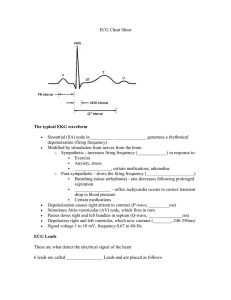
02.02 EKG (ECG) Waveforms Outline Overview 1. The heart’s electrical activity that stimulates the atria and ventricles to contract produce a waveform on an EKG 2. These waveforms are broken down into in a P wave, QRS complex and T wave. Nursing Points 1. P wave 1. Atrial depolarization 1. Positive deflection 2. PR interval 1. Beginning of P wave to beginning of QRS 2. Time it takes for electrical current to reach ventricles 1. 0.12-0.20 seconds 2. QRS Complex 1. Ventricular depolarization 1. Negative and positive deflection 2. QRS interval 1. Beginning of the Q wave to ending of S wave 2. Time it takes for the electrical current to travel through the ventricles 1. 0.06 -012 seconds 3. T wave 1. Ventricular repolarization 1. Positive deflection 2. QT interval 1. Beginning of QRS to the end of T wave 2. Time it takes for the ventricles to contract and relax 1. 0.36-.044 seconds 3. ST segment 1. End of QRS complex to the beginning of T wave 2. Time between ventricular depolarization and repolarization Assessment 1. Recognize PQRST waveforms on EKG 2. Check pulse if abnormal waveforms are observed Therapeutic Management 1. Recognize and report abnormal waveforms 1. Long PR interval 2. Prolonged QRS Complex 3. Tall T waves 03.05 Atrial Fibrillation (A Fib) Outline Overview 1. Atrial fibrillation 1. Multiple disorganized cells produce additional electrical impulse in atria 1. Causes atria to quiver at a fast rate 1. <300 bpm 2. Unable to effectively contract 1. Pooling of blood in atria 2. High risk for stroke 2. AV node blocks some of the electrical impulses from reaching the ventricles 1. Rapid irregular ventricular contractions By J. Heuser – Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=465397 Nursing Points General 1. Characteristics of Atrial fibrillation 1. Rhythm 1. Irregular 2. Rate 1. Atrial rate 1. >300 bpm 2. Wavy baseline 2. Ventricular rate 1. 60-100 bpm 2. >100 bpm 1. “Rapid Ventricular Response” (RVR) 3. P:QRS ratio 1. No obvious P waves 1. Wavy baseline 2. Not measurable 4. PR interval 1. Not measurable 5. QRS complex 1. 0.06-0.12 seconds Assessment 1. Patient Presentation 1. Palpitations 2. Fatigue 3. Lightheaded/Syncope 2. Acute or chronic 1. If chronic 1. Monitor rate/meds 2. If acute 1. Convert to NSR 3. Atrial and ventricular rates 1. RVR 4. Decreased Cardiac Output 1. Syncope 2. Hypotension 5. PT/INR 1. If taking Coumadin Therapeutic Management 1. Nursing Interventions 1. Acute or chronic 2. 12 Lead EKG 3. Restore NSR 4. Assess for s/s of stroke 2. Convert to NSR 3. Control ventricular rate 1. Medications 1. Antiarrhythmics 2. BB 3. Calcium Channel Blockers 2. Transesophageal Echocardiogram (TEE) or Cardioversion (CV) 3. Ablations 4. Decreased risk for stroke 1. Anticoagulants 1. Coumadin (Warfarin) 2. Xarelto (Rivaroxaban) 3. Eliquis (Apixaban) Nursing Concepts 1. EKG Rhythms 2. Perfusion 3. Clotting Patient Education 1. Do not miss a dose of on anticoagulants 1. Check PT/INR as instructed 2. Check radial pulse 1. Report if >100 ▪ Treatment: blood thinners (esp. if 48 hours or greater), antidysrhythmics (Cardizem, Amiodarone, Digoxin, etc.) or cardioversion (if hemodynamically unstable AND < 48 hours) 03.06 Premature Atrial Contraction (PAC) Outline Overview 1. Premature atrial contraction 1. Additional stimulus initiated in the atria 1. Not originated by SA node 2. Causes a premature contraction by the atria 1. Decreased filling time in atria 2. Common arrhythmia 3. Normal ventricular contraction will follow the early atrial contraction 2. Must have an underlying rhythm Nursing Points General 1. Characteristics of PAC 1. Rhythm 1. Regular 2. Irregular with PAC 1. Abnormal P wave 2. Rate 1. Normal 2. Depends on underlying rhythm 3. P:QRS ratio 1. 1:1 4. PR interval 1. 0.12-0.20 seconds 2. Depends on underlying rhythm 5. QRS complex 1. 0.06-0.12 seconds 2. Depends on underlying rhythm Assessment 1. Patient Presentation 1. Fluttery feeling in chest 2. Feeling of “heart skipping” 3. Dizzy 2. Electrolytes Therapeutic Management 1. Nursing Interventions 1. Determine underlying rhythm 2. Determine frequency of PACs 2. Determine the cause 1. Caffeine intake 2. Electrolyte imbalance 3. MI 3. Treat the cause 4. Symptomatic 1. Beta blockers 5. Asymptomatic 1. Continue to monitor Nursing Concepts 1. EKG Rhythms Patient Education 1. Check radial pulse 1. Report if >100 2. Notify MD if symptomatic 03.07 Supraventricular Tachycardia (SVT) Outline Overview 1. Supraventricular tachycardia 1. Increased electrical stimulation in atria or AV node 1. Stimulates ventricles to contract rapidly 1. 150-250 BPM 2. Decreasing cardiac output Nursing Points General 1. Characteristics of Supraventricular Tachycardia 1. Rhythm 1. Regular 2. P waves 1. Pointed 2. Hidden in T wave 2. Rate 1. 150-250 BPM 3. P:QRS ratio 1. Visible P waves 1. 1:1 2. Non-visible P waves 1. Not measurable 4. PR Interval 1. Visible P waves 1. <0.20 seconds 2. Non-visible P waves 1. Not measurable 5. QRS complex 1. <0.12 seconds Assessment 1. Patient Presentation 1. Palpitations 2. Fluttering in chest 3. SOB 4. Lightheaded 5. Chest pain 2. Decreased Cardiac Output 1. Syncope 2. Hypotension Therapeutic Management 1. Nursing Interventions 1. Stable/Unstable 2. 12 Lead EKG 2. Determine the cause/Treat the cause 3. Control heart rate 1. Vagal Maneuvers 2. Medications 1. BB 2. Calcium Channel Blockers 3. ACLS guidelines 1. Stable 1. Adenosine 2. Unstable 1. Cardioversion (CV) Nursing Concepts 1. EKG Rhythms 2. Perfusion Patient Education 1. Check radial pulse 1. Report if >100 Treatment: vasovagal maneuver (mild symptoms, HR 150s up to 170, BP stable), Adenosine (moderate symptoms, HR 170s-190s, at or just above stable), synchronized cardioversion (HR 190s up to 230 or more, many symptoms, BP unstable) ; depends on symptoms & whether stable or unstable hemodynamically 03.08 Premature Ventricular Contraction (PVC) Outline Overview 1. Premature ventricular contraction 1. Additional stimulus initiated in the ventricle 1. Causes a premature contraction of the ventricles 1. Decreased filling time 1. Decreased cardiac output 2. Ventricles contract before atria can contract (no P wave) 2. Must have underlying rhythm Nursing Points General 1. Characteristics of PVC 1. Rhythm 1. Irregular with PVC 2. Regular 1. Depends on underlying rhythm 2. Rate 1. Normal 1. Depends on underlying rhythm 3. P:QRS ratio 1. No P wave during PVC 1. Not measurable 2. 1:1 1. Depends on underlying rhythm 4. PR interval 1. Not measurable during PVC 2. 0.12-0.20 seconds 1. Depends on underlying rhythm 5. QRS complex 1. > 0.12 during PVC 1. Abnormal looking Assessment 1. Patient Presentation 1. Feeling of “heart skipping a beat” 2. Pounding heart beat 2. Electrolytes 3. VS 4. Oxygen saturation Therapeutic Management 1. Nursing Interventions 1. Determine underlying rhythm 2. Determine frequency of PVCs 1. Bigeminy 2. Trigeminy 2. Determine/treat the cause 1. Caffeine intake 2. Electrolyte imbalance 3. Hypoxia 4. Medications 5. MI 3. Asymptomatic 1. Continue to monitor 4. Symptomatic/Frequent 1. Medications 1. Antiarrhythmics 2. Beta blockers 3. Calcium channel blockers 2. Implantable Cardioverter Defibrillator 3. Ablations Nursing Concepts 1. EKG Rhythms 2. Perfusion Patient Education 1. Notify MD if symptomatic 2. Limit caffeine intake 03.09 Ventricular Tachycardia (V-tach) Outline Overview 1. Ventricular Tachycardia 1. Multiple unorganized electrical signals in the ventricles 1. Ventricles contract at a rate of 150-250 bpm 2. May or may not have pulse 3. Significantly reduces CO and perfusion Nursing Points General 1. Characteristics of Ventricular tachycardia 1. Rhythm 1. Regular 2. Irregular 2. Rate 1. 150-250 bpm 1. Ventricular rate 3. P:QRS ratio 1. No P waves 1. Not measurable 4. PR interval 1. No P waves 1. Not measurable 5. QRS complex 1. > 0.12 seconds 2. “Wide” Assessment 1. Patient Presentation 1. Palpitations 2. Chest pain 3. Decreased CO 1. Hypotensive 2. LOC changes 3. Lightheaded 4. Syncope 2. Pulse or pulseless 3. Electrolytes Therapeutic Management 1. Nursing Interventions 1. Determine if a pulse is present 2. Sustained or Unsustained 1. Monomorphic 2. Polymorphic 2. Determine/Treat the cause 1. Electrolytes 2. MI 3. Abnormal heart conditions 3. Follow ACLS guidelines 1. V-tach with pulse 1. Amiodarone IV 2. Magnesium Sulfate IV 3. Synchronized Cardioversion (CV) 2. Pulseless V-tach 1. CPR 2. Defibrillate 3. Epinephrine Nursing Concepts 1. EKG Rhythms 2. Perfusion Patient Education 1. Seek medical help Treatment: Monomorphic & stable- Amiodarone IV, if polymorphic then Phenytoin or IV Magnesium Cardiovert if drug therapy fails 03.10 Ventricular Fibrillation (V Fib) Outline Overview 1. Ventricular Fibrillation 1. Multiple unorganized electrical signals in the ventricles 1. Causing the ventricles to quiver 1. Wavy lines 2. Heart not able to pump blood out 1. Zero cardiac output 3. Life threatening emergency 1. Cardiac arrest Nursing Points General 1. Characteristics of Ventricular fibrillation 1. Rhythm 1. Irregular 2. Rate 1. Not measurable 3. P:QRS ratio 1. Not measurable 4. PR interval 1. Not measurable 5. QRS complex 1. Not measurable Assessment 1. Patient Presentation 1. Cardiac arrest 2. Will NEVER have a pulse! Therapeutic Management 1. Nursing Interventions 1. CPR 2. Follow ACLS guidelines 1. CPR 2. Defibrillate 3. Epinephrine 4. Amiodarone Nursing Concepts 1. EKG Rhythms 2. Perfusion 03.11 1st Degree AV Heart Block Outline Overview 1. 1st degree AV heart block 1. Conduction delay in the AV node 1. Prolonged conduction from the atria to ventricles 2. PR interval >0.20 seconds Nursing Points General 1. Characteristics of 1st degree AV heart block 1. Rhythm 1. Regular 2. Irregular 2. Rate 1. Varies 2. Depends on underlying rhythm 3. P:QRS ratio 1. 1:1 4. PR interval 1. >0.20 seconds 5. QRS complex 1. 