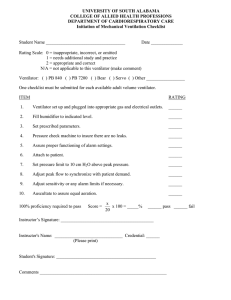
USER MANUAL LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04 (69) REV. 06 GMP CERTIFICATE ISO 9001:2008 ISO 13485:2003/EN ISO 13485:2012 1 de 88 LUNG VENTILATOR LEISTUNG LUFT 3 2 of 88 R 04-04(69) Rev. 06 LUNG VENTILATOR LEISTUNG LUFT 3 Manufacturing, Distribution and Technical Support by: LEISTUNG EQUIPAMENTOS LTDA. Street: 202, João Ropelatto City: Jaraguá do Sul – SC District: Nereu Ramos Zip Code: 89265-520 Phone: +55 47 3371-2741 Fax: +55 47 3371-9267 VAT No.: 04.187.384/0001-54 I.E.: 254.417.108 Op Auth.: GHL3983MX9H2 GMP Certificate ISO 13485:2003/EN ISO 13485:2012 ISO 9001:2008 Website: www.leistungbrasil.com E-mail: leistung@leistungbrasil.com Technical Responsible: Eng. Mateus Emrich Monnerat CREA/SC 088984-3 ANVISA registration: Technical name: Pressure and Volume Lung Ventilator Commercial name: Lung Ventilator Leistung Luft 3 ANVISA registration no.:: 80203470012 3 of 88 R 04-04(69) Rev. 06 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 CONTENTS CONTENTS .................................................................................................................................... 3 GUIDELINES AND LEISTUNG EQUIPAMENTOS LTDA.’S STATEMENT ON ELECTROMAGNETIC COMPATIBILITY (EMC) .................................................................................................................. 8 SIMBOLOGY ............................................................................................................................... 12 1 – MEANING OF THE STANDARDIZED SYMBOLS, PRINTED ON THE EQUIPMENT, INTERNAL AND EXTERNAL .............................................................................................................................................. 12 2 – MEANING OF THE STANDARDIZED SYMBOLS, PRINTED ON THE EQUIPMENT’S PACKING .............. 13 3 – MEANING OF THE SYMBOLS, PRINTED ON THE EQUIPMENT’S USER MANUAL ............................... 15 CHAPTER 1 - PRESENTATION ....................................................................................................... 16 WARNINGS, PRECAUTIONS AND NOTES................................................................................................ 19 WARNINGS ............................................................................................................................................ 19 PRECAUTIONS........................................................................................................................................ 20 NOTES .................................................................................................................................................... 21 CHAPTER 2 – INTRODUCTION ...................................................................................................... 22 VENTILATOR SPECIFICATIONS ............................................................................................................... 23 ELECTRONIC BLENDER OPERATION (AIR-O2 MIXER) .............................................................................. 29 FIO2 READING......................................................................................................................................... 29 CHAPTER 3 – ASSEMBLY AND CONNECTION ................................................................................ 30 EQUIPMENT ASSEMBLY ......................................................................................................................... 30 SCREEN CONNECTION ........................................................................................................................... 31 POWER SOURCE CONNECTION ............................................................................................................. 31 EQUIPMENT CONNECTION .................................................................................................................... 33 CONNECTION TO THE GAS SUPPLY SOURCE .......................................................................................... 33 BREATHING CIRCUIT .............................................................................................................................. 35 ARTICULATED ARM ASSEMBLY .............................................................................................................. 37 CHAPTER 4 – INSTRUCTIONS, CONTROLS AND ALARMS ............................................................... 37 INSTRUCTIONS OF USE .......................................................................................................................... 38 SCREEN CALIBRATION ........................................................................................................................... 38 TOUCH SCREEN CALIBRATION ............................................................................................................... 39 PATIENT PARAMETERS .......................................................................................................................... 41 CIRCUIT .................................................................................................................................................. 41 SELF-TEST............................................................................................................................................... 41 4 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 LAST PATIENT BUTTON .......................................................................................................................... 42 SCREEN .................................................................................................................................................. 42 ICON PANEL ........................................................................................................................................... 43 ALARMS AREA........................................................................................................................................ 44 INFORMATION AREA ............................................................................................................................. 44 OPERATIVE AREA ................................................................................................................................... 45 KIND OF TRIGGER .................................................................................................................................. 45 OPERATIVE INFORMATION.................................................................................................................... 45 SELECTION CONTROLS ........................................................................................................................... 45 STANDBY MODE .................................................................................................................................... 45 AIRWAY PRESSURE BAR (BARGRAPH) ................................................................................................... 46 DYNAMIC MONITORING AREA AND ALARMS ........................................................................................ 46 GRAPHICS AREA ..................................................................................................................................... 46 ÁDJUSTMENT AREA ............................................................................................................................... 47 WAVEFORMS ......................................................................................................................................... 47 SQUARE FLOW WAVEFORM (CONTÍNUOUS) ........................................................................................ 47 DESCENDING RAMP 50% FLOW WAVEFORM ........................................................................................ 48 DESCENDING RAMP FLOW WAVEFORM ............................................................................................... 48 ASCENDING RAMP FLOW WAVEFORM ................................................................................................. 48 SINUSOIDAL FLOW WAVEFORM (ROUND) ............................................................................................ 48 SENSIBILITY ............................................................................................................................................ 48 DIRECT ACCESS AREA ............................................................................................................................. 48 MAIN MENU AREA ................................................................................................................................. 50 VENTILATORY MODES ........................................................................................................................... 52 VOLUME CONTROLLED VENTILATION – (VCV)....................................................................................... 52 PRESSURE CONTROLLED VENTILATION – (PCV) ..................................................................................... 53 SUPPORT PRESSURE VENTILATION OR CONTINUOUS POSITIVE AIRWAY PRESSURE – (PSV/CPAP) ...... 53 SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION BY VOLUME WITH SUPPORT PRESSURE – SIMV (VCV)+PSV .................................................................................................................................... 53 SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION WITH SUPPORT PRESSURE – SIMV (PCV)+PSV .............................................................................................................................................. 54 PRESSURE REGULATED WITH VOLUME CONTROLLED – (PRVC) ............................................................ 54 NON-INVASIVE VENTILATION (NIV) ....................................................................................................... 54 MANDATORY MINUTE VENTILATION WITH PRESSURE – (MMV+PSV) .................................................. 54 BIPHASIC PRESSURE VENTILATION – (BIPHASIC) ................................................................................... 54 PRESSURE SUPPORT VENTILATION WITH ASSURED TIDAL VOLUME – (PSV+VT) .................................. 54 NEONATAL VENTILATORY MODES......................................................................................................... 55 CONTINUOUS FLOW .............................................................................................................................. 55 NASAL CPAP ........................................................................................................................................... 55 HFNC – HIGH FLOW NASAL CANNULA ................................................................................................... 55 BACKUP VENTILATION ........................................................................................................................... 55 LUNG MECHANICS ................................................................................................................................. 56 GRAPHICS .............................................................................................................................................. 59 REMOTE MONITORING ......................................................................................................................... 61 FUNCTIONAL SETUP .............................................................................................................................. 61 OPERATIVE SETUP ................................................................................................................................. 62 CHAPTER 5 - ALARMS.................................................................................................................. 63 5 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 ALARM AUDIO INHIBITION (SILENCE) .................................................................................................... 63 HIGH PRIORITY ALARM CONDITION ...................................................................................................... 64 1 - MICROPROCESSOR ........................................................................................................................... 64 2 – LOW GAS SUPPLY PRESSURE ............................................................................................................ 64 3 – LOW BATTERY .................................................................................................................................. 64 4 – MAXIMUM INSPIRATORY PRESSURE ............................................................................................... 64 5 - INTERRUPTED CYCLE ALARM ............................................................................................................ 64 6 - MINIMUM INSPIRATORY PRESSURE ................................................................................................. 64 7 – DISCONNECTION OF THE PATIENT CIRCUIT ..................................................................................... 65 8 – DISCONNECTION OF THE PROXIMAL FLOW SENSOR ....................................................................... 65 9 – HIGH PRESSURE OF SUPPLY GASES .................................................................................................. 65 MEDIUM PRIORITY ALARM CONDITION ................................................................................................ 65 10 – MINIMUM FIO2 .............................................................................................................................. 65 11 – MAXIMUM FIO2.............................................................................................................................. 65 12 - APNEA ALARM ................................................................................................................................ 65 13 – MINIMUM TIDAL VOLUME ............................................................................................................ 66 14 – MAXIMUM RESPIRATORY FREQUENCY.......................................................................................... 66 15 – MINIMUM RESPIRATORY FREQUENCY .......................................................................................... 66 16 – POWER OUTAGE ............................................................................................................................ 66 LOW PRIORITY ALARM CONDITION ....................................................................................................... 66 17 - MAXIMUM TIDAL VOLUME ............................................................................................................ 66 18 - I:E RATIO INVERSION ...................................................................................................................... 66 19 – PEEP ALARM................................................................................................................................... 66 20 – MINIMUM MINUTE VOLUME ........................................................................................................ 67 21 - MAXIMUM MINUTE VOLUME ........................................................................................................ 67 COLORS AND MEANINGS OF THE LUMINOUS INDICATIONS ................................................................. 71 SETUP OF THE ALARMS, SOUND AND LUMINOUS SIGNALS ON THE SCREEN ........................................ 71 CHAPTER 6 – EXHALATION VALVE, PATIENT CIRCUIT AND PROXIMAL SENSOR.............................. 73 EXHALATION VALVE............................................................................................................................... 73 PATIENT CIRCUIT ................................................................................................................................... 74 PROXIMAL SENSOR................................................................................................................................ 74 CHAPTER 7 – CLEANING, DISINFECTION AND STERILIZATION ........................................................ 76 DISASSEMBLY OF THE EXHALATION VALVE AND THE PATIENT CIRCUIT ................................................ 76 CLEANING .............................................................................................................................................. 77 DRYING .................................................................................................................................................. 77 STERILIZATION ....................................................................................................................................... 78 PHYSICAL METHOD................................................................................................................................ 78 USEFUL LIFE OF ACCESSORIES ............................................................................................................... 79 ANNEX 1 – VENTILATOR LUFT3’S ACCESSORIES ............................................................................ 80 OPTIONAL ACCESSORIES (NOT INCLUDED WITH THE EQUIPMENT) ...................................................... 83 6 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 ANNEX 2 – PREVENTIVE MAINTENANCE ...................................................................................... 84 ANNEX 3 – BLOCK DIAGRAM ....................................................................................................... 86 ANNEX 4 – WARRANTY ............................................................................................................... 87 ANNEX 5 – GLOSSARY ................................................................................................................. 88 7 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 GUIDELINES AND LEISTUNG EQUIPAMENTOS LTDA.’S STATEMENT ON ELECTROMAGNETIC COMPATIBILITY (EMC) Guidelines and Manufacturer’s Statement – Electromagnetic Emission The Lung Ventilator Luft 3 is designated for use in electromagnetic environments as specified below. It is recommended that the user or client of the Lung Ventilator Luft 3 ensures that the equipment is being used in such environment. Compliance Electromagnetic Environments – Guidelines RF Emissions ABNT NBR IEC CISPR11 Group 1 The Lung Ventilator Luft 3 utilizes RF energy only for its internal functions. However, its RF emissions are very low and it is not likely to cause any interference on nearby electronic equipment. RF Emissions ABNT NBR IEC CISPR11 Class A Harmonic Emissions IEC 61000-3-2 Class A Emission Tests Emissions due to fluctuation of the voltage/flickering IEC 61000-3-3 Complies The Lung Ventilator Luft 3 is suitable for use in al lestablishments other than domestic, and may be used in domestic establishments and those directly connected to the public low-voltage power supply network that supplies buildings used for domestic purposes, provided the following warning is heeded: Warning: This equipment is designated for use only by healthcare professionals. This equipment may cause radiointerference or interrupt the operation of nearby equipment. It may be necessary to adopt mitigation procedures, such as reorientation or reallocation of the Lung Ventilator Luft 3, or the blindage of the place. IN ORDER TO AVOID RF INTERFERENCE, THE LUNG VENTILATOR LUFT 3 SHALL NOT BE USED WHEN STACKED OVER OTHER EQUIPMENT. IN CASE THAT IS NEEDED, IT IS RECOMMENDED TO OBSERVE THE NORMAL USE OF THE EQUIPMENT. 