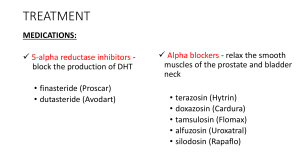
BENIGN PROSTATIC HYPERPLASIA (BPH) Adult Nursing / Practical Supervisor Dr. Haider Ali written by Ali Rajeh Benign Prostatic Hyperplasia (BPH) Benign prostatic hyperplasia (BPH), also known as benign prostatic hypertrophy, is a histologic diagnosis characterized by proliferation of the cellular elements of the prostate, leading to an enlarged prostate gland. Chronic bladder outlet obstruction (BOO) secondary to BPH may lead to urinary retention, impaired kidney function, recurrent urinary tract infections, gross hematuria, and bladder calculi. Anatomical view of the prostate The prostate is a walnut-sized gland that forms part of the male reproductive system. It is located anterior to the rectum and just distal to the urinary bladder. It is in continuum with the urinary tract and connects directly with the penile urethra. It is therefore a conduit between the bladder and the urethra. The gland is composed of several zones or lobes that are enclosed by an outer layer of tissue (capsule). These include the peripheral, central, anterior fibromuscular stroma, and transition zones. BPH originates in the transition zone, which surrounds the urethra. Causes The actual cause of prostate enlargement is unknown. Factors linked to aging and changes in the cells of the testicles may have a role in the growth of the gland, as well as testosterone levels. Men who have had their testicles removed at a young age (for example, as a result of testicular cancer) do not develop BPH. Risk factors Risk factors for prostate gland enlargement include: Aging. Prostate gland enlargement rarely causes signs and symptoms in men younger than age 40. About onethird of men experience moderate to severe symptoms by age 60, and about half do so by age 80. Family history. Having a blood relative, such as a father or a brother, with prostate problems means you're more likely to have problems. Diabetes and heart disease. Studies show that diabetes, as well as heart disease and use of beta blockers, might increase the risk of BPH. Lifestyle. Obesity increases the risk of BPH, while exercise can lower your risk. Signs and symptoms When the prostate enlarges, it may constrict the flow of urine. Nerves within the prostate and bladder may also play a role in causing the following common symptoms: Urinary frequency Urinary urgency Nocturia Incomplete bladder emptying Dribbling Diagnosis Digital rectal examination Laboratory studies Urinalysis Urine culture Prostate-specific antigen (PSA) Electrolytes blood urea nitrogen (BUN), creatinine Ultrasonography Endoscopy of the lower urinary tract Complications Complications of an enlarged prostate can include: Sudden inability to urinate (urinary retention). Urinary tract infections (UTIs). Bladder stones. Bladder damage. Kidney damage. Treatment of BPH Drugs Drugs are usually tried first. Alpha-adrenergic blockers relax certain muscles of the prostate and bladder outlet and may improve the flow of urine. Men who also have erectile dysfunction (impotence) may be treated with daily tadalafil because this drug may help relieve both erectile dysfunction and BPH. Surgery If drugs are ineffective, surgery can be done. Surgery offers the greatest relief of symptoms but may cause complications. There are several types of minimally invasive or surgical therapies. Transurethral resection of the prostate (TURP) A lighted scope is inserted into your urethra, and the surgeon removes all but the outer part of the prostate. TURP generally relieves symptoms quickly, and most men have a stronger urine flow soon after the procedure. Transurethral incision of the prostate (TUIP) A lighted scope is inserted into your urethra, and the surgeon makes one or two small cuts in the prostate gland — making it easier for urine to pass through the urethra. Transurethral microwave thermotherapy (TUMT) The doctor inserts a special electrode through your urethra into your prostate area. Microwave energy from the electrode destroys the inner portion of the enlarged prostate gland, shrinking it and easing urine flow. TUMT might only partially relieve your symptoms, and it might take some time before you notice results. Transurethral needle ablation (TUNA) In this procedure, a scope is passed into your urethra, allowing doctor to place needles into your prostate gland. Radio waves pass through the needles, heating and destroying excess prostate tissue that's blocking urine flow. TUNA may be an option in select cases, but the procedure is rarely used any longer. Nursing Management A. Facilitating Urinary Elimination 1. Provide privacy for the patient and allow enough time for voiding. 2. Palpate/percuss suprapubic area to check for bladder distention. 3. Encourage to increase oral fluid intake up to 2-4L of water as tolerated. 4. Assist with the catheter insertion as indicated. Monitor vital signs and input and output. Maintain patency of the catheter. 5. Administer medications as ordered and provide health teaching on how to check for the side-effects. Alpha-adrenergic blockers – orthostatic hypotension, syncope, blurred vision, impotence, rebound hypertension if discontinued suddenly Finasteride (Proscar) – impotence, hepatic dysfunction, interference with PSA testing B. Relieving of pain 1. Assess pain, noting location, intensity, and duration. Use the scale of pain. 2. Provide a calm and quiet environment. 3. Encourage to use hot sitz baths. 4. Provide rest periods.