0.06-0.12 second Assessment 1. Patient Presentation 1. Asymptomatic 2. VS Therapeutic Management 1. Nursing Interventions 1. Continue to monitor 2. Determine/treat possible causes 1. Electrolytes 2. Medications 3. MI 3. Symptomatic bradycardia 1. ACLS guidelines Nursing Concepts 1. EKG Rhythms Patient Education 1. Count radial pulse 1. Report if <60 or >100 and symptomatic 1st degree is associated with MI, CAD, rheumatic fever, hyperthyroidism, electrolyte imbalances, & vagal stimulation (this can be as simple as the pt. bearing down to have a bowel movement). The P wave is the normal shape and rate just longer in duration. These pts are asymptomatic but this can signal more serious AV blocks. Treatment will be to stop the offending medication, give stool softeners, correct electrolyte imbalances, etc. 03.12 2nd Degree AV Heart Block Type 1 (Mobitz I, Wenckebach) Outline Overview 1. 2nd degree AV heart block type 1 1. Impulse from atria have difficulties reaching ventricles 1. AV node is defective 1. Progressively prolonged PR interval 2. Some QRS are dropped 2. Also called 1. Mobitz Type 1 2. Wenckebach Nursing Points General 1. Characteristics of 2nd degree AV heart block type 1 1. Rhythm 1. Regular 2. Irregular 2. Rate 1. Varies 1. Depends on underlying rhythm 3. P:QRS ratio 1. 1:1 1. Except in dropped QRS 4. PR interval 1. Progressively prolonged 1. Then QRS dropped 5. QRS complex 1. 0.06-0.12 seconds Assessment 1. Patient presentation 1. Asymptomatic Therapeutic Management 1. Nursing interventions 1. Continue to monitor 2. Know underlying rhythm 2. Determine/treat cause 1. Electrolytes 2. Medications 1. Digoxin 3. MI 3. Treat if symptomatic bradycardia 1. ACLS Nursing Concepts 1. EKG rhythms Patient Education 1. Count radial pulse 1. Report if symptomatic 03.13 2nd Degree AV Heart Block Type 2 (Mobitz II) Outline Overview 1. 2nd degree AV heart block type 2 1. Impulse from atria have difficulties reaching ventricles 1. 1. Defective AV node 2. Defective conduction system in ventricles 1. Dropped QRS 2. Also called 1. Mobitz Type II Nursing Points General 1. Characteristics of 2nd degree AV heart block type 2 1. Rhythm 1. Regular 2. Irregular 2. Rate 1. Varies 1. Usually slow 3. P:QRS ratio 1. 1:1 1. Except in dropped QRS 4. PR interval 1. Normal 1. 0.12-0.20 seconds 2. Prolonged 1. >0.20 seconds 5. QRS complex 1. 0.06-0.12 seconds Assessment 1. Patient presentation 1. Lightheaded 2. Dizzy/Syncope 3. S/S of decreased CO Therapeutic Management 1. Nursing interventions 1. Assess patient 2. VS 3. Notify MD 2. ACLS guidelines 1. Atropine 2. Prepare patient for pacemaker 1. Temporary if unstable 1. Transcutaneous 2. Permanent Nursing Concepts 1. EKG rhythms 2. Perfusion Patient Education 1. Seek medical help 03.14 3rd Degree AV Heart Block (Complete Heart Block) Outline Overview 1. 3rd degree AV heart block 1. Complete heart block 2. Atria are contracting at own pace 1. Signal unable to get to the ventricles 3. Ventricles are contracting at own slow pace 1. Decreased CO and perfusion 4. Dissociation between P waves and QRS complex 1. NO relationship between the atria and ventricles Nursing Points General 1. Characteristics of 3rd degree AV heart block 1. Rhythm 1. Regular 1. P to P 2. Regular 1. R to R 2. Rate 1. Varies 1. Usually slow 1. Ventricular rate 2. More P waves 1. Normal atrial rate 3. P:QRS ratio 1. No relationship between P waves and QRS 1. Not measurable 4. PR interval 1. No relationship between P waves and QRS 1. Not measurable 5. QRS complex 1. Wide 1. >0.12 seconds Assessment 1. Patient presentation 1. Fatigue 2. Dizzy/Syncope 3. Decreased CO 1. Hypotensive 2. Chest pain 2. Medical emergency Therapeutic Management 1. Nursing interventions 1. Assess patient 2. Therapeutic management 1. Pacemaker 1. Temporary if unstable/emergent Nursing Concepts 1. EKG rhythms 2. Perfusion Patient Education 1. Seek medical help 2. Defibrillation ▪ Defib for Vfib and pulseless Vtach ▪ Always continue chest compressions when waiting for defibrillator to charge & resume ASAP after discharge ▪ Monophasic defibrillators send energy in 1 direction so joules are set as high as 360j, biphasic sends energy in two directions so joules can be from 120-200j ▪ NEVER place pads over a pacemaker or AICD Asystole is cardiac standstill or “without contractions” there is no ventricular electrical electricity & no rate or rhythm, no pulse, and no C.O Some atrial electrical activity may be evident; if atrial electrical activity present, the rhythm is called P-wave Asystole The causes & clinical significance of asystole is extensive myocardial damage (from ischema or infarction), hypoxia, hypo/hyperkalemia, hypothermia, acidosis, drug OD, acute respiratory failure, ventricular aneurysm, and traumatic cardiac arrest Treatment is CPR & Epi, this will not be defibrillated because there is no rhythm to convert. 02.05 Nursing Care and Pathophysiology of Coronary Artery Disease (CAD) Outline Overview Pathophysiology: Coronary arteries are responsible for delivering oxygen to the heart. CAD occurs when plaque forms in the arteries. This plaque narrows the arterial space or the lumen. This narrowing causes blood flow to be impaired. When the blood flow is impaired oxygen delivery is inadequate. Oxygen can not supply the heart adequately. When oxygen is not sufficiently and adequately supplied to the heart tissue, ischemia occurs. 1. Coronary artery disease 1. Buildup of plaque in main vessels 2. Primary causes = high blood pressure and cholesterol 3. Sign = chest pain 1. Nursing Points General 1. Major vessels 1. Inner walls damaged 2. Inflammation 1. Plaque sticks to walls 2. Clots form 3. Blockage –> loss of blood supply to heart 2. Risk factors 1. Smoking 2. High blood pressure 3. Obesity 4. Diabetes 5. Hyperlipidemia 6. Family history 3. Complications 1. Acute coronary syndrome–>plaque breaks off and occludes coronary artery 1. STEMI (ST segment elevation myocardial infarction)–>”widowmaker” 1. Near or complete blockage 2. NSTEMI (non ST Segment elevation myocardial infarction) 1. Partial blockage 3. Unstable angina 4. Concerned for—>cardiac arrest Assessment 1. Presentation 1. Chest pain 2. Arrhythmia–>listen to heart 3. Shortness of breath 4. Elevated blood pressure 5. Possibly asymptomatic–>until MI 2. Doctor orders 1. Electrocardiogram (EKG) 2. Cholesterol levels 3. CT scan–>visualize vessel occlusion and stenosis 4. Angiogram–>view inside vessels 5. Stress test–>view blood flow Therapeutic Management 1. Medications 1. Cholesterol medications–>Statins 1. Decrease plaque in blood 2. Anticoagulants 1. Avoid blood clotting 3. Beta blockers 1. Decrease workload of heart 4. Calcium channel blockers 1. Relax vessels, allow blood through 5. Nitroglycerin 1. Open arteries, allow blood through–>decrease chest pain 2. Procedures 1. Angioplasty–>go in through vein to open vessels 2. Stent placement–>keep vessel open 3. Coronary artery bypass surgery–>new vessel pathway around blockage Nursing Concepts 1. Clotting 1. Walls damaged, plaque sticks, clots form 2. Perfusion 1. Build-up of plaque and blood clots–>decrease perfusion 3. Oxygenation 1. Decreased perfusion=decreased oxygenation of heart 4. EKG Rhythms 1. Show if heart damaged Patient Education 1. Quit smoking 2. Stay active 3. Eat healthy diet 4. Control stress 5. Manage diabetes Major cause of CAD is atherosclerosis Clinical Manifestations of CAD Angina Angina occurs because the myocardial cells are deprived of oxygen and glucose needed for aerobic metabolism and contractility. Anaerobic metabolism begins and lactic acid accumulates, this lactic acid irritates myocardial nerve fibers and transmits pain message to cardiac nerves and upper thoracic posterior nerve roots which accounts for referred cardiac pain to shoulders, neck, lower jaw, arms Management FIRST: Provide O2 Get ECG to find out if STEMI Give Nitrates (to vasodilate for symptomatic relief) & Morphine (to pain that SNS stimulation & decrease O2 demand) Aspirin THEN: Get to cath lab ASAP! If no cath lab then thrombolytic therapy Beta blockers (eg, metoprolol): indicated in all patients unless contraindicated 03.02 Nursing Care and Pathophysiology for Heart Failure (CHF) Outline Pathophysiology: In heart failure, the heart does not pump effectively. This can occur because of many reasons but usually, because there has been damage to the heart tissue. The heart is not able to pump enough fluid forward so fluid then backs up. This fluid backup increases work on the heart as it tries to keep up and cannot. Overview The heart is a pump, circulates blood throughout the body. Heart failure = pump failure. Heart failure occurs when the heart cannot pump enough blood to supply the body’s needs. Nursing Points General 1. Pump Failure 1. Decreased perfusion forwards 2. Increased congestion backwards 2. Causes 1. Myocardial Infarction 1. Dead muscle can’t pump 2. Hypertension 1. ↑ afterload = ↑ stress on heart muscle 3. Valve Disorders 1. Blood not moving in right direction 2. Inefficient pump 3. Diagnostics 1. BNP (Brain Natriuretic Peptide) – stretch of LV 2. Echocardiogram 1. Ejection Fraction 2. Can diagnose valve disorder 3. Chest X-Ray (CXR 1. Cardiomegaly 2. Pulmonary Edema 4. Complications 1. Volume Overload 1. Pulmonary Edema 2. Exacerbations 2. Decreased Perfusion 1. Heart 1. Angina, MI 2. Arrhythmias 2. Organs 1. Impaired Kidney Function Assessment 1. Right-Sided Heart Failure 1. Decreased Pulmonary Perfusion 1. ↓ oxygenation 2. ↓ activity tolerance 3. 