NUR+211+Endocrine+Disorders+of+the+Thyroid+and+Parathyroid+Halcomb copy
advertisement

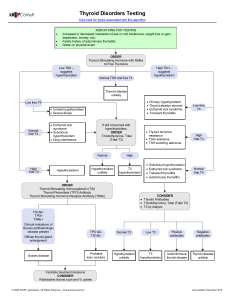
Disorders of the Thyroid and Parathyroid Glands Lisa Halcomb, DNP, MSN, RN Thyroid Gland • Major function is the production, storage, and release of thyroid hormones • Thyroxine (T4) • Triiodothyronine (T3) • Thyrocalcitonin (CT) Hypothyroidism • One of the most common medical disorders • Destruction of thyroid tissue • Disease of the anterior pituitary • After stopping thyroid hormones • Cretinism Hypothyroidism Clinical Manifestations • • • • • • • • • • • Fatigue, lethargy Slowed speech Cold intolerant Hair loss Dry, course skin, hair Constipation Weight gain Menstrual disturbances Cardiac disorders Anemia Myxedema Hypothyroidism Diagnostic Assessment • Free Thyroxine levels (FT4) are low • TSH may be high or low • These lab values, when combined with the history and physical assessment provide the diagnosis. Hypothyroidism Management • Managed on an out patient bases, unless becomes acute • Restore a euthyroid state with thyroid replacement: levothyroxine Sodium (Synthroid) – Caution with CAD – Start on smaller doses for these pts. – Instruct to report chest pain ASAP Hypothyroidism Management • • • • • • • • • Nutrition Decreased calories Written Life long therapy S/S of hyper and hypothyroidism Periodic levels checked Assess for constipation Avoid sedatives, narcotics Anticoagulants, digitalis Hypothyroidism Myxedema Coma • Untreated hypothyroidism leads to coma • Patients who are compromised • Hypotension • Bradycardia • Hypothermia • Hyponatremia • Hypoglycemia • Respiratory failure Hyperthyroidism • Sustained, increased production of thyroid hormone • Second most common endocrine disorder • Can be temporary or permanent. • Hypermetabolism and increased sympathetic nervous system activity Hyperthyroidism Grave’s Disease • A multisystem autoimmune disease of unknown etiology • Thyroid enlargement (goiter) • Increased production of thyroid hormones • Usually ophthalmopathy (exophthalmos) Hyperthyroidism Clinical Manifestations • • • • • • • • • • • • increased HR, RR, and BP intolerance to heat hyperglycemia palpitations increased appetite weight loss diarrhea warm, moist skin thin nails and hair loss fatigue nervousness and tremors rapid speech menstrual irregularities • exophthalmos Hyperthyroidism Exopthalmus • Bulging of eyeball • Impaired venous return • Corneal ulcerations, loss of vision • Dark glasses if light sensitive • Elevate HOB Hyperthyroidism Diagnostic Assessment • TSH is the single best screening tool • TSH will be low • T3 and T4 will be high • A thyroid scan Hyperthyroidism Management • Pharmacological measures • PTU and Tapazole inhibit the synthesis of thyroid hormones • Iodine – SSKI and Lugol’s solution – Only for short-term use – s/s of Iodine toxicity • Beta-blockers – for symptomatic relief of thyrotoxicosis • Thyroid ablation Hyperthyroidism Thyroidectomy • • • • • Subtotal thyroidectomy Endoscopic Watch for hypothyroidism Monitor for hypocalcemia! Explain about monitoring for airway following surgery Hyperthyroidism Thyroidectomy Pre-op Care • • • • Alleviate symptoms Give Iodine Client education Room preparation – O2 – Suction – Tracheostomy tray • Tetany – IV calcium available Hyperthyroidism Thyroidectomy Post-op Care • Assessment – Hemorrhage – Tracheal compression • Semi-fowlers, avoid movement of neck and tension on suture line • Monitor V/S freq. • Assess for tetany – tingling of toes, fingers, around mouth, muscle twitching, or apprehension, and hoarseness – Trousseau’s sign – Chvostek’s sign • Pain medication Hyperthyroidism Thyroidectomy Discharge Care • Thyroid levels must be monitored biweekly x 1 month • Avoid synthetic thyroid replacement • Reduce calorie intake to reduce weight gain • Adequate Iodine, but not excessive • Exercise to help stimulate thyroid gland regeneration • Avoidance of heat Hyperthyroidism Nutritional Considerations • High calories • • • • 4000 – 5000 cal/day Six meals a day High protein snacks Increase carbohydrates for energy • Avoid – Highly seasoned – High fiber – Caffeine Hyperthyroidism Thyroid Storm • Precipitated by a stressor – – – – Infection Trauma Surgery Too much Synthroid • Clinical manifestations – Fever – Tachycardia – HTN Hyperthyroidism Thyroid Storm • Thyroid Storm – PTU and Tapozole – K+ Iodide (SSKI) and Dexamethasone – Beta-blockers • Specifically: – Hyperthermia – Cardiovascular – Fluid and electrolytes – Neurological Parathyroid Glands • Four small glands on the thyroid • Parathyroid hormone (PTH) • Bone – Ca+ – Phosphorous • Kidney – Vitamin D – Ca+ and phosphorous • GI – Vitamin D – Ca+ absorption Hypoparathyroidism • Decreased PTH • Clinical manifestations are due to low Ca+ levels • Tingling • Muscle tension • Muscle spasms • Laryngeal spasms • Anxiety Hypoparathyroidism Nursing Interventions • Manage acute conditions • IV calcium • Rebreathing CO2 in a bag • Home Care: – Ca+ supplements – Vit. D – High Ca+ food – Monitor Ca+ levels – Teach s/s Hyperparathyroidism • Increased secretion of PTH • These high levels of PTH result in hypercalcemia and hypophosphatemia • Problems with bone density • Kidneys can’t handle the excess Ca+ • Excess Ca+ also is deposited in soft tissue Hyperparathyroidism Clinical Manifestations • • • • • • • May be overt symptoms or asymptomatic If Ca > 12, may see mental status changes May lead to coma and death Diagnostic assessment Increased PTH Increased Ca (usually > 10 mg/dl) Decreased Phosphorous (usually < 3 mg/dl) • Treatment is based on the severity of manifestations Hyperparathyroidism Non-Surgical Management • Conservative management • Medications • Phosphates can also be used to decrease Ca levels • Monitor calcium levels • Encourage ambulation Hyperparathyroidism Parathyroidectomy • • • • • Criteria Usually per scope Auto-transplantation Ca+ supplements Post-op care is similar to thyroidectomy • Tetany, may need IV calcium gluconate Hypopituitarism • Hyposecretion of the pituitary hormones. A deficiency of only one is “selective hypopituitarism”. A total destruction is “panhypopituitarism” • The most common cause is a tumor • Other causes include trauma, or accidental destruction in surgery • Lab results will determined by which hormones are affected • Surgery or radiation to tumor • Hormone replacement therapy