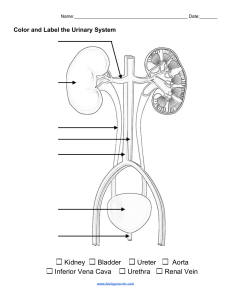
Chapter 32 Structure and Location of the Kidney: • • Structure: o Paired, bean-shaped organs o Multiobular structure, composed of up to 18 lobes o Each lobule is composed of nephrons, the functional units of the kidney Location: o Outside the peritoneal cavity in the back of the upper abdomen o One on each side of the vertebral column at the level of the 12th thoracic to 3rd lumbar vertebrae Kidney: • • • • Each is smaller than a person’s fist, the two organs process approximately 22% to 25% of the cardiac output or 1100 mL/ minutes Left Kidney sits higher than the right Waste that goes into the (from the renal vein) kidney comes from your circulation Kidneys are not able to regenerate o When you reach the age of 40, you lose 10% of function Function of the nephron*** • • • • • • The kidney has no ability to regenerate nephrons. o Therefore, with aging, there is a generalized decrease in functioning nephrons. o In fact, adults tend to lose approximately 10% of their nephrons for each decade beginning at 40 years of age. Blood flows into the glomerular capillaries from the afferent arteriole and flows out of the glomerular capillaries into the efferent arteriole, which leads into the peritubular capillaries. The glomerulus consists of a compact tuft of capillaries encased in a thin, doublewalled capsule called Bowman capsule. Fluid and solutes from the blood are filtered through the capillary membrane into a fluid-filled space in Bowman capsule, called Bowman space. The portion of the blood that is filtered into the capsule space is called the filtrate. The mass of capillaries and its surrounding epithelial capsule are collectively referred to as the renal corpuscle. Capillary System Supplying the Nephron: • • The glomerular capillary membrane is composed of 3 layers: o Capillary endothelial later o Basement membrane o Single-celled capsular epithelial layer The outer epithelial layer that covers the glomerulus is continuous with the epithelium that lines the Bowman capsule. • The cells of the epithelial layer have unusual octopus-like structures that possess a large number of extensions, or foot processes (i.e., podocytes), which are embedded in the basement membrane that lies between the capillary endothelium and the outer epithelial layer. o These foot processes form slit pores through which the glomerular filtrate passes. Four Segments of the Nephron Tubule: • • • • Proximal Convoluted Tubule o A highly coiled segment; drains into the Bowman Capsule o Approximately 65% of all absorptive and secretory processes of the tubular system take place in the proximal tubule. *** o Many substances, such as glucose, are freely filtered in the glomerulus and reabsorbed by energy-dependent cotransport carrier mechanisms.*** o Reabsorption: ▪ Na ▪ Cl ▪ HCO3 ▪ K ▪ H2O o Secretions: ▪ H+ ▪ Organic acids and bases Loop of Henle o A thin looped structure o The loop of Henle plays an important role in controlling the concentration of the urine. ▪ It does this by establishing a high concentration of osmotically active particles in the interstitium surrounding the medullary (Middle) collecting tubules where the antidiuretic hormone (ADH) exerts its effects.*** o The loop of Henle, taken as a whole, always reabsorbs more Na+ and Cl− than water. ▪ This is in contrast to the proximal tubule, which reabsorbs Na+ and water in equal proportions.*** o Reabsorption (thin descending Lopp of Henle): ▪ H2O Distal Convoluted Tubule o A distal coiled portion Collecting Tubule o Joins with several tubules to collect the filtrate Na+ Transport as the Driving Force: • • • Na+/K+ ATPase maintains the concentration gradient Symport Antiport o May result in heart or kidney failure Question: Which of the following best describes the function of the nephron? A. B. C. D. The detoxification of blood The retention of important organic materials found in the filtrate The reabsorption of water, electrolytes, and other substances from the bloodstream The synthesis and storage of urine Rationale: The resorption of water, electrolytes, and other substances from the bloodstream is the main function of the nephrons. *ADH also known as vasopressin The Juxtaglomerular Complex: • • The juxtaglomerular complex is thought to represent a feedback control system that links changes in the GFR (how much you pee) with renal blood flow.