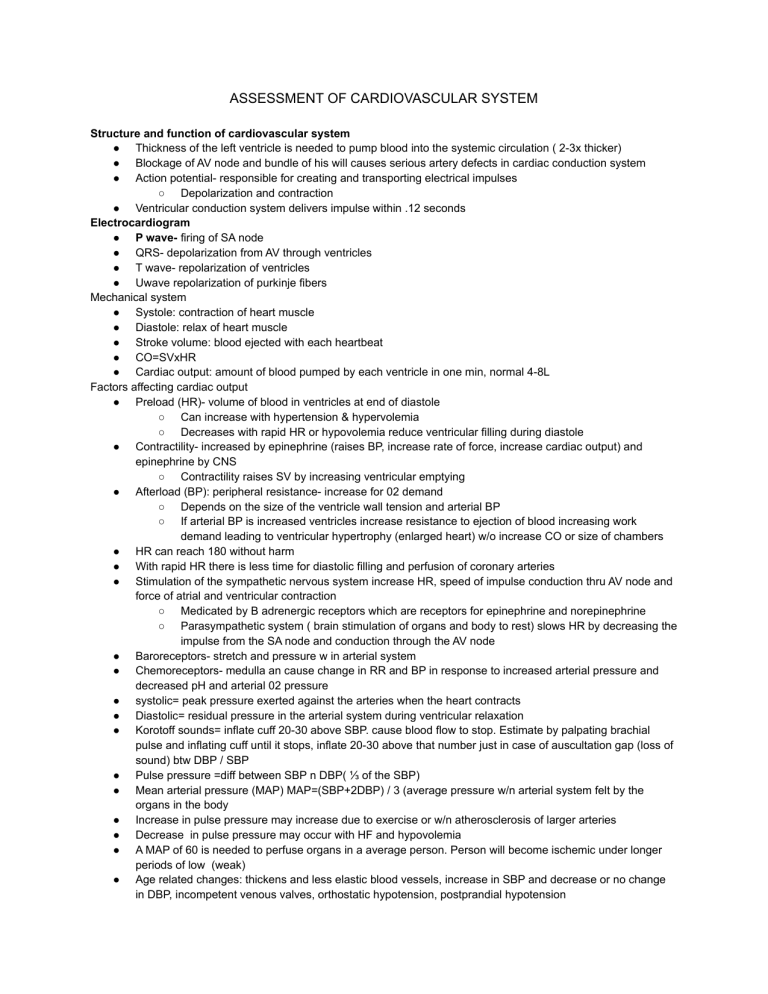
ASSESSMENT OF CARDIOVASCULAR SYSTEM Structure and function of cardiovascular system ● Thickness of the left ventricle is needed to pump blood into the systemic circulation ( 2-3x thicker) ● Blockage of AV node and bundle of his will causes serious artery defects in cardiac conduction system ● Action potential- responsible for creating and transporting electrical impulses ○ Depolarization and contraction ● Ventricular conduction system delivers impulse within .12 seconds Electrocardiogram ● P wave- firing of SA node ● QRS- depolarization from AV through ventricles ● T wave- repolarization of ventricles ● Uwave repolarization of purkinje fibers Mechanical system ● Systole: contraction of heart muscle ● Diastole: relax of heart muscle ● Stroke volume: blood ejected with each heartbeat ● CO=SVxHR ● Cardiac output: amount of blood pumped by each ventricle in one min, normal 4-8L Factors affecting cardiac output ● Preload (HR)- volume of blood in ventricles at end of diastole ○ Can increase with hypertension & hypervolemia ○ Decreases with rapid HR or hypovolemia reduce ventricular filling during diastole ● Contractility- increased by epinephrine (raises BP, increase rate of force, increase cardiac output) and epinephrine by CNS ○ Contractility raises SV by increasing ventricular emptying ● Afterload (BP): peripheral resistance- increase for 02 demand ○ Depends on the size of the ventricle wall tension and arterial BP ○ If arterial BP is increased ventricles increase resistance to ejection of blood increasing work demand leading to ventricular hypertrophy (enlarged heart) w/o increase CO or size of chambers ● HR can reach 180 without harm ● With rapid HR there is less time for diastolic filling and perfusion of coronary arteries ● Stimulation of the sympathetic nervous system increase HR, speed of impulse conduction thru AV node and force of atrial and ventricular contraction ○ Medicated by B adrenergic receptors which are receptors for epinephrine and norepinephrine ○ Parasympathetic system ( brain stimulation of organs and body to rest) slows HR by decreasing the impulse from the SA node and conduction through the AV node ● Baroreceptors- stretch and pressure w in arterial system ● Chemoreceptors- medulla an cause change in RR and BP in response to increased arterial pressure and decreased pH and arterial 02 pressure ● systolic= peak pressure exerted against the arteries when the heart contracts ● Diastolic= residual pressure in the arterial system during ventricular relaxation ● Korotoff sounds= inflate cuff 20-30 above SBP. cause blood flow to stop. Estimate by palpating brachial pulse and inflating cuff until it stops, inflate 20-30 above that number just in case of auscultation gap (loss of sound) btw DBP / SBP ● Pulse pressure =diff between SBP n DBP( ⅓ of the SBP) ● Mean arterial pressure (MAP) MAP=(SBP+2DBP) / 3 (average pressure w/n arterial system felt by the organs in the body ● Increase in pulse pressure may increase due to exercise or w/n atherosclerosis of larger arteries ● Decrease in pulse pressure may occur with HF and hypovolemia ● A MAP of 60 is needed to perfuse organs in a average person. Person will become ischemic under longer periods of low (weak) ● Age related changes: thickens and less elastic blood vessels, increase in SBP and decrease or no change in DBP, incompetent venous valves, orthostatic hypotension, postprandial hypotension ● ● ● ● ● ● ● Assessment of cardiovascular system: health info, history of present illness, past health history, past and current meds, surgery or other treatments, functional health patterns, perception of health, nutrition, elimination, activity/exercise, sleep