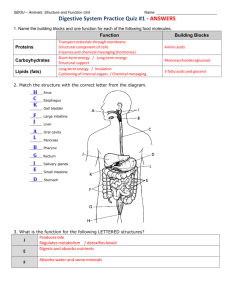
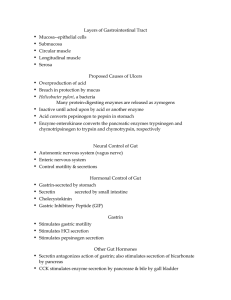
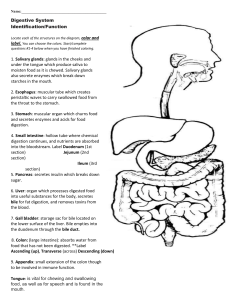
Human p h y iology The Digestive System INTRODUCTION TO THE DIGESTIVE SYSTEM Within the lumen of the gastrointestinal tract, large food molecules are hydrolyzed into their monomers (subunits). These monomers pass through the inner layer, ormucosa, of the small intestine to enter the blood or lymph in a process called absorption. Digestion and absorption are aided by specializations of the gastrointestinal tract. Functions of the GI Tract Motility: ▫ Movement of of food through the GI tract. Ingestion: Taking food into the mouth. Mastication: Chewing the food and mixing it with saliva. Deglutition: Swallowing the food. Peristalsis: Rhythmic wave-like contractions that move food through GI tract. Functions of the GI Tract (continued) • Secretion: ▫ Includes both exocrine and endocrine secretions. Exocrine: HCl, H20, HC03-, bile, lipase, pepsin, amylase, trypsin, elastase, and histamine are secreted into the lumen of the GI tract. Endocrine: Stomach and small intestine secrete hormones to help regulate the GI system. ▫ Gastrin, secretin, CCK, GIP, GLP-1, guanylin, VIP, and somatostatin. Functions of the GI Tract (continued) • Digestion: ▫ Breakdown of food particles into subunits (chemical structure change). • Absorption: ▫ Process of the passage of digestion (chemical subunits) into the blood or lymph. • Storage and elimination: ▫ Temporary storage and elimination of indigestible food. Layers of the Gastrointestinal Tract The GI tract from the esophagus to the anal canal is composed of four layers, or tunics. Each tunic contains a dominant tissue type that performs specific functions in the digestive process. The four tunics of the GI tract, from the inside out, are the mucosa, submucosa, muscularis, and serosa Digestive System (GI) • GI tract divided into: ▫ Alimentary canal. ▫ Accessory digestive organs. • GI tract is 30 ft long and extends from mouth to anus. Insert fig. 18.2 Layers of GI Tract • Composed of 4 tunics: ▫ Mucosa. ▫ Submucosa. Muscularis. Serosa. Mucosa • Lines the lumen of GI tract. ▫ Consists of simple columnar epithelium. • Lamina propria: ▫ Thin layer of connective tissue containing lymph nodules. • Muscularis mucosae: ▫ Thin layer of smooth muscle responsible for the folds. Folds increase surface area for absorption. • Goblet cells: ▫ Secrete mucus. Submucosa • Thick, highly vascular layer of connective tissue. • Absorbed molecules enter the blood and lymphatic vessels. • Submucosal plexus (Meissner’s plexus): ▫ Provide autonomic nerve supply to the muscularis mucosae. Muscularis • Responsible for segmental contractions and peristaltic movement through the GI tract. ▫ Inner circular layer of smooth muscle. ▫ Outer longitudinal layer of smooth muscle. • Contractions of these layers move food through the tract; pulverize and mix the food. • Myenteric plexus located between the 2 muscle layers. ▫ Major nerve supply to GI tract. Fibers and ganglia from both sympathetic and parasympathetic nervous systems. Serosa • Binding and protective outer layer. • Consists of areolar connective tissue covered with simple squamous epithelium. Regulation of the GI Tract • Extrinsic innervation: ▫ Parasympathetic nervous system: Vagus and spinal nerves: Stimulate motility and GI secretions. ▫ Sympathetic nervous system: Postganglionic sympathetic fibers that pass through submucosal and myenteric plexuses and innervate GI tract: Reduce peristalsis and secretory activity. Regulation of the GI Tract (continued) • Enteric nervous system: ▫ Sites where parasympathetic fibers synapse with postganglionic neurons that innervate smooth muscle. • Submucosal and myenteric plexuses: ▫ Local regulation of the GI tract. • Paracrine secretion: ▫ Molecules acting locally. • Hormonal secretion: ▫ Secreted by the mucosa. From Mouth to Stomach • Mastication (chewing): ▫ Mixes food with saliva which contains salivary amylase. Enzyme that can catalyze the partial digestion of starch. • Deglutition (swallowing): ▫ Begins as a voluntary activity. ▫ Involves 3 phases: Oral phase is voluntary. Pharyngeal