8 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Guidelines and Manufacturer’s Statement – Electromagnetic Immunity The Lung Ventilator Luft 3 is designated for use in electromagnetic environments as specified below. It is recommended that the user or client of the Lung Ventilator Luft 3 ensures that the equipment is used in such environment.. Electromagnetic environment Emission tests Test Level ABNT Level of Guidelines NBR IEC 60601 Compliance Electrostatic discharges (ESD) ± 6 kV by contact ± 8 kV by air IEC 61000-4-2 Fast transient burst / Pulse train (“Burst”) ± 2 kV at supply lines IEC 61000-4-4 ± 1kV at input/output lines Surges ± 1 kV line(s) to line(s) IEC 61000-4-5 ± 2 kV line(s) to ground < 5% Ut (> 95% voltage drop in Ut) per 0.5 cycles. ± 6 kV by contact ± 8 kV by air ± 2 kV at supply lines ± 1kV at input/output lines ± 1 kV line(s) to line(s) ± 2 kV line(s) to ground < 5% Ut Floors should be wooden, concrete or ceramic. If the floor is covered by synthetic material, the relative humidity shall be of at least 30%. The quality of the power supply should be that of a typical commercial or hospital environment. The quality of the power supply should be that of a typical commercial or hospital environment. (> 95% voltage drop in Ut) per 0.5 cycles. 40% Ut 40% Ut Power outage, short interruptions and voltage variations on the power supply input lines. IEC 61000-4-11 (60% voltage drop in Ut) per 5 cycles (60% voltage drop in Ut) per 5 cycles 70% Ut 70% Ut (30% voltage drop in Ut) per 25 cycles. (30% voltage drop in Ut) per 25 cycles. Quality of the power supply should be that of a typical commercial or hospital environment. If the user of the Lung Ventilator Luft 3 requires continuous operation during power interruption, it is recommended that the Lung Ventilator Luft 3 is supplied by an uninterrupted power supply or a battery. < 5% Ut < 5% Ut (> 95% voltage drop in Ut) per 5 seconds. Magnetic fields at the power supply frequency IEC 61000-4-8 3A/m (> 95% voltage drop in Ut) per 5 seconds. 3A/m Magnetic fields on the supply frequency should be at levels characteristic of a typical hospital or commercial environment. Ut IS THE POWER SUPPLY VOLTAGE ALTERNATED BEFORE THE APPLICATION OF THE TEST LEVEL. 9 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Guidelines and Manufacturer’s Statement – Electromagnetic Immunity The Lung Ventilator Luft 3 is designated for use in electromagnetic environments as specified below. It is recommended that the user or client of the Lung Ventilator Luft 3 ensures that the equipment is being used in such environment. Immunity tests Test level ABNT NBR IEC 60601 Level of Compliance Electromagnetic environment Guidelines Portable and Mobile RF equipment should not be used close to any part of the Lung Ventilator Luft 3, including cables, from a separation distance lower than the recommendation, calculated out of the applicable equation for the transmitter's frequency. RF Conducted 3 Vrms IEC 61000-4-6 150 kHz to 80 MHz out of ISM bandsa Recommended separation distance: d= 1,17 [ P ] ½ 3V d= 1,20 [ P ] ½ 10 Vrms Radiated RF IEC 61000-4-3 150 kHz to 80 MHz out of ISM bandsa 10 V d=1,20 [ P ] ½ 80 MHz até 800 MHz 10 V/m 80 MHz up to 2,5 GHz 10 V/m d= 2,30 [ P ] ½ 800 MHz até 2,5 GHz where P is the maximum nominal power output of the transmitter in watts (W), according to the transmitter's manufacturer, and d is the separation distance recommended in meters (m). It is recommended that the field intensity established by the RF transmitter, as determined through an electromagnetic inspection on the placeC is lower than the compliance level in each frequency band D. Interference may occur around the equipment marked with this symbol: NOTE 1 At 80 MHz and 800 MHz, the highest frequency band is applied. NOTE 2 These guidelines may not be applicable in every situation. The electromagnetic propagation is affected by the absorption and reflection of structures, objects and people. A In the ISM (Industrial, Scientific and Medical) frequency bands between 150 kHz and 80 MHz are 6.765 MHz up to 6.795 MHz; 13.553 MHz up to 13.567 MHz; 26.957MHz up to 27.283 MHz and 40.66 MHz up to 40.70 MHz. B The compliance levels on the ISM frequency bands between 150 kHz and 80 MHz and the frequency range between 80 MHz up to 2,5 GHz are intended to reduce the probabibly that the mobile and portable communication devices cause interference if inadvertly brought to the patient’s environment. For this reason an additional factor of 10/3 is used to calculate the recommended separation distance for transmitters in this frequency range. C The field intensities established by fixed transmitters, such as base radio stations, phones (cellular / wireless), portable ground radios, amateur radios, AM and FM transmission and TV transmission cannot be theoretically predicted with accuracy. To asses the electromagnetic environment due to fixed RF transmitters, it is recommended to consider an electromagnetic inspection of the place. If the field intensity measure at the place in which the Lung Ventilator Luft 3 is used exceeds the level of compliance used above, the Lung Ventilator Luft 3 should be observed to verify if the operation is regular. If an abnormal performance is detected, additional procedures may be necessary, such as reorienting or reallocation of the Lung Ventilator Lut 3. D Over the frequency range of 150 kHz up to 80 MHz, the field intensity must be lower than 3 V/m. 10 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Recommended separation distance between the portable and mobile RF equipment and the Lung Ventilator Luft 3 The Lung Ventilator Luft 3 is intended for use in electromagnetic environments in which irradiated RF disturbances are controlled. The client or customer of the Lung Ventilator Luft 3 may help preventing electromagnetic interferences by keeping a minimum distance between the portable or mobile RF communication equipment (transmitters) and the Lung Ventilator Luft 3 as recommended below, according to the maximum communication equipment's output power. Separation distance according to the transmitter's frequency (meters) m 150 kHz up to 80 MHz out of ISM Bands 150 kHz up to 80 MHz in the ISM Bands 80 MHz up to 800 MHz 800 MHz up to 2,5GHz d= 1,17 [ P ] ½ d= 1,20 [ P ] ½ d= 1,20 [ P ] ½ d= 2,30 [ P ] ½ 0,01 0,12 0,12 0,12 0,23 0,1 0,37 0,37 0,37 0,72 1 1,17 1,20 1,20 2,30 10 3,70 3,79 3,79 7,27 100 11,70 12,00 12,00 23,00 Transmitter's maximum nominal output power W For transmitters with a nominal output power which is not listed above, the recommended separation distance d in meters (m) may be determined by using the applicable equation of the transmitter's frequency, where P is the transmitter's maximum nominal output power in watts (W), according to the transmitter's manufacturer. NOTE 1 In 80 MHz and 800 MHz, the separation distance is applied to the higher frequency range. NOTE 2 In the ISM (Industrial, Scientific and Medical) frequency bands between 150 kHz and 80 MHz are 6.765 MHz up to 6.795 MHz; 13.553 MHz up to 13.567 MHz; 26.957MHz up to 27.283 MHz and 40.66 MHz up to 40.70 MHz. NOTE 3 An additional factor of 10/3 is used to calculate the recommended separation distance for transmitters in the ISM frequency bands between 150 kHz and 80 MHz and on the frequency range of 80 MHz up to 2.5 GHz to reduce the probability of interference that mobile communication equipment may cause if inadvertently taken into patient areas. NOTE 4 These guidelines may not apply in all situations. Electromagnetic propagation is affected by the absorption and reflection of structures, objects and people. 11 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 SIMBOLOGY 1 – MEANING OF THE STANDARDIZED SYMBOLS, PRINTED ON THE EQUIPMENT, INTERNAL AND EXTERNAL Symbol Standard/Norm Description IEC 60417-5032 Alternating Current IEC 60417-5031 Direct Current IEC 60417-5017 Functional Ground Terminal IEC 60417-5019 Protective Ground Terminal ISO 7000-0434A Attention! Consult the documents IEC 60417-5264 Connected (Connection to Internal or External Power Source) IEC 60417-5265 Disconnected (Disconnection to Internal or External Power Source) IEC 60417-5840 Type B Equipment IEC 60878 ISO 3864-B.3.6a Risk of Electrical Shock IEC 60417-5016 Fuse ISO 7010-M002 Consult Instructions of Use 12 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 2 – MEANING OF THE STANDARDIZED SYMBOLS, PRINTED ON THE EQUIPMENT’S PACKING Symbol Standard Description ISO 780:1997 (E) No. 1 FRAGILE Handle carefully ISO 780:1997 (E) No. 3 THIS SIDE UP Indicate the position of the package’s up side ISO 780:1997 (E) No. 4 PROTECT FROM SUNLIGHT The package must be kept out of sunlight ISO 780:1997 (E) No. 6 PROTECT AGAINST RAIN The package must be kept out of rain ISO 780:1997 (E) No. 14 MAXIMUM STACKING UP Indicates the maximum number of packages that can be stacked up for transport and storage ISO 780:1997 (E) No. 2 DO NOT USE HOOKS 13 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 ISO 780:1997 (E) No. 8 DO NOT ROLL THE PACKAGE ISO 780:1997 (E) No. 17 TEMPERATURE LIMIT Indicates the limit temperature for stocking and handling the package 14 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 3 – MEANING OF THE SYMBOLS, PRINTED ON THE EQUIPMENT’S USER MANUAL Symbol Standard Description IEC 60878 ISO 3864-B.3.6a RISK OF ELECTRICAL SHOCK ISO 7010-W001 ISO 7000-0434A -------------------- WARNING! Condition before which there is a possibility of production damage to the operator or others. ATTENTION! Condition before which there is the possibility of damaging the equipment, its accessories or others. NOTE Specifies important observations which need to be considered for a correct use of the equipment. MANUFACTURER EN 980 15 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 CHAPTER 1 - PRESENTATION In the User Manual the necessary information for the correct use of the LUFT 3 ventilator are presented. The indicators related to the application and the regulation, mentioned in this manual, are for orientation only. The physician shall adapt it, according to his/her own criteria, to the patient's need. GENERAL MODEL ANVISA Registry Luft 3 No: 80203470012 MEDICAL DEVICE CLASSIFICATION OPERATION MODE Classification according to the type against electrical shock (Isolation). Classification according to the type of protection against electrical shock. Level of protection against harmful water penetration CLASS III Continuous Operation CLASS I Internally Energized Device TYPE B IP22 EQUIPMENT not suitable to use near an ANESTHETIC MIXTURE THAT IS FLAMMABLE WITH AIR, OXYGEN (O2) or NITROUS OXIDE (NO2). PHYSICAL CHARACTERISTICS Dimensions PARAMETERS VALUES Height 1.473 mm Width 550 mm Depth 530 mm Equipment’s Weight 28,0 Kg Case’s Weight 10,0 Kg Monitor’s Weight 5,4 Kg Trolley’s Weight 12,6 Kg EXTERNAL POWER SUPPLY VOLTAGE – CURRENT 100V – 240V ~ 0,6A – 0,29A FREQUENCY 47 to 63 Hz. POWER 70 VA 250V ~ 2,0A 20mm SB (Slow) FUSE INTERNAL POWER SUPPLY Battery Commutation Voltages lower than 90 Vac. Nominal Voltage 10,8V ~ 11,1V Nominal Capacity Type Autonomy 13,2Ah Lithium battery (Li+) Complete Battery Charge 360 minutes autonomy 77ºF (25ºC) Working Temperature Range Discharge -20ºC ~ +60ºC Charge 0ºC ~ +45ºC 16 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Storage -20ºC ~ +60ºC Nominal Working Temperature +25ºC ± 3ºC Voltage Fluctuation 12,6 Vdc to 25°C Lifespan 300 to 500 cycles Charging Time 15 hours Partial charge time 4 hours (for 2 hours of autonomy) TOTAL AUTONOMY IS GUARANTEED FOR SPECIFIC CONDITIONS OF POWER CONSUMPTION. THE PARTIAL CHARGE TIME WAS CONSIDERED WITH THE BATTERY PARTIALLY DISCHARGED AND ASSESSED THE CHARGE TIME NECESSARY TO RETAKE MORE THAN 2 HOURS OF AUTONOMY. TO TEST THE BATTERY YOU MUST CYCLE THE EQUIPMENT OPERATING ON THE BATTERY FOR 5 MINUTES AND CHECK THE SYMBOL THAT INDICATES THE BATTERY CHARGE LEVEL. IN CASE THE COLOR IS GREEN OR YELLOW, THE BATTERY IS IN GOOD CONDITIONS OF USE. SPECIFICATIONS INFORMED BY THE MANUFACTURER. INTERNAL BATTERY AND FUSE ARE NOT REPLACEABLE BY THE OPERATOR. RISK OF ELECTRICAL SHOCK. THE CASE MUST BE REMOVED ONLY BY QUALIFIED PERSONNEL. THE SWITCHING FOR THE INTERNAL BATTERY HAPPENS AUTOMATICALLY, WITHOUT EXTERNAL INTERVENTION. IT DOES NOT INTERFERE THE EQUIPMENT'S OPERATION, BUT TRIGGERS AN ALARM AS EXPLAINED ON CHAPTER 5 - ALARMS. WHENEVER THE EQUIPMENT IS CONNECTED TO THE EXTERNAL ELECTRICAL SOURCE THE BATTERY IS RECHARGING. ELECTRICAL OUTPUT FOR THE MONITOR VOLTAGE – CURRENT 12 V 5A POWER 60 VA THE OUTPUT CURRENT FOR THE DISPLAY IS LIMITED IN 5A BY THE POWER SUPPLY'S OVERLOAD FUNCTION, WHICH ALSO PROTECTS THIS PLUG AGAINST ELECTRICAL DEAD-SHORTS AND OVERHEATING. PNEUMATIC INPUTS OXYGEN (O2) DISS 9/16” – 18 input AIR DISS 3/4” – 16 input PRESSURE 250 – 700 kPa (2,5 - 7 bar) FLOW Up to 180 L/min USE ONLY MEDICAL GRADE GASES. ALWAYS USE THE FILTER FOR THE COMPRESSED AIR NETWORK. 17 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 ENVIRONMENTAL SPECIFICATIONS R 04-04(69) Rev. 06 VALUES +10ºC to 35ºC +2ºC to 40ºC (*) 10% to 95% Operation Non condensable Relative Humidity 0% to 95% Storage - Transport Non condensable Operation 40 – 100 kPa Atmospheric Pressure Storage - Transport 40 – 100 kPa THE VOLUME AND PRESSURE MEASURES ARE STANDARIZED BY THE BAROMETRIC PRESSURE AT SEA LEVEL (BTPS) AND THEY ARE COMPENSATED IN FUNCTION OF THE ALTITUDE. Environment Temperature Operation Storage - Transport (*) THE VENTILATOR'S STORAGE FOR LONG PERIODS AT TEMPERATURES HIGHER THAN 27ºC OR WITHOUT ELECTRICAL CONNECTION FOR PERIODS LONGER THAN TWO MONTHS MAY AFFECT THE INTERNAL BATTERY'S LIFESPAN. IN CASE OF STORAGE OF THE VENTILATOR FOR LONG PERIODS, IT IS RECOMMENDED TO REMOVE THE INTERNAL BATTERY IN ORDER TO AVOID LEAKAGES. REQUEST AUTHORIZED TECHNICAL SUPPORT'S SUPPORT. THE EQUIPMENT LUFT3 COMPLIES WITH THE FOLLOWING STANDARDS: ABNT NBR IEC 60601-1 – Electromedical equipment – Part 1: General safety prescriptions. ABNT NBR IEC 60601-1-2 – Electromedical equipment - Part 1-2: General requirements for basic safety and essential performance – Collateral standard: Electromagnetic compatibility – requirements and assay. ABNT NBR IEC 60601-1-4 - Electromedical equipment - Part 1-4: General safety prescriptions - Collateral standard: Programmable electromedical systems. ABNT NBR IEC 60601-1-8 - Electromedical equipment - Part 1-8: General requirements for basic safety and essential performance - Collateral standard: General requirements, assays and guidelines for alarm systems in electromedical equipment and electromedical systems. ABNT NBR IEC 60601-2-12 - Electromedical equipment - Part 2-12: Particular prescriptions for lung ventilator safety – Critical care ventilators. 18 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 WARNINGS, PRECAUTIONS AND NOTES WARNINGS TO AVOID THE RISK OF ELECTRICAL SHOCK, THIS EQUIPMENT SHALL BE CONNECTED ONLY TO ONE SOURCE OF POWER SUPPLY WITH PROTECTIVE GROUNDING. CONSTANT ATTENTION OF SPECIALIZED PERSONNEL IS REQUIRED WHENEVER THE PATIENT IS CONNECTED. WHENEVER THE EQUIPMENT IS IN USE, AN ALTERNATIVE WAY OF VENTILATION MUST BE AVAILABLE. OPERATIONAL PROBLEMS REQUIRE IMMEDIATE CORRECTIVE ACTION. THE ALARMS DO NOT IMPLY TOTAL SAFETY IN CASE OF A DEFECT IN THE EQUIPMENT. THE PROFESSIONAL IN CHARGE OF ITS USE SHALL, ACCORDING TO HIS/HER OWN CRITERION AND KNOWLEDGE, USE THE EQUIPMENT ACCORDING TO THE NEEDS OF THE PATIENT. DO NOT USE ANTI-STATIC TUBES NOR ELECTRICAL CONDUCTORS IN THE PATIENT CIRCUIT. DO NOT STERILIZE THE EQUIPMENT WITH ETHYLENE OXIDE. THERE IS A HIGH PROBABILITY TO OCCUR IRREVERSIBLE DAMAGE IN THE VENTILATOR COMPONENTS. THE EQUIPMENT MUST BE CONNECTED TO AC VOLTAGE WITH PROTECTIVE GROUND CONNECTION. THE EQUIPMENT MAY BE AFFECTED BY HIGH FREQUENCY ELECTROMAGNETIC INTERFERENCE (SUCH AS CELLULAR, WIRELESS TELEPHONE, DEFIBRILLATORS, ELECTRO-SURGICAL KNIVES, MAGNETIC RESONANCE, ETC.). USE LAST CHAPTER'S TABLE OF EMISSION GUIDELINES AND ELECTROMAGNETIC IMMUNITY TO DETERMINE THE CORRECT SEPARATION DISTANCE. THE USE OF ACCESSORIES AND CABLES OTHER THAN THE SPECIFIED, WITH EXCEPTION TO THE ONES FURNISHED BY LEISTUNG AS SPARE PARTS FOR INTERNAL COMPONENTS, MAY RESULT IN AN INCREASE OF THE EMISSION OR THE REDUCTION OF THE LUFT 3's IMMUNITY. BEFORE THE FIRST UTILIZATION AND AFTER THE UTILIZATION IN EACH PATIENT, IT IS NECESSARY TO CLEAN THE VENTILATOR. TO STERILIZE THE ACCESSORIES, FOLLOW THE INSTRUCTIONS ON CHAPTER 7 – . 19 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 DANGER OF ELECTRICAL SHOCK: NEVER DISASSEMBLE THE CASE OF THE EQUIPMENT. IN THE EVENT OF PROBLEMS OF DIFFICULTIES, CONTACT AN AUTHORIZED TECHNICAL SERVICE. THE EQUIPMENT MUST BE SUPPLIED BY BATTERY WHEN THERE IS DOUBT ABOUT THE INTEGRITY OF THE GROUND CONNECTOR, TAKING CARE NOT TO EXCEED THE BATTERY LIFE. ONLY CONNECT TO THE EQUIPMENT ITEMS WHICH ARE SPECIFIED AS BEING PART OF LUFT 3 OR WHICH ARE COMPATIBLE. THE COMPANY RESPONSIBLE FOR THE EQUIPMENT SHALL DO ALL THE SPECIFIED PROCEDURES OF CLEANING, STERILIZATION AND DISINFECTION. THE COMPANY RESPONSIBLE FOR THE EQUIPMENT SHALL ASSURE THAT THE ASSEMBLY OF THE LUFT 3 AND ANY MODIFICATION DURING ITS WORKING TIME WILL FOLLOW THE EVALUATION REQUIREMENTS OF THE RULE NBR IEC 60601-1: 2010. NO CHANGE IN THIS EQUIPMENT IS ALLOWED. PRECAUTIONS IN CASE OF FAILURE OF ELECTRICAL SUPPLY OR INPUT GAS, THE VENTILATOR ENABLES SPONTANEOUS VENTILATION. THE RESISTANCE OF THE EXPIRATION BRANCH WITH THE EQUIPMENT WITHOUT SUPPLY IS 3.0 cmH2O/L/s AT 30 L/min. AND 3.2 cmH2O/L/s AT 60 L/min. THE RESISTANCE OF THE INSPIRATION BRANCH IS LOWER THAN 5 cmH2O/L/s AT 60 L/min. DURING THE WARRANTY PERIOD, THE PERMANENCE OR MOVEMENT OF THE EQUIPMENT SHALL BE PERFORMED WITH ITS ORIGINAL PACKAGING, WITH ITS CORRESPONDING INTERNAL PROTECTION; OTHERWISE IT WILL RESULT IN LOSS OF THE WARRANTY. NEVER STERILIZE THE VENTILATOR. THE INTERNAL COMPONENTS ARE NOT COMPATIBLE WITH THE STERILIZATION TECHNIQUES. FOLLOW THE INSTRUCTIONS FOR THE EQUIPMENT CLEANING AND COMPONENTS STERILIZATION AS SHOWN ON CHAPTER 7 – OF THIS MANUAL. NEVER OPERATE THE EQUIPMENT EXPOSED TO DIRECT HEAT OR SUNLIGHT. NEVER COVER OR POSITION THE EQUIPMENT IN A WAY THAT BLOCKS THE AIR ENTRY FOR COOLING. 20 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 TO ENSURE THE ELECTRICAL PROTECTION AND TO AVOID RISK OF FIRE, NEVER CHANGE THE FUSE. IN CASE THE EQUIPMENT STOPS WORKING, CONTACT THE AUTHORIZED TECHNICAL SERVICE. THE IMPROPER REPLACEMENT OF FUSES NULLIFIES THE WARRANTY AND REPRESENTS A RISK FOR THE OPERATION OF THE EQUIPMENT, THE SAFETY OF THE OPERATOR AND THE PATIENT. NOTES THE VENTILATOR IS A MEDICAL EQUIPMENT AND SHALL BE OPERATED BY A QUALIFIED AND TRAINED PROFESSIONAL, UNDER THE DIRECT SUPERVISION OF A PHYSICIAN. BY THE END OF THE EQUIPMENT'S LIFETIME, DO NOT DISCARD ITS COMPONENTS IN REGULAR TRASH CANS. FOR THAT, CONTACT: WWW.LEISTUNGBRASIL.COM. ELECTRIC DIAGRAMS, CIRCUIT DIAGRAMS, COMPONENT LISTS, DESCRIPTIONS, CALIBRATION INSTRUCTIONS, AS WELL AS TRAININGS CAN BE PROVIDED BY LEISTUNG EQUIPAMENTOS LTDA. BY AN AGREEMENT BETWEEN THE PARTS. LEISTUNG EQUIPAMENTOS LTDA. IS A COMPANY OF CONTINUOUS IMPROVING IN ITS PRODUCTS, AND TECHNICAL SPECIFICATIONS MAY CHANGE WITHOUT PREVIOUS NOTICE. IN CASE YOU FACE ANY MALFUNCTION, PLEASE COMMUNICATE LEISTUNG EQUIPAMENTOS LTDA.'s TECHNICAL SERVICE. THE COMPANY RESPONSIBLE FOR THE EQUIPMENT IS THE ENTITY WHICH LEGALLY AND MORALLY RESPONDS FOR THE USE AND MAINTENANCE OF THE LUNG VENTILATOR LUFT 3. THIS ENTITY MAY BE, FOR EXAMPLE, A HOSPITAL AND A PHYSICIAN OR A LEGAL PERSON. THE COMPANY RESPONSIBLE FOR THE EQUIPMENT IS THE ENTITY WHICH LEGALLY AND MORALLY RESPONDS FOR THE USE AND MAINTENANCE OF THE LUNG VENTILATOR LUFT 3. THIS ENTITY MAY BE, FOR EXAMPLE, A HOSPITAL AND A PHYSICIAN OR A LEGAL PERSON. 