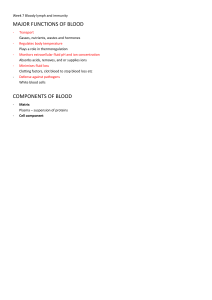
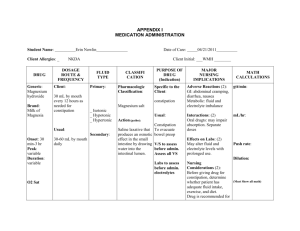
Fundamentals of Nursing\ Theory Fluid and Electrolyte Fluid and Electrolyte Dr. Sabah Abdullah Lec.4 Terms: Inter- Between Intra- Within Extra- Outside Hypo- Under, beneath, deficient Hyper- Above, beyond, excessive 1 Fundamentals of Nursing\ Theory Fluid and Electrolyte Body fluids: the term refers to both fluid and electrolyte. Homeostasis: is the state of equilibrium of internal body environment and balance of body fluid. Fluid compartments: The body’s fluid is contained within three compartments: 1. Cells (Cars) 2. Blood vessels. (The lines) 3. Tissue space (space between the cells and blood vessels).(space between cars) Cell BODY FLUIDM COMPARTMENT blood vessles Distribution of body fluid: 1. Intracellular fluid: fluid found inside the cells. 2. Extracellular fluid: fluid found outside the cells. a. Intravascular fluid: plasma b. Interstitial fluid: fluids surround the cells. Movement of Body Fluids and Electrolytes - Small particles such as ions, oxygen, and carbon dioxide move easily across cells membranes. larger molecules such as glucose and proteins have more difficulty moving between fluid compartments. Solutes محلول مذابare substances dissolved in a liquid. For example, when sugar is added to coffee, the sugar is the solute. Solute: crystalloids + colloids A solvent مذيبis the component of a solution that can dissolve a solute. In the body, water is the solvent; the solutes include electrolytes, gases such as oxygen and carbon dioxide, glucose, urea, amino acids, and proteins 2 tissue space Fundamentals of Nursing\ Theory Fluid and Electrolyte Osmosis: the movement of water molecules from a less concentrated area to a more concentrated area in an attempt to equalize the concentration of solutions on two sides of a membrane. Osmolality: The concentration of solutes in body fluids Tonicity: refer to the osmolality of one solution in relation to another solution. Electrolytes: charged ions capable of conducting electricity, are present in all body fluids and fluid compartments. Sodium (Na+), Potassium (K+), Calcium (Ca2+), Magnesium (Mg2+), Chloride (Cl− ) Electrolytes Functions is: • Maintaining fluid balance. • Contributing to acid–base regulation . • Facilitating enzyme reactions. • Transmitting neuromuscular reactions. Regulating Body Fluids: FLUID INTAKE - Average adult drinks about 1,500 mL/day The additional 1,000-mL volume is acquired from foods and from the oxidation of these foods during metabolic processes. The thirst mechanism is the primary regulator of fluid intake. The thirst center is located in the hypothalamus of the brain. FLUID OUTPUT The routes of fluid output include: - Urine Normal urine output for an adult is 1,400 to 1,500 mL per 24 hours, or at least 0.5 mL per kilogram per hour. • Feces 100–200 ml 24 • Insensible losses (through the skin as perspiration and through the lungs as water vapor in expired air). - Insensible losses Lungs 350–400 Skin 350–400 Sweat 100 3 Fundamentals of Nursing\ Theory Fluid and Electrolyte FACTORS AFFECTING BODY FLUID, ELECTROLYTES, AND ACID–BASE BALANCE: 1. 2. 3. 4. 5. Age : can create critical fluid imbalances in children much more rapidly than adult Infants 28 days-1 year: because their higher metabolic rate increases fluid loss. Kidney: immature kidneys are less able to conserve water. Respiratory rate : increases insensible fluid losses. Sex and Body Size: Water accounts for approximately 60% of an adult man’s weight, but approximately 52% of an adult woman’s weight. In someone who is obese this percentage may be even lower, with water accounting for only 30% to 40% of the person’s weight. 6. Environmental Temperature: People with an illness and those participating in strenuous activity are at increased risk for fluid and electrolyte imbalances when the environmental temperature is high. Both electrolytes and water are lost through sweating. When only water is replaced, electrolyte depletion is a risk 7. Lifestyle : Lifestyle factors such as diet, exercise, stress, and alcohol consumption affect fluid, electrolyte, and acid–base balance. DISTURBANCES IN FLUID VOLUME, ELECTROLYTE, AND ACID–BASE BALANCE: Fluid imbalance: FLUID VOLUME DEFICIT: occurs when the body loses both water and electrolytes from the ECF in similar proportions. Causes: (a) abnormal losses through the skin, gastrointestinal tract, or kidney. (b) decreased intake of fluid. (c) bleeding. Example on fluid volume deficit: Hypovolemia: fluid is initially lost from the intravascular compartment. Loss of water and electrolytes from: • Vomiting • Diarrhea • Excessive sweating • Polyuria • Fever • Nasogastric suction • Abnormal drainage or wound losses. Dehydration: occurs when water is lost from the body, leaving the client with excess sodium. Dehydration clinically detected with the patients: - hyperventilating, have a prolonged fever, are in diabetic ketoacidosis, receiving enteral feedings with insufficient water intake. 