Uploaded by
Mirah Bognalbal
Anesthesiology Exam Prelims: Cranial Nerves & Pain Pathways
advertisement
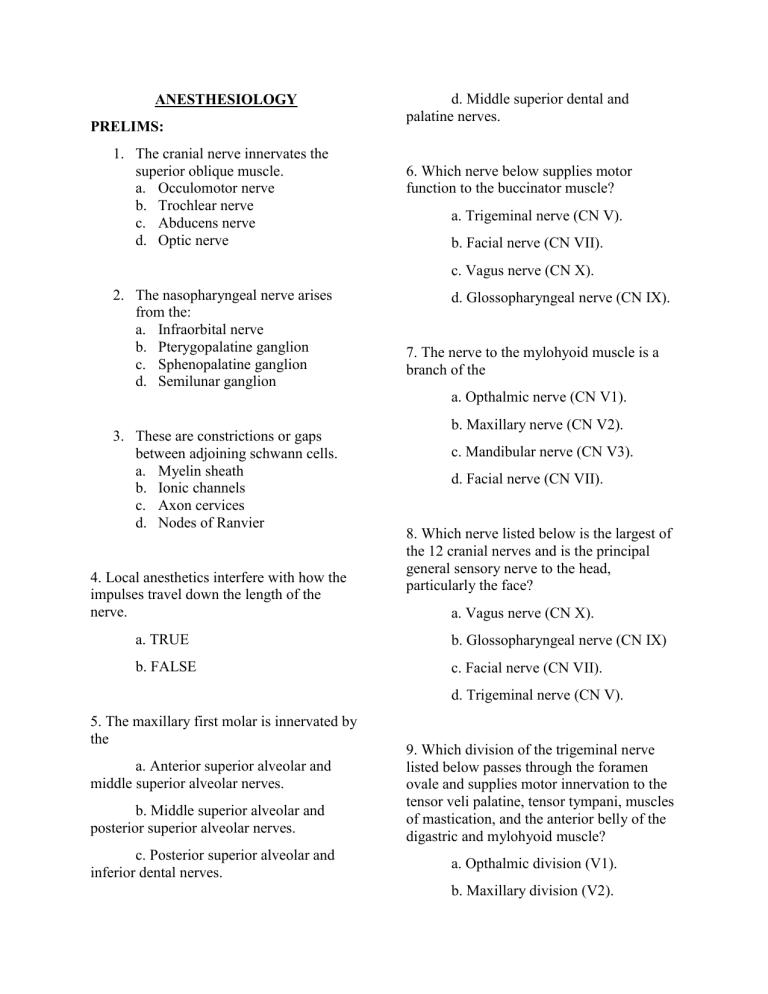
ANESTHESIOLOGY PRELIMS: 1. The cranial nerve innervates the superior oblique muscle. a. Occulomotor nerve b. Trochlear nerve c. Abducens nerve d. Optic nerve d. Middle superior dental and palatine nerves. 6. Which nerve below supplies motor function to the buccinator muscle? a. Trigeminal nerve (CN V). b. Facial nerve (CN VII). c. Vagus nerve (CN X). 2. The nasopharyngeal nerve arises from the: a. Infraorbital nerve b. Pterygopalatine ganglion c. Sphenopalatine ganglion d. Semilunar ganglion d. Glossopharyngeal nerve (CN IX). 7. The nerve to the mylohyoid muscle is a branch of the a. Opthalmic nerve (CN V1). 3. These are constrictions or gaps between adjoining schwann cells. a. Myelin sheath b. Ionic channels c. Axon cervices d. Nodes of Ranvier 4. Local anesthetics interfere with how the impulses travel down the length of the nerve. b. Maxillary nerve (CN V2). c. Mandibular nerve (CN V3). d. Facial nerve (CN VII). 8. Which nerve listed below is the largest of the 12 cranial nerves and is the principal general sensory nerve to the head, particularly the face? a. Vagus nerve (CN X). a. TRUE b. Glossopharyngeal nerve (CN IX) b. FALSE c. Facial nerve (CN VII). d. Trigeminal nerve (CN V). 5. The maxillary first molar is innervated by the a. Anterior superior alveolar and middle superior alveolar nerves. b. Middle superior alveolar and posterior superior alveolar nerves. c. Posterior superior alveolar and inferior dental nerves. 9. Which division of the trigeminal nerve listed below passes through the foramen ovale and supplies motor innervation to the tensor veli palatine, tensor tympani, muscles of mastication, and the anterior belly of the digastric and mylohyoid muscle? a. Opthalmic division (V1). b. Maxillary division (V2). c. Mandibular division (V3). d. None of the above. is due to liberation of which of the following neurotransmitter substance? a. Acetylcholine. 10. Which cranial nerve listed below provides motor innervation that allows for movement of the mandible? b. Hydroxylcholine. c. Cholinesterase. d. Acetylsalicylic acid. a. Trigeminal nerve (CN V). b. Olfactory (CNI). c. Facial nerve (CN VII). d. Vagus nerve (CN X). 14. Which of the following is not a transmitter substance released by the nerve cells at the time of impulse transmission? a. GABA. 11. How do local anesthetics affect the nerve membrane? a. They increase potassium flux. b. They increase the membrane excitability by increasing the membrane's permeability to sodium ions. c. They decrease the membrane's permeability to sodium ions and reduce the membrane excitability. d. They increase the calcium and chloride flux. 12. Which of the following innervates the buccal gingiva of the maxillary second premolar? b. Succinylcholine. c. Dopamine. d. Acetylcholine. 15. The best monitor of the level of analgesia is a. respiration. b. muscle tension. c. verbal response. d. eye movements. 16. The synthesis of procaine by ____________ in 1905 initiated a new era in local anesthesia. a. Buccal nerve. a. Niemann. b. Middle superior alveolar nerve. b. Koller. c. Anterior superior alveolar nerve. c. Halsted. d. Posterior superior alveolar nerve. d. Einhorn. 17. The maxillary first and second premolars are innervated by the 13. Alteration of the cell membrane permeability following a threshold stimulus a. ASA nerve b. MSA nerve and PSA nerve. d. Glutamate. c. PSA nerve. d. MSA nerve. 22. The pain pathway that extends from the spinal cord to the ventroposteromedial (VPM) nucleus of the thalamus. 18. The first synthetic amide local anesthetic synthesized in 1943 is a. Spinothalamic tract. a. Xylocaine. b. Trigemino pontoamygdaloid tract. b. Procaine. c. Spinoreticulothlamic tract. c. Cocaine d. none of the above. d. none of the above 19. He introduced epinephrine as a "chemical tourniquet" in 1903 23. The pain pathway that extends from the spinal cord to the intralaminar nucleus of the thalamus. a. Alfred Einhorn. a. Spinothalamic tract. b. Carl Koller. b. Spino pontoamygdaloid tract. c. Heinrich Braun. c. Spinoreticulothalamic tract. d. William Halsted. d. none of the above. 20. In the absence of MSAN, pulpal innervation of the mesiobuccal root of maxillary first molar as well as roots of the maxillary premolars comes from 24. The trigeminal nucleus is composed of a. 2 motor nuclei and 3 sensory nuclei. a. Nasopalatinenerve. b. PSA nerve. c. ASA nerve. d. Anterior or greater palatine nerve. 21. The following are peripheral mediators of pain, EXCEPT a. Prostaglandin. b. Bradykinin. c. Histamine. b. 2 sensory nuclei and 2 motor nuclei. c. 3 sensory nuclei and a motor nucleus. d. 2 sensory nuclei and a motor nucleus. 