*** In approximately one fifth of the juxtamedullary nephrons, the loops of Henle and special hairpin-shaped capillaries called the vasa recta descend into the medullary portion of the kidney. Endocrine Function of the Kidney: • • • • Juxtaglomerular Complex The Renin–Angiotensin–Aldosterone Mechanism o Plays important part in regulation of blood pressure o Renin functions by means of angiotensin II to produce vasoconstriction of the efferent arteriole to prevent large decreases in the GFR. o Angiotensin II also increases sodium reabsorption indirectly by stimulating aldosterone secretion from the adrenal gland and directly by increasing sodium reabsorption by the proximal tubule cells. o The renin–angiotensin–aldosterone (RAA) mechanism.*** Erythropoietin o Regulates the differentiation of red blood cells in bone marrow o Erythropoietin is a glycoprotein hormone that is produced by fibroblasts in the renal interstitium and regulates the production of red blood cells in the bone marrow. o The synthesis of erythropoietin is stimulated by tissue hypoxia, which may be brought about by anemia, residence at high altitudes, or impaired oxygenation of tissues because of cardiac or pulmonary disease. o Person with end-stage kidney disease is often anemic because of an inability of the kidneys to produce erythropoietin. o This anemia is usually managed by the administration of a recombinant erythropoietin (epoetin alfa) produced through DNA technology to stimulate erythropoiesis.*** o Vitamin D o Increases calcium absorption from the gastrointestinal tract o Helps regulate calcium deposition in bone o Activation of vitamin D occurs in the kidneys. o Vitamin D increases calcium absorption from the gastrointestinal tract and helps to regulate calcium deposition in the bone. o It also has a weak stimulatory effect on renal calcium absorption. o Although vitamin D is not synthesized and released from an endocrine gland, it is often considered a hormone because of its pathway of molecular activation and mechanism of action. o Vitamin D exists in two forms—natural Question: Which of the following hormones is produced in the kidney? A. B. C. D. ADH Erythropoietin Aldosterone Angiotensin Rationale: Erythropoietin is formed in the kidney in response to decreased blood oxygenation. Action of Diuretics: • • • Loop Diuretics: o Exert their effect in the thick ascending loop of Henle o Example: ▪ Furosemide (Lasix) Thiazide Diuretics o Prevent the reabsorption of NaCl in the distal convoluted Tubule o Example: ▪ Chorhtalidone (Thalitone) used for Hypertension The Aldosterone Antagonists (potassium-sparing diuretics) o Reduce sodium reabsorption and increase potassium secretion in the late distal tubule and cortical collecting tubule site regulated by aldosterone o Used for Cronic Heart Failure o Examples: ▪ Spironolactone and Eplerenone Characteristics of Normal Urine: • • • • • A clear, amber-colored fluid ** Approximately 95% water and 5% dissolved solids The kidneys normally produce approximately 1.5 L of urine each day. Contains metabolic wastes and few or no plasma proteins, blood cells, or glucose molecules If you have blood in your urine, you are also going to have protein in your urine Renal Clearance: • Definition: o The volume of plasma that is completely cleared each minute of any substance that finds its way into the urine (1300 mL/Minute) • Determining Factors: o The ability of the substance to be filtered in the glomeruli o The capacity of the renal tubules to reabsorb or secrete the substance Tests for Renal Function: • • • • • • Urinalysis: o Color: ▪ Yellow amber o Appearance: ▪ Clear to clightly hazy o PH: ▪ 4.5-8 • Average person has a pH of 5-6 Glomerular Filtration Rate o The GFR can be measured clinically by collecting timed samples of blood and urine. o Creatinine is produced by muscles as a product of the metabolism of a molecule called creatine. ▪ The formation and release of creatinine are relatively constant and proportional to the amount of muscle mass present. ▪ Creatinine is freely filtered in the glomeruli, is not reabsorbed from the tubules into the blood, and is only minimally secreted into the tubules from the blood. • Therefore, its blood values depend closely on the GFR. o The comparison of creatinine levels in the blood and urine can provide a useful measure of GFR. o The clearance rate for creatinine is the amount that is completely cleared by the kidneys in 1 minute. Blood Tests o Serum creatinine o Blood urea nitrogen Cystoscopy: o the visualization of the bladder by the insertion of an instrument called a cystoscope through the urethra into the bladder. o Ureteroscopy involves the