VR & Task-Oriented Training for Pediatric Hand Burns
advertisement

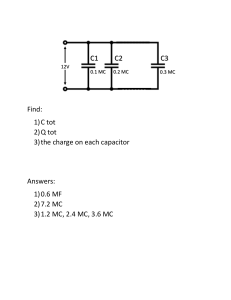
Archives of Physical Medicine and Rehabilitation journal homepage: www.archives-pmr.org Archives of Physical Medicine and Rehabilitation 2021;102:1059-66 ORIGINAL RESEARCH Effects of Virtual Reality and Task-Oriented Training on Hand Function and Activity Performance in Pediatric Hand Burns: A Randomized Controlled Trial Fatma Alzahraa H. Kamel, PhD,a,b Maged A. Basha, PhDb,c From the aDepartment of Physical Therapy for Surgery, Faculty of Physical Therapy, Cairo University, Cairo, Egypt; bDepartment of Physical Therapy, College of Medical Rehabilitation, Qassim University, Qassim, Buraidah, Saudi Arabia; and cDepartment of Physical Therapy, El-Sahel Teaching Hospital, General Organization for Teaching Hospitals and Institutes, Cairo, Egypt. Abstract Objective: To assess the efficacy of a motion-sensing, hands-free gaming device and task-oriented training (TOT) programs on improving hand function, activity performance, and satisfaction in pediatric hand burns. Design: A randomized controlled trial. Setting: Outpatient rehabilitation center. Participants: Fifty children with deep partial-thickness or full-thickness hand burns. (NZ50; mean age, 10.701.64y; range, 7-14y) Interventions: Children were randomized into 1 of the following 3 groups: the motion-sensing, hands-free gaming device group that used interactive video games plus traditional rehabilitation (TR); the TOT group that used real materials plus TR; and the control group that only received TR, all groups received the interventions 3 days per week for 8 weeks. Main Outcome Measures: We assessed the children at the baseline and after 8 weeks of intervention. The primary outcome measures were the Jebsen-Taylor Hand Function Test, Duruoz Hand Index (DHI), and Canadian Occupational Performance Measure (COPM). The secondary outcome measures were range of motion (ROM) of the digits, grip strength, and pinch strengths (tip, palmer, and lateral pinch). Results: There was a significant increase in all measurements of the motion-sensing, hands-free gaming device and TOT groups compared with that of the control group postintervention (P<.05). There was no significant change in Jebsen-Taylor Hand Function Test, COPM performance, ROM, grip strength, and tip and lateral pinch strengths between the motion-sensing, hands-free gaming device group and TOT group (P>.05), whereas there was a significant increase in DHI, COPM satisfaction, and palmer pinch strength (P<.05) in the motion-sensing, hands-free gaming device group compared with the TOT group postintervention. Conclusions: The motion-sensing, hands-free gaming device and TOT programs resulted in significant improvement in hand function, activity performance and satisfaction, ROM of the digits, grip strength, and pinch strengths in pediatric hand burns compared with the traditional hand rehabilitation. Archives of Physical Medicine and Rehabilitation 2021;102:1059-66 ª 2021 by the American Congress of Rehabilitation Medicine The severity and prevalence of hand burns is well recognized, with rehabilitation implications and final outcomes well beyond what can be measured by evaluating the affected percentage of total body surface area on its own.1 The function of the hands is 1 of the key determinants of the quality of life in pediatric hand burns (PHB). PHB can induce different hand deformities and Clinical Trial Registration No.: NCT04497103. Disclosures: none. contractures, and the functional skills gained after hand burn disproportionately affects the child’s capacity to reintegrate completely into their preinjured position in society.2-6 Despite traditional rehabilitation (TR) of PHB, hand function can remain impaired,7-10 and two-thirds of patients with full-thickness hand burn injuries change careers because of their functional hand disability.11 Virtual reality (VR) has been used in functional rehabilitation of upper extremity defects, and task-specific training efficacy increased through repetitive and positive feedback when tasks 0003-9993/21/$36 - see front matter ª 2021 by the American Congress of Rehabilitation Medicine https://doi.org/10.1016/j.apmr.2021.01.087 1060 were ordered in a random training series.12,13 Xbox Kinecta is an interactive and enjoyable training device that produces a virtual rehabilitation scene that systemically manages the intensity of training.14 In randomized controlled trials, Kinect-based VR rehabilitation used in patients with burns,15,16 patients with