25. This theory proposes that pain is not a separate entity, but results from overstimulation of other primary sensations (touch, light, sound, etc.) a. Specificity theory (Rene Descartes, Muller, Von Frey) 1644. b. Central summation (pattern) theory (Goldscheider) 1894. c. Sensory interaction theory (Noordenbos). d. Gate control theory (Melzack and Wall) 1965. 26. This part provides metabolic support for the entire neuron (pseudo-unipolar neuron) and does not participate in the transmission of impulse 29. The entire nerve conduction process requires a. 3 secs. b. 1 sec. c. .7 msec. d. 3 msec. 30. During the repolarization state, sodium moves against its concentration gradient outside of the nerve membrane. This process requires the expenditure of energy in the form of a. phosphorous. a. axon. b. ATP. b. cell body. c. ADP. c. dentrite. d. chemical energy. d. both a and c. 31. It refers to the leaping of impulse from one node to the next. a. saltatory conduction. 27. Which of the following specialized cells produce myelin sheath in the CNS b. osmosis. a. Schwann cells. c. sodium pump. b. chromaffin cells. d. filtration. c. acinar cells. d. Oligodendrocytes. 28. This refers to the magnitude of the decrease in negative transmembrane potential that is necessary to initiate an action potential (impulse) a. Threshold potential. b. intensity. 32. At a certain point during nerve conduction process, a new impulse can be initiated at this time but only by a stronger than normal stimulus. This condition is known as a. absolute refractory period. b. impulse propagation. c. relative refractory period. d. none of the above. c. firing threshold. d. none of the above. 33. Which nerve listed below provides taste sensation on the tongue? a. Vagus nerve (CN X). d. Inferior alveolar nerve. b. Glossopharyngeal nerve (CN IX). c. Facial nerve (CN VII). d. Trigeminal nerve (CN V). 38. The inferior alveolar nerve is the largest branch of the mandibular division. a. The statement is true. 34. General sensation on the anterior 2/3rd of the tongue is provided by which of the following nerves? a. Vagus nerve (CN X). b. Glossopharyngeal nerve (CN IX). c. Facial nerve (CN VII). d. Trigeminal nerve (CN V). 35. Which of the following are meningeal branches of the trigeminal nerve that innervate the dura mater? a. Nervus spinosus. b. Middle meningeal nerve. b. The statement is false. 39. The temporalis muscle, masseter and lateral pterygoid muscles are innervated by the a. Lingual nerve. b. Inferior alveolar nerve. c. Mylohyoid nerve. d. Buccal nerve. 40. The anterior belly of the digastric muscle is innervated by the c. Infraorbital nerve. a. Chorda tympani nerve. d. Both a and b are correct. b. Mylohyoid nerve. 36. All of the following nerves branch off from the anterior division of the mandibular nerve, except a. Medial pterygoid nerve. b. Lateral pterygoid nerve. c. Buccal nerve. d. Deep temporal nerve. 37. The tensor veli palatini and the tensor tympani muscles are innervated by the a. Medial pterygoid nerve. b. Lateral pterygoid nerve. c. Buccal nerve. c. Tensor Tympani nerve. d. Palatine nerves. 41. The incisive nerve is sensory to the a. skin of the chin and the skin and mucous membrane of the lower lip. b. pulpal tissues of the mandibular first premolar, canine, and incisors via the dental branches. c. skin and mucous membrane of the upper lip. d. pulpal tissues of the maxillary premolars, canine, and incisors via the dental branches. 42. The MSAN and ASAN are branches within the a. Pterygopalatine fossa. c. Long buccal nerve and incisive nerve. d. Inferior alveolar nerve. b. Cranium. c. Infraorbital canal. d. Face. 43. The superior dental plexus is composed of smaller nerve fibers from the three superior alveolar nerves (PSAN, MSAN, and ASAN). In the mandible, the inferior dental plexus is composed of smaller fibers from the inferior alveolar nerve. a. The first statement is true, second statement is false. b. The first statement is false, second statement is true. c. Both statements are correct. d. Both statements are incorrect. 46. The primary innervation of the mandibular canine and incisors comes from the incisive branch of IAN. Possible accessory innervation of the aforementioned teeth may come from the nasopalatine nerve. a. The first statement is true, second statement is false. b. The first statement is false, second statement is true. c. Both statements are correct. d. Both statements are incorrect. 47. The four basic processes (in chronological order) involved in nociception are as follows a. Perception, transduction, modulation and transmission. 