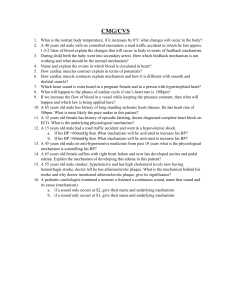
NURSING CAREPLAN FORM Date _____________ Nursing Diagnosis Desired patient outcome Nursing intervention s Rationale Evaluation of desired patient outcome Standard: Decreased Cardiac Output (SMART) Specific, Measureable, Attainable, Realistic, Timed Assess, Diagnostic, Actions/ Treatments, Meds, Teaching, Geriatric (or developmental). Other Patient Specific Interventions Explains why. Relates to the problem and desired outcome R/T (related to) Altered heart rhythm, altered preload, altered afterload, altered contractility, behavioral/emo tional changes Short term goal: Patient will remain free of side effects from medication used to improve cardiac output. Indicates if DPO met, partially met, or not met and criteria used to determine this. Focus on patient response rather than nurse action Short term goal: Met partially. Patient had no complaints of furthering symptoms from medication (Lasix) such as dizziness, drowsiness, or drop in blood pressure. Patient did have lowered potassium levels with no symptoms. Long term goal: Patient will maintain adequate cardiac output as evidence by blood pressure, pulse rate, and rhythm within controlled parameters. Long term AEB (as evidenced by) abnormal heart rhythm with defibrillator, jugular vein distention, edema in lower extremities, weakened extremity pulses, dyspnea upon activity, increase in restlessness Assessments: Assess patient’s vital signs, especially heart rate and blood pressure goal: unable to assess due to time constraints. Patients blood pressure, pulse rate is stable currently. Tachycardia, 0654 vitalsdecreased 97.3 temp, oxygen pulse 64, saturation, and respirations hypotension are 18, O2 sat typical signs of 100%, B/P decreased 150/68. cardiac output. 1007 vitalsCardiomegaly is 97.6 temp, a condition that pulse 68, results from respirations chronic 18, O2 sat hypertension 97%, B/P which reduces 148/67. cardiac output because of Vital signs reduction in show amount of blood increased B/P the heart which patient pumps. has chronic hypertension. Patient is on 2 L of oxygen via nasal cannula. Assess patient’s skin Assess peripheral pulses, pulse deficits, capillary refill Assess patient for edema Changes in skin color, moisture, and temperature show signs of SNS involvement in decreased cardiac output and decreased oxygenation. Skin is cold, clammy, diaphoretic, pale, cyanotic, edematous. Decreased cardiac output causes weakened peripheral pulses and sluggish or nonexistent capillary refills. Pulse deficits occur when there is a decreased cardiac output because of poor peripheral perfusion. In compromised cardiac system, Patient is of African descent, so membranes were assessed. They are rosy pink and moist. Skin is dry and warm. No pulse deficits detected. Capillary refill less than 3 seconds. Weakened lower extremity pulses due to lower peripheral edema (1+). Generalized lower edema Assess for Jugular neck vein distention Assess mental status or level of consciousness Assess breath sounds and breathing patterns fluid retention is common because of the hearts inability to pump efficiently. Fluid is backed up from the right side of the heart causing elevated pressures in jugular veins. This is most often found in HF, right ventricular MI, COPD, Heart Block, arrythmias or fluid volume overload. Changes are from decreased oxygen reaching the brain because of decreased blood flow. Shallow, rapid respirations and crackles are all common in left sided heart failure. non pitting. Jugular vein distention noted on both sides of patient’s neck. Patient is alert and oriented x 4. Patient upon admission was extremely SOA, bilateral crackles. Patient now has clear lung fields, use of accessory Assess patient’s Input and output Labs/Diagnostic Studies Assess patient’s electrolyte levels Evaluate cardiac enzymes Decreased output is a sign of decreased cardiac output because of profusion issues to organs (kidneys) Often treatment increases output which depletes electrolytes by urination. Cardiac Enzymes are deposited in the blood stream when damage has occurred in the cardiac muscle. muscles upon exertion as well as c/o SOA upon exertion. Patient has taken self to restroom without monitoring. Patient’s levels of potassium have decreased due to Lasix treatment. Potassium level is 3.4. Potassium protocol ordered and patient was given 20 meq of potassium. Lab to recheck. Troponin levels were within normal limits. Evaluate BNP and Creatine Actions/Treatments Decrease oxygen needs of the body Follow a cardiac diet Troponin levels are the best way to effectively evaluate if damage is or has occurred. BNP elevation without CREA elevation is a sign of HF. Creatinine levels elevated at 1.71. ProBNP extremely elevated at 34202. This should be no greater than 450 in adults 75-99. Oxygen Patient I on supplementation 2Liters of may decrease oxygen via the body’s nasal canula. compensatory mechanisms (increased HR, RR, B/P) and rest or reduced activity to decrease the body’s demands. Diet healthy for Patient is the ordered a cardiovascular cardiac diet. system which is Patient states low in fats, high they eat the in fiber, low in right foods but salt will not elaborate. Medications Administer diuretics Patient teaching Educate patient on importance of daily weights Geriatric considerations Assess for