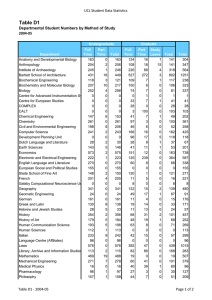
ENT Undergraduate Lecture Mr Rejali ENT Consultant University Hospital, Coventry Plan • 3 lecture: – Otology – Rhinology – Head and Neck – Practical session Otology • • • • • • Anatomy / Physiology History Examination Outer ear problems Middle Ear Problems Inner Ear Problems Otology Anatomy External Ear 1 • External – Pinna • Skin • Cartilage – External audiotary meatus (canal) • Lateral/Outer 1/3 in cartilages and produce wax • Medial 2/3 in bone and wax free – Skin migration Otology Anatomy External Ear 2 • External auditory meatus/canal • Ear wax (and hair) produced in outer 1/3 of ear canal • Ear wax (cerumen) more soluble in water • Rare cause of hearing loss unless impacted on to tympanic membrane or blocking canal completely and with a thickness of >2-m mm Otology Anatomy Middle Ear 1 • Air containing space in temporal bone. • Three ossicles (Mallus, incus and stapes) transfer sound from air to inner ear fluids • Common site of pathology Otology Anatomy Middle Ear 2 • • • • • Tympanic membrane Right ear Attic Handle of malleus Light reflex Otology Anatomy Middle Ear 3 • Eustachian tube equalises pressure between middle ear and atmosphere Otology Anatomy Inner Ear 1 • Cochlea – Hearing • Semicircular canal – Angular acceleration • Vestibule – Linear acceleration Otology Physiology Cochlea • Sound transmission through middle ear • Oval - Round Window travelling wave. • Tonotopic distribution of organ of corti Otology Physiology Vestibular Function • Macula in saccule and utricle - linear acceleration • Crista in semi-circular canal – angular acceleration Otology History • Outer ear: – Pain – Discharge: scant, serous – Hearing loss, late • Middle ear: – Hearing loss (conductive) – Discharge: moderate mucoid – Pain • In acute otitis media until tympanic membrane perforates • Chronic otitis media only if complicated e.g. otitis externa or intracranial complications Otology History • Inner ear: – Hearing loss (sensoneural) – Vertigo – Tinnitus Otology Examination • • • • • Wash hands (MRSA) Intro Ask about tenderness Which is better ear Inspect pinna, mastoid area • Otoscopy – External auditory canal – Tympanic membrane • Hearing test • Other test: cranial nerve (esp VII), co-ordination and romberg Tuning Fork Test • Rinne – Air conduction louder than bone conduction • Weber – Lateralises to side of conductive loss and away from sensoneural hearing loss • Clinical hearing test Otology Diagnosis • • • • • Surgical Sieve Outer ear Middle Ear Inner Ear Hearing loss – Conductive – Sensoneural Otology Investigations • • • • Pure Tone Audiogram Tympanogram CT MRI Otology Management • • • • Explanation Advice Medical Surgical Haematoma/Seroma of Pinna • Aspirate x2 (sterile conditions) • Compression bandage • Review in 24hrs • If re-accumulate proceed to formal drainage and quilting stitch Otology External • Pinna skin tumour Otitis Externa • • Otitis Externa Acute – – – – – – • Painful Serous discharge Moist swollen canal Tympanic membrane intact Pseudomonas aeroginosa Treat topical toilet and antibiotics Chronic – – Eczema Topical toilet and steroids Otitis Externa • Furuncle localised infection and pain • put wick with 10% icthamol/glycerine • Or incise and drain under local anaesthetic Furuncle/Abscess of Hair Follicle Otology External • Exostoses – Cold water swimmers • Osteomas – Bening neoplasia Otology Middle • Tympanosclerosis – Previous infection or trauma. – Usually of no significance Otology Middle • Retracted