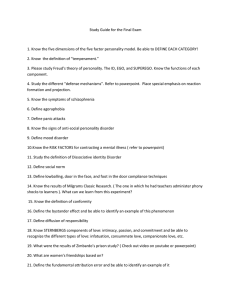
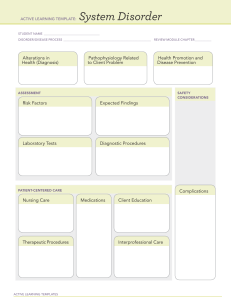
Being detained under the mental health act To be found mentally ill under the mental health act 2007 (NSW) you have to: - Have a condition that seriously impairs, either temporarily or permanently, your mental function Be at risk of harming yourself or other people You do not have to have a diagnosis to be considered “mentally ill” As a mentally disordered person you can only be kept in hospital for up to three working days and a doctor must reassess you every 24 hours. You cannot be admitted to hospital more than three times each month A developmental disability is not enough on its own to be admitted Steps to becoming assessed as mentally ill: (Note: a psychiatrist has to assess in either step 1 or 2) - Step 1: examination by an authorized medical officer o Can go home if not considered mentally ill Step 2: second assessment by authorized medical officer o May be kept to be assessed by third doctor Step 3: third assessment o Has to be psychiatrist You will be held until you see the mental health review tribunal You can be given ECT against your will - Patient must have been viewed by doctors Police or an ambulance officer can detain and take a person to a psychiatric hospital if they believe they are mentally ill or at harm to yourself or others You can be detained even when you voluntarily enter hospital Advertising Must not advertise in a way that - Is false Offers gifts, discount to attract customers Uses testimonials Mandatory reporting of other practitioners - You do not need to make a report If they are intoxicated in their private life Sexual activity with a former client can be misconduct Concerns include: impairment, intoxication while practicing, departure from accepted professional standards, and sexual misconduct APS code of ethics A: Respect for the rights and dignity of people and peoples - Justice - - o No discrimination o Assist to address unfair discrimination Respect Informed consent o Explaining the services o Explaining the risks Privacy o Avoid invasion of information that is not necessary Confidentiality o Safeguard information gathered B: Propriety Competent to deliver psychological services - - Competence o Seek supervision as required Record keeping o Keep records for 7 years o If under 18 keep records until they are 25 years Maintain professional boundaries Research o After published can provide data to other competent professionals who seek to verify claims o Participant id needs to be removed C: Integrity Exercising power appropriately - Reputable behaviour Conflict of interest (multiple relationships Do not engage in sexual activity with a client or anybody closely related to a client within 2 years of terminating the professional relationship Do not accept as a client a person they have had sexual activity with You cannot receive remuneration or give for referring clients Business succession plan A business succession plan ensures that a psychologist and his/her advisers know what will happen to the business and client files in the event that the psychologist wishes to sell the practice, retire or is unable to practise due to death or injury, and should clearly identify who is responsible for completing all necessary tasks. Should include: - Identification of a professional nominee Office information and security arrangement Location of client records and contact details Instructions for notifying clients Details of professional indemnity insurance Medicare “Better Access” referrals - Retain referral documents for up to 24 months Referral must be made by GP, a mental health treatment plan has been completed (MHTP) After completed practitioner should make a report to the referring medical practitioner including: o Assessments carried out o Treatment provided o Recommendations Competencies Every psychologist must undertake 10 hours of peer supervision yearly Areas of competence: - Knowledge of the discipline Ethical, legal and professional matters Psychological assessment and measurement Intervention strategies Research and evaluation Communication and interpersonal relationships Working within a cross-cultural context Practice across the lifespan Information that is subpoenaed should be divulged to the client. This will reduce the amount of damage done to the therapeutic relationship. Avoiding dual relationships: - Set clear boundaries Informed consent CTO - Made when a mental health tribunal finds you a “mentally ill person” at the mental health inquiry A medical practitioner must make this A hearing can occur if you are absent Maximum length of CTO is 12 months however most are made for 6 months If you do not comply police can be called by the case manager to take you to the psychiatric hospital If you still do