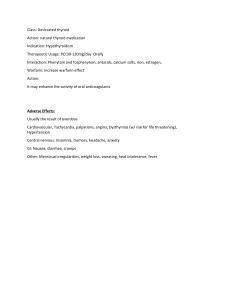
Rex Stephen S. de Ungria, MD (Resident-in-Charge) B.G. 45 y/o Female Date of Admission: May 22, 2019 Vaginal Spotting 1 month PTA 16 days PTA 11 days PTA • (+) cessation of menses on April 2019 • Took PT reveals negative result • (+) persistence of above symptoms now acc by constipation and bloatedness, sought consult and revealed (+)PT • TVS-H-mole/molar pregnancy • Labs: B-Hcg >10,000 IU/ml and HBsAg Reactive • Sought consult • Labs done which revealed same result • Was advised for possible operation 7 days PTA 1 day PTA • Consulted in our institution with no subjective complaints • Dx: G6P5 (5005) Molar Pregnancy 11 1/7 wks AOG • Possible TAH-BS • Labs: TSH-0.01(L), FT3-5.99 (H), FT4-2.22 • Given PTU 50mg tab • (+) Vaginal spotting not asscoiated with other symptoms hence admitted ADMISSION HEENT: (-) headache (-) Proptosis CARDIOVASCULAR :(-) chest pain (-) easy fatigability (-) palpitations (-) orthopnea (-) PND RESPIRATORY: (-) cough (-)dyspnea (-) shortness of breath (-) hemoptysis (-)pleuritic chest pain GIT: (-) changes in bowel habit (-) vomiting (-) diarrhea (-) melena (-) constipation NEURO: (-) loss of consciousness (-) seizures GUT: (-) polyuria (-) urgency (-) frequency (-) oliguria (-) anuria MUSCULOSKELETAL: (-) muscle pain (-) swelling (-) bone defmormity (-) weakness (-) atrophy ENDOCRINE: (+) heat intolerance (-) cold intolerance (-) weight gain (-) weight loss (-) polyuria (-) polydipsia (-) polyphagia HEMATOLOGIC: (-) bruisability (-) easy fatigability (-) pallor (+) Hyperthyroidism (May 2019) PTU 50mg tab (+) PTB (2017) Completed treatment (-) Hypertension (-) Bronchial Asthma/COPD (-) known allergies (+) Prev Incision and Drainage of Abscess left Breast in 2008 which denies of any anesthesia complications Non smoker Non alcoholic beverage drinker conscious, coherent, ambulatory VS: BP 110/70 HR 94/min RR 18/min height 5’4’’ weight 46.5 kg Pink palpebral conjunctivae, anicteric sclerae No naso-aural discharge, no TPC, tonsils not enlarged Mallampati II, TMD 5cms, MO 4-5cms, (-) dentures Supple neck with good mobility SCE, clear & equal BS AP, NRRR, (-) murmurs appreciated Flabby soft, abdomen, nontender Extremities: pulses full and equal (-) edema Neuro Examination: GCS 15 (E4 V5 M6) Immunology TSH- 0.01 FT3- 5.99 FT4- 2.22 and Serology (5/21/19) Chemistry (5/18/19) FBS – 3.74 BUN – 2.8 mmol/L Creatinine – 52.40 umol/L SGPT(ALT) – 16.30 SGOT (AST) – 19.20 Serum K – 4.15 mmol/L Serum Na – 138.0 mmol/L Serum Cl – 101.10 CBC (5/18/19) Hemoglobin – 136 Hematocrit – 0.42 HEMATOLOGY (5/18/19) Prothrombin Time - 10.9 Protime Activity - 100% Activated Partial Thromboplastin Time – 28.6 Bleeding Time - 2.00 Chest Minimal hypertrophic degenerative changes of the thoracic spine otherwise normal chest Tumor Xray (5/17/19) Markers (5/9/19) >10,000 mIU/ml Serology (5/9/19) HbsAg - Reactive Given the very high thyroid hormone levels, preoperative thyroid storm should be kept in mind There is not enough time available for optimizing patient’s clinical and biochemical condition ASA III MAL II Medical Problems H-mole pregnancy Hyperthyroidism HBsAg - reactive Combined Spinal and Epidural Anesthesia Administer IV fluids Administer PTU 200-400mg via NGT Administer Hydrocortisone 50-100mg IV or Dexamethasone 8-12mg/day Beta blockers titrated to achieve heart rate below 90 beats per minute • Awake with ongoing IVF D5LR 1L • BP 135/80; HR 69/min; RR 20/min; SPO2 100% • Hooked to O2 2-3LPM/NC Prior to Inductio n 9:50AM • VS: BP 100/60 HR 80/min RR 18 SPO2 100%, hooked to O2 3LPM/NC • LLDP; Asepsis and antisepsis; Local Infiltration w/ Lidocaine 2%;Epidural tap L3 L4 using touhy G18, (+) Inductio LORTA, catheter (4cm) threaded cephalad with ease; (-) n CSF (-) blood (-) paresthesias preceeded with spinal tap L4 L5 Quincke SNG 25 (+) CSF clear & free-flowing (10:12A