tympanic mebrane – Often no treatment needed – Differentiate from perforation – Occasionally progress to cholesteatoma Otology Middle • TM perforation • If dry may need no treatment • If recurrent infection can be repaired. Otology Middle • Acute otitis media – Pain – Hearing loss – Later otorrhea Acute Mastoiditis • IV antibiotics • Surgery Otology Middle • Otitis media with effusion – glue ear • Middle ear fluide • Common in children • Hearing loss • Infection starts process • Treatment conservative, Grommets Otology Middle • Cholesteatoma Otology Middle Ear • Mastoid cavity Otology Inner Ear • Balance: Balance is determined by a complex combination of inputs into the brain. • These inputs are: – Vision – Proprioception (sensation of position of joints) – Inner ear • Integration by brain Otology Inner Ear • Vertigo illusion of movement – Hallmark of vestibular dysfunction – Rotary – Linear Otology Inner Ear • Benign Paroxysmal Positional Vertigo • Vestibular Neuronitis • Meniere's Disease • Recurrent vestibulopathy • Differentiate from central vestibular causes. Vestibular signal balance Normal balanced input Pathological Left ear in this case Increased Reduced or signal nosignal signal Increased Vestibular Menieres BPPVNeuronitis Brain will get used to new situation but not to a frequently changing one. Otology Inner Ear • Presbyacusis • Congenital Hearing Loss Otology Inner Ear • Tinnitus • Acoustic neuroma Facial Palsy • Upper vs Lower motor neurone pattern. Facial Palsy • Not all are Idiopathic (Bells Palsy) – Assess other cranial nerves – Ear – Parotid • Symptoms/signs which suggest other aetiology – Above exam +VE – Slow onset – Little, no or incomplete recovery Facial Palsy • Eye care. If concern d/w Ophthalmic team. – – • • Tape eye closed at night after Lacrilube Hypomellose eye drops PRN during day Steroids (Prednisolone 40mg od for one week) are indicated early in the course of the disease (less than 3 days) if there are no contraindications. Acyclovir if signs of herpes zoster infection (vesicles in TM or pharynx or palate. (400mg five times a day for 10 days) The End of Otology Section Rhinology • • • • • Anatomy Physiology History Examination Pathology Rhinology Anatomy 1 • External • Internal – Lateral wall – Medial wall Rhinology Anatomy 2 • Nasal septum – Little’s area – Epistaxis Rhinology Anatomy 3 • Paranasal Sinuses – – – – Frontal Maxillary Ethmoid Sphenoid Rhinology Physiology • Nose – Warms, moisten – Filter – Mucociliary • Sinuses – Function unknown Rhinology History • • • • • • Nasal obstruction Anterior rhinorrhoea Olfaction Facial pain Sneezing Epistaxis Rhinology Examination • Examination – Inspect external nose – Palpate external nose – Evaluate nasal airway • Steam pattern on metal tongue depressor – Inspect nasal mucosa • Use otoscope • Lateral, medial – Inspect palpate over sinuses – Endoscopy – Olfaction Rhinology Investigation • Allergy testing – IgE levels – RAST (Blood test) – Skin Prick Testing • Plain X ray – inaccurate • CT Rhinology Allergic Rhinitis 1 • IgE mediated allergic reaction – Seasonal/Hay fever, allergy to pollen – Perennial – allergy to House Dust Mite – Other: cat etc • Nasal obstruction, sneezing, rhinorrhoea, eye symptoms Rhinology Allergic Rhinitis 2 • Investigations – RAST test – Skin Prick test Rhinology Allergic Rhinitis 3 • Treatment – Allergen Avoidance – Anti-histamine • Topical • Systemic – Steroid • Topical spray or Drops • Oral (limited use) – Leukotriene antagonist – Immunotherapy