44. Possible accessory innervation of the maxillary molars and premolars could come from the a. Nasopalatine nerve. b. Incisive nerve. c. Anterior palatine nerve. b. Modulation, perception, transduction, and transmission. c. Transduction, transmission, perception, and modulation. d. Transmission, modulation, transduction, and perception. d. Mental nerve. 45. Possible accessory innervation of the mandibular molars and premolars could come from the a. Long buccal nerve and mylohyoid nerve. b. Mylohyoid nerve and incisive nerve. 48. The type of receptor found in A delta fibers is classified as a. Polymodal receptor. b. High-threshold mechanoreceptors. c. Chemoreceptors. d. all of the above. 49. This area in the brain identifies the intensity, type and location of the pain sensation and relates the sensation to past experiences, memory and cognitive activities. 53. Which one of the following nerves is found within the cavernous sinus? a. Trochlear nerve. b. Glossopharyngeal nerve. a. Reticular system. c. Abducens nerve. b. Somatosensory cortex. d. Occulomotor nerve. c. Limbic system. d. all of the above. 50. The modulation of pain involves inhibiting transmission of pain impulses in the a. Dorsal horn of spinal cord. b. Ventral root of the spinal cord. c. Limbic system. d. Hypothalamus. 51. The skin of the upper lip is innervated by the a. Superior palpebral nerve. b. Superior labial nerve. 54. No 55. The pterygopalatine ganglion gives rise to a. Frontal nerves. b. Zygomatic nerves. c. Pterygopalatine nerves. d. Infraorbital nerves. 56. Your answer in the previous question includes the following nerves except? a. Nasopalatine nerves. b. Anterior or greater palatine nerves. c. Posterior superior alveolar nerve. d. Zygomatic nerves. c. Superior alveolar nerve. d. Incisive nerve. 52. Sensation on the skin of the lower lip is supplied by the a. Mental nerve. b. Incisive nerve. c. Inferior labial nerve. d. Mylohyoid nerve. 57. The undivided nerve of the mandibular branch of the trigeminal nerve gives rise to the following nerves a. Middle meningeal nerve and lateral pterygoid nerve. b. Nerve to the medial pterygoid muscle and lateral pterygoid nerve. c. Nervus spinusus and nerve to the medial pterygoid muscle. d. Nervus spinusus. 58. Wala 59. Sensation in the skin of the cheek, the retromolar triangle, as well as the buccal gingiva of the mandibular molars and the mucobuccal fold in that region is supplied by the a. Posterior superior alveolar nerve. I 63. Sensation of the skin on the angle of the jaw is supplied by: a. Trigeminal nerve b. Facial nerve c. 2nd cervical spinal nerve d. 1st cervical spinal nerve b. Long buccal nerve. c. Mylohyoid nerve. d. Middle superior alveolar nerve. 60. The nerve that is commonly associated with parenthesis is the: a. Inferior alveolar nerve 64. According to this pain theory, pain signals that originate in an area of injury or disease do not travel directly or automatically to the brain. Rather, there exists within the spinal cord and trigeminal nucleus a 'mechanism' that determines the degree to which pain signals are transmitted to the brain. b. Lingual nerve a. Specificity theory. c. Myohyoid nerve b. Surface charge theory. d. Nerve to the medial pterygoid muscle c. Gate control theory. d. Summation theory. 61. The zygomatic nerve branches off from the maxillary nerve and enters the orbital cavity through the: a. Superior orbital fissure b. Infraorbital canal c. Inferior orbital fissure d. Foramen Ovale 65. The Tensor veli palatini is innervated by the a. Lesser (middle and posterior) palatine nerve. b. Nerve to the medial pterygoid muscle. c. Nerve to the lateral pterygoid muscle. 62. Ganglion is to nucleus as schwann cells is to: d. Anterior or greater palatine nerve. a. Neuron b. Oligodendrocytes c. Leukocytes d. Chromaffin cells 66. The tensor tympani is innervated by the: a. Nerve to the medial pterygoid muscle b. Auriculotemporal nerve c. Accessory nerve d. Nervus spinusus 67. The following muscles of mastication are supplied by the buccal nerve, except: 71. Pulpal innervation of maxillary anterior teeth including the supporting structures on the labial aspect of these teeth comes from the a. PSA nerve. a. Masseter muscle b. MSA nerve. b. Temporalis muscle c. ASA nerve. c. Lateral pterygoid d. All of the above. d. Medial pterygoid muscle 68. The thalamic nucleus which receives impulses coming from the trigeminal nucleus is called a. Ventroposteromedial thalamic nucleus. b. Intralaminar thalamic nucleus. c. Substancia gelatinosa. 72. The following nerves are found within the common tendinous ring or annulus of Zinn, except a. Occulomotor nerve. b. Abducens nerve. c. Nasociliary nerve. d. Frontal nerve. d. Geniculate nucleus. 