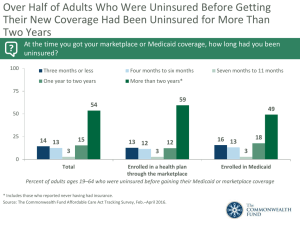
Exam 2 [SOCI-175]: Lecture Notes Key: examples, important information, statistics, terminology Lecture 5 - Health Insurance & Health Care Reform I. Shifting Institutional Foundations of Health Insurance A. US welfare state historically has operated through employment, marriage, & children B. Rates of coverage typically has relationship w/ age 1. Adults 18-64 have been vulnerable a) Increasing rates until 1970 then saw decrease which was a different trend than other age groups creating a large gap 2. 65 & older insured rated improved dramatically increased with creation of medicare a) Ex) in 1960, only 50% of elders had insurance 3. Children’s rate improved with children’s medicaid in 1990s C. ACA tried to lessen the gaps & breaking reliance on traditional ways of obtaining insurance II. Significance of Attachment A. Affordable Care Act succeeded in reducing uninsured by 31% B. Unattached: no connections to institutions 1. AKA not marriage, no job, not military, etc. 2. We see largest changes in those who are unattached as ACA breaks institutional ties a) For the unattached, ACA reduced uninsured by 41% III. ACA & Decline in Effects of Attachment A. ACA reduced the effects of attachment 1. Labor market [61%] a) Much less likely to be uninsured if you are employed 2. Marriage [reduces attachment by 78%] IV. V. VI. VII. VIII. 3. Family [45%] Some History A. Number of uninsured is growing 1. Steady increase from 1987-1999 → ~42 million uninsured in 1999 B. Uninsured likely to continue to increase as the cost of care increases C. For a long time, employment was the biggest contributor to being insured 1. Much smaller part was individually purchases insurance Recent Changes A. In 2018, 11% of non-eldery were uninsured [decrease from 17% in 2000] B. ACA produced large decline in those who are not insured in 2012 Trends in Employer Provided Insurance A. % of those getting insurance by employer decreased slightly as now people have different options with ACA [aka employer is not as dominant as in the past] How People Lose Insurance A. Lose a job, lose Medicaid eligibility, Lose a spouse, employer denies coverage, Priced out as market premiums increased 1. Losing medicaid as one makes more money or children ages out [overall positive reasons as one is doing “better” in life] 2. 17% of workers who are offered insurance decline mostly because of the expense 3. % of workers paying over 10% of their income to insurance premiums increase from 20 to 33% [aka wages are not increasing at same rate as premiums] Is Being Uninsured a Problem? A. The uninsured may get care through ER services or willingness to pay out of pocket IX. X. 1. By law, no ED can deny services based on insurance aka no systematic exclusion from services B. Uninsured might choose to be uninsured [as they are in good health or don’t want treatment] C. Consider a cascade of effects: external or spillover effects 1. Bad for you being the one uninsured but also other people Characteristics of Uninsured A. Not limited to the unemployed [unemployed are NOT the dominant sector of uninsured] 1. More than 80% of uninsured children and adults live in working families (at least 1 employed in family) 2. AKA one policy recommendation would be demanding employers to have insurance plans/provide benefits which would decrease majority of uninsured Other Demographics A. Vulneranbility with age, race, & sex B. Young adults are especially vulnerable, but they are not the only ones 1. Probability of being uninsured is 29.4% for those 18-24 years old a) ACA has decreased this slightly as they have extended how long young adults can be until parents insurance b) Argument that 18-24 are relatively healthy individual are healthy & can possibly tolerate 1-2 years of being uninsured 2. 14.5% probability of being uninsured between 55-64 aka right before medicare C. African Americans are 2x as likely to be uninsured, hispanics 3x 1. Aka 2-3x higher uninsured rates in minority population D. Men are more likely to be uninsured, but women are less likely to have employer-provided insurance XI. XII. XIII. XIV. Income A. Not entirely limited to the poor, but certainly more common among the poor 1. ¼ of the uninsured made over 50,000 [well resourced people] 2. Most of the uninsured is below the poverty line but there are some that do relatively well economically 3. Possible argument: there is a population who are just willing to pay out of pocket since they are relatively healthy B. AKA we cannot just extend Medicaid to reduce the rates as there are people with high incomes Out-of-pocket A. Out of pocket expenses for the uninsured are high 1. 10% have expenses that exceed 10% of their income 2. 