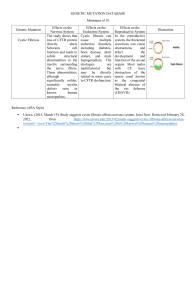
Management of Cystic Fibrosis Through the Lifespan Kevin Tran OMS-III With respect to the patient, what is cystic fibrosis? “Cystic fibrosis is a genetic disease. Only a thousand American children per year are diagnosed as having it. Some ten million people in the United States carry the defective gene, but the disorder is recessive: a child will develop the condition only if both parents are carriers and both pass on a copy. The gene…produces a mutant protein that interferes with cells’ ability to manage chloride. This is what makes sweat from people with CF so salty. (Salt is sodium chloride, after all.) The chloride defect thickens secretions throughout the body, turning them dry and gluey. In the ducts of the pancreas, the flow of digestive enzymes becomes blocked, making a child less and less able to absorb food…The effects on the lungs, however, are what make the disease lethal. Thickened mucus slowly fills the small airways and hardens, shrinking lung capacity. Over time, the disease leaves a child with the equivalent of just one functioning lung. Then half a lung. Then none at all.” -Atul Gawande, 2004, “The Bell Curve”, The New Yorker Life Expectancy & Complications ● ● ● ~45 years Morbidity and mortality are mostly caused by bronchiectasis, small airway obstruction, and progressive respiratory impairment Complications ○ Epithelial cell dysfunction in: ■ Pancreas ● Malabsorption ■ Liver ● Biliary cirrhosis ■ Sweat glands ● Heat shock ■ Vas Deferens/Cervix ● infertility Common Presentation in Older Adults ● ● ● ● ● ● Recurrent sinopulmonary infections Refractory, uncontrolled asthma Unexplained bronchiectasis Multiple episodes of pneumonia Frequent pancreatitis Male infertility with absence of the vas deferens Lung Health ● ● Most children will begin monitoring FEV1 & FVC starting at age 5 Sputum Cultures every 3 months Pseudomonas Aeruginosa CF Foundation Guidelines ● Inhaled antibiotic therapy to treat initial or new growth from an airway culture, preferably tobramycin 300 mg BID q28 days ● No benefit in routine use of antibiotics in preventing the acquisition of P. aeruginosa ● Obtaining routine airway cultures every 3 months via oropharyngeal swab ● DO NOT recommend prophylactic use of oral antistaphylococcal antibiotics ● Aztreonam for chronic for mild, moderate, and severe infections Pulmonary Hygiene ● Nebulized hypertonic saline ○ ● ● 4 ml ampules of 7% saline ■ Nebulized albuterol given before saline airway hyperreactivity and bronchoconstriction ○ No effect on rate of decline in pulmonary function and only moderate improvement in level of lung function ○ Reduction in # of exacerbations, antibiotic use for exacerbations, and absenteeism from normal activities (school, work, social gatherings, etc.) Following nebulized hypertonic saline, will proceed with some form of airway clearing technique ○ No data to suggest that one technique is superior to another Adult patients with chronic Pseudomonas infection also concurrently take antibiotics (Aztreonam) Other Chronic Medications for Maintenance of Lung Health ● ● ● Dornase alpha ○ Recombinant DNase that thins the mucus by breaking down extracellular DNA in sputum Elexacaftor/Tezacaftor/Ivacaftor ○ CFTR conductance regulators ■ IVA ● Potentiates CFTR protein by increasing the probability of it being open ■ TEZ ● Aids in processing and trafficking of CFTR to the cell membrane ■ ELX ● Increases amount of CFTR when used in conjunction with IVA/TEZ Chronic Ibuprofen for ages 6-17 ○ moderate evidence to support the use of ibuprofen twice daily for slowing the progression of CF lung disease in patients who’s FEV1 was 60% greater than predicted, i.e. Nutrition ● Nutritions is important in CF patients for 2 primary reasons: ○ ○ ● Higher BMI is associated with better lung function as well as survival ○ ○ ○ ● Birth-24 months: 50th percentile weight and height with respect to CDC growth chart 2-20 years: 50th percentile weight with respect to CDC growth chart >20: Female BMI: 22, Male BMI: 23 Diets emphasize high fat, with fats making up 35-40% of energy needs ○ ○ ● Increased metabolic demand as pulmonary effort increases secondary to advancing lung disease Impaired nutrient absorption secondary to pancreatic insufficiency Diets encourage high fat additives in order to meet caloric