stroke,17 children with cerebral palsy,18 and children with arthritis19 resulted in increased upper extremity function and activity performance and participation and has superior results on outcomes compared with TR. Task-oriented training (TOT) concentrates on performance and engagement in compliance with the recommendations of the International Classification of Functioning, Disability and Health. In TOT the child learns problem-solving skills and successful alternative techniques by adjusting to various situations to accomplish the activity. TOT literature reports that in neurologic and musculoskeletal patients the use of problem-solving skills is superior to training requiring numerous repeated movement patterns for increasing function and participation of the upper extremity.19-22 VR has been used in burn studies mainly for pain management and increase range of motion (ROM) in acute burns.15,16,23,24 No studies in the existing literature have assessed the effect of Xbox Kinect-based rehabilitation or TOT in PHB. The objective of this work was to evaluate the efficacy of Xbox Kinect and TOT in PHB in enhancing hand function, activity performance and satisfaction, ROM of digits, grip strength, and pinch strengths. Methods Trial design This was a randomized controlled trial conducted between May 2018 and September 2019. We recruited all participants from the burn units of teaching hospitals in Cairo, Egypt. All of the children’s guardians signed an informed consent form. The Ethics Committee granted approval for this study (The Research Ethics Committee, Faculty of Physical Therapy, Cairo University), and the study was conducted in compliance with the Declaration of Helsinki. This study was registered in ClinicalTrials.gov (NCT04497103). Participants The inclusion criteria involved individuals (mean age, 10.701.64y; range, 7-14y) with deep partial-thickness or fullthickness hand burns induced by either scaled or flame thermal burn, involvement of >50% of the hand and wrist, total body surface area involvement <30%, recent acute care discharge, and List of abbreviations: ADL activities of daily living COPM Canadian Occupational Performance Measure DHI Duruoz Hand Index JTHFT Jebsen-Taylor Hand Function Test PHB pediatric hand burns ROM range of motion TOT task-oriented training TR traditional rehabilitation VR virtual reality F.A.H. Kamel, M.A. Basha spontaneous healing within 1 month or after 2 weeks of splitthickness or full-thickness skin graft. Individuals were excluded from this study if they had infection, tendon injuries, muscle injury, fracture, degenerative joint diseases, peripheral nerve diseases, juvenile arthritis, or pre-established psychological and physical disorders (extreme aphasia, cognitive and developmental deficits that can influence rehabilitation). Randomization We randomly allocated 50 patients with PHB into 1 of 3 groups: the Xbox Kinect-based rehabilitation group (Xbox group) (nZ17), TOT group (nZ16), or control group (nZ17). Randomization was done using opaque, randomly-numbered envelopes. After baseline assessment, the individuals opened the envelopes to determine their group placement. The randomization was done by an independent physical therapist who was not involved in this study at any stage. Interventions The TR program was carried out in 40-minute sessions 3 times weekly for 8 weeks for all children in the 3 groups. TR included immersion in paraffin, gentle massaging using moisturizing gel, stretching exercises, ROM exercises, mobilizing techniques, strength training (initially performed in static mode and advanced dynamically in the fifth week by using elastic bands), desensitizing, and occupational therapy. In the home program parents and children were taught how to splint/position themselves against contractures, apply scar massage, exercise, use compression garments and inserts, and train themselves on their own.25 Baseline Canadian Occupational Performance Measure (COPM) assessments were used to create personalized treatment objectives for each child. Focusing on top-priority functional tasks enabled the child to select the optimal motor strategies to achieve functional requirements. We determined rehabilitation protocols by considering the assessment outcomes and the child’s personality, roles, level of performance, and personal goals. An individualized training protocol was developed after determining the individual’s 5 most significant problems after activities assessment and analysis. The Xbox and TOT groups conducted on average 50-minute sessions 3 