M) • Bupivacaine 0.5% Heavy 15mg, Spinal Level T6, catheter secured (10:15A M10:25am ) • • • • VS: BP 130/80 HR 90/min SPO2 100% Cefuroxime 1.5g IV Midazolam1.5mg Hydrocortisone 100mg IV TAHBS Started 19mins from Induction 24mins of the procedure 44 mins of the procedure • VS: BP: 90/60 HR: 65/min RR 18/min SPO2 98% Temp-33.8 C • BP 80/45mmHg HR 55/min T-33.9 C • Ephedrine 5mg/IV • BP 80/40mmHg HR 50/min T-33.9 C • Ephedrine 5mg/IV 65mins of the procedure 159 mins of the procedure • BP: 120/70 HR 65/min SPO2 99% T-33.8C • Levobupivacaine 15mg via epidural catheter, then 10mg after 10 mins, then 25mg after 10 mins • BP 120/80 HR 60/min SPO2 99% • Epidural analgesia: Morphine Sulfate 0.2mg FIRST DOSE given TAHBS • drowsy to arousable, follow commands ended • BP 120/70; HR 68/min; RR 18/min; SPO2 99% after 179 mins s/p TAHBS • Drowsy to arousable • BP 120/80 HR 85bpm • (-)NVE • SCE, clear BS Post-op Orders • O2 2-3LPM/NC • IVF: PLR 1L x 8 hours • Ketorolac 30mg/IV q6 • Paracetamol 600mg IV PRN for pain Post-op Orders • Epidural Analgesia as ff: • Morphine SO4 0.2mg in 50cc PNSS, 10CC q 12 hrs x 3 doses c/o AROD At the ward (12th post-op hour) • Conscious, coherent • BP110/70 HR 78 • No subjective complaints • 2ND Dose of Morphine 0.2mg in 10 ml given via epidural catheter At the ward (24th post op hour) • Consciou, coherent • No subjective complaints • BP 90/60 HR 70 • Pain scale: 4/10 • 3RD dose of Morphine was not given At the ward (36th post-op hour) • Conscious, coherent • No subjective complaints • BP 90/50 HR 68 • PS: 3/10 • Still 3rd dose of Morphine was not given. • Epidural Catheter remove blue tip intact • Pain med shifted to oral by main service HYPERTHYROIDISM Hyperthyroidism refers to hyperfunctioning of the thyroid gland, with excessive secretion of active thyroid hormones. result from one of three pathologic processes: 1. Graves disease 2. Toxic multinodular goiter 3. Toxic adenoma Signs and Symptoms: Regardless of the cause, the signs and symptoms of hyperthyroidism are those of a hypermetabolic state. The patient is anxious, restless, and hyperkinetic and may be emotionally unstable. Signs and Symptoms: Wasting, weakness, and fatigue of the proximal limb muscles are common. The patient usually complains of extreme fatigue but an inability to sleep. Signs and Symptoms: Increased bone turnover and osteoporosis may occur. A fine tremor of the hands and hyperactive tendon reflexes are common. Weight loss despite an increased appetite occurs secondary to increased calorigenesis. Bowel movements are frequent and diarrhea is not uncommon. The cardiovascular system is most threatened by hypermetabolism of peripheral tissues, increased cardiac work with tachycardia, dysrhythmias (commonly atrial) and palpitations, a hyperdynamic circulation, increased myocardial contractility and cardiac output, and cardiomegaly. The cardiovascular system is most threatened by: • • • • • • hypermetabolism of peripheral tissues increased cardiac work with tachycardia dysrhythmias (commonly atrial) palpitations hyperdynamic circulation increased myocardial contractility and cardiac output cardiomegaly • Graves disease • • • • toxic diffuse goiter etiology is unknown occurs in females (female/male ratio is 7:1) between the ages of 20 and 40 years appears to be a systemic autoimmune disease • Graves disease • caused by thyroid-stimulating antibodies that bind to TSH receptors in the thyroid, activating adenylcyclase and stimulating thyroid growth, vascularity, and hypersecretion of T4 and T3 • thyroid is usually diffusely enlarged, becoming two to three times its normal size • Graves disease • • ophthalmopathy occurs in 30% of cases and may include upper lid retraction, a wide-eyed stare, muscle weakness, proptosis, and an increase in intraocular pressure Diagnosis is confirmed by the presence of thyroid-stimulating