21 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 CHAPTER 2 – INTRODUCTION The ventilator LUFT 3 was developed to be among the most complete lung ventilators in the market, the equipment LUFT 3 features a 17” screen which allows adjustment of inclination and rotation with resistive touch screen panel displaying an image of 800x600 pixels in a useful image area of 335 cm x 270 cm, showing an intuitive and user-friendly interface of easy operation, offering quick and safe ajudstment for each ventilatory parameters, as well as it offers a pleasing operation for the professional and allows more attention towards the patient. The LUFT 3 provides all necessary ventilation modes for therapies in Adult, Pediatric and Noenatal patients, besides an advanced lung mechanics menu for the correct diagnosis, offering high quality ventilation adapted for each patient, able to be used on the most complex and demanding therapies, ventilating from premature neonatal patients (0,3kg) to patients with morbid obesity (>300kg) in an efficient and reliable way. The ventilator consists of a flexible breathing circuit, a controlling system, a gas source, the monitor and the alarms. The controlling system (microcontroller) regulates the pressure, the volume and the positive pressure respiration flow delivered to the patient, as well as the fraction of inbreathed oxygen (FiO2) based on the value of the selected control variables. The sensors disposed within the ventilator and within the breathing circuit are able to measure the pressure or flow in the airway and provide feedback so that it automatically adjusts its output. The communication interface allows the user to know and to configure the information of the control parameters, variables of the monitoring and condition of the alarms. The Touch Screen technology enables a great ease of handling which allows the operator access to all parameters of the equipment quickly, accurately and securely, making the work of the professional nice and smooth, allowing the same to focus on the patient treatment. The equipment has an operating system with preset or custom settings. The alarm system has warnings and reminders, clear and oriented to help in the safe decision-making of the professional. The equipment power may be sourced both from the electrical network and from the internal battery. The internal battery's power shall be used for short-term ventilations or during failures of the electrical network. The ventilator receives gases (Air and O2) from the room's medical gas network whose flow to the patient may be regulated by flow control valves, in order to reach the FiO2 you want provide to the patient, the air and oxygen are internally mixed. The gas mixture is delivered to the patient through a flexible breathing circuit consisting of two branches of corrugated silicone tracheas and a system for quick and safe interconnection, which prevents any possibility of error. It also includes a default parameters configuration which ensures a fast and safe ventilation start, therefore avoiding the self-cycling and allowing a patient recovery without major interferences . Pulmonary insufflation during mechanical ventilation occurs when a flow of air is applied in the airway this additional pressure increases the intrapulmonary pressure and produces a transpulmonary pressure gradient between the alveoli and the pleural space. The control of the inspiratory and expiratory phase is performed through the exhalation valve which operates actively. The ventilator LUFT 3 is designated to ventilate by positive pressure adult, pediatric and neonatal patients. It is intended to operate in hospital environments, more specifically Intensive Care Units (ICU) with proper electrical installations and proper medical gases installations. The equipment is not intended to be used in transportation outside the hospital nor homecare. It shall be used only by trained personnel and under the supervision of healthcare professionals. The device may be used in invasive mode as well as non-invasive mode. However, LEISTUNG EQUIPAMENTOS excludes from its production and commercialization process endotracheal and tracheostomy tubes, facial and endonasal masks, suction probes, etc. 22 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Contraindications for the use The application of mechanical ventilation is associated to the possibility of emerging complications. The knowledge of them is responsibility of the professional in charge of the equipment and exceeds the level of information contained in this manual. VENTILATOR SPECIFICATIONS LUFT 3 CONFIGURATIONS Adult – Pediatric – Neonatal Adult – Pediatric Pediatric – Neonatal VENTILATION MODES PATIENT TYPE VENTILATION VOLUME CONTROLLED (VCV) ASSISTED / CONTROLLED PRESSURE CONTROLLED (PCV) PRESSURE REGULATED VOLUME CONTROL (PRVC) PRESSURE SUPPORT (PSV) ADULT CONTINUOUS POSITIVE PRESSURE (CPAP) SPONTANEOUS AND NON INVASIVE (NIV) PEDIATRIC HFNC – HIGH FLOW NASAL CANNULA SIMV (VCV) + PSV SIMV (PCV) + PSV VARIÁBLES MINUTE (MMV) + PSV PSV + ASSURED TIDAL VOLUME BIPHASIC PRESSURE (APRV+PSV) NEONATAL ASSISTED / VOLUME CONTROLLED (VCV) CONTROLLED PRESSURE CONTROLLED (PCV) 23 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 CONTINUOUS FLOW PRESSURE SUPPORT (PSV) CPAP SPONTANEOUS Nasal CPAP HFNC – HIGH FLOW NASAL CANNULA VARIÁBLES SIMV (PCV) + PSV SPECIFICATIONS Backup Ventilation Emergency Ventilation FIO2: Inspiratory Time I:E Ratio Frequency Tidal Volume Minute Volume Sensibility Pressure Controlled (PCV) Pressure Support (PSV) Inspiratory Pressure Rise Time Expiratory Sensibility Apnea Time PEEP / CPAP Nebulization TGI Inspiratory Flow Base Flow Expiratory Flow Sigh (VCV mode) AUTOMATIC Inspiratory Pause (VCV mode) Manual Inspiratory Pause Manual Expiratory Pause O2 100% PCV or VCV in adult, pediatric and neonatal In all ventilation modes 21 to 100% 0,1 to 30,0 seconds 5:1 - 1:99 1 - 180 R.P.M. 2,0 to 2500 ml 0,01 to 25,0 l BY FLOW: 0,2 to 15 L/min BY PRESSURE: -0,2 to -15,0 cm H2O (compensated PEEP) 1 to 80 cm H2O over PEEP (with adjustable “Rise Time”) 0 to 80 cm H2O over PEEP (with adjustable “Rise Time”) -10 to 120 cmH2O 6 levels Adjustable from 5 to 80% of the initial flow 5 to 60 seconds 0 to 50 cm H2O 1 to 20 min. synchronized with the inspiratory phase and with automatic compensation of the insp. volume and FiO 2 Synchronized with the expiratory phase On VCV: Automatic adjustment from 0 to 200 L/min. On PCV e PSV: from 0 to 200 L/min. Continuous flow on neonatal: 2 to 15 L/min. Inspiratory flow on neonatal: 0 to 30 L/min. Maximum flow in any mode of 250 L/min. Off up to 50 L/min. Up to 200 L/min. Cycles per hour, quantity, maximum tidal volume and manual trigger 0,1 to 2,0 seconds with plateau value 0,1 to 30 seconds 0,1 to 30 seconds Oxygenation for aspiration maneuver with synchronized system - 1 to 20 min 24 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 Flow waveform Automatic bypass of the AIR – O2 network R 04-04(69) Rev. 06 Square / 100% Descending ramp / 50% Descending ramp / Sinusoidal / Ascending Ramp In case of failure in one of them, the equipment continues operating normally Adjusted in 120 cmH2O Inspiratory pressure inner safety valve Regulatory pressure valve of Air and O2 input Internally incorporated in the equipment Maintains the equipment in standby without changing the programmed values Standby Scales Automatic updated for vertical and horizontal readings Freeze Possibility of reading graphics RS232 signal connector USB signal connector For external communication with software and signals input For equipment's Service and Software update. THE CONDITIONS UNDER WHICH IT IS EXPRESSED FLOW, VOLUME AND LEAKAGE SPECIFICATIONS, ARE EXPRESSED IN “STPD” CONDITIONS (OPERATION TEMPERATURE OF 20º AND ATMOSPHERIC PRESSURE OF 101,3 KPA), EXCEPT THOSE ASSOCIATED WITH THE VENTILATOR’S RESPIRATORY SYSTEM, WHICH ARE EXPRESSED IN BTPS CONDITIONS (ENVIRONMENTAL ATMOSPHERIC PRESSURE AND OPERATION TEMPERATURE OF 37ºC). ALL THE MEASURED VENTILATORY VARIABLES ARE FILTERED AT 30 Hz AND CONDITIONED USING ANALOGICAL AND DIGITAL DATE PROCESSING TECHNIQUES. THE ACCURACY OF THE PRESSURE MEASUREMENTS IS ± 2% OF FULL SCALE (120 cmH2O) + 4% OF THE ACTUAL READING. THE REST OF THE SPECIFIED VALUES HAVE A MAXIMUM ERROR OF +/- 10%. THE EQUIPMENT HAS A SAFETY VALVE THAT OPENS WHEN IT REACHES THE MAXIMUM PRESSURE OF 120 cmH2O, RELEASING THE EXCESSIVE PRESSURE. NEGATIVE PRESSURE (SUB-ATMOSPHERIC) IS NOT AVAILABLE IN THE EXPIRATORY PHASE. WHEN ADDING ACCESSORIES OR OTHER COMPONENTS OR SUBASSEMBLIES TO THE VENTILATION SYSTEM OF THE LUNG VENTILATOR (BREATHING SYSTEM DELIMITED BY THE GAS INPUT PORTS AND THE PATIENT CONNECTION PORT AND/OR EXHAUST PORT), THE PRESSURE GRADIENT BETWEEN THE VENTILATOR’S VENTILATION SYSTEM AND THE PATIENT CONNECTION PORT MAY INCREASE. OUTPUT PARAMETERS (MONITORING) AIRWAY PRESSURE: PEAK, PLATEAU, MEAN, BASE (PEEP) INSPIRATORY TIME EXPIRATORY TIME I:E RATIO AND SPONTANEOUS BREATHINGS INSPIRATORY PAUSE INSPIRED / EXHALED TIDAL VOLUME (DISTAL & PROXIMAL) TOTAL AND SPONTANEOUS INSPIRATORY PEAK FLOW (DISTAL & PROXIMAL) EXPIRATORY PEAK FLOW (DISTAL & PROXIMAL) 25 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 DYNAMIC COMPLIANCE TOTAL, CONTROLLED AND SPONTANEOUS FREQUENCY GRAPHICAL INDICATOR OF SPONTANEOUS AND MECHANICAL CYCLES TOTAL, CONTROLLED AND SPONTANEOUS MINUTE VOLUME (DISTAL & PROXIMAL) FiO2 CONCENTRATION INSPIRATORY AND EXPIRATORY TIME CONSTANT COMPRESSIBLE VOLUME TI/TTOT RELATION etCO2 (OPTIONAL) CO2 INSPIRED (OPTIONAL) TOTAL LEAKAGE VENTILATION LEVEL (mL/Kg) LUNG MECHANICS AUTOPEEP DYNAMIC COMPLIANCE STATIC COMPLIANCE INSPIRATORY RESISTANCE EXPIRATORY RESISTANCE SLOW VITAL CAPACITY P0.1 (AIRWAY OCCLUSION PRESSURE) P-V CURVE WITH LOW FLOW TOBIN INDEX STRESS INDEX WORK OF BREATHING ALARMS MAXIMUM AIRWAY INSPIRATORY PRESSURE MINIMUM AIRWAY INSPIRATORY PRESSURE MAXIMUM AND MINIMUM EXHALED TIDAL VOLUME MAXIMUM AND MINIMUM EXHALED MINUTE VOLUME APNEA WITH ADJUSTABLE TIME MAXIMUM RESPIRATORY FREQUENCY MINIMUM RESPIRATORY FREQUENCY PATIENT CIRCUIT DISCONNECTION PROXIMAL FLOW SENSOR DISCONNECTION MAXIMUM AND MINIMUM PEEP AND CONTINUOUS PRESSURE GAS SUPPLY SOURCE (AR - O2) (HIGH & LOW PRESSURE) POWER OUTAGE LOW BATTERY CHARGE MICROPROCESSOR (INOPERATIVE VENTILATOR) INTERRUPTED CYCLE IN PRESSURE MODES MAXIMUM AND MINIMUM FiO2 INVERTED I:E RATIO THE ALARMS ARE TRIGGERED IN PRIORITY ORDER WITH AUDIBLE WARNINGS AND/OR MESSAGES ON THE SCREEN. GRAPHICS PRESSURE – TIME FLOW – TIME VOLUME – TIME CO2 – TIME (OPTIONAL) 26 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 VOLUME – PRESSURE LOOP FLOW – VOLUME LOOP PRESSURE – FLOW LOOP CO2 – VOLUME LOOP (OPTIONAL) TENDENCY CURVES (UP TO 72 HOURS) PEAK AND BASE PRESSURE FLOW TIDAL VOLUME MINUTE VOLUME FREQUENCY DYNAMIC COMPLIANCE ALARMS LOG LAST 1000 ALARMS AND EVENTS WITH DATE AND TIME OTHER MENUS INDICATION MENU OF HOURS OF USE AND SERVICES PERFORMED ALTITUDE ADJUSTMENT FOR VOLUME COMPENSATION POSSIBILITY OF EXCHANGING THE LANGUAGE ALARM AUDIO VOLUME ADJUSTMENT CIRCUIT CHANGE/TEST INITIAL SELF-TESTS ALTITUDE COMPENSATION ATMOSPHERIC PRESSURE CAPTURE OXYGEL CELL DETECTION PATIENT CIRCUIT SELF-TEST VERIFICATION OF HOURS OF USE SENSORS CALIBRATION PROXIMAL SENSOR DETECTION PROXIMAL SENSOR CALIBRATION CIRCUIT LEAKAGE MEASUREMENT CIRCUIT COMPLIANCE MEASUREMENT EXPIRATORY FLOW SENSOR CALIBRATION OXYGEN CELL CALIBRATION INTERNAL FLOW SENSORS CALIBRATION PROPORTIONAL AIR VALVE TESTS PROPORTIONAL O2 VALVE TESTS PEEP CONTROL VALVE TESTS DETECTION AND INITIALIZATION OF THE CAPNOGRAPH (OPTIONAL) OTHER VENTILATOR SAFETY CHARACTERISTICS AUTOMATIC COMPENSATION OF GASES LEAKAGE COMPENSATION IN ALL VENTILATORY MODES (NIV) SAVED LOG OF EVENTS AND ALARMS EVEN AFTER POWER FAILURE WARNING OF MAINTENANCE NEEDED BY HOURS OF USE POSSIBILITY OF OPERATION WITHOUT FLOW SENSOR POSSIBILITY OF OPERATION WITHOUT PROXIMAL SENSOR POSSIBILITY OF OPERATION WITHOUT OXYGEN CELL THE LINE TEST (SELF-TEST) IS PERFORMED BY THE OPERATOR WHENEVER THE EQUIPMENT IS TURNED ON. ONCE THE SELF-TEST IS FINISHED, THE DEVICE PERFORMS A CALIBRATION WITHOUT THE OPERATOR'S INTERVENTION. WHEN IT'S NECESSARY, THE EQUIPMENT PERFORMS AN AUTOMATIC CLEANING ON THE FLOW SENSORS (EXHALATION VALVE) WITHOUT HAVING ITS REGULAR OPERATION INTERRUPTED. 27 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 IN CASE OF LEAKAGE IN THE PATIENT CIRCUIT DURING THE INITIAL TEST (SELF-TEST), THE EQUIPMENT WILL DISPLAY ON THE SCREEN A MESSAGE INDICATING THE LEAKAGE VALUES. FOR THE CORRECT OPERATION OF THE EQUIPMENT, IT IS IMPORTANT TO HAVE NO LEAKAGE IN THE PATIENT CIRCUIT. DURING THE EXHALATION FLOW TEST, THE GAS LINES (AIR AND O2) MUST DELIVER A MINIMUM FLOW OF 100 L/MIN, SO THAT IT DOES NOT INTERFERE THE OPERATION OF THE SAME. IN CASE OF BAD CONNECTION, WRONG ASSEMBLY OR INVERSION OF THE SENSORS, THE EQUIPMENT WILL DISPLAY ON THE SCREEN A MESSAGE INDICATING FLOW READING ERROR, AND THE OPERATOR SHALL CONFIRM WHETHER THE EQUIPMENT WILL WORK WITH OR WITHOUT EXHALATION FLOW READINGS. BY THE END OF THE CIRCUIT’S COMPLIANCE TEST THE EQUIPMENT DISPLAY ON THE SCREEN THE VALUE TO BE AUTOMATICALLY COMPENSATED IN ml/cmH2O. THE VALUE MEASURED DURING THE LINE TEST IS AVAILABLE FOR CONSULTATION ON THE EQUIPMENT’S MENU. IF NECESSARY THE TEST CAN BE RUN AGAIN WITH THE EQUIPMENT TURNED ON AT THE OPTION OF THE MENU “CIRCUIT CHANGE/TEST” AND A NEW CIRCUIT COMPLIANCE VALUE IS MEASURED AND COMPENSATED. ALL THE MEASURED AND/OR COMPUTED VENTILATORY VARIABLES, WHICH ARE DISPLAYED OR USED FOR CONTROL ARE SAMPLED AT A FREQUENCY OF 30HZ AND PROCESSED BY DIGITAL AND ANALOGIC PROCESSING TECHNIQUES. 28 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 ELECTRONIC BLENDER OPERATION (AIR-O2 MIXER) FiO2 (Fraction Inpired Of Oxygen) indicates the amount of Oxygen that is mixed with the gas breathed by the patient. Generally speaking, it may vary from 21% (79% Nitrogen and 21% O2) up to 100% (pure Oxygen), for example a FiO2 of 60% means that 60% of the volume breathed by the patient will be oxygen and the other 40% of the volume will be nitrogen and other gases. The FiO2 found in the Lung Ventilator LUFT 3 is generated by an electronic blender system, which dispenses any external mixer. The mixture is performed by two proportional actuators, known as Proportional Valves, named this way because they control proportionally the AIR and O2 flows that passes through each one of them. Each flow is read by their respective pneumotachographs (device used for flow measuring), which send to the CPU the current value of the flow generated by the Proportional Valves. The FiO2 value is given by the fraction of gas delivered through each Proportional Valve, where each one of them is responsible only by part of the total inspired gas volume. This system is very accurate because it works with physical values well known, such as volume, pressure and flow and the variations on the Oxygen concentration on the Ambient Air are small, as well as the percentage of the Oxygen 100% provided. This is enough for the control to calculate the value of the flow that each valve will have to deliver to the patient, therefore obtaining, with a very low error chance, the correct FiO2. Picture 1 FIO2 READING The FiO2 is performed through a permanent, non-consumable internal sensor which monitors the patient’s FiO2 in the inspiratory branch and does not need maintenance or replacement. The permanent internal sensor is standard with the Lung Ventilator LUFT3. It is possible to monitor the FiO2 through the option of a oxygen cell (Galvanic technology) or through a Paramagnetic cell which is internally installed in the casing. In case the galvanic cell is used, the equipment performs the verification of the integrity and calibration during the equipment’s initial test. In case it is identified any damage on the oxygen cell, the equipment automatically switches for the permanent internal sensor without damage or loss on the patient’s FiO2 monitoring. For the maintenance of the oxygen cell, the equipment must be sent to the authorized technical support. The permanent internal sensor does not require maintenance and its calibration is performed during the preventive maintenance. 29 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 CHAPTER 3 – ASSEMBLY AND CONNECTION EQUIPMENT ASSEMBLY Picture 2 Picture 3 1. Assemble the equipment over the 2 sockets of the trolley, as marked in the figure above. 2. To fix the equipment, release the back nuts, remove the back cover and thread the locknut, as on the pictures below, after securing the equipment, fit the back cover and lock it with the nuts again. Picture 4 Picture 2 30 of 88 Picture 6 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 3. Place the monitor over the equipment through a movement rod, as on the pictures below, fixing in a way that it is firm and safe. Picture 3 Picture 4 THE ASSEMBLED EQUIPMENT HAS LIMITATIONS REGARDING THE RISK OF TIPPING (FALLING), AND MAY BE TILTED IN A MAXIMUM OF 5 DEGREES DURING ITS USE. WHEN MOVING THE ASSEMBLED EQUIPMENT, PRECAUTIONS SHALL BE TAKEN WHEN INCLINING THE DEVICE TO PREVENT IT FROM TIPPING OVER. THE TRANSPORTATION OF THE EQUIPMENT SHALL BE PERFORMED IN ITS ORIGINAL PACKAGING, WITH THE TROLLEY AND THE LCD SCREEN DISASSEMBLED. SCREEN CONNECTION The cable inputs are different to guarantee there are no mistakes during installation. Plug the cables on the monitor and equipment according to the numbers on the pictures below. Picture 10 Picture 5 31 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 POWER SOURCE CONNECTION The power source connection may be found at the rear of the case. On the ventilator’s case, the operating voltage values are displayed together with the nominal current and nominal power of the equipment. You will also find the values corresponding to the fuses, as indicated on the picture below. A power source with external battery may be connected to the power source connection, doubling the equipment’s autonomy time. Picture 11 THE EQUIPMENT IS EQUIPPED WITH 2A 20mm SB DELAYED FUSES, FIT FOR POWERING FROM 100V UP TO 240V~. ELECTRICAL CHARACTERISTICS OF THE DEVICE MAY BE FOUND ON THE CHAPTER 1 - PRESENTATION OF THIS MANUAL. THE INPUT POWER SUPPLY IS UNIVERSAL AND THE EQUIPMENT OPERATES ON ANY VOLTAGE RANGE (100V UP TO 240V) WITHOUT THE NEED OF INTERVENTION FROM THE OPERATOR, EVEN WHEN THERE IS A REDUCTION OF LINE VOLTAGE DURING THE NORMAL OPERATION. CHECK WHETHER THE EQUIPMENT IS CONNECTED TO A GROUNDED POWER OUTLET IN ORDER TO GUARANTEE THE CORRECT OPERATION OF THE EQUIPMENT. NEVER TURN ON THE DEVICE WITHOUT GROUND CONNECTION. THE ELECTRICAL INSTALLATION IN WHICH THE VENTILATOR WILL BE CONNECTED MUST COMPLY WITH THE TECHNICAL STANDARD NBR 13534, WHICH ESTABLISHES THE MINIMUM CONDITIONS OF THE ELECTRICAL INSTALLATIONS IN ASSISTANCE HEALTH CARE ESTABLISHMENTS. 