2. Increased Systematic Congestion 1. Peripheral Edema 2. ↑ JVD 3. ↑ Preload 4. Weight Gain 5. Fatigue 6. Liver / GI Congestion 2. Left Sided Heart Failure 1. Decreased Systemic Perfusion 1. Skin pale or dusky 2. ↓ Peripheral pulses 3. Slow capillary refill 4. ↓ renal perfusion 1. ↓ urine output 2. Kidney Injury / Failure 2. Increased Pulmonary Congestion 1. Pulmonary edema 1. Cough 2. Pink/frothy sputum 3. Crackles 4. Wheezes 5. Tachypnea 6. SOB on Exertion 2. Anxiety/restlessness Therapeutic Management Goal is to decrease workload on heart while still increasing cardiac output. Discussed in more detail in Therapeutic Management Lesson 1. Decrease Preload 2. Decrease Afterload 3. Increase Contractility Patient Education Discussed in more detail in Therapeutic Management Lesson 1. Diet & Lifestyle Changes 2. Medication Instructions 3. Activity Restrictions 4. Frequent Follow-Ups Medications ▪ ▪ ▪ ▪ ▪ ▪ Vasodilators improves coronary artery blood flow by dilating the coronary arteries. Reduces preload, afterload (in high doses), & increases myocardial O2 supply Morphine dilates pulmonary and systemic blood vessels, reducing preload and afterload Positive inotropes increase myocardial contractility and are used for patients with evidence of cardiogenic shock or with low CO Diuretics are the first line for treating patients with volume overload ACE inhibitors block RAAS by inhibiting the conversion of angiotensin I to II, reduce afterload & SVR, inhibit ventricular remodeling Pts unable to tolerate ACE inhibitors are given angiotensin II receptor blockers (ARBs) promote afterload reduction & vasodilation Stages of Heart Failure A At high risk for HF, but without structural heart disease B Structural heart disease, but without signs or symptoms o C Structural heart disease with prior or current symptoms o D Refractory HF requiring specialized interventions BNP Heart Failure Guidelines So there are multiple ways that we can diagnose and classify heart failure, but we just want you to know these three. The lab value we use is called Brain Natriuretic Peptide or BNP – this is released whenever the ventricles are stretched. So in Congestive Heart Failure patients when they’re severely volume overloaded, we can see this number jump into the thousands. In the labs course we will talk in much more detail about this value, so be sure to check that out. Clinical Signs of Heart Failure So let’s look at what this patient looks like when you actually see them in practice… In the module intro we asked y’all to brainstorm what you thought this patient looked like. Guys if you get nothing else about Heart Failure, THIS is the part you’ve got to get. Remember we said that there’s decreased perfusion forward and increased congestion backwards, right? So in right-sided heart failure we’re going to see some oxygenation problems because of decreased perfusion to the lungs. They may struggle with activity because they just don’t have enough blood flow for their lungs! Then backwards we see that congestion into the system – they are way overloaded in the systemic circulation – so what does that mean? That means peripheral edema – okay how would you feel if you swelled up like crazy? You’d be tired, you’d probably gain some weight? Some of that fluid may even collect in the gut and make you nauseous. Then because the blood can’t get past the heart from the body, it even backs up into the neck and you’ll see this crazy jugular venous distention – it looks like a rope on their neck!! So if you’re seeing these signs of excessive volume out in the body – you gotta think right sided heart failure! Okay, so what about the left? Well they actually have decreased perfusion to the body. Remember your signs of decreased perfusion? They’re gonna be pale, decreased pulses, maybe slow cap refill, and their skin might even be cold, right? Signs of decreased perfusion. Then, we see the congestion happening in their lungs – y’all their lungs are full of fluid! How would you feel? You’d be struggling to breathe, right? They’ll have a cough, and their sputum will be pink and frothy because there’s just so much blood pumping through the lungs! Imagine if this was you and had all this fluid in your lungs – what position would you want to be in? You lay down and you’ll feel like you’re drowning – a lot of these patients sleep with lots of pillows or even in a recliner. Some of them even lose weight because it becomes a choice to either eat or breathe! So if you see these severe respiratory issues and fluid on the lungs, you’ve got to think Left-sided heart failure! So right sided the classic sign is the systemic overload and left-sided classic sign is pulmonary edema. If you get this you can pick out any issues they’ll have! Complications of Heart Failure Now, there are quite a few other complications of heart failure, but the one I really want y’all to understand is what happens when the kidneys don’t get perfused. So here’s our heart failure patient who has decreased perfusion forward and increased congestion backward. They’re volume overloaded, probably struggling to breathe, and now, they aren’t perfusing their kidneys. When the kidneys lose blood flow, it stimulates the Renin-Angiotensin-Aldosterone system (RAAS). You will learn more about this in pharmacology, but what you need to know is that it causes three main things to happen in the body. 1. The first is water retention because of aldosterone and ADH. The kidneys see a lack of flow and think they need to hold onto water! So it is increasing the preload (or stretch) on ventricles whose preload is already sky-high! 2. The second is vasoconstriction. This is the body trying to pull blood towards the heart to increase the blood pressure – this increases afterload (the force the heart has to pump against) – in a patient whose heart is already struggling as it is! 3. And the third is the RAAS activates the Sympathetic Nervous System – it’s basically telling the heart to work harder and faster – which it cannot do! The end result is MORE volume overload, MORE stress on the heart muscle, and a perpetuated cycle that never ends. That’s why I call it the cycle of death. What you’ll see when we look at therapeutic management in the next lesson is that the majority of therapy is aimed at breaking this cycle. So let’s recap – anything that can affect the heart’s ability to pump effectively can cause heart failure, including an MI, hypertension, and valve disorders. Right-sided heart failure presents with symptoms of decreased pulmonary perfusion and increased systemic congestion – so they’re swollen, gain weight, lots of edema. Left-sided is the opposite – decreased systemic perfusion and increased pulmonary congestion, so these patients are really struggling to breathe. We diagnose with a BNP, Chest X-ray, and Echocardiogram. And don’t forget that the impact this has on the kidneys can make the problem worse – we’ll talk about how we work to break that cycle of death for these patients. Nursing Care and Pathophysiology of Myocardial Infarction (MI) Outline Overview of Myocardial Infarction (MI) Sudden restriction of blood supply to a portion of the heart causing ischemia and death to the muscle tissue Nursing Points General 1. Myocardial infarction literally translates into “heart muscle death” and is the result of a complete loss of blood flow, or perfusion to the heart. 2. Oxygen supply can’t meet oxygen demand 3. Is often caused by atherosclerotic plaque breaking off of the vessel wall and causing acute loss of blood flow through the coronaries. Nursing Assessment 1. Chest pain 1. Burning, squeezing, crushing, etc 2. Radiation of pain 2. Shortness of breath 3. Irregular heart rate 4. Altered Vital Signs: 1. Hypertension vs Hypotension (shock) 2. Tachycardia 3. Abnormal EKG 4. Low O2 Saturation 5. Altered Labs: 1. Troponins! 2. Lipid profile 3. CBC/BMP Myocardial Infarction Therapeutic Management 1. Antiplatelet and Anticoagulant Medications 1. Prevent platelet aggregation and reduce viscosity of blood 2. Aspirin and IV heparin 2. Vasodilatory Agents 1. Nitroglycerin, Morphine 3. Time is Tissue: PCI (Percutaneous Coronary Intervention) should be performed within 90 minutes 1. To cath lab to attempt coronary artery stenting to restore blood flow 4. CABG (Coronary Artery Bypass Grafting) 1. In both emergent or non-emergent situations if PCI is unsuccessful 5. High-dose statin 6. Beta-blockers/ACE-inhibitors 7. Vital Sign and Lab Monitoring Nursing Concepts 1. Perfusion 2. Oxygenation Patient Education for Myocardial Infarction 1. Diet/Exercise 2. Smoking Cessation 3. Taking new medications as prescribed 4. Follow up Nursing Interventions MONA: Morphine Oxygen Nitroglycerin Aspirin (ASA) *note – this is only a mnemonic and not the correct order of administration – see rationale for details* RATIONALE Initial treatment for acute coronary syndrome. Morphine: given ONLY if aspirin and nitroglycerin do not relieve chest pain. Initial dose is 2-4 mg IV. Oxygen: helps for you to remember to check oxygenation for chest pain – if under 94% or if patient is short of breath give 2L NC initially. Administer oxygen only when clinically relevant. Nitroglycerin: This is the initial medication given, along with aspirin. This medication dilates the blood vessels to help allow any blood flow that might be impeded. Give 0.4 mg sublingual tab, wait 5 minutes, if the chest pain is not relieved administer another dose. This can happen 3 times total. Monitor a patient’s blood pressure, hold for a systolic BP of less than 90 mmHg. Aspirin: given to thin the blood and decrease mortality risk. A total of 4 baby aspirin (81 mg each) can be given for a total of 324 mg, or a single 325 mg dose. 12-Lead ECG If initial 12-lead ECG indicates inferior MI, do a right-sided 12-lead ECG. RATIONALE Assess a 12 lead ECG immediately on anyone complaining of chest pain to determine if an ST elevated MI is occurring. If it is-Take the patient to the cath lab STAT! If the ECG is a normal sinus or otherwise non-concerning rhythm, place them on a 3 or 5 lead cardiac monitor for frequent re-assessing. Right sided 12 lead ECG shows the right side of the heart to assess for right ventricular ischemia. **Inferior MI’s need to be treated differently!