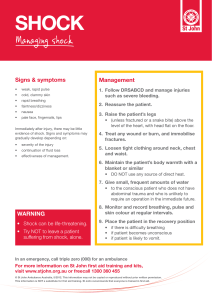
SHOCK OBJECTIVES Definition Pathology Types & their Causes Clinical Features Effects Hospital management Prevention Definition This is the failure of circulation to adequately supply oxygen to the tissues. OR is the complete collapse of circulatory system and depression of all vital centers accompanied by a fall in the blood pressure. Pathology of shock If the amount of blood is not enough, it’s shared according to priorities. This is associated with vascular constriction so to help increase blood volume and supply to vital centers. However, if the neuro –vessel constrictor mechanism fails, there is diminished blood supply rich in oxygen to the brain leading to poor function of the medulla oblongata where the vital centers are located hence shock occurs Physiological changes during shock This involves what happens when shock occurs. Once shock has been produced, there can either be compensation or un compensation. 1. COMPESATION When compensation of shock occurs, blood is drawn from other organs like the stomach, intestines, muscles and the skin to the vital organs like the heart, lungs, brain and eventually the patient recovers from shock 2. UNCOMPESATION The normal compensatory mechanism may fail so that less blood is carried to the heart . This is associated with reduced cardiac output resulting in continued reduction of the blood pressure and deterioration of the patient’s condition. Types of shock and their causes 1. HYPOVOLAEMIC SHOCK OR OLIGEAMIC SHOCK This type of shock is due to reduced blood volume circulating in the body which may be due to the following; I. Heamorrhagic shock; Severe loss of blood. II. Non heamorrhagic shock; Severe loss of body fluids e.g. in Burns , Gastroenteritis 2. NEUROGENIC SHOCK This type of shock occurs as a result of emotional trauma or depression of nerves and nerve centers. This occurs inform of fainting or common faint. This is associated with relaxation of the arterioles in the muscles, common causes include; Damage to the spine and the brain stem and loss of sympathetic outflow. Severe pain where by the nerves supplying the area are compressed Horrifying site or hearing bad news. Prolonged anesthesia 3. CARDIOGENIC SHOCK This occurs in an acute heart disease when the damaged heart muscle cannot maintain an adequate cardiac output. The causes include; Myocardial infarction Pulmonary embolism Trauma with structural damage to the heart 4. SEPTIC SHOCK (BACTERAEMIC , ENDOTOXIC) This is caused by severe infection in which bacterial toxins are released into the circulation. The endothelium forming the walls of the blood vessels is damaged by the bacterial toxins causing them to dilate resulting into hypertension. This process involves both depression of the heart and loss of fluid from circulation into the body tissues. The fluid loss is due to capillary leakage and may give rise to oedema. This treated by use of antibiotics. 5. ANAPHYLACTIC SHOCK This is a severe allergic response that may be triggered in sensitive individuals by substances like drugs, peanut causing vasodilation provoked by systemic release of mediators like histamine and bradykinin causing venous hypotension. 6. METABOLLIC SHOCK ; This is due to metabolic & endocrine diseases e.g. insulin shock Clinical features of shock Sudden or gradual onset associated with lowered blood pressure that comes as a result of poor function of the heart to pump blood at the required rate. The pulse is usually rapid and weak, although sometimes it is below normal in rate due to poor circulation in arteries with decreased volume. Respirations are rapid and shallow which may be due to poor ventilation in the lungs and air passages. Paleness of the face, greyish lips and cyanosis of the ear lobes due to lack of enough oxygen in the blood circulation .The patient’s face is expressionless. The skin is cold, white and clammy due to less blood supply to the skin so as to conserve blood to the vital centers. The temperature is subnormal due to reduced blood supply to the skin and this reduces the requirements of the tissues for the diminished oxygen available. There is low blood pressure systolic and diastolic and sometimes it is unrecordable. The eyes are still and the patient takes little or no interest in his surroundings, although he may answer solely questions that are asked .He may make no complain of pain due to insensitivity. There is muscle relaxation and loss of muscle tone due to diminished blood supply to the skin / muscles. There is diminished urinary output so as to conserve fluid in the body and it also indicates inadequate tissue perfusion. Effects of shock Blood pressure falls. Blood flowing to the heart decreases and the heart beats faster. Blood vessels in the peripheral constricts so that the available blood is sent to the vital centers e.g. heart brain , etc.