32 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 EQUIPMENT CONNECTION Picture 12 On the front part of the equipment, there are the inputs for the following connections: A – Exhalation Valve B – Patient Circuit C – Nebulizer D – Capnograph E – Proximal Sensor F – RS232 communication connector RS232 Communication Connector for communication with software and accepts sensor connection for oximetry. CONNECTION TO THE GAS SUPPLY SOURCE The connection to the gas sources is found on the rear of the case. On the ventilator's case, the corresponding Air and Oxygen (O2) inputs are indicated. 33 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Picture 13 AIR INPUT Male connector DISS 3/4” –16 OXYGEN INPUT (O2) Male connector DISS 9/16”-18 AT THE EDGE OF THE PRESSURE TUBES, THE CORRESPONDING FEMALE CONNECTORS SHALL BE USED . THE SCREWABLE CONNECTIONS USED IN THE GAS INPUTS ARE FOLLOWING THE STANDARD CGA V5 WHICH ESTABLISHES THE RULES FOR MINIMAL EXIGIBLE CONDITIONS FOR THIS TYPE OF CONNECTION. THE AIR AND OXYGEN INPUTS ARE MANUFACTURED WITH VALVES THAT PREVENT REVERSE FLOW OF GASES THROUGH THE INPUT PORTS AND THE GAS CROSSFLOW. INPUT PRESSURE 250 – 700 kPa (2,5 to 7 bar) 250 – 700 kPa (2,5 to 7 bar) 60 L/min. 180 L/min. AIR OXYGEN (O2) MINIMUM FLOW SUPPLY MAXIMUM FLOW DO NOT USE THE EQUIPMENT IN THE PRESENCE OF FLAMMABLE ANESTHETIC GASES. THERE IS DANGER OF EXPLOSION AND/OR FIRE. THE USE OF COMPRESSED, CLEAN AND DRY AIR AND OXYGEN IS A MUST IN ORDER TO AVOID CONTAMINATION THAT AFFECTS THE OPERATION OF THE EQUIPMENT. 34 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 IN CASE OF FAILURE IN ONE OF THE GAS SUPPLY SOURCES (AIR OR O2) THE EQUIPMENT CONTINUES OPERATING WITH THE REMAINING GAS SOURCE (AIR OR O2). THE LUNG VENTILATOR LEISTUNG LUFT 3 SUPPORTS INPUT PRESSURE UP TO 1000 KPA (10,2 BAR), IT IS NOT NECESSARY TO USE EXTERNAL REGULATING VALVES UNTIL THIS PRESSURE. BREATHING CIRCUIT Use the breathing circuit according to your need: Adult, Pediatric or Neonatal. The difference is in the diameter of the tubes, which interferes in the resistance of the breathing circuit. On the front of the equipment there are connections for: - Exhalation Valve - Breathing Circuit - Proximal Sensor - Nebulizer - Capnograph - Connector Picture 14 ON RESPIRATORY CIRCUITS WHICH CONTAIN WATER TRAPS ON THEIR BRANCHES (INSPIRATORY/EXPIRATORY), VERIFY THEIR HERMETICITY TO PREVENT LOSS OF VOLUME IN THE CIRCUIT. WHEN THE CALIBRATION OF THE PATIENT LINE IS PERFORMED, THE NEBULIZER SHALL NOT BE CONNECTED ON IT. 35 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 VERIFY THE CORRECT POSITION OF THE EXHALATION VALVE'S DIAPHRAGM. CHECK CHAPTER 6 – exhalation valve, patient CIRCUIT and proximal . FOR EFFECT OF THE STANDARD NBR IEC 60601-1, THE PATIENT CIRCUIT IS CONSIDERED APPLIED PART, TYPE B. THE CONNECTORS OF THE PATIENT CIRCUIT ARE CONICAL TYPES 22mm IN ADULT AND 15mm IN NEONATAL AND THEY ARE IN ACCORDANCE WITH THE STANDARD ISO 5356-1 (NBR13475), WHICH DETERMINES THE MIMIMAL EXIGIBLE CONDITIONS FOR THIS KIND OF CONNECTORS. 36 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 ARTICULATED ARM ASSEMBLY 1- Hold the assembled articulated arm. Picture 15 2- Position the arm over the support, located at the laterals of the trolley. Screw the arm until it is firm. Picture 16 3- Even with the arm fixed on the trolley, it can be easily turned for either of the sides. Picture 17 37 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 CHAPTER 4 – INSTRUCTIONS, CONTROLS AND ALARMS INSTRUCTIONS OF USE When the equipment is turned on the initial page is displayed, where you can select the kind of patient to ventilate, the gender, height, theoretical weight, ventilatory volume per kilogram and you can also select the kind of patient interface and its dimensions. Picture 18 SCREEN CALIBRATION On the back part of the screen there is its calibration panel. The panel contains five buttons, when the monitor is turned on, a led light will remain lit. To calibrate the screen press the key indicated on the rear panel, the screen will begin to calibrate automatically. 38 of 88 Picture 19 LUNG VENTILATOR LEISTUNG LUFT 3 By pressing the button R 04-04(69) Rev. 06 there are several functions of configuration, with the keys to navigate through the functions and pressing the button to enter and enable the functions. The button to return and the button turns the screen on and off. It is possible to adjust the screen’s angle of view and rotation. To adjust the screen’s angle it’s necessary to hold firmly the LCD monitor’s border and move the screen to the desired position, then the screen will remain in that position. It is possible to adjust the LCD monitor on the vertical to adapt it to the operator’s height, making the visualization clear and the handling of the touch screen practical for people of any stature. It is also possible to adjust the monitor on the horizontal, with the rotation of the z axis of the equipment. TOUCH SCREEN CALIBRATION In order to calibrate the Touch Screen, the equipment must be in its Initial Page (picture 18). Press the button which is behind the equipment as indicated on the picture below: Picture 20 39 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 After pressing the Touch Screen calibration button and the equipment’s screen will turn black with a yellow cross, press the center of the yellow cross and hold it until it turns green, as shown on the picture below: Picture 21 Touch again the center of the second yellow cross until its color turns green, as shown on the picture below, as soon as the cross’ color changes to green, the screen will be calibrated and it will return to the Initial Page (Picture 18). Picture 22 40 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 PATIENT PARAMETERS The selection of the kind of patient influences the options of ventilatory modes and the values of the initial working parameters. Once the patient is selected (adult, pediatric and neonatal), this choice will be marked with the blue color, according to the pictures (Picture 23, Picture 24 and Picture 25), and everything else will be on the grey color, the same happens with the choice of Picture 24 Picture 23 the patient's gender. In case it is needed to change the parameters, you shall select the new option. This will automatically cancel the previous selection. The Height, Weight and Volume are adjusted with the keys Up-Down, located in the same field selected. When Adult is selected, it is needed to inform the height and the ventilatory volume per kg. The equipment will calculate the theoretical weight. In case of Pediatric or Neonatal patients, it is needed to inform the weight Picture 25 and ventilatory volume of the latter. CIRCUIT When selected Tube or Cannula, it will activate the diameter configuration of the same, in case of selecting Mask, it becomes selectable directly between Active or Passive humidification. The equipment will automatically compensate the kind of circuit used accordingly to the selected configuration. Picture 6 SELF-TEST Once the Patient and the Circuit information are set, the patient circuit must be installed on its proper connections (as it is shown on Picture 14). Picture 27 The Y connector's output shall be blocked and the Initial Page's green color button “Start Test” shall be pressed (Picture 27). The equipment will perform a test on the patient circuit, verifying if there is any leakage. The wrong obstruction of the output may cause the equipment to warn about leakages on the system. During the initial self-test the equipment will read the patient circuit’s compliance, this value is informed on the screen and automatically compensated. 41 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Check if the Exhalation Valve (Picture ) is correctly assembled, with its transparent membrane intact, and check if the sensor is not inverted, otherwise the equipment will not be able to make the flow readings. In case there is any circuit leakage during the self-test, the equipment will display on the screen a message “ The equipment presented leakage bigger than 4 L/min at 60 cmH2O”. It is extremely important not to have any leakage in the patient circuit in order to make the equipment work correctly . During the test of the gases lines (Air and O2) the test should deliver a flow bigger than 100 L/min, In case the pressure is out of the specified range, a warning will be displayed on the screen with the message “Input pressure lower than 3,0 kg/cm²”. During the line test the equipment will perform the calibration of the expiratory flow sensor, in case there is any detection of failure the equipment will inform with 3 possible messages indicating the specific failure or possible solution and will give the option of operating without the expiratory flow sensor, if chosen not to use the expiratory flow sensor, the equipment will present on the screen only the reading of inspired flow. “Error on the flow reading. Possible inversion of the exhalatory valve’s hoses” indicating that the silicon hoses of the exhalation valves are inverted (Picture 85). The second possible message will be “Erro on the flow reading. Check the exhalation valve” indicated that the internal flow reading membrane (Picture 85) of the exhalation valve is damaged. The third indicates “Error on the flow reading. Error value: 15, 35 or 80 L/min.” Indicating that the input flow is limited, not reaching the value specified on the screen, the suggestion is to check the pressure and flow of the gases network. When the equipment’s circuit Compliance Test is finished, the screen display the values which will be compensated by the equipment. After some time of use in a patient, some characteristics measured during the initial circuit and peripherals test may have changed due to circumstances such as temperature, humidity and stowage. As a consequence, it may be needed to run the command “Circuit Test”. For this, it is not necessary to turn off the equipment. To access this command, go to “Menu, Configurations, Change/Test the Circuit”. The variations on the circuit may be significant within the first two operating hours, tending to establish soon afterwards. In case a message is displayed on the screen asking for the preventive maintenance, the corresponding icon will appear on the Icon Panel (Picture 30). You can carry on with the test by pressing “Continue”. WHEN THE PATIENT CIRCUIT IS CALIBRATED, THE NEBULIZER SHOULD NOT BE CONNECTED. IT IS RECOMMENDED TO RESPECT THE ESTIMATED HOURS FOR THE CONTROL AND CALIBRATION OF THE EQUIPMENT'S INTERNAL ELEMENTS IN ORDER TO ASSURE ITS CORRECT OPERATION FOR A PROPER VENTILATION AND TO AVOID SEVERE FAILURES. LAST PATIENT BUTTON By pressing this key when you turn on the device, it will automatically retrieve the configuration from the last patient, searching the parameters stored on the equipment's internal memory. Picture 28 SCREEN Once the ventilator passes through the line test, the main page is displayed. The same is presented in such a way that it allows the operator a quick localization of the information which the professional 42 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 needs to see, enabling high operability. The screen is divided by sectors in distinct areas: Icon Panel, Alarm Area, Dynamic Monitoring Area and Alarms Configuration, Information Area, Operative Area, Adjustment Area, Graphics Area, Direct Access Panel and Menu with applications and configuration options. Picture 29 ICON PANEL Initially, three icons are displayed on the panel, but more can be displayed depending on the operation that is been performed or due to a certain situation, for example, upon the activation of an alarm. Clock: Indicates the date and time when the equipment was turned on and the current time. Hand: Enables/Disables the Touch function from the screen, thus changing the icon. Plug/Battery: Indicated that the equipment is connected on the power grid or on the battery, changing the icon on the screen. The battery symbol is a bar proportional to the Picture 30 battery charge which varies from 0 to 100%. The color of the proportional bar changes accordingly to the charge level range, being green the safe level, yellow is not recommended to initiate the transport without power supply and red to connect the equipment to the power as soon as possible. Volumetric Capnography: This icon indicates that the Volumetric Capnography function is active. It enables the monitoring of the volumetric capnography curves, upon continuous 43 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 visualization on the screen, registering the Carbon Dioxide (CO2) elimination in relation to the exhaled volume. Oximeter: This icon indicates that the Oximeter function is active, performing the reading of the Heart Rate, SpO2 and also SpO2/FiO2. Alarm: Indicates that new alarm notifications were triggered on the equipment. A list with the alarm logs will be displayed if you touch that icon. Configuration: This icon is displayed on the panel in case preventive maintenance is needed. Silence: This icon is displayed on the panel when the audio alarm is inhibited (check CHAPTER 5 - ALARMS). ALARMS AREA On the top part of the screen, the alarm messages are displayed. According to its priority level, it will display a Red message (HIGH PRIORITY ) or Yellow (LOW PRIORITY ALARM CONDITION ). Ver CHAPTER 5 - ALARMS. Picture 31 INFORMATION AREA Picture 82 It is divided in 3 parts: 1. Operative area; 2. Kind of trigger; 3. Operative information. 44 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 OPERATIVE AREA In this area, it is indicated the ventilatory mode in which the equipment is working and the selected kind of patient. Picture 9 KIND OF TRIGGER The kind of trigger is represented by three icons. The first one indicates that the equipment is in Standby mode, the second one indicates that the patient is breathing by him/herself and the third one indicates that the patient is breathing through the ventilator. Picture 34 OPERATIVE INFORMATION Area where additional information is displayed, such as Theoretical Weight or Height of the Patient, Interface Tube or Canulla and its dimensions, Active Humidification or Passive, Oxygen Cell Active or Inactive, operative guide, etc. This information may vary according to the ventilatory mode and its aplication in use. For example, some data can be visualized according to the picture below. Picture 105 SELECTION CONTROLS On the bottom right part of the screen, there is the Control Panel which allows you to increase or decrease the adjustable functions of the equipment and confirm or cancel the modification on the values. “ACCEPT” Picture 36 “DECREASE” “CANCEL” “INCREASE” STANDBY MODE Picture 11 In order to access the Standby mode, just press its icon. This mode keeps the equipment in sleep mode and with the alarms function disabled, until it is reconnected to the patient, without losing the operative parameters. 45 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 AIRWAY PRESSURE BAR (BARGRAPH) At the right of the monitoring area, there is a vertical bar in white color which indicates the Pressure in the Airway. On its left, in red, it's the configured values of the alarms for Maximum and Minimum Pressure. DYNAMIC MONITORING AREA AND ALARMS The parameters resulted from the ventilation can be monitored on two numeric columns on the left side of the screen. The column on the left shows the parameters that have an alarm . - Maximum and Minimum Pressure - Maximum and Minimum Tidal Volume - Maximum Frequency - Maximum and Minimum Minute Volume - FiO2 - Ventilation Level In red, in a smaller size, there are indicators of the maximum and minimum values set to trigger the alarms. Picture 12 In order to adjust them, you need to touch the value you wish to change and press “+” or “-”, according to your needs, and then press the keys to “Confirm” or “Cancel” this selection. The value of the Tidal Volume (V.Tidal) informed on the screen corresponds to the value measured by the Picture 40 expired volume sensor during the patient's expiration. When the ventilator works without the Tidal Volume sensor, this value is Picture 39 informed in RED because it refers to the value delivered by the ventilator during the inspiration, instead of the value measured during expiration. Below the Tidal Volume is presented the Ventilation Level that indicates to the operator the tidal volume in relation to the theoretical weight expressed in mL/Kg and updated cycle by cycle. At the column on the right, there are parameters which do not have an alarm. On this panel, there are six movable buttons colored in a light grey color and an arrow in black color to the left. They move themselves when you press that arrow. GRAPHICS AREA In the graphics area, up to 5 curves can be seen: Curve of Pressure – Time: The Pressure – Time graphic shows the changes produced on the airway pressure. The pressure is represented in centimeters of water column (cmH2O) and the time is expressed in seconds (s). Curve of Flow – Time: The Flow – Time graphic shows the gradual changes produced on the inspiratory flow. The flow is represented in liters per minute (L/min.) and the time is expressed in seconds (s). Curve of Volume – Time: The Volume – Time graphic shows the gradual changes of delivered volume to the patient. The volume is expressed by liters (L) and time by seconds (s). 