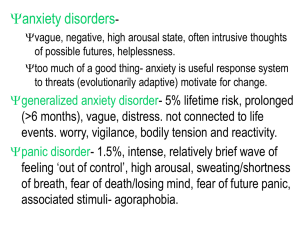
MC Matlala AC Maluka CONTENT INTRODUCTION HISTORY GENERAL DESCRIPTION AETIOLOGY CLINICAL FEATURES CULTURAL CONSIDERATIONS TYPES DIAGNOSTIC CRITERIA AND DIFFERENTIAL DIAGNOSIS COMORBIDITY COURSE AND PROGNOSIS MANAGEMENT REFERENCES Types of Anxiety Disorders Separation Anxiety Disorder Panic Attack Specifier Selective Mutism Substance/Medication-Induced Anxiety Disorder Anxiety Due to another Medical Condition Generalized Anxiety Disorder Social Anxiety Disorder (Social Phobia) Panic Disorder Specific Phobia Agoraphobia Introduction • Everyone feels anxiety from time to time in our everyday lives. • The adaptive value of anxiety may be that it helps us plan and prepare for possible threat. • We may feel an anxiety/anxious when we are facing an important event such as an exam, or a job interview or when we perceive some threat or danger. • However, such everyday anxiety is generally occasional, mild, and brief, while the anxiety felt by someone who is suffering from anxiety disorder occurs frequently, more intense and can last longer. • Anxiety that does not go and can get worse over time and the symptoms can interfere with daily activities. General Description • Anxiety: a mood state characterized by strong negative emotion and bodily symptoms of tension in anticipation of future danger or misfortune • Anxiety disorders - all have unrealistic, irrational fears or anxieties of disabling intensity as their principal and most obvious manifestation. • Anxious persons falsely justify their fear, set up a vicious circle of anxiety, distorted perception, and increased anxiety. • People with these varied disorders differ from one another both in terms of the relative preponderance of fear or panic versus anxiety symptoms that they experience and in the kinds of objects or situations that most concern them. • Many people with one anxiety disorder will experience at least one more anxiety disorder concurrently or at a different point in their lives. General Description • The symptoms of anxiety are expressed through three interrelated response systems: the physical system, the cognitive system, and the behavioural system. 1. Physical System - When a person perceives or anticipates danger, the brain sends messages to the sympathetic nervous system, which produces the fight/flight response. The activation of this system produces many important chemical and physical effects that mobilize the body for action. 2. Cognitive System - Since the main purpose of the fight/flight system is to signal possible danger, its activation produces an immediate search for a potential threat. Activation of the cognitive system often leads to subjective feelings of apprehension, nervousness, difficulty concentrating, and panic. 3. Behavioural System - The overwhelming urges that accompany the fight/flight response are aggression and a desire to escape the threatening situation. E.g., Avoidance perpetuates anxiety Aetiology Heridatory influences • More common in first-degree relatives of affected individuals • Identical twins: 45% (MZ > DZ concordance) • Relatives : 20% • Panic disorder has a 4-7 chance of incidence in first-degree relatives. • Specific phobias may aggregate by type within families. Biological influences • Catecholamine (“fight or flight reaction”) and serotonin modulation. • The GABA receptor, the primary inhibitory transmitter in the brain, plays an important role in the modulation of arousal and anxiety. • Anxiolytics increase GABA and decrease anxiety • Oversensitive respiratory control centre in brain stem • Lactic acid infusion and carbon dioxide inhalation bring out panic disorder. Aetiology Psychological influences • More uncontrollable stressful life events • Behavioural inhibition -Tendency to be agitated, distressed, and cry in unfamiliar or novel settings • Observed in infants as young as 4 months (May be inherited • Temperament - Predicts anxiety in childhood and social anxiety in adolescence • Neuroticism - Tendency to react with frequent negative affect • Linked to anxiety and depression • Higher levels linked to double the likelihood of developing anxiety disorders • Previous anxiety disorder + stress --> relapse Aetiology Cognitive Factors • Sustained negative beliefs about future Bad things will happen Engage in safety behaviours • Belief that one lacks control over environment More vulnerable to developing anxiety disorder Childhood trauma or punitive parenting may foster beliefs Serious life events can threaten sense of control • Attention to threat Tendency to notice negative environmental cues Selective attention to signs of threat Cultural Considerations • The experience