20% used savings, 17% borrowed from friends, 7% took out loans or 2nd mortgages 3. MAJOR reason for bankruptcy B. People are NOT forgoing health care all together 1. The most money being spent on hospital inpatient 2. Even dental care is being taken care of as people pay out of pocket for it (yet still get the care) C. Therefore, being uninsured is both a financial vulnerability & a medical vulnerability Worry Continues EVEN after ACA A. Even with ACA, there are still difficulties paying & medical bills are still expensive 1. Nearly half of those who struggled to pay medical bills report major impacts on their family 2. 26% have had problems paying medical bills in the last year Prescription Drugs XV. XVI. A. Polypharmacy: increasing use of prescriptions B. 35% of those who are taking 4 or more drugs report difficulty paying for prescriptions [which is more than those who have fewer medications] C. Paying for prescriptions can be a burden to household budget 1. 58% spend more than $100 a month on Rx D. For those 65 and old, the difficulties paying for prescription decreases as a result of medicare E. Overall, the BEST predictor for mortality & predicting life expectancy is people evaluating their own health as excellent, good, poor, etc. Worry Among the Uninsured A. 2x as common in the uninsured to be unable/have problems paying medical bills [29%] B. 75% of the uninsured worry about bills if they get sick compared to only 44% of those who are insured C. For each dimension of worry, the uninsured is just as worried as they were in the past but ACA lessened the SIZE of that population Effects on Individual Health A. Uninsured women with breast cancer are 49% more likely to die than privately insured women B. Self-rated health declines with exposure to uninsurance C. Consider chronic disease & primary care D. Health decreases over time with no insurance E. Adjusted odds 1. Being uninsured reduces the chances you are in good health by 21% [therefore, no insurance IS a detriment to health] 2. 75% less likely to have a regular source of care aka having to float physician to physician a) With regular care, people usually report better health outcomes as a result of continuity of care 3. Some tests such as mammogram, pap test, blood pressure check, & others are relatively cheap and easy to receive a) However, uninsurance reduces the likelihood of having these tests performed by either delaying or forgoing care XVII. XVIII. XIX. Diabetes A. Common group for study as it is chronic & can be differences in quality of care [relatively simple tasks are critical for care] B. No insurance does lead to less care (quite lower than insured) 1. Undermines quality of services leading to more negative long term health outcomes 2. Ex) Foot exam for insured is 60% with uninsured (over a year) being 36% Getting Insurance Changes Behaviors A. Testing a causal relationship: not the characteristics of those who forgo insurance B. Eligibility for Medicare at 65 increases use of cholesterol screening C. When comparing to those right before Medicare eligibility to then with Medicare, the difference in amount of people who are continuously insured with chronic conditions only increased slightly with increasing care 1. However, with those who were continually uninsured and then was covered under Medicare, the percent of those with chronic conditions increased their care Uninsurance May Affect the Community A. Multilevel casualty B. 5% increase in the insured population is associated with a 10.5% increase in the likelihood that an insured adult will report unmet needs C. We are all in the market for health services XX. D. In an area with less insured people, those insured people say they have more unmet needs 1. Ex) Hospitals increasing prices, longer to schedule appointments as they have to take care of more people with no insurance 2. Therefore we ALL suffer when there is more uninsured in the area [string argument for community effect & healthcare reform] Ultimately May Affect Population Health A. TB & local uninsurance rate in urban areas 1. Correlation between % of the uninsured to TB cases aka higher risk for tuberculosis for everyone in that area whether insured or not B. Problem of unobserved variables: weak evidence C. More income inequality = lower life expectancy 1. High correlation between uninsured and poverty (does provide some argument that uninsured population is bad for everyone) Lecture 6 - Politics of Health Care Reform I. Politics, Public Opinion, & Health Care Reform A. American public has long had conflicting views about health policy 1. Much dissatisfaction w/ healthcare system, private health insurance, & managed care companies (HMOs) a) You