** 3 or 5 Lead monitoring RATIONALE No matter the outcome of the 12 lead ECG, placing a patient on a form of cardiac monitoring is key. You are worried about a worsening condition such as cardiac arrest. Cardiac Catheterization with Percutaneous Coronary Intervention (PCI) RATIONALE A patient who has an ST elevated MI (STEMI) will be rushed to the cath lab so they can locate the clot and place a stent to regain blood flow to the heart. A patient may also go to the cath lab without having a STEMI, and they may still find a clot. Most NON-STEMI’s are treated without catheterization. BP Monitoring The measurement is determined by the doctor, who is determining this based on evidence based research married with patient factors. It can be measured by the systolic BP or the Mean Arterial Pressure (MAP). This can also be monitored by an arterial line. RATIONALE This is important because the higher the blood pressure, the more pressure is on a clot. It isn’t out of the question for someone to have more than one clot, and increased pressure could break free a clot lodge itself somewhere else either in the heart, lungs, brain, or extremity. Heparin RATIONALE This is an anticoagulant that breaks up blood clots (as well as prevents them). Monitor aPTT or Anti-Xa Q6H to adjust and maintain therapeutic levels. For STEMI Bolus: 60 units/kg (max 4,000 units) Continuous infusion: 12 units/kg/hr -Adjust according to your organization’s nomogram (Q6H- based on results of aPPT or Anti-Xa) For N-STEMI Bolus: 60-70 units/kg (max 5,000 units) Continuous Infusion: 12-15 units/kg/hr -Adjust according to your organization’s nomogram (Q6H- based on results of aPPT or Anti-Xa) Insert Large Bore IV and draw initial Cardiac Enzymes RATIONALE IV access is important for administration of medications, possible interventions if angina worsens, and any scans that may be needed to rule out thrombosis. Cardiac enzymes further serve to rule out Myocardial Infarction and can give an indication to the extent of myocardial damage. Troponin I CK CK-MB Myoglobin Monitor Cardiac Enzymes: Troponin I Creatine Kinase-MB (CKMB) RATIONALE The values of these enzymes are based on your institutional laboratory technique. If they are elevated it indicates that the cardiac muscle is stressed out or injured. Troponin I is an enzyme that helps the interaction of myosin and actin in the cardiac muscle. When necrosis of the myocyte happens, the contents of the cell eventually will be released into the bloodstream. o Troponin can become elevated 2-4 hours after in ischemic cardiac event and can stay elevated for up to 14 days. Creatine Kinase MB: This enzyme is found in the cardiac muscle cells and catalyses the conversion of ATP into ADP giving your cells energy to contract. When the cardiac muscle cells are damaged the enzyme is eventually released into the bloodstream. o CKMB levels should be checked at admission, and then every 8 hours afterwards. Left coronary artery is called the widow maker Code Meds CABG Coronary artery bypass grafting is a surgery that improves blood flow to heart & is open heart surgery A healthy artery or vein from the body is connected, or grafted, to the blocked coronary artery. This grafted artery or vein bypasses the blocked portion of the coronary artery & creates a new path for oxygen-rich blood to flow to the heart muscle The goals of CABG is to improve the pt’s chance of survival, allowing them to resume a more active lifestyle, improve the pumping action of heart that may be damaged by a heart attack, lowering the risk of heart attack (in some patients, such as those who have diabetes), improving quality of life, reducing angina & other coronary heart disease symptoms. Steps to rhythm analysis 1. Determine rhythm (is it irregular?) For atrial rhythm, measure P-P intervals For ventricular rhythm, measure R-R intervals 2. Determine rate (How fast?) 1 lg blk=300, 2 lg blks=150, 3 lg blks=100, 4 lg blks=75, 5 lg blks-60, etc 3. Evaluate P wave – present?, normal size/shape?, one P for every QRS 4. Determine duration of PR interval – 0.12-0.20? Consistent? 5. Determine duration of QRS complex – 0.06-0.10? Same shape & size? Come after every P wave? 6. Evaluate T waves – present? Normal shape? Normal amplitude? 7. Determine duration of QT interval – duration a normal 0.36 to 0.44 second? As heart rate increases, QT interval decreases; when QTc is longer than 0.50 men/women, torsades de pointes likely to develop 8. Evaluate other components - ectopic beats? U wave present? repolarization of the Purkinje fibers d/t hypokalemia CPR-BLS (Basic Life Support) Outline Nursing Points General 1. CPR-BLS 1. CPR = Cardiopulmonary Resuscitation 1. Chest compressions 1. For circulation 2. Rescue Breathing 2. BLS = Basic Life Support 2. Assessment 1. Check scene for safety 2. Check for level of consciousness 1. If unconscious 1. Tap or shake shoulder 2. “Are you okay?” 2. If unresponsive 1. If others are around 1. Delegate 1. Bystanders call 911 2. Bystanders get AED 2. Start CPR 2. If alone 1. Call 911 2. Get AED if available 3. Start CPR 3. CPR 1. CAB Acronym 1. Chest compressions 1. Kneel next to shoulders and neck 2. Heel of hand over center of chest 1. Between nipples 3. Place other hand on top 4. Elbows straight 5. Shoulder placement 1. Directly over hands 6. Compressions 1. 2 inches deep 2. Rate = 100-120 per minute 1. Sing “Stayin’ Alive” for rhythm 3. 30 per cycle 2. Airway open 1. Head tilt, chin lift 1. Palm on forehead 2. Tilt head back 3. Lift chin with other hand 3. Breathing 1. Use barrier 1. Make seal 2. Breaths 1. 2 per cycle 2. 1 second each 3. Watch chest for rise and fall 1. Ensures air gets in 4. AED 1. Automated External Defibrillator 2. Analyzes heart rhythm 3. Determines if electric shock needed 4. Step by step voice instructions 5. Visual aids for hearing impaired 6. Placement and maintenance 1. Placement 1. Highly visible 1. Common areas 2. Bright colors 3. Mounted on walls 2. Maintenance 1. Monthly 1. Battery testing 2. Pad inspections 3. Accessory check 4. Calibration 02.05 Nursing Care and Pathophysiology of Acute Respiratory Distress Syndrome (ARDS) Outline Overview Acute Respiratory Distress Syndrome 1. Causes – anything causing inflammatory response in lungs 1. Bacteremia, Sepsis 2. Trauma, fat embolus 3. Burns + Fluid Resuscitation 4. Massive transfusion 5. Pneumonia, Aspiration 6. Drug overdose 7. Near drowning Pathophysiology: There are 4 phases within acute respiratory distress syndrome (ARDS). ARDS occurs rapidly and usually within 90 minutes of the body’s inflammatory response and between 24-48 hours of lung injury. In phase 1 there is an injury to the capillary endothelium of the pulmonary system. In phase 2 there is an injury to the basement membrane, interstitial space, alveolar epithelium. The damage to the lungs causes permeability so now fluid fills the alveoli (where it doesn’t belong) and this will impair gas exchange. In phase 3 there is damage to the alveoli because of the fluid that causes atelectasis and hypoxemia. In phase 4 the products of cell damage cause the formation of a hyaline membrane. This membrane is thick and will further prevent oxygen exchange. In this phase with impaired gas exchange, respiratory acidosis occurs. The damage to the lungs that occurs can not be reversed. Nursing Points General 1. Inflammatory Response 1. Cytokines 1. Alveolar damage 2. Scarring 3. Decreases lung compliance 2. Increased capillary permeability 1. “Floods” alveoli 2. Decreases gas exchange 2. Early recognition improves survival Assessment 1. Symptoms of underlying condition 2. Chest X-ray → diffuse bilateral infiltrates 1. “White Out” 3. Refractory Hypoxemia 1. P/F Ratio (PaO2 / FiO2) 2. Mild <300 3. Moderate <200 4. Severe <100 Therapeutic Management 1. Treat underlying cause 2. Ventilatory Support 1. High levels of PEEP 2. Prone position – improve flow into lungs 3. Special Vent Modes 1. APRV 2. Oscillator 3. Prevent Complications 1. O2 toxicity – keep sats 85-90% 2. Ventilator Acquired Pneumonia – prevent infection 3. Barotrauma – keep volumes 4-6 mL/kg 1. Damage caused by too much pressure in noncompliant lung Nursing Concepts 1. Oxygenation 2. Gas Exchange 3. Infection Control Patient Education 1. Educate family on severity of condition and probable course 2. Possible need for tracheostomy 3. Purpose for endotracheal tube and ventilator 4. Recovery time, may need rehab 5. Infection control precautions • • • • Type of pulmonary edema not related to heart failure Sudden progressive form of acute respiratory failure Alveolar capillary interface becomes damaged and more permeable to intravascular fluid • Alveoli fill with fluid Hallmark features • • • Bilateral patchy infiltrates on chest x-ray No signs or symptoms of heart failure No improvement in PaO2 despite increasing oxygen delivery Pulmonary System Barotrauma As lung inflation pressures increase, risk for barotrauma increases. Barotrauma results when the increased airway pressure distends the lungs and possibly ruptures fragile alveoli or emphysematous blebs. Patients with noncompliant lungs (e.g., COPD) are at greatest risk for barotrauma. • • • • • • • • • • • • Ventilator-associated pneumonia • Strategies for prevention of ventilator-associated pneumonia • Strict infection control measures • Elevate HOB 45 degrees or more to prevent aspiration Barotrauma • Rupture of overdistended alveoli during mechanical ventilation • To avoid, ventilate with smaller tidal volumes • Higher Paco2 • Permissive hypercapnia Volutrauma • Occurs when large tidal volumes are used to ventilate noncompliant lungs • Alveolar fracture and movement of fluids and proteins into alveolar spaces • Avoid by using smaller tidal volumes or pressure-control ventilation Stress ulcers • Bleeding from stress ulcers occurs in 30% of patients with ARDS on mechanical ventilation • Management strategies • Correction of predisposing conditions • Prophylactic antiulcer agents • Early initiation of enteral nutrition Renal failure • Occurs from decreased renal tissue oxygenation from hypotension, hypoxemia, or hypercapnia • May also be caused by nephrotoxic drugs used for infection associated with ARDS 2 kinds of inotropes: positive inotropes & negative inotropes. Positive inotropes strengthen force of heartbeat. Negative inotropes weaken force of heartbeat. Relieve bronchospasm – Albuterol Reduce airway inflammation – corticosteroids Reduce pulmonary congestion – Furosemide, Morphine, etc. Reduce anxiety & pain – Ativan, Fentanyl, etc. For atrial fibrillation - calcium channel blockers (Cardizem) & β-adrenergic blockers (Metoprolol) For infections – Zithromax & Rocephin • • • • Ethical considerations-pt’s values No Living will or DNR then life-saving measures are continued Closest relative- spouse, parents, siblings, etc. If disagreement between parents or siblings Hospital ethics committee 05.05 Nursing Care and Pathophysiology for Pulmonary Embolism Outline Overview 1. A pulmonary embolism is a life-threatening blood clot in the lungs caused by an embolus (usually blot clot) from a vein in the lower extremity, or from clots that form after surgery. 