73. The common tendinous ring or annulus of Zinn is the origin of the 69. Maxillary nerve is to foramen rotundum as Opthalmic nerve is to a. Infraorbital canal. b. Foramen ovale. c. Superior orbital fissure. a. Intraocular muscles. b. Extraocular muscles. c. Orbicularis oculi muscles. d. Axial muscles. d. Foramen lacerum. 74. The muscles at the floor of the mouth is innervated by: 70. Pulpal innervation of the mandibular 2nd bicuspid comes from the a. Inferior alveolar nerve b. Mental nerve. c. Incisive nerve. d. Lingual nerve. a. Lingual nerve b. Mylohyoid nerve c. Long buccal nerve d. Inferior alveolar nerve 75. Cold sensation in the mouth is received by the 80. The following cranial nerves are classified as purely motor, except a. A delta fibers. a. Hypoglossal nerve. b. Krause end bulbs. b. Facial nerve. c. C fibers. c. Abducens nerve. d. Free nerve endings. d. Vagus nerve. 76. Throbbing pain is transmitted by a. A delta fibers. b. B fibers. c. C fibers. d. A beta fibers. 77. Foramen lacerum provides entry for the a. Nervus spinusus. b. External carotid artery. c. Internal carotid artery. d. Internal maxillary artery. 78. Sensation in the skin of the chin is supplied by the a. Incisive nerve. b. Lingual nerve. c. Buccal nerve. d. Mental nerve. 79. The interseptal bone in multi-rooted teeth is innervated by the a. Interradicular nerves. b. Interdental nerves. c. Dental nerves. d. All of the above. LABORATORY 1. The anterior superior alveolar nerve. a. provides sensation to the palatal mucosa in the region of the premaxilla. b. provides innervation to the pulp, buccal mucosa, periodontal ligament, and the mucous membrane of the maxillary cuspid and incisors. c. provides general sensation at the anterior 2/3 of the tongue. d. sensory from the middle part of the upper eyelid. 2. The Nasociliary Nerve a. is sensory to the skin over the apex and ala of the nose. b. Innervates the masseter muscle. c. is sensory to the lining of mastoid 4. The Middle Superior Alveolar Nerve a. provides innervation to the pulp, buccal mucosa, periodontal ligament, and the mucous membrane of the upper molars except the mesiobuccal root of first molar. b. provides innervation to the pulp, buccal mucosa, periodontal ligament, and the mucous membrane of the upper premolars and the mesiobuccal root of first molar. c. provides sensation to the palatal soft tissues and bone anterior to the first premolar. d. None of the above. 5. The Supraobital nerve a. Largest branch of V3. b. sensory from the middle part of the upper eyelid. c. Innervates the masseter muscle. cells. d. is sensory to the skin of the lower d. All of the above. eyelid. 6. The maximum dose of epinephrine in healthy adult patient is: 3. The Posterior Superior Alveolar Nerve a. .04 mg a. Sensory to the TMJ. b. sensory to the anterior two-thirds of the tongue. b. .14 mg c. .2 mg d. .34 mg c. sensory to the skin over the zygomatic bone. d. provides innervation to the pulp, buccal mucosa, periodontal ligament, and the mucous membrane of the upper molars root of first molar. except the mesiobuccal 7. Zygomaticotemporal nerve a. sensory to the skin over the zygomatic bone. b. sensory from the skin of the temporal region. c. sensory from the mucous membrane of the soft palate and tonsil area. d. innervates the skin of the chin and the skin of the lower lip. d. Sensory to the skin of the lower eyelid. 11. The Lingual nerve a. General sensation at the anterior 2/3 of the tongue. b. Gustatory sensory to the anterior two-thirds of the tongue. c. sensory to the lining of mastoid cells. 8. The Anterior or greater palatine nerve a. sensory to the lining of mastoid d. Sensory to the skin of the lower eyelid. cells. b. innervates the pulp tissues of the mandibular first premolar, canine and incisors. c. provides sensation to the palatal soft tissues and bone from premolar to molars. d. innervates the skin of the chin and the skin of the lower lip. 9. The Inferior Alveolar Nerve a. Largest branch of V3. b. sensory from the middle part of the upper eyelid. 12. The Nasopalatine nerve a. provides sensation to the palatal mucosa in the region of the premaxilla. b. innervates the pulp tissues of the mandibular first premolar, canine and incisors. c. provides sensation to the palatal soft tissues and bone anterior to the first premolar. d. innervates the skin of the chin and the skin of the lower lip. 13. The Mental nerve c. Innervates the masseter muscle. d. sensory to the TMJ. 10. The Lingual nerve a. General sensation at the anterior 2/3 of the tongue. b. Gustatory sensory to the anterior two-thirds of the tongue. c. sensory to the lining of mastoid cells. a. sensory to the lining of mastoid cells. b. innervates the pulp tissues of the mandibular first premolar, canine and incisors. c. provides sensation to the palatal soft tissues and bone anterior to the first premolar. d. innervates the skin of the chin and the skin of the lower lip. 14. The Incisive Nerve a. sensory to the lining of mastoid cells. b. provides sensory innervation to the buccal gingiva of the mandibular molar. d. innervates the pulp tissues of the mandibular first premolar, canine and incisors. 