46 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Curve of Volume – Pressure: Besides the information about the volume, pressure and compliance, it's possible to indicate the PEEP need or its increase, when the ventilation has to designate an important part of the generated pressure and the volume to obtain a recruitment and opening of the airway. The pressure is represented in centimeters of water column (cmH2O) and the pressure is expressed in liters (L). Curve of Flow – Volume: With these loops it's diagnosed the flow obstruction standards, showing up as a depression. If we see it during the expiratory phase, we have an expiratory obstruction; if we see it during both phases, the obstruction is inspiratory and expiratory. The flow is represented in liter per minute (L/min.) and the volume is expressed in liters (L). ÁDJUSTMENT AREA Picture 41 At the lower part of the screen there are the parameters programmable by the operator. To modify them, you must press over the icon of the desired parameter, to change the values you must press “+” or “-” on the selection control panel and afterwards “confirm” or “cancel” it. Note that when a function is selected it changes its color according to the picture below and when the values are changed the blue bar increases or decreases its height accordingly. Picture 42 WAVEFORMS The flow of a mechanical ventilator is quantified by the inspiration waveforms. These waveforms demonstrate how the ventilator delivers air to the patient. In controlled modes the inspiratory phase is identified by a graphic in blue color and the spontaneous modes are identified by a graphic in orange color, for all modes the expiratory phase is identified by a graphic in white color. When the patient performs an effort enough to trigger the equipment, this cycle is spontaneous, it has the orange color and therefore the monitored parameters in this cycle are spontaneous, as for example, the respiration frequency. The pattern of flow waveform may be changed on the VCV mode in order to suit the ventilatory demand or the physical conditions of the patient's respiratory system. On the pressure modes, you cannot change the waveform pattern (The flow is adjustment by equipment’s control system based on the patient’s physical compliance and resistance characteristics). There are five waveform patterns that may be used. SQUARE FLOW WAVEFORM (CONTÍNUOUS) With this adjustment, the flow accelerates fastly and reaches a flow value which will be maintained during inspiration. The delivered flow will be constant and will produce a volume waveform like an ascending ramp, and pressure curve will be made of a stair step and an ascending ramp, the peak inspiratory pressure will happen at the end of the inspiration. The value of the delivered flow will be lower than the other flow waveforms shapes. Usually the value of the peak pressure will be higher in this waveform than in comparison with the Picture 43 descending and descending 50% waves, with exception to a patient with elevated resistance. The value of the flow will be automatically calculated by the equipment according the pro programmed volume and inspiratory time. 47 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 DESCENDING RAMP 50% FLOW WAVEFORM This waveform uses a fast flow acceleration followed by a slow deceleration. This pattern may request higher flows to obtain the programmed value. This waveform may be used to provide a better distribution of the inspired air. This waveform promotes a reduction of the inspiratory pressure in patients with high resistance when compared with the descending flow waveform. Picture 14 DESCENDING RAMP FLOW WAVEFORM This flow waveform uses a fast flow acceleration followed by a deceleration until zero. This flow waveform may required much higher flows to obtain the programmed value. This wave may be used to provide a better distribution of the inspired air. Picture 15 Picture 16 ASCENDING RAMP FLOW WAVEFORM This waveform starts with a zero flow and increases linearly until it reaches a peak value, followed by a fast cut of the flow. In relation to this ascending ramp waveform pattern, the corresponding patterns for pressure and volume are seen as an upward concave shape In relation to this ascending ramp waveform pattern, the corresponding patterns for pressure and volume are seen as an upward concave shape. The peak pressure value will be the highest in this flow waveform. SINUSOIDAL FLOW WAVEFORM (ROUND) This kind of waveform accelerates the flow slowly to a maximum value at the middle of the inspiratory time and reduced towards the end of the expiration. The maximum airway pressure is reduced here. This wave can be used without generating a high airway pressure as happens when using square flow Picture 17 waveform. SENSIBILITY Sensibility is the threshold value that mus be reached by the patient to perform the trigger of the inspiratory cycle, the measuring of the patient’s inspiratory efforts and may be monitored through the reduction of the pressure or the variation of the air flow which occurs during the patient’s effort to breathe. By touching the sensibility icon it is possible to switch between trigger by pressure (cmH2O) or by Picture 18 flow (L/min.) and also adjust the desired valued for triggering the equipment. On the controlled ventilation modes, such as the VCV, PCV and PRVC, the sensibility acts to provide gases to the patient in case the same makes an effort sufficient to trigger the next cycle. DIRECT ACCESS AREA This area includes the most frequent options of use, allowing an easy and quick access. To access these options, just touch the desired icon. When the options are enabled (according to the operative mode), the icons and letters will be displayed in dark blue color; when they are not enabled, they will be displayed in white color and their icon will not be displayed. 48 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Nebulizer: When accessing this function, the ventilator will request you for the programming of time of operation, once established, the the oxygen output flow is activated synchronized with the inspiration. It is informed, in green, the programmed time and in red the total time of operation. This output is automatically deactivated once the time set by the operator is reached, or manually by repeating the process and choosing the time 0 s. Picture 50 Oxygen: The goal is to simplify the handling of the equipment during the procedures on the airway and/or alveoli recruitment maneuvers sebsequent to a depressurization, besides facilitating the initial ventilation of the patient when the same enters the unit until his/her clinical and semiological evaluation. (The maximum FiO2 alarm shall be turned off, as explained on the CHAPTER 5 - ALARMS). By pressing the button 100% Oxygen, it starts a sequence to ventilate the patient with pure oxygen, where the operator Picture 19 can choose between 1 up to 20 minutes. As soon as the time is selected, the ventilator will display on the message area, in green the time elapsed since when this modality was turned on and in red the remaining time until its completion. Picture 49 The disconnection of the ventilator can be done without modifying the equipment's operation and by silencing all the alarms automatically for 30 seconds. Changes in ventilatory parameters and the base pressure (PEEP), always respecting the ventilatory mode in which the procedure has started, are allowed. Once the selected time is completed, the equipment will return to the fraction of inspired oxygen used before starting this function. To manually abort this procedure, the operator will have to access again the option 100% Oxygen and select the time 0 (zero). Manual Trigger: It starts the ventilatory cycle at the moment the user wants. It is used to increase the level of manual ventilation. Its use will change the resulting Respiratory Frequency and consequently the I:E ratio (for maneuvers of oxygenation for suction with synchronized system). The manual trigger will only be allowed by the equipment after the end of the exhalation of the patient, avoiding the double cycle and the increase of the inspiratory pressure.). Inspiratory Pause: The inspiratory pause is a prolongation of the programmed inspiratory time (from 0.10 up to 2s), during which the exhalation Picture 52 valve remains closed, the pressure remains constant and the flow is zero. It is available on the VCV mode, because on the PCV mode, when there is a time cycled variable, the same function can be obtained with the prolongation of the inspiratory time. Once the pause is established, the ventilator informs (in the functions area) the resulting Inspiratory Pause and the resulting Plateau Pressure. To activate the manual pause press and maintain pressed the button during the desired time, the equipment will perform the manual inspiratory pause. Similarly for the Picture 53 manual expiratory pause. 49 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Expiratory Sensibility: On the PSV mode and the combined modes which includes Support Pressure, it's possible to adjust the value of the flow which generates the change from the inspiratory phase to the expiratory phase (cycled). It is expressed in percentage of the inspired peak flow's value and may be adjusted between 5% and 80%. The flow has a descending wave shape, the ventilator cycles when the selected threshold is crossed by the flow. A smaller expiratory sensibility value will cause the increment of the inspiratory time. A low expiratory sensibility may difficult the cycling in case leakages in the patient circuit happen due to the fact that the leakage can be bigger than the selected threshold. Picture 54 Graphics Freeze: It freezes the graphics displayed on the screen, showing the grid with vertical and horizontal dashed cursors, making it easier to read the curve values, keeping active the patient monitoring using the output values and the Airway pressure bar. To unfreeze press the key again. Detect Capnography: Pressing “Detect Capnography” after connecting the sensor will make the equipment identify that the sensor is connected and the symbol will change to Picture 55 “Volumetric Capnography”. Picture 56 Volumetric Capnography: It is the graphic record, easy and non-invasive of the CO2 concentration on the gas that is exhaled during the ventilatory cycle. This record can be done according to the partial CO2 pressure exhaled at the end of the expiration (ETCO2), which will be influenced by the following factors: 1- Metabolic CO2 production; 2- The transportation performed by pulmonary perfusion; 3- The elimination by pulmonary ventilation. Measurement is performed by using a capnograph which utilizes infrared spectrograph in a line arrangement or “MAIN-STREAM”. The use of this parameter is very broad, as it allows to estimate the level of ventilation, detection of asynchrony, correct placement of the endotracheal tube, etc. The measurement of the level of ETCO2 related to the exhaled volume by the patient gives origin to the volumetric capnography, which will allow to establish other variables such as dead anatomic space, dead alveolar space and effective ventilation level. Maximum Inspiratory Time: The change from the inspiratory to the expiratory phase can also occur when the inspiratory time exceeds the value programmed by the operator in T. Ins. Max. MAIN MENU AREA By pressing the word “Menu", the screen will slide to the MAIN MENU, where there are 6 options. The wanted option shall be pressed, after 10 seconds the menu will be hidden. VENTILATORY MODES 50 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 -VCV -PCV -PSV/CPAP -SIMV(VCV)+PSV -SIMV(PCV)+PSV -PRVC -NIV -MMV+PSV -PSV+ASSURED VT -BIPHASIC LUNG MECHANICS -AutoPEEP -Compliance - Resistance -Low Flow PV Curve -Slow Vital Capacity -P0.1 -Tobin Index -Stress Index GRAPHICS Picture 20 -From 1 to 5 curves -Scale/Time REMOTE MONITORING -Alarms Log -Trends -Lung Mechanics -Patient Circuit Compliance FUNCTIONAL SETUP -PEEP Alarm -Sighs -TGI -Circuit Change/Test OPERATIVE SETUP -Maintenance -Language -Altitude Compensation -Date/Time -Sound Level 51 of 88 Picture 58 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 VENTILATORY MODES By selecting a ventilatory mode, the operator is determining what kind of variable he wants to control during the inspiration. Access the “Menu of Ventilatory Modes”, where the desired mode is selected (pressing “…next” allows the visualization of the remaining ventilatory modes) and the selection is confirmed, displaying on the screen the selected parameters, curves and resulting values. All the modes available on the equipment (AdultPediatric-Neonatal) have a pre-set configuration from the factory: these configurations are average values and must be adjusted by the physician to become values appropriated for each patient. The ventilator does not interrupt its operation during the change from one mode to another. The ventilatory modes are divided in basic modes and integrated modes; in the first group, it is included the ventilation modes controlled by pressure and support pressure. In Picture 60 Picture 59 Picture 61 these modes, you can control only one variable continuously while in the integrated modes, although controlling one variable at a time, you can change the kind of control according to the characteristics of the patient's ventilation. The inspiratory flow can be adjusted directly or indirectly by the user, through the configuration of ventilatory variables such as volume, inspiratory time, I:E ratio, flow waveform or directly by the flow itself, depending on the ventilatory mode. When the flow is adjusted indirectly, by adjusting the variables previously mentioned, the resultant of this flow is equated by the equipment and informed on the screen in blue color. On the ventilatory modes with pressure control where the flow is equated and directly controlled by the equipment based on the compliance and resistance conditions of the patient, the operator may perform an adjustment on the peak flow, adjusting the control variable “Rise Time”. The expiratory flow is adjustable for each kind of patient (adult, pediatric and neonatal). It is automatically adjusted for leakage compensation by the user or to adjust the PEEP value which will influence on the expiratory resistance. VOLUME CONTROLLED VENTILATION – (VCV) In this mode, the ventilator controls the volume delivered to the patient, integrating the air volume and the inspiratory time selected by the operator, i.e., it behaves like a flow controller cycling per volume. The inspiratory flow is adjustable and indicated in blue color during the adjustment of volume or inspiratory time. Therefore, to perform changes on the flow speed, you shall modify the tidal volume or the inspiratory time, or even both of them together, according to the necessary ventilation. When controlling the flow, it is possible to choose among constant flow waveforms, descending waveforms, sinusoidal or ascending, being then possible to observe the consequent modifications on the peak flow and the morphology of the curves of Pressure – Time and Flow – Time. The resulting pressure is the free variable, which will be determined based on the physical and mechanical conditions of the respiratory system. The inspiratory cycle trigger can be time, flow or pressure because it is an assisted-controlled mode. 52 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 PRESSURE CONTROLLED VENTILATION – (PCV) In this mode the ventilator will positively pressurize the patient's respiratory system during the inspiratory time programmed by the operator. To obtain it, once the established pressure level is reached, it will start a deceleration on the speed of the flow. This deceleration is the consequence of the respiratory system's physical condition and is not controlled by the ventilator. It is therefore a pressure controlled mode and cycled by time, being possible for the operator to manually change the peak flow or the “Rise Time”. The resulting tidal volume is the free variable and consequently this kind of ventilation requires an increased pathophysiological analysis of the patient, whom shall be permanently monitored by trained staff, as well as a correct programming of the volume alarms. The beginning of the ventilatory cycle can occur by time, flow or pressure because it is an assistedcontrolled mode. As the inspiratory flow is resulting from the equipment's programming and from the physical conditions of the respiratory system, the produced flow waveform is invariably decelerated, observing variations on the flow's speed by the end of an inspiration, i.e. the inspiration can be finished without the flow reaching the zero value; reaching the zero value coincided with the end of the inspiration or before that. SUPPORT PRESSURE VENTILATION OR CONTINUOUS POSITIVE AIRWAY PRESSURE – (PSV/CPAP) It is a mode developed to adapt the ventilator to the spontaneous ventilation of the patient, being the level of pressure exchange over the base pressure the only control variable that must be programmed. Because it is a mode controlled by the patient, the flow speed will adapt not only to the physical conditions of the system, but also to the inspiration and exhalation efforts of the patient, respecting the established pressure level. Due to this, it is defined as a spontaneous mode, assisted by the flow and limited by the pressure. As a spontaneous mode, the beginning of the inspiration will only happen upon detection of a signal of flow or pressure generated by the patient, finishing as standard when the flow speed slows to 25% of the initial speed. This value can be changed by the operator in about (percentages 80, 75, 70, 65, 60, 55, 50, 45, 40, 35, 30, 25, 20, 15, 10, 5) to adjust the end of the inspiration with the conditions and/or needs of the patient. As safety parameters, it is stipulated a criterion of maximum inspiratory time (adjustable) and a criterion of pressure (5 cmH2O over the maximum programmed pressure) which, in case of detection, will make the equipment pass to the exhalation phase. Once the control variable is the pressure level and the free variable is the volume, it is worth reminding that (in constant physical conditions) the latter will be proportional to the patient's inspiratory effort and the programmed support pressure. In case of programming 0 (zero) support pressure, pressure changes will not happen over the established base, therefore you will get a level of continuous positive airway pressure (CPAP), being the main difference in relation to the PSV the fact that the volume exchange during the inspiration will depend only on the patient, as the same will not receive any flow assistance. “To adjust this mode, the back-up ventilation shall be previously programmed”. SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION BY VOLUME WITH SUPPORT PRESSURE – SIMV (VCV)+PSV It is a ventilatory alternative which with you can start the weaning from the mechanical ventilation, its function is to lower the quantity of the ventilator's mandatory ventilations in order to have the patient spontaneously ventilate in each cycle, synchronizing the beginning of the mandatory cycle with the patient's inspiration effort. The mandatory ventilations will be controlled by volume (SIMV/VCV), reminding you that the function of the mandatory ventilations are of assuring a level of ventilation and oxygenation, avoiding any ventilatory contingence. One of the historical disadvantages of this mode was the muscular fatigue produced by the patient having to spontaneously breathe without any kind of assistance, so that nowadays this ventilation is assisted with support pressure (PSV). 53 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION WITH SUPPORT PRESSURE – SIMV (PCV)+PSV It allows spontaneous ventilations with support pressure and mandatory ventilations by controlled pressure, resulting in a descending flow and always respecting the inspiratory time and the frequency programmed by the operator. The support pressure and the controlled pressure are different on the fact that the support pressure finishes when it reaches the minimum patient flow (adjustable through the exhalation sensibility) and the controlled pressure is limited to the inspiratory time programmed by the operator. PRESSURE REGULATED WITH VOLUME CONTROLLED – (PRVC) It is an Assist/Control mode in which the operator must establish the desired tidal volume and the maximum pressure control level. Once initiated, the ventilator will automatically change the level of control pressure in order to assure the volume requested by the user. The main advantage of this mode is that you can assure the tidal volume with lower pressure level. NON-INVASIVE VENTILATION (NIV) This ventilatory mode gives the operator the possibility to ventilate the patient without invading his airway. The operational functioning is similar to the support pressure mode, with the following differences: - In case of leakage, there is compensation (up to 50 L/min) without producing self-triggering . - It is possible for the operator to manually establish the time limit variable in order to get a better expiratory synchrony. MANDATORY MINUTE VENTILATION WITH PRESSURE – (MMV+PSV) In this mode, the ventilators works operationally as in the support pressure mode, with the difference that the operator establishes a minimum minute volume which shall ventilate the patient, in case he doesn't reach this value, the ventilator will increase the support pressure in order to increase the ventilation and reach the desired value. BIPHASIC PRESSURE VENTILATION – (BIPHASIC) On the mode Biphasic Pressure, there are two levels of pressure in the airways, which are switching between themselves, and the patient can breathe spontaneously with an independent support pressure level. It is equivalent to a Support Pressure + PEEP mode, however with two PEEP values, a high one and a low one which go switching according to an established time for each one. PRESSURE SUPPORT VENTILATION WITH ASSURED TIDAL VOLUME – (PSV+VT) To use this mode, the operator shall set a tidal volume, which will be established as a minimum value for each patient's inspiration. With this ventilation mode, once the patient initiates the inspiration, the ventilator will control the pressure through the flow assist (PS), however, in case it is reached the flow value in which the exhalation phase should pass and the desired volume was not reached yet, it will behave as a flow controller until it insufflates the establish air quantity set by the operator. 