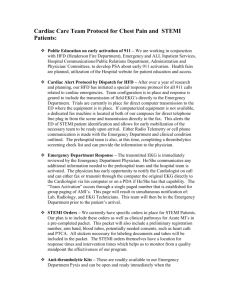
© The State of Queensland (Queensland Health) 2012 Contact CIM@health.qld.gov.au (Affix identification label here) URN: STEMI Clinical Pathway Family name: (ST-Elevation Myocardial Infarction) Given name(s): For Interventional Cardiac Facilities Address: Facility: Date of birth: Sex: M F I Clinical Pathways Never Replace Clinical Judgement Care Outlined In This Pathway Must be Altered If It Is Not Clinically Appropriate For The Individual Patient Pathway commenced Date:.......................................... Time:......................... Initials:............................... Has patient transferred from another facility? STEMI date:............................... Time:............................... Initials:.................... If STEMI > two days ago, commence daily care on page 5 Late presentation: Pathway ceased Yes Yes Date:................................ Time:.................................... Date:.......................................... Time:......................... Reason:.................................................................... Initials:.................. Treating consultant (print name):................................................................................................................. Thrombolysis: Yes Date:................................ Time:............................... Type:................................................................................................................. No Chest x-ray: Yes Date:................................ Echocardiogram: Scheduled? Yes Date:................................ Performed? Yes Date:................................ Angiogram: Scheduled? Yes Date:................................ Performed? Yes Date:................................ Angioplasty (PCI): Scheduled? Yes Date:................................ Performed? Yes Date:................................ Not for angiogram, Reason:................................................................................................ Not for PCI, Reason:.................................................................................................................. Coronary Artery Bypass Grafts (CABG): Surgical referral completed? Yes Date:................................. Cardiac surgeon review? Yes Date:................................. Scheduled for CABG? Yes Date:................................. Mat. No.: 10206020 Documentation Instructions: v6.00 - 02/2012 Not for echocardiogram, Reason:................................................................................. • • • • • • Initials - Indicates action / care has been ordered / administered. N/A - Indicates preceding care / order is not applicable. Crossing out - Indicates that there is a change in the care outlined. V - Indicates a variation from the pathway on that day, in that section. When applicable flag it in the “Variance column”, then document in the free text area as instructed. Key Medical Nursing Pharmacy Allied Health Cardiac Rehab Symbols guide care to a primary professional stream, it is a visual guide only and its direction is not intended to be absolute. Every person documenting in this clinical pathway must supply a sample of their initials and signature below. Signature Log: SW028b ÌSW028bmÎ Not for CABG, Reason:.............................................................. Initials Patient with chest pain ED Chest Pain Medical Assessment Tool Signature Print name Acute Coronary Syndrome suspected/under investigation Cardiac Chest Pain Risk Stratification Pathway Intermediate Risk Chest Pain Clinical Pathway Page 1 of 12 Role Acute Coronary Syndrome diagnosed NSTEACS Mgt. Plan NSTEACS Pathway OR STEMI Mgt. Plan STEMI Pathway STEMI Pathway Interventional Do Not Write in this binding margin Procedures: (Affix identification label here) URN: STEMI Clinical Pathway Family name: (ST-Elevation Myocardial Infarction) Given name(s): For Interventional Cardiac Facilities Address: Date of birth: Sex: M F I Signature Log (continued): Initials Signature Print name Role DO not write in this binding margin Page 2 of 12 (Affix identification label here) URN: STEMI Clinical Pathway Family name: (ST-Elevation Myocardial Infarction) Given name(s): For Interventional Cardiac Facilities Address: Date of birth: All care givers who initial are to sign signature log Medical Key Sex: Nursing Pharmacy M Allied Health Discharge Checklist • Review with patient and carer: Resumption of lifestyle activities (sexual activity, physical activity, return to work) Driving / pilot / commercial licensing Current status, diagnostic and therapeutic