Introduction to Immunohematology: Blood Transfusion History
advertisement

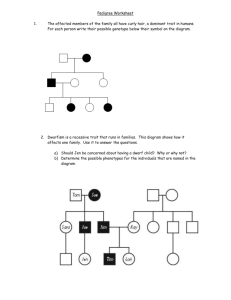
Introduction to Immunohematology Immunohematology • Immunohematology: • commonly known as , is a branch of hematology which studies antigen-antibody reactions and analogous phenomena as they relate to the pathogenesis and clinical manifestations of blood disorders. • Preparation of blood and blood components for transfusion as well as selection of appropriate, compatible components for transfusion. • Study the antibody production by the host when exposed to foreign antigens. • Blood Banking: • refers to the process of collecting, storing, and processing blood and the distribution of RBCs and blood components. • Transfusion medicine: • branch of medicine that is concerned with transfusion of blood and blood components. Historical Overview • 1492: first time a blood transfusion was recorded in history. • Pope Innocent VII received blood from three different individual. “Clotting was the principal obstacle to overcome” • 1867: • English surgeon Joseph Lister uses antiseptics to control infection during transfusions. • 1869: finding a non-toxic anticoagulant • Braxton Hicks recommends . • This was perhaps the first example of blood preservation research. • 1873-1880 US physicians transfuse milk (from cows, goats, and humans). • 1901: discovery of ABO Blood Group system • Landsteiners Law • If an agglutinogen is present on red blood cell membrane, the corresponding agglutinin must be absent in the plasma. • If an agglutinogen is absent on the red blood cell membrane, then corresponding agglutinin must be present in the plasma. • 1902: discovery of blood type AB. • Von Decastello and Sturli • 1907: • Ludvig Hektoen suggests that the safety of transfusion might be improved by crossmatching. • 1908: • French surgeon Alexis Carrel devises a way to prevent clotting by sewing the vein of the recipient directly to the artery of the donor. This vein-to-artery or direct method, known as anastomosis, is practiced by a number of physicians. • The procedure proves unfeasible for blood transfusions, but paves the way for successful organ transplantation, for which Carrel receives the Nobel Prize in 1912. • 1908: • Moreschi describes the AHG reaction (a direct way of visualizing an Ag-Ab reaction that has taken place but is not directly visible). The Ag-Ab react with each other, then, after washing to remove any unbound antibody, the AHG reagent is added and binds between the Ab that are stuck onto the Ag. • 1911: divided group A into 2 subgroups. • Von Dungern and Hirszfel • 1912: • Roger Lee, a visiting physician at the Massachusetts General Hospital, along with Paul Dudley White, develops the Lee-White clotting time. Lee’s studies lead to the terms "universal donor" and "universal recipient". • 1913: • Edward E. Lindemann was the first to succeed to perform blood transfusion. • 1914: • An unprecedented accomplishment in blood transfusion was achieved in 1914 • Albert Hustin reported the use of sodium citrate as an anticoagulant solution for transfusions. • 1915: • Lewisohn determined the minimum amount of citrate needed for anticoagulation and demonstrated its nontoxicity in small amounts. • 1916: • Development of preservative solutions to enhance the metabolism of the RBC. • Francis Rous and Turner introduced a citrate-dextrose solution for the preservation of blood. • 1927-1947: • MNSs and P blood group system was discovered. • 1930’s – RBC membrane was better understood (metabolism, deformability & permeability) • 1932: • The first hospital-based blood depot is established in a Leningrad hospital. • 1937: • Bernard Fantus, director of therapeutics at the Cook County Hospital in Chicago, establishes the first hospital blood bank in the US. In creating a hospital laboratory that can preserve and store donor blood, Fantus originates the term "blood bank." • World war II (1939-1945): • stimulated blood preservation research because the demand for blood and plasma increased. • 1941: Dr. Drew was appointed director of the first American Red Cross Blood Bank at Presbyterian Hospital • 1939-40: • The Rh blood group system is discovered by Karl Landsteiner, Alex Wiener, Philip Levine, and R.E. Stetson and is soon recognized as the cause of the majority of transfusion reactions. • 1940: • Edwin Cohn, a professor of biological chemistry at Harvard Medical School, develops cold ethanol fractionation, the process of breaking down plasma into components and products. Albumin, a protein with powerful osmotic properties, plus gamma globulin and fibrinogen are isolated and become available for clinical use. John Elliott develops the first blood container (vacuum bottle). • 1943: • Loutit and Mollison of England introduced the formula for the preservative ACD. • 1945: • Coombs, Mourant, and Race describe the use of antihuman globulin (later known as the “Coombs Test”) to identify “incomplete” antibodies. • 1947: • The American Association of Blood Banks (AABB) is formed to promote common goals among blood banking practitioners and the blood donating public. • Publication of the “journal of Clinical Investigation”. • Hospitals responded immediately, and in 1947, blood banks were established in many major cities of the United States. • 1949-1950: • The US blood collection system includes 1,500 hospital blood banks, 46 community blood centers, and 31 American Red Cross regional blood centers. • 1950: • Audrey Smith reports the use of glycerol cryoprotectant for freezing red blood cells. • 1950: • Carl Walter and W.P. Murphy, Jr., introduce the plastic bag for blood