54 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 NEONATAL VENTILATORY MODES It contains the ventilatory modes VCV, PCV, PSV, PSV/CPAP, Nasal CPAP, SIMV, Continuous Flow and HFNC. The modes (VCV, PCV, PSV, SIMV and HFNC) conceptually work in the same way as on the adult and pediatric categories and the operator shall adapt the programmed values to the category of patient which is being ventilated. In neonatal the guaranteed volume is performed by the ventilatory mode VCV, where the lung volume in each cycle is controlled and guaranteed by the equipment according to the programming of the operator. CONTINUOUS FLOW In this operative mode, the operator shall establish the flow speed, the inspiratory pressure limit (P CONT), the inspiratory time and the respiratory frequency. Once establishes all these values, the equipment will deliver flow at a fixed speed, closing totally or partially the active exhalation valve (to avoid surpassing the programmed pressure) during the inspiratory time established by the operator. During this mode the equipment has the possibility of performing a measurement of the delivered tidal volume only when the neonatal proximal flow sensor is connected. This ventilatory mode is also known as TCPL (Time Controlled with Pressure Limit). NASAL CPAP This mode allows the user to establish the CPAP level and connect it to the patient through a nasal cannula. The ventilator will compensate the leakage, keeping the pressure level established and allowing the spontaneous ventilation of the patient. HFNC – HIGH FLOW NASAL CANNULA This mode allows the user to establish the flow level and the concentration of inspired O2 through the adjustment of the FiO2 connecting the patient through a nasal cannula. The ventilator will compensate the leakages, maintainin the level of flow and FiO 2 established and allowing the patient’s spontaneous ventilation. BACKUP VENTILATION In case one wishes to visualize the configured parameters in Back Up ventilation during the patient's ventilation, he shall enter the “Menu”, “Ventilatory Modes”, by selecting the current mode the backup ventilation window will automatically open with the configured parameters. The goal of the backup ventilation is to ensure the patient’s ventilation during a spontaneous ventilatory mode in case of a prolonged apnea or any eventuality which difficults the equipment from recognizing the patient’s inspiratory effort. The backup ventilation is available in all ventilatory modes. I.e., in all the ventilatory modes the lung ventilator will send controlled ventilatory cycles in case the patient does not perform efforts which trigger the inspiratory sensibility, maintaining the oxygenation of the patient. In spontaneous ventilatory modes its programming is extremely important, since once the patient does not perform efforts, the equipment will respect the programmed time and configuration, delivering the backup ventilation (support). The parameters to adjust are: Ventilatory Modes: As default, the equipment proposes a mode controlled by volume, however the operator can choose for a ventilation mode controlled by pressure. Apnea Time: The maximum tolerable time by the ventilator without the patient starting an inspiration, once this time is elapsed, the equipment will send a sound and light alarm, ventilating the patient in a mode which is controlled, determined and programmed by the operator. 55 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Phase variables time and cycling: Ti, Fr, Vol. or Pres. The peep level continues being the one programmed in advance by the time the apnea occurred. For the equipment to operate in the desired spontaneous mode, the operator will have to “confirm” the backup ventilation from the Control Panel. If the selected mode is PSV/CPAP, NIV, (MMV)+PSV, (PSV + Assured VT), Nasal CPAP, Biphasic, will show the window for “Backup Ventilation”, where the programming is mandatory To confirm the programming the operator must press the key “confirm”. If the selected mode is SIMV(VCV)+PSV, SIMV(PCV)+PSV, (Biphasic), the ventilator will give the operator the possibility of using the backup ventilation; for this, it must be “confirmed” or “canceled” on the Control Panel. The ventilator will automatically leave this mode in case the patient recovers his spontaneous ventilation In the controlled modes such as VCV, PCV and PRVC the backup ventilation is adjusted by the respiratory frequency in which the patient’s minimum respiratory frequency is determined, in case the patient has spontaneous responses and surpasses the inspiratory sensibility threshold, the respiratory frequency will be higher than programmed, but it will never be less than the programmed backup frequency. LUNG MECHANICS It is accessed from the “Main Menu”. The equipment cannot be in Standby mode because there will be no access to the icon. AutoPEEP: The function is defined as the persistence of a positive alveolar pressure at the end of the expiration, not intentional, due to the presence of a pulmonary expiratory volume higher than the residual functional capacity foreseen. It occurs in patients undergoing mechanical ventilation as a consequence of initiating an inspiratory phase with positive pressure, before the exhalation time was sufficient for the complete exhalation of the previously inspired volume. The result of this phenomenon is a progressive increase in the pulmonary volume and pleural pressure with each breath. The function is not evident, being possible to change sharply the alveolar dynamics and constitute a recognized risk in situations that affect the flow during the expiration, leading to an unnecessary increase of the respiratory system’s mechanical work. To perform the measurement of the AutoPEEP Picture 62 function, press “Menu, Lung Mechanics” and Picture 63 “AutoPEEP”. When you select the icon the measurement of the function's value starts, where the ventilator will perform an exhalation pause up to 2.0 seconds with the exhalation valve closed in three consecutive cycles, and then showing on the graphical display the residual PEEP value that stays on the lung by the end of the expiration cycle. The results will be informed on the area D (functions area) during 30s, as on the picture below. Picture 64 56 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Compliance and Resistance: The compliance of the respiratory system is defined as the variation of volume per unit of pressure change. The function explores the thoracic lung distensibility and the airway resistance through the relation of the values obtained of the Peak Pressure, Plateau, PEEP and Tidal Volume. For the static compliance, the volume variations refer to the static plateau pressure, and for the dynamic compliance the volume variation refers to the peak inspiratory flow. The dynamic mechanical properties relates to the situations in which the flow varies over the time, while the static properties highlights the absence of flow. In order to access the function “Compliance and Resistance”, press “Menu, Lung Mechanics” and “Compliance and Resistance”, as soon as a new lateral window opens, put the “V.Tidal” value, then “confirm” and press “Start”. The values will appear as on the picture below. Picture 65 PV Curve with Low Flow: The ventilator will measure the lower and upper inflection points of the pressure curve per time through continuous insufflation of constant flows using low flow. To request the measurement of inflection points, the “Low Flow PV Curve” must be selected on “Menu, Lung Mechanic”. This feature prompts the operator to establish the Maximum Tidal Volume, Maximum Pressure and Flow which shall insufflate the patient's lungs during the maneuver. After placing the requested values, press the key “confirm”, the equipment will perform a prolonged expiration, leading the pressure from the base value to zero, so that afterwards it insufflates the air on the pre-determined flow until it reaches the established pressure and/or volume value. This way, it eliminates the resistive components from the airway, thus allowing the equipment to automatically establish the lower and upper inflection points which will be displayed on the screen as graphical forms. Slow Vital Capacity: The Vital Capacity is the maximum volume that can be exhaled after the maximum inspiration. The tool provides the maximum lung capacity through slow inspirations of the patient. To use this tool you must select “Menu, Lung Mechanic”, “Low Vital Capacity” and the equipment will display on the upper quadrant the values of CRV current (tidal) and CRV best, displaying the values in Liters. P0.1: The function P0.1 is a parameter used during the process of weaning from the mechanical ventilation and is defined as the airway occlusion pressure in during the first 100ms of the inspiration. To use this tool you must select “Menu, Lung Mechanic”, “P0.1” and the equipment will show the values on the upper quadrant of the screen. According to the III Brazilian Consensus on Mechanical Ventilation (2007), P0.1 values greater than 6 cmH2O predict weaning failure. Tobin Index (RSBI): The Tobin Index or RSBI (Rapid Shallow Breathing Index) is measured by the relation between the respiratory frequency and the tidal volume. In order to use this tool, the ventilator must be in Assisted Mode with maximum PEEP of 5 cmH2O and Support Pressure between 8 cmH2O and 10 cmH2O. After adjusting these parameters, select the option “Tobin Index” on the “Menu, Lung Mechanics” and the equipment will display the measured value on the upper quadrant of the screen. According to the III Brazilian Consensus on Mechanical Ventilation (2007), Tobin Index values greater than 104 cpm/L predict weaning failure. TOBIN INDEX'S VALUE MAY BE AFFECTED BY FACTORS SUCH AS: PEEP VALUE AND SUPPORT PRESSURE HIGHER THAN THE ONES DETERMINED BY THE MANUFACTURER. Stress Index: By selecting this option, the ventilator will establish a constant flow wave until delivering the Tidal Volume selected by the operator. Soon it will perform an analysis of the growing pendent of 57 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 the Pressure – Time curve, establishing n as the “Optimal Level of Distensibility”, which will allow the user to know the lung distensibility level by the following way: - n smaller than 1: The lung can continue increasing its volume. - n bigger than 1: The lung is over distended. 58 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 GRAPHICS In order to access the graphics menu, select “Menu, Graphics” and a screen will appear indicating the number of graphics to be displayed on the equipment's screen. The graphics are presented with color differentiation between the inspiratory and the expiratory phase. In inspiratory phase the equipment-controlled trigger cycles are showed in blue color and the spontaneous trigger cycles are presented in orange color, the expiratory phase is always in white color. One Curve: Picture 68 Two Curves: Picture 66 Picture 67 Picture 69 59 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 Three Curves: R 04-04(69) Rev. 06 Four Curvas: Picture 71 Five Curves: Picture 70 Picture 72 Scale/Time: Through this option, the operator is able to indirectly select the number of ventilatory cycles which will be displayed on the ventilator's screen, being its main utility the better visualization and interpretation of the graphics displayed by the ventilator. In case one wishes to change one of the graphics, or even select another function, pressing any curve on the screen will show another screen as on the picture aside which will allow you to change the selected curve or to select another function which is displayed there. When the Capnography is enabled, the function “CO2 Time” will be displayed in blue color. Picture 73 60 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 REMOTE MONITORING Within the option Remote Monitoring it is possible to select the options: Alarms Log: It will display a list with the events and alarms that were produced since the moment the equipment was turned on, where it shows the time, date and the kind of event or alarm that is activated and its priority level. It shows initially the 5 first events, as on the picture below. After turning off the equipment this log remains stored in the memory and may be consulted when restarting the lung ventilator. Picture 76 Trends: By accessing the option Trends, it is displayed in a graphic the stored variables according to the availability on the equipment. By pressing over the desired function, a window will open where the equipment provides 4 options of visualization: 8, 16, 24 or 72 hours. The vertical scale is automatically acomodated by the ventilator and cnanot be modified by the user. The measured variables are displayed in while color, while the red line shows the time during which the ventilator remained in Stanby. Picture 74 Picture 75 Lung Mechanics: On this window are presented numerical trends, showing the measured values of the last lung mechanics reading performed, having as goal to provide the operator with reference data, before performing a new exploration of the respiratory system. Circuit compliance value: Displays the compliance value measured during the initial line test or during the last circuit test. FUNCTIONAL SETUP PEEP Alarm: In this option it is possible to change the values of the PEEP alarm. The operator can choose to work within the limits of 2, 4, 6, 8 and 10 cm/H2O. THE ALARM WILL BE TRIGGERED WHENEVER THE PRESSURE IS BELOW OR ABOVE THE FIXED VALUE FOR PEEP, BEING ITS ACTIVATION IMMEDIATELY OR THROUGH PRIORITY, HAVING AS A MAXIMUM TIME 5 SECONDS. TGI (Intratracheal Gas Insufflation): Once this option is selected, the ventilator will send a flow of 6 L/m during the expiratory phase through the same output used by the nebulizer, without a time limit. The pure oxygen flow used may change the gas mixture which is provided to the patient. This variation can be lowered by adjusting the FiO2 value. Sighs: The option Sighs allow you to program: Sighs/Cycle (Sigh Quantity): the quantity of consecutive sighs (from 1 to 3) which happened in each cycle. Picture 76 Cycles/Hour: the quantity of times (5, 10, 15, 20) in which the sigh 61 of 88 Picture 78 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 cycle will repeat in an hour. V. Tidal: enters the value of additional volume (the same will be added to the already programmed volume) which will be delivered by the ventilator with each sigh. Change/Test of Circuit: It allows to repeat the Circuit Tests without the need to restart the ventilator when you change some component of the patient/ventilator interface, or when there are doubts about the hermeticity of the circuit. OPERATIVE SETUP Maintenance: In this option it's visualized the software version, the hours of use of the ventilator, as well as the corresponding hours to do the maintenances. THE MANUFACTURER RECOMMENDS TO RESPECT THE PREDICTED HOURS FOR THE CONTROL AND CALIBRATION OF THE EQUIPMENT'S INTERNAL ELEMENTS IN ORDER TO ENSURE ITS CORRECT OPERATION FOR A PROPER VENTILATION OF THE PATIENT AND THE PREVENTION OF SERIOUS FAILURE. (CHECK ANNEX 2 – PREVENTIVE MAINTENANCE). Language: In this option the operator can select in which language he wants the equipment. There are three options: Portuguese, English and Spanish. IT IS IMPORTANT TO REMIND THAT, IN ORDER TO PERFORM THE LANGUAGE CHANGE ON THE EQUIPMENT, THE OPERATOR NEEDS TO RESTART THE MACHINE. Picture 79 Altitude Compensation: In order to have a better accuracy on the measurement of the flow and volume, the equipment performs a correction Picture 80 according to the height above sea level at the place of its operation. For that, it is necessary to perform an altitude compensation. The adjustment is done in MASL (meters above sea level). The compensation can be up to 6000 masl. THE MANUFACTURER RECOMMENDS TO PERFORM THE ALTITUDE ADJUSTMENT FOR THE CORRECT OPERATION OF THE EQUIPMENT, IN CASE THAT IS NECESSARY. Date/Time: In this function you can configure the options: Time (24h format), Minutes, Day, Month and Year (two last numbers). Sound Level: This function adjusts the equipment's sound volume in a 20 to 20 scale and the loudest volume is 100. 62 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 CHAPTER 5 - ALARMS The alarms are used to watch the relation between the patient and the equipment, triggering when for some reason it reaches values of risk for the patient. The purpose of this section is to define the alarms categories, visual and auditory indicators and the urgency level of the operator's response. ALARM AUDIO INHIBITION (SILENCE) The operator will be able to momentarily silence the alarm, but always persisting the visual indication, for that the operator shall touch the Alarm indication. Touching it once, it triggers the inhibition for 30 seconds; touching quickly twice it triggers the inhibition for 60 seconds; continuously holding it (for longer than 2 seconds), it cancels the Audible Alarm inhibition. Picture 81 For indication of the Alarm's Audio Inhibition, the picture below (a bell crossed by a dashed X, symbol IEC 60417-5576) shows on the Icons Area (Picture 30), and it stays there for as long as the inhibition persists. If during this time a new or different condition of the alarm happens, it will be announced by eliminating the previous silence condition. The following description of the alarms is in sequence of Priority, from the Highest (Microprocessor) to the Lowest (Maximum Minute Volume). Adjustable Sound Level: This function adjusts the volume of the equipment's Audible Alarms in a scale of 20 to 20 and the highest volume is 100. This function may be found at “Menu” in “Operative Setup”. 63 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 HIGH PRIORITY ALARM CONDITION Picture 82 1 - MICROPROCESSOR This alarm is activated if a critical failure happens, preventing the microprocessor of controlling the equipment (inoperative ventilator). It lights a visual warning and triggers a continuous audible signal. Simultaneously, all the gas supply valves are disconnected and the anti-suffocation valve is enabled, which allows the environmental air input in the patient's circuit. 