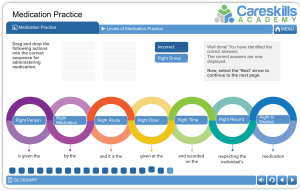
PHARMACOLOGY FUNDAMENTAL CONCEPTS OF PHARMACOLOGY Drugs Prototype Pharmacology Pharmacogenetics/Pharmacogenomics Pharmacognosy Pharmacy Toxicology Posology Therapeutic effect Side effect Drug allergy Anaphylactic rx Drug tolerance Cumulative effect Drug abuse Drug dependence Addiction Habituation Controlled drugs/scheduled drugs Idiosyncratic Drug interaction Drug antagonism Summation Synergism Potentiation Bioavailability Half-life Short-half life Long-half life Medication Response Therapeutic Index (TI) DRUGS GENERAL PROPERTIES A B C THERAPEUTIC ACTIONS Palliative Curative Supportive Substitutive Chemotherapeutic Restorative CATEGORIES OF DRUG ACTION Stimulation Depression Replacement SELAUSO. P 2ND YR Chemicalsabsorbed exhibit response or action Drug commonly prescribed Study of drugs (hx, sources, physical, chemical prop) Studies how a person's genes affect responds to medications. Study of drugs derived from natural resources Science of PCD (preparing, compounding, dispensing) study of harmful effect of drugs Study of dosage Desired/primary effect of drugs Unintended/secondary Immunologic rx to drug (e.g. hypersensitivity) Severe rx (life-threatening) occurs immediately after administered e.g. respi distress/CV collapse (epi as med) Body gets used to a medicine so that either more medicine is needed or different medicine is needed. Repeated administration of a drug produce effects that are more pronounced than those produced by the first dose drug toxicity (e.g. alcohol) Inappropriate intake of drugs e.g. cannabis (Alzheimer’s; seizures; ALS) Reliance to drugs Tissues required it; aids for normal body functioning; w/ withdrawal effect Psychological; emotional reliance; cravings; no withdrawal effect Affect mind & behavior; dispensed w/ prescription Drug rx is different from what is expected; abnormal drug rx Combination of 2 drugs increase or decrease the effect of one or both 1 of the 2 drugs interfere the action of the other Effects of 2 drugs are added = sum of each drugs added Effect of 2 drugs are added > sum of each drug added 1 of 2 drugs increases the effect of the other drug % of drugs to reach the systemic circulation Time of medication in the body to drop by 50%. Affected by liver & kidney. Takes 4 half-life to achieve steady state of serum concentration Medication leave quickly (4-8hrs) Medication leave slowly ( > 24 hrs). > risk of medication accumulation & toxicity. Can give med at longer interval w/o loss of therapeutic effect. Take longer time to reach steady state Regulate by medication dosing to maintain plasma levels between minimum effect concentration (MEC) and toxic concentration. Margin between MEC and toxic concentration Do not confer any new function/response Exert multiple action Drug interaction result from interaction of drug & func. molecule Relieves symptoms but does not cure the disease itself; given to terminally ill pt Treats the disease/condition (antibiotics) Sustains body function until other tx of body response can take over (alopurinol) Replaces body fluids/substances (IVF, electrolytes.) Destroys malignant cells Returns body to health (vitamins) Increase cell activity/secretion is reduced Decrease cell activity/secretion is reduced Replaces essential body compounds PHARMACOLOGY Inhibition Irritation HOW DRUGS ARE NAMED Chemical name Reflects its chemical composition & molecular structure Generic name Brand name HOW DRUGS ARE CLASSIFIED General terms Legal Classification GENERIC VS BRAND NAME Generic Brand Therapeutic equivalence MAJOR AREAS OF PHARMACOLOGY Pharmacokinetics Pharmacodynamics pharmacotherapeutics PHARMACOKINETICS Absorption Distribution Metabolism/Biotransformation Excretion Killing/destroying organism Causes inflammation/discomfort to the body 4-Thia-1 azabicyclo (3.2.0) heptane-2- carboxylic acid, 6[(aminophenylacetyl) amino])-3,3-dimethyl- 7-oxo ampicillin Ampicin Chemical similarity; Biological effect/use; Physiologic/chemical action OTC; Prescription Drugs; Illegal/Recreational Drugs Company develops drugs & give its official name, cheaper, preferred by pt and insurance companies; each med has only 1 generic name Drug commercial name, one medication have multiple trade name Same chemical composition, FDA, generic drug is interchangeable with brand name drug ADME Biochemical/physiological/MOA Use of drugs as treatment Site of administration into blood stream (blood flow, pain, stress, food, exercise, solubility, pH, drug concentration dosage form) Types of absorption passive, active, pinocytosis Sites of absorption in GIT mouth/oral cavity, stomach, small intestine Hepatic first pass