rest pattern, cognitive percept pattern, self perception, role relationships, sexuality, coping, values CAD = lipoprotein gene links, Cardiomyopathy= autosomal and x linked dominant mutations, hypertension= genetic, environmental and lifestyle factors Objective data= physical exam, vitals, peripheral vascular inspection, palpitation, auscultation Common sites for palpating arteries: carotid, brachial, popliteal, posterior tibial, dorsalis pedis, femoral, ulnar, radial Anatomic landmarks: Aortic, Pulmonic, Erb's point, tricuspid, mitral (apical) Pericardial friction rubs: pericarditis, inflamed surfaces of the pericardium move against each other ○ High pitched scratchy sounds, may be intermittent and ast days to hours Cardiac Biomarkers ○ Troponin T (cTnT) <0.1ng/ml ( test for cardiac injury/ischemia) draw 3 sets of troponin 3-6 hrs apart ○ Troponin I (cTnI) neg:<0.03ng/ml ■ Rises w/in 4-6 hrs peaks 10-24 hrs, detected up to 10-14 days ○ Creatine kinase (CK) ■ Three isoenzymes ■ CK-MB cardiac specific ■ Rises in 3-6 hours peaks 12-24 hrs, returns to baseline within 12-48 hrs ○ Copeptin <10pmol vasopressin concentrations, high levels indicate MI, higher in men with stress and exercise. Influenced by fasting and water load ○ Myoglobin- crushing injuries, electric injuries, extreme exertion if high levels (no number) ○ Additional blood studies ■ C reactive protein (CRP) marker for inflammation, atherosclerosis (hard narrow arteries due to build up of plaque) ● Low < 1mg ● Moderate 1-3mg ● High >3 ○ Homocysteine- elevated increased risk for CVAD peripheral vascular disease and stroke (b12 deficits) ■ 4-14mol/l ○ Cardiac natriuretic peptide markers ■ Atrial, bType <100, Ctype ■ Increased levels of BNP signify heart failure ■ Nt pro BNP ○ Serum lipids ■ Triglycerides- fatty acids- elevation indicate cardiovascular disease and diabetes ● Males 40-160 mg/dl ● Female 35-135 mg/dl ○ Avoid alcohol 24 hrs before testing, fasting or nonfasting state ● Cholesterol- blood lipid ass with arteriosclerosis. High levels of risk for cardiovascular disease. Can obtain in a non fasting or fasting state. ○ <200 mg/dl ● Phospholipids ○ Lipoprotein- lipids must bind to protein to circulate in blood ■ 4 classes ● Chylomicrons ● Low density lipoprotein <130mg/dl (LDL) ○ Moderate risk for CAD 130-159 ○ High risk >160 ● High density lipoprotein (HDL) ○ Male >45 mg/dl ○ Female >55 mg/dl ○ ○ Low risk CAD greater than or equal to 60 ○ High risk CAD ;ess than 40mg ● Low risk HDL ratio <3 ● High risk HDL ratio 3-5 ● Increased risk ratio >5 Diagnostic studies ■ 12 lead- 12 diff views ECG machine record activity. Resting ECG can identify conduction problems, dysrhythmias, heart position, cardiac hypertrophy, pericarditis, myocardial ischemia or infarction, pacemaker activity and effectiveness of drug therapy ● Nursing resp.: prepare skin and apply leads. Place in supine or elevated if breath is short. Tell pt that no discomfort is involved and lie still ● During: insure pt lies still to decrease motion artifact ■ 6 minute walk test- distant pt can walk in 6 min. Measure response to treatments and determine functional capacity for activities of daily living. ● Nursing resp: tell pt to wear comfy shoes inform pt to carry or pull 02 if used routinely ● During: encourage to walk as quickly as possible ■ Chest xray- pt is placed in 2 upright positions to examine lung fields and heart size. Lateral and posteroanterior. Helps with HF diagnosis pulmonary edema and heart size ● Nursing resp: ask about freq of recent x ray and chance of pregnancy. Provide lead shielding to areas not viewed. Remove jewelry or metal objects that may obstruct view of