4 Fundamentals of Nursing\ Theory Fluid and Electrolyte FLUID VOLUME EXCESS: occurs when the body retains both water and sodium in similar proportions to normal ECF. Hypervolemia :fluid is initially increased blood volume. Causes: (a) excessive intake of sodium chloride. (b) administering sodium-containing infusions too rapidly, particularly to clients with impaired regulatory mechanisms. (c) disease processes that alter regulatory mechanisms, such as heart failure, renal failure, cirrhosis of the liver EDEMA: Excess interstitial fluid Overhydration: occurs when water is gained in excess of electrolytes, resulting in low serum osmolality and low serum sodium levels. Water is drawn into the cells, causing them to swell. Electrolyte Imbalances SODIUM: Sodium (Na+)It is found in most body secretions, for example, saliva, gastric and intestinal secretions, bile, and pancreatic fluid. Function: regulating water balance. Hyponatremia is a sodium deficit, or serum sodium level of less than 135 mEq/L Causes: - Gastrointestinal fluid loss Sweating Use of diuretics Clinical manifestation: Lethargy, confusion, apprehension Muscle twitching Abdominal cramps Anorexia, nausea, vomiting Headache Seizures, coma. Nursing Interventions: Monitor fluid intake and output. Monitor laboratory data (e.g., serum sodium). Assess client closely if administering hypertonic saline solutions. Encourage food and fluid high in sodium if permitted (e.g., table salt, bacon, ham, processed cheese). Limit water intake as indicated. 5 Fundamentals of Nursing\ Theory Fluid and Electrolyte Hypernatremia: is excess sodium in ECF, or a serum sodium of greater than 145 mEq\L. Causes: Loss of Water • Insensible water loss (hyperventilation or fever) • Diarrhea • Water deprivation Gain of Sodium • Parenteral administration of saline solutions • Hypertonic tube feedings without adequate water • Excessive use of table salt (1 tsp contains 2,300 mg of sodium) ,Conditions such as: • Diabetes insipidus • Heat stroke Clinical manifestation: Thirst Dry, sticky mucous membranes Tongue red, dry, swollen Weakness Severe hypernatremia: • Fatigue, restlessness • Decreasing level of consciousness • Disorientation • Convulsions. Nursing Intervention: Monitor fluid intake and output. Monitor behavior changes (e.g., restlessness, disorientation). Monitor laboratory findings (e.g., serum sodium). Encourage fluids as ordered. Monitor diet as ordered (e.g., restrict intake of salt and foods high in sodium). POTASSIUM: (K+) Hypokalemia: is a potassium deficit, defined as a serum potassium level of less than 3.5 mEq/L. Causes: Loss of Potassium • Vomiting and gastric suction • Diarrhea • Heavy perspiration • Use of potassium-wasting drugs (e.g., diuretics) • Poor intake of potassium (as with debilitated clients, alcoholics, anorexia nervosa) • Hyperaldosteronism Clinical manifestation: Muscle weakness, leg cramps Fatigue, lethargy Anorexia, nausea, vomiting Decreased bowel sounds, decreased bowel motility Cardiac dysrhythmias Depressed deep-tendon reflexes Weak, irregular pulses Laboratory findings: Serum potassium < 3.5 mEq/L Arterial blood gases (ABGs) may show alkalosis T-wave flattening and ST-segment depression on EC. Nursing intervention: Monitor heart rate and rhythm. Monitor clients receiving digitalis (e.g., digoxin) closely, because hypokalemia increases risk of digitalis toxicity. Administer oral potassium as ordered with food or fluid to prevent gastric irritation. Administer IV potassium solutions at a rate no faster than 10–20 mEq/h; never administer undiluted potassium intravenously. For clients receiving IV potassium, monitor for pain and inflammation at the injection site. Teach client about potassium-rich foods. Teach clients how to prevent excessive loss of potassium (e.g., through abuse of diuretics 