use of a smaller, thinner scope that may be used to remove stones from the ureter and aid in the treatment of ureteral disorders, such as ureteral strictures. Ultrasonography: o is used to visualize the structures of the kidneys and has proved useful in the diagnosis of many urinary tract disorders, including congenital anomalies, renal abscesses, hydronephrosis, and kidney stones. Radiology and other image studies QUESTION: Normal Urine should ___. A. Be cloudy B. Have a pH of 7.0 or greater C. Have a specific gravity of 1.0 D. Be sterile Rationale: There will be no bacteria present in a healthy urinary tract. Renal Casts: • • Casts are molds of the distal nephron lumen Casts develop when the protein concentration of the urine is high (as in nephrotic syndrome), urine osmolality is high, and urine pH in low *** Specific Gravity: • • The specific gravity of urine varies with its concentration of solutes The urine specific gravity provides a valuable index of the hydration status and functional ability of the kidneys Serum Creatinine Levels: • In addition to its use in calculating the GFR, the serum creatinine level is used in estimating the functional capacity of the kidneys Measurement of PVR can be achieved quickly, accurately, and painlessly by the use of ultrasonography (bladder scan). A PVR value of less than 50 mL is considered adequate bladder emptying, and more than 200 mL indicates inadequate bladder emptying Chapter 33 *Whilm’s tumor is the #1 kidney tumor in a child Fetal Anomalies: • • Most common: o Anomalies in shape and position Less common are disorders involving: o A decrease in renal mass ▪ Example: • Agenesis, hypogenesis o A change in renal structures Organ Development: • • Dysgenesis: o Failure of an Organ to develop normally Agenesis: o The complete failure of an organ to develop o Newborns with bilateral renal agenesis— ▪ a rare condition in which the kidney fails to develop at all—are stillborn or live for only a few hours. ▪ ▪ Unilateral renal agenesis occurs in about 1 of 1000 to 2000 newborn infants. Boys are affected more often than girls.4 Detection of unilateral agenesis may be delayed because the healthy kidney usually undergoes compensatory hypertrophy and performs the function of the missing kidney. o In renal hypoplasia, the kidneys do not develop to normal size and contain fewer renal lobes. o Like agenesis, hypoplasia more commonly affects only one kidney. o When both kidneys are affected, renal failure progressively develops. • Hypoplasia: o Failure of an organ to reach normal size Potter Syndrome: • Characteristic facial features of newborns with renal agenesis o o o o o • • • The eyes are widely separated and have epicanthic folds. The ears are low set. The nose is broad and flat. The chin is receding. Limb defects often are present. Newborns with renal agenesis often have characteristic facial features, previously called Potter syndrome, resulting from the effects of oligohydramnios. Without the amniotic fluid to protect and cushion, the uterus may compress the developing fetus. The eyes are widely separated and have epicanthic folds, the ears are low set, the nose is beaklike, the chin is receding, and limb defects are often present. Causes of Neonatal Renal Failure with Potter Phenotype: • • • Cystic renal dysplasia o caused by an abnormality in the differentiation of kidney structures during embryonic development. o It is characterized by undifferentiated tubular structures surrounded by primitive embryonic tissue and may contain smooth muscle and cartilage. o Noncommunicating cysts of varying size may replace normal renal parenchyma. Obstructive uropathy: o usually classified according to site, degree, and duration of obstruction.Lower urinary tract obstructions are located below the ureterovesical junction and are bilateral in nature. o Upper urinary tract obstructions are located above the ureterovesical junction and are usually unilateral. o The condition causing the obstruction can cause complete or partial occlusion of urine outflow. o When the obstruction is of short duration (i.e., less than a few days), it is said to be acute and is usually caused by conditions such as renal calculi. Autosomal recessive polycystic disease • Unilateral agenesis (uncommon) Cystic Disease of the Kidney: • • • Definition: o Fluid-filled sacs or segments of a dilated nephron Causes: o Tubular obstructions that increase intratubular pressure o Changes in the basement membrane of the renal tubules that predispose to cystic dilation Types: o Simple and acquired renal cysts ▪ Simple cysts are a common disorder of the kidney. The cysts may be single or multiple, unilateral or bilateral, and they usually are less than 1 cm in diameter, although they may grow larger. ▪ Most simple cysts do not produce signs or symptoms or compromise renal function.