don’t want anything between you and your physician as your relationship is special 2. However most americans remain satisfied w/ their current medical care, do no trust federal government to do what is right, don’t like change to their existing plans, & do not favor a single payer plan II. III. a) People hold government apart from healthcare often [they don’t trust; surprisingly since government is large payer in the field] b) Americans dislike change [they do not want to have to seek new provider] c) Single pay plan: one entity that would pay for all services, not well supported (1)Ex) Medicare for All B. Public opinion oscillates Timeline of an Earlier Failure A. Highest health care costs & only democracy with a substantial fraction uninsured B. Early 1993: Clinton convenes task force 1. Organized under secrecy C. “Managed Competition” 1. Employer mandate: employers would be required to provide health insurance 2. Financed by payroll taxes & regulatory mechanisms 3. Unemployed would be covered by an HMO-like plan 4. Health care alliances: state-wide risk pooling, would negotiate for consumers, purchase insurance for groups of employers up to a certain size at a reduced cost D. It is NOT an individual mandate such as the ACA but rather an employer [large gap in the labor force being uninsured] E. Initially, it was very well received yet fear of lack of finances and choices had it lose support The Boomerang A. Sept 1993: Speech 1. “To fix a health care system that is badly broken… Giving every American health security -- health care that is always there, health care that can never be taken away” IV. V. a) Provide security for everyone not only uninsured → tried to resonate that it is a more secure foundation to provide benefits for families 2. Aligned the program with social security a) Aka providing you with security in old age & poor health 3. At time of speech, there was a large spike in people believing healthcare reform is a key issue that congress needed to address [over 50%] but then declined B. Sept. 1994: Senator George Mitchell announces death of the plan Failure - aka why the US does not have national insurance A. Reasons for failure of clinton’s plan 1. Market oriented reforms - not aimed at cost-control or universal coverage 2. Public opinion was key since there the Democratic majority was slim 3. Unintended Consequences 4. Marie Ruggie & paradox of liberal intervention 5. Unions & health care B. Culture, Institutions, Politics 1. Americans are individualized 2. Invested interest & stalemates 3. Doesn’t promote large scale changes Cultural Explanations A. Commitment to distinct public & private spheres 1. We see health as private at its core a) Ex) someone’s health is not public knowledge, hipaa B. Limited government [don’t want intrusive gov] 1. Overall enthusiasm for government that governs the least is best 2. However, government changes for healthcare reform puts lots of regulation on the US aka more government VI. C. US = most individualized of the Anglo-American countries 1. Individuals are responsible for their own health 2. Ex) people’s dislike when people say they shouldn’t smoke D. Public opinion undermines political efforts 1. Concerns about choice a) Ex) Restricting what physicians you could see 2. Concerns about taxes a) In order to pay for the new system, benefit to me as insured are limited (especially since most americans are insured) compared to most expensive E. Creates changes that one may never personally benefit you or your family F. Argument that culture does support national health insurance yet when its attached to increases in government spending or bureaucracies the support decreases Institutional Explanations A. Many vested interests in status quo 1. Many people are invested in health future (Ex - consumers, hospitals, etc) 2. Insurance companies would hurt if single payer B. Prone to stalemate 1. Pluralism as opposed to a more central administration a) More opportunities for opponents of welfare spending to intervene b) We don’t have a strong central admn. compared to European countries 2. Separation of powers a) Everyone is aligned in health care reform 3. Not an unusually strong executive branch or left party C. We have political system that is dominated by 2 parties and 3rd parties are often the ones to introduce this legislation VII. VIII. D. Federalist system allows for protection of multiple voices, but some have argued it leads to more stalemates Political A. Hidden benefits, obvious costs 1. Penalties on employers 2. Regulations on insurers 3. Taxes on manufacturers & high income people 4. Reductions in Medicare payment a) Belief that more robust people under 65 means healthier over 65 B. Political