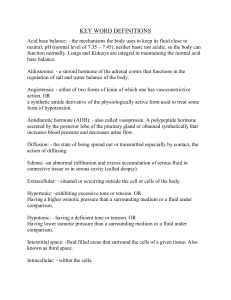
Final Exam Review Topics to Study 1. RAAS system a. BNP versus troponin~Brain natriuretic peptide- peptide that is secreted from the heart ventricular muscle – these peptides are secreted in response to increased blood volume and blood pressure, which stretch the heart tissue. ~B-type natriuretic peptide BNP- a peptide produced and released by the ventricles when the patient has fluid overload as a result of heart failure. Used to diagnosed HF, particularly diastolic HF in the patient with dyspnea. Early warning symptoms that the heart has decreased compliance long before the symptoms occur. ~Troponin- is a myocardial muscle protein released into the bloodstream with injury to myocardial muscle. The rise of troponin indicates cardiac necrosis or acute MI. It can occur several hours after the onset of chest pain. Levels should be assessed again in 3 to 6 hours. b. Aldosterone- response to low blood pressure by water and sodium saving hormone because it causes the kidney reabsorb water and sodium, preventing them from being excreted into the urine. The response allows more water and sodium to be returned to the blood, increasing blood pressure, blood volume, and perfusion 2. Cardiac catheterization ~Most definite but most invasive test in the diagnosis of heart disease. It is a study of right or left side of the heart and the coronary arteries. Palpitations may occur, feeling heat or hot flash and the desire to cough. Inform consent must be obtained. Renal dysfunction must be assessed. Contrast induced renal dysfunction can result from vasoconstriction and the direct toxic effect of the contrast agent on the renal tubules. Hydrate patient before and after cardiac catheterization. ~Complications such as PE, thrombophlebitis, vagal response --- Right sided heart catheterization. Mi, stroke, arterial bleeding, thromboembolism, dysrhythmias----L sided heart catheterization. Cardiac tamponade, hypovolemia, pulmonary edema, hematoma or blood loss at the insertion site, and reaction to contrast medium for both R and L sided Cath. Obtain 12 lead. ~Report chest pain, dysrhythmias, decreased LOC, bleeding (hold bleeding site)~, hematoma, and dramatic change of peripheral pulses in the affected extremity and RRT. 3. Complications of left sided heart failure ~Pulmonary problems or congestion- hacking cough, worse at night, ~Dyspnea, breathlessness, crackles wheezes in the lungs, frothy, pink-tinged sputum, tachypnea, S3 and S4 summation gallop ~Hypoxia, hypoxemia, pulsus alternans, DO, orthopnea, paroxysmal nocturnal dyspnea (PDN) ~Decrease cardiac output- oliguria, angina, restlessness, tachycardia, pallor, cool extremities ~Crackles in both lungs, tachycardia, tachypnea, S3 gallop 4. Lithium , same as amiodarone --- causes hypothyroidism and diabetes insipidus. ~It can impair thyroid hormone production- hypotension, bradycardia, decreased activity tolerance, dysrhythmias, enlarge heart, hypoventilation, pleural effusion, dyspnea, lethargy, slowness speech ~If taken a long time especially with older clients, it can cause lithium toxicity and show s/s of hypothyroidism ~Inadequate cellular regulation- sleeping 14 to 16 hours, generalized weakness, anorexia, muscles aches, paresthesia, constipation, cold intolerance, decreased libido, ~Can cause hypothyroidism ~An antagonist for hyponatremia—caused by SIADH ~Specific gravity decreased – 1.005 ---low osmolarity --- (50-200 mOsm ) ~Drug related DI – dehydration, excessive urination, excessive thirst, shock from fluid loss ~Can exacerbate psoriasis 5. Hypoglycemia protocol ~Pt blood glucose <40 and if pt is unable to swallow and unconscious ~Inject 1 g of glucagon ~Recheck blood glucose afterwards ~Give 15 mg of orange juice 6. Trach decannulation procedures ~Always have the size of tracheostomy size and one smaller at the bedside along with a tracheostomy insertion tray. Ventilate pt, using manual resuscitation bag and facemask while the other nurse calls RRT. ~Extend pt’s neck and open tissues or the stoma with curved Kelly clamp to secure the airway. 