2. Causes decreased perfusion, hypoxemia, and if large enough, right-sided heart failure. 3. Management includes stabilizing the cardiopulmonary system and anticoagulant therapy. Nursing Points General When a blood clot breaks free and travels through the vascular system, it has the potential to become lodged and block blood flow. With a pulmonary embolism, this blood clot breaks free and travels through the right side of the heart and gets lodged in the pulmonary blood vessels, preventing blood from becoming oxygenated (and thereby decreasing perfusion to lung tissue). This is a life-threatening emergency and must be handled quickly, and precautions are always indicated. Assessment 1. Signs/Symptoms 1. Anxiety 2. Dyspnea/Tachypnea 3. Chest pain 4. Hypoxemia 5. Rales 6. Fever 7. Diaphoresis 8. Hemoptysis 2. Diagnostic Testing 1. Vital signs 2. ABG 3. CXR 4. V/Q lung scan 5. D-dimer 1. Negative D-dimer used to rule out PE on patients with a low likelihood of a DVT. 2. If positive, further testing necessary 6. Imaging with contrast dye 1. 1. 1. Spiral CT 2. Pulmonary angiogram Therapeutic Management 1. Therapeutic Management 1. Cardiopulmonary stabilization 1. Monitor for hypoxemia 2. Assess vital signs 3. Listen to lung sounds frequently 1. Rales 4. Heart sounds 5. Assess circulation 1. Peripheral edema 2. Distended neck veins 6. Monitor for feelings of anxiety/fear 7. HOB elevated 8. Oxygen as ordered 9. Analgesics 1. Morphine 2. Anticoagulation 1. Baseline labs 1. Platelet count 1. DO NOT administer if <100,000/mm 2. If value drops to half of baseline, consider HIT 2. Hemoglobin/Hematocrit 1. A drop can indicate hemorrhage 3. aPTT 1. Reflects response to treatment for titration of heparin 2. Monitor for bleeding 1. Bruising 2. Bloody stools 3. Hematuria 4. Gums/teeth 5. Flank pain 1. Nursing Concepts Clotting, Gas exchange, Oxygenation Patient Education 1. Oral anticoagulants 1. Side effects 2. Bleeding precautions 3. Follow up appointments 2. Pain management 1. Clot may still exist at discharge 1. ~4 weeks to dissolve 2. Pain medications as ordered 3. Activity 1. As tolerated 4. Some of the typical diagnostic test that you would do our abgs, chest X Ray, an ECG and this might be to check for atrial fibrillation, troponin levels which may be done to check for clots in coronary arteries & b/c of the pt’s c/o chest pain. The D dimer is going to be elevated once that clot starts to degrade, it is possible with the D dimer to get a false negative though. The CT scan requires a patient to get IV contrast. If the patient cannot get IV contrast then they will do a ventilation perfusion scan where they will inhale radioisotopes. A pulmonary angiography is the most sensitive diagnostic test but it is invasive and expensive. This angiography is considered the gold standard for diagnosing a pulmonary embolism and advances in medicine and technology have made this procedure safer. 5. Prevention is the best medicine in this case in order to keep a pulmonary embolism from happening. That is the reason why hospitals have come up with the VTE protocol that is the venous thromboembolism protocol that involves anticoagulants like heparin injections or lovenox injections, sequential compression devices, and Ted hose. If the patient has already had a PE then you would want to anti coagulate them so that you could prevent any further emboli. To help with any problem related to that pulmonary embolism you will want to give them oxygen and if it is significant enough they may have to go on the mechanical ventilator. Pulmonary toilet refers to any method used to assist in clearing secretions from the airways. This could be chest physiotherapy, maintaining hydration status, coughing and deep breathing, or using an incentive spirometer. This patient may have chest pain or they have been in mobile because of thoracic or abdominal pain which has compromised the respiratory system even more 6. The goal of anticoagulant therapy is to prevent clots from forming and it takes into account the patience VTE risk. Once the patient has already had a problem with clots they will be started on drug therapy to prevent any more clots from forming such as warfarin, heparin, lovenox, or other coagulation inhibitors. If the patients PE is significant enough they may want to go ahead and give thrombolytics which will break up the clot. 7. A patient that is hemodynamically unstable with a massive pulmonary embolism bit is not able to have thrombolytic therapy maybe a candidate 4 a pulmonary embolectomy. 2 prevent further emboli an IVC filter maybe the treatment for patients that are at high risk. A catheter in the femoral vein is placed in the inferior vena cava and a filter is deployed that will prevent clots from going into the pulmonary system complications with this device can be misplacement, migration, and perforation. 8. A tracheostomy is a surgically created stoma (opening) in the anterior part of the trachea (Fig. 26.3, A). A tracheostomy may be done to (1) establish a patent airway, (2) bypass an upper airway obstruction, (3) facilitate removal of secretions, (4) permit long-term mechanical ventilation, and (5) assist with weaning from mechanical ventilation. All tracheostomy tubes have a faceplate, or flange, which rests against the neck, and an obturator, which is used to help insert the tube. Many tracheostomy tubes have an outer cannula (which keeps the airway patent), and an inner cannula (which can be disposable or non disposable and removed for cleaning). At a minimum, you must assess the tracheostomy site every shift. Confirm the patency of the tracheostomy tube. Observe the site for any redness, inflammation, edema, ulceration, or signs of infection. Sterile dressing changes should be done every 12 hours. Clean around the stoma with normal saline and apply a sterile pre-cut dressing around the tracheostomy tube site. You can complete dressing changes more often based on your assessment. Change the tracheostomy tapes after the first 24 hours and then as needed (Fig. 26.5 and Table 26.9). A 2-person technique, 1 person to stabilize the tracheostomy and the other to change the tapes, is best practice to ensure that the tracheostomy does not become accidentally dislodged during the procedure. In some places, the HCP and/or respiratory therapist may complete this task. At the end of the procedure, place 2 fingers underneath the tapes to ensure they are not too tight around the neck. When turning and repositioning the patient, take care not to dislodge the tracheostomy tube. Because tube replacement may be difficult in the immediate postoperative period, several precautions are required, including (1) keep a replacement tube of equal or smaller size at the bedside, readily available for emergency reinsertion; (2) do not change tracheostomy tapes for at least 24 hours after the surgical procedure; and (3) if needed, the HCP performs the first tube change usually no sooner than 7 days after the tracheostomy. If the tube is accidentally dislodged, immediately call for help. While waiting for the HCP, a respiratory therapist, or other designated individual to arrive, several options may be used (depending on your nursing scope of practice and specific agency policies and procedures). It is essential that you know and understand your role and scope of practice for care of the patient with a tracheostomy. mmediately call for help. Quickly assess the patient’s level of consciousness, ability to breathe, and the presence or absence of any respiratory distress. If respiratory distress is present, you can quickly use a hemostat to spread the opening where the tube was displaced. Insert the obturator in the replacement (spare) tracheostomy tube, lubricate with saline, and insert the tube into the stoma. Once the tube is inserted, remove the obturator at once so that air can flow through the tube. TABLE 26.8 Suctioning a Tracheostomy Assess the need for suctioning hourly. Indications include visible coughing, coarse crackles or wheezes over large airways, moist cough, increase in peak inspiratory pressure on mechanical ventilator, and restlessness or agitation. Neurologic patients may not show any signs and/or symptoms of the need to be suctioned, so suctioning once per shift (at minimum) is recommended. Do not suction routinely. 1. If suctioning is indicated, explain procedure to patient. 2. Collect necessary sterile equipment: suction catheter (no larger than half the lumen of the tracheostomy tube), sterile water, cup, and personal protective equipment (PPE). If a closed tracheal suction system is used, the catheter is enclosed in a plastic sleeve and reused (Fig. 26.4). No other equipment is needed. 