and esophageal phases are involuntary. Cannot be stopped. ▫ Larynx is raised. ▫ Epiglottis covers the entrance to respiratory tract. From Mouth to Stomach (continued) • Involuntary muscular contractions and relaxations in the mouth, pharynx, larynx, and esophagus are coordinated by the swallowing center in the medulla. • Esophagus: ▫ Connects pharynx to the stomach. Upper third contains skeletal muscle. Middle third contains a mixture of skeletal and smooth muscle. Terminal portion contains only smooth muscle. Esophagus • Peristalsis: ▫ Produced by a series of localized reflexes in response to distention of wall by bolus. • Wave-like muscular contractions: ▫ Circular smooth muscle contract behind, relaxes in front of the bolus. ▫ Followed by longitudinal contraction (shortening) of smooth muscle. Rate of 2-4 cm/sec. ▫ After food passes into stomach, LES constricts. Insert 18.4a Stomach • Most distensible part of GI tract. ▫ Empties into the duodenum. • Functions of the stomach: ▫ Stores food. ▫ Initiates digestion of proteins. ▫ Kills bacteria. ▫ Moves food (chyme) into intestine. Stomach • Contractions of the stomach churn chyme. ▫ Mix chyme with gastric secretions. ▫ Push food into intestine. (continued) Insert fig. 18.5 Stomach • Gastric mucosa has gastric pits in the folds. • Cells that line the folds deeper in the mucosa, are gastric glands. (continued) Insert fig. 18.7 Gastric Glands • Secrete gastric juice: ▫ ▫ ▫ ▫ Goblet cells: mucus. Parietal cells: HCl and intrinsic factor. Chief cells: pepsinogen. Enterochromaffin-like cells (ECL): histamine and serotonin. ▫ G cells: gastrin. ▫ D cells: somatostatin. ▫ Stomach: ghrelin. HCl Production • Parietal cells secrete H+into gastric lumen by primary active transport, through H+/ K+ ATPase pump. • Parietal cell’s basolateral membrane takes in Cl- against its electrochemical gradient, by coupling its transport with HC03-. Insert fig. 18.8 HCl Production (continued) • HCl production is stimulated: ▫ Indirectly by gastrin. ▫ Indirectly by ACh. • ACh and gastrin stimulate release of histamine. ▫ Histamine: Stimulates parietal cells to secrete HCl. HCl Functions • Makes gastric juice very acidic. ▫ Denatures ingested proteins (alter tertiary structure) so become more digestible. • Activates pepsinogen to pepsin. ▫ Pepsin is more active at pH of 2.0. Insert fig. 18.9 Digestion and Absorption in the Stomach • Proteins partially digested by pepsin. • Carbohydrate digestion by salivary amylase is soon inactivated by acidity. • Alcohol and aspirin are the only commonly ingested substances absorbed. Gastric and Peptic Ulcers • Peptic ulcers: ▫ Erosions of the mucous membranes of the stomach or duodenum produced by action of HCl. • Zollinger-Ellison syndrome: ▫ Ulcers of the duodenum are produced by excessive gastric acid secretions. • Helicobacter pylori: ▫ Bacterium that resides in GI tract that may produce ulcers. • Acute gastritis: ▫ Histamine released by tissue damage and inflammation stimulate further acid secretion. Protective Mechanisms of Stomach • Parietal and chief cells impermeable to HCl. • Alkaline mucus contains HC03-. • Tight junctions between adjacent epithelial cells. • Rapid rate of cell division (entire epithelium replaced in 3 days). • Prostaglandins inhibit gastric secretions. Small Intestine • Each villus is a fold in the mucosa. • Covered with columnar epithelial cells interspersed with goblet cells. • Epithelial cells at the tips of villi are exfoliated and replaced by mitosis in crypt of Lieberkuhn. • Lamina propria contain lymphocytes, capillaries, and central lacteal. Insert fig. 18.12 Absorption in Small Intestine • Duodenum and jejunum: ▫ Carbohydrates, amino acids, lipids, iron, and Ca2+. • Ileum: ▫ Bile salts, vitamin B12, electrolytes, and H20. Intestinal Enzymes • Microvilli contain brush border enzymes that are not secreted into the lumen. ▫ Brush border enzymes remain attached to the cell membrane with their active sites exposed to the chyme. • Absorption requires both brush border enzymes and pancreatic enzymes. Intestinal Contractions and Motility • 2 major types of contractions occur in the small intestine: ▫ Peristalsis: Slow movement. Pressure at the pyloric end of small intestine is greater than at the distal end. ▫ Segmentation: Major contractile activity of the small intestine. Contraction of circular smooth muscle. Mix chyme. Insert fig. 18.14 Contractions of Intestinal Smooth Muscles • Occur automatically in response to endogenous pacemaker activity. • Rhythm of contractions is paced by graded depolarizations called slow waves. ▫ Slow waves produced by interstitial cells of Cajal. ▫ Slow waves spread from 1 smooth muscle cell to another through nexuses. Insert fig. 18.15 Contractions of Intestinal Smooth Muscles • When slow waves above threshold, it triggers APs by opening of VG Ca2+channels. • Inward flow of Ca2+: ▫ Produces the upward depolarization phase. ▫ Stimulates contraction of smooth muscle. • Repolarization: ▫ VG K+channels open. Slow waves decrease in amplitude as they are conducted. • May stimulate contraction in proportion to the magnitude of depolarization. Cells and Electrical Events in the Muscular is Insert fig. 18.16 Large Intestine • Outer surface bulges outward to form haustra. • Little absorptive function. ▫ Absorbs H20, electrolytes, several vitamin B complexes, vitamin K, and folic acid. Intestinal microbiota produce significant amounts of folic acid and vitamin K. Bacteria ferment indigestible molecules to produce short-chain fatty acids. Does not contain villi. • Secretes H 0, via active transport of NaCl into 2 intestinal lumen. ▫ Guanylin stimulates secretion of Cl- and H20, and inhibits absorption of Na+(minor pathway). Membrane contains Na+/K+ pumps. ▫ Minor pathway. Fluid and Electrolyte Absorption in the Intestine • Small intestine: ▫ Most of the fluid and electrolytes are absorbed by small intestine. Absorbs about 90% of the remaining volume. ▫ Absorption of H20 occurs passively as a result of the osmotic gradient created by active transport. Aldosterone stimulates NaCl and H20 absorption in the ileum. • Large intestine: ▫ Absorbs about 90% of the remaining volume. Absorption of H20 occurs passively as a result of the osmotic gradient created by active transport of Na+ and Cl-. Defecation • Waste material passes to the rectum. • Occurs when rectal pressure rises and external anal sphincter relaxes. • Defecation reflex: ▫ Longitudinal rectal muscles contract to increase rectal pressure. Relaxation of internal anal sphincter. ▫ Excretion is aided by contractions of abdominal and pelvic skeletal muscles. Push feces from the rectum. Structure of Liver • Liver largest internal organ. ▫ Hepatocytes form hepatic plates that are 1–2 cells thick. ▫ Arranged into functional units called lobules. • Plates separated by sinusoids. ▫ More permeable than other capillaries. • Contains phagocytic Kupffer cells. • Secretes bile into bile canaliculi, which are drained by bile ducts. Structure of Liver (continued) Insert fig. 18.20 Hepatic Portal System • Products of digestion that are absorbed are delivered to the liver. • Capillaries drain into the hepatic portal vein, which carries blood to liver. ▫ ¾ blood is deoxygenated. ▫ Hepatic vein drains liver. Enterohepatic Circulation • Compounds that recirculate between liver and intestine. ▫ Many compounds can be absorbed through small intestine and enter hepatic portal blood. ▫ Variety of exogenous compounds are secreted by the liver into the bile ducts. • Can excrete these compounds into the intestine with the bile. Insert fig. 18.22 Major Categories of Liver Function Bile Production and Secretion • The liver produces and secretes 250–1500 ml of bile/day. • Bile pigment (bilirubin) is produced in spleen, bone marrow, and liver. ▫ Derivative of the heme groups (without iron) from hemoglobin. • Free bilirubin combines with glucuronic acid and forms conjugated bilirubin. ▫ Secreted into bile. • Converted by bacteria in intestine to urobilinogen. ▫ Urobilogen is absorbed by intestine and enters the hepatic vein. Recycled, or filtered by kidneys and excreted in urine. Metabolism of Heme and Bilirubin Bile Production and Secretion • Bile acids are derivatives of cholesterol. ▫ Major pathway of cholesterol breakdown in the body. • Principal bile