options and general prognosis Chest pain home management plan Education and counselling for all current medications • Group Healthy Eating education session attended? Do Not Write in this binding margin Yes (specify): No (refer to community health or outpatient group session) • Given: Written and personalised risk factor control information (smoking, nutrition, diabetes, stress management, high blood pressure and cholesterol) Information on disease process (eg. atherosclerosis) ‘My Heart My Life’ book or similar Written medication information: Consumer Medicines Information Discharge Medication Record (DMR) • Cardiac rehab OPD referral completed? Yes No • Heart Failure Service referral completed? Yes N/A • Stress / Depression identified? Yes No (if Yes, refer to psychologist / social worker) Medications Discharge medications review for: • ACE inhibitors: Indicated? Yes No Given? Yes No Indicated? Yes No Given? Yes No Indicated? Yes No Given? Yes No • Clopidogrel (or alternative): Indicated? Yes No Given? Yes No Yes No Given? Yes No If Not Given, specify reason: • Aspirin: If Not Given, specify reason: • Beta Blockers: Mat. No.: 10206020 SW028b ÌSW028bmÎ v6.00 - 02/2012 If Not Given, specify reason: If Not Given, specify reason: • Statins: Indicated? If Not Given, specify reason: • Sublingual Glyceryl Trinitrate PRN: Supplied at discharge? Yes • Discharge script completed and sent to pharmacy? No (If No, reason: Yes Appointments Patient to make appointment with General Practitioner within one week Cardiologist Other (specify):........................................................ Forms • Medical discharge summary • Travel forms, if required ( not required) • Medical certificate, if required ( not required) Page 3 of 12 No ) I Cardiac Rehab Initials Rehabilitation / Education F Date (Affix identification label here) URN: STEMI Clinical Pathway Family name: (ST-Elevation Myocardial Infarction) Given name(s): For Interventional Cardiac Facilities Address: Date of birth: All care givers who initial are to sign signature log Category Investigations Sex: Medical Key Nursing Emergency (ED) Presentation Date: Day 1 Pharmacy M Allied Health Time: AM Admission to CCU F I Cardiac Rehab PM ND V • ECG on arrival to CCU (right sided ECG V4R if inferior mycoardial infarction), repeat with pain or clinical deterioration and review by MO (observe for signs of reocclusion post PCI) • If had Lysis, conduct ECGs 90 mins 6 hrs and 12 hrs post Lysis N/A • Continuous cardiac monitoring (ST segments if available) • TnI (6–8hrs after presentation) • Request for next day: Medications and Pain Management ELFT TFT FBC COAGS BGL Fasting glucose / Lipids • Check the allergy status of the patient by referring to the medication chart • Record weight and height on medication chart DO not write in this binding margin • Confirm Aspirin given • Confirm Clopidogrel (or alternative) given • Glyceryl Trinitrate prescribed? Yes If Yes, No Contraindicated (eg. Aortic stenosis) Intravenous Sublingual prn • Other intravenous infusions: • Review need for: Observations Treatments Enoxaparin (or alternative) (refer to STEMI Management Plan, p.2, 0-24hrs) IV Heparin (or alternative) • Follow post PCI / Lysis protocol, then if stable Q4H (or as per MO order*) TPR, BP, heart sounds (HS) and breath sounds (BS), SaO2, rhythm check, circulation and pain assessment. Neurological observations post-lysis *Record alternate frequency: • Assess, manage and report chest pain • Blood glucose level (BGL) monitoring - frequency: (if newly diagnosed, refer to Diabetic Educator) N/A • Daily weight and/or fluid balance chart N/A • Check angiogram puncture site N/A • Deep breathing, coughing and leg exercises Nutrition • Healthy Heart diet Other (specify): • If for fasting lipids / glucose, no food after 8pm (may have H2O) Mobility / Elimination / Hygiene N/A • Strict rest in bed for 12 hrs post STEMI (12–24 hours post successful PCI/ Lysis, patient may go to toilet on wheelchair with telemetry [must be supervised], provided they are pain free, and off ionotropic and oxygen therapy) – Record alterations in mobility: • Sponge in bed • Mouth care after meals and prn Other Care (specify) Education and Discharge Plan • Basic explanation to be given of: AMI Diagnostic procedures Mobilisation and bed exercises Risk factors My Heart My Life book or similar Expected Outcomes Patient demonstrates: A - Achieved • Complete patient assessments (eg. falls risk and Waterlow assessment) V - Variance • Painfree • ST segment or T wave changes resolving • Other (specify): Page 4 of 12 A V (Affix identification label here) URN: STEMI Clinical Pathway