17. Wala c. innervates the skin of the chin and the skin of the lower lip. d. innervates the pulp tissues of the mandibular first premolar, canine and incisors. 15. The Auriculotemporal Nerve a. Largest branch of V3. b. sensory from the middle part of the upper eyelid. 19. The Masseter Nerve a. sensory from the middle part of the upper eyelid. b. sensory to from the skin of the upper eyelid and lateral part of the eyebrow region. c. Sensory to the skin of the lower eyelid. c. Innervates the masseter muscle. d. Innervates the masseter muscle. d. sensory to the TMJ. 20. The Chorda tympani 16. The Inferior Palpebral nerve a. sensory to the lining of mastoid cells. b. Sensory to the skin of the lower a. General sensation at the anterior 2/3 of the tongue. b. Gustatory sensory to the anterior two-thirds of the tongue. eyelid. c. sensory to the lining of mastoid c. sensory from the middle part of thE upper eyelid. d. Innervates the masseter muscle. 18. The Nervus tentorii a. sensory to the lining of mastoid cells. b. provides sensory innervation to the buccal gingiva of the mandibular molar. c. innervates the skin of the chin and the skin of the lower lip. cells. d. Sensory to the skin of the lower eyelid. 21. Taste from the posterior third of the tongue is supplied by the a. Facial nerve. b. Glossopharyngeal nerve. c. Trigeminal nerve. d. Hypoglossal nerve. 22. Cranial nerve VI innervates the a. Medial rectus muscle. b. Superior rectus muscle. c. Lateral rectus muscle. d. Inferior rectus muscle. 23. Muscles of the tongue are innervated by the a. Glossopharyngeal nerve. b. Hypoglossal nerve. c. Facial nerve. d. Trigeminal nerve. 24. The nervus spinosus reenters the cranium through the a. Foramen rotundum. b. Foramen ovale. c. Foramen lacerum. d. Foramen spinosum. 25. It is also known as the buccinator nerve. a. Facial nerve. b. Mylohyoid nerve. c. Long buccal nerve. d. Anterior belly of the digastric muscle. a. Epinephrine.. MIDTERMS : b. Norepinephrine. 1. Which one of the following statement is not true regarding difficulty of reachieving profound anesthesia? a. More likely to develop if nerve function returns before reinjection. b. The duration, intensity, and spread of anesthesia with reinjection are greatly reduced. c. Patient may develop tolerance to a drug that is administered repeatedly. d. Patient may develop allergic reaction after readministration of local anesthetic. c. Isoproterenol. d. Phenylephrine. 5. — 6. The maximum dose of epinephrine in healthy adult patient is a. .04 mg. b. .14 mg. C. .2 mg. d. .34 mg. 2. Stimulation of ß receptors produces the following, EXCEPT; a. Vasodilation. 7. The maximum dose of norepinephrine 1:30,000 in healthy adult patient is b. Bronchodilation. a. .04 mg. c. Vasoconstriction. b. .14 mg. d. Increased heart rate and strength of contraction C. .2 mg. d. .34 mg. 3. Stimulation of a receptors by a sympathomimetic drug usually produces a response that includes a. Reuptake and vasoconstriction. b. Bronchodilation. c. Lipolysis. 8. Levonordefrin is available commercially as: a. Isuprel. b. Neo-Cobefrin. C. Levophed. d. Neo-synephrine. d. Increased heart rate and strength of contraction. 9. It is considered as the weakest vasoconstrictor. 4. Which of the following is a pure a-adrenergic agonist? a. Isuprel. b. Neo-Cobefrin. C. Levophed. d. Neo-synephrine. 10. Levonordefrin should be avoided in patients who are taking 14. Most clinically useful local anesthetic are classified as of action. a. Class A agent. b. Class B agent. a. B-blockers. C. Class C agent. b. Tricyclic antidepressants. d. Class D agent. c. MAO inhibitors. d. All of the above. 11. Stimulation of this sympathetic receptors produces reuptake of the drug. 15. The Hydrophillic group in local anesthetic agent is usually made up of: a. Benzoic acid. b. Tertiary amine. a. al receptor. c. Ester. b. a2 receptor. d. Amide. c. B1 receptor. d. B2 receptor. 12. The following factors may influence the rapid absorption of Local anesthetic, EXCEPT: a. Application of cold in the injection site. 16. Regional anesthesia is contraindicated in the following cases, EXCEPT a. patient is below the age of reason b. mental deficiencies. c. allergy to local anesthetics. d. minor infection b. Application of heat in the injection site. c. Vasodilating property of the drug. d. absence of vasopressor. 