7. ABG 8. Small versus large bowel obstruction ~Small bowel obstruction ~Abdominal discomfort or pain possibly accompanied by visible peristalsis waves in upper and middle abdomen ~Upper and epigastric abdominal distention ~Nausea, and early, profuse vomiting (may contain fecal material) ~Obstipation ~Severe fluid and electrolyte imbalances ~Metabolic alkalosis (not always present) ~Large bowel obstruction ~Intermittent lower abdominal cramping ~Lower abdominal distention ~Minimal or no vomiting ~Obstipation or ribbon-like stools ~No major fluid, and electrolyte imbalances ~Metabolic acidosis (not always present) ~Obstruction above ileum –causes early profuse vomiting of partially digested food and chyme, changing to watery contents containing bile and mucus ~Obstruction in the large intestine-- produces vomitus with an orange, brown color and foul odor caused by bacterial overgrowth, which may be fecal contamination 9. Assessing airway ~Pulse oximeter to determine oxygen saturation ~Hypoventilation ~Stridor ~Pt not breathing ~Upper obstruction ~Anxiety ~Low O2 saturation ~Post op patients ~CPR initiation ~Unconscious patient 10. Metabolism 11. Cervical spine injuries ~Controls diaphragm—breathing ~Assess airway ~Assess breathing depth, rate, respirations ~Assess swallowing or gag reflex 12. Malignant Hyperthermia ~Ask pt about hx of malignant hyperthermia an inherited muscle disorder which is acute life threatening complications of certain drugs used for general anesthesia. Causes increased calcium levels in muscle cells and increased muscle metabolism. Serum calcium and potassium levels are increased, and is metabolic rate, leading to acidosis, cardiac dysrhythmias, and high body temperature. ~ Elevated end tidal carbon dioxide, decreased oxygen saturation, tachycardia, muscle rigidity of the jaw and upper chest, hypotension, tachypnea, skin mottling, cyanosis, myoglobinuria--muscle protein in the urine due to rhabdomyolysis. ~Dantrolene is the approved treatment of MH ~Post-op complications ~Happens when patient before, during, or after surgery when anesthesia is given. ~Provide heated blanket, check vs, assess pt such as skin temperature, shivering 13. Extravasation versus infiltration ~Vesicant medications (amiodarone, vancomycin, ciprofloxacin and venous irritants that have a pH less than 5.0, they can cause severe tissue damage if they escape into the subcutaneous—do not use midline catheters. ~Extravasation- blistering, tissue sloughing, or necrosis from infiltration into the surrounding tissue. ~Infiltration- occurs when Iv solution leaks into the tissues around the vein. The early sign of infiltration swelling, coolness, tingling, or redness. Dc the drug immediately –remove catheter. 14. Adrenal gland hypofunction ~Inadequate secretion of adrenocorticotropic hormone (ACTH) –hypopituitarism ~Addison’s crisis—the need for cortisol and aldosterone ---hypoglycemia, shock, hyperkalemiaassociated cardiac problems ~Lethargy, increased salt craving, GI problems, anorexia, nausea and vomiting, diarrhea, abdominal pain, wt loss, hx of radiation and abdomen ~Assess for hypoglycemia (tachycardia, tremors, sweating, headaches), fluid depletion, hyperkalemia (dysrhythmias and cardiac arrest), hyponatremia (hypotension, decreased LOC--first indicators). ~Anemia, hyponatremia, hypotension, hyperkalemia, hypercalcemia ~Nursing priority— prevent cardiac arrest, dysrhythmias, fluid loss, hypoglycemia, hypotension ~Labs- increased H&H, BUN, ~Weigh pt for fluid loss or gain and assess VS 1 to 4 hrs ~Hyperpigmentation- Vitiligo ~Occurs in sudden cessation of long-term, high dose corticosteroids 15. Hormones of the anterior & posterior pituitary ~AP ~Thyroid-stimulating hormone or thyrotropin, TSH (thyroid) ~Adrenocorticotropic hormone or corticotropin, ACTH (adrenal cortex) ~Luteinizing hormone, LH or Leydig cell-stimulating hormone, LCSH (Ovary and testes) ~Follicle-stimulating hormone, FSH (Ovary and testes) ~Prolactin, PRL (Mammary glands) ~Growth hormone, GH (Bone and tissue) ~Melanocytes-stimulating hormone, MSH (Melanocytes) ~PP ~Oxytocin ~Antidiuretic Hormone (ADH)- vasopressin