**** o Medullary cystic disease: ▪ a group of renal disorders that have their onset in childhood. Common characteristics of this ARPKD are small, shrunken kidneys and the presence of a variable number of cysts, usually concentrated at the corticomedullary junction. o Polycystic kidney disease ▪ Autosomal recessive polycystic kidney disease ▪ Autosomal dominant polycystic kidney disease Causes of Urinary Tract Obstruction: • • • • • • • Developmental defects Calculi (stones) Pregnancy Benign prostatic hyperplasia Scar tissue resulting from infection and inflammation Tumors Neurologic disorders such as spinal cord injury Damaging Effects of Urinary Obstruction • • • Stasis of urine: o Predisposes to infection and stone formation Development of Backpressure o Interferes with renal blood flow and destroys kidney tissue Manifestations: o Depend on : ▪ The site of obstruction ▪ The cause ▪ The rapidity with which the condition developed o Common symptoms: ▪ ▪ ▪ Pain Signs and symptoms of UTI Manifestations of renal dysfunction Kidney Stones: • • • • • • • • • Definition: o Crystalline structures that form from components of the urine Also known as renal calculi Requirements for formation: o A nidus (nucleus) to form o A urinary environment that supports continuous crystallization of stone components The most common cause of upper urinary tract obstruction is urinary calculi*** o Most development in the kidneys Kidney stone formation requires a supersaturated urine and an environment that allows the stone to grow. The risk for stone formation is increased when the urine is supersaturated with stone components (e.g., calcium salts, uric acid, magnesium ammonium phosphate, cystine). Factors influencing the formation of Kidney Stones: o The concentration of stone components in the urine o The ability of stone components to complex and form stones o The presence of substances that inhibit stone formation o Most kidney stones (75% to 80%) are calcium stones—calcium oxalate, calcium phosphate, or a combination of the two materials.** o Emerging research indicates that 13% to 44% of calcium oxalate stones are culture positive, with Escherichia coli and Pseudomonas spp. representing the leading organisms. Types of kidney stones: o Calcium stones ▪ Oxalate or phosphate o Magnesium ammonium phosphate stones o Uric acid stones o Cystine stones Treatment: o Preventative ▪ ▪ ▪ o o o Dietary restriction Calcium salt supplementation Thiazide diuretics • Cellulose phosphate Treatment for pain Antibiotic infection Removing stones ▪ Ureteroscopy removal ▪ Percutaneous removal ▪ Extracorporeal lithotripsy o Diagnosis ▪ ▪ ▪ ▪ Urinalysis Radiography Intravenous pyelography Ultrasonography Types of Urinary Tract Infections: • • • • • • Asymptomatic Bacteriuria Symptomatic infections Lower UITs o Cystitis Upper UITs o Pyelonephritis UTIs are a frequent type of bacterial infection seen by health care providers. UTIs include several distinct entities, including asymptomatic bacteriuria, symptomatic infections, lower UTIs such as cystitis, and upper UTIs such as pyelonephritis.*** Causes of UTI: • Most uncomplicated UTIs caused by Escherichia coli • Other uropathic pathogens include o Staphylococcus saprophyticus in uncomplicated UTIs o Both non–E. coli gram-negative rods (Proteus mirabilis, Klebsiella pneumoniae, Enterobacter, Pseudomonas, and Serratia) o Gram-positive cocci (Staphylococcus aureus, group B streptococcus) in complicated UTIs Most caused by bacteria that enter through the urethra • Causes of UTIs associated with Stasis or Urine Flow: • • • Anatomic obstructions o Urinary tract stones o Prostatic hyperplasia o Pregnancy o Malformations of the ureterovesical junction Increased pressure resulting in reflux Functional obstructions: o Neurological bladder o Infrequent voiding o Detrusor (bladder) muscle instability o Constipation Question: is the following statement True or False? Static urine flow will predispose your patients to development of a UTI True: Rationale: Static urine flow will predispose your patient to development of a UTI. Glomerulonephritis: • • Immune mechanisms o Glomerular antibodies o Circulating antigen-antibody complexes Characteristics o Hematuria