17. Which of the following is the local anesthetic of choice for patients with plasma cholinesterase deficiency? a. Mepivacaine. 13. The vasodilator activity of local anesthetics affect: a. Onset of action and duration. b. Tetracaine. c. Propoxycaine.. d. Procaine. b. potency only. c. duration only. d. Potency and duration. 18. The local anesthetics suitable for use in dentistry as topical anesthetic agent include a. Benzocaine and Procaine. c. 2% Lidocaine epinephrine. b. Pocaine and Lidocaine with 1:100,000 d. All of the above. c. Benzocaine and Lidocaine. d. Benzocaine and Mepivacaine. Question 23 Amide type of local anesthetics undergo biotransformation primarily in the Question 19 The patient developed allergy administration of amide type of local after anesthetics. The most propable cause is due to a. Anesthetic drug. b. Contamination. c. Epinephrine. d. Methylparaben. Question 20 Faulty technique in the induction of local anesthetics will most likely result in a. b. c. d. Ineffective anesthesia Bradycardia Hypertension Prolonged Anesthesia Question 21 In large doses, this anesthetic solution should be avoided in patients suffering from idiopathic methemoglobinemia a. b. c. d. Propoxycaine Lidocaine Prilocaine Mepivacaine a. Lungs. b. Kidneys. c. Liver. d. Blood. Question 24 The only local vasoconstriction is anesthetic which causes a. Lidocaine. b. Mepivacain. c. Prilocaine. d. Cocaine. Question 26 The use of epinephrine for local hemostasis during surgery might result in a. cardiac arrhythmia. b. acute asthmatic attack. c. drastic drop of BP. d. hypoglycemia. Question 22 Which of the following is considered as short acting anesthetics? a. 2% Mepivacaine with 1:20,000 Levonordefrin. b. 4% Prilocaine. Question 27 The directly acting sympathomimetic amines exert their actions directly on adrenergic receptors and include the following, EXCEPT a. Norepinephrine. b. Amphetamines. c. Adrenalin. Question 32 d. Levonordefrin. Stimulation of beta 2 adrenergic receptors produces Question 28 Drugs that will temporarily interrupt propagation of impulse when injected into the tissue is called a. Antibiotics. b. Decreases gastric secretion. c. Bronchodilation. d. Pupillary dilation. b. Analgesics. Question 33 c. Local anesthetics. Vasoconstrictors are use with local anesthetics to _________, EXCEPT: d. Narcotics. Question 29 Which of the following is not an adverse effect of vasoconstrictors? a. b. c. d. a. Bradycardia. Palpitation Hypertension Hypotension Bradycardia a. Decrease blood flow in site of surgery b. Prevent absorption of local anesthetics into general circulation c. Prolong the action of local anesthetics d. Potentiates or increases anesthetic effect Question 34 Epinephrine stimulates these adrenergic receptors in the cardiovascular system. a. Alpha and Beta. Question 30: a. Inhibiting synthesis of norepinephrine b. Competitive inhibition of post junctional adrenergic receptors c. Increasing the metabolism of norepinephrine d. All of the above Question 31 Which of the following is a brand name of Bupivacaine? b. Beta only. c. Alpha only. d. Neither Alpha nor Beta. Question 35 Which of the following is an endogenous cathecolamine? a. Ampethamine. a. Benzocaine. b. Phenylephrine. b. Ravocaine. c. Dopamine. c. Citanest. d. Ephedrine. d. Sensorcaine. Question 36 c. Benzocaine. Which of the following is not a requirement of an ideal local anesthetic agent d. Lidocaine. a. It must be non-toxic. b. It must me easily administered. c. It must be water soluble. d. Its effect must be irreversible. Question 40 Local anesthetic drugs block a. motor conduction only. b. synaptic transmission only. c. motor and sensory conduction. Question 37 d. sensory conduction only. Effectiveness of a local anesthetic depends on the following, EXCEPT a. addition of vasoconstrictor. b. concentration of drug used. c. acidic tissue pH. d. chemical nature of drug. Question 41 The anesthetic drug that produces powerful stimulation of cerebral cortex is a. Cocaine. b. Bupivacaine. c. Tetracaine. Question 38 d. Lidocaine. At which tissue pH will the local anesthetic be effectively diffused? a. Below 7. b. 9.1 c. 7.4 d. pH doesn't play a role. Question 42 When vasoconstrictors produce constriction of arterioles, the site of action is at which receptor? a. Alpha. b. Beta.. c. Gamma. d. Delta. Question 39 Which of the following exhibits weakest effectivity as a topical anesthetics? a. Tetracaine. b. Mepivacaine. Question 43 Each of the following drugs is considered to be an indirect-acting catecholamines, EXCEPT a. Dopamine. b. Amphetamine. c. Tyramine. Question 48 d. Methamphetamine. High pH (basic) of LA tends to shifts toward the free base form resulting to formation of more RN. a. The statement is true. Question 