polarization Affordable Care Act A. Key Elements 1. Immediately provides small businesses with a tax credit to provide coverage, and in 2014, by providing tax credits to those who need help in buying insurance -- representing the largest middle class tax cut for healthcare in history a) Uses language to try and make benefits more obvious b) Tries to pitch benefits broadly for middle class [not only the poor] 2. Sets up a new competitive private health insurance market – through state Exchanges -- giving millions of Americans and small businesses access to affordable coverage, and the same choices of insurance that members of Congress will have. 3. Holds insurance companies accountable by keeping premiums down and preventing many types of insurance industry abuses and denials of care, and ending discrimination against Americans with pre-existing conditions 4. Puts our budget and economy on a more stable path, since it is expected to reduce the deficit by more than $100 IX. X. XI. billion over the next ten years – and by more than $1 trillion over the second decade – by cutting government overspending and reining in waste, fraud and abuse 5. Extends how long one can stay on parent’s insurance B. An individual mandate (individuals are required to buy insurance) with no public option Timeline of Success A. Public opinion surrounding need for “radical change” oscillates highly 1. Ex) High percentage in 1992 [42%] supported radical changes for health care yet it quickly went down to 15% by 1994 and then up again B. Need for reform in general stays pretty high consistently C. There is doubt however if we need to completely throw it out as its completely flawed or only changes to existing 1. Republicans were divided whether it should be modified or scrapped entirely Ongoing trends are very similar to Clinton’s years A. When Clinton started, 57% didn’t think reform would affect families, but dropped to 37% and percent expecting negative impact increased from 20-40% B. Political resistance exists towards reform as it has possibility of changing your PERSONAL healthcare (something which you may be satisfied with) → people don’t want change 1. Increasing slope with 10% thinking they would be worse off with reform in 2009 up to 35% in 2010 2. Not obvious benefits contributes to this Taxes and Ambivalence About Reform A. Public willingness to pay more to increase # of insured americans oscillates right near 50% XII. XIII. XIV. B. Lingering concern that Americans will pay more in taxes without receiving benefits → need to be obvious benefits as most americans are satisfied w/ their insurance Desire for Reform but Reluctance to Pay A. Changes in variation of support when asking about elements instead of the ACA in general 1. Support for subsidy for chronically ill is very high [over 60%] as there is sympathy from American Public 2. Minor Medicaid expansion is below 50% and then support decreases more with minor subsidy for low income then further down for major medicaid expansion then even lower for major subsidy for low income B. All support for aspects of reform decrease as taxes increase as more money of your paycheck goes to these healthcare reform 1. When more money than baseline is needed for subsidies for chronic illness, people support it only at 55% so there is slight decrease C. Cost enters equation and benefits aren’t obvious → lower support Package vs. Elements A. Large gap between those who support [46%] and oppose [42%] the healthcare reform yet when specific elements asked with how important they are for congress to address, overall pretty high support 1. 76% thought it was really important that people could not be coverage based on pre-existing conditions 2. 71% agreed we needed to close the doughnut hole (gap in what medicare will pay) B. Discontinuity with overall support but then asking specifics of the ACA demonstrates the hidden benefits that are not obvious Public Support has Grown XV. XVI. A. Increasing public support is exactly what would be anticipated as more Americans started to see positives or benefit personally → see it less of a radical change than prior 1. Benefits are more obvious 2. Public support reached above public disapproval in 2017 B. There is still disapproval & political resistance 1. Implications for future of ACA aka legal resistance Physician Support has Grown A. Increase physician support over time with decreasing disapproval B. AKA public opinion, physician support, & more are all moving the same direction towards support for ACA Recent & Ongoing Challenges A. Legal 1. Texas v. United States: filed by 20 Republican state attorneys general and governors and two individuals, who argued that after Congress zeroed