demands without increasing burden of increased volume Due to pancreatic insufficiency, patients are also required to take pancreatic enzyme supplements Nutritionists are often times critical components in the multi-disciplinary team as CF patients also have issues with vitamin and mineral deficiencies Management of CF Exacerbations ● ● There is insufficient evidence to recommend for or against continued use of inhaled antibiotics in patients treated with the same antibiotics intravenously for the treatment of an acute exacerbation of pulmonary disease. ○ Once-daily dosing of aminoglycosides is preferable to 3-times daily dosing for treatment of an acute exacerbation of pulmonary disease. ○ Empiric use of two antibiotics is recommended because inadequate coverage (i.e., using a single antibiotic to which the organism is resistant) results in dire outcomes ○ Continue use of chronic therapies for maintenance of lung health during treatment of an acute exacerbation of pulmonary disease Airway clearance therapy be increased as part of the treatment of an acute exacerbation of pulmonary disease. Cystic Fibrosis Related Diabetes ● For all intents and purposes, it’s sort of okay to think about CFRD as a Type I DM ○ ○ ● ● A relatively late complication of CF that occurs in 50% of patients > age of 30 Diagnosis is via annual oral glucose tolerance testing beginning at age 10 ○ ● In alpha cells, CFTR has a role in glucagon suppression In beta cells, CFTR promotes membrane depolarization, calcium oscillation, and insulin secretion as well insulin filled vesicle trafficking HbA1c is not recommend as it underestimates hyperglycemia due to increased RBC turnover in CF patients due to chronic inflammation The only recommended treatment for CFRD is insulin Transition of Care and Closing Thoughts ● Lifestyle considerations need to be addressed as the pediatric patient continues aging into adolescents ○ ○ ○ Alcohol ■ Excessive alcohol intake carries a higher risk in CF patients given their propensity for liver disease, pancreatitis, DM, and decreased bone density Exercise ■ Helpful in that it helps with mucus clearance as well as improves bone density Sex ■ 98% of men have absent vas deferens but it is still possible to get an STD ■ Men can still also father biological children through sperm harvesting ■ 50% of women are unable to become pregnant and pregnancy in women with FEV1 <50-60% is associated with worse outcomes Works Cited Berk, J. (2020, August 3). #1: Cystic Fibrosis Licked-ty split with Dr. Whittney Warren. The Curbsiders. https://thecurbsiders.com/cribsiders/1. Cross, J. (2006). MEDLINE, pubmed, PubMed Central, and the NLM. Editors' Bulletin, 2(1), 1–5. https://doi.org/10.1080/17521740701702115 Cystic fibrosis Foundation. Cystic Fibrosis Foundation. (n.d.). https://www.cff.org/. Cystic Fibrosis: Diagnosis, Sweat testing, and newborn screening. (2016). Cystic Fibrosis, 110–122. https://doi.org/10.3109/9781439801826-9 Dinwiddie, R. (1990). Clinical aspects of mucoid pseudomonas aeruginosa infections. Pseudomonas Infection and Alginates, 13–28. https://doi.org/10.1007/978-94-009-1836-8_2 Dornase alpha. (2015). Reactions Weekly, 1579(1), 159–159. https://doi.org/10.1007/s40278-015-11119-y Works Cited continued Galietta, L. J. V. (2006). Cystic fibrosis transmembrane conductance regulator pharmacotherapy. Cystic Fibrosis, 88–104. https://doi.org/10.1183/1025448x.00035007 Gawande, A., Specter, M., & Groopman, J. (2004, November 29). How good is my doctor? The New Yorker. https://www.newyorker.com/magazine/2004/12/06/the-bell-curve. Kelly, A., & Moran, A. (2013). Update on cystic fibrosis-related diabetes. Journal of Cystic Fibrosis, 12(4), 318–331. https://doi.org/10.1016/j.jcf.2013.02.008 Mucolytic therapy and airway CLEARANCE TECHNIQUES. (2016). Cystic Fibrosis, 256–270. https://doi.org/10.3109/9781439801826-17 Schaedel, C., de Monestrol, I., Hjelte, L., Johannesson, M., Kornfält, R., Lindblad, A., Strandvik, B., Wahlgren, L., & Holmberg, L. (2002). Predictors of deterioration of lung function in cystic fibrosis*. Pediatric Pulmonology, 33(6), 483–491. https://doi.org/10.1002/ppul.10100 Schindler, T., Michel, S., & Wilson, A. W. (2015). Nutrition management of cystic Fibrosis in the 21st century. Nutrition in Clinical Practice, 30(4), 488–500. https://doi.org/10.1177/0884533615591604