44 The first sensation usually lost administration of a local anesthetic is b. The statement is false. after c. Both statements are true.. a. Pain. d. Both statements are false. b. Pressure. c. Touch. Question 49 d. Proprioception. Low pH (acidic) of LA tends to shifts toward the cationic form resulting to formation of more RNH+. Question 45 Which of the following is a local anesthetic subject to inactivation by plasma esterases? a. b. c. d. a. The statement is true. b. The statement is false. Lignospan Marcaine Polocaine Novocain Question 46 Local anesthetics interfere with the transport of which of the following ions during drug-receptor interaction? a. Chloride. b. Sodium. c. Both statements are true. d. Both statements are false. Question 50 The role of sodium metabisulfate in local anesthetic agent is: a. b. c. d. Presrvative Fungicide Reducing agent Vasoconstrictor c. Potassium. Question 51 d. Calcium. Symptoms of epinephrine overdose following a local anesthetic injection may include all of the following, EXCEPT Question 47 EMLA is a mixture of a. Lidocaine and Prilocaine. b. Mepivacaine and Lidocaine. a. Restlessness. b. Hypotension. c. Apprehension. d. Palpitation. c. Lidocaine and Xylocaine. d. Mepivacaine and prilocaine. Question 52 Trismus during block anesthesia is a result of a. Massive edema. b. Damage to medial pterygoid muscle. c. Damage to lateral pterygoid muscle. Question 57 d. Damage to IAN. Bupivacaine, a local anesthetic agent, is used in dentistry in the concentration of Question 54 The primary organ for the excretion of local anesthetic and its metabolites is the a. Lungs. a. 2 %. b. 4%. c. 1.5% d. 0.5%. b. Liver. c. Kidney.. Question 58 d. Skin. The site of action of local anesthetic is on the a. Axoplasm. Question 55 b. Epineurium Sodium bicarbonate when given with local anesthetics has which of the following effect? c. Nerve membrane. d. Perineurium. a. Causes rapid elimination of the anesthetic drug. b. Decrease diffusion of the anesthetic drug. Question 59 Oraqix is used for c. Increase onset and depth of anesthesia. a. Gow Gates Technique. d. Causes rapid absorption of the anesthetic drug. b. Gasserian ganglion block. c. Intrapulpal anesthesia. d. Anesthetizing intact mucosa Question 56 All of the following are complications of LA toxicity, EXCEPT a. Cardiac depression. Question 60 The most common emergency seen after the use of local anesthetic is b. CNS depression. a. Trismus. c. Paresthesia. b. Syncope. d. Respiratory depression. c. Toxic reaction. d. Swelling b. Infiltration produces adequate anesthetia in primary molar so there's no need to perform block anesthesia. c. Two times as potent as lidocaine, mepivacaine, and prilocaine. Question 62 d. Only amide local anesthetic that also contains an ester group. Which of the following will happen if intravascular injection of LA with epinephrine was done accidentally? a. Hypotension + Bradycardia. b. Hypertension + Bradycardia. c. Hypertension + Tachycardia. Question 66 The maximum recommended dose of Articaine in healthy patient is a. 1.3 mg/kg. d. Hypotension + Tachycardia. b. 5 mg/kg. Question 63 c. 7 mg/kg. A patient who had history of hepatitis a month ago should be preferably given which anesthetic agent? d. 2 mg/kg. a. Lidocaine. b. Propoxycaine. c. Mepivacaine. d. Procainamide. Question 67 During mandiblock, local anesthetic solution is deposited as close as possible to the: a. b. c. d. Coronoid notch Neck of mandibular condyle External oblique ridge Lingula Question 64: Which one of the following regional techniques requires extraoral landmarks? a. b. c. d. e. High tuberosity approach Traditional IAN block Gow gates technique Vazirani-Akinosi Technique Question 68 The following affects the duration of local anesthesia, EXCEPT a. Protein binding capacity of local anesthetic. b. Addition of vasoconstrictor. Question 65 All are true about use of Articaine in pediatric patient, EXCEPT a. It's an amide which is metabolized in the liver. c. Vasodilator activity of local anesthetic. d. Non-nervous tissue diffusibility. Question 69 Which space has the highest incidence of infection after Classical IAN Block administration? a. Buccal space. b. Pterygomandibular space c. Parapharygeal space. d. Pretracheal space. Question 70 Which of the following anesthetic agents would be preferred in long dental procedure? a. Lignospan. b. Isocaine. c. Citanest. d. Vivacaine. Question 73 It is considered as the safest of all local anesthetics. a. Xylonibsa. b. Citanest. c. Septocaine. d. Marcaine. Question 74 All are true about use of Benzocaine, except: a. Poor sustainability in water b. Poor absorption into the cardiovascular system c. Not suitable for injection d. Inhibits the antibacterial