Family name: (ST-Elevation Myocardial Infarction) Given name(s): For Interventional Cardiac Facilities Address: Date of birth: All care givers who initial are to sign signature log Category Investigations Do Not Write in this binding margin Medications and Pain Management Medical Key Day 2 of pathway Days post STEMI: Sex: Nursing Pharmacy Date: M Allied Health AM Ward: F I Cardiac Rehab PM ND V A V • ECG performed daily, repeat with pain or clinical deterioration and review by MO • Continuous cardiac monitoring • FBC ELFT Fasting Lipids / glucose • Considered for angiography (if Yes, withhold AM subcut anticoagulation, Metformin and others as indicated) Preparation and education completed as per angiogram pathway TnI TFT APTT (if on IV anticoagulation as per protocol/nomogram) • Confirm prescription of Aspirin, Statin, Beta blockers, Clopidogrel (or alternative) and ACE inhibitors • Glyceryl Trinitrate prescribed? Yes If Yes, No Contraindicated (eg. Aortic stenosis) Intravenous Sublingual • Other intravenous infusions: • Review need for: Observations Treatments Enoxaparin (or alternative) (refer to STEMI Management Plan, p.2, 0-24hrs) IV Heparin (or alternative) • 4 hourly (or as per MO order*) temperature, pulse, resps, rhythm check, BP, breath sounds, heart sounds, SaO2 (on room air) and circulation *Record alternate frequency: • Assess, manage and report chest pain • Blood glucose level (BGL) monitoring - frequency: (if newly diagnosed, refer to Diabetic Educator) N/A • Daily weight and/or fluid balance chart, if indicated N/A • Check angiogram puncture site N/A • Patent IVC – change if cubital fossa inserted in DEM/ED (remove if not required) Insertion date: Resite date: • Deep breathing, coughing and leg exercises Nutrition • Healthy Heart diet Other (specify): Mat. No.: 10206020 SW028b ÌSW028bmÎ v6.00 - 02/2012 • If fasting bloods, confirm blood collection before breakfast Mobility / Elimination / Hygiene N/A • Gentle mobilisation, shower with supervision, toilet privileges permitted (if pain free and TnI reducing). - Record alterations in mobility: Other Care (specify) Education and Discharge Plan • Discuss treatment plan with patient / carer Expected Outcomes Patient demonstrates: A - Achieved • Commence discharge checklist on p.3 V - Variance • Painfree • ST segment or T wave changes resolving • Other (specify): Page 5 of 12 (Affix identification label here) URN: STEMI Clinical Pathway Family name: (ST-Elevation Myocardial Infarction) Given name(s): For Interventional Cardiac Facilities Address: Date of birth: All care givers who initial are to sign signature log Category Investigations Medical Key Day 3 of pathway Days post STEMI: Sex: Nursing Date: Pharmacy M Allied Health AM Ward: F I Cardiac Rehab PM ND V A V • ECG performed daily, repeat with pain or clinical deterioration and review by MO • Continuous cardiac monitoring • Telemetry • Monitoring ceased - time: • Daily Bloods as requested (FBC if on IV or subcut antithrombotic) Considered for angiography (if Yes, withhold AM subcut anticoagulation, Metformin and others as indicated) Preparation and education completed as per angiogram pathway • Other test: • Confirm prescription of Aspirin, Statin, Beta blockers, Clopidogrel (or alternative), ACE inhibitors and Sublingual Glyceryl Trinitrate • Other intravenous infusions: • Review need for: Observations Treatments DO not write in this binding margin Medications and Pain Management • Enoxaparin (or alternative) (refer to STEMI Management Plan, p.2, 0-24hrs) IV Heparin (or alternative) • QID or BD as indicated (or as per MO order*) temperature, pulse, resps, rhythm check, BP, breath sounds, heart sounds, SaO2 (on room air) and circulation *Record alternate frequency: • Assess, manage and report chest pain • Blood glucose level (BGL) monitoring - frequency: • Daily weight and/or fluid balance chart, if indicated N/A • Check angiogram puncture site N/A • Patent IVC resite date: Nutrition • Healthy Heart diet OR IVC removed Other (specify): • If fasting bloods, confirm blood collection before breakfast Mobility / Elimination / Hygiene N/A N/A • Increase mobilisation if painfree • Self care Other – Record alterations in mobility/hygiene: Other Care (specify) Education and Discharge Plan • Discuss treatment plan with patient / carer Expected Outcomes Patient demonstrates: A - Achieved • Review discharge checklist on p.3 V - Variance • Painfree • ST segment or T wave changes resolving • Other (specify): Page 6 of 12 (Affix identification label here) URN: STEMI Clinical Pathway Family name: (ST-Elevation Myocardial Infarction) Given name(s): For Interventional Cardiac