6 Fundamentals of Nursing\ Theory Fluid and Electrolyte CALCIUM: Ca2+ Hypocalcemia is a calcium deficit, defined as a total serum calcium level of less than 8.5 mg/dL or an ionized calcium level of less than 4.5 mEq/L. Causes: • Hypoparathyroidism • Acute pancreatitis • Hyperphosphatemia • Thyroid carcinoma Inadequate Vitamin D Intake • Malabsorption • Hypomagnesemia • Alkalosis • Sepsis • Alcohol abuse Clinical manifestation: Severe depletion of calcium can cause tetany with muscle spasms and paresthesias (numbness and tingling around the mouth, hands, and feet), and can lead to seizures. Two signs indicate hypocalcemia: Chvostek’s sign is a contraction of the facial muscles in response to tapping the facial nerve in front of the ear. Trousseau’s sign is a carpal spasm in response to inflating a blood pressure cuff on the upper arm to 20 mmHg greater than the systolic pressure for 2 to 5 minutes Nursing intervention: Closely monitor respiratory and cardiovascular status. Take precautions to protect a confused client. Administer oral or parenteral calcium supplements as ordered. When administering intravenously, closely monitor cardiac status and ECG during infusion. Hypercalcemia is a calcium excess, defined as a total serum calcium level greater than 10.5 mg/dL, or an ionized calcium level of greater than 5.5 mEq/L Causes: • Prolonged immobilization Conditions such as • Hyperparathyroidism • Malignancy of the bone. Clinical manifestation: 7 Fundamentals of Nursing\ Theory Fluid and Electrolyte Lethargy, weakness Depressed deep-tendon reflexes Bone pain Anorexia, nausea, vomiting Constipation Polyuria, hypercalciuria Flank pain secondary to urinary calculi Dysrhythmias, possible heart block Nursing intervention Increase client movement and exercise. Encourage oral fluids as permitted to maintain a dilute urine. Teach clients to limit intake of food and fluid high in calcium. Encourage ingestion of fiber to prevent constipation MAGNESIUM (Mg2+): Hypomagnesemia is a magnesium deficiency, defined as a serum magnesium level of less than 1.5 mEq/L. Causes: •Chronic alcoholism • Pancreatitis • Burns •Diarrhea Clinical manifestation: Neuromuscular irritability with tremors Increased reflexes, tremors, convulsions Positive Chvostek’s and Trousseau’s, Tachycardia, elevated blood pressure, dysrhythmias Disorientation and confusion Vertigo Anorexia, dysphagia Respiratory difficulties Nursing intervention: •Assess clients receiving digitalis for digitalis toxicity. Hypomagnesemia increases the risk of toxicity. Take protective measures when there is a possibility of seizures: • Assess the client’s ability to swallow water prior to initiating oral feeding. • Initiate safety measures to prevent injury during seizure activity. • Carefully administer magnesium salts as ordered. Encourage clients to eat magnesium-rich foods if permitted (e.g., whole grains, meat, seafood, and green leafy vegetables) Hypermagnesemia is a magnesium excess, defined as a serum magnesium level above 2.5 mEq/L, due to increased intake or decreased excretion. Causes: • Renal failure • Adrenal insufficiency • Treatment with magnesium salts. Clinical manifestation: Peripheral vasodilation, flushing Nausea, vomiting Muscle weakness, paralysis Hypotension, bradycardia Depressed deep-tendon reflexes Lethargy, drowsiness Respiratory depression, coma Respiratory and cardiac arrest if hypermagnesemia is severe. 8 Fundamentals of Nursing\ Theory Fluid and Electrolyte Nursing intervention: • Monitor vital signs and level of consciousness when clients are at risk. • Assess the reflexes if absence notify the physician. CHLORIDE (Cl−): Hypochloremia is a chloride deficit, defined as a serum chloride level below 95 mEq/L, and is usually related to excess loss of chloride through the GI tract, kidneys, or sweating. Hypochloremic clients are at risk for alkalosis, and may experience muscle twitching, tremors, or tetany. Hyperchloremia is a chloride excess, defined as a serum chloride level above 108 mEq/L. Excess replacement of sodium chloride or potassium chloride is a risk factor for high serum chloride levels, as are conditions that lead to hypernatremia. The manifestations of hyperchloremia include acidosis, weakness, and lethargy, with the risk of dysrhythmias or coma. Nursing Process: Fluid and Electrolyte disorders I. Assessment: Include data collection: subjective and objective data 1. Physical Assessment for Fluid, Electrolyte: No. 1. system Skin Possible Abnormal Findings Flushed, warm, very dry Moist or diaphoretic Cool and pale 2. Mucous membranes Mucous membranes dry, dull in appearance; tongue dry and cracked 3. 