not comply then you are taken to hospital and administered medication without consent Legal requirements following the death of a client - Contact professional indemnity insurance provider to ask legal obligations Documents that should be provided include file notes, a brief statement explaining work with the client, treatment plan, any risk assessment When a client is deceased you are able to give information to the executor of the will only when the estate administration is finalized Continued professional development - A total of 30 hours per year should be completed with at least 10 hours of peer consultation - You must have a portfolio that includes activities completed, hours, a learning plan 10 hours of active cpd are recommended e.g. attending seminars Ethical guidelines - Records must be kept a minimum of 7 years since client had last contact If working with someone under 18 must keep records until they are 25 years old One school psychologist per 500 students Client’s requesting files - You can only refuse if there is a risk, impact on others privacy, and legal matters Cannot provide protected psychological test material or information provided by other party other than client Assessment The Adaptive Behavior Assessment System (3rd ed) (ABAS) - Measures behaviours displayed at home, school, and work Young children to young adults Assesses: communication, community use, functional academics, home living, health and safety, leisure, self-care, self-direction, social, work - Is also is essential to help diagnose an intellectual delay as you need a cognitive and functional assessment to diagnose K10 (DEPRESSION) - In aus scored 1-5 for each question, US 0-4 WHODAS 2.0 – World Health Organisation Disability Assessment Schedule - Measures difficulties due to health and mental conditions TESTS I MUST KNOW: 1. WAIS IV (Wechsler Adult Intelligence Scale) - <69 extremely low 70-79 borderline 80-89 low average 90-109 average 110-119 high average 120-129 superior 130+ very superior 2. WISC IV (Wechsler Intelligence Scale for Children) 3. PAI, 2007 (Personality Assessment Inventory) Only for people 18 and over and must have 4th grade reading level Maximum number of unanswered questions – 17 Generally cannot interpret scale if more than 20% missing The skyline provides a reference point for score that are unusual in a clinical setting (2SDs over the mean) t score 70+ Mean T score 50 T score 60 (1sd above mean) is when you warrant interpretation, T score 70 (2sd) Validity scales – inconsistency, infrequency (whether they respond carelessly), negative impression, positive impression Clinical scales – somatic complaints (preoccupied with health matters), anxiety (3 scales cognitive, affective & physiological), anxiety-related disorders (phobias, ptsd, ocd), depression (3 scales cognitive, affective & physiological), mania (activity level. Grandiosity & irritability), paranoia (hypervigilance, persecution & resentment), schizophrenia, borderline features (affective instability, identity problems, negative relationships, self-harm), antisocial features, alcohol problems, drug problems Treatment scales (not for diagnosis) – aggression, suicidal ideation, stress, nonsupport (lack of perceived social support), treatment rejection Interpersonal scales – dominance, warmth Supplemental indexes – suicide potential, violence potential, treatment process (how difficult are they likely to treat), malingering, Rogers discriminant function (distinguish between people simulating psychiatric disorder) 4. DASS (Depression, Anxiety and Stress Scale) 5. K-10 (Kessler-10) 10-19 – well 20-24 – mild mental disorder 25-29 – moderate 30-50 – severe mental disorder 6. SDQ (Strengths and Difficulties Questionnaire) TESTS I MUST BE FAMILIAR WITH: 1. WPPSI III - Wechsler Preschool and Primary Scale of Intelligence (and WPPSI-IV A&NZ Standardised Edition) - Australian standardized version released April 2014 - 14 subtests, 4 for 2.6-3.11 years, 11 for 4-7.3 years - Core tests: Information, block design, object assembly, receptive vocabulary (has one substitution test) (2.6-3.11) - Core tests: Information, vocabulary, word reasoning, block design, matrix reasoning, picture concepts, symbol search (4-7.3) 2. SB5 - Stanford–Binet Intelligence Scales - Originally designed to test mental retardation - 10 subtests (5 verbal, 5 non-verbal), fluid reasoning, knowledge, quantitative reasoning, visualspatial processing, and working memory - 2-89+ years (NO AUSTRALIAN NORMS) - Takes 45-60 minutes to administer - IQ M=100, SD=15 3. KAIT - Kaufman Adolescent and Adult Intelligence Test - 6 subtests used to create three IQs – crystallised, fluid and composite) - 11-85+, approximately 1 hour to administer, NO AUS NORMS - IQ M=100, SD=15 4. WASI - Wechsler Abbreviated Scale