Pulmonary Function Testing: Spirometry & Interpretation
advertisement
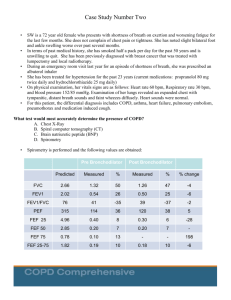
Pulmonary Function Robert C. Strunk, MD Strominger Professor of Pediatrics Washington University School of Medicine St. Louis Children’s Hospital Division of Allergy, Immunology, and Pulmonary Medicine Disclosures Employment Research Interests NHLBI Financial Interests Washington University School of Medicine None Chair, Pediatric Adjudication Committee, GSK study of safety and benefit of FP/salmeterol vs. FP Spirometry For now, spirometry is best test to: • Monitor asthma status • Look for evidence of asthma • Look for evidence of other diagnoses Volume-Time Plot Forced Vital Capacity Maneuver Airflow, L/sec Lung volume Definitions FVC – Forced Vital Capacity Volume of air exhaled after a maximal inspiration to total lung capacity. This volume is expressed in Liters FEV1 – Forced Expiratory Volume in 1 second Volume of air exhaled in the first second of expiration. This volume is expressed in Liters FEF 25-75% Mean expiratory flow during the middle half of the FVC maneuver; reflects flow through later emptying airways, not necessarily the small airways FEV1/FVC – Ratio (%) Volume of air expired in the first second, expressed as a percent of FVC Performance of FVC maneuver Patient assumes the position (typically standing) • Puts nose clip on • Inhales maximally • Puts mouthpiece in mouth and closes lips around mouthpiece (open circuit) • Exhales as hard and fast and long as possible • Repeat instructions if necessary – effective coaching is essential • Give simple instructions • Repeat minimum of three times (check for repeatability) Special Considerations in Pediatric Patients Ability to perform spirometry dependent on developmental age of child, personality, and interest. Patients need a calm, relaxed environment and good coaching. Patience is key. Be creative Use incentives Even with the best of environments and coaching, a child may not be able to perform spirometry. ATS Acceptable Criteria Within Maneuver Free from artifacts, such as • • • • • • Cough during the first second of exhalation Glottis closure that influences the measurement Early termination or cut-off Effort that is not maximal throughout Leak Obstructed mouthpiece Good starts • Extrapolated volume < 5% of FVC or 0.15 L, whichever is greater Satisfactory exhalation • Duration of ≥ 6 s (3 s for children < 10) or a plateau in the volume– time curve or • If the subject cannot or should not continue to exhale ATS Acceptable Criteria Within Maneuver After three acceptable spirograms have been obtained, apply the following tests • The two largest values of FVC must be within 0.150 L of each other • The two largest values of FEV1 must be within 0.150 L of each other If both of these criteria are met, the test session may be concluded If both of these criteria are not met, continue testing until • Both of the criteria are met with analysis of additional acceptable spirograms or • A total of eight tests have been performed (optional) or • The patient/subject cannot or should not continue Save, as a minimum, the three satisfactory maneuvers Spirometry Interpretation: So what constitutes normal? Normal values vary and depend on: • • • • Height Age Gender Ethnicity Spirometry Interpretation: Obstructive vs. Restrictive Defect Obstructive Disorders • Characterized by a limitation of expiratory airflow so that airways cannot empty as rapidly compared to normal (such as through narrowed airways from bronchospasm, inflammation, etc.) Examples: • Asthma • Emphysema • Cystic Fibrosis Restrictive Disorders • Characterized by reduced lung volumes/decreased lung compliance Examples: • Interstitial Fibrosis • Scoliosis • Obesity • Lung Resection • Neuromuscular diseases • Cystic Fibrosis Spirometry Interpretation: Obstructive vs. Restrictive Defect Obstructive Disorders • • • • • FVC nl or↓ FEV1 ↓ FEF25-75% ↓ FEV1/FVC ↓ TLC nl or ↑ Restrictive Disorders • • • • • FVC ↓ FEV1 ↓ FEF 25-75% nl to ↓ FEV1/FVC nl to ↑ TLC ↓ Severity of any spirometric abnormalities based on the FEV1 Degree of severity FEV1 % predicted Mild >70 Moderate 60-69 Mod severe 50-59 Severe 35-49 Very Severe < 35 based on ATS/ERS criteria Criteria Used at Washington University PFT Lab FEV1 Normal (82-118% predicted) FVC Normal (82-118% predicted) TLC < 80 % predicted for restriction RV/TLC above 30% for air trapping Degree of severity Mild Moderate Severe FEV1 % predicted > 70 50-70 < 50 When you see the tracings below, which of these prompts should you give the participant Take in a deeper breath Blow out harder and faster Try not to cough Blow out longer Good Test The flow volume loop below is representative of Extrapolation or time zero error Clipped inspiratory loop Obstructive pattern Restrictive pattern Glottic closure When you see the tracings below, which of these prompts should you give the participant Blow out longer Good Test Take in a deeper breath Try not to cough Blow out harder and faster When you