with red cell casts o o o o • A diminished glomerular filtration rate (GFR) Azotemia ▪ (presence of nitrogenous wastes in the blood) Oliguria Hypertension o Acute postinfectious glomerulonephritis usually occurs after infection with certain strains of group A beta-hemolytic streptococci** Causes: o Diseases that provoke a proliferative inflammatory response of the endothelial, mesangial, or epithelial cells of the glomeruli o The inflammatory process: ▪ Damages the capillary wall ▪ Permits red blood cells to escape into the urine ▪ Produces hemodynamic changes that decrease the GFR Cellular Changes in Glomerular Disease: • • • • • • • • Proliferative: o Endothelial o Mesangial o Leukocyte o Crescent formation Basement membrane thickening Sclerosis Fibrosis Diffuse glomerular changes Focal glomerular changes Segmental glomerular changes Mesangial changes Urinary Changes in Glomerulonephritis: • • • • • • • Proteinuria (protein) Hematuria (blood) Pyuria (pus) Oliguria (low urine output) Edema (swelling) Hypertension (high blood pressure) Azotemia (Elevated levels of urea and nitrogen in the blood) Question: Glomerulonephritis will result from which of the following? A. B. C. D. E. Basement membrane thickening Sclerosis Fibrosis Hypercellularity All of the above Rationale: Each of these changes can lead to glomerulonephritis. Tubulointerstitial Disorder: • Damage to the proximal, loop, or distal portion of the nephron o Acute tubular necrosis o Renal tubular acidosis o Pyelonephritis o The effects of drugs and toxins ▪ Gentamycin Proximal and Distal Tubular Acidosis: • Renal tubular acidosis: o Proximal tubular disorders that affect bicarbonate reabsorption o Distal tubular defects that affect the secretion of fixed metabolic acids Major Groups of Renal Neoplasms: • • Embryonic kidney tumors occurring during childhood o Wilms tumor ▪ Onset at 3 to 5 years ▪ In one or both kidneys ▪ WT1 mutation on chromosome 11 Adult kidney cancers o Renal cell carcinoma Chapter 34 Renal Failure: • • Definition: o A condition in which the kidneys fail to remove metabolic end products from the blood and regulate the fluid, electrolyte, and pH balance of the extracellular fluids** Underlying Causes: o Renal disease o Systemic disease o Urologic defects of nonrenal origin Prevention and Early Diagnosis of Acute Renal Failure: • Assessment measures to identify persons at risk for development of acute renal failure o Those with preexisting renal insufficiency and diabetes o Elderly persons (due to the effects of aging on renal reserve) Types of Renal Failure: • • Acute Renal Failure o Abrupt in onset o Often is reversible if recognized early and treated appropriately Chronic Renal Failure: o The end result of irreparable damage to the kidneys o It develops slowly, usually over the course of a number of years o Hypertension and diabetic kidney disease are the two main causes of CKD in the United States.** o A GFR of less than 15 mL/min/1.73 m, usually accompanied by most of the signs and symptoms of uremia, or o A need to start renal replacement therapy (dialysis or transplantation)” Prerenal Cases if Acute Renal Failure: • • • • Hypovolemia Decreased vascular filling Heart failure and cardiogenic shock Decreased renal perfusion due to vasoactive mediators, drugs, diagnostic agents Postrenal Causes of Acute Renal Failure • • Bilateral ureteral obstruction Bladder outlet obstruction Question: Congestive Heart Failure would be a(n) ___ cause of renal failure A. Prerenal B. Intrarenal C. Postrenal Rationale: Prerenal causes of acute kidney injury include profound depletion of vascular volume, impaired perfusion due to heart failure and cardiogenic shock, and decreased vascular filling because of increased vascular capacity. Intrinsic or Intrarenal Causes of Acute Renal Failure: • Acute tubular necrosis o Prolonged renal ischemia o Exposure to nephrotoxic drugs, metals, organic solvents o Intratubular obstruction resulting from hemoglobinuria, myoglobinuria, myeloma light chains, or uric acid casts o Acute renal disease Common causes of Chronic Renal Disease: • • • • • • • • • Hypertension Diabetes mellitus Polycystic kidney disease Obstructions of the urinary tract Glomerulonephritis Cancers Autoimmune disorders Diseases of the heart or lungs Chronic use of pain medication Stages of the Progression of Chronic Renal Failure: • • • • • Albuminuria serves as a key marker of kidney damage.Urine normally contains small amounts of protein***. Mild reduction of GFR to 60 to 89 mL/min/1.73 m2 