2 – LOW GAS SUPPLY PRESSURE This alarm is activated if the pressure of any of the supply gases is below 2,5 kg./cm2. This alarm is automatically canceled once the supply pressure is reestablished. It can't be manually changed, however it can be silenced for 60 seconds through the SILENCE option. 3 – LOW BATTERY This alarm is activated when the battery’s tension is lower than 10.8 V while the equipment is without external power supply. In case a battery failure is identified and turns the battery inoperative this alarm will be triggered. This alarm cancels itself automatically when reestablishing the battery charge. 4 – MAXIMUM INSPIRATORY PRESSURE This alarm is activated if the airway pressure surpasses the value fixed on the Maximum Pressure Limit control. It triggers the sound and a light indication that indicates High Inspiratory Pressure, it is deactivated if the cause that activated the alarm returns to values lower than the adjusted limit. 5 - INTERRUPTED CYCLE ALARM Available only on the modes with pressure control (PCV, PS). It will be activated in case the inspiration is interrupted by the Pressure Limit variable, indicating possible causes to the user, such as high rise time or airway obstruction. The pressure limit variable acts when the instantaneous pressure exceeds the programmed pressure in 15 cmH2O, for a pre-determined initial period. Its goal is to prevent hypoventilation or possible inadequacies of the equipment to the patient 6 - MINIMUM INSPIRATORY PRESSURE This alarm is activated if, by the end of an inspiration, the pressure didn't reach the value fixed on the Low Inspiratory Pressure control. It activates the sound and the visual indication of Low Inspiratory Pressure. Once the alarm is activated, by reestablishing the pressure it automatically deactivates the sound and the visual indication on the screen. It may indicate excessive leakage or disconnection of the patient line. 64 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 7 – DISCONNECTION OF THE PATIENT CIRCUIT This alarm is activated when the equipment cannot maintain the values of minimum pressure and PEEP due to a disconnection of the patient circuit, activating the sound and light indication, by connecting back the circuit and restablishing the pressure, the alarm is automatically deactivated. 8 – DISCONNECTION OF THE PROXIMAL FLOW SENSOR Available on the modes where the proximal sensor is applicable, this alarm immediately indicates that there is poor connection or disconnection between the connector of the proximal sensor and the equipment, activating a sound indication and light indication on the screen. Once the proximal sensor is connected again, the sound and screen indications are deactivated. 9 – HIGH PRESSURE OF SUPPLY GASES This alarm is activated if the pressure of any of these supply gas inputs (air or oxygen) is higher than 7,0 kg/cm2. This alarm cancels itself automatically when normalizing the supply pressures. MEDIUM PRIORITY ALARM CONDITION Picture 83 10 – MINIMUM FIO2 If upon mixing the O2 does not reach the minimum programmed value within the first 5 cycles, the visual and audible alarms will be activated; they can be silenced during 5 ventilatory cycles while the condition that generated it shall be fixed. 11 – MAXIMUM FIO2 It is triggered when the value of the FiO2 keeps above the value adjusted by the operator. The maximum FiO2 alarm can be disabled. This allows the operation with O2 concentrations equal to 100%. 12 - APNEA ALARM See apnea and back up ventilation. The Apnea alarm is triggered if the time between two consecutive inspiratory efforts to trigger the equipment is higher than the established apnea time. The equipment automatically changes to the Backup Ventilation mode, until the patient's demand is reestablished or another ventilation mode is selected. It activates the intermittent sound and the intermittent red warning indicating Apnea. It can be silenced through the Silence option. If the cause of the alarm activation disappears, it will silence automatically. 65 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 13 – MINIMUM TIDAL VOLUME It establishes minimum admissible value of inspired tidal volume. If the resulting value of inspired tidal volume maintains low for 3 ventilatory cycles, it activates the alarm with light, sound and messages on the screen. 14 – MAXIMUM RESPIRATORY FREQUENCY It activates if the resulting frequency is higher than the value established on the alarm. When there is leakage or disconnection of the circuit, it may activate an auto-cycling, which triggers the alarm. 15 – MINIMUM RESPIRATORY FREQUENCY It is activated if the resulting frequency is lower than the established value on the alarm and higher than the apnea gap time. In case the apnea gap time is exceeded, the apnea alarm will trigger and the ventilator enter in backup ventilatory mode. This alarm is automatically cancelled with the retake of the spontaneous respiratory frequency of the patient in a value superior to the alarm. 16 – POWER OUTAGE This alarm is activated in case of a power outage while the equipment is on. This alarm is automatically turned off when the power is reestablished . LOW PRIORITY ALARM CONDITION Picture 84 17 - MAXIMUM TIDAL VOLUME It established the maximum acceptable inspired tidal volume. If the resulting value of inspired tidal volume remains high during 3 ventilatory cycles, the alarm is triggered with audible indications and messages on the screen. 18 - I:E RATIO INVERSION It activates when the inspiration time is longer than the exhalation time. Due to this condition, it may be part of the ventilatory strategy, it does not indicate messages on the screen nor the sound alarms are activated, this condition makes the color which with are monitored the values become red, warning the operate of the occurred. 19 – PEEP ALARM 66 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 It activates when the value of PEEP is different in ± 4 cmH2O of the programmed value, to adjust this alarm it is enough to set the desired PEEP, and the ventilator will calcualte the necessary values of Maximum and Minimum PEEP. 20 – MINIMUM MINUTE VOLUME The value of minute volume remains below the value of the alarm established by the operator during 5 consecutive respiratory cycles. 21 - MAXIMUM MINUTE VOLUME The value of the minute volume remains above the value of the alarm established by the operator during 5 consecutive respiratory cycles. THE ALARMS OF THE INPUT GASES, POWER OUTAGE AND LOW VOLTAGE ARE ONLY ACTIVATED WHEN THE EQUIPMENT IS OPERATIONAL. THE ALARMS ARE NOT TRIGGERED IN STANDBY MODE. THE SOUND PRESSURE LEVEL OF THE ALARMS, MEASURED AT 1M AWAY FROM THE EQUIPMENT IS APPROXIMATELY 80DB. THE PRE-ADJUSTED ALARM VALUES ARE AVERAGE VALUES AND THEY SHALL BE ADJUSTED FOR EACH PATIENT, DEPENDING ON THE CLINICAL CASE AND THE SITUATION OF USE. THE USE OF PRE-ADJUSTED ALARM VALUES MAY BE DANGEROUS FOR THE PATIENT DEPENDING ON THE CASE AND ITS USE. IT IS RECOMMENDED FOR THE OPERATOR OR USER TO CHECK THE EQUIMENT, ALARMS CHECKING LIST, ESPECIALLY IN EVENTUAL OPERATOR OR USER CHANGES. AFTER COMPLETE POWER RETURN, THE EQUIMENT CONFIGURATION. OUTAGE/BATTERY DISCHARGE AND FURTHER RESTARTS WITH THE STANDARD ALARM IT SHALL BE AVOIDED TO ADJUST THE ALARMS IN EXTREME VALUES, THIS MAY TURN THE ALARMS USELESS FOR THE PATIENT'S SAFETY. EVERY TIME THAT A CONTROL VARIABLE IS ADJUSTED, ADAPT THE ALARMS' LIMITS ACCORDING TO THE VALUES OF THIS VARIABLE. IN CASE THE VENTILATOR BECOMES INOPERATIVE, A MESSAGE WILL BE DISPLAYED ON THE INFORMATION AREA RECOMMENDING THE EQUIPMENT TO BE RESTARTED. RELATION OF ALARM, POSSIBLE CAUSE AND NECESSARY ACTION Description Cause Necessary Action 1. Microprocessor - Serious failure of the equipment, it is immediately triggered after the occurrence. - It is caused by the crashing of the ventilator's central processing board. 67 of 88 - Don't use the ventilator in case this failure occurs; - Contact the technical support. LUNG VENTILATOR LEISTUNG LUFT 3 2. Low Supply Gas Pressure - The pressure of the High Air Pressure supply, O2 or the Oxygen cylinder is lower than 2.5kg/cm²; it triggers automatically after the occurrence. 3. Low Battery - The ventilator operates without power supply and the battery's tension is lower than 10.8 V, it triggers immediately after the occurrence. 4. Max. Insp. Pressure - During the inspiration, the airway pressure surpasses the maximum value established, it is triggered Immediately after the occurrence. 5. Interrupted Cycle - - The instantaneous inspiratory pressure surpasses in 12 cmH2O the programmed pressure, it is immediately triggered after the occurrence. 6. Min. Insp. Pressure - By the end of an inspiration, the pressure does not surpass the minimum value established, it immediately triggers after the occurrence. 7. Patient Circuit Discon. - Equipment cannot maintain the values of minimum pressure and PEEP due to a disconnection of the patient circuit, trigger immediately after the occurrence. 8. Discon. of Proximal Sensor - Indicates that there is a poor connection or disconnection between the proximal sensor’s connector and the equipment, trigger immediately after the occurrence. 9. High Supply Gas Pressure - The high pressure line of Air, O2 or the Oxygen cylinder is higher than 7,0 kg/cm². - Low gas supply pressure; - There are more equipment using AIR than the network can bear; - Pressure regulator of O2 cylinder cannot supply enough flow; - Battery is discharged or in a poor state of conservation; - Use of the equipment for a long period of time without external power supply; - Poor adaptation of the patient to the adjusted ventilatory parameters; - Change of the airway physical conditions; - Airway obstruction; - Patient's cough; - Patient circuit's tube partially or totally obstructed. R 04-04(69) Rev. 06 - Verify the High Pressure Gas network; - Adapt the network to the demand of necessary gas; - Change the regulator or adjust it (depending on each model). - Change the O2 cylinder. - Supply external power, proper electrical grid; - Contact the authorized technical service to change the battery; - Verify the patient's condition; - Check the ventilator's adjusted parameters; - Verify the patient circuit; - Evaluate the Respiratory Mechanics; - Correct the Alarm's Limit of the ventilatory parameters, if needed. - Poor adaptation of the patient to the ventilator; - Airway obstruction; - Patient's cough; - Programmed Rise Time is too high; - Verify the patient's condition - Check the ventilator's adjusted parameters; - Verify the patient / ventilator interface; - Lower the Rise Time; - Evaluate the synchrony between patient/ventilator; - Leakage or disconnection of the patient circuit; - Excessive inspiratory effort; - Verify the patient circuit; - Verify if the exhalation valve is correctly assembled. - Leakages or disconnection of the patient circuit. - Check the patient circuit; - Check if the exhalation valve is assembled correctly. - Poor connection ir disconnection of the equipment’s proximal sensor. - Check the connection of the proximal sensor with the equipment. - Low network line pressure; - Pressure network adjustment higher than the supported; - Pressure regulator of the Air - Check the high pressure gas netweork; - Adequate the gas network pressure of the hospital;. 68 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 or O2 cylinder is damaged with pressure higher than 7,0 kgf/cm²; 10. Minimum FIO2 - The value of FiO2 maintains itself below the established value of alarm, triggers after three consecutive ventilatory cycles. 11. Maximum FIO2 - The value of FiO2 maintains itself above the established value of alarm, triggers after three consecutive ventilatory cycles. 12. Apnea Alarm - O tempo compreendido entre dois esforços inspiratórios consecutivos é superior ao tempo de apneia estabelecido, aciona imediatamente após a ocorrência. 13. Minimum Tidal Volume - The Volume's value remains below the established value of the alarm during 3 consecutive ventilatory cycles, triggers after the third cycle. 14. Maximum Respiratory Frequency - The respiratory frequency is higher than the established value. It triggers immediately after the occurrence. 15. Minimum Respiratory Frequency - The spontaneous respiratory frequency is lower than the programmed value and higher than the selected apnea value. 16. Power outage - Failure of the power supply. It is triggered immediately after the occurrence. 17. Maximum Tidal Volume - The exhaled volume remains above the adjusted volume's value. It is triggered after 3 consecutive cycles. R 04-04(69) Rev. 06 - Replace the regulator or adjust it (depending on each model). - There is no connected AIR or pure O2 at the ventilator’s input. - End of the lifespan of the Oxygen concentration reading cell. - Check the gas inputs; - Contact the Authorized Technical Support for replacement of the cell. - There is no connected AIR or pure O2 at the ventilator’s input. - End of the lifespan of the Oxygen concentration reading cell. - Check the gas inputs; - Contact the Authorized Technical Support for replacement of the cell. - The patient is not spontaneously breathing/ - Obstruction on the patient/ventilator interface; - Adjusted time for apnea is too low; - Trigger sensibility is too high; - AutoPEEP presence; - Failure on the exhalation flow sensor. - Leakage or disconnect of the patient circuit. - Increase of the airway resistance or reduction of the lung's compliance value. - The patient is spontaneously breathing at a high frequency; - Leakages or disconnection may cause the auto-trigger. - The patient is spontaneously breathing at a low frequency; - Programmed inspiratory sensibility is high and the patient doesn’t match the necessary effort. - The power line voltage is below the specified value; - The cable that connects to the power line was disconnected or broken; - Internal fuse is blown; - The airway resistance or the pulmonary compliance may have improved (in pressure control modes). 69 of 88 - Evaluate the patient's condition (consider changing to a mandatory mode); - Verify the patient/ventilator interface; - Evaluate the Synchrony between the patient/ventilator; - Calibrate or replace the expiratory flow sensor. - Evaluate the patient's condition. - Verify the ventilatory parameters; - Correct the Alarm's limit if necessary; - Evaluate the condition of the patient; - Verify the ventilatory parameters; - Verify the patient/ventilator interface; - Correct the alarm's limit if necessary. - Evaluate the condition of the patient; - Verify the ventilatory parameters; - Correct the alarm's limit if necessary; - Arrange power line as per the specifications; - Verify the power line cable; - Contact an Authorized Technical Support. - Evaluate the patient's condition. - Verify the ventilatory parameters; - Correct the Alarm’s limit if necessary; LUNG VENTILATOR LEISTUNG LUFT 3 18. I:E Ratio Inversion - The inspiratory time is longer than the exhalation time, it is triggered immediately after the occurrence. 19. PEEP Alarm - The value of PEEP remains below or above the established value. It is immediately triggered after the occurrence.. 20. Minimum Minute Volume - The value of the minimum minute volume remains below the one established by the operator. It is triggered after 5 consecutive cycles. 21. Maximum Minute Volume - The value of the minute volume remains above the value established by the operator. It is triggered after 5 consecutive cycles. - Adjust of inspiratory time longer than the exhalation time. R 04-04(69) Rev. 06 - Verify the ventilatory parameters. - Excessive leakages on the patient circuit; - Failure of the exhalation flow sensor. - If being used, verify the bacteriological filter and change it if necessary; - Verify if the exhalation valve is correctly assembled. - Leakages or disconnections of the patient circuit (in volume control modes); - Increase of the airway resistance, or reduction of the lung's compliance (in pressure control modes); - Evaluate the patient's condition; - Verify the ventilatory parameters; - Correct the Alarm's limit if necessary; - The patient is spontaneously breathing at a high frequency; - Leakages and disconnections may cause the auto-trigger; - Failure on the exhalation flow sensor; - Accumulated water on the exhalation flow sensor; - Evaluate the patient's condition; - Verify the ventilatory parameters; - Verify the patient/ventilator interface; - Correct the Alarm's limit if necessary; - Calibrate or change the exhalation flow sensor. THE CHART ABOVE IS INDICATED IN RELATION TO THE PRIORITY OF ALARM'S TRIGGERING, CONSIDERING 1 AS THE HIGHEST PRIORITY AND 19 AS THE LOWEST PRIORITY. WHEN TWO ALARMS CONDITIONS ARE SIMULTANEOUSLY TRIGGERED, THE VENTILATOR WILL TRIGGER THE ONE WITH THE HIGHEST PRIORITY, ACCORDING TO THE RANKING INDICATED ON THE CHART ABOVE (RELATION OF ALARM, POSSIBLE CAUSE AND NECESSARY ACTION). THE ALARM SYSTEM HAS ITS PRIORITIES FIXED, AS WELL AS THE DELAYS AND THE CHARACTERISTICS INDICATED ON THE CHART ABOVE ( RELATION OF ALARM, POSSIBLE CAUSE AND NECESSARY ACTION), IT CANNOT BE CHANGED BY THE OPERATOR OR ANY OTHER METHOD. 70 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 COLORS AND MEANINGS OF THE LUMINOUS INDICATIONS These signals were developed in accordance with the Standard IEC 60601-1-8, see the chart with the meanings of the Alarms from that standard: COLOR ALARM PRIORITY Red High Yellow Medium Yellow Low MEANING The announced failure may cause Death or Irreparable Harm immediately or in the mediumterm, or Immediately Irreparable Harm. The announced failure may cause Death or Irreparable Harm in the long-term; Repairable Harm in the medium-term or Lesser Harm or discomfort immediately. The announced failure may cause Repairable Harm in the long-term or Lesser Harm or Discomfort in the medium or long-term. Position of the Operator Danger. It requires an immediate response from the operator. Caution. It requires a response from the operator. Caution. It requires a response from the operator. SETUP OF THE ALARMS, SOUND AND LUMINOUS SIGNALS ON THE SCREEN COLOR ALARM PRIORITY LUMINOUS SIGNAL ON THE SCREEN AUDIBLE SIGNAL Red High Intermittent Alarm Signal 10 pulses with 10 seconds interval Yellow Medium Intermittent Alarm Signal 3 pulses with 10 seconds interval Yellow Low Continuous Alarm Signal 2 pulses with 20 seconds interval STANDARD ALARMS SETUP Max. P. = 40 cmH2O Min. P. = 5 cmH2O VCV ADULT PCV PSV (VCV/PCV) + PSV Max. Vol. = 0,600 L Min. Vol. = 0,150 L Max. Minute Vol. = 15 L Min. Minute Vol. = 1 L Max. Freq. = 30 cpm PEEP = 4 cmH2O Apnea = 15 seconds PEDIATRIC VCV 71 of 88 Max. P. = 30 cmH2O LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 PCV Min. P. = 5 cmH2O PSV Max. Vol. = 0,4 L (VCV/PCV) + PSV Min. Vol. = 0,05 L Max. Minute Vol. = 10 L Min. Minute Vol. = 0,5 L Max. Freq. = 30 cpm PEEP = 4 cmH2O Apnea = 15 seconds ALARMS CHECKING LIST Max. P. Min. P. VCV ADULT PCV PSV (VCV/PCV) + PSV Max. Vol. Min. Vol. Max. Minute Vol. Min. Minute Vol. Max. Freq. PEEP Apnea Max. P. Min. P. VCV PEDIATRIC PCV PSV (VCV/PCV) + PSV Max. Vol. Min. Vol. Max. Minute Vol. Min. Minute Vol. Max. Freq. PEEP Apnea 72 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 CHAPTER 6 – EXHALATION VALVE, PATIENT CIRCUIT AND PROXIMAL SENSOR EXHALATION VALVE The picture below shows the assembly of the exhalation valve. Picture 85 WHEN ASSEMBLYING THE EXHALATION VALVE, PUT THE MEBRANE (DIAPHRAGM) AS SHOWN ON THE PICTURE WITH THE CURVE SALIENCE DOWN. THE BIGGER HOSE MUST BE ON THE EXTERNAL SIDE OF THE EXHALATION VALVE, AT THE TERMINALS MARKED WITH A SALIENT DOT. DO NOT DRY NOR CLEAR THE EXHALATION VALVE WITH COMPRESSED AIR. DO NOT INSERT IN THE EXHALATION VALVE PIERCING OR CUTTING MATERIALS. 