medication must be taken 30 mins before or 1/2 hrs after meal to absorption and avoid HFP decrease therapeutic action Site of absorption to site of action (circulation, permeability, plasma protein binding) Bioavailability % of drug dose that reaches systemic circulation Sequence of chemical event that change drugs into less active form (age, nutrition, amounts of hormones, liver disease) Liver (soul & site for metabolism), HFP Process of elimination of drugs (GFR, tubular secretion rate, urine pH, renal blood flow, diuretics, blood concentration levels, half-life BARRIERS & ABSORPTION PATTERN Oral SL/Buccal Rectal, Vaginal ID, topical SQ, IM Inhalation IV SELAUSO. P 2ND YR Sites (kidney, intestines, lungs, mammary, sweat, salivary gland) HFP; presence of food; medication subtherapeutic effect Swallowing before dissolution activate medication through gastric PH quick absorption due to highly vascular membrane Presence of stool/infectious material limit tissue contacts easy absorption Close proximity of epidermal cells slow, gradual absorption Capillary walls large specs absorption highly depends on solubility Inspiratory effect rapid absorption No barrier immediate/directly enters blood and complete PHARMACOLOGY OUTCOME OF METABOLISM renal secretion Inactivation of medications (HFP) therapeutic effect Activation of pro-drugs into active forms = drug toxicity toxicity when active forms become inactive forms toxicity when inactive forms become active forms (result if liver is destroyed) OLD AGE & DRUGS Altered memory Less acute vision renal function Incomplete & slower absorption proportion of fat to lean liver function organ sensitivity Altered quality of organ responsiveness PHARMACODYNAMICS MOA Indication Contraindication Maintenance dose Loading dose Potency Receptor site Receptor theory Agonist* Affinity Efficacy Antagonist* Competitive-antagonism Partial agonist* Receptors Ligand binding domain ONSET, PEAK, DURATION Onset Peak Duration DOSE RESPONSE & MAXIMAL EFFICACY Dose response Maximal efficacy SIDE EFFECTS, ADVERSE RX, TOXIC EFFECTS Side effects Adverse rx Toxic effect/toxicity THERAPEUTIC INDEC Therapeutic index Therapeutic ratio Therapeutic range or window SELAUSO. P 2ND YR How a drug produces its effect Reason why a drug is prescribed Situations that make tx risky and should not be given Exact amount of a drug administered to maintain drug blood level in therapeutic range Large initial dose given to achieve immediate effect Strength of drug Where drug bind to produce effect Drug bind to produce/block effect Drugs that stimulate response (affinity & efficacy) Ability to produce an effect Ability to attach to receptors Drugs that block/do not stimulate response Both agonist/antagonist drugs compete for the same receptor site Act as agonist/antagonist depends on receptor site, limited affinity to receptor Drug binding sites (proteins, glycoproteins, proteolipids, enzymes) Where the drugs specifically bind Time it takes to reach the MEC (minimum effective concentration) Drug reaches highest blood or plasma concentration Length of time drug has pharmacologic effect Relationship between minimal vs maximal amt of drug dose needed to produce a desired effect All drugs have maximum drug effect Unintended effect Dangerous rx anaphylaxis Exceeds therapeutic range of drugs monitored by plasma (serum) Relationship between drugs desired therapeutic effect and its adverse effect Measures margin of safety of drug (LD50; ED50) LD50/ED50 Range of plasma concentration that produces desired effect w/o toxicity PHARMACOLOGY PHARMACOTHERAPEUTICS Acute therapy Empiric therapy Maintenance therapy Supplemental/replacement Supportive Palliative UNCONTROLLED VS CONTROLLED Uncontrolled substance Controlled substance TYPES OF MEDICATION PRESCRIPTION Routine/standard Single/one-time Stat PRN Standing PREGNANCY CATEGORIES Category A Category B Category C Category D Category X Medication is active, short-termed; based on critical state only maintain stability Based on practical experience rather than pure scientific data For pt w/ unresolved chronic conditions to control condition Replenish/substitute for missing substances Maintains other threated body system until pts condition resolves Used for end stage or terminal disease to make pt comfortable as possible. Alleviate s/sx Do not pose risk of abuse/addiction e.g. antibiotics Potential for abuse & dependence Medication given on a regular schedule w/ or w/o termination date/specific no. of doses Once at a specific time, common for preop Once and immediately, emergencies Specified dosage, frequency, condition when med can be administered Specific circumstances