days a week for 8 weeks. The TOT program involved the preparation of materials required for the training, including exercise bands, coordination tools, skill cubes, therapeutic putty, screw sets, Velcro cylinders, buttons, clothes, rope, spoons, pencils, and so on. The training progression took place by increasing the difficulty of tasks, changing the number of repeats, increasing or decreasing activity performance time, and modifying the materials being used (eg, smooth/tough for resistive bands or therapeutic putty, picking up objects of different sizes with Velcro cylinders, large/small buttons for buttoning). A physical therapist evaluated the Xbox games to detect technical features that could have therapeutic uses, the conformity of games according to the required activity, the pattern of movement required, and levels of complexity and transitions between levels of complexity. We selected games for each child that related to the 5 significant problems detected during the child-focused analysis outcomes. During the training, the child was required to copy the actions of the avatar on the screen. The closer the child’s movements were to the fluency, position, and speed of the avatar’s activity, the greater the child’s score. The Xbox Kinect games www.archives-pmr.org Rehabilitation of Pediatric Hand Burns were then chosen based on the child’s performance level and the rehabilitation plan designed under the guidance of a physiotherapist. Progression developed in the games through modifications such as increased or decreased game time, increased focus on endurance games, or the addition of more levels to increase difficulty. 1061 size was based on a pilot study of 5 individuals in each group. Sample size calculation was conducted using G*POWER statistical software, version 3.1.9.2e and F test- MANOVA: Repeated measures, within-between interaction. Statistical analysis Outcome measures We conducted all measurements at baseline and after intervention (after 8 weeks). The assessor, who was blinded to the treatment allocation, collected the outcome measures. The primary outcome measurements were the Jebsen-Taylor Hand Function Test (JTHFT), Duruoz Hand Index (DHI), and COPM. Secondary outcomes included total active ROM of the digits, grip strength, and pinch strengths (tip, palmer, and lateral pinch). The JTHFT is a standard and objective method designed to measure the performance speed of standardized tests through 7 items reflecting different hand functions commonly used in daily living activities. A slower time indicates a less desirable outcome, with coefficients ranging from 0.6-0.99; this test is reliable and valid. The test-retest reliability for the total time of both hands is high (rZ0.97 and rZ0.98).26 DHI is an 18-item self-reported scale designed to evaluate activity limitation of the hand in the kitchen, performing hygiene or office activities, while dressing, and during other general activities. The children’s items were scored on a 6-point Likert scale. The total scores ranged between 0-90, with a higher score indicating poor hand function.27 COPM is a personalized test intended to track variations in the self-perception of a child’s occupational performance over time. This is a commonly used measure applicable to all children with perceived challenges in performing tasks of daily living in selfcare or social activity. The COPM includes 2 (performance and satisfaction) scores of 10 each. The child is required to prioritize up to 5 difficulties they find to be most significant or necessary and rate their performance and satisfaction on a standard 10-point scale. COPM is a valid, responsive, and reliable scale, and 1.9 improvements in score are considered clinically significant for satisfaction and 1.4 for performance.28,29 Measurement of the total active ROM was carried out by a hand-held steel finger goniometer.b During assessment, the evaluator requested the child flex every digit as much as he or she could and assessed the overall active flexion. Next, extension limitations were evaluated for zero-degree extension of the same digits.30,31 For the statistical analysis, we used the data of each digit’s total active ROM. Hand grip strength was measured using a Jamar hydraulic dynamometerc and pinch strengths (tip, palmer, and lateral pinch) were assessed using a pinch dynamometer.d The assessment position was recommended by the American Society of Hand Therapists. Each test was repeated 3 times with an interval of 30seconds between trials, and the mean value was documented in kg.32 