3. Check suction source and regulator. Adjust suction pressure to no greater than 125 mm Hg pressure with tubing occluded. 4. Assess heart rate and rhythm, respiratory rate and SpO2 to provide baseline for detecting changes in patient condition during suctioning. 5. Wash hands and put on PPE. 6. Use sterile technique to open package, fill cup with sterile water, put on sterile gloves, and connect catheter to suction tubing. Designate one hand as contaminated for (1) connecting and disconnecting the tubing at the suction catheter, (2) using the manual bag-valve-mask (BVM), and (3) operating the suction control. Suction sterile water through the catheter to test the system. 7. Provide preoxygenation for a minimum of 30 seconds by (1) adjusting ventilator to deliver 100% O2 or (2) using a reservoir-equipped BVM connected to 100% O2. The method chosen depends on whether the patient is attached to a mechanical ventilator or has a tracheostomy tube in place but is spontaneously breathing and receiving supplemental O2. The patient who has a long-term chronic tracheostomy and is not acutely ill may be able to tolerate suctioning without using a BVM. 8. Gently insert catheter without suction to the point at which the patient coughs. Do not insert the catheter until you meet resistance (this is the carina, and repeated trauma with suction catheter can promote bleeding). Apply suction as you slowly begin to withdraw the catheter. 9. Apply continuous suction for no more than 10 to 15 seconds. 10. Observe the patient during the suctioning procedure. Immediately stop suctioning and remove the suction catheter from the patient’s trachea if the patient becomes bradycardic or hypotensive, a dysrhythmia occurs, or SpO2 decreases to less than 90%. A vagal response may have occurred. 11. After each suction pass, wait at least 30 seconds before suctioning again. Always hyperoxygenate for at least 30 seconds (via mechanical ventilator or BVM with 5 or 6 breaths) in between each suctioning pass. 12. Repeat procedure until airway is clear. Limit insertion of suction catheter to as few times as possible. If airway is not clear after 3 suction passes, allow the patient to rest before additional suctioning. 13. Return O2 concentration to prior setting. 14. Rinse catheter. If using the in-line suction catheter (via mechanical ventilation), ensure that normal saline used to flush out the suction catheter does not enter the patient’s airway. For disposable suction catheters, dispose of catheter by wrapping it around fingers of gloved hand and pulling glove over catheter. Discard equipment in proper waste container. 15. Suction the oropharynx or use mouth suction. 16. Reassess heart rate and rhythm and SpO2. Auscultate to assess changes in lung sounds. 17. Record time, amount, and character of secretions and patient response to suctioning. TABLE 26.9 Tracheostomy Care The following are general guidelines for basic tracheostomy care. Become familiar with the specific policies and/or procedures in your agency: 1. Explain procedure to patient. 2. Use tracheostomy care kit or collect necessary sterile equipment (e.g., suction catheter, 1 pair sterile gloves, 1 pair nonsterile gloves, water basin, tracheostomy ties, tube brush or pipe cleaners, 4 × 4–inch gauze pads, sterile water or normal saline, tracheostomy dressing [optional]). NOTE: Clean rather than sterile technique is used at home. 3. Place patient in semi-Fowler’s position. 4. Assemble needed materials on bedside table next to patient. 5. Wash hands. Put on PPE. 6. Auscultate chest sounds. If wheezes or coarse crackles are present, suction the patient if unable to cough up secretions (Table 26.8). Remove soiled dressing and clean gloves. 7. Open sterile equipment, pour sterile H2O or normal saline into 2 compartments of sterile container or 2 basins, and put on sterile gloves. NOTE: Hydrogen peroxide (3%) is only used if an infection is present. If it is used, rinse the inner cannula and skin with sterile H2O or normal saline afterward to prevent trauma to tissue. 8. If present, unlock and remove inner cannula. Many tracheostomy tubes do not have inner cannulas. Care for these tubes includes all steps except for inner cannula care. 9. Replace a disposable inner cannula with a new cannula. With a non disposable cannula: • Immerse inner cannula in sterile solution and clean inside and outside of cannula using tube brush or pipe cleaners. • Rinse cannula in sterile solution. Remove from solution and shake to dry. • Insert inner cannula into outer cannula with the curved part downward, and lock in place. 10. Remove dried secretions from stoma using 4 × 4–inch gauze pad soaked in sterile water or saline. Gently pat area around the stoma dry. Be sure to clean under the tracheostomy flange (faceplate), using cotton swabs to reach this area. 11. Place dressing around tube (Fig. 26.5). Use a pre-cut tracheostomy dressing or unlined gauze. Do not cut the gauze because threads may be inhaled or wrap around the tracheostomy tube. Change the dressing as needed. Wet dressings promote infection and stoma irritation. 12. Change tracheostomy tapes, using a 2-person change technique. Tie tracheostomy tapes securely with room for 2 fingers between tapes and skin (Fig. 26.5). To prevent accidental tube removal, secure the tracheostomy tube by gently applying pressure to the flange of the tube during the tape changes. Do not change tracheostomy tapes for 24 hours after the tracheostomy procedure. 13. Some patients prefer tracheostomy tapes made of Velcro, which are easier to adjust. 14. Repeat care 3 times/day and as needed. Mechanical ventilation is the process by which the FIO2 (21% [room air] or more) is moved in and out of the lungs by a mechanical ventilator. Mechanical ventilation is not curative. It is a means of supporting patients until they recover the ability to breathe independently. It can also serve as a bridge to long-term mechanical ventilation or until a decision is made to stop ventilatory support. Indications for mechanical ventilation include (1) apnea, (2) inability to breathe or protect the airway, (3) acute respiratory failure (see Chapter 67), (4) severe hypoxia, and (5) respiratory muscle fatigue Types of Mechanical Ventilation The 2 major types of mechanical ventilation are negative pressure and positive pressure ventilation. Negative Pressure Ventilation Negative pressure ventilation involves the use of chambers that encase the chest or body and surround it with intermittent subatmospheric (or negative) pressure. The “iron lung” was the first form of negative pressure ventilation. It was developed during the polio epidemic. Intermittent negative pressure around the chest wall pulls the chest outward, reducing intrathoracic pressure. Air rushes in via the upper airway, which is outside the sealed chamber. Expiration is passive. The machine cycles off, allowing chest retraction. This type of ventilation is like normal ventilation in that decreased intrathoracic pressures produce inspiration, and expiration is passive. Negative pressure ventilation is noninvasive and does not need an artificial airway. Positive Pressure Ventilation Positive pressure ventilation (PPV) is the main method used with acutely ill patients (Fig. 65.19). During inspiration the ventilator pushes air into the lungs under positive pressure. Unlike spontaneous ventilation, intrathoracic pressure is raised during lung inflation rather than lowered. Expiration occurs passively as in normal expiration. There are 2 categories of PPV: volume and pressure ventilation.13 Volume Ventilation With volume ventilation, a predetermined VT is delivered with each inspiration. The amount of pressure needed to deliver the breath varies based on compliance and resistance factors of the patient-ventilator system. So, the VT is consistent from breath to breath, but airway pressures vary. Pressure Ventilation With pressure ventilation, the peak inspiratory pressure is predetermined. The VT delivered to the patient varies based on the selected pressure and compliance and resistance factors of the patient-ventilator system. Careful attention must be given to the VT to prevent unplanned hyperventilation or hypoventilation. For example, when the patient breathes out of synchrony with the ventilator, the pressure limit may be reached quickly, and the volume of gas delivered may be small. Alarm Possible Causes High-pressure limit • Secretions, coughing, or gagging • Patient fighting ventilator (ventilator asynchrony) • Condensate (water) in tubing • Kinked or compressed tubing (e.g., patient biting on ET tube) • ↑ Resistance (e.g., bronchospasm) • ↓ Compliance (e.g., pulmonary edema, ARDS, tension pneumothorax, atelectasis, pneumonia) • Improper alarm setting • ET tube inserted too far (e.g., right mainstem bronchus or carina) Interventions • Clear secretions and ↑ sedation • Reassure patient • Remove water from ventilator tubing • Unkink tubing, insert bite block, or reposition patient • Give bronchodilator • Assess breath sounds, obtain chest x-ray • Adjust ET tube Low-pressure limit • Total or partial ventilator disconnect • Loss of airway (e.g., total or partial extubation) • ET tube or tracheotomy cuff leak (e.g., patient speaking, grunting) Interventions • Check connections • Confirm adequate tidal volume and ET tube position with chest x-ray • Reinflate cuff Positive end-expiratory pressure (PEEP) is a ventilatory maneuver, or mechanical ventilator setting, in which positive pressure is applied to the airway during exhalation. Normally during exhalation, airway pressure drops to near 0, and exhalation occurs passively. With PEEP, exhalation is passive but pressure falls to a preset level, often 