action of amoxycillin Question 71 Question 76 The absolute maximum dose of Lidocaine in healthy patient is Epinephrine is a. 200 mg. b. 400 mg. c. 500 mg. a. an alcohol derivative. b. a pyrocatechin derivative. c. a phenol derivative. d. a benzoyl derivative. d. 600 mg. Question 77 Question 72 The absolute maximum dose of Prilocaine in healthy patient is a. 200 mg. b. 400 mg. c. 500 mg. d. 600 mg. In inferior alveolar nerve block, the needle should not penetrate more than a. 1/2 inch. b. 1/8 inch. c. 3/4 inch. d. 2 inches. Question 79 The dissociation constant of Lidocaine HCI is This injection technique secures regional anesthesia by depositing a suitable amount of anesthetic solution within close proximity to a main nerve trunk. a. 7.7. a. Paraperiosteal injection. b. 7.9. b. Field block. c. 8. c. Nerve block. d. 8.1. d. Supraperiosteal injection. Question 80 Question 83 Deep injections are avoided if the patient is The nerves anesthetized in the infraorbital nerve block are the following, except a. anemic. a. ASA nerve. b. under ASA therapy. b. MSA nerve. c. under anti-coagulant therapy. c. PSA nerve. d. under antibiotic therapy. d. Superior labial nerve. Question 81 Question 84 Five minutes after inferior alveolar nerve block is administered, the patient develops paralysis of skin of the forehead, eyelid and upper lip on the same side of the face. This may be the result of a. diffusion of the anesthetic solution into the V1. b. injection of anesthetic solution into the capsule of the parotid gland and consequent blockade of CN VII. c. anesthesia to the motor branches of the mandibular nerve supplying the muscles of mastication. d. anesthesia to the otic region. Patient with very limited mouth opening can receive all of the following injection techniques, except a. Vazirani-Akinosi Technique. b. Gow-Gates Technique. c. Long buccal nerve block. d. Paraperiostial injection. Question 85 Hydrolysis of Procaine HCI occurs mainly in the a. Liver. Question 82 b. Lungs. c. Kidney. d. Blood. b. Mepivacaine HCI. c. Articaine HCI. Question 86 The direct-acting adrenergic amines exert their actions directly on adrenergic receptors and include the following, except a. Norepinephrine. b. Adrenaline. c. Dopamine. d. Amphetamine. d. none of the above.. Question 90 In adults patients, about block, should be deposited during nasopalatine nerve a. 1 ml. b. .45 ml. c. 1.4 ml. d. 1.8 ml. Question 87 Parasympathomimetic drugs produce which of the following? a. Vasodilation. b. Vasoconstriction. c. Dry skin. d. cardiac stimulation. Question 88 Question 91 The closed-mouth approach to the inferior alveolar nerve is known as the a. Gow-Gates technique. b. Halsted technique.. c. Akinosi technique. d. Traditional technique. Which one of the following is classified as short duration local anesthetics? a. 2% Mepivacaine HCI with 1:20,000 Levonordefrin. b. 2% Lidocaine HCI with 1:100,000 Epinephrine. Question 92 Commercially injectable local anesthetics are usually a. acidic. c. 4% Prilocaine HCI. b. basic. d. All of the above. c. hypertonic. d. hypotonic. Question 89 In large doses, this anesthetic solution should be avoided in patients suffering from idiopathic methemoglobinemia. a. LidocaineHCI. Question 93 Which of the following exhibits weakest effectivity as a topical anesthetic? a. Lidocaine. b. Tetracaine. Question 97 c. Benzocaine. Vasoconstrictors not having hydroxyl groups in the 3rd and 4th position of the aromatic molecule are d. Mepivacaine. a. catechols. Question 94 b. not catechols. Long duration local anesthetics usually last for c. not amines.. a. 45 75 minutes. d. benzoic acid derivatives. b. 120 minutes. c. 180 minutes or more. Question 98 d. 90 minutes. This vasoconstrictor is not recommended in dentistry because it may cause tissue damage. Question 95 a. Epinephrine. If anesthesia of the mandibular incisors only is required, it is possible to use which of the following injection techniques b. Noradrenaline.. c. Dopamine. d. Felypressin. a. mental nerve block. b. inferior alveolar nerve block. Question 99 c. incisive nerve block. d. labial and lingual paraperiosteal injections. The only local anesthetic with thiophene attached to the aromatic ring is a. Lidocaine. b. Mepivacaine Question 96 Catecholamines have characteristics, except the c. Articaine. following d. Prilocaine. a. they are parasympathomemitic drugs. b. they have hydroxyl substitutions in the 3rd and 4th positions of the aromatic ring. c. they also contain an amine group (NH2) attached to the alipathic chain. d. none of the above.. Question 100 In administering PSAN block, long needle should be avoided to prevent: a. b. c. d. Needle breakage Hematoma Paralysis of the nerve All of the above