Sample size calculation Sample size was calculated considering the difference in COPM among the 3 groups to be 0.45 (effect size), significance levelZ0.05, and with 80% power. Sample size was calculated to be 17 individuals per group, with a 1:1:1 ratio. The presumed effect www.archives-pmr.org We carried out descriptive and analysis of variance tests to compare the patients’ characteristics between groups. For comparison of categorical data sets between groups, the chi-square test was used. The Shapiro-Wilk test was used to evaluate normal data distribution, and Levene’s homogeneity test of variances was performed to assess the homogeneity between groups. Mixed model multivariate analysis of variance was conducted to compare clinical outcomes within and between groups. For subsequent multiple comparison, post hoc tests using the Bonferroni correction were implemented. The significance level was set to P<.05 for all statistical analyses. All statistical analyses were conducted using SPSS version 22.f Results The patient flow diagram throughout the study is shown in figure 1. Fifty children participated in this study and 4 children left the intervention for various reasons and their measurements were not included in the analysis. There were no significant differences in the demographics and clinical characteristics of the children (total body surface area, hospital stay, burn location, etiology of burn) between the 3 groups at baseline evaluation (P>.05) (Table 1). Mixed design multivariate analysis was performed to evaluate the difference between individuals in the 3 groups using the amount of change in their scores on the outcome measures. Statistically significant multivariate effects were found for the groups’ interventions, Wilk’s AZ0.16, F26,62Z3.64, P<.001, ƞ2Z0.6; for time, Wilk’s AZ0.01, F13,31Z413.2, P<.001, ƞ2Z0.99; and for the interaction between groups and time, Wilk’s AZ0.01, F26,62Z22.75, P<.001, ƞ2Z0.91. Eight-week univariate analysis of variances revealed significant change for JTHFT, F2,43Z25.18, P<.001, ƞ2Z0.54; for DHI, F2,43Z62.61, P<.001, ƞ2Z0.74; for COPM performance, F2,43Z16.93, P<.001, ƞ2Z0.44; for COPM satisfaction, F2,43Z38.08, P<.001, ƞ2Z0.64; for thumb ROM, F2,43Z112.62, P<.001, ƞ2Z0.84; for index ROM, F2,43Z52.87, P<.001, ƞ2Z0.71; for middle finger ROM, F2,43Z34.02, P<.001, ƞ2Z0.61; for ring finger ROM, F2,43Z43.68, P<.001, ƞ2Z0.67; and for little finger ROM, F2,43 Z31.73, P<.001, ƞ2Z0.6; for grip strength, F2,43 Z 68.0, P<.001, ƞ2Z0.76; for tip pinch strength, F2,43 Z 97.49, P<.001, ƞ2Z0.82; for lateral pinch strength, F2,43Z46.37, P<.001, ƞ2Z0.68; and for palmer pinch strength, F2,43Z51.55, P<.001, ƞ2Z0.71. Between-group comparison There was no significant difference between the 3 groups in all measurements preintervention (P>.05). However, there was a significant increase in DHI, COPM satisfaction, and palmer pinch strength in the Xbox group compared with the TOT group postintervention (P<.05); however, there was no significant change in 1062 F.A.H. Kamel, M.A. Basha Fig 1 Patient flow diagram throughout the study. JTHFT and COPM performance, ROM, grip strength, and tip and lateral pinch strengths between the Xbox group and TOT group (P>.05). In addition, there was a significant increase in all measurements of Xbox and TOT groups compared with that of the control group postintervention (P<.05), as in tables 2 and 3. Within-group comparison There was a significant improvement in all measurements postintervention compared with baseline in the Xbox, TOT, and control groups (P<.001), with the exception being there was no significant change in tip pinch strength in the control group (PZ.06) (Table 4). Discussion Children differ from adults in their need for extra encouragement strategies and rehabilitation programs because of their fear of movement and often refusal to engage in rehabilitation programs owing to pain, anxiety, and distress.24 The aim of this study was to investigate the impact of different rehabilitation programs in PHB on hand function and activity performance. The main results of the current study showed statistically significant differences between the Xbox and TOT groups regarding DHI scores, COPM satisfaction, and palmer pinch strength (P<.05), but no statistically significant differences between the Xbox and TOT groups regarding JTHFT, activity performance, ROM, grip strength, and tip and lateral pinch strength (P>0.5). However, both the Xbox and TOT groups had larger improvements than the control group in all outcomes. Regarding within-group