heart and lungs ■ Echocardiogram ● Contrast, M-mode, 2 dimensional, color flow imaging, real time 3 dimensional, pharmacologic echocardiogram ○ Ultrasound transducer- 4 positions on the chest to record sound waves bounced off heart ■ Record direction of flow thru heart and transforms to audio and graphic data ■ Measures abnormalities, congenital heart defects, wall motion, EF, heart function ■ IV contrast agent may be used to enhance image ■ NURSING: ● Before: left side lying pt. Tell pt about procedure and sensations pressure and mechanical movement from head of the transducer. May be difficult to obtain in pt with COPD due to large amt of air between heart and chest wall ○ Pharm Echo: substitute for the exercise stress test in persons unable to exercise. IV adenosine dobutamine, dipyridamole is given as a single bolus over 10 sec while echo is performed to detect wall motion abnormalities ■ Before: obtain baseline achieved. ■ During: Monitor pt for signs and symp of distress or side effects (shortness or breath, dizzy, nausea) Aminophylline may be given to prevent reverse side effects of dipyridamole ■ SPECT single photon emission computed tomography- determine size or risk of infarction and size. Small amounts of radioactive isotope are injected IV and recordings are made of the activity emitted over a specific area of the body. Circulation of the isotope can detect coronary artery blood flow, shunts, ventricular motion, EF, size of chambers ● NURSING: before- short fasting. Obtain IV access for isotope injection. Remove all jewelry from chest wall start ECG ○ During: pt sit still ○ After: encourage fluids to excrete radioactive substance ■ ■ ■ ■ ■ ■ ■ PET Positron emission tomography: highly sensitive in distinguishing viable and nonviable heart tissue. Nitrogen 13 ammonia injected IV first and scanned to evaluate myocardial perfusion. A second radioactive isotope fluro 18 is then inj. And scanned to show metabolic function of heart. In an ischemic heart both scans differ. Baseline resting scan is usually done for comparison ● Before: obtain IV access to inject the tracer substance. Pts should be NPO except for water and meds for at least 4 hr prior. Fast and refrain from tobacco and caffeine 24 hrs before the test if exercise is part. Hold glucose IV and change to normal saline. Check glucose levels. the glucose level must be btw 60-140 mg for accurate glucose metabolic activity ● during : lie completely still ● After: enc. Fluids to excrete radioactive substance MUGA scan multigated acquisition (cardiac blood pool): small amt of pt blood removed mixed with a radioactive substance isotope and reinjected IV. with the ECG used for timing, images obtained during cardiac cycle. Indicated in HF, MI or valve disease. Can evaluate the effect of various cardiac or cardiotoxic drugs on the heart and the cardiac EF. ● Before: explain procedure. Obtain IV access for removal of blood samples and reinjection of isotope. Start ECG Nuclear imaging- IV injection of radioactive isotopes. Radioactive is counted over the heart by a scintillation camera. Information about heart contractility, myocardial perfusion, acute injury shown. ● before : women must remove bra to decrease breast artifact. IV access for isotopes. Explain that a radioactive isotope is a small, diagno. Amount and will lose most of its radioactivity in a few hours. Tell pt that they will b lying still on back with arms extended overhead for 20 min ● During: repeat scans are done within a few min to hrs after injection Stress perfusion imaging: combo of exercise and echocardiogram. Differ in left ventricular wall motion and thickening before and after exercise are evaluated