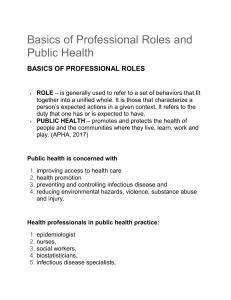
Basics of Professional Roles and Public Health BASICS OF PROFESSIONAL ROLES ROLE – is generally used to refer to a set of behaviors that fit together into a unified whole. It is those that characterize a person’s expected actions in a given context. It refers to the duty that one has or is expected to have. PUBLIC HEALTH – promotes and protects the health of people and the communities where they live, learn, work and play. (APHA, 2017) Public health is concerned with 1. improving access to health care 2. health promotion 3. preventing and controlling infectious disease and 4. reducing environmental hazards, violence, substance abuse and injury. Health professionals in public health practice: 1. epidemiologist 2. nurses, 3. social workers, 4. biostatisticians, 5. infectious disease specialists, 6. physicians, 7. health educators, and 8. field workers Characteristic of Collaboration CHARACTERISTICS OF COLLABORATION Inter professional collaboration begins with mutual respect, clear communication, and a focus on patient as the center of care. These characteristics are necessary to the development of shared goals and shared decision making. The end result is collaboration PROFESSION A profession is defined as a calling requiring specialized knowledge and long and intensive academic preparation (Merriam-Webster, 2015) EDUCATION Education is extended, is standardized and takes place in institutions of higher learning. UNIQUE BODY OF KNOWLEDGE It is specific to the professional discipline and serves as the basis for the practice of the profession (Birden et. Eal, 2014) SERVICE A specific need of society is served by the profession. Professions are characterized by their service. There is a sense of calling to the discipline, a sense of mission and a responsibility to the public. AUTONOMY Autonomy is defined as the quality or state of being selfgoverning. Self-governing or self-regulation, means that it is only members of the profession themselves who decided what is required educationally and legally to become and remain a practitioner of that profession. CODE OF ETHICS Code of ethics is a written document encompassing the set of rules based on values and standards of conduct to which practitioners of a profession are expected to conform. A code of ethics acts as a framework for decision making and is an example of a standard for practice. SCOPE OF PRACTICE Scope of practice denotes those activities that members of a specific profession are legally allowed to do as a result of their education. Special interest in understanding Interprofessional Collaboration Practice 1. Collaboration between healthcare providers should be the professional norm. 2. No single profession owns a specific skill or activity. 3. No professional has enough skills or knowledge to perform all aspects of the profession’s scope of practice. PROFESSIONAL IDENTITY DEVELOPMENT Part of the professionalization process is the development of your own professional identity. Professional identity is defined as one’s professional selfconcept based on attributes, beliefs, values, motives, and experiences. Professional identity development is a lifelong process. Self-reflection as a Learning Tool SELF REFLECTION AS A LEARNING TOOL Self-reflection can be defined as the ability to engage in introspection with the willingness to learn something about oneself in the process and the desire to grow and change. Components of Self-reflection 1. Examination of our own feelings and thoughts 2. Willingness to learn something from engaging in introspection. Skills Needed for self-reflection 1. Awareness – being conscious of oneself, including beliefs, values, qualities, strengths, and limitations. (Enuku & Evawoma-Enuku, 2015) 2. Description – refers to the ability to state the characteristics of something in a non-judgmental manner. (Enuku & Evawoma-Enuku, 2015) 3. Critical analysis – is the ability to examine the components, internal structure, and interactions of a whole to understand it. (Enuku & Evawoma-Enuku, 2015) 4. Synthesis – is the ability to form a single coherent idea out of several different elements. (Enuku & Evawoma-Enuku, 2015) 5. Evaluation – is the ability to pass judgment over something using a set of criteria or standards. (Enuku & EvawomaEnuku, 2015) 6. Action intervention – is the ability to decide whether and how to take action, once a new perspective has been developed through self-reflection (Sherwood & Horton-Deutsch, 2012) Roles and Responsibilities in the Context of Teamwork ROLES AND RESPONSIBILITIES IN THE CONTEXT OF TEAMWORK What is a Healthcare team? Group can be defined as two or more individuals who are connected to one another by social; relationships. Interprofessional Collaborative Healthcare Team is defined as a team that engages in cooperation, coordination, and collaboration that is characterized by the relationships between the professionals involved in the delivery of patientcentered care. Clarify roles in Healthcare teams All team members must be able to explain team roles and responsibilities, for themselves and for other team members, as a precursor to clarifying how the team members, as a precursor to clarifying how the team will work together in a specific. TIPS FOR BETTER TEAMWORK - Team understands the goals and is committed to attaining them. - Creativity, innovation, and different viewpoints are expected - Communication is open, honest, and respectful. - People are comfortable taking reasonable risk - Members of the team make high quality decisions together The Competency of Roles and Responsibilities Competencies of Roles and Responsibilities Knowing the roles and responsibilities of a member of the health care team is important to clearly identify the tasks with a professionals scope of practice for which a professional will be responsible in a given care situation and further, to identify those that may overlap with those of one or more other healthcare professionals