see the tracings below, which of these prompts should you give the participant Take in a deeper breath Blow out harder and faster Try not to cough Blow out longer Good Test The flow volume loop below is representative of Extrapolation or time zero error Clipped inspiratory loop Obstructive pattern Restrictive pattern Glottic closure Back Extrapolation Exhalation Time During Obstruction Spirometry-Induced Bronchospasm Coaching is Key Bronchodilator Response Obstruction Restrictive Pattern Patient example Child with inspiratory stridor - Vocal Cord Dysfunction Patient example 12 year old boy presents with exerciseinduced wheeze for 1 year Not responsive to bronchodilator used preexercise, ICS, OCS Fixed airway obstruction Obstruction due to abnormalities of the vocal cords after trauma of intubation and prolonged intubation Additional history Automobile accident at age 11 years Intubated at scene of accident Comatose for 1 month, followed by complete neurologic recovery FEF 25-75% What is it? What does it measure? Is it a measure of small airways? FEF 25-75% What is it? • Mean expiratory flow during middle half of FVC maneuver What does it measure? • Flow from airways that empty in the middle half of FVC maneuver Is it a measure of small airways? • Maybe in normals • In asthma, or obstructive disease, it measures flow from more obstructed airways which could be small or larger with more obstruction A problem with FEF: Variability Dysanapsis Green, Mead, Turner. Variability of maximum expiratory flow-volume curves. J Appl Physiol 1974 37:67-74 • Variability in flows among healthy adults not altered when flows were corrected for vital capacity • Lung static recoil and bronchomotor tone contributed little to variability Concluded that variability in flows between individuals due to differences in airway size independent of lung/parenchyma size Differences may have embryological basis, reflecting disproportionate but physiologically normal growth within an organ Dysanapsis Mead. Dysanapsis in normal lungs assessed by the relationship between maximal flow, static recoil, and vital capacity. Am Rev Respir Dis 1980 121:339-342 • “There is no association whatsoever between airway diameter and lung size.” • There are differences between men and women (men 17% larger than women) and between boys and men (boys in late teens similar to girls, suggesting that growth in males occurs late) Measures Of Dysanapsis Mead used maximal expiratory flow/static recoil pressure at 50% VC Weiss and coworkers have used FEF25-75/FVC as a surrogate FEF25-75/FVC is correlated with FEV-1/FVC FEV-1/FVC is the best measure: obtained from spirometry and normal values available Dysanapsis Is Affected By Asthma Weiss et al. Effects of asthma on pulmonary function in children. A longitudinal population-based study. Am Rev Respir Dis 1992 145:58-64. • East Boston cohort of 5-9 year old school children followed prospectively until age 13 years • Active asthma • Yes to “Has a doctor ever told you that your child has asthma.” • Wheezing symptoms present in that study year • Boys with asthma had significantly larger FVC, but normal FEV-1 • Girls with asthma had significantly lower FEV-1, but normal FVC Compared to children with no history of asthma, after adjusting for previous level of pulmonary function, age, height, and personal and maternal smoking Clinical Correlates Of Asthma Related To Dysanapsis Studies of East Boston cohort of school children by Weiss and colleagues Degree of response to eucapneic hyperventilation: • Correlated with FEF25-75/FVC, but not FEF25-75 • Correlated with FVC (higher levels associated with increased response) In both studies, response also correlated with current asthma and report of a respiratory illness that led to activity restriction Case History of dysanapsis Pulmonary function results at age 7 • FVC 157% predicted • FEV-1 115% predicted Case History Pulmonary function results at age 7 • FVC 157% predicted (82-120%) • FEV-1 115% predicted (82-120%) Case History Pulmonary function results at age 7 • FVC 157% predicted (82-120%) • FEV-1 115% predicted (82-120%) • FEV-1/FVC = 65% (> 80%) Case History Pulmonary function results at age 7 • FVC 157% predicted • FEV-1 115% predicted • FEV-1/FVC = 65% Results obtained 1 month after severe exacerbation requiring intubation and ventilation 1st admission occurred at age 21 months Intubation admission was #28, with first documented hypercarbia with exac at age 4 years Spirometry History Age FVC % pred FEV-1 % pred FEV-1/FVC 6 7 8 9 10 11 12 13 14 143 157 149 159 127 147 119 100 78 126 115 119 129 95 96 91 77 57 79 65 72 73 66 58 67 71 68 Conclusions Spirometry is: • Useful in asthma diagnosis and management • Useful in diagnosis of conditions that can present with wheezing, or airway noise that can be hard to distinguish from wheezing • Requires considerable expertise, particularly in children FEF25-75% does not measure small airways, but instead airways more obstructed that empty later in exhalation