acids are: ▫ Cholic acid. ▫ Chenodeoxycholic acid. Combine with glycine or taurine to form bile salts. Bile salts aggregate as micelles. • 95% of bile acids are absorbed by ileum. (continued) Insert fig. 18.25 Detoxification of the Blood • Liver can remove hormones, drugs, and other biologically active molecules from the blood by: ▫ Excretion into the bile. ▫ Phagocytosis by Kupffer cells. ▫ Chemical alteration of the molecules. Ammonia is produced by deamination of amino acids in the liver. Liver converts it into urea. Excreted in urine. Detoxification of the Blood (continued) • Inactivation of steroid hormones and drugs. ▫ Conjugation of steroid hormones and xenobiotics make them anionic. Can be transported into bile by multispecific organic anion transport carriers. ▫ Steroid and xenobiotic receptors stimulate production of cytochrome P450 enzymes. Secretion of Glucose, Triglycerides and Ketones • Liver helps regulate blood glucose concentration by: ▫ Glycogenesis and lipogenesis. ▫ Glycogenolysis and gluconeogenesis. • Contains enzymes required to convert free fatty acids into ketone bodies. Production of Plasma Proteins • Albumin and most of the plasma globulins (except immunoglobulins) are produced by the liver. • Albumin: ▫ Constitutes 70% of the total plasma protein. Contributes most to the colloid osmotic pressure in the blood. • Globulins: ▫ Transport cholesterol and hormones. ▫ Inhibit trypsin. ▫ Produce blood clotting factors I, II, III, V, VII, IX, XI. Gallbladder • Sac-like organ attached to the inferior surface of the liver. • Stores and concentrates bile. • When gallbladder fills with bile, it expands. ▫ Contraction of the muscularis layer of the gallbladder, ejects bile into the common bile duct into duodenum. • When small intestine is empty, sphincter of Oddi closes. ▫ Bile is forced up to the cystic duct to gallbladder. Pancreas • Exocrine: ▫ Acini: Secrete pancreatic juice. • Endocrine: ▫ Islets of Langerhans: Secrete insulin and glucagon. Insert fig. 18.26 Pancreatic Juice • Contains H 0, HC0 2 3 and digestive enzymes. Pancreatic Juice • Complete digestion of food requires action of both pancreatic and brush border enzymes. ▫ Most pancreatic enzymes are produced as zymogens. ▫ Trypsin (when activated by enterokinase) triggers the activation of other pancreatic enzymes. • Pancreatic trypsin inhibitor attaches to trypsin. ▫ Inhibits its activity in the pancreas. Fig. 18.29 Neural and Endocrine Regulation • Neural and endocrine mechanisms modify the activity of the GI system. • GI tract is both an endocrine gland, and a target for the action of hormones. Regulation of Gastric Function • Gastric motility and secretion are automatic. • Waves of contraction are initiated spontaneously by pacesetter cells. • Extrinsic control of gastric function is divided into 3 phases: ▫ Cephalic phase. ▫ Gastric phase. ▫ Intestinal phase. Cephalic Phase • Stimulated by sight, smell, and taste of food. • Activation of vagus: ▫ Stimulates chief cells to secrete pepsinogen. ▫ Directly stimulates G cells to secrete gastrin. ▫ Directly stimulates ECL cells to secrete histamine. ▫ Indirectly stimulates parietal cells to secrete HCl. • Continues into the 1st30 min. of a meal. Gastric Phase • Arrival of food in stomach stimulates the gastric phase. • Gastric secretion stimulated by: ▫ Distension. ▫ Chemical nature of chyme (amino acids and short polypeptides). Stimulates G cells to secrete gastrin. Stimulates chief cells to secrete pepsinogen. Stimulates ECL cells to secrete histamine. Histamine stimulates secretin of HCl. ▫ Positive feedback effect. As more HCl and pepsinogen are secreted, more polypeptides and amino acids are released. Gastric Phase (continued) • Secretion of HCl is also regulated by a negative feedback effect: ▫ HCl secretion decreases if pH < 2.5. ▫ At pH of 1.0, gastrin secretion ceases. D cells stimulate secretion of somatostatin. Paracrine regulator to inhibit secretion of gastrin. Insert. Fig. 18.30 Intestinal Phase • Inhibits gastric activity when chyme enters the small intestine. • Arrival of chyme increases osmolality and distension. ▫ Activates sensory neurons of vagus and