of anxiety is pervasive across cultures • Ethnicity and culture may affect the expression, developmental course, and interpretation of anxiety symptoms • Culturally specific syndromes: Taijin kyofusho - Japanese fear of offending or embarrassing others Kufungisisa - means “too much thinking”. A term of distress expressed by the peoples of Shona in Zimbabwe. Ataque de nervios—this expression refers to a sense of being out of Control and is recognized among many Latinos from the Caribbean. Clinical Features of Anxiety Disorders Physical Cognitive Behavioural Dizziness Thoughts of being scared or hurt Self-deprecatory or self- critical thoughts Increased respiration Thoughts of feeling incompetent and inadequate Blanking out or forgetfulness Nausea Thoughts of bodily injury Thoughts of going crazy Upset stomach Thoughts of images of monsters or animals Thoughts of contamination Fatigue Difficulty concentrating Thoughts of appearing foolish Vomiting Images of harm to loved ones Sweating Numbness Heart palpitations Blurred vision Increased heart rate Seperation Anxiety Disorder • Separation anxiety disorders is defined as excessive anxiety, fear or avoidance behavior upon separation from attachment figures to a degree that is developmentally inappropriate or about possible harm to them with the refusal to go out, travel or participate in events or activities that entail physical separation; fear of being alone and recurring nightmare involving separation. • Symptoms of SAD often lead to significant distress in daily functioning and somatic complaints, which presents when separation is anticipated or experienced. • Previous versions of DSM listed SAD under the section ‘disorders usually first diagnosed in infancy, childhood, or adolescence’. • The current classification acknowledges that SAD may be diagnosed throughout the entire lifespan. • To meet the diagnostic criteria, the features of SAD should be present for at least four weeks in children and for at least six months in an adult. Panic Attack Specifier • Esssentail feature is the abrupt surge of intense fear or intense discomfort that reaches peak within minutes and during which physical and cognitive symptoms occur. • Panic attack can arise from either a calm state or an anxious state. • There are two characteristic types of panic attacks: expected and unexpected. • Panic attacks can occur in the context of any mental disorder and some medical conditions, with the majority never meeting criteria for panic disorder. Selective Mutism • Selective mutism is a relatively rare childhood disorder and is underdiagnosed and undertreated. • It is characterized by consistent failure to speak in situations where speaking is socially expected (example, at school), while being able to speak freely in other situations (example, at home). • The person who has selective mutism is not limited to interactions with adults and their situation is not explained by the absence of familiarity with the spoken language. • Estimated to occur in 0.7% of children • Average age of onset is 3-4 years • May be an extreme type of social phobia, but there are differences between the two disorders Substance/Medication-Induced Anxiety Disorder • Direct result of a toxic substance, including drugs of abuse, medication, poison, and alcohol, among others • Laboratory asssessment (urine toxiclology) may be useful to measuresubstanc intoxication aspart of an assessment for the disorder Anxiety Due to another Medical Condition • The essential feature is significant anxiety that is judged to be best explained as a physiological effects of another medical condition. • Symptoms can include anxiety symptoms or panic attacks. • The judgement that symptoms are best explained by the associated physical condition must be based on evidence from the history, physical examination, or laboratory findings. • Several medical conditions can cause symptoms similar to those of anxiety disorders E.g., endocrine disease, cardiovascular disorders, respiratory illness, and neurological illness. • Is diagnosed when medical condition is known to induce anxiety and when the medical condition preceded the onset of the anxiety. Diagnostic criteria for Seperation Anxiety Disorder A. Developmentally inappropriate and excessive fear or anxiety concerning separation from those to whom the individual is attached, as evidenced by at least three of the following: 1. Recurrent excessive distress when anticipating or experiencing separation from home or from major attachment figures. 2. Persistent and excessive worry about losing major attachment figures or about possible harm to them, such as illness, injury, disasters, or death. 