out the individual mandate penalty the entire ACA should be eliminated as it is unconstitutional a) Supreme court REJECTED in June 2021 B. Political [main source of barriers] 1. Growing polarization & partisanship 2. States unlikely to expand medicaid a) Southern states, Texas, Wisconsin, Wyoming, South Dakota, & Kansas b) Most successful challenge = allowing states NOT to expand Medicaid (where government would pay for difference) C. Social 1. Beneficiaries are difficult to identify 2. Affordable dimension of act has had mixed success a) There are still people who get surprise medical bills that undermine financials, have to pay more than anticipated b) More people are insured [success] yet still problems with costs Lecture 7 - Medicalization & Construction of Diagnoses I. Medicalization A. Medicalization: process by which nonmedical problems become defined & treated as medical problems, using a medical framework or a medical intervention to treat it 1. Definition by Peter Conrad 2. Controversial topic 3. Expands authority of medicine into new domains as these interact with the need to have good health to do roles in society 4. Includes behavioral problems B. “Nonmedical” 1. Not a dysfunction a) Poor health is fundamentally a dysfunction → something is not working the way it should 2. Not within the traditional remit of medicine 3. Not what medicine has treated in the past C. Ex) andropause, baldness, ADHD, depression, homosexuality 1. Andropause: male menopause as testosterone levels decrease a) New medicalization = medications to add testosterone & with treatment it is now considered medical/disorder II. 3 Issues A. What do disease “labels” do? 1. Labels that we affix to a set of symptoms have POWER III. IV. V. 2. Ex) Not a trivial transition between being sad & having depression B. What criteria do we use to define illness? 1. Illness changes as appreciate of human function changes C. What do we do with spectrum disorders? 1. Disorders that exist naturally on a continuum a) Ex) Depression, High Blood Pressure 2. Drawing a line between normal & abnormal Google Book Ngram A. Major Depression, Chronic Fatigue, & ADHD were not spoken about/topic prior to 1980 (with CF not until 1990) B. In 1980s, DSM3 was published leading to rise 1. It is not that ADHD just increased in prevalence however that the language changed C. Increases in use were quick/slope was high meaning that when we create these disorders, they quickly become part of societal conversations 1. Impact of medicalization - we treat medical matters with importance D. A Comparison 1. Mortality trend has improved so the essence of life does not draw as much attention a) Ngram of resources around death decreased Hypertension A. High blood pressure is categorical (normal, prehypertension, high blood pressure stage 1 & 2) 1. When you take a medication for hypertension, it means you have the disease despite having no actual symptoms B. Risk increases at the different classifications C. Highly predictive of cardiovascular issues later Continuity of Risk A. Risk of heart attack increases with age VI. VII. VIII. B. As blood pressure increase, risk of heart attack increases C. There is no sharp discontinuity/stepping stages for heart attack risk, but rather a continual and steady increase 1. Therefore, if we as society want to reduce mortality, we should care about all levels of blood pressure D. The entire curve of heart attacks shift left when treatments were available (Ex - antihypertensives) 1. If we only focused on the extreme values, there would not nearly be the same degree of movement to lower risk 2. Meaning everyone should be taking these medications to shift left (not only extremes) E. The underlying risk is much more continuous yet the highest risk are being treated 1. Ex) Everyone should be trying to lower BP such as limiting salt Populations & Treatment A. If we shift blood pressure distribution by decreasing BP, some risks, such as reduction in stroke, occur but on a very small degree 1. AKA we will not see any shift left if we only focus on the extremes [would not reduce mortality by much] The Labeling Debate A. What need does a diagnosis serve? B. Who stands to benefit from diagnosis C. When is a diagnosis credible? D. Why do we think diagnoses are categorical in the first place? E. Are risk and illness the same? Rosenhan 1973 - Being Sane in Insane Places A. Prior to DSM3, classification of psychiatric disorders were not as specific B. 8 “pseudopatients” were sent to a psychiatric hospitals IX. X. 1. Coached them to gain access (Ex - delusions, hearing voices) C. Results 1. They were not detected 2. Psychiatric labels stuck 3. Pseduopatients felt powerlessness & depersonalization