abnormal signs of decreased cardiac output and HF Assess side effects of cardiac meds Diuretics reduce excess fluid in vascular and tissue systems. This reduces the workload of the heart and decreases the body’s demands. Daily weights can help monitor fluid retention which can exacerbate CHF symptoms Fatigue and depression are often sign of decreased cardiac output and HF because of the body’s inability to adapt to demands Metabolism in the elderly is slow due to decreased kidney and liver function and are more likely to experience toxic side effects Patient received 40mg Lasix IV push once daily. Patient stated understanding of education. Patient has noted daytime fatigue and fatigue with activity Patient creatinine level is elevated at 1.71. This could be related to treatment of CHF exacerbation with Lasix. Creatinine levels signifies impaired kidney function. Potassium levels decreased to 3.4. Potassium protocol ordered and 20 meq of potassium given. Nursing Diagnosis Desired patient outcome Nursing intervention s Rationale Evaluation of desired patient outcome Standard: Activity intolerance (SMART) Specific, Measurable, Attainable, Realistic, Timed Assess, Diagnostic, Actions/ Treatments, Meds, Teaching, Geriatric (or developmental). Other Patient Specific Interventions Explains why. Relates to the problem and desired outcome Related to: Decreased Cardiac output, decreased oxygen supply, sedentary lifestyle, compromised oxygen Short Term Goal: Patient will maintain normal skin conditioning such as being warm, pink, and dry. Long Term Goal: Patient will Indicates if DPO met, partially met, or not met and criteria used to determine this. Focus on patient response rather than nurse action Short Term Goal: Met. Patients mucus membranes stayed rosy pink, warm and dry. Long Term transport demonstrate increased tolerance to activity by not showing signs of labored breathing with little activity. Goal: Unable to assess due to time restraint. Patient had labored breathing at sat dropping when moving around in room. As Evidence By: Congestive heart failure, oxygen usage, labored breathing and O2 stat dropping upon activity Assessment Assess vital signs Assessing patient’s vital signs especially at rest makes it easier to compare vital signs with and without activity. 0654 vitals97.3 temp, pulse 64, respirations 18, O2 sat 100%, B/P 150/68. 1007 vitals97.6 temp, pulse 68, respirations 18, O2 sat 97%, B/P 148/67. Patient is on oxygen at 2 L. Patients baseline Assess for generalized weakness Assess circulatory condition Assess respiratory status reading of 100% oxygenation dropped to 97% when making their bed. Weakness Patient’s foot hinders a pushes and patient’s ability handgrips to perform tasks strong and efficiently and even. Fair the body’s Range of ability to motion. function Patient has properly under proper gait the demand of without use of oxygen and assistive blood devices. There is an Patient was imbalance diagnosed between oxygen with CHF and supply and has been demand. The hospitalized heart cannot for efficiently exacerbations. pump enough Lower oxygenated extremity blood to support peripheral tissues. pulses weak, capillary refill within normal limits. Jugular vein distention noted. Left sided heart Patient has failure causes jugular vein blood to back distention up into the lungs causing problems breathing. Assess for exertional dyspnea Lab/ diagnostic studies Dyspnea or SOA is identified as difficult or labored breathing. Monitor oxygen Monitoring saturations oxygenation which is common in right sided heart failure. When right sided heart failure is present, usually the left side is affected also. Patient has diagnosis of CHF. With treatment lung fields sound clear. Patient is receiving 2 Liters of oxygen via nasal canula. Patient had difficulty talking at faster speeds because of SOA. Patient had SOA symptoms like labored breathing after activity (making own bed and walking around room) Patient on 2L of oxygen via Evaluate CBC, BNP, Creatinine, electrolytes and BUN/CRE status will ensure quick intervention if oxygen demands are not met. Lab work may indicate reason behind symptoms that cause activity intolerance such as possible anemia, cardiac insufficiencies, respiratory insufficiencies, nutritional insufficiencies. nasal canula. Continuous tele and pulse ox. Saturation staying at 97% or above. Patient creatinine level is elevated at 1.71. This could be related to treatment of CHF exacerbation with Lasix. Creatinine levels signifies impaired kidney function. Potassium levels decreased to 3.4. Potassium protocol ordered and 20 meq of potassium given. Troponin levels were within normal limits. Creatinine levels elevated at 1.71. Pro- Actions/TX Provide oxygen therapy Employ energy saving strategies Medications Administer Oxygen therapy allows the respiratory and cardiovascular system to not work as hard for appropriate oxygenation Energy saving strategies include pacing and frequent resting during activities. This allows patient to not exert self too much at any given time during activity Diuretics reduce BNP extremely elevated at 34202. This should be no greater than 450 in adults 75-99. HCT 32.1 (low), RBC 3.64 (low), HGB 10.1 (low) which all indicate anemia. This can lead to oxygenation issues. Patient is on oxygen therapy 2 liters via nasal canula Encouraged