collection (safe and easy preparation of multiple blood components from a single unit of whole blood) • 1953: • The AABB Clearinghouse is established, providing a centralized system for exchanging blood among blood banks. Today, the Clearinghouse is called the National Blood Exchange. • Development of the refrigerated centrifuge in 1953 further expedites blood component therapy. SINGLE BAG : Designed for collection, storage and transfusion of whole blood. TRIPLE BAG : Separation into red cells, platelet concentrate and plasma. DOUBLE BAG : Separation of whole blood into red cell and plasma. QUADRUPLE BAG : Separation into red cells, platelet concentrate, cryoprecipitate and plasma • 1957: • The AABB forms its committee on Inspection and Accreditation to monitor the implementation of standards for blood banking. • Gibson introduced an improved preservative solution, citratephosphate-dextrose (CPD), which was less acidic and eventually replaced ACD as the standard preservative used for blood storage. • 1958: • The AABB publishes its first edition of Standards for a Blood Transfusion Service (now titled Standards for Blood Banks and Transfusion Services). • 1959: • Max Perutz of Cambridge University deciphers the molecular structure of hemoglobin, the molecule that transports oxygen and gives red blood cells their color. • 1960: • The AABB begins publication of TRANSFUSION, the first American journal wholly devoted to the science of blood banking and transfusion technology. In this same year, A. Solomon and J.L. Fahey report the first therapeutic plasmapheresis procedure • 1961: • The role of platelet concentrates in reducing mortality from hemorrhage in cancer patients is recognized. • 1962: • The first antihemophilic factor (AHF) concentrate to treat coagulation disorders in hemophilia patients is developed through fractionation. • 1964 : • Plasmapheresis is introduced as a means of collecting plasma for fractionation. • 1965: • Judith G. Pool and Angela E. Shannon report a method for producing Cryoprecipitated AHF for treatment of hemophilia. • 1967: • Rh immune globulin is commercially introduced to prevent Rh disease in the newborns of Rh-negative women. • 1969: • S. Murphy and F. Gardner demonstrate the feasibility of storing Platelets at room temperature, revolutionizing platelet transfusion therapy. • 1970: • Blood banks move toward an all-volunteer blood donor system. • 1971: • Hepatitis B surface antigen (HBsAg) testing of donated blood begins. • 1972: • Apheresis is used to extract one cellular component, returning the rest of the blood to the donor. • 1979: • A new anticoagulant preservative, CPDA-1, extends the shelf life of whole blood and red blood cells to 35 days. • Early 1980s: • With the growth of component therapy, products for coagulation disorders, and plasma exchange for the treatment of autoimmune disorders, hospital and community blood banks enter the era of transfusion medicine (doctors trained specifically in blood transfusion actively participate in patient care). • 1981: • First Acquired Immune Deficiency Syndrome (AIDS) case reported. • 1983: • Additive solutions extend the shelf life of red blood cells to 42 days. • 1984: • Human Immunodeficiency Virus (HIV) identified as cause of AIDS • 1985: • The first blood-screening test to detect HIV is licensed and quickly implemented by blood banks to protect the blood supply. • 1987: • Two tests that screen for indirect evidence of hepatitis are developed and implemented, hepatitis B core antibody (anti-HBc) and the alanine aminotransferase test (ALT). • 1989: • Human-T-Lymphotropic-Virus-I-antibody (anti-HTLV-I) testing of donated blood begins. • 1990: • Introduction of first specific test for hepatitis C, the major cause of “non-A, non-B” hepatitis. • 1992: • Testing of donor blood for HIV-1 and HIV-2 antibodies (anti-HIV-1 and anti-HIV-2) is implemented • 1996: • HIV p24 antigen testing of donated blood begins. Although the test does not completely close the HIV window, it shortens the window period. • 1997: • U.S. Gov’t issues two reports suggesting ways to improve blood safety, including regulatory reform. National Blood Data Resource Center founded by AABB to collect, analyze and distribute data on all aspects of blood banking and transfusion medicine. • 1998: • HCV lookback campaign — a public health effort to alert anyone who may have been exposed to the hepatitis C virus (HCV) through blood transfusions before July 1992 so they can receive medical counseling and treatment if needed. • 1999: • Blood community begins implementation of Nucleic Acid Amplification Testing (NAT) under the FDA’s Investigational New Drug (IND) application process. NAT employs a testing technology that directly detects the genetic materials of viruses like HCV and HIV. • 2002: • West Nile virus identified as transfusion transmissible. • 2002: • Nucleic acid amplification test (NAT) for HIV and HCV was licensed by the Food and Drug Administration. • 2003: • First-ever National Blood Foundation forum unites leaders in blood banking and transfusion medicine • 2003: • FDA issues final guidance regarding “Revised Recommendations for the Assessment of Donor Suitability and Blood and Blood Product Safety in Cases of Known or Suspected West Nile Virus Infection.” • 2003: • First West Nile Virus-positive unit of blood intercepted. • 2003: • Guidance on Implementation of New Bacteria Reduction and Detection Standard issued. • 2004: • AABB receives $2.4 Million CDC grant to reduce transfusion-transmitted HIV in Africa and South America. • 2005: • FDA approves the first West Nile virus (WNV) blood test