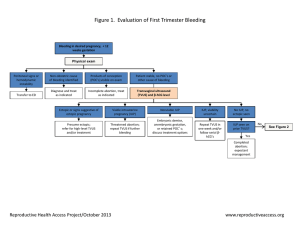
Management of ectopic pregnancy depends primarily on patient stability Stable • Pregnancy can't be identified on US • β-hCG titer < 1500-2000 mIU Unstable • Pregnancy can be identified on US • β-hCG titer > 1500-2000 mIU • Hypotension • Tachycardia • Peritoneal irritation Unruptured ectopic Ruptured ectopic Possible ectopic Expectanat managment Further blood test taken 48 hours later: 1. In viable IUP, β-hCG double every 48 hours. 2. In miscarriage, β-hCG expected to halve every 48 hours. 3. In ectopic pregnancy, β-hCG increase or drop slightly outside these limits. • β-hCG titer < 6000 mIU • Gestational sac size < 3.5 cm • Absence of fetal heart motion • β-hCG titer > 6000 mIU • Gestational sac size ≥ 3.5 cm • Fetal heart motion is seen Early ectopic Late ectopic Medical managment Surgical managment • IM Methotrexate single dose (1mg/kg) (folic acid antagonist inhibits DNA synthesis). • Patients should be followed up with β-hCG titer to ensure her response to therapy and a second dose is prescribed only if β-hCG level doesn’t fall adequately. • When medical management failed surgical management should be done. • "Laparoscopy" is commonly used but "Laparotomy" is preferred for hemodynamecally unstable patient to arrest the bleeding, and for patient with multiple surgeries and adhesions. • Surgery performed depends on the amount of tubal damage and the patient's wishes for furure fertility: 1. Complete salpingectomy (removal of the entire fallopian tube) 2. 3. 4. Partial salpingectomy (removal of a portion of the fallopian tube) Salpingotomy (closed incision made through the anumesentiric border of the fallopian tube to remove the POC) Salpingostomy (open incision made through the anumesentiric border of the fallopian tube to remove the POC) • Patients who don’t have salpingectomy should followed up with β-hCG titer 3-7 days post-op to confirm that no β-hCG producing cells remain to reinvade the tube. ABCDE approach should be used to stabilize the patient first