with ultrasound. Postexercise images are taken within 1 min of stopping exercise. ● Before: prepare for the treadmill or bike. Tell pt of importance of timely return to examination table for imaging after exercise (CMRI) Cardiovascular magnetic resonance imaging: noninvasive imaging tech obtains info about heart tissue, EF, aneurysms, CO, and patency of proximal arteries. Measures regurgitant fraction that may determine valve repair or replacement. It does not involve ionizing radiation and is an extremely safe procedure. Provides images in multiple planes with uniformly good resolution. ● Before: check for preg, allergies, renal function. Have pt remove all metal. Remove metallic foil patches. Pt may need to be fasting. Assess for claustrophobia and the need for anti anxiety meds. ● Contraindicated: pt with implanted metallic devices or other metal fragments unless noted to be MRI safe. Ask about any history of surgical insertion of staples, plates, dental bridges, or other metal. ● during : lie completely still CTA coronary CT angiography: Ct with injected IV contrast medium to obtain images of coronary vessels and diagnose CAD. used to evaluate chest pain and monitor the progression of coronary vascular disease. ● Before: asses for contrast allergy. Obtain IV access needs to fast for several hours prior. A B-blocker may be given before the test to control HR. ● During: pt must have a reg heart rhythm for accurate testing. Cardiac catheterization: insertion of catheter into heart via vein (right side heart) and artery (left side). Procedure done to evaluate chest pain and obtain info about the aorta inferior vena cava, pulmonary artery and veins. Measures pressures within the heart chambers. Contrast medium is injected to help see structures and motion of the heart. ■ ■ ■ Coronary angiography contrast medium is injected directly into coronary arteries to evaluate patency and collateral circulation. ● Before ○ asses for allergies esp to contrast dye ○ Perform baseline ass, vitals, pulse ox, heart and breath sounds, neurovascular assess of extremities ○ Withhodfl food and fluids 6-12 hrs ○ Assess baseline lab values (creatinine, cardiac biomarkers) ○ Teach pt and caregiver about procedure and post procedure care ○ Explain the use of local anesthesia at insertion site, placement of catheter, flushed feeling when dye injected and possible flutter sensation of heart as its passed ○ Give sedative drugs as ordered and others ● Post Procedure ○ Perform assessment and compare baseline: vitals, pulse ox, HR and breath sounds. Note hypotension or hypertension and signs of pulmonary emboli ○ Assess neuro status, peripheral pulses, color and sensation of extremity ○ Place compression device over arterial site to achieve hemostasis if indicated ○ Observe insertion site for hematoma and bleeding every 15 min for the first hr ○ Monitor ECG for dysrhythmias or other chantes ○ Monitor chest pain and other pain and discomfort ○ Maintain bedrest as ordered for femoral access ○ Maintain IV and or oral fluid intake and monitor output ○ Teach pt and caregiver about discharge care including ss to report to HCP. (site complications, chest pain) and activity restriction IVS Intravascular ultrasound: during catheterization a small ultrasound probe is introduced into coronary arteries. Used to assess blood vessel patency, size and consistency of plaque, arterial walls, and effectiveness or intracoronary artery treatment ● Before and after same as catheterization Fractional flow reserve: during catheterization a special wire is inserted into the coronary arteries to measure pressure and flow. Information is used to determine need for angioplasty or stenting