Hoboken, NJ: Pearson References • Memorial Health System. (2020). Spot a stroke-B.E.F.A.S.T. https://www.memorialmedical.com/services/stroke-services/spot-a-stroke-fast • Samarpan Physiotherapy Clinic. (2019, March 2). List of abnormal gait. https://samarpanphysioclinic.com/2019/03/02/list-of-abnormal-gaitphysiotherapy-treatment/ • Willis, L.M. (2017). Health Assessment Made Incredibly Visual (3rd ed.). Philadelphia, PA: Wolters Kluwer.