Respiratory Physiology Lecture: System Functions & Structure
advertisement

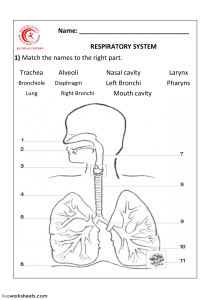
RESPIRATORY PHYSIOLOGY LECTURE 1 DR R F Mapanga Lecturer Availability • Available on arrangement via email or telegram • Will be in the Department of Biomedical Sciences, Physiology Unit, Main Campus, office 72. • Always available on email – mapangarudo@gmail.com and also on Telegram username: RFionaMaps. Learning outcomes • By the end of the lecture students should be able to: • Describe the function (s) of the respiratory system • Distinguish between internal and external respiration • Describe the structural and functional differences in the different zones of the respiratory tract • Explain the roles of the different types of cells in the respiratory tract • Relate the knowledge acquired to some clinical examples The human respiratory system The lungs The human respiratory system • What is its primary function? • The transport of gases in and out of the body also known as respiration: a. External Respiration: O2 absorption & CO2 removal from body b. Internal respiration: O2 utilization & CO2 production by cells & gaseous exchanges between cells & their fluid medium • Other functions include: • • • • • Blood reservoir ~500 - 1000ml Metabolism- synthesis and catabolism Immunological and mechanical defence Traps and dissolves blood clots Regulation of blood pH Organization of the respiratory system • There are two lungs, the right and the left, each divided into lobes • The right has three lobes and the left has two lobes • Lungs are made up mostly of alveoli ~150 million per lung & these are the sites of gas exchange with blood • Inspiration/ inhalation is the movement of air from the external environment through the airways into the alveoli during breathing • Expiration is movement in the opposite direction • At rest ~4 L of air enters and leave the alveoli per min while 5L of blood passes through the pulmonary capillary • During heavy exercise, airflow can increase 30 to 40 fold & blood flow 5 to 6 fold Regions of the respiratory system • Airflow through the system can be broken down into • Upper airway (gas transport) • consists of the nose, mouth, pharynx, and larynx • The conducting airway/zone (only gas transport) • Consists of trachea, bronchi, bronchioles & terminal bronchioles • Upper airway & conducting zone = anatomic dead space (~150ml) • The alveolar airway - respiratory zone (gas exchange occurs) • Consists of respiratory bronchioles, alveolar ducts and alveoli sacs The conducting zone • Larynx opens into the trachea, which in turn branches into two bronchi, one of which enters each lung • Walls of trachea and bronchi contain cartilage for support and also making them cylindrical • First airway branches with no cartilage are known as bronchioles The conducting zone • The conducting zone serves a number of functions: • Provides a low resistance pathway for air flow • Defense against microbes & other toxins – carried out by cilia, mucus & phagocytes • Epithelial cells secrete a number of molecules • immunoglubulins-IgA, collectins-surfactant proteins A and D, defensins, ROS & RNS • Chemokines & cytokines that recruit traditional immune cells • Muco-ciliary escalator can move very small particles (~2-5 μm) away from the lungs at 16mm/min • Cilia bathed in periciliary fluid & a mucus layer on top • Warms & moisten the air Cellular transition from conducting airway to the alveolus Clinical correlation • Absence of ciliary motility is common in smokers and can also be as a result of genetic or environmental conditions • This can result in chronic sinusitis, recurring lung infections and bronchiectasis • Examples are cystic fibrosis & primary ciliary dyskinesia (Kartagener’s) (read more) Cystic fibrosis • A gene that codes for the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) located on the longer arm of chromosome 7 is abnormal • A regulated chloride channel on the apical membrane of the epithelia is defective leading to enhanced movement of water and sodium out of the airways. • secretions are sticky reducing the periciliary layer and inhibiting mucociliary escalator CFTR https://youtu.be/6IbP1ASGv9w Innervation of the bronchi • The walls of the bronchi and bronchioles are innervated by ANS • Nerve cells in the airways stimulated by: • mechanical stimuli • presence of unwanted substances in the airways (inhaled dusts, cold air, noxious gases, and cigarette smoke) • In turn, they signal the respiratory centers to contract the respiratory muscles and initiate sneeze or cough reflexes. • The receptors show rapid adaptation when they are continuously stimulated to limit sneeze and cough under normal conditions. Innervation of bronchi • The β2 -adrenergic receptors help mediate bronchodilation & increase bronchial secretions (e.g., mucus) • α1 -adrenergic receptors inhibit secretions. • Cholinergic – bronchoconstriction • Non cholinergic –non adrenergic • are modulators of the pulmonary circulation that are not inhibited by adrenergic or cholinergic blockade • response can be either vasodilation or constriction. Alveolar airway – respiratory zone • There are more than 20 generations of branches in the lungs – each resulting in narrower, shorter and more numerous tubes • Alveoli begin to appear attached to respiratory bronchioles and increase in number in the alveolar ducts until they end in clusters of grapelike structures known as alveoli Alveolar airway – respiratory zone • The divisions increase surface area from ~2.5 cm2 in the trachea to ~11,800 cm2 in the alveoli. • Humans have 300 million alveoli, and the total area of the alveolar walls in contact with capillaries in both lungs is ~75 m2 Alveolar airway – respiratory zone • The air and blood are separated only by the alveolar epithelium and the capillary endothelium, so they are about 0.2 – 0.5 μm apart • Velocity of airflow declines to very low values Alveolar airway – respiratory zone • The alveoli are lined by two types of epithelial cells. • Type I cells • flat cells with large cytoplasmic extensions • primary lining cells of the alveoli • cover ~ 95% of the alveolar epithelial surface area. Alveolar airway – respiratory zone • Type II cells • granular pneumocytes - thicker • contain lamellar bodies that are exocytosed to release tubular myelin • Make up 5% of the surface area • important in alveolar repair. • They produce surfactant which reduces surface tension Alveolar airway – respiratory zone • The alveoli also contain other specialized cells e.g. • pulmonary alveolar macrophages (PAMs, or AMs), • • • • • • • • an important component of the pulmonary defense system originate from the bone marrow. PAMs are actively phagocytic and ingest small particles Their effect can be detrimental when they ingest large amounts of the substances in cigarette smoke or other irritants, they may release lysosomal products into the extracellular space to cause inflammation lymphocytes, plasma cells, neuroendocrine cells, mast cells. STRUCTURE FUNCTION nose / nasal cavity warms, moistens, & filters air as it is inhaled pharynx (throat) passageway for air, leads to trachea larynx the voice box, where vocal chords are located trachea (windpipe) bronchi tube from pharynx to bronchi rings of cartilage provide structure, keeps the windpipe "open" trachea is lined with fine hairs called cilia which filter air before it reaches the lungs two branches at the end of the trachea, each lead to a lung bronchioles a network of smaller branches leading from the bronchi into the lung tissue & ultimately to air sacs alveoli the functional respiratory units in the lung where gases (oxygen & carbon dioxide) are exchanged (enter & exit the blood stream) Summary • Identified the functions of the respiratory system • Described the different regions of the respiratory system according to their ultimate functions in external respiration • Described the cellular make up difference of the respiratory system • Explained the different functions of the various types of cells along the respiratory system • Connected the information to some clinical disease states