No risk for fetus, no evidence of fetal harm Little to no risk in pregnant, insufficient, no risk in animal studies Benefits outweighs the risk, animal risk to fetus Benefit could out weight the risk, life threatening condition Risk outweigh benefits 10 RIGHTS OF SAFE MEDICATION ADMINISTRATION Right client/patient Right medication Right dose Right time Right route Right documentation Right client education Right assessment Right evaluation Right to refuse SOURCES OF DRUG INFORMATION Drug handbook Physician’s desk reference Package inserts Nursing journals Medical letter MIMS (monthly index of medical specialties) SCHEDULES OF CONTROLLED SUBSTANCE Schedule I Schedule II Schedule III Schedule IV Schedule V SELAUSO. P 2ND YR COMMON MEDICATION ERROR Wrong med/IVF Incorrect dose/IV rate Wrong client, route, time Administration of an allergy-inducing med Omission of dose/ administration of extra dose Incorrect discontinuation of med/IVF Inaccurate prescribing Inadvertently giving a medication that has similar name LEGAL ASPECTS OF DRUG ADMINISTRATION RA9165; RA6425 Dangerous drug act 2002 RA6675 Generic act 1988 RA9502 Cheaper medicine act 2008 RA9173 Nursing law 2002 High potential for abuse, not currently accepted for medical use High potential for abuse, currently accepted for medical use, lead to strong physical and psychological dependence High potential for abuse, require new prescription q 6 mos or 5 refills, medically accepted, cause dependence Low potential for abuse, limited physical/psycho dependence, medically accepted Low potential for abuse, dispense w/o prescription, medically accepted w/ limited potential for dependence PHARMACOLOGY ROUTES OF ADMINISTRATION Oral/enteral Tablets, capsules, liquids, suspensions, elixirs, lozenges Most common route SL, Buccal Sublingual: under the tongue Buccal: between the cheek and the gum Directly enters the bloodstream and bypasses the liver. Transdermal Medication in a skin patch for absorption through the skin, producing systemic effects Topical Painless, Limited adverse effects Instillation (drops, ointments, sprays) Generally used for eyes, ears, and nose NURSING ACTION Contraindication: vomiting, decreased GI motility, absence of gag reflex, difficulty swallowing, decreased level of consciousness Take irritating meds with small amount of food Administer med on empty stomach (30 mins to 1 hr before meal, 2 hr after meal) Advantage: Safe, cheap, easy, convenient Disadvantage: Highly variable absorption, Inactivation & HPF, Cooperative, conscious Clients should not eat or drink while the tablet is inplace or until it has completely dissolved. When administering the LIQUIDS, SUSPENSIONS, AND ELIXIRS, pour it into a cupon flat surface. Make sure the base of the meniscus(lowest fluid line) is at the level of the dose. Wash the skin with soap and water, and dry itthoroughly before applying a new patch. Place the patch on a hairless area, and rotate sites dailyto prevent skin irritation. Apply with a glove, tongue blade, or cotton‐tipped applicator. Do not apply with a bare hand. Eyes Have clients sit upright or lie supine, tilt their headslightly, and look up at the ceiling. Rest your dominant hand on the clients’ forehead, hold thedropper above the conjunctival sac about 1 to 2 cm, dropthe medication into the center of the sac, avoid placing itdirectly on the cornea, and have them close the eye gently. If they blink during instillation, repeat the procedure. Apply gentle pressure with your finger and a clean facialtissue on the nasolacrimal duct for 30 to 60 seconds toprevent systemic absorption of the medication. If instilling more than one medication in the same eye,wait at least 5 min between them. For eye ointment, apply a thin ribbon to the edge of thelower eyelid from the inner to the outer canthus. Ears Have clients sit upright or lie on their side. Straighten the ear canal by pulling the auricle upwardand outward for adults or down and back for children.Hold the dropper 1 cm above the ear canal, instill the medication, and then gently apply pressure with yourfinger to the tragus of the ear unless it is too painful. Do not press a cotton ball deep into the ear canal. Ifnecessary, gently place it into the outermost part of theear canal. Have clients remain in the side‐lying position ifpossible for 2 to 3 min after instilling ear drops. Nose Use medical aseptic technique when administeringmedications into the nose. Have clients lie supine with their head positioned to allowthe medication to enter the appropriate nasal passage. Use your dominant hand to instill the drops, supportingthe head with your nondominant hand. Instruct clients