antibodies in the context of a low TSH level and elevated T4 and T3 levels • Toxic multinodular goiter • • • • arises from long-standing simple goiter occurs mostly in patients older than age 50 may present with extreme thyroid enlargement that can cause dysphagia, globus sensation, and possibly inspiratory stridor from tracheal compression this is common when the mass extends into the thoracic inlet behind the sternum • Toxic multinodular goiter • • In severe cases, superior vena cava obstruction syndrome may also be present diagnosis is confirmed by a thyroid scan demonstrating “hot” patchy foci throughout the gland or one or two “hot” nodules • Treatment • first line of treatment for hyperthyroidism is an antithyroid drugs • • Methimazole Propylthiouracil (PTU) • Treatment • • • • interfere with the synthesis of thyroid hormones by inhibiting organification and coupling PTU has the added advantage of inhibiting the peripheral conversion of T4 to T3 Euthyroid state can almost always be achieved in 6–8 weeks with either drug if a sufficient dosage is used • Treatment • • • Iodide in high concentrations inhibits release of hormones from the hyperfunctioning gland Inorganic iodide inhibits iodide organification and thyroid hormone release This phenomenon is known as the WOLF-CHAIKOFF EFFECT • Treatment • High concentrations of iodide decrease all phases of thyroid synthesis and release and result in reduced gland size and possibly a decrease in vascularity • Treatment • effects occur immediately but are short-lived • reserved for preparing hyperthyroid patients for surgery, managing patients with actual or impending thyroid storm, and treating patients with severe thyrocardiac disease • Treatment • There is no need to delay surgery in a patient with otherwise well-controlled thyrotoxicosis in order to initiate iodide therapy • • Treatment IODIDE • • administered orally as a saturated solution of potassium iodide (SSKI) 3 drops PO every 8 hours for 10–14 days • Treatment • radiographic contrast dye ipodate or iopanoic acid (0.5–3.0 g every day) contains iodide and demonstrates beneficial effects similar to those of inorganic iodide • inhibits the peripheral conversion of T4 to T3 • antagonize thyroid hormone binding to receptors • Treatment • Antithyroid drug therapy should precede initiation of iodide treatment, because administration of iodide alone will increase thyroid hormone stores and exacerbate the thyrotoxic state • Treatment • What about patients who are allergic to iodide? • Lithium carbonate 300 mg PO every 6 hours may be given in place of potassium iodide or ipodate • Treatment • β-Adrenergic antagonists • • • may relieve signs and symptoms of increased adrenergic activity such as anxiety, sweating, heat intolerance, tremors, and tachycardia Propranolol offers the added features of impairing the peripheral conversion of T4 to T3 over 1-2 weeks Propanolol given over 12-24 hours decreases tachycardia, heat intolerance, anxiety and tremor • Treatment • Ablative therapy with radioactive iodine 131 (131I) or surgery • is recommended for patients with Graves disease for whom medical management has failed, as well as for patients with toxic multinodular goiter or a toxic adenoma • Treatment • • • Hyperthyroidism during pregnancy is treated with low dosages of antithyroid drugs these drugs do cross the placenta and can cause fetal hypothyroidism But if the mother remains euthyroid while taking small dosages of an antithyroid drug, the occurrence of fetal hypothyroidism is rare • Treatment • Radioactive iodine treatment is contraindicated during pregnancy, as is oral iodide therapy, because it can cause fetal goiter and hypothyroidism • Thyroid storm occurring in pregnancy is managed in the same way as in nonpregnant patients • MANAGEMENT OF ANESTHESIA • hyperthyroid patients undergoing