to screen donors of blood, organs, cells and tissues. Genetics- Basic concepts Review of Basic Genetics- Terminologies • Genes→ Are units of inheritance that encode for certain traits or visible characteristics. • Chromosomes→ linear arrangement of genes. • Phenotype→ The phenotype is the physical expression of inherited genes • Genotype→ The set of alleles for a given trait carried by an organism. • Alleles→ alleles are defined as alternative forms of a gene. A portion within the chromosome that codes for the traits/genes. • Locus (loci) → specific location of genes within the chromosomes. • Autosomal→ inherited on one of the 22 pairs of autosomal chromosomes • Sex-linked→ genes inherited on the sex-chromosomes (X chromosomes) • Dominant→ a gene that is when expressed whenever the allele is present. • Recessive→ a gene that is not expressed even the allele is present. Silent gene can only be expressed if two identical genes are present. • Codominant→ a pair of genes in which neither is dominant over the other. Two different genes that are inherited at the same loci on a pair of chromosomes. • Homozygous→ having two identical genes for a given trait. • Heterozygous→ having two unidentical genes for a given trait. Mendel’s Law of Inheritance • Gregor Mendel: an Australian monk and mathematician who used sweet pea plants growing in a monastery garden to study physical traits in organisms and how they are inherited. • He studied the inheritance of several readily observable pea plant characteristics, notably flower color, seed color, and seed shape and based his first law of inheritance. Law of Independent segregation • 1st Generation→ “Parental” • Consisted of all red or all white flowers • Homozygous for red flower or • Homozygous for white flower • First-filial generation→ crossbreed of homozygous red and homozygous white flower • Second-filial generation→ crossbreed of First-filial generation. Law of independent segregation Law of Independent Assortment • States that “genes for different traits are inherited separately from each other.” • Members of one gene pair separate from one another independently of the member of other gene pairs. • This allows for all possible combinations of genes to occur in the offspring. • If a homozygote that is dominant for two different characteristics is crossed with a homozygote that is recessive for both characteristics. • the F1 generation consists of plants whose phenotype is the same as that of the dominant parent. • However, when the F1 generation is crossed in the F2 generation, two general classes of offspring are found. • Parental type: Exact characteristics as the parental generation • Reciprocal type: mixture of dominant feature and recessive feature. Law of Independent assortment Inheritance Patterns • The interpretation of pedigree analysis requires the understanding of various standard conventions in the representation of data figures. • Males are always represented by squares and females by circles. • A line joining a male and female indicates a mating between the two, and offspring are indicated by a vertical line. • A double line between a male and female indicates a consanguineous mating. • A stillbirth or abortion is indicated by a small black circle. • Deceased family members have a line crossed through them. • The propositus in the pedigree is indicated by an arrow pointing to it and indicates the most interesting or important member of the pedigree. Different Inheritance Patterns • Autosomal Recessive • X-linked Dominant • X-linked Recessive • Autosomal Dominant Autosomal Recessive inheritance • “Autosomal” refers to traits that are not carried on the sex chromosomes. • A recessive trait is carried by either parent or both parents but is not generally seen at the phenotypic level unless both parents carry the trait. • In some cases a recessive trait can be genetically expressed in a heterozygous individual but is often not seen at the phenotypic level. X-linked Dominant Inheritance • If the father carries the trait on his X chromosome, he has no sons with the trait, but all his daughters will have the trait. • Women can be either homozygous or heterozygous for an Xlinked trait. • and therefore when mothers have an X-linked trait, their daughters inherit the trait in a manner identical to autosomal inheritance. • The sons have a 50 percent chance of inheriting the trait or not. • Because the trait is dominant, the sons who inherit it will express the trait. • The Xga blood group system is one of the few blood group systems that follow an X-linked inheritance pattern. X-linked Recessive Inheritance • the father always expresses the trait but never passes it on to his sons. • The father always passes the trait to all his daughters, who are then carriers of the trait. • In the homozygous state, X’Y, the males will express the trait, whereas only the rare homozygous females, X’X’, will express the trait. • with an X-linked recessive trait, a disease-carrying gene can be passed from generation to generation with many individuals not affected. Autosomal Dominant Inheritance • All the members of a family that carry the allele show the physical characteristic. • Generally, each individual with the trait has at least one parent with the trait • Unlike X-linked traits, autosomal traits usually do not show a difference in the distribution between males and females, and this can be a helpful clue in their evaluation. Punnett Squares • A Punnett square illustrates the probabilities of phenotypes from known or inferred genotypes • Portrays the potential offspring’s phenotypes or parent’s probable genotype