Facilities Address: Date of birth: All care givers who initial are to sign signature log Category Investigations Medical Key Day 4 of pathway Days post STEMI: Sex: Nursing Date: Pharmacy M Allied Health AM Ward: F I Cardiac Rehab PM ND V A V • ECG performed daily, repeat with pain or clinical deterioration and review by MO • Continuous cardiac monitoring • Telemetry • Monitoring ceased - time: • Daily Bloods as requested (FBC if on IV or subcut antithrombotic) Do Not Write in this binding margin Medications and Pain Management • Considered for angiography (if Yes, withhold AM subcut anticoagulation, Metformin and others as indicated) Preparation and education completed as per angiogram pathway • Other test: • Confirm prescription of Aspirin, Statin, Beta blockers, Clopidogrel (or alternative), ACE inhibitors and Sublingual Glyceryl Trinitrate • Other intravenous infusions: • Review need for: Observations Treatments Enoxaparin (or alternative) (refer to STEMI Management Plan, p.2, 0-24hrs) IV Heparin (or alternative) • QID or BD as indicated (or as per MO order*) temperature, pulse, resps, rhythm check, BP, breath sounds, heart sounds, SaO2 (on room air) and circulation *Record alternate frequency: • Assess, manage and report chest pain • Blood glucose level (BGL) monitoring - frequency: • Daily weight and/or fluid balance chart, if indicated N/A • Check angiogram puncture site N/A • Patent IVC resite date: Nutrition • Healthy Heart diet OR IVC removed Other (specify): Mat. No.: 10206020 SW028b ÌSW028bmÎ v6.00 - 02/2012 • If fasting bloods, confirm blood collection before breakfast Mobility / Elimination / Hygiene N/A N/A • Increase mobilisation if painfree • Self care Other – Record alterations in mobility/hygiene: Other Care (specify) Education and Discharge Plan • Discuss treatment plan with patient / carer Expected Outcomes Patient demonstrates: A - Achieved • Review discharge checklist on p.3 V - Variance • Painfree • ST segment or T wave changes resolving • Other (specify): Page 7 of 12 (Affix identification label here) URN: STEMI Clinical Pathway Family name: (ST-Elevation Myocardial Infarction) Given name(s): For Interventional Cardiac Facilities Address: Date of birth: All care givers who initial are to sign signature log Category Investigations Medical Key Day 5 of pathway Days post STEMI: Sex: Nursing Date: Pharmacy M Allied Health AM Ward: F I Cardiac Rehab PM ND V A V • ECG performed daily, repeat with pain or clinical deterioration and review by MO • Continuous cardiac monitoring • Telemetry • Monitoring ceased - time: • Daily Bloods as requested (FBC if on IV or subcut antithrombotic) Considered for angiography (if Yes, withhold AM subcut anticoagulation, Metformin and others as indicated) Preparation and education completed as per angiogram pathway • Other test: • Confirm prescription of Aspirin, Statin, Beta blockers, Clopidogrel (or alternative), ACE inhibitors and Sublingual Glyceryl Trinitrate • Other intravenous infusions: • Review need for: Observations Treatments DO not write in this binding margin Medications and Pain Management • Enoxaparin (or alternative) (refer to STEMI Management Plan, p.2, 0-24hrs) IV Heparin (or alternative) • QID or BD as indicated (or as per MO order*) temperature, pulse, resps, rhythm check, BP, breath sounds, heart sounds, SaO2 (on room air) and circulation *Record alternate frequency: • Assess, manage and report chest pain • Blood glucose level (BGL) monitoring - frequency: • Daily weight and/or fluid balance chart, if indicated N/A • Check angiogram puncture site N/A • Patent IVC resite date: Nutrition • Healthy Heart diet OR IVC removed Other (specify): • If fasting bloods, confirm blood collection before breakfast Mobility / Elimination / Hygiene N/A N/A • Increase mobilisation if painfree • Self care Other – Record alterations in mobility/hygiene: Other Care (specify) Education and Discharge Plan • Discuss treatment plan with patient / carer Expected Outcomes Patient demonstrates: A - Achieved • Review discharge checklist on p.3 V - Variance • Painfree • ST segment or T wave changes resolving • Other (specify): Page 8 of 12 SW028b ÌSW028bmÎ Mat. No.: 10206020 v6.00 - 02/2012 Do Not Write in this binding margin Insert additional days here if applicable. Page 9 of 12 (Affix identification label here) URN: STEMI Clinical Pathway Family name: (ST-Elevation Myocardial Infarction) Given name(s): For Interventional Cardiac Facilities Address: Date of birth: Sex: M F I Variance Codes Actions A:1 Recurrent chest pain (Differentiate Chest Pain Type; ischaemic, pericarditis or chest wall pain) • • • • • • Administer O2 if