in a given care situation. For true collaboration to take place, each professional who is a member of the health care team must be part of the planning. They must plan together with other professionals, with patients and families, with nonprofessional organizations and volunteers, within and between organizations, and within communities to clearly identify who will be responsible for certain roles (IPEC, 2011). Use the knowledge of one's own role and those of other professions to appropriately assess and address the healthcare needs of patients and to promote and advance the health of the population served (IPEC, 2016). The Sub-competencies of Roles/Responsibilities for Interprofessional Practice Specific Sub-competencies of Roles/Responsibilities (RR) for Interprofessional Practice: RR1. Communicate one's roles and responsibilities clearly to patients, families, community members, and other professionals. - Informing – mutual understanding - Obtain conformation - Asking the team members or agreement - Clarification RR2. Recognize one's limitations in skills, knowledge, and abilities. - Self reflection related to your roles and responsibility - Self awareness - Consultation - Seek consultation to an expert RR3. Engage diverse professionals who complement one's own professional expertise, as well as associated resources, to develop strategies to meet specific health and healthcare needs of patients and populations. - Need to fully involve / engage collaboration - Ongoing Communication – collective expertise - Goal / objectives – ex: - To avoid misunderstanding - synchronous – communicate at the same time- meetings, phone consultation, endorsement, rounds - Asynchronous, electronic/ email, text mess, written / post it - Planning RR4. Explain the roles and responsibilities of other providers and how the team works together to provide care, promote health, and prevent disease. - Ability to explain the roles and responsibilities - Communicating others health professionals role and responsibilities - Not operate based Stereotypes – can contribute erroneous ideas about profession – can lead to devaluating RR5. Use the full scope of knowledge, skills, and abilities of professionals from health and other fields to provide care that is safe, timely, efficient, effective, and equitable. - Ex; daily exercise – physical therapy RR6. Communicate with team members to clarify each member's responsibility in executing components of a treatment plan or public health intervention. - Involves respect of the role and contribution of each member - Inefficient distribution of work RR7. Forge interdependent relationships with other professions within and outside of the health system to improve care and advance learning. - Dependence on the expertise - Shared language - Trust - Interdependence - Rr3, 5, 9, 7 are almost the same - The more people and you will learn, respect and trust RR8. Engage in continuous professional and interprofessional development to enhance team performance and collaboration. - Lifelong learning individual Ex; certification – or immunizing certification Educational activity like seminar / webinars Read journals / news / training/ conferences Responsible to maintain and improve our skills and knowledge - Evidence based practice RR9. Use unique and complementary abilities of all members of the team to optimize health and patient care. - Implement RR10. Describe how professionals in health and other fields can collaborate and integrate clinical care and public health interventions to optimize population health. - Optimize population - Population health - Ex: aware of the community - Aware the public needs / health within the place you serve - Encourage – community outreach programs - Medical missions - Testing and screening – to know whether the person need to isolate - Immunization/ vaccination Continuum of Interprofessional Education (IPE) Continuum of Interprofessional Education (IPE) An enhanced professional education model capturing essential concepts of interprofessional education NOTE: CE = continuing education; CIPE = continuing interprofessional education; IPE = interprofessional education. SOURCE: Owen and Schmitt, 2013 (Links to an external site.). © 2013 The Alliance for Continuing Education in the Health Professions, the Society for Academic Continuing Medical Education, and the Council on Continuing Medical Education, Association for Hospital Medical Education. Published online in Wiley Online Library (wileyonlinelibrary.com (Links to an external site.)). doi: 10.1002/chp.21173. This model builds on earlier thinking about a patient-centered approach to learning in the health professions and describes the intersections of IPE with basic education, graduate education, and continuing IPE; it also captures the understanding that point-of-care learning is a key component of lifelong learning (Josiah Macy Jr. Foundation, 2010). This broad definition of continuing education encompasses all learning (formal, informal, workplace, serendipitous) that enhances understanding and improves patient care (IOM, 2010; Nisbet et al., 2013). All of these elements are important in linking IPE to individual, population, and system outcomes. NOTE: For this model, “graduate education” encompasses any advanced formal or supervised health professions training taking place between completion of foundational education and entry into unsupervised practice. The interprofessional learning continuum (IPLC) model encompasses four interrelated components: a learning continuum; the outcomes of learning; individual and population health outcomes; system outcomes such as organizational changes, system efficiencies, and cost-effectiveness; and the major enabling and interfering factors that influence implementation and overall outcomes. It must be emphasized that successful application of this model is dependent on how well the interdependent education and health care systems, as described in the previous chapter, are aligned.