on nonsignificant blockages ● Before and after same as catheterization Electrophysiology study (EPS): invasive study to record intracardiac electrical activity using catheters ( with multiple electrodes) inserted via the femoral or jugular vein into the right side of the heart. Catheter electrodes record the activity in diff heart structures. Can induce and stop dysrhythmias. Insertion of a pacemaker or implantable cardioverter defibrillator or ablation of a dysrhythmia pathway may be done during or right after the EPS. ● Before- antidysrhythmic drugs may be stopped several days before study. Keep patient NPO 6-8 hrs before the test. Give premedication to promote relaxation if ordered. IV assess. IV sedation often used ● After: vitals, ECG monitored, bedrest 6-8 hrs after ● ● ● ● ● HYPERTENSION As BP increase so does ○ MI, HF, stroke, renal disease ○ ⅓ adults in US ○ High priority ○ Blood pressure=cardiac output x Systemic vascular resistance Factors influencing BP ○ Sympathetic nervous system (fight or flight) ■ Activation increases HR and cardiac contractility ■ Vasoconstriction and renin release ■ Increase in CO and SVR ○ Baroreceptors ■ Sensitive to stretching ■ Send impulses to sympathetic vasomotor center ■ Vascular endothelium essential to regulation of vasodilating and vasoconstricting substances. ■ Renal system- control sodium excretion and ECF volume ■ RAAS system ■ Prostaglandins ■ endocrine system- epinephrine and norepinephrine from adrenal medulla ■ Aldosterone from adrenal medulla ■ ADH from posterior pituitary Hypertension classification ○ Normal <120 and <80 ○ Elevated 120-129 and <80 ○ Hypertension, stage 1 130-139 or 80-89 ○ Hypertension, stage 2 greater than or equal to 140 or greater than or equal to 90 Etiology of hypertension ○ Primary hypertension- essential or idiopathic ■ Elevated BP without an identified ■ 90% to 95% of all cases ■ Exact cause unknown but several contributing factors ○ Secondary hypertension ■ Elevated BP with a specific cause ■ 5% to 10% of adult cases ■ Clinical findings relate to underlying cause ■ Treatment aimed at removing or treating cause Pathophysiology Primary Hypertension ○ Persistently increased SVR ○ Abnormalities in any mechanisms involved in maintaining of normal BP ○ Risk factors of primary hypertension ■ Age ■ Alcohol ■ Diabetes mellitus ■ Elevated serum lipids ■ Excess dietary sodium ■ Gender ■ family history ■ Obesity ■ Ethnicity ■ sedentary lifestyle ■ socioeconomic status ■ Stress ○ Genetic links ■ ■ ● ● ● Diff sets of genes regulate BP at diff times Children and siblings of persons with hypertension should be screened and strongly advised to adopt healthy lifestyles to reduce the risk ■ Water and sodium retention ● Only 1 in 3 people who consume high sodium diet develop hypertension ● The effect on sodium in BP has a strong genetic component ○ Stress and increased SNS activity ■ Causes increased vasoconstriction ■ Increased HR ■ Increased renin release Clinical manifestations of hypertension “ silent killer” ○ Fatigue ○ Dizziness ○ Palpitations ○ Angina ○ Dyspnea Complications ○ Target organ disease ■ Heart ■ Brain ■ Peripheral vascular disease ■ Kidney ■ Eyes Diagnostic test ○ Measure BP ○ Urinalysis ○ BUN and serum creatinine ○ Creatinine clearance ○ Serum electrolytes, glucose ○ Serum lipid profile ○ Uric acid levels ○ ECG ○ Echocardiogram ○ Ambulatory BP ■ noninvasive , fully automated system that measures BP at present intervals over 24 hrs ■ Teach patient to hold arm still and keep diary ■ Many applications for us Nursing diagnoses ● ● ● ● ● ● Ineffective health management Anxiety Sexual dysfunction Risk for decreased cardiac perfusion Risk for ineffective