a) That they were not being seen/heard, but rather seen only through diagnosis label b) Stress of powerlessness increases risk of developing a real/more psychiatric symptoms D. Szasz proclaims mental illness a “myth” E. There is extreme power in the label so we need to be extremely careful w/ diagnoses [need more specific guidelines] Some Engines of Medicalization A. The Specificity Revolution 1. Focus on discrete entities 2. The form is as important as the content 3. Instinct to categorize derives from SR (direct identification of pathogens/entities causing specific symptoms/problems; all illnesses are governed by specific process) B. Consumers 1. Patients sometimes demand treatment & recognition C. Medical Innovations & Technology 1. New treatments can increase the diagnosis of the condition 2 Competing Conceptions of Mental Illness A. Mental illness exists on a continuum 1. Symptom-focused a) Ex) lack of motivation for depression b) Each symptom is important 2. Degrees of depression 3. Emphasis on atypicality of illness → not everyone with same disorder has same exact effects XI. XII. B. Mental illness is categorical 1. It’s specific, qualitatively distinct 2. You have a mental illness or you don’t 3. It brings resources to the issue Benefits of Categorical Assessment A. Diagnostic decisions are categorical, even if illness is not 1. Taxon: underlying discrete entity a) For some illnesses, there may be underlying taxon even if we don’t know it yet 2. Research can guide cut-points when a taxon exists B. Provides an estimate of need based on clinically significant criteria 1. Better to count cases even if they are artificial (resonate more on a 0-10 scale) 2. Puts resources toward mental illness 3. Guides disease management C. Allows individuals to feel part of a group 1. Validates the experience of illness/ they are not alone D. Allows for reliable assessment 1. All professionals can reach the same diagnosis 2. Uses language that is fundamentally useful; everyone plays by same rules The Costs of Categorical Assessment A. Diagnosis as “Reified Measurement” B. Not based on formal/scientific evidence C. Process of reification 1. Assessing specific symptoms 2. Splitting symptoms along arbitrary cut-points 3. Promoting criteria D. A diagnosis reduces information 1. Diagnoses confound the attributes of people, such as symptoms, with judgements about those attributes XIII. XIV. a) Ex of judgements) at what level are symptoms more significant, causes of trauma for PTSD are more important E. Diagnoses are stigmatized 1. Urge caution as once we affix the label, it comes with negative connotations 2. Stigma attached to diagnosis [not necessarily underlying symptoms] Measuring Continuously: the K-6 A. Alternative to categorical B. 0-4 scoring leading to a 13+ cut off C. Which symptoms in the last 30 days have you had… hopelessness, worthless, that everything was an effort, restless, nervous, so depressed that nothing could cheer you up 1. These symptoms are non specific psychological distress that have lots of psychiatric validity 2. 30 days is a narrow window of time → hard to remember past that, symptoms often come simultaneously a) If we truly think these are illnesses, there would be more than 1 symptom D. Results 1. Many people reported no symptoms, but there is a long tail of those rating these symptoms frequently 2. We should respect the distribution as these are all everyday symptoms of distress [we all have these symptoms at baseline] Measuring Categorically: the DSM A. The Diagnostic and Statistical Manual (DSM): 1. Reliability → consistent across psychiatrists a) Rosenhan experiment showed need to be able to distinguish from those who has illnesses vs those who don’t across the board XV. 2. Theory neutrality: what causes a disorder is not important to what is happening right now in order to diagnose 3. Avoid a) False positives: finding a mental illness when really there is not one [overdiagnosing] b) False negatives: not finding a mental illness when really there is one [underdiagnosing] B. We want measures that are… 1. Sensitive: so that, when applied correctly, no false negatives arise 2. Specific: so that no false positives arise 3. But DSM favors specificity a) Idea that MOST people don’t suffer from psychiatric disorders (this is considered to have the least consequences) C. We want true prevalence, not clinical prevalence 1. With the creation of DSM, we now have ability to see how many are truly suffering vs. getting treatment [can lead to better science] An Example: Criteria for Major Depressive Episode A. Arbitrary: based on impression 1. Ex) needs 5 or more symptoms B. Highly specific 1. Ex) weight loss/gain [more than 5%] C. In