to breathe through the mouth, stay in asupine position, and not blow their nose for 5 min afterdrop instillation. SELAUSO. P 2ND YR PHARMACOLOGY Inhalation Administered through metered dose inhalers (MDI) ordry‐powder inhalers (DPI) Nasogastric & Gastronomy tube SELAUSO. P 2ND YR MDI Instruct clients to: Remove the cap from the inhaler’s mouthpiece. Shake the inhaler vigorously five or six times. Hold the inhaler with the mouthpiece at the bottom. Hold the inhaler with your thumb near the mouthpieceand your index and middle fingers at the top. Hold the inhaler about 2 to 4 cm (1 to 2 in) away fromthe front of your mouth or close your mouth around themouthpiece of the inhaler with the opening pointing toward the back of your throat. Take a deep breath and then exhale. Tilt your head back slightly, press the inhaler, and, atthe same time, begin a slow, deep inhalation breath.Continue to breathe in slowly and deeply for 3 to 5 seconds to facilitate delivery to the air passages. Hold your breath for 10 seconds to allow the medicationto deposit in your airways. Take the inhaler out of your mouth and slowly exhale through pursed lips. Resume normal breathing. A spacer keeps the medication in the device longer,thereby increasing the amount of medication the devicedelivers to the lungs and decreasing the amount ofmedication in the oropharynx. For clients who use a spacer: Remove the covers from the mouthpieces of the inhaler and of the spacer. Insert the MDI into the end of the spacer. Shake the inhaler five or six times. Exhale completely, and then close your mouth aroundthe spacer’s mouthpiece. Continue as with an MDI. DPI Instruct clients to: ● Do not shake the device. ● Take the cover off the mouthpiece. ● Follow the manufacturer’s directions for preparing themedication, such as turning the wheel of the inhaler orloading a medication pellet. ● Exhale completely. ● Place the mouthpiece between your lips and take a deepinhalation breath through your mouth. ● Hold your breath for 5 to 10 seconds. ● Take the inhaler out of your mouth and slowly exhalethrough pursed lips. ● Resume normal breathing. ● Clients who need more than one puff should waitthe length of time the provider specifies beforeself‐administering the second puff. ● Instruct clients to rinse their mouth out with water orbrush their teeth if using a corticosteroid inhaler toreduce the risk of fungal infections of the mouth. ● Instruct clients to remove the canister and rinse theinhaler, cap, and spacer once a day with warm runningwater and dry them completely before using the inhaler again. ● Verify proper tube placement. ● Use a syringe and allow the medication to flow in bygravity or push it in with the plunger of the syringe. ● To prevent clogging, flush the tubing before and aftereach medication with 15 to 30 mL of warm sterile water. ● Flush with another 15 to 30 mL of warm sterile waterafter instilling all the medications. PHARMACOLOGY Suppositories Parenteral Intradermal Use for tuberculin testing or checking for medication orallergy sensitivities. SQ, IM SQ: Use for small doses of nonirritating, water‐solublemedications, such as insulin and heparin. SELAUSO. P 2ND YR General guidelines Use liquid forms of medications; if not available, consider crushing medications if appropriate guidelines allow. Do not administer sublingual medications through the NG tube (may give sublingual medications under the tongue). Do not crush specifically prepared oral medications (extended/time‐release, fluid‐filled, enteric‐coated). Administer each medication separately. Do not mix medications with enteral feedings. Completely dissolve crushed tablets and capsule contents in 15 to 30 mL of sterile water prior to administration. Rectal Wear gloves for the procedure. Rectal suppositories (thin, bullet-shaped medication) Position clients in the left lateral position orSims’ position. Insert the suppository just beyond theinternal sphincter. Instruct clients to remain flat or in the left lateralposition for at least 5 min after insertion to retainthe suppository. Absorption times vary with the medication. Vaginal Position clients supine with their knees bent and theirfeet flat on the bed and close to their hips (modifiedlithotomy or dorsal recumbent position). Insert the suppository along the posterior wall of thevagina 7.5 to 10 cm (3 to 4 in). remain supine for at least 5 minafter insertion to retain the suppository. ● The vastus lateralis is best for infants 1 yearand younger. ● The ventrogluteal site is preferable for IM injections andfor injecting volumes exceeding 2 mL. ● The deltoid site has a smaller muscle mass and can onlyaccommodate