4. Eyes Fontanels (infant) 5. Cardiovascular system Eyeball feels soft to palpation Fontanel bulging, firm Fontanel sunken, soft Tachycardia, bradycardia; irregular; dysrhythmias Weak and thready; bounding Hypotension Postural hypotension 6. Respiratory system Increased or decreased rate and depth of respirations 7. Neurologic Decreased LOC, lethargy, stupor, or coma Disoriented, confused; difficulty concentrating Facial muscle twitching including eyelids and lips on side of stimulus Carpal spasm: contraction of hand and fingers on affected side 9 Fundamentals of Nursing\ Theory 2. Clinical Measurements: A. Daily Weights B. Vital Signs C. Fluid Intake and Output 1) Oral fluids 2) Tube feedings 3) Parenteral fluids 4) IV medications: 5) Catheter or tube irrigants 6) Urinary output: 7) Vomitus and liquid feces 8) Tube drainage 9) Wound and fistula drainage 10) Foods that are or become liquid Fluid and Electrolyte II. Nursing Diagnosis: 1. Deficient Fluid Volume: Decreased intravascular, interstitial, and/ or intracellular fluid. This refers to dehydration, water loss alone without change in sodium. 2. Excess Fluid Volume: Increased isotonic fluid retention. 3. Risk for Imbalanced Fluid Volume: Vulnerable to a decrease, increase, or rapid shift from one to the other of intravascular, interstitial, and/or intracellular fluid, which may compromise health. This refers to body fluid loss, gain, or both. 4. Risk for Deficient Fluid Volume: Vulnerable to experiencing decreased intravascular, interstitial, and/or intracellular fluid volumes, which may compromise health. 5. Impaired Gas Exchange: Excess or deficit in oxygenation and/or carbon dioxide elimination at the alveolar-capillary membrane. 6. Impaired Oral Mucous Membrane related to fluid volume deficit 7. Impaired Skin Integrity related to dehydration and/or edema 8. Decreased Cardiac Output related to hypovolemia and/or cardiac dysrhythmias secondary to electrolyte imbalance (K+ or Mg2+) 9. Ineffective Tissue Perfusion related to decreased cardiac output secondary to fluid volume deficit or edema • Activity Intolerance related to hypervolemia 10. Risk for Injury related to calcium shift out of bones into extracellular fluids • Acute Confusion related to electrolyte imbalance. III. Planning: Maintain or restore normal fluid balance. • Maintain or restore normal balance of electrolytes in the intracellular and extracellular compartments. • Maintain or restore gas exchange and oxygenation. • Prevent associated risks (tissue breakdown, decreased cardiac output, confusion, other neurologic signs). IV. Implementing: (intervention) 1) Enteral Fluid and Electrolyte Replacement - Fluid Intake Modifications 11 Fundamentals of Nursing\ Theory - Fluid and Electrolyte Dietary Changes Oral Electrolyte Supplements 2)Parenteral Fluid and Electrolyte Replacement - Intravenous Solutions Types 1 ISOTONIC SOLUTIONS - 0.9% NaCl (normal saline) - Lactated -Ringer’s (a balanced electrolyte solution) - 5% dextrose in water (D5W) 2 3 HYPOTONIC SOLUTIONS - 0.45% NaCl (half normal saline) - 0.33% NaCl (onethird normal saline) HYPERTONIC SOLUTIONS - 5% dextrose in normal saline (D5NS) 5% - dextrose in 0.45% NaCl (D5 1/2NS) 5% - dextrose in lactated Ringer’s (D5LR) implementation - Isotonic solutions such as normal saline (NS) and lactated Ringer’s initially remain in the vascular compartment, expanding vascular volume. Assess clients carefully for signs of hypervolemia such as bounding pulse and shortness of breath. - 5W is isotonic on initial administration but provides free water when dextrose is metabolized, expanding intracellular and extracellular fluid volumes. D5W is avoided in clients at risk for increased intracranial pressure (IICP) because it can increase cerebral edema - Hypotonic solutions are used to provide free water and treat cellular dehydration. These solutions promote waste elimination by the kidneys. - 11 Hypertonic solutions draw fluid out of the intracellular and interstitial compartments into the vascular compartment, expanding vascular volume. Do not administer to clients with kidney or heart disease or clients who are dehydrated. Watch for signs of hypervolemia.