Moderate reduction of GFR to 30 to 59 mL/min/1.73 m2 Severe reduction in GFR to 15 to 29 mL/min/1.73 m2 Kidney failure with a GFR < 15 mL/min/1.73 m2, with a need for renal replacement therapy Question: a GFR of ___ best describes renal failure. A. B. C. D. 60 to 89 mL/min/1.73 m2 30 to 59 mL/min/1.73 m2 15 to 29 mL/min/1.73 m2 <15 mL/min/1.73 m2 Rationale: Less than 15 mL/min/1.73 m2 is the result of significantly decreased renal filtration and is the cut-off point of renal failure. Clinical Manifestations of Chronic Renal Failure: • • Accumulation of nitrogenous wastes Alterations in water, electrolyte, and acid–base balance • • • • • • • • • • • • • Mineral and skeletal disorders Anemia and coagulation disorders The accumulation of nitrogenous wastes in the blood, or azotemia, is an early sign of kidney failure, usually occurring before other symptoms become evident. Urea is one of the first nitrogenous wastes to accumulate in the blood, and the BUN level becomes increasingly elevated as CKD progresses.*** Uremia, which literally means “urine in the blood,” is the term used to describe the clinical manifestations of kidney failure. Few symptoms of uremia appear until at least two thirds of the kidney’s nephrons have been destroyed. Uremia differs from azotemia, which merely indicates the accumulation of nitrogenous wastes in the blood and can occur without symptoms. Approximately 90% of potassium excretion is through the kidneys Hypertension and alterations in cardiovascular function Gastrointestinal disorders Neurologic complications Disorders of skin integrity Immunologic disorders Hemodialysis: • A hemodialysis system, or artificial kidney, consists of three parts: a blood delivery system, a dialyzer, and a dialysis fluid delivery system. *** Disorders of Water, Electrolyte, and Acid-Base Balance: • • • Sodium and water balance o The kidneys function in the regulation of extracellular fluid volume. Potassium balance o Approximately 90% of potassium excretion is through the kidneys. Acid–base balance o The kidneys normally regulate blood pH by eliminating hydrogen ions produced in metabolic processes and regenerating bicarbonate. Question: Which of the following alterations may affect drug efficacy in a patient with CKD? A. B. C. D. Loss of K+ Alteration in pH Loss of albumin Increased Ca2+ Rationale: Loss of albumin will result in altered drug metabolism via increased intermediates and faster action. Treatment of Renal Failure: • Medical Management o Dialysis • ▪ Hemodialysis ▪ Peritoneal dialysis o Transplantation Dietary Management ▪ The major component in the treatment of CKD is nutritional management. ** o Protein: ▪ Restriction of dietary proteins may decrease the progress of renal impairment in people with advanced renal disease. ▪ Proteins are broken down to form nitrogenous wastes, and reducing the amount of protein in the diet lowers the BUN and reduces symptoms. o Carbohydrates, fat, calories o Potassium o Sodium and fluid intake CKD in Elderly: • • Normal decrease in the GFR with age o Increased detrimental effects of nephrotoxic drugs Greater incidence of cerebrovascular, cardiovascular, and skeletal system effects Chapter 35 Structure of the bladder: • • Parts: o Fundus (body) o Neck (posterior urethra) Urine: o Passes from the kidneys to the bladder through the ureters ▪ Ureters: • Enter the bladder bilaterally at a location toward its base and close to the urethra ▪ Trigone: • The triangular area bounded by the ureters and the urethra *Detrusor Muscle is a network of smooth muscle fibers and helps with the process of micteration (peeing) Bladder: • • A muscle that is important to the bladder function is the external sphincter o A circular muscle composed of striated muscle fibers that surrounds the urethra distal to the base of the bladder Muscles in the bladder neck are sometime referred to as internal urethral sphincter o It’s a continuation of the detrusor muscle Three main levels of Neurologic Control of Bladder Function: • • • • Spinal cord reflex centers*** o The centers for reflex control of bladder functions are located in the sacral (S1-S4) and thoracolumbar (T11-L2) segments of the spinal cord. o The parasympathetic lower motor neurons (LMNs) for the detrusor muscle of the bladder are located in the sacral segments of the spinal cord; their axons travel to the bladder by way of the pelvic nerve. o LMNs for the external sphincter are also located in the sacral segments of the spinal cord. o These LMNs receive their control from