up to 1 mL of fluid. ● Use a needle size and length appropriate for the typeof injection and the client’s size. Syringe size shouldapproximate the volume of medication. ● Use a tuberculin syringe for solution volumes smaller than 0.5 mL. ● Rotate injection sites to enhance medication absorption, and document each site. ● Do not use injection sites that are edematous, inflamed,or have moles, birthmarks, or scars. ● For IV administration, immediately monitor clients fortherapeutic and adverse effects. ● Discard all sharps (broken ampule bottles, needles) inleak‐ and puncture‐proof containers. ● Use small amounts of solution (0.01 to 0.1 mL) in atuberculin syringe with a fine‐ gauge needle (26‐ to27‐gauge) in lightly pigmented, thin‐skinned, hairless sites (the inner surface of the mid‐forearm or scapulararea of the back) at a 10° to 15° angle. ● Insert the needle with the bevel up. A small bleb should appear. Do not massage the site after injection. ● Use a 3/8‐ to 5/8‐inch, 25‐ to 27‐gauge needle or a28‐ to 31‐gauge insulin syringe. Inject no more than1.5 mL of solution. ● Select sites that have an adequate fat‐pad size (abdomen,upper hips, lateral upper arms, thighs). ● For average‐size clients, pinch up the skin and inject at a 45° to 90° angle. For clients who are obese, usea 90° angle. PHARMACOLOGY IM: Use for irritating medications, solutions in oils, andaqueous suspensions. ● The most common sites are ventrogluteal, dorsogluteal,deltoid, and vastus lateralis (pediatric). ● Use a needle size 18‐ to 27‐gauge (usually 22‐ to25‐gauge), 1‐ to 1.5‐inch long, and inject at a 90° angle. Solution volume is usually 1 to 3 mL. Divide largervolumes into two syringes and use two different sites. ADVANTAGES ● Use for poorly soluble medications. ● Use for administering medications that haveslow absorption for an extended period of time(depot preparations). IV DISADVANTAGES ● IM injections are more costly. ● IM injections are inconvenient. ● There can be pain with the risk for local tissue damageand nerve damage. ● There is a risk for infection at the injection site.Z‐TRACK ● Use for administering medications, fluid, andblood products. ● Vascular access devices can be for short‐term use(catheters) or long‐term use (infusion ports). Use16‐gauge devices for clients who have trauma, 18‐gauge during surgery and for blood administration, and 22‐ to24‐gauge for children, older adults, and clients whohave medical issues or are stable postoperatively. ● Peripheral veins in the arm or hand are preferable. Askclients which site they prefer. For newborns, use veinsin the head, lower legs, and feet. After administration,immediately monitor for therapeutic and adverse effects. ADVANTAGES ● Onset is rapid, and absorption into the blood isimmediate, which provides an immediate response. ● This route allows control over the precise amount ofmedication to administer. ● It allows for administration of large volumes of fluid. ● It dilutes irritating medications in free‐flowing IV fluid. Epidural SELAUSO. P 2ND YR DISADVANTAGES ● IV injections are even more costly. ● IV injections are inconvenient. ● Absorption of the medication into the blood isimmediate. This is potentially dangerous if giving thewrong dosage or the wrong medication. ● There is an increased risk for infection or embolismwith IV injections. ● Poor circulation can inhibit the medication’s distribution ● Use for IV opioid analgesia (morphine or fentanyl). ● The clinician advances the catheter through the needleinto the epidural space at the level of the fourth orfifth vertebra. ● Use an infusion pump to administer medication. PHARMACOLOGY DOSAGE CALCULATION Basic medication dose conversion andcalculation skills are essential for providing safenursing care.Nurses are responsible for administering thecorrect amount of medication by calculating theprecise amount of medication to give. Nursescan use three different methods for dosagecalculation: ratio and proportion, formula(desired over have), and dimensional analysis. STANDARD CONVERSION FACTOR 1 mg 1000mcg 1g 1000mg 1kg 1000g 1L 1000ml 1tp 5ml 1tbsp 15ml 1tbsp 3 tsp 1kg 2.2lb 1gr 60mg IV FLOW RATES Macrodrip set 10 drops = 1 ml 15 drops = 1 ml 20 drops = 1 ml Microdrip set 60 microdrips = 1 ml Blood set 10 drops = 1ml SELAUSO. P 2ND YR PEDIA DOSAGES CLARK’S RULE weight (lbs) x AD 150 FRIED’S RULE (<1yr) Age in mos x AD 150 YOUNG’S RULE (>1yr) Age in yrs x AD Age in yrs + 12 General Formula A = desired strength x stock volume Stock on hand Gtts/min Cc/hr No. of hrs Volume in CC x gttfactor No.of hrs x 60 min/hr Volume in CC No. of hrs Volume in CC No. of hrs Volume in CC x gtt factor Gtts/min x 60min/hr