3. Persistent and excessive worry about experiencing an untoward event (e.g., getting lost, being kidnapped, having an accident, becoming ill) that causes separation from a major attachment figure. 4. Persistent reluctance or refusal to go out, away from home, to school, to work, or elsewhere because of fear of separation. 5. Persistent and excessive fear of or reluctance about being alone or without major attachment figures at home or in other settings. Diagnostic criteria for Seperation Anxiety Disorder 6. Persistent reluctance or refusal to sleep away from home or to go to sleep without being near a major attachment figure. 7. Repeated nightmares involving the theme of separation. 8. Repeated complaints of physical symptoms (e.g., headaches, stomachaches, nausea, vomiting) when separation from major attachment figures occurs or is anticipated. B. The fear, anxiety, or avoidance is persistent, lasting at least 4 weeks in children and adolescents and typically 6 months or more in adults. C. The disturbance causes clinically significant distress or impairment in social, academic, occupational, or other important areas of functioning. D. The disturbance is not better explained by another mental disorder, such as refusing to leave home because of excessive resistance to change in autism spectrum disorder; delusions or hallucinations concerning separation in psychotic disorders; refusal to go outside without a trusted companion in agoraphobia; worries about ill health or other harm befalling significant others in generalized anxiety disorder; or concerns about having an illness in illness anxiety disorder. Diagnostic criteria for Panic Attack Specifier An abrupt surge of intense fear or intense discomfort that reaches a peak within minutes, and during which time four (or more) of the following symptoms occur: Note: The abrupt surge can occur from a calm state or an anxious state. 1. Palpitations, pounding heart, or accelerated heart rate. 2. Sweating. 3. Trembling or shaking. 4. Sensations of shortness of breath or smothering. 5. Feelings of choking. 6. Chest pain or discomfort. 7. Nausea or abdominal distress. 8. Feeling dizzy, unsteady, light-headed, or faint. 9. Chilis or heat sensations. 10. Paresthesias (numbness or tingling sensations). 11. Derealization (feelings of unreality) or depersonalization (being detached from oneself). 12. Fear of losing control or “going crazy.” 13. Fear of dying. Note: Culture-specific symptoms (e.g., tinnitus, neck soreness, headache, uncontrollable screaming or crying) may be seen. Such symptoms should not count as one of the four required symptoms. Diagnostic criteria for Selective Mutism A. Consistent failure to speak in specific social situations in which there is an expectation for speaking (e.g., at school) despite speaking in other situations. B. The disturbance interferes with educational or occupational achievement or with social communication. C. The duration of the disturbance is at least 1 month (not limited to the first month of school). D. The failure to speak is not attributable to a lack of knowledge of, or comfort with, the spoken language required in the social situation. E. The disturbance is not better explained by a communication disorder (e.g., childhood- onset fluency disorder) and does not occur exclusively during the course of autism spectrum disorder, schizophrenia, or another psychotic disorder Diagnostic criteria for Substance/Medication-Induced Anxiety Disorder A. Panic attacks or anxiety is predominant in the clinical picture. B. There is evidence from the history, physical examination, or laboratory findings of both (1)and (2): 1. The symptoms in Criterion A developed during or soon after substance intoxication or withdrawal or atter exposure to a medication. 2. The involved substance/medication is capable of producing the symptoms in Criterion A. C. The disturbance is not better explained by an anxiety disorder that is not substance/ medicationinduced. Such evidence of an independent anxiety disorder could include the following: The symptoms precede the onset of the substance/medication use; the symptoms persist for a substantial period of time (e.g., about 1 month) atter the cessation of acute withdrawal or severe intoxication: or there is other evidence suggesting the existence of an independent non-substance/medication-induced anxiety disorder (e.g., a history of recurrent non-substance/medication-related episodes). D. The disturbance does not occur exclusively during the course of a delirium. E. The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. Diagnostic criteria for Anxiety Due to another Medical Condition A. Panic attacks or anxiety is predominant in