order to be diagnosed with depression, you have to have depressed mood or have loss of interest pleasure D. Once you categorize the person with depression, we don’t know whether the have 5 or 7 symptoms but rather that they passed threshold 1. Same for when someone has 4 symptoms as they are under threshold and aren’t diagnosed XVI. XVII. XVIII. E. The symptoms have to impact your roles/functioning [very parsons like] The DSM in a survey A. National Comorbidity Survey & Replication B. Survey instrument based on the DSM (and later the International Classification of Disease) C. They took the DSM and symptoms and crafted a survey asking the questions 1. ex) for insomnia symptoms - Have you ever had 2 weeks or more when nearly every night you had trouble falling asleep? D. Benefit: can gain true prevalence Prevalence is High, Mild Disorders Common A. ¼ of adult americans meet diagnostic threshold for at least 1 disorder [this is high] B. 7% reach threshold for 3 or more disorders C. Most disorders are mild: for % of those suffering from 1 disorder, 59% are mild D. Very few examples of bipolar NOT being serious [83% are serious] E. Depression is also more often serious [30%] F. Anxiety disorders are common but they tend to more mild than other disorders G. Comorbidities: many are suffering from several disorders 1. Argument that the DSM may have created too many disorders and some should be combined a) Ex) Depression & anxiety under 1 The US is Unusual A. Prevalence of Mental Illnesses in the US is the highest than any other country [26% suffer from any disorder in 12 months] 1. Shanghai is the lowest at 4.3% B. Not one Nigerian suffers from ADHD XIX. XX. C. One argument could be that it is American Culture yet countries with similar cultures (such as european countries) are much lower D. Closest competitor is Ukraine with 20.5% prevalence E. Netherlands substance abuse is 3% compared to 3.8% in US yet Netherlands has much less regulations F. Further evidence that classification does not work since there should be cross national consistency Psychiatric Symptoms are Like Blood Pressure A. One can predict what happens in 10 years if you look at what happens currently B. Study that looked at series of outcomes → hospitalizations, work disability, SMI, suicide attempt 1. Like blood pressure, there is no fine line between mild/moderate/more 2. A mild case of mental illness doubles odds compared to non cases a) Even a mild case is predictive of something such as a serious mental illness 3. Severe mental illness multiples odds by 15 for consequences later 4. With severe, 42.4% have consequences C. It is risky to get rid of mild disorders (one possible argument to lessen prevalence) since mild still increases odds (3x for a SMI) 1. There are risks for NOT labeling The “Tyranny” of Diagnosis A. Diagnoses are indispensable [difficult to imagine system w/o classification] 1. Fills cognitive & emotional needs a) Provides explanation of behavior/experience 2. A “password” to care a) Point of entry to receive services b) ex) Insurance companies will cover visits/services with a specific diagnosis 3. Bureaucratic imperative a) Ability to count cases, validity for insurance companies 4. The form of creating diagnoses has been around a long time a) Ex) Zande Witch Doctor B. Diagnoses are neither positive nor negative, but they are absolutely sovereign [extreme power] 1. Disease categories provide meaning (not all of which is alienating) and a way to manage relationships with medical institutions 2. Treatments solidify discrete diagnoses Lecture 8 - Physician Socialization, the Informal Curriculum, Medical Errors I. Themes in Physician Socialization Research A. Types of Curricula 1. Public (“formal”): basic science, facts; transmitted through lectures & text a) Ex) anatomy class 2. Private (“hidden”): dealing w/ uncertainty & emotions; transmitted through allusion, parables, gossip, jokes a) Ex) lessons of medicine such as dealing with uncertainty, how to deal with cases with no cure, dealing w/ emotions B. More important? 