cerebral and renal perfusion Potential complications : stroke, MI Nursing planning ● ● ● ● Maintain BP Follow therapeutic plan Experience minimal side effects of therapy Manage and cope with this condition Implementation ● Health promotion ● ● ● ● ● ● ● ○ primary prevention via lifestyle mods ○ Individual pt eval and education ○ Screening programs ○ Cardiovascular isk factor modification Ambulatory care ○ Evaluate therapy effect ○ Detect and report adverse eff ○ Asses and enhance compliance ○ Pt and caregiver teaching Home BP monitoring ○ Proper equip, procedure, freq, recording and reporting, target BP Hypertension in older people ○ Increased incidence w age ○ Isolated systolic hypertension older than 50 most common ○ White coat hypertension ( hypertension in medical environment) ○ Age related physical change ○ Altered drug absorption, metabolism, excretion ○ Wide gap and subseq beats ( auscultatory gap) ○ Increased risk for orthostatic hypotension ○ Goal BP older than 60 less than 150/90 ■ Drugs: ● Thiazide diuretic ● Calcium channel blockers ● ACE inhibitors ○ Caution NSAID Hypertensive Crisis ○ SBP less than 180 and DBP less than 110 ■ Hypertensive urgency ● Develop hours to days ● May not req hospitalization ■ Hypertensive emergency ● Very severe problems can result if prompt treatment not obtained ■ Rate of rise more important that absolute value ○ Clinical Manifestations ■ Encephalopathy ● Headache, nausea/vomiting, seizures, confusion, coma ■ Renal insufficiency ■ Cardiac decompensation ● MI,HF, pulmonary edema ■ Aortic dissection ■ Hospitalization ● IV therapy: titrated MAP ● Monitor cardiac renal function ● Neuro checks ● Determine cause ● Education to avoid future crisis Primary hypertension Pathophysiology Altered RAAS Renin-angiotensin aldosterone system ○ Increased renin activates RAAS ○ Renin levels do not decrease in response to elevated BP Insulin resistance and hyperinsulinemia ○ High insulin levels stimulate SNS activity and impair nitric oxide mediated vasodilation Primary hypertension ○ Endothelial dysfunction ■ Imparied response to nitric oxide dilation ■ Elevated endothelin vasoconstriction ● Interprofessional care ○ Overall goals ■ Control BP ■ Reduce CVD risk factors and target organ disease ○ Life style modifications ■ Weight reduction ● Weight loss 22lbs may decrease SBP by 5-20 mm Hg ● Calorie restriction and physical activity ■ DASH eating plan ● Fruits, veggies,fat-free or low fat milk, whole grains, fish, poultry, beans, seeds and nuts ■ Dietary sodium reduction ● 2300 mg/day for healthy adults ● < 1500 mg/day for ○ AA ○ Middle aged and older ○ Those with hypertension, diabetes, or chronic kidney disease ● Moderation of alcohol intake ■ Physical activity ● Moderate-intensity aerobic activity, at least 30 min most days a week ● vigorous activity aerobic activity at least 20 min 3 days a week ● Muscle strengthening activities at least 2 times a week ● Flexibility and balances exercises 2 times a week ■ Avoidance of tobacco products ● Nicotine causes vasoconstriction and elevated BP ● Smoking cessation reduces risk factors within 1 year ■ Psychosocial risk factors ● Low socioeconomic status, social isolation, and lack of support, stress, negative emotions ● Activate SNS and stress hormones ■ Drug therapy ■ Follow up care ■ Identify, report, and minimize side effects ● Orthostatic hypotension ● Sexual dysfunction ● Dry mouth ● Freq urination ■ Time of day drug taken Resistant hypertension: failure to reach the goal of an appropriate 3 drug therapy regimen that includes diuretic. Reasons: ○ Improper BP measurement ○ Drug induced ○ Associated conditions ○ Identifiable causes of secondary hypertension ●