(compensated shock) As it progresses, blood supply to the internal organs is cut off, they undergo necrosis ad lose their functioning. If not treated in time, vital organs don’t receive blood and shock becomes irreversible. The final stage is death. Management of a patient with shock Aims of management I. To restore normal tissue perfusion. II. To ensure quick return of body function to normal. III. To prevent any likely complications. The patient is put in a flat position however the foot of the bed may be elevate using bed blocks so as to facilitate adequate blood supply to the vital centers in the brain by flow of gravity. Proper ventilation in the room should be ensured and the colour of the patients’ extremities should be observed for cyanosis. Reassurance of the patient as well as the relatives to alley anxiety. The patient should also be handled gently to prevent unnecessary disturbances. Adequate warmth is provided to the patient by covering him/ her with enough blankets however over heating should be avoided since this is associated with dilatation of the skin vessels hence blood supply to the vital centers. A warm swabbing may be done on the whole face and the whole body. Monitoring of vital signs is very essential which is done half hourly, hourly, two hourly until the patient is stable. Observations of temperature is done to assess degree of tissue perfusion, blood pressure monitoring is essential for assessment of improvement of hypotension. Pulse rate is also monitored regularly and findings recorded on the vital observation chart and abnormal findings are reported. Fluid replacement is done which must be done intravenously so as to quickly restore the circulating volume. Fluid input and output must be recorded on a fluid balance chart so as to prevent fluid overload. Electrolyte imbalance must also be corrected. Assessment of renal function should be done by monitoring urine output and severe cases an indwelling catheter must be passed. Oxygen administration should be done in case of cyanosis or respiratory distress. Blood transfusion should be done in case of severe haemorrhage so as to restore the loss and hence help in the functioning of the heart, hence increasing blood pressure and blood supply to the vital centers. Drugs to be administers to the patient include; dopamine in low dose infusion to improve the blood pressure, hydrocortisone 100mg to stabilize cell membranes hence improvement of cellular function, antibiotics are essential in case of presence of a bacterial infection like amoxicillin 500mg 8hrly. NOTE In case of slow patient’s response or inadequate, the diagnosis of the cause may have to be revised. However, once the patient’s condition has improved, every precaution must be taken to ensure that shock does not reoccur. Return to sitting up position should be instituted gradually and observantly. Prevention of shock PREOPERATIVE MEASURES The patient should be kept warm on his journey to theatre from the ward. Blankets used to cover the patient should be warm. Patient’s fear and anxiety should be allayed before surgery and tranquillizing drugs should be administered. Vital observations with special emphasis on blood pressure should be done for early identification of shock and hence quick management or control of its occurrence. Blood and fluid replacement should be done in good time to prevent possible oligeamic shock. Therefore major operations should be commenced only if satisfactory infusions have been established. INTRAOPERATIVE MEASURES Continuous monitoring of the patient’s vital signs is done throughout the operation which is recorded regularly as well as drugs and fluids administered. The head of operating table is lowered if the blood pressure falls. The anesthetist induces and maintains adequate level of the anesthesia, ensuring good oxygenation and tissue perfusion POSTOPERATIVE MEASURES The patient should be kept warm on the way from theatre to ward. Fluid and electrolyte replacement, rest and relief from pain are continued. Gentle handling of the patient by the nursing staff is very important in prevention of shock. Vital observation monitoring and recording should still be continued.