1. Human side of medicine vs. technical side 2. Organizational Policy vs. organizational culture: what do hospitals stimulate ought to happen vs what society says ought to happen II. III. C. 2 examples: how do physicians learn from mistakes? Cope with death? Uncertainty in 5 Areas of Medical Training (Renee Fox) A. Incomplete mastery of available knowledge B. Limitations in current medical knowledge 1. Ex) Covid C. Difficulty distinguishing personal ignorance from limitations of medical knowledge D. Client response 1. Uncertainty dealing with actual people E. Instructor quasi-norms → personal expectations by those teaching on how to practice medicine Learning to Cope with Uncertainty A. Knowledge 1. Master, specialize (claiming ignorance is forgiven), adopt a schools develop around uncertainty) 2. As knowledge of medicine expands, there is pressure to specialize 3. Having a particular practice matters in ways to minimize doubts B. Diagnosis 1. Gain experience, experience is self-validating, requires no outside reference [experience diminishes uncertainty] a) No outside references if it has worked in the past 2. Clinical expertise often overrides scientific evidence 3. Experience is self-validating (lots of physicians are not using EBM but rather previous experiences/successes) C. Treatment 1. Emphasize technique/process rather than outcome D. Client Response 1. The “crock”: no clear medical problem, threatens the doctors role, because nothing is learned IV. V. VI. a) If one is interested in gaining experience/always learning from the cases, a crock patient adds nothing Consequences of Coping A. Over time, physicians become less stressed by uncertainty B. Greater confidence in particular methods, development of practice patterns 1. Harder to change behavior [stuck in habits] C. Increased specialization D. Decreased focus on the patient E. Should we be concerned? 1. Consider autonomy of medicine 2. How are errors policed? What are medical errors? A. Institute of Medicine Definition 1. Medical Error: failure of a planned action to be completed as intended (Ex - an error of execution) or the use of a wrong plan to achieve an aim (Ex - an error of planning) a) Used for counting medical errors 2. Adverse Event: injury caused by medical management rather than underlying condition of the patient a) Adverse effect attributable to error = “preventable adverse event” b) Negligent adverse events represent a subset of preventable adverse events that satisfy legal criteria used in determining negligence (1)Ex) whether care provided failed to meet standard of care reasonably expected of average physician qualified B. Bosk argues that medical errors are contested [no strict definition ut we have to argue what is an error vs. what is not] Types of Errors A. Diagnostic VII. 1. Error of delay in diagnosis 2. Failure to employ indicated tests 3. Use of outmoded tests or therapy 4. Failure to act on results of monitoring or testing B. Treatment 1. Error in performance of an operation, procedure, or test 2. Error in administering treatment 3. Error in dose or method of using a drug 4. Avoidable delay in treatment or in responding to an abnormal test 5. Inappropriate (not indicated care) C. Preventive 1. Failure to provide prophylactic treatment 2. Inadequate monitoring or follow-up of treatment D. Other 1. Failure of communication 2. Equipment failure 3. Other system failure IOM Report: to Error is Human A. One study in Colorado & Utah found that adverse events occurred in 2.9% of hospital admissions; 6.6% of those lead to death B. Another study in NY found adverse events in 3.7% of admissions w/ 13.6% of those leading to death C. When extrapolated over US, these studies suggest anywhere from 44,000-98,000 deaths a year from adverse events D. Even using lower estimate, deaths due to preventable adverse events EXCEED those to motor vehicle accidents [43,000], breast cancer [42,000], or AIDS [16,000] E. Medication errors alone cause 7,000 deaths F. Estimated cost is between $17-29 billion VIII. G. Highest error rates with serious consequences are most likely in ICU, operating rooms, & EDs H. Medical errors have SIGNIFICANT impact Forgive & Remember A. How is self-regulation achieved? 1. Freidson: referrals to high-quality docs 2. Parsons: trust allows for malfeasance 3. No one policies physicians expect physicians themselves 4. Best practice of medicine is physicians policing themselves B. Social Control 1. External: audit by outside parties a) Does not occur 2. Internal:done by physicians 3. Informal-internal: everyday control a) No formal punishments, daily, you wouldn’t lose license b) This is the self-control; this taught; strongest, most valid way c) Informal curriculum works well as physicians take mistakes VERY seriously however there also needs to be tolerance of mistakes [learning from them] 4. Formal-internal: review of performance 5. We want strong self-control C. Norms & Errors 1. Errors are NOT categorical, cut and dry 2. Errors are essentially contested a) Draw in character/history of that physician 3. They are negotiated D. Medical hierarchies 1. Attending physician: completed residency a) Informal relies on what attendings tell ones below 2. Fellows, residents, medical students: supervised by attendings 3. Surgical errors a) Easiest to study (high stakes) b) Surgeons have to make decisions quickly