of Intelligence (and WASI II, no Australian norms) - 4 subtests from the WIAS and gives an idea of perceptual and verbal reasoning - 6-89 years, 30 mins to administer 5. WJ III COG - Woodcock-Johnson Test of Cognitive Abilities III (INTELLIGENCE) - 10 tests, 2-90+ years, 40 minutes administration - 1:1 interviewing and paper and pencil tasks - There are Australian norms 6. WIAT II - Wechsler Individual Achievement Test (and WIAT-III, no Australian norms) (APTITUDE) - Assesses academic achievement - Reading, maths, written language, oral language - Age range 4-85 (only has aus norms from 4-19 years) 7. ABAS (and ABAS II) - Adaptive Behavior Assessment System - Designed for those with intellectual disabilities or disorders that interfere with daily function - Can monitor progress over time - Covers 10 adaptive skills - Forms: Adult, parent/caregiver (0-5), parent (5-21), teacher/daycare (2-5), teacher (5-21) - Ages 0-89 - Measures: communication, community use, functional academics, home/school living, health and safety, leisure, self-care, self-direction, social, and work - NO AUS NORMS 8. WMS IV – Wechsler Memory Scale Fourth Edition - added brief cognitive status - Adult battery and older adult battery 9. WRAML2 - Wide Range Assessment of Memory and Learning Second Edition - Verbal memory index, visual memory, attention/concentration - 5-90 years - M=100, SD=15 10. SDS - Self Directed Search (and 2nd Australian Edition 2012, Form R) (CAREER) - Career counselling tool - 6 personality types: realistic, investigative, artistic, social, enterprising, conventional 11. Strong - Strong Interest Inventory (CAREER) - Measurement of interests, now a career planning tool - Typically used for high school or transition periods - Can be scored by anyone 12. 16PF 5th Ed - Sixteen Personality Factor Questionnaire Fifth Edition - Based on Cattell primary personality factors - Has impression management index to assess social desirability - 5 global factors: extraversion, anxiety, toughmindedness, independence, self-control - Has aus norms ages 17-62 13. NEO-PI-R - NEO Personality Inventory (and NEO-PI-3 and NEO-4; no Australian norms) - Has self or rater forms - Only neo-pi-r has aus norms 14. PHQ 9 - Patient Health Questionnaire 9 Item. (DEPRESSION) - Measures depression as per dsm-iv guidelines 15. BDI - Beck Depression Inventory (and BDI-2) - 21 items - self-administered - No aus norms - 29-63 severe depression 16. GAF - Global Assessment of Functioning - DSM-IV axis 5 17. STAI - State Trait Anxiety Inventory - 40 item self report - state measures how they feel right now - trait measures how they generally feel - There is a separate scale for children 18. ORS - Outcome Rating Scale - 4 item visual analogue scale - Measures distress - Can be used for feedback on treatment 19. MMPI-2 - Minnesota Multiphasic Personality Inventory-2 - Measures psychopathology - 567 items with scales to detect faking bad 20. CBCL - Achenbach Child Behaviour Checklist and Teacher/Youth reports ODD versus conduct disorder - ODD fights against authority figure, lose tempers, argue, resists rules. It is a fight against being controlled Conduct disorder – older child violates rights of others, intimidation, stealing or deliberate destruction of property, lack of empathy – difference is they will try to control others CLUSTER B PERSONALITY – “wild” – borderline, antisocial, histrionic, narcissistic CLUSTER C – “worried” – avoidant, dependent, obsessive compulsive Schizoaffective disorder – has hallucinations/delusions but also has a depressed or manic mood Brief psychotic disorder – 1+ symptom lasting 1 day to 1 month Schizophreniform disorder – 1 to 6 months duration Schizoaffective disorder – mood symptoms present for majority Schizophrenia – At least 6 months duration Difference between hypomania and mania – hypo is not severe enough to be hospitalized and lasts at least 4 days mania lasts at least 7 days Cyclothymia – like bipolar but doesn’t meet the extremes (at least 2 years for adults, 1 year for children) CLINICAL SIGNIFICANCE: Is whether the result would be expected in less that 15% of the population Anxieties: Separation – occurs for at least 4 weeks Selective mutism – 4 weeks Social anxiety disorder – 6 months Panic disorder – after attack followed by 1 month at least of concern about panic attack GAD – 6 months Trauma: Reactive attachment disorder – no attachment to parent caused by neglect, changes in caregivers, before age 5 Disinhibited social engagement disorder – approaches unfamiliar adults. Caused by neglect, change in caregivers, must be 9 months old at least PTSD – exposed to threat, one or more intrusion symptoms associated with event, avoidance of stimuli – MORE THAN 1 MONTH Adjustment disorders – within 3 months of onset, lasts up to 6 months