patient to take rest during activity and allow for relaxation to decrease oxygen demands of the body. Patient diuretics Nursing Diagnosis Standard: Risk for impaired skin integrity excess fluid in vascular and tissue systems. This reduces the workload of the heart and decreases the body’s demands. Resting or pacing activity increases tolerance for activity. received 40mg Lasix IV push once daily. Teaching Teach patient the importance of mixing activity with periods of rest. Patient stated understanding. Encouraged them to take their time when moving in the room and talking. Patient is at medium fall risk due to recent fall at home, IV apparatus and weakened state. Geriatric implications Assess fall risk Poor balance, weakened muscle tone, fear of falling all affect motility, effort and tolerance Desired patient outcome Nursing intervention s Rationale Evaluation of desired patient outcome (SMART) Specific, Measurable, Attainable, Realistic, Timed Assess, Diagnostic, Actions/ Treatments, Meds, Teaching, Geriatric (or developmental). Other Patient Explains why. Relates to the problem and desired outcome Indicates if DPO met, partially met, or not met and criteria used to determine this. Focus on patient response Specific Interventions Related To: advanced age, physical limitations, alteration in skin turgor, xerosis, impaired circulation Short term goal: Patient’s skin will remain intact throughout shift. Long Term goal: Patient’s edema will subside and return to normal baseline. As evidence Assessment by: age, activity intolerance, dry skin, edema, CHF exacerbation Assess overall skin condition Assess Braden scale rather than nurse action Short term goal: Met. Patient remained free of skin openings, redness. Long term goal: Unable to assess due to time constraints. Patient still has non pitting edema in lower extremities and slightly pitting edema in left arm. Assessing the Patient skin is patient’s overall dry and flaky. skin condition Edema present can identify in lower weakened and extremities problemed areas (non-pitting) that may need and in left arm attention (slightly pitting). Patients skin is warm and normal for race. Braden scale is Patient was at a quick and medium risk easy assessment of skin tool used to identify patients at risk for skin integrity issues. breakdown due to chronic illnesses, age, and skin condition at the time. Assess edema Skin that is Edema present taught or in lower edematous is at extremities greater risk for (non-pitting) imparities and in left arm (slightly pitting). Assess for skin Irritations may Patient skin is irritations result is itching extremely dry or blisters that and flaky. potentially can Patient has no lead to skin complaints of breakdown/ope pruritis. ning Moisture cream applied. Assess moisture Moisture Patient skin is contributes to dry. Room maceration environment which can lead is not to quickened humidified skin breakdown. and cool. Patient is continent of bowel and bladder. Assess patient’s Sensing Patients ability to feel pressure or pain ability to feel pain or pressure gives patients pain or the sensation to pressure is move to intact. alleviate symptoms. Assess patient’s mobility status Labs/Diagnostic Studies Evaluate CBC Actions/Treatments Encourage ambulation Keep edematous extremities elevated. Treat or prevent Immobility may cause the patient inability to shift, turn or move off pressure areas resulting in skin breakdown. Patient can ambulate on own. Patient is at a weakened state and has activity intolerance but can shift off pressure areas. Anemia can HCT 32.1 lead to (low), RBC decreased 3.64 (low), oxygenation of HGB 10.1 the tissues (low) which therefore all indicate potentially anemia. This increasing can lead to healing time tissue and decreasing oxygenation function. issues. Ambulation Encourage increases patient to circulation to move but to tissue and do so at a prevent pressure paced rate. breakdown Elevation helps Encourage reduce edema patient to keep by promoting left arm absorption of elevated with fluid and pillow and promoting place lower blood flow back extremities on toward the ottoman for heart. elevation when sitting. Dry skin may Applied dry skin Medications Use diuretics when appropriate to treat fluid retention Teaching Keep edematous extremities elevated. Geriatric Implications Assess patients sense of pressure and pain Use lotion and moisturizers to prevent dry skin. Assess patients cause pruritis moisturizer and lead to open cream to dry in skin barrier. flaky skin areas on legs and arms to prevent cracking and soothe itching. Fluid retention Patient is leads to taking 40 mg edematous areas Lasix IV push that can cause daily to skin integrity reduce fluid issues. retention. Elevation helps Educated reduce edema patient to keep by promoting left arm absorption of elevated with fluid and pillow and promoting place lower blood flow back extremities on toward the ottoman for heart. elevation when sitting. Patient stated understanding. Aging causes Patients change in ability to feel sensation that pain or are felt and pressure is recognized. intact. Dry skin can Moisturizer lead to a break was applied to in skin barrier. dry skin areas on legs and arms of patient. Advanced age Patient is in age 4/2016 leads to normal late seventies. changes in skins elasticity and ability to regenerate.