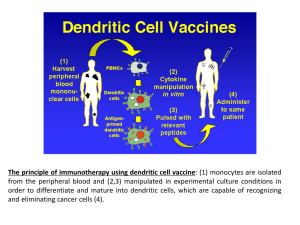
Pharm Sci 310: Cancer Treatment The goals of this lecture are to familiarize students with some basics of tumor formation, treatments for cancer, and the side effects of cancer treatment. Reading (you are only responsible for the parts of these that we specifically discuss in class). These are all written for a lay audience. http://www.cancer.org/treatment/treatmentsandsideeffects/treatmenttypes/chemotherapy/whatitish owithelps/index.htm http://www.cancer.org/Treatment/TreatmentsandSideEffects/TreatmentTypes/Chemotherapy/Che motherapyPrinciplesAnIn-depthDiscussionoftheTechniquesanditsRoleinTreatment/index Drugs to know Paclitaxel (Taxol) and nab-paclitaxel (Abraxane) Imatinib (Gleevec) Nivolumab (Opdivo) (and diagnostic test PD-L1 IHC 28-8 pharmDx) Some hints on drugs: chemicals that target kinases usually end in "nib" Monoclonal antibodies usually end in "mab" Lecture slides are attached. Introduction Cancer Treatments Overview Cytotoxic (cell killing agents) Targeted therapies Targeting the tumor microenvironment Progress/future of cancer therapy SOME DEFINITIONS Tumor- abnormal mass of cells resulting from defects in normal control of cell survival, proliferation and differentiation Benign tumor: does not invade the surrounding tissues or spread to other parts of the body. But can they cause health issues? Malignant tumor (=cancer): can invade surrounding tissue and spread to other parts of the body (metastasize), will get worse Often named after where they arise What is technical definition of chemotherapy? EARLIEST CANCER THERAPIES Edwin Smith Papyrus- about 3000 BC describes tumors/ulcers of breast removed by cauterization but “There is no treatment”. Celsus (Roman physician 28-50 B.C.) "After excision, even when a scar has formed, none the less the disease has returned.” Galen (2nd century Greek doctor) did write that some breast tumors could be cured by excision if caught early enough mid-1800s anesthesia allowed more surgeries Late 1800s Thomas Beatson tested oophorectomy for breast cancer (hormone ablation) A VERY BRIEF HISTORY OF CANCER THERAPY 1900- radiation Around 1950- cytotoxic chemotherapies nitrogen mustard and methotrexate 1990s- “targeted therapies” monoclonal antibodies to target tumors 2000s- “targeted therapies” kinase inhibitors, anti-angiogenesis agents 2010- prostate cancer cellular immunotherapy 2010s- “checkpoint inhibitors” as immune modulators 2017- genetically modified T cells (CAR-T) 1) 2) 3) 4) 5) 6) 7) CANCER TREATMENTS Surgery Radiation Chemotherapy “Targeted” therapies Immunotherapies Hormonal therapies Hyperthermia (heat) REGIMENS - Name of drug(s) Dose How often How long How given Introduction Cancer Treatments Overview Cytotoxic (cell killing agents) Targeted therapies Targeting the tumor microenvironment Progress/future of cancer therapy CANCER CHEMOTHERAPY - Usually refers to cytotoxic (= cell killing agents) - Generally target rapidly dividing cells - Usually small molecules MICROTUBULES -Important part of cellular structure (cytoskeleton) NIH -Also act as “tracks” for transport of materials within cell MICROTUBULES- CONTINUED http://dms.dartmouth.edu/compton/photos/photos/html/Mitotic_spindle.html - Part of the mitotic spindle - Made of polymerized tubulin subunits - Dynamic structures Skop lab MICROTUBULE (SPINDLE) POISONS Example: Paclitaxel (Taxol) Originally discovered as natural product isolated from bark of yew tree What is its mechanism of action? PACLITAXEL (TAXOL) Originally thought to induce a “mitotic arrest” by “poisoning” mitotic spindle At clinical doses, now thought to cause abnormal chromosome segregation http://stm.sciencemag.org/content/6/229/229ra43/F1.expansion.html PACLITAXEL (TAXOL) - Variety of solid tumors - Some common acute side effects- nausea, vomiting, hypotension, hypersensitivity - Delayed toxicities: neuropathy, myelosuppression - Nanoparticle formulation nab-paclitaxel (Abraxane) may reduce some toxicities , PACLITAXEL (TAXOL) - Resistance: increased expression of proteins that pump drug out of cell; expression (increased or mutant) of proteins that promote mitosis or block cell death; changes in tubulin , Which of the following statements is CORRECT? • A) Nab-paclitaxel generally causes more toxicities than paclitaxel • B) Paclitaxel is thought to destabilize microtubules and therefore block microtubule polymerization • C) One mechanism of paclitaxel resistance is that cancer cells increase expression of proteins that pump the