73 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 PATIENT CIRCUIT The picture below shows the assembly of the patient circuit. Picture 86 PROXIMAL SENSOR The proximal sensor must be connected to the Y Connector and the Endotracheal Tube in such a way that the reading hoses of the sensor stay upwards and the connection with the patient is higher than the side connected to the Y Connector, as shown on the picture below: 74 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 Picture 87 WHEN COMPONENTS OF THE BREATHING CIRCUIT, OTHER COMPONENTS OR SUBASSEMBLIES FOR THE VENTILATOR'S RESPIRATORY SYSTEM ARE ADDED, THE PRESSURE GRADIENT THROUGH THE VENTILATOR'S RESPIRATORY SYSTEM, MEASURED IN RELATION TO THE PATIENT’S CONNECTION INPUT, MAY INCREASE. UPON REDOING THE CIRCUIT TEST (SELF-TEST), THIS GRADIENT IS AUTOMATICALLY CORRECTED BY THE EQUIPMENT. A BAD CLOSURE OF THE MEMBRANE (DIAPHRAGM) MAY CAUSE THE READING OF THE EXHALED PARAMETERS TO BE WRONG. THE MEMBRANE (DIAPHRAGM) MUST BE LEANED AGAINST THE COVER'S ACCOMODATION FOR WHICH IT IS CONVENIENT TO FIRST PUT IT ON THE COVER AND MAKE SURE IT IS WELL LEANED AND ONLY THEN SCREW THE COVER ON THE BODY. AT THE END OF THE SCREWING, DON'T MAKE A STRONG ADJUSTMENT OF THE COVER TO THE BODY. ADJUST IT SOFTLY. VERIFY IF THE TWO PLASTIC TUBES ARE COMPLETELY CLEAR OF HUMIDITY, SO THAT THEY CAN CORRECTLY MEASURE THE PRESSURE DIFFERENCES. WHEN STERILIZING THE VALVE, DO NOT DISCONNECT THE PLASTIC TUBES BECAUSE THEY HAVE DEFINED POSITIONS AND TO AVOID DEFORMING THE INTERNAL MEMBRANE (TRANSPARENT), BECAUSE THIS ONE IS RESPONSIBLE FOR ESTABLISHING THE PRESSURE DIFERENCES WHICH THE EQUIPMENT MEASURES IN ORDER TO ESTABLISH THE PATIENT'S OUTPUT PARAMETERS. IF THE MEMBRANE IS FOLDED OR DAMAGED THE MEASURING WILL NOT BE CORRECT. IT MUST BE KNOWN THAT DURING THE USE OF THE EQUIPMENT IN A PATIENT, AFTER A DETERMINED PERIOD OF TIME, THE PARAMETERS MEASURED AT THE INITIAL TEST OF THE BREATHING CIRCUIT AND PERIPHERALS, MAY VARY DUE TO THE TEMPERATURE, HUMIDITY, PLACE, ETC... THE VARIATIONS ON THE CIRCUIT MAY BE MORE SIGNIFICATIVE WITHIN THE FIRST HOURS OF OPERATION, STABILIZING LATER. 75 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 CHAPTER 7 – CLEANING, DISINFECTION AND STERILIZATION The Exhalation Valve and the Patient Circuit are classified as semi critical articles, which makes it necessary to perform a high level disinfection or sterilization for the reuse. Once the material, for any circumstance contacts sterile tissue or vascular system, it shall be sterilized. To perform this, the procedures indicated on this protocol shall be followed, according to the classification of the valve after its use, which are: DISASSEMBLY OF THE EXHALATION VALVE AND THE PATIENT CIRCUIT The Exhalation Valve and the Patient Circuit must be disassembled before the beginning of the steps below for a better effectiveness of the procedures. In order to do that, follow the instructions below: 1. 2. 3. 4. Remove the exhalation valve from the patient circuit; Remove the exhalation valve's cover from its body by unscrewing it; Extract the silicon membrane; The complete disassemble of the Exhaust Valve will result in 6 components (as picture below): Valve’s Cover, Silicon Membrane, Valve’s Body, Flow Sensor and Hose; 5. The complete disassemble of the Patient Circuit (Picture 86) will result in some components (depending on the circuit): Patient Circuit's Tracheas (4x) or (5x), Y Connector, Connectors (if there are) and Drains (if there are). Picture 88 76 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 CLEANING It is the process which aims at removing visible dirt – organic and inorganic and, hence removal of the microbial load. The cleaning of components such as valve, patient circuit, proximal sensor should always precede the process of disinfection or sterilization, being the most important process of the decontamination. If there is dirt on the valve, on the circuit, or the proximal flow sensor, it won't have success in the next procedures. The valve and the circuit must be cleaned for every patient, initially following the disassemble recommendations as per the disassembly item. After this first step, we recommend to follow the instructions mentioned below: EXHALATION VALVE – PROXIMAL SENSOR Immerse the components in detergent solution, preferably using a multi-enzymatic detergent in a solution of 3 ml for each liter of water during 5 minutes; Rinse the components with plenty of clean water, removing all the solution with the aid of a sponge. PATIENT CIRCUIT Perform the washing in a validated thermo-disinfector using enzymatic detergent and purified water, heated at 45°C ±5°C, during 55 minutes and finishing with 3 rinses. OS AGENTES DE LIMPEZA MUITAS VEZES CONTÊM ADITIVOS QUE PODEM DANIFICAR OS MATERIAIS UTILIZADOS NA VÁLVULA EXALATÓRIA. NO CASO DE QUALQUER DÚVIDA, FORNECEDOR/FABRICANTE DEVE SER CONTATADO. NÃO É ACONSELHÁVEL A UTILIZAÇÃO DE ÁGUA EM JATO E /OU ÁGUA SOB PRESSÃO PARA O ENXÁGUE DOS COMPONENTES, UMA VEZ QUE PODEM OCORRER DANOS QUE COMPROMETAM O FUNCIONAMENTO DA VÁLVULA. A ESPONJA UTILIZADA PARA A REMOÇÃO DE SUJIDADE APÓS A IMERSÃO EM SOLUÇÃO DEVE SER MACIA, COM AUSÊNCIA DE PALHAS DE AÇO. RECOMENDAMOS CUIDADOS NA MANIPULAÇÃO DA MEMBRANA DE SILICONE PARA QUE A MESMA NÃO DOBRE NEM DANIFIQUE. RECOMENDA-SE O ENXÁGUE COM ÁGUA TRATADA, LIVRE DE CONTAMINANTES, ENDOTOXINAS E MINERAIS. OS COMPONENTES PODEM SER LIMPOS EM LAVADORAS ULTRASSÔNICAS QUE SÃO POTENCIALIZADAS PELO ULTRASSOM. DRYING Drying is an important process, because the humidity interferes on the processes of disinfection and sterilization. We recommend the drying for each component as described below: 77 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 VALVE DRYING METHODS COMPONENTS Air Dryer (warm or cold) Valve’s body X X X Valve’s cover Flow sensor Clean cloth (ex: compress) X X X Membrane Medicinal Compressed Air X X DRYING OF THE VALVES MUST BE PERFORMED ACCORDING TO THE STANDARDS OF SERVICE FOR RESPIRATORY COMPONENTS DRYING, PAYING ATTENTION TO THE MAXIMUM TEMPERATURE SPECIFIED IN EACH PROCESS. AFTER DRYING, THE COMPONENTS MUST BE INSPECTED TO VERIFY THE AUSENCE OF DIRT. THE NEXT STEPS SHALL BE TAKEN ONLY IF THE COMPONENTS ARE COMPLETELY CLEAN AND FREE OF ORGANIC AND INORGANIC MATTER. THE CLOTH USED FOR DRYING MUST BE SOFT, MUST NOT RELEASE FIBERS AND MUST BE MADE OF A LIGHT COLOR IN ORDER TO FACILIATE THE VISUALIZATION OF THE MATERIAL'S DIRT. PATIENT CIRCUIT Dry in automatic dryers, operating in 60°C ± 10°C for 60 minutes. After drying the materials must be packed in cirurgical-grade paper, with an indicator of sterilization printed in transparent plastic filme with identification of sterilization date, sterilization validity, lot number, customer’s name and description of the material. STERILIZATION It is the process which destroys all kinds of microbial life and is performed by physical or chemical procedures. The methods indicated for the sterilization of the components are: THE STERILIZATION METHODS ARE FOLLOWED ACCORDING TO THE STANDARDS ISO 17664, ISO 11135-1 AND ISO 17665-1 PHYSICAL METHOD PATIENT CIRCUIT Autoclave Under Saturated Steam Pressure: The tracheas must be sterilized in proper individual packages without touching the chamber walls, during 4 minutes at 134°C / 137°C. 78 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 EXHALATION VALVE General specifications: o Pre-conditioning Vacuum..........................................3 pulses Humidification................................3 steam discharges o Sterilization cycle Time..........................................15 minutes Temperature................................134°C Pressure.......................................2,2 bar o Drying cycle High pressure vacuum..............20 minutes IT IS RECOMMENDED THE USE OF INDICATORS OF THE STERILIZATION PROCESS TO CONTROL THE PERFORMANCE RESULTS OF THE STERILIZATION CYCLE. PERSONAL PROTECTIVE EQUIPMENT USED BY PROFESSIONALS THAT WILL PERFORM THE PROCEDURES MENTIONED ABOVE IS DETERMINED AND INSPECTED BY THE HEALTH SERVICE ACCORDING TO THE STANDARDS AND STANDARDIZED ROUTINES BY THE SAME. USEFUL LIFE OF ACCESSORIES EXHALATION VALVE Maximum Number of Cleaning/Sterilization cycles: 50 cycles. PATIENT CIRCUIT Maximum Number of Cleaning/Sterilization cycles: 6 cycles. DO NOT PILE THE TRACHEAS, DO NOT LEAN THEM AGAINST THE CHAMBER WALLS, AND DO NOT PUT THE PIECES WITHOUT THE PROPER PACKAGE. THE RESPIRATORY CIRCUIT, THE EXHALATION VALVE AND THE ACCESSORIES, SUCH AS THE ASPIRATION BOTTLE AND THE HUMIDIFER, SHALL BE CLEANED, STERILIZED AND DISINFECTED BEFORE THE FIRST USE. 79 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 ANNEX 1 – VENTILATOR LUFT3’S ACCESSORIES Illustrative images DESCRIPTION ARTICULATED ARM FUNCTION ARTICULATED SUPPORT FOR THE PATIENT CIRCUIT MONITOR’S POWER SUPPLY CABLE CABLE FOR POWER SUPPLY INPUT OF THE MONITOR TOUCH CONTROLLER CABLE SIGNAL CABLE TO CONTROL THE TOUCH SCREEN POWER CABLE ELECTRICAL POWER SUPPLY NOTE: ONLY THE CABLE INCLUDED WITH THE EQUIPMENT SHALL BE USED VIDEO CABLE CABLE FOR VIDEO SIGNALS 80 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 PATIENT CIRCUIT (ADULT CIRCUIT) R 04-04(69) Rev. 06 THE PATIENT CIRCUIT IS BUILT UNDER THE STANDARD ISO 5367 AND REGISTERED AT THE MINISTRY OF HEALTH BY THE MANUFACTURER AIR FILTER AIR INPUT COALESCENT FILTER HIGH PRESSURE HOSE (MEDICAL AIR) GAS SUPPLY (MEDICAL AIR) STANDARD LENGTH: 3 METERS OPTIONAL LENGTH: SPECIAL MEASUREMENT HIGH PRESSURE HOSE (MEDICAL OXYGEN) GAS SUPPLY (MEDICAL OXYGEN) STANDARD LENGTH: 3 METERS OPTIONAL LENGTH: SPECIAL MEASUREMENT USER MANUAL INFORMATION ABOUT THE FUNCTIONS, REQUIREMENTS AND OPERATION OF THE EQUIPMENT 81 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 LOCKNUT USED TO FASTEN THE EQUIPMENT ON THE TROLLEY TROLLEY SUPPORT DESK FOR THE EQUIPMENT, ON WHEELS WITH A BRAKE SYSTEM TEST RESISTANCE IT SIMULATES THE RESISTANCE TO VERIFY THE CYCLING OF THE EQUIPMENT EXHALATION VALVE ONLY THE MODEL SUPPLIED WITH THE VENTILATOR LUFT3 MUST BE USED Merely illustrative images. 82 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 OPTIONAL ACCESSORIES (NOT INCLUDED WITH THE EQUIPMENT) Must be acquired separately. OPTIONAL PATIENT CIRCUIT WITH EXHALATION VALVE AND NEBULIZER (PEDIATRIC/NEONATAL CIRCUIT) INTERFACE EQUIPMENT-PATIENT NOTE: ONLY THE MODEL PROPER FOR THE VENTILATOR LUFT 3 SHALL BE USED TEST LUNG (ADULT) VERIFICATION OF OPERATION AND CYCLING OF THE EQUIPMENT TEST LUNG (NEONATAL) VERIFICATION OF OPERATION AND CYCLING OF THE EQUIPMENT CAPNOGRAPHY SENSOR “MAINSTREAM” SENSOR FOR CAPNOGRAPHY PROXIMAL SENSOR PROXIMAL FLOW READING LUFT 3 SOFTWARE SOFTWARE WHICH ALLOWS CONNECTION OF THE EQUIPMENT WITH A COMPUTER Merely illustrative images THE USE OF ACCESSORIES AND CABLES WHICH ARE NOT SPECIFIED BY LEISTUNG EQUIPMENTOS LTDA. MAY RESULT IN ELECTROMAGNETIC EMISSION INCREASING OR IMMUNITY REDUCTION OF THE EQUIPMENT. 83 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 ANNEX 2 – PREVENTIVE MAINTENANCE A preventive maintenance shall be performed according to the following schedule: Maintenance 1st 2nd 3rd 4th 5th Hours of Use 3500 7000 10500 14000 17500 It is recommended to contact Leistung Equipamentos to send the equipment after exceed the hours of the chart above or 1 year after performing the last preventive maintenance. The preventive maintenance shall be performed by qualified personnel and respecting its corresponding protocols. To access the function which indicated the preventive maintenances press “Menu”, “Operative Setup”, “Maintenance”. LUFT 3 RUNS AN AUTO-TEST OF THE BATERRY CONDITION EVERY 5 MINUTES, HOWEVER IT IS RECOMMENDED TO DISCONNECT IT FROM THE POWER GRID (NETWORK) AT LEAST ONCE IN A MONTH, LEAVING IT ON ITS AUTONOMY, FOR MAINTENANCE AND FOR TESTING THE BATTERY CONDITION. THE MANUFACTURER DOES NOT TAKE RESPONSABILITY FOR ANY DAMAGE CAUSED OR SPECIAL DAMAGES. WHEN THE HOURS OF USE EXCEED THE HOURS INDICATED ON THE CHART ABOVE, THE EQUIPMENT WILL DISPLAY AN AUTOMATIC MESSAGE WHEN TURNING ON THE EQUIPMENT WITHOUT BLOCKING ANY FUNCTIONS. ALARMS SYSTEM INTEGRITY TEST 1 – With the test lung connected to the equipment, turn the “VCV” mode on; on the alarms area configure the P.max for a value lower than the peek value displayed on the screen. It shall trigger the alarm “MAXIMUM INSPIRATORY PRESSURE”. 2 – Adjust the alarm value of P.max for a value higher than the Peak showed on the screen and disconnect the test lung. It shall trigger the alarm “MINIMUM INSPIRATORY PRESSURE”. 3 – Adjust the alarm value of F.max for a value lower than the one displayed on the screen, after 10 cycles it shall trigger the alarm “MAXIMUM INSPIRATORY FREQUENCY””. 4 – Adjust the alarm value of Minimum Volume for a value higher than the one showed in “Vt”, it shall trigger the alarm “MINIMUM TIDAL VOLUME”. 5 – Adjust the alarm value of Maximum Volume for a value lower than the one showed in “Vt”, it shall trigger the alarm “MAXIMUM TIDAL VOLUME”. 6 – Disconnect the Pneumotachograph from the exhalation valve, it shall trigger the alarm “PEEP”. Connect it again. 7 – Select one of the spontaneous mode (PSV), after elapsing the adjusted Apnea time, it shall trigger the “APNEA CONDITION” alarm”. 84 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 8 - Disconnect the high pressure Air hose from the gas inlet, it shall trigger the “LOW O2/AIR INPUT PRESSURE”. Put the air hose again and repeat this procedure with the OXYGEN hose, it shall trigger the same alarm. 9 – Disconnect the power supply cable from its jack, it shall trigger the alarm “POWER FAILURE”. 10 – Keeping the equipment without power connection for about 75% of its autonomy shall trigger the alarm “LOW BATTERY”. IT IS RECOMMENDED TO PERFORM THIS TEST ALONG WITH THE PREVENTIVE MAINTENANCE, ALREADY DESCRIBED ON THE BEGINNING OF THIS CHAPTER. EACH TEST IS INDEPENDENT AND MAY BE PERFORMED OUTSIDE THE SUGGESTED ORDER. THE TIME BETWEEN THE PARAMETERS ADJUSTMENT AND THE ALARMS TRIGGERING CAN VARY IN EACH TEST. 85 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 ANNEX 3 – BLOCK DIAGRAM The picture below represents the Ventilator LUFT3's pneumatic diagram. Picture 89 86 of 88 R 04-04(69) Rev. 06 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 ANNEX 4 – WARRANTY This equipment has a warranty of 12 (twelve) months, counting from the date of the purchase, being them 03 (three) months corresponding to the legal term and 09 (nine) months the contractual term, where Leistung is responsible for any failure or manufacturing defect. The warranty will only have validity with the presentation of this term duly stamped and signed by LEISTUNG EQUIPAMENTOS LTDA., accompanied with the corresponding Invoice. On the process of observing irregularities within the warranty time, shall the purchaser in possession of the mentioned documents report it to the aftersales service of LEISTUNG EQUIPAMENTOS LTDA. through the Phone: +55 47 3371-2741 or through the e-mail posvendas@leistungbrasil.com. The installation of the equipment is purchaser's responsibility and will have to be made in the exact terms as described on the instructions manual, under penalty of losing the warranty. The same will happen (warranty loss) if the use and handling of the equipment do not follow the technical specification described on the manual, including the preventive maintenance periods. Beside the already established, it will also cause the loss of warranty, the occurrence of the following situations caused by the purchaser or third parties: a) Finish of the warranty time; b) The identification level is changed, damaged or removed from the equipment, as well as its seal; c) When the installation, use and maintenance of the equipment is not performed according to the specifications of the instructions manual; d) When it is observed that the damages were caused by circumstances related to the deficiency of the electrical and/or pneumatic installation, or by fluctuations/differences of tension in which the equipment is operated; e) When the defects are caused by drops, hits or any other kind of external damage, or also by the bad use of the equipment; f) When it is detected the opening of the equipment by people other than LEISTUNG EQUIPAMENTOS LTDA.'s technical support. 87 of 88 LUNG VENTILATOR LEISTUNG LUFT 3 R 04-04(69) Rev. 06 ANNEX 5 – GLOSSARY ALARM: It is a light or audio signal, or both kinds, that occurs when there is any variation on the equipment. ASSISTED EXPIRATION: It is the expiratory flow generated by the negative switch at trans-respiratory pressure due to an external agent (such as a respiratory pressure drop to a value lower than the reference value). ASSISTED INSPIRATION: It is the inspiratory flow generated by positive switch at trans-respiratory pressure due to an external agent (such as an increment in the respiratory pressure generating a value higher than the reference value). ASSISTED VENTILATION: It is the process of providing a respiration with positive pressure as a reaction of the patient's inspiratory effort. AUTOPEEP: It is the pulmonary pressure at the end of the expiration ; COMPLIANCE: It is the relation between volume and pressure. CYCLE: Ending a mechanically supported inspiration . EXPIRATORY PHASE (EXPIRATION): It is the part of the ventilatory cycle which covers from the beginning of the expiratory flow until the beginning of the inspiratory flow. EXPIRATORY TIME: It is the duration of the expiratory phase, expressed in seconds. FLOW: Traffic gas rate that gets in and out of the lungs. I:E RATIO: It is the relation between the inspiration time and the expiratory time. INSPIRATORY PHASE (INSPIRATION): The part of the ventilatory cycle which covers from the beginning of the inspiratory flow until the beginning of the expiratory flow. In the inspiratory phase, it is included any inspiratory pause . INSPIRATORY TIME: It is the duration of the inspiratory phase, expressed in seconds. As the inspiratory time increases, the mean respiratory pressure and the I:E ratio increases too. LIMIT: To establish a maximum value of pressure, volume and flow during the inspiration with mechanical support (or expiration), the maximum volume pre-established for the pressure, volume or flow during an assisted inspiration (or expiration). NEBULIZER: An aerosol generator that requires a gas source to nebulize liquid medicines. NON-INVASIVE VENTILATION: Ventilation technique performed through facial mask. PEEP: Positive End-Expiratory Pressure. SENSIBILITY: It is the measurement of the patient's effort to start a cycle. SIGHS: It is a number of additional respirations performed during a defined time interval. SPONTANEOUS BREATHING: It is the breathing started and finished by the patient. STATIC COMPLIANCE: It is the relation between the volume and the pressure in spots without gas flow. TGI: Tracheal Gas Insufflations during the expiration. TRANS-RESPIRATORY PRESSURE: The difference of pressure between the respiratory airway and the surface of the body. VOLUME: Space occupied by material measured in cubic millimeters or liters. WEANING: Gradual reduction of ventilation support. WOB: Work of Breathing. Jaraguá do Sul, February 19, 2018. _____________________________ MATEUS EMRICH MONNERAT TECHNICAL RESPONSIBLE 88 of 88