the motor cortex through the corticospinal tract and send impulses to the external sphincter through the pudendal nerve. Innervation: o Pelvic nerve innervates detrusor. o Pudendal nerve o Hypogastric Micturition center in the pons Cortical and subcortical centers Question: is the following statement True or False? The micturition reflex involves both sympathetic and parasympathetic input. True: the reflex is both conscious and unconscious Storage and Emptying of Urine: • Micturition or the act of bladder emptying involves both sensory and motor functions associated with bladder emptying *** AND Drugs: • • Nicotinic (N) receptors are found in the synapses between the preganglionic and postganglionic neurons of the sympathetic and the parasympathetic system, as well as in the neuromuscular end plates of the striated muscle fibers of the external sphincter and pelvic muscles. Muscarinic (M) receptors are found in the postganglionic parasympathetic endings of the detrusor muscle Urine Tests and Studies: • • • Laboratory and Radiographic Studies o Urine tests and x-rays Urodynamic Studies Uroflowmetry o Cystometry o Urethral pressure profile o Sphincter electromyography o Ultrasound bladder scan Question: Increased PVR volumes is the result of ___? A. B. C. D. Hematuria Detrusor muscle weakness Infection Drug treatment B. Rationale: Detrusor muscle weakness results in decreased void pressure and therefore greater volume left in the bladder. Alteration in Bladder Function: • • Types: o o Causes o o Urinary obstruction with retention or stasis of urine Urinary incontinence with involuntary loss of urine Structural changes in the bladder, urethra, or surrounding organs Impairment of neurologic control of bladder function Signs of Outflow Obstruction and Urine Retention: • • • • • • • Bladder distention Hesitancy Straining when initiating urination Small and weak stream Frequency Feeling of incomplete bladder emptying Overflow incontinence Common causes of Neurogenic Bladder: • • • • • • • Stroke and advanced age Parkinson disease Spinal cord injury Injury to the sacral cord or spinal roots Radical pelvic surgery Diabetic neuropathies Multiple sclerosis Neurogenic Bladder Disorders: • • Spastic Bladder Dysfunction o Failure to store urine o Neurologic lesions above level of the sacral cord allow neurons in the micturition center to function reflexively without control from the CNS centers. Flaccid Bladder Dysfunction o Bladder emptying is impaired. o Neurologic disorders affect motor neurons in the sacral cord or peripheral nerves that control detrusor muscle contraction and bladder emptying. Treatments for Neurogenic Bladder Disorders: • • • • Catheterization Bladder retraining Pharmacologic manipulation Surgical procedures Question: Which of the following is not a cause of neurogenic bladder? A. B. C. D. Parkinson disease Spinal cord injury Alzheimer disease Injury to the sacral cord or spinal roots E. Radical pelvic surgery Rationale: Alzheimer disease is primarily a cognitive condition, not motor related. Types of Incontinence: • • • • Stress Incontinence o Involuntary loss of urine during coughing, laughing, sneezing, or lifting o Increases intra-abdominal pressure Urge Incontinence o Involuntary loss of urine associated with a strong desire to void (urgency) Overflow Incontinence o Involuntary loss of urine occurs when intravascular pressure exceeds the maximal urethral pressure because of bladder distention in the absence of detrusor activity Mixed Incontinence o Combination of stress and urge incontinence Diappers: • There are many neurologic conditions that predispose to urinary incontinence. The transient and often treatable causes of urinary incontinence in older adults may best be remembered with the acronym DIAPPERS: o D stands for dementia/dementias o I for infection (urinary or vaginal) o A for atrophic vaginitis o P for pharmaceutical agents o P for psychological causes o E for endocrine conditions (diabetes) o R for restricted mobility o S for stool impaction Bladder Cancer: • • Signs: o Increased frequency o Urgency o Dysuria o Hematuria Cancerous Lesion Types: o Superficial o Invasive Diagnosis Measures for Cancer of the Bladder: • • Cytologic studies Excretory urography • • • • • Cystoscopy Biopsy Ultrasonography CT scans MRI Treatment Methods for Bladder Cancer: • • • Treatment methods depend on o The cytologic grade of the tumor o The lesion’s degree of invasiveness Methods include o Surgical removal of the tumor o Radiation therapy o Chemotherapy