3 to 20 cm H2O. Lung volume during expiration and between breaths is greater than normal with PEEP. Ventricular Assist Devices A ventricular assist device (VAD) provides short- and long-term support for the failing heart and allows more mobility than the IABP. VADs are inserted into the path of flowing blood to augment or replace the action of the ventricle. Some VADs are implanted internally (e.g., peritoneum). Others are positioned externally. A typical VAD shunts blood from the left atrium or ventricle to the device and then to the aorta Continuous Positive Airway Pressure Continuous positive airway pressure (CPAP) restores functional residual capacity (FRC) and is similar to positive end-expiratory pressure (PEEP). However, the pressure in CPAP is delivered continuously during spontaneous breathing, preventing the patient’s airway pressure from falling to 0. For example, if CPAP is 5 cm H2O, airway pressure during expiration is 5 cm H2O. During inspiration, we generate 1 to 2 cm H2O of negative pressure. This reduces airway pressure to 3 or 4 cm H2O. CPAP is often used to treat obstructive sleep apnea. Bilevel Positive Airway Pressure In addition to O2, bilevel positive airway pressure (BiPAP) provides 2 levels of positive pressure support: higher inspiratory positive airway pressure and lower expiratory positive airway pressure.13 Like CPAP, the patient must be able to spontaneously breathe and cooperate with this treatment (Fig. 65.14). BiPAP is used for COPD patients with HF and acute respiratory failure and for patients with sleep apnea. Its use after extubation can help prevent reintubation. Patients with shock, altered mental status, or increased airway secretions cannot use BiPAP because of the risk for aspiration and the inability to remove the mask. ET intubation is common in ICU patients requiring mechanical ventilation for short periods of time (e.g., less than 2 weeks). Other indications for intubation include (1) upper airway obstruction (e.g., burns, tumor, bleeding), (2) apnea, (3) high risk for aspiration, (4) ineffective clearance of secretions, and (5) respiratory distress Steps for ET Begin then bagging them with 100% O2 for at least 3-5 mins, positioning them supine in the “sniffing” position, rapid sequence intubation (RSI) is a combination of sedation & paralytics to decrease aspiration & injury. Because RSI intubation needs to happen quickly, so pts with a difficult airway should not be done this way. Some of the problems related to intubation are chipping teeth, neck mobility if there is a suspected spinal cord injury, increased salivation, and difficulty swallowing. A patient may bite down on the tube, so a bite block or sedation may be necessary. ET tube needs to be secured very well and the nurse needs to ensure that does not move by frequently assessing position. Mouth care can be difficult, because of the size of the oral cavity with an ET tube and bite block. Once intubated inflate the cuff & confirm placement by attaching a CO2 detector, if in the esophagus then CO2 is not detected. Then listen for bilateral breath sounds & epigastric area for no sounds, watch for symmetric rise & fall. Check SpO2. If correct placement then hook up to ventilator & secure the ETT. Obtain a chest xray to confirm placement. Before intubation is started, preoxygenate the patient using the BVM and 100% O2 for 3 to 5 minutes. Each intubation attempt is limited to less than 30 seconds. Ventilate the patient between successive attempts using the BVM and 100% O2. Rapid-sequence intubation (RSI) is the rapid, concurrent administration of both a sedative and a paralytic drug during emergency airway management to induce unconsciousness for intubation. A sedative-hypnotic-amnesic (e.g., propofol, etomidate [Amidate]) is given to induce unconsciousness, along with a rapid-onset opioid (e.g., fentanyl) to blunt the pain of the procedure. This is followed with a drug (e.g., rocuronium) to produce skeletal muscle paralysis.17 Monitor the patient’s O2 status during the procedure with pulse oximetry. After intubation, inflate the cuff. Confirm the placement of the ET tube while continuing to manually ventilate the patient using the BVM with 100% O2. Use an EtCO2 detector to confirm proper placement by noting the presence of exhaled CO2 from the lungs (Fig. 65.16). Place the detector between the BVM and ET tube and look for a color change (indicating the presence of CO2) or a number. At least 5 or 6 exhalations with a consistent CO2 level must be present to confirm tube placement in the trachea.13 Auscultate the lungs for bilateral breath sounds and the epigastrium for the absence of air sounds. Observe the chest for symmetric chest wall movement. SpO2 should be stable or improve Obtain a chest x-ray to confirm tube location (2 to 6 cm above the carina in the adult). This position allows the patient to move the neck without moving the tube or causing it to enter the right mainstem bronchus. Once proper positioning is confirmed with x-ray, record and mark the position of the tube at the lip or teeth or nose. Pulmonary System Barotrauma As lung inflation pressures increase, risk for barotrauma increases. Barotrauma results when the increased airway pressure distends the lungs and possibly ruptures fragile alveoli or emphysematous blebs. Patients with noncompliant lungs (e.g., COPD) are at greatest risk for barotrauma. • • Ventilator-associated pneumonia • Strategies for prevention of ventilator-associated pneumonia • Strict infection control measures • Elevate HOB 45 degrees or more to prevent aspiration Barotrauma • Rupture of overdistended alveoli during mechanical ventilation • To avoid, ventilate with smaller tidal volumes • Higher Paco2 • Permissive hypercapnia Volutrauma • Occurs when large tidal volumes are used to ventilate noncompliant lungs • Alveolar fracture and movement of fluids and proteins into alveolar spaces • Avoid by using smaller tidal volumes or pressure-control ventilation Stress ulcers • Bleeding from stress ulcers occurs in 30% of patients with ARDS on mechanical ventilation • Management strategies • Correction of predisposing conditions • Prophylactic antiulcer agents • Early initiation of enteral nutrition Renal failure • Occurs from decreased renal tissue oxygenation from hypotension, hypoxemia, or hypercapnia • May also be caused by nephrotoxic drugs used for infection associated with ARDS 2 kinds of inotropes: positive inotropes & negative inotropes. Positive inotropes strengthen force of heartbeat. Negative inotropes weaken force of heartbeat. Relieve bronchospasm – Albuterol Reduce airway inflammation – corticosteroids Reduce pulmonary congestion – Furosemide, Morphine, etc. Reduce anxiety & pain – Ativan, Fentanyl, etc. For atrial fibrillation - calcium channel blockers (Cardizem) & β-adrenergic blockers (Metoprolol) For infections – Zithromax & Rocephin • • • • Ethical considerations-pt’s values No Living will or DNR then life-saving measures are continued Closest relative- spouse, parents, siblings, etc. If disagreement between parents or siblings Hospital ethics committee • • • • • • • • • • Artifical airway nursing care For thick secretions you need to make sure that the pt. is adequately hydrated can add extra water to tube feedings. Use humidify, just make sure that you are routinely assessing for accumulated condensation which will increase the pressure in the ventilator tubing. Make sure to empty excess condensation in the tubing away from the pt. Thick, copious secretions could also indicate developing pneumonia. Chest percussion and turning every two hours will mobilize secretions. Oral care- Brush teeth BID, oral swabs with 1.5% hydrogen peroxide every 2-4 hrs, chlorhexidine oral rinse twice a day, moisturizer to lips, oropharyngeal suctioning & reposition and retape ET tube every 24 hours. 02.02 EKG (ECG) Waveforms Outline Overview 1. The heart’s electrical activity that stimulates the atria and ventricles to contract produce a waveform on an EKG 2. These waveforms are broken down into in a P wave, QRS complex and T wave. Nursing Points 1. P wave 1. Atrial depolarization 1. Positive deflection 2. PR interval 1. Beginning of P wave to beginning of QRS 2. Time it takes for electrical current to reach ventricles 1. 0.12-0.20 seconds 2. QRS Complex 1. Ventricular depolarization 1. Negative and positive deflection 2. QRS interval 1. Beginning of the Q wave to ending of S wave 2. Time it takes for the electrical current to travel through the ventricles 1. 0.06 -012 seconds 3. T wave 1. Ventricular repolarization 1. Positive deflection 2. QT interval 1. Beginning of QRS to the end of T wave 2. Time it takes for the ventricles to contract and relax 1. 0.36-.044 seconds 3. ST segment 1. End of QRS complex to the beginning of T wave 2. Time between ventricular depolarization and repolarization Assessment 1. Recognize PQRST waveforms on EKG 2. Check pulse if abnormal waveforms are observed Therapeutic Management 1. Recognize and report abnormal waveforms 1. Long PR interval 2. Prolonged QRS Complex 3. Tall T waves Nursing Concepts 1. EKG Rhythms ECG The electrical activity of the heart is measured by electrodes & recorded on the electrocardiogram. The P wave starts with the firing of the SA node, causing a depolarization of the atria. The QRS starts with the firing of the AV node causing a depolarization of the ventricles. The T wave represents the repolarization of the ventricles. The spaces between the different waves – PR, QRS, & QT intervals – are the time that it takes for impulse to travel from one area to another. Any delay in the intervals indicates a dysfunction. 