surgery, Euthyroidism should definitely be established preoperatively • Elective cases should wait a substantial time (6–8 weeks) for the anti thyroid drugs to become effective • MANAGEMENT OF ANESTHESIA In emergency cases: • • • • Use of an IV β-blocker, ipodate, glucocorticoids, and PTU is usually necessary. No IV preparation of PTU is available so it must be taken orally, via a nasogastric tube, or rectally Glucocorticoids (dexamethasone 2 mg IV every 6 hours) should be administered to decrease hormone release and reduce the peripheral conversion of T4 to T3 • MANAGEMENT OF ANESTHESIA • Evaluation of the upper airway for evidence of tracheal compression or deviation caused by a goiter is an important part of the preoperative evaluation • MANAGEMENT OF ANESTHESIA • Establishment of adequate anesthetic depth is extremely important to avoid exaggerated sympathetic nervous system responses • MANAGEMENT OF ANESTHESIA • Drugs that stimulate the sympathetic nervous system should be avoided: • • • • • Ketamine Pancuronium Atropine Ephedrine Epinephrine • MANAGEMENT OF ANESTHESIA • For maintenance of anesthesia, any of the potent inhalation agents may be used • A concern in hyperthyroid patients is organ toxicity secondary to an increase in drug metabolism • Hyperthyroid patients may have co-existing muscle disease (e.g. myasthenia gravis) with reduced requirements for the nondepolarizing muscle relaxants; therefore careful titration is required • MANAGEMENT OF ANESTHESIA • For treatment of intraoperative hypotension, a direct-acting vasopressor (phenylephrine) is preferred • Ephedrine, epinephrine, norepinephrine, and dopamine should be avoided or administered in extremely low doses to prevent exaggerated hemodynamic responses • MANAGEMENT OF ANESTHESIA • Regional anesthesia can be safely performed and in fact may be a preferred technique • Epinephrine-containing local anesthetic solutions should be avoided • Removal of the thyrotoxic gland does not mean immediate resolution of thyrotoxicosis • MANAGEMENT OF ANESTHESIA • The half-life of T4 is 7–8 days • β-blocker therapy may need to be continued in the postoperative period • THYROID STORM • a life-threatening exacerbation of hyperthyroidism precipitated by trauma, infection, medical illness, or surgery • THYROID STORM • can present with similar intraoperative and postoperative signs and symptoms like Malignant Hyperthermia such as: • • • hyperpyrexia tachycardia hypermetabolism • THYROID STORM • most often occurs in the postoperative period in untreated or inadequately treated hyperthyroid patients after emergency surgery • Patients manifest extreme anxiety, fever, tachycardia, cardiovascular instability, and altered consciousness • THYROID STORM • Treatment includes rapid alleviation of thyrotoxicosis and general supportive care • Dehydration is managed with IV administration of glucose-containing crystalloid solutions • Fever is countered by cooling measures such as cooling blanket, ice packs and administration of cool humidified oxygen • THYROID STORM • β-Blockers should be titrated to decrease heart rate to less than 90 beats per minute • Dexamethasone 2 mg every 6 hours or cortisol 100–200 mg every 8 hours can be used to decrease hormone release and conversion of T4 to T3 • THYROID STORM • • Antithyroid drugs (PTU 200–400 mg every 8 hours) administered through a nasogastric tube, orally, or rectally • THYROID STORM • If circulatory shock is present, IV administration of a direct vasopressor (phenylephrine) is indicated • β-adrenergic blocker or digitalis is recommended for atrial fibrillation accompanied by a fast ventricular response • THYROID STORM • Serum thyroid hormone levels generally return to normal within 24–48 hours, and recovery occurs within 1 week • The mortality rate for thyroid storm remains surprisingly high at approximately 20%. Good Evening!!!