indicated – (SaO2 < 93% or evidence of shock) Administer Sublingual Glyceryl Trinitrate Perform ECG MO Review Repeat TnI If re-infarction, consider urgent PCI A:2 Cardiac arrest • • • • • • • • Basic Life Support — CPR Code Blue Advanced Life Support — Defibrillation Basic Life Support — CPR Code Blue Emergency transthoracic pacing, transvenous pacing Basic Life Support — CPR Code Blue A:2.1 Ventricular Fibrillation (VF) or Pulseless Ventricular Tachycardia (VT) A:2.2 Unconscious Complete Heart Block / Asystole A:2.3 Pulseless Electrical Activity A:3 Other arrhythmias: A:3.1 Conscious sustained Ventricular Tachycardia A:3.2 First episode of Atrial Fibrillation (AF) or other Supra Ventricular Tachycardia (SVT) A:3.3 First episode of Heart Block; 2nd or 3rd degree AV Block • Urgent MO review: • Urgent MO review: - unstable patient (hypotensive): call Medical Emergency Team; stable patient within 5 mins unstable patient: within 5 mins; stable patient: 15–60 mins A:11 • Urgent MO review: - unstable patient (hypotensive/syncope): call Medical Emergency Team; - stable patient within 5 mins • Prepare for transthoracic pacing, transvenous pacing Left ventricular failure (with Pulmonary • Sit patient upright Oedema) • Administer O2, consider CPAP / BiPAP • Urgent MO review • Immediate S/L nitrate as bridge to IV titrated nitrates • Morphine PRN • Diuretics • Correction of hypertension with nitrate +/- additional antihypertensive agent • Strict fluid balance chart, consider IDC Pericarditis • MO review • Consider analgesia • Consider echocardiogram Pulmonary embolus (PE) / Deep vein • Urgent MO review thrombosis (DVT) • Anticoagulation • CTPA or VQ Scan +/- Leg Ultrasound • O2 if indicated • Bed rest Renal failure (Significant worsening of renal • Assess volume state and urine output function as defined by rising creatinine or • Urgent MO review; 1–2hrs worsening GFR) • Strict fluid balance chart, consider IDC • Treat hyperkalaemia Pulmonary complications (Cough, sputum • MO review production, fever and pleuritic chest pain) • Chest X-ray • Sputum M/C/S • Assessment for pneumonia • Exclusion of pulmonary embolism Severe nausea • MO review • Consider anti-emetic Adverse drug reactions • MO review • Cease and / or withhold drug ACS medications contraindicated / Withheld • Check with MO A:99 Other A:4 A:5 A:6 A:7 A:8 A:9 A:10 Page 10 of 12 DO not write in this binding margin A. Patient Variances (Affix identification label here) URN: STEMI Clinical Pathway Family name: (ST-Elevation Myocardial Infarction) Given name(s): For Interventional Cardiac Facilities Address: Date of birth: Sex: M F I Do Not Write in this binding margin Variance Codes (continued) A. Patient Variances Actions A:12 Cardiogenic shock (Hypotension with peripheral shutdown and poor urine output, assess age of patient and comorbidities, seek senior medical officer / ICU input early) • • • • • A:13 Haemorrhage A:13.1 Post PCI, access site haematoma / bleed A:13.2 A:13.3 Retro-peritoneal bleeding (hypotension, abdominal pain, poor urine output) Other bleeding A:13.4 Post Lysis (STEMI), change in neurological status A:14 Urgent MO review Consider inotropes Urgent Echocardiogram Fluid balance chart and consider urinary catheter Consider intra-aortic balloon pump • Follow hospital angiogram protocol • • • • • Urgent MO review Frequent neurological observations Cease anti-coagulants CT Head Neurosurgical review Coronary artery bypass surgery B. Discharge / Treatment Delay Variances B:1 Treatment delay B:6 Blood tests delayed B:11 Transfer to private hospital B:2 Delay in transfer B:7 Delay in chest X-ray B:12 Change of plan / orders B:3 No bed available B:8 Delay in stress test B:13 Self discharge B:4 No monitored bed available B:9 Medication not available B:14 Overnight stay B:5 Interdepartmental issues involving care B:10 Patient discharged home off pathway C. Staff Variances C:1 Medical C:2 Nursing C:3 Allied Health C:4 Unable to provide patient education Clinical Events / Variance Variance Code Describe variances to clinical path and any other patient related notes. Document as Variance / Action / Outcome Mat. No.: 10206020 SW028b ÌSW028bmÎ v6.00 - 02/2012 Date / Time Page 11 of 12 Initials (Affix identification label here) URN: STEMI Clinical Pathway Family name: (ST-Elevation Myocardial Infarction) Given name(s): For Interventional Cardiac Facilities Address: Date of birth: Sex: M F I Clinical Events / Variance (continued) Date / Time Variance Code Describe variances to clinical path and any other patient related notes. Document as Variance / Action / Outcome Initials DO not write in this binding margin Page 12 of 12