produces an inhibitory neural reflex: Inhibits gastric motility and secretion. In the presence of fat, enterogasterone inhibits gastric motility and secretion. • Hormone secretion: ▫ Inhibit gastric activity: Somatostatin, CCK, and GLP-1. Enteric Nervous System • Submucosal and myenteric plexuses contain 100 million neurons. • Include preganglionic parasympathetic axons, ganglion cell bodies, postganglionic sympathetic axons; and afferent intrinsic and extrinsic sensory neurons. Enteric Nervous System • Peristalsis: • ACh and substance P stimulate smooth muscle contraction above the bolus. • NO, VIP, and ATP stimulate smooth muscle relaxation below the bolus. (continued) Insert fig. 18.31 Paracrine Regulators of the Intestine • Serotonin (5-HT): ▫ Stimulates intrinsic afferents, which send impulses into intrinsic nervous system; and activates motor neurons. • Motilin: ▫ Stimulates contraction of the duodenum and stomach antrum. • Guanylin: ▫ Activates guanylate cyclase, stimulating the production of cGMP. cGMP stimulates the intestinal cells to secrete Cl- and H20. Inhibits the absorption of Na+. • Uroguanylin: ▫ May stimulate kidneys to secrete salt in urine. Intestinal Reflexes • Intrinsic and extrinsic regulation controlled by intrinsic and paracrine regulators. • Gastroileal reflex: ▫ Increased gastric activity causes increased motility of ileum and movement of chyme through ileocecal sphincter. • Ileogastric reflex: ▫ Distension of ileum, decreases gastric motility. • Intestino-intestinal reflex: ▫ Overdistension in 1 segment, causes relaxation throughout the rest of intestine. Secretion of Pancreatic Juice • Secretion of pancreatic juice and bile is stimulated by: • Secretin: ▫ Occurs in response to duodenal pH < 4.5. ▫ Stimulates production of HC03- by pancreas. ▫ Stimulates the liver to secrete HC03-into the bile. • CCK: ▫ Occurs in response to fat and protein content of chyme in duodenum. ▫ Stimulates the production of pancreatic enzymes. ▫ Enhances secretin. ▫ Stimulates contraction of the sphincter of Oddi. Digestion and Absorption of Carbohydrates • Salivary amylase: ▫ Begins starch digestion. • Pancreatic amylase: ▫ Digests starch to oligosaccharides. ▫ Oligosaccharides hydrolyzed by brush border enzymes. • Glucose is transported by secondary active transport with Na+into the capillaries. Insert fig. 18.32 Digestion and Absorption of Protein • Digestion begins in the stomach when pepsin digests proteins to form polypeptides. • In the duodenum and jejunum: ▫ Endopeptidases cleave peptide bonds in the interior of the polypeptide: Trypsin. Chymotrypsin. Elastase. ▫ Exopeptidases cleave peptide bonds from the ends of the polypeptide: Carboxypeptidase. Aminopeptidase. Digestion and Absorption of Protein (continued) • Free amino acids absorbed by cotransport with Na+. • Dipeptides and tripeptides transported by secondary active transport using a H+gradient to transport them into the cytoplasm. • Hydrolyzed into free amino acids and then secreted into the blood. Insert fig. 18.33 Digestion and Absorption of Lipids • Arrival of lipids in the duodenum serves as a stimulus for secretion of bile. • Emulsification: ▫ Bile salt micelles are secreted into duodenum to break up fat droplets. • Pancreatic lipase and colipase hydrolyze triglycerides to free fatty acids and monglycerides. ▫ Colipase coats the emulsification droplets and anchors the lipase enzyme to them. ▫ Form micelles and move to brush border. Digestion and Absorption of Lipids (continued) • Free fatty acids, monoglycerides, and lysolecithin leave micelles and enter into epithelial cells. ▫ Resynthesize triglycerides and phospholipids within cell. Combine with a protein to form chylomicrons. • Secreted into central lacteals. Transport of Lipids • In blood, lipoprotein lipase hydrolyzes triglycerides to free fatty acids and glycerol for use in cells. • Remnants containing cholesterol are taken to the liver. ▫ Form VLDLs which take triglycerides to cells. ▫ Once triglycerides are removed, VLDLs are converted to LDLs. LDLs transport cholesterol to organs and blood vessels. • HDLs transport excess cholesterol back to liver. Absorption of Fat