0.20-P wave 0.6-.12-qrs Depolarization represents the mechanical activity of contractions, or systole, which is the ejection of blood from the ventricles. Relaxation otherwise known as diastole is when the ventricles get refilled. Stroke volume is the amount of blood ejected from the ventricle with each heartbeat. To calculate cardiac output you would multiply the heart rate X the stroke volume. Generally 100mls fill the left ventricle but only 60mls is pushed into circulation. ▪ ▪ Stroke volume: Amt of blood ejected with each heart beat Cardiac output: Amt of blood pumped by each ventricle in 1 minute ▪ Normal 4-8 L/min • When cells are injured, they release their contents, including enzymes and other proteins, into the circulation. These biomarkers are useful in the diagnosis of myocardial injury and infarction. Cardiac-specific troponin is a myocardial muscle protein released into circulation after injury or infarction. Two subtypes, cardiac-specific troponin T (cTnT) and cardiacspecific troponin I (cTnI), are specific to myocardial tissue. Normally the level in the blood is very low, so a rise in level is diagnostic of myocardial injury. cTnT and cTnI are detectable within hours (on average of 4 to 6 hours) of myocardial injury, peak at 10 to 24 hours, and can be detected for up to 10 to 14 days. Troponin is the biomarker of choice in the diagnosis of MI. • • • Cardiac Biomarkers Creatine kinase (CK) – found in variety of organs, tissues Three isoenzymes CK-MM – specific to skeletal muscle CK- BB – brain & nervous tissue CK-MB - cardiac specific - specific for myocardial injury or infarction Rises in 3-6 hours, peaks in 12-24 hours, returns to baseline within 12-48 hours (level peak & return to normal can be delayed in one who had large MI) Additional blood studies C-Reactive protein – found in liver during acute inflammation Risk factor for coronary artery disease (CAD) Homocysteine (amino acid) Elevated levels increased risk for CAD, peripheral vascular disease (PVD), and stroke Diagnostic Studies of Cardiovascular System Cardiac natriuretic peptide markers Three types Atrial natriuretic peptide (ANP) - atrium B-type natriuretic peptide (BNP) – ventricles (best-cardiac or respiratory cause of dyspnea) C-type natriuretic peptide – endothelial, renal epithelial cells Increased levels of BNP levels signify heart failure Electrocardiogram • The basic P, QRS, and T waveforms are used to assess cardiac activity. Deviations from the normal sinus rhythm can indicate problems in heart function. • There are many types of electrocardiographic monitoring, including a resting 12-lead ECG, ambulatory ECG monitoring, and exercise or stress testing. • Continuous ambulatory ECG (Holter monitoring) can provide diagnostic information over a greater period of time than a resting 12-lead ECG. • An event monitor or loop recorder is used to document less frequent ECG events. An event monitor is a portable unit that uses electrodes to store ECG data once triggered by the patient. A disadvantage of this type of monitoring is that if symptoms occur for only a brief time, they may be over before the patient puts on the device and triggers it to record. Likewise, if patients are extremely symptomatic (e.g., syncopal), they may not be physically able to trigger the ECG recording. • An implantable loop recorder is used for patients who are suspected to have serious yet rare dysrhythmias. This small recorder is implanted though a small incision into the chest wall. It is activated to record either by the patient through a remote device or automatically if the heart rate exceeds or goes below a set rate. External loop recorders are worn for a month and require electrodes continually placed on the skin. This device only records when activated by the patient when symptoms occur. • Cardiac symptoms frequently occur only with activity due to the demand on the coronary arteries to provide more oxygen. Exercise testing is used to evaluate the heart’s response to physical stress. This helps to assess CVD and set limits for exercise programs. Exercise testing is used for individuals who do not have restrictions related to walking or using a bicycle. • The echocardiogram uses ultrasound (US) waves to record the movement of the structures of the heart. In the normal heart, ultrasonic sound waves directed at the heart are reflected back in typical configurations. • A contrast echocardiography involves the addition of an IV contrast agent (e.g., albumin microbubbles, agitated saline) to assist in defining the images, especially in technically difficult patients (e.g., obese). • The echocardiogram provides information about abnormalities of (1) valvular structures and motion, (2) cardiac chamber size and contents, (3) ventricular and septal motion and thickness, (4) pericardial sac, and (5) ascending aorta. • The ejection fraction (EF) or the percentage of end-diastolic blood volume that is ejected during systole can also be measured. The EF provides information about the function of the left ventricle during systole. • Stress echocardiography, a combination of treadmill test and US images, evaluates wall motion abnormalities. This test provides the information of an exercise stress test with the information from an echocardiogram. For those individuals unable to exercise, an IV drug (e.g., dobutamine [Dobutrex], dipyridamole [Persantine]) is used to produce pharmacologic stress on the heart while the patient is at rest. • Transesophageal echocardiography (TEE) provides more precise echocardiography of the heart than surface 2-D echocardiography by removing interference from the chest wall and lungs. The TEE uses a flexible endoscope probe with an US transducer in the tip for imaging of the heart and great vessels. The probe is passed into the esophagus to the level of the heart, and M-mode, 2-D, Doppler, and color-flow imaging can be obtained. TEE is contraindicated if the patient has a history of esophageal disorders, dysphagia, or radiation therapy to the chest wall. Patients will require sedation during a TEE. Cardiac Catheterization • Cardiac catheterization is a common outpatient procedure. It provides information about CAD, coronary spasm, congenital and valvular heart disease, and ventricular function. • Cardiac catheterization is also used to measure intracardiac pressures and O2 levels, as well as CO and EF. • With injection of contrast media and fluoroscopy, the coronary arteries can be seen, chambers of the heart can be outlined, and wall motion can be observed. • Cardiac catheterization is done by inserting a radiopaque catheter into the right and/or left side of the heart. • For the right side of the heart, a catheter is inserted through an arm vein (basilic or cephalic) or a leg vein (femoral). Pressures are recorded as the catheter is moved into the vena cava, the right atrium, the right ventricle, and the pulmonary artery. The catheter is then moved until it is wedged or lodged in position. This blocks the blood flow and pressure from the right side of the heart and looks ahead through the pulmonary capillary bed to the pressure in the left side of the heart (pulmonary artery occlusive pressure). This pressure assesses the function of the left side of the heart. • The left heart catheterization is done by inserting a catheter into a femoral or brachial artery. The catheter is passed in a retrograde manner up to the aorta, across the aortic valve, and into the left ventricle. Coronary angiography is done with a left-sided heart catheterization. • The catheter is positioned at the origin of the coronary arteries, and contrast medium is injected into the arteries. Patients often feel a temporary flushed sensation with dye injection. The images identify the location and severity of any coronary blockages. • Complications of cardiac catheterization include bleeding or hematoma at the puncture site, allergic reactions to the contrast media, looping or kinking of the catheter, infection, thrombus formation, aortic dissection, dysrhythmias, MI, stroke, and puncture of the ventricles, cardiac septum, or lung tissue. END-OF-LIFE CARE The goals for EOL care are to (1) provide comfort and supportive care during the dying process, (2) improve the quality of the patient’s remaining life, (3) help ensure a dignified death, and (4) provide emotional support to the family. T AB LE 9. 2 Physical Manif estation s at E nd of Lif e System Cardiovascular system Gastrointestinal system Manifestations • Increased heart rate; later slowing and weakening of pulse • Irregular rhythm • Decreased BP • Delayed absorption of drugs given IM or subcutaneously • Slowing or cessation of GI function (may be enhanced by pain-relieving drugs) • Gas accumulation • Distention and nausea • Loss of sphincter control, producing incontinence • Bowel movement before imminent death or at time of death System Integumentary system Musculoskeletal system Respiratory system Sensory system Manifestations • Mottling on hands, feet, arms, and legs • Cold, clammy skin • Cyanosis of nose, nail beds, knees • “Waxlike” skin when very near death • Gradual loss of ability to move • Sagging of jaw resulting from loss of facial muscle tone • Difficulty speaking • Swallowing becoming more difficult • Difficulty maintaining body posture and alignment • Loss of gag reflex • Jerking seen in patients on high doses of opioids • Increased respiratory rate • Cheyne-Stokes respiration • Inability to cough or clear secretions resulting in grunting, gurgling, or noisy congested breathing (death rattle or terminal secretions) • Irregular breathing, gradually slowing down to terminal gasps (may be described as guppy breathing) System Manifestations • Usually last sense to disappear Hearing Sight Taste and smell • Blurring of vision • Sinking and glazing of eyes • Blink reflex absent • Eyelids stay half-open • Decreased with disease progression Touch • Decreased sensation • Decreased sense of pain and touch Urinary system • Gradual decrease in urine output • Incontinence of urine • Inability to urinate