the clinical picture. B. There is evidence from the history, physical examination, or laboratory findings that the disturbance is the direct pathophysiological consequence of another medical condition. C. The disturbance is not better explained by another mental disorder. D. The disturbance does not occur exclusively during the course of a delirium. E. The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. Coding note: Include the name of the other medical condition within the name of the men tal disorder (e.g., 293.84 [F06.4] anxiety disorder due to pheochromocytoma). The other medical condition should be coded and listed separately immediately before the anxiety disorder due to the medical condition (e.g., 227.0 [D35.00] pheochromocytoma; 293.84 [F06.4] anxiety disorder due to pheochromocytoma Differential Diagnosis for Seperation Anxiety Disorder Communication disorders Neurodevelopmental disorders Schizophrenia and disorders Social anxiety disorder other psychotic Differential Diagnosis for Panic Attack Specifier Other paroxysmal episodes (eg., anger attacks) Anxiety disorder due to another medical condition Substance /medication-induced anxiety disorder Differential Mutism Diagnosis • Social anxiety disorder • Seperation anxiety disorder • Specific phobia • Oppositional behaviours • Communication disorders for Selective Differential Diagnosis for Substance/Medication Induced Anxiety Disorder • Substance Intoxication and substance withdrawal • Anxiety disorder (not induced by substance/medication) • Delirium • Anxiety condition disorder due to another medical Differential diagnosis for Anxiety Due to another Medical Condition • Delirium • Mixed presentation of symptoms (mood and anxiety) • Substance/medication induced anxiety disorder • Anxiety disorder • Illness anxiety disorder • Adjustment disorders • Associated feature of another mental disorder • Other specified or unspecified anxiety disorder Comorbidity SEPERATION ANXIETY DISORDER PANIC ATTACK SPECIFIER • Specific phobia Anxiety disorders • PTSD Depressive disorders • Panic disorder Bipolar disorders • Generalised anxiety disorder Impulse-control disorders • Personality disorder Substance use disorders • Depressive disorders • Bipolar disorders Course and prognosis • Most anxiety disorders tend to be chronic disorders. • Panic disorder tends to present in late adolescence to early adulthood. It has perhaps a bimodal distribution (late adolescence and mid-30’s). • It can be chronic, but waxing and waning. • At 6-10 years follow- up, 1/3 patients appear to be well, about 1/2 have improved but are still symptomatic, and 1/5 – 1/3 feel the same or worse. • There is a high risk of relapse after (somatic) treatment. Management - Psychotherapy Behavioural Interventions Cognitive-Behavioral Therapy (CBT) • Exposure - to feared stimulus • The most effective procedure for treating most anxiety disorders • Systematic desensitization • Flooding: prolonged repeated exposure • Response prevention prevents child from engaging in escaping or avoidance stimuli • Modeling and reinforced practice • Use of coping strategies to control symptoms than escape or avoid Relaxation Deep breathing • Almost always used with exposure-based treatments • Coping Cat • Skills training and exposure combat problematic thinking • Computer-based CBT has also been shown to be effective Management Psychopharmacotherapy Anxiolytics: drugs that reduce anxiety • Benzodiazepenes Valium Xanax • Antidepressants Tricyclics Selective Serotonin Reuptake Inhibitors (SSRIs) Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) • D-cycloserine (DCS) - Enhances learning and can bolstered treatment effectiveness • Side effects can be problematic with continuing medication Management Family interventions • Provides education about the disorder • Helps families cope with their feelings • Medications can reduce symptoms and most effective when combined with CBT • Treatments are directed at modifying: Distorted information processing Physiological reactions to perceived threat Sense of a lack of control Excessive escape and avoidance behaviors Reference List American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders 5th ed. American Psychiatric Association. Comer, R. J., & Comer, J. S. (2018). Abnormal psychology 10th ed. Worth Publishers. Makhafula, K., & Lake, M. (2019). Anxiety, obsessive-compulsive, and trauma-related disorder. In A. Burke (Eds.), Understanding psychopathology: South African Perspective (3rd ed, pp. 161200). Oxford. Sadock, B. J., Sadock, V. A., & Ruiz, P. (2014). Kaplan and Sadock's synopsis of psychiatry: Behavioral sciences/clinical psychiatry 11th ed. Lippincott Williams & Wilkins.