drug out • D) Paclitaxel would be an example of a targeted cancer therapy OTHER SIDE EFFECTS CYTOTOXIC AGENTS CAN CAUSE - GI Effects (Nausea, vomiting, diarrhea or constipation) - Alopecia - Changes in the taste of food - Neuropathies - Bone marrow (myelosuppression) - Impact fertility - Secondary malignancies - Some are vesicants - Hand-foot syndrome - ”Chemo brain” Introduction Cancer Treatments Overview Cytotoxic (cell killing agents) Targeted therapies Targeting the tumor microenvironment Progress/future of cancer therapy TARGETED THERAPIES - Goal- attack tumor cells while sparing normal cells - Target molecular pathways involved in cancer cell survival/progression TARGETED THERAPIES: KINASE INHIBITORS Target enzymes that are different in cancer cells than other cells Kinases are frequent “drugable targets” What do kinases do? Some kinases have abnormal activity in cancer (over-expression, mutation, other mechanisms) EXAMPLE: CML Chronic myeloid leukemia (CML) frequently harbors a specific chromosomal abnormality called a translocation (the specific translocation found in most CML cells is called the Philadelphia chromosome) - Philadelphia chromosome can be present in ALL RESULT OF TRANSLOCATION: BCR-ABL fusion The result of the Philadelphia chromosome: fusion "oncoprotein" called BCR-ABL that harbors constitutively active ABL kinase activity Druker, B. J. Blood 2008;112:48084817 RATIONAL THERAPY: IMATINIB (GLEEVEC) Ciba-Geigy (now Novartis) were testing small molecule kinase inhibitors (including trying to find ones that would target ABL) Brian Druker had cell culture models for CML Tested the compounds to find one that seemed to be selective for killing CML cells Result: Imatinib (Gleevec) RATIONAL THERAPY: IMATINIB (GLEEVEC) Estimated CML 5 year survival now 95% Imatinib also inhibits other kinases important in other tumors - In addition to CML and ALL used to treat other cancers/conditions driven by cKIT, PDGFRA IMATINIB (GLEEVEC): ISSUES -Side Effects: Fluid retention, muscle cramps, others -Resistance: Common cause is due to point mutations in BCR-ABL - Drugs have been developed to inhibit Imatinib-resistant BCR-ABL Introduction Cancer Treatments Overview Cytotoxic (cell killing agents) Targeted therapies Targeting the tumor microenvironment Progress/future of cancer therapy Nivolumab (OPDIVO) “checkpoint” DAKO.Agilent Nivolumab= anti-PD1 antibody Nivolumab (OPDIVO) - Side effects include rash and fatigue - Can also more rarely see severe immune-related adverse events (irAEs) - Thought to be caused by general immunologic enhancement Nivolumab (OPDIVO) - Can be used in therapy for a variety of solid tumors - Sometimes in combination with an inhibitor of another “checkpoint”, a kinase inhibitor, or traditional chemotherapy - Not all patients respond- Why? - One hypothesis is that higher mutational load = better response - For some tumor types, FDA requires screening tumor for PD-L1 expression (biomarker for response) Nivolumab (OPDIVO) PD-L1 IHC 28-8 pharmDx DAKO.Agilent Introduction Cancer Treatments Overview Cytotoxic (cell killing agents) Targeted therapies Targeting the tumor microenvironment Progress/future of cancer therapy • How have cancer rates and survival rates changed over time? LIFETIME RISKS IN US Developing invasive cancer: 39.5% 2nd leading cause of death 2020: estimated 1.8 million new cases of cancer will be diagnosed Cancer statistics, 2022 CA A Cancer J Clinicians, Volume: 72, Issue: 1, Pages: 7-33, First published: 12 January 2022, DOI: (10.3322/caac.21708) Cancer statistics, 2022 CA A Cancer J Clinicians, Volume: 72, Issue: 1, Pages: 7-33, First published: 12 January 2022, DOI: (10.3322/caac.21708) Cancer statistics, 2022 CA A Cancer J Clinicians, Volume: 72, Issue: 1, Pages: 7-33, First published: 12 January 2022, DOI: (10.3322/caac.21708) Cancer statistics, 2022 CA A Cancer J Clinicians, Volume: 72, Issue: 1, Pages: 7-33, First published: 12 January 2022, DOI: (10.3322/caac.21708) The future? More personalized medicine Better vaccines/immunotherapy Better uses/modifications of existing drugs Circumventing resistance New drug targets Detection/prevention Better drug delivery Lifestyle changes True or false • Cancer mortality rates per 100,000 people have been increasing in the past 30 years SUMMARY Definitions (benign, malignant, metastatic, chemotherapy, etc.) History of cancer treatment Cancer treatments Chemotherapy Targeted therapy Immunotherapy War on Cancer: detection, prevention or treatment? The future