Rhinology Deviated Nasal Septum • Aetiology – Congenital – Traumatic • Symptom – Nasal obstruction – Bilateral or Unilateral • Sign • Treatment – As for rhinitis – Surgery Rhinology Perforation of Nasal Septum 1 • Aetiology – – – – – Idiopathic Trauma Tumour Wegener’s/SLE Chromic/Sulphuric acid or Cocaine • Symptoms – Nasal obstruction – Crusting – Epistaxis Rhinology Perforation of Nasal Septum 2 • Treatment – Exclude serious causes – Treat as rhinitis – Nasal douching – Septal button – Surgery (success poor) Rhinology Nasal Polyps • Aetiology – Not known • Symptoms – Nasal Obstruction – Rhinorrhoea • Treatment – Topical steroid medication – Surgery Rhinology Sinusitis 1 • Aetiology – Infective – Acute vs. Chronic • Not all facial pain is sinusitis • Symptoms – Facial pain – Nasal discharge – Nasal obstruction • Signs Rhinology Sinusitis 2 • Treatment – Acute • Decongestants • Antibiotic – Chronic • Topical steroid medication • (Antibiotics) This is not sinusitis • Many patients with It is a dental infection “sinusitis” have idiopathic facial pain syndrome • Complication – Ethmoiditis – Common in children Rhinology Epistaxis 1 • Aetiology – – – – – Idiopathic Trauma Tumours (Coagulopathy) (Hypertension) • Treatment – First aid/Resusitation – Cautery – Nasal Packing Rhinology Epistaxis 2 • Anaesthetise prior to cautery Rhinology Sino-nasal carcinoma and Nasopharyngeal Carcinoma • Rare • Aetiology – Wood dust – Nickel dust, Chromium • Symptoms – Nasal obstruction – Scant regular epistaxis Rhinology • Ethmoiditis • ENT must be involved. • Must be admitted. • Potentially serious. • Rx: ab, decong +/- surg. Rhinology Nasal Fracture Septal Haematoma • Can be manipulated • Consider the rest of head injury and facial skeleton Rhinology Nasal Fracture Septal Haematoma • Septal haematoma – Soft swelling – Must be drained within 12 hours End of Rhinology Section Laryngology (Mouth Pharynx Larynx -Throat) Section Laryngology • • • • • Anatomy History Examination Investigations Pathology Laryngology Anatomy 1 • Anatomy Mouth Laryngology Anatomy 2 • Anatomy Oropharynx Laryngology Anatomy 3 • Anatomy - Neck Laryngology Anatomy 4 Laryngology History 1 • Dysphagia (wt loss) – Solid – Liquid • • • • • Dysphonia Neck pain Referred otalgia Haemoptysis (Globus pharyngeus) Laryngology History 2 • Smoking • Alcohol Laryngology Examination 1 • Mouth – Inspection • • • • • • • • • Start from hard palate and work down Hard Palate Sup alveolar ridge Sup bucco-alveolar sulcus Buccal mucosa Inf bucco-alveolar sulcus Inferior alveolar ridge Floor of mouth Tongue – Palpation of above (esp tonge and floor of mouth) – Listen to voice – Neck • Neck Laryngology Examination 2 • Neck (have a system) – Intro – Ask about pain/tenderness – Exposure above clavicles – Inspect from front and side – Inspect while swallowing – Palpate from behind Laryngology Examination 3 • Neck (have a system) – Palpate from behind • • • • • • • • • Start from mastoid Down posterior triangle Up posterior border of sternocleiodo-mastoid Down ant border SCM Work up ant triangle including thyroid (ask patient to swallow when at thyroid) Continue working up anterior triangle: feel laryngeal cartilage, hyoid. Sumandibular and submental area. Finish with parotid and preauricular area. If you did feel a lesion further local (percussion of sternum or auscultation), regional & systemic examination may be needed (eg thyroid or other lymph node groups) Laryngology Examination 4 Laryngology Investigations • Bloods – TFT – Ca – Thyroid antibodies • • • • • FNA CXR USS Neck CT MRI Laryngology Tonsillitis • Sore throat • Pyrexia • White follicles on tonsils • Penicillin • Recurrent episodes treat with tonsillectomy • (Glandular fever) Laryngology Quinsy (Peritonsiller abscess) • Infection spreads to peritonsiller tissues and can form abscess • Asymmetrical swelling • Treat with drainage + antibiotics Laryngology Adenoids Laryngology Pharynxl/Larynx/Mouth Carcinoma Laryngology Pharynx Lymphoma • No specific local symptoms • B symptoms • Mucosa usually not ulcerating • Check other lymph groups (neck, axilla and inguinal) and spleen Laryngology Neck lump Various “Benign” • • • • Normal structures Reactive lymph nodes Mumps Sebaceous cyst Laryngology Neck lump various Laryngology Neck lump Thyroid lump • Thyroid lumps move with swallowing • Benign – Multinodular goitre / Adenoma • Malignant –thyroid – Dysphonia – Dysphagia – Metastases • Ix – Bloods (TFT, Ca, Thyroid Antibodies), FNA, USS/CT • Rx – Conservative/Medical/Surgical Laryngology Neck lump Salivary Gland Neoplasia • Parotid swellings – Mainly benign – Usually pleomorphic salivary adenoma • Submandibular gland – Usually inflammatory Laryngology Neck lump Thyroglossal Cyst • Thyroglossal cyst • Moves/tethered with/to floor of mouth • Before removal check to insure normal thyroid exists • Diff diagnosis: – Dermoid – Lymph node – Sebaceous cyst Laryngology Neck lumps Branchial Cyst • Congenital • Treatment excision Laryngology Neck lump Metastatic Neck Nodes • Neoplasia – Benign (very common) – Malignant • Primary – Carcinoma – Lymphoma (common) • Secondary metastases (always consider this) – – – – Mouth Pharynx Larynx Infraclavicular (lung, breast, stomach) Laryngology Neck lump TB • Usually multiple nodes • Cold abscess • If draining do so for weeks Laryngology Larynx Carcinoma • Dysphonia / Hoarseness for >3 weeks Laryngology Larynx Reinke’s Oedema • Smoking Laryngology Larynx Vocal Cord nodules • Vocal cord nodules Laryngology Dysphagia • Liquid – neurological • Solid – mechanical – Tumour – Pharyngeal pouch (regurgitation) Laryngology Dysphonia • Dysphonia >3 weeks needs investigation • Risk for ca: smoker, drinker. • Other suspicious symptoms: wt loss , dysphagia. • Benign: Reinke’s Oedema, Nodules, Inhaler laryngitis, Functional Dysphonia • Malignant: local (ca), distant bronchogenic ca’ causing recurrent laryngeal nerve palsy Laryngology Snoring Obstructive Sleep Apnoea • Partial obstruction of airway – – – – Snoring High BMI Pharyngeal Nasal • Recurrent obstruction to airway fragmenting sleep – Daytime somnolescence – Similar aetiology to snoring – Treatment: lifestyle, CPAP, surgery. Laryngology Larynx Epiglottitis • 4 year old drooling toxic child • Do nothing! • Get other people • Go to theatre Laryngology Acute Airway 1 • • • • Stridor. Tachopneic Cyanosis (very late sign) Acute – Foreign Bodies – Inflammatory Swelling • Chronic – Tumour. Larynx Bronchous. Laryngology Acute Airway 2. First Aid. Choking. Foreign Body Baby and adult Heimlich Laryngology Acute Airway 4 Tracheostomy • If first aid measure fail and patients life is in danger consider tracheostomy (cricothyroidotomy). • You will need: – Scalpel/Knife – Straw/Pen with inner part removed/Paper rolled up Laryngology Acute Airway 5 Tracheostomy Identify cricothyroid membrane Laryngology Acute Airway 6 Tracheostomy Horizontal cut. 2cm wide. Deep enough. Insert airway. Laryngology Acute Airway 3. First Aid. Choking. Foreign Body. Dog THE END Questions?