comparison, there were statistically significant differences after 8 weeks (P<.001) in all groups except for tip pinch strength in the control group (P>0.5). This study suggests that the similar improvements in several of the outcome measures in the Xbox and TOT programs resulted from many causes, including the 2 programs centered on identifying the 5 most significant problems in activities of daily living www.archives-pmr.org Rehabilitation of Pediatric Hand Burns Table 1 1063 Baseline demographic characteristics of the 3 groups Age (y) Sex, n (%) Female Male Weight (kg) Height (cm) Hand dominance, n (%) Right Left TBSA (%) Hospital stay (d) Burn location, n (%) Palmer Dorsal Circumference Etiology of burn, n (%) Flame Scaled Xbox Group (nZ17) TOT Group (nZ16) Control Group (nZ17) Mean SD Mean SD Mean SD P Value 10.561.98 10.281.4 11.241.41 .23 7 (41.18) 10 (58.82) 42.356.02 140.511.88 7 (43.75) 9 (56.25) 38.885.25 136.911.72 7 (41.18) 10 (58.82) 40.187.11 140.512.36 .99 13 (76.47) 4 (23.53) 22.353.59 34.654.46 13 (81.25) 3 (18.75) 24.562.66 37.52.61 13 (76.47) 4 (23.53) 23.883.82 35.822.86 .93 6 (35.3) 5 (29.4) 6 (35.3) 6 (37.5) 5 (31.3) 5 (31.3) 6 (35.3) 6 (35.3) 5 (29.4) .99 7 (41.2) 10 (58.8) 6 (37.5) 10 (62.5) 7 (41.2) 10 (58.8) 0.97 .27 .62 .17 .07 NOTE. Data are mean SD unless otherwise stated. P values <.05 indicate statistical significance. Abbreviation: TBSA, total body surface area. (ADL) as an intervention plan by COPM; the child having an active role in the program of rehabilitation vs TR; and the child concentrating on enjoying the games instead of their involvement in a treatment program, thereby decreasing pain and fear and leading to higher activity performance. The changes of DHI scores were statistically superior in the Xbox group and may be demonstrated by increased strength of the proximal muscles. One potential reason is that Xbox games do not concentrate exclusively on the movement of fingers and wrists but also involve repetitive movements aimed at the proximal muscles, and proximal muscle stabilization is essential for better performance in playing. Shoulder girdle stabilization allows the force to transmit through the myofascial pathway for optimal recruitment of the hand muscles33,34 and also gains in pinch grip strength and handgrip strength.35 VR is supposed to increase motor performance by encouraging brain plasticity and brain reorganization via active engagement, feedback, and movement repetition.36 The variation in COPM satisfaction after intervention has been statistically significant in favor of the Xbox group, and this may be attributed to Xbox trainings that are interactive, provide stimulation, immediate feedback, enhance engagement, and reward accomplishments.15,16 To our knowledge, there are no studies comparing Xbox Kinect-based VR and TOT for the rehabilitation of PHB; however, there are a few studies that reported beneficial effects of the Kinect-based VR in the rehabilitation of pediatric burns.15,16 These studies reported that using the Xbox Kinect in the treatment of upper limb burns is associated with a significant decrease in pain and kinesiophobia, increased ROM and selfreported time spent exercising, greater satisfaction, and improved function. In hand burn studies,9,37 one study reported that, 8 weeks of interactive robot treatment in PHB resulted in increased ROM, grip strength, and hand function.9 Joo et al showed that 4 weeks of VR-based rehabilitation in adult burned hand resulted in a significant increase in patient satisfaction, www.archives-pmr.org work, hand function, aesthetics, performance in ADL, and decreased pain compared with TR.37 The TOT literature concentrates on patients with stroke and patients with arthritis.19-22 These studies found that TOT resulted in a significant increase in arm and hand function, participation in ADL, exercise compliance, and the enjoyment of the participant in participating and inspiring elements of TOT was demonstrated. The results of this study are in agreement with studies that used purposeful activities in patients with pediatric burns.10,38 Omar et al reported increased ROM of finger digits, decreased pain, more motivation and enjoyment, and improved functional activity and performance of hands in ADL when patients with PHB engaged in 3 weeks of purposeful exercises on the principle of game playing rather than TR.10 Study limitations Although the findings of this study are promising, there are other limitations that should be addressed. First, we believe that Xbox Kinect and TOT could increase children’s motivation and reduce the avoidance of fear, yet we did not investigate children kinesiophobia or motivation, which may affect adherence to treatment. Second, absence of control over the home training may affect outcomes. Third, the limited sample size compromises our findings’ accuracy. Fourth, the fairly short follow-up duration did not determine whether the changes will continue long term. Therefore, more trials are needed to determine the long-term impact. Fifth, the children were not blinded and were aware of the kind of therapy they received. More trials that include hand rehabilitation are needed for patients with fourth-degree burns with severe neuromuscular injuries. One of the most advantageous aspects of Xbox Kinect and TOT for promoting physical activity and therapy is that they could be played at home and are completely unaffected by difficulties (ie, climate, availability, and transportation) that generally limit involvement in other types of physical activity. More studies are 1064 Table 2 F.A.H. Kamel, M.A. Basha Clinical characteristics of the 3 Groups at baseline and after 8 weeks of intervention Characteristics JTHFT (s) Baseline 8-weeks DHI Baseline 8-weeks COPM -performance Baseline 8-weeks COPM -satisfaction Baseline 8-weeks Thumb ROM (deg.) Baseline 8-weeks Index ROM (deg.) Baseline 8-weeks Middle ROM (deg.) Baseline 8-weeks Ring ROM (deg.) Baseline 8-weeks Little ROM (deg.) Baseline 8-weeks Grip strength (kg) Baseline 8-weeks Tip pinch (kg) Baseline 8-weeks Lateral pinch (kg) Baseline 8-weeks Palmer pinch (kg) Baseline 8-weeks Xbox Group (nZ17) TOT Group (nZ14) Control Group (nZ15) F-Value P Value 173.1814.7 131.5310.49 179.2115.1 139.4314.11 181.3313.19 158.2714.43 1.41 17.47 .26 .0001 35.356.24 13.473.53 37.077.7 20.797.45 40.04.98 31.076.03 2.15 37.18 .13 .0001 3.121.45 7.651.27 2.571.22 6.791.05 2.931.28 5.41.24 0.66 14.11 .52 .0001 2.241.03 8.181.01 2.070.62 6.211.25 2.330.98 4.531.30 37.77 0.16 .74 .0001 75.0616.92 105.0613.64 72.4314.12 98.7114.46 69.4714.72 80.413.84 0.53 13.12 .6 .0001 165.5313.89 187.5314.63 164.5713.68 185.010.81 162.818.81 170.017.25 0.12 6.52 .88 .003 166.2915.7 186.014.18 163.2916.17 185.3611.47 160.9318.64 170.1318.02 0.41 5.57 .67 .007 178.8215.4 195.8212.48 175.0713.89 194.2112.66 171.8717.01 178.9316.27 0.81 6.91 .45 .003 163.3517.71 182.5913.72 166.013.09 183.2912.93 159.3317.01 167.616.77 0.63 5.59 .54 .007 19.883.14 26.063.42 18.213.04 24.712.87 19.43.38 21.43.5 1.07 8.31 .35 .0008 1.570.27 2.560.36 1.510.33 2.760.41 1.650.27 1.750.27 0.85 34.28 0.43 .0001 3.180.38 4.190.3 3.050.27 3.990.32 3.090.34 3.410.31 0.63 26.65 .54 .0001 2.420.34 3.610.39 2.270.55 3.010.59 2.150.37 2.470.36 1.7 25.87 .019 .0001 NOTE. Data are mean SD. P values <.05 indicate statistical significance. needed to investigate if Xbox Kinect and TOT will be beneficial for training patients with PHB at home. Conclusion In conclusion, Xbox Kinect and TOT are interactive and enjoyable training methods that may be clinically-effective rehabilitation tools for functional treatment in patients with PHB, can be easily adapted to changes in performance, and are reported to produce improvement in hand function and activity performance and satisfaction in children with hand burns. c. Jamar Hydraulic Hand Dynamometer; Fabrication Enterprises Inc. d. Jamar Pinch Gauge Dynamometer, model no. PG-30; B and L Engineering. e. G)POWER statistical software, version 3.1.9.2; HeinrichHeine-Universitat. f. SPSS for Windows, version 22.0; IBM Corp. Keywords Burns; Rehabilitation; Virtual reality Suppliers Corresponding author a. Xbox Kinect; Microsoft Corporation. b. Baseline 1 Finger Goniometer; Fabrication Enterprises Inc. Maged A. Basha, PhD, Department of Physical Therapy, El-Sahel Teaching Hospital, General Organization for Teaching Hospitals www.archives-pmr.org Between-group effects of all outcome measures after 8 weeks of intervention. Xbox vs TOT Xbox vs Control TOT vs Control Outcomes MD (99% CI) P Value MD (99% CI) P Value MD (99% CI) P Value Partial ƞ2 JTHFT (s) DHI COPM performance COPM satisfaction Thumb ROM (deg.) Index ROM (deg.) Middle ROM (deg.) Ring ROM (deg.) Little ROM (deg.) Grip strength (kg) Tip pinch (kg) Lateral pinch (kg) Palmer pinch (kg) e7.9 e7.32 0.86 1.96 6.35 2.53 0.64 1.61 e0.7 1.35 e0.19 0.2 0.61 .3 .003 .16 .0001 .64 .99 .99 .99 .99 .79 .42 .11 .002 e26.7 e17.6 2.25 3.64 24.66 17.53 15.87 16.89 14.99 4.66 0.82 0.78 1.15 .0001 .0001 .0001 .0001 .0001 .004 .01 .004 .017 .0007 .0001 .0001 .0001 e18.8 e10.3 1.39 1.68 18.31 15.0 15.22 15.28 15.69 3.31 1.01 0.59 0.54 .001 .0001 .01 .001 .003 .02 .03 .01 .018 .03 .0001 .0001 .007 0.45 0.63 0.4 0.64 0.38 0.23 0.21 0.24 0.21 0.28 0.62 0.55 0.55 (e19.59, 3.79) (e12.50, e2.13) (e0.22, 1.94) (0.9, 3.03) (e6.21, 18.89) (e10.56, 15.62) (e12.70, 13.99) (e10.87, 14.09) (e13.79, 12.4) (e1.61, 4.30) (e0.51, 0.13) (e0.08, 0.48) (0.2, 1.01) (e38.21, e15.27) (e22.67, e12.50) (1.19, 3.31) (2.6, 4.69) (12.34, 36.98) (4.68, 0.38) (2.77, 28.97) (4.64, 29.14) (2.14, 27.84) (1.76, 7.56) (0.51, 1.13) (0.51, 1.06) (0.75, 1.54) (e30.87, e6.80) (e15.62, e4.94) (0.28, 2.5) (0.58, 2.78) (5.39, 31.24) (1.53, 28.48) (1.48, 28.97) (2.43, 28.13) (2.20, 29.17) (0.27, 6.36) (0.68, 1.14) (0.3, 0.87) (0.12, 0.96) Rehabilitation of Pediatric Hand Burns www.archives-pmr.org Table 3 NOTE. P values <.05 indicate statistical significance. Abbreviations: CI, confidence interval; deg., degrees; MD, mean difference; ƞ2, eta squared. Table 4 Within-group changes for all outcome measures from baseline to 8 weeks of intervention JTHFT(s) DHI COPM performance COPM satisfaction Thumb ROM (deg.) Index ROM (deg.) Middle ROM (deg.) Ring ROM (deg.) Little ROM (deg.) Grip strength (kg) Tip pinch (kg) Lateral pinch (kg) Palmer pinch (kg) Xbox Group (nZ17) TOT Group (nZ14) Control Group (nZ15) Change From Baseline to 8 wks Change From Baseline to 8 wks Change From Baseline to 8 wks MD (99% CI) P Value MD (99% CI) P Value MD (99% CI) P Value 41.65 21.88 e4.53 e5.94 e30.0 e22.0 e19.71 e17.0 e19.25 e6.18 e0.99 e1.01 e1.19 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 39.79 16.29 e4.21 e4.14 e26.29 e20.43 e22.07 e19.14 e17.29 e6.5 e1.24 e0.94 e0.74 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 23.07 9.93 e2.47 e2.2 e10.93 e7.2 e9.2 e7.07 e8.27 e2.0 e0.09 e0.31 e0.32 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .0001 .06 .0001 .0001 (37.74, 45.55) (20.28, 23.48) (e5.05, e4.01) (e6.53, e5.35) (e31.83, e28.17) (e24.14, e19.86) (e21.92, e17.49) (e18.84, e15.16) (e21.23, e17.24) (e6.75, e5.6) (e1.11, e0.88) (e1.11, e0.9) (e1.31, e1.07) (18.91, 27.22) (7.23, 10.64) (e3.02, e1.92) (e2.83, e1.57) (e12.89, e8.98) (e9.48, e4.92) (e11.56, e6.84) (e9.03, e5.11) (e10.39, e6.14) (e2.62, e1.39) (e0.22, e0.03) (e0.43, e0.2) (e0.45, e0.19) 1065 NOTE. P values <.05 indicate statistical significance. Abbreviations: CI, confidence interval; deg., degrees; MD, mean difference. (35.48, 44.09) (14.52, 18.05) (e4.79, e3.64) (e4.8, e3.49) (e28.32, e24.27) (e22.79, e18.07) (e24.51, e19.63) (e21.17, e17.12) (e19.49, e15.09) (e7.14, e5.86) (e1.37, e1.12) (e1.06, e0.82) (e0.87, e0.61) 1066 and Institutes, 2 Youssef Karam St., Borham, Elsahel, Cairo Governorate 11697, Cairo, Egypt. E-mail addresses: bashamaged@gmail.com and M.Basha@qu.edu.sa. Acknowledgment We thank Shady A. Basha, MSc, PT for assisting with data collection and performing the randomization. F.A.H. Kamel, M.A. Basha 20. 21. 22. References 1. Kowalske KJ, Greenhalgh DG, Ward SR. Hand burns. J Burns Care Res 2007;28:607-10. 2. Gupta RK, Jindal N, Kamboj K. Neglected post burns contracture of hand in children: analysis of contributory socio-cultural factors and the impact of neglect on outcome. J Clin Orthop Trauma 2014;5:215-20. 3. Choi M, Armstrong MB, Panthaki ZJ. Pediatric hand burns: thermal, electrical, chemical. J Craniofac Surg 2009;20:1045-8. 4. Anzarut A, Chen M, Shankowsky H, Tredget EE. Quality-of-life and outcome predictors following massive burn injury. Plast Reconstruct Surg 2005;116:791-7. 5. Palmieri TL, Nelson-Mooney K, Kagan RJ, et al. Impact of hand burns on health-related quality of life in children younger than 5 years. J Trauma Acute Care Surg 2012;73:S197-204. 6. Fufa DT, Chuang SS, Yang JY. Post burn contractures of the hand. J Hand Surg Am 2014;39:1869-76. 7. Sheridan RL, Baryza MJ, Pessina MA, et al. Acute hand burns in children: management and long-term outcome based on a 10-year experience with 698 injured hands. Ann Surg 1999;229:558-64. 8. Liodaki E, Kisch T, Mauss KL, et al. Management of pediatric hand burns. Pediatr Surg Int 2015;31:397401. 9. Samhan AF, Abdelhalim NM, Elnaggarb RK. Effects of interactive robot-enhanced hand rehabilitation in treatment of paediatric handburns: a randomized, controlled trial with 3-months follow-up. Burns 2020;46:1347-55. 10. Omar MT, Hegazy FA, Mokashi SP. Influences of purposeful activity versus rote exercise on improving pain and hand function in pediatric burn. Burns 2012;38:2618. 11. Nuchtern JG, Engrav LH, Nakamura DY, Dutcher KA, Heimbach DM, Vedder NB. Treatment of fourth-degree hand burns. J Burn Care Rehabil 1995;16:36-42. 12. Da Gama A, Fallavollita P, Teichrieb V, et al. Motor rehabilitation using Kinect: a systematic review. Games Health J 2015;4:123-35. 13. Placidi G. A smart virtual glove for the hand telerehabilitation. Comput Biol Med 2007;37:1100-7. 14. Fager SK, Burnfield JM. Patients’ experiences with technology during inpatient rehabilitation: opportunities to support independence and therapeutic engagement. Disabil Rehabil Assist Technol 2014;9:121-7. 15. Voon K, Silberstein I, Eranki A, Phillips M, Wood FM, Edgar DW. Xbox Kinect based rehabilitation as a feasible adjunct for minor upper limb burns rehabilitation: a pilot RCT. Burns 2016;42:1797-804. 16. Lozano EI, Potterton JL. The use of Xbox KinectTM in a pediatric burns unit. South Afr J Physiother 2018;74:a429. 17. Lee G. Effects of training using videogames on the muscle strength, muscle tone, and activities of daily living of chronic stroke patients. J Phys Ther Sci 2013;25:595-7. 18. Chang YJ, Han WY, Tsai YC. A Kinect-based upper limb rehabilitation system to assist people with cerebral palsy. Res Dev Disabil 2013;34:3654-9. 19. Arman N, Tarakci E, Tarakci D, Kasapcopur O. Effects of video gamesebased task-oriented activity training (Xbox 360 Kinect) on 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. activity performance and participation in patients with juvenile idiopathic arthritis a randomized clinical trial. Am J Phys Med Rehabil 2019;98:174-81. Abdullahi A, Mohammed AA. A novel approach to upper limb task specific training in children with hemiparesis. Int J Phys Med Rehabil 2014;2:6. Almhdawi K. Effects of occupational therapy task-oriented approach in upper extremity post-stroke rehabilitation. Occup Ther Int 2016;23: 444-56. Srikesavan CS, Shay B, RobinsonDB, et al. Task-oriented training with computer gaming in people with rheumatoid arthritis or osteoarthritis of the hand: study protocol of a randomized controlled pilot trial. Trials 2013;14:69. Miller K, Rodger S, Kipping B, Kimble RM. A novel technology approach to pain management in children with burns: a prospective randomized controlled trial. Burns 2011;37:395-405. Parry I, Painting L, Bagley A, Kawada J, Molitor F, Sen S. A pilot prospective randomized control trial comparing exercises using videogame therapy to standard physical therapy: 6 months follow-up. J Burns Care Res 2015;36:534-44. Moore ML, Dewey WS, Richard RL. Rehabilitation of the burned hand. Hand Clin 2009;25:529-41. Jebsen RH, Taylor N, Trieschmann R, Trotter MJ, Howard LA. An objective and standardized test of hand function. Arch Phys Med Rehabil 1969;50:311-9. Duruöz MT. Hand function: a practical guide to assessment. New York: Springer; 2014. p 55-62. Dedding C, Cardol M, Eyssen IC, et al. Validity of the Canadian Occupational Performance Measure: a client-centered outcome measurement. Clin Rehabil 2004;18:660-7. Eyssen IC, Steultjens MP, Oud TA, et al. Responsiveness of the Canadian occupational performance measure. J Rehabil Res Dev 2011; 48:517-28. Rayan GM, Akelman E. The hand: anatomy, examination, and diagnosis. Philadelphia, PA: Wolters Kluwer Health | Lippincott Williams & Wilkins; 2012. Adams L, Greene L, Topoozian E. Range of motion. In: American Society of Hand Therapists, ed. Clinical assessment recommendations. 1992. p 55-70, Philadelphia, PA: American Society of Hand Therapists. Villafane JH, Valdes K. Reliability of pinch strength testing in elderly subjects with unilateral thumb carpometacarpal osteoarthritis. J Phys Ther Sci 2014;26:993-5. Mandalidis D, O’Brien M. Relationship between hand-grip isometric strength and isokinetic moment data of the shoulder stabilisers. J Bodyw Move Ther 2010;14:19-26. Huijing PA, Baan GC. Myofascial force transmission: muscle relative position and length determine agonist and synergist muscle force. J Appl Physiol 2003;94:1092-107. Kobesova A, Dzvonik J, Kolar P, Sardina A, Andel R. Effects of shoulder girdle dynamic stabilization exercise on hand muscle strength. Isokinet Exerc Sci 2015;23:21-32. Rathinam C, Mohan V, Peirson J, Skinner J, Nethaji KS, Kuhn I. Effectiveness of virtual reality in the treatment of hand function in children with cerebral palsy: a systematic review. J Hand Ther 2019; 32:426-434.e1. Joo SY, Cho YS, Lee SY, Seok H, Seo CH. Effects of virtual realitybased rehabilitation on burned hands: a prospective, randomized, single-blind study. J Clin Med 2020;9:731. Melchert